Abstract
Objectives
American Indian and Alaska Native (AI/AN) communities have been disproportionately affected by the coronavirus disease 2019 (COVID-19) pandemic. This study examines whether neighborhood characteristics mediate AI/AN versus White-non-Hispanic Veteran COVID-19 infection disparities, and whether mediation differs based on proximity to reservations.
Methods
Using Veteran Health Administration’s (VHA) national database of VHA users evaluated for COVID-19 infection (3/1/2020–8/25/2020), we examined whether census tract neighborhood characteristics (percent households overcrowded, without complete plumbing, without kitchen plumbing, and neighborhood socioeconomic status [n-SES]) mediated racial disparities in COVID-19 infection, using inverse odds-weighted logistic models controlling for individual-level characteristics. Using moderated mediation analyses, we assessed whether neighborhood mediating effects on disparities differed for those residing in counties containing/near federally recognized tribal lands (i.e., Contract Health Service Delivery Area [CHSDA] counties) versus not.
Results
The percent of households without complete plumbing, percent without kitchen plumbing, and n-SES partially mediated AI/AN-White-non-Hispanic COVID-19 infection disparities (accounting for 17–35% of disparity) to a similar extent in CHSDA and non-CHSDA counties. The percent of households without kitchen plumbing had stronger mediating effects for CHSDA than non-CHSDA residents.
Conclusions
Neighborhood-level social determinants of health may contribute to the disproportionate COVID-19 infection burden on AI/ANs; differences are exacerbated among AI/ANs living near reservations.
Keywords: COVID-19, Racial, Ethnic disparities, Social determinants of health, Neighborhoods, Veterans
Introduction
American Indian and Alaska Native (AI/AN) communities have been disproportionately affected by the coronavirus disease 2019 (COVID-19) pandemic [1]. The Centers for Disease Control and Prevention (CDC) reported that the incidence of COVID-19 among AI/ANs was 3.5 times that of White non-Hispanic (White-nH) individuals [2]. It is imperative to understand both individual- and macro-level factors that independently contribute to these disparities to inform public health efforts to reduce the devastating effects of COVID-19 among AI/ANs.
There is growing evidence that social determinants of health, including the social and physical characteristics of the neighborhoods where people live (e.g., poverty, segregation, and crowded housing), contribute to COVID-19’s disproportionate impact on racial/ethnic minorities [3–7]. There is less research on the role of neighborhood-level social determinants of health on COVID-19’s impact on AI/ANs [1, 8, 9]. AI/ANs have experienced historical trauma, including European and American colonialism and genocide, displacement from their native lands onto reservations, and forced assimilation through compulsory boarding schools, which have led to higher psychological distress and substance use [10–12]. The enduring effects of these historical traumas and of racism that they continue to experience contribute to a variety of social determinants of health that have deleteriously affected their physical health (e.g., obesity) [13, 14] and likely play a role in COVID-19 disparities. Among these social determinants, the physical and social contexts of the neighborhoods in which AI/ANs live (e.g., high poverty, food deserts) likely contribute to cumulative disadvantages above and beyond individual-level risk factors that exacerbate their risk for COVID-19 relative to other racial/ethnic groups [13, 15].
In particular, neighborhood-level social determinants may mediate disparities in COVID-19 infections among AI/ANs compared to White-nHs. A recent study that examined macro-level social determinant correlates of COVID-19 infections on American Indian reservations found that reservations with a higher proportion of households without plumbing had higher COVID-19 infection rates [1]. This community characteristic may help explain why COVID-19 infections are higher among AI/ANs than White-nHs, since AI/ANs are more likely than White-nHs to live in communities that lack access to running water [16]. A lack of running water presents challenges to frequent handwashing, which is crucial for infection control. Additionally, AI/ANs live in communities with greater socioeconomic disadvantage [17], resulting in limited public health infrastructure and underfunded healthcare resources that may exacerbate COVID-19 infection [1, 18]. A recent ecological study found more COVID-19 cases in zip codes with greater socioeconomic disadvantage and indigenous population concentration in New Mexico [19]. New Mexico has a large American Indian population (11% of the state’s population) that account for a disproportionate share of the state’s COVID-19 cases (> 50% of COVID-19 cases), and contains multiple tribal reservations [19]. AI/ANs also live in communities with a higher percentage of overcrowded households than the US average [17]. This may put them at increased risk of transmission within the households and makes it challenging to social distance [9], especially since a larger proportion of AI/ANs have essential jobs where they need to work in-person compared to groups like White-nHs [20]. However, overcrowded households may also reflect cultural preferences to live in multigenerational households [21]. This practice, which may be more common among households on or near reservations where there are stronger ties to cultural practices, can confer resilience and reinforce collective efforts to protect tribal elders.
It is also possible that neighborhood social determinants’ mediating effects on AI/AN COVID-19 disparities may differ based on whether individuals live on or near reservations versus not, because the social, physical, and cultural contexts are vastly different [22, 23]. For example, while AI/ANs living on or near reservations may be able to benefit from sustained cultural and tribal ties [23], those who do not live near reservations may experience worse health that results from cultural isolation [24]. However, those living on or near reservations frequently travel between tribal and non-tribal lands, which may increase COVID-19 exposure and transmission [23, 25]. Thus, it is important to recognize that there is no monolithic AI/AN experience: while some live on reservations in the most rural regions of the USA, others live in rural towns, suburban cities, and urban metropolises [23, 26], each of which have unique neighborhood contexts that can affect COVID-19 infection. In fact, more than three-quarters of American Indian individuals do not reside on reservations [27], and approximately one-third do not live on or near tribal lands [23]. Most of the focus on AI/AN disparities, although limited, has been among those living on reservations, including a few studies exploring the role of these social factors of Indian reservations on COVID-19 infection [1, 17]. Little is known about COVID-19 infection among AI/ANs not residing on reservations, or how differences in these social and structural factors may aid in understanding AI/AN-White-nH differences in infection risk.
To address these gaps, we take advantage of a national, geographically diverse sample from the Veterans Health Administration (VHA) that includes AI/AN Veterans living on or near reservations and those not living on/near reservations. AI/ANs serve in the US military at five times the national average, providing a robust sample in VHA [28].
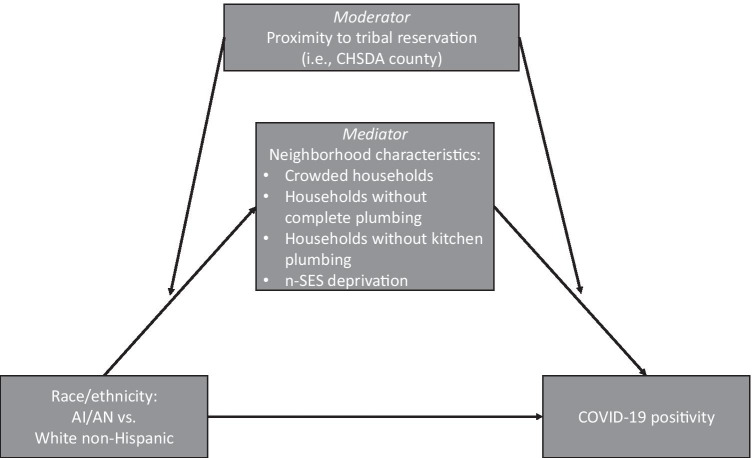
The objective of this analysis was to examine whether the mediating effects of neighborhood characteristics on AI/AN versus White-nH COVID-19 infection disparities differed based on whether or not individuals resided on or near reservations (moderated mediation). Figure 1 illustrates the proposed relationships among these variables. We hypothesized that the magnitudes of the mediating effects of these neighborhood characteristics would differ between those living on or near reservations and those not residing in these communities.
Fig. 1.
Conceptual framework for moderated mediation of neighborhood characteristics and CHSDA county residence on AIAN/White non-Hispanic disparities in COVID-19 infection
Methods
Data and Sample
Individual-level Veteran characteristic data came from VHA’s national database of individual-level information on evaluation and care related to COVID-19 [29], and from VHA’s electronic medical records (VA Corporate Data Warehouse). Neighborhood characteristic data came from the 2014–2018 US Census [30] and were linked to Veteran-level data through census tract identifiers. Our sample included White-nH and AI/AN Veterans who received a COVID-19 test from 3/1/2020 to 8/25/2020 at any VHA site. We excluded Veterans who were also VHA employees.
Measures
Our dependent variable was an indicator of whether Veterans tested positive or negative for COVID-19 based on COVID-19 polymerase chain reaction tests from nasopharyngeal swab specimens measured between 3/1/2020 and 8/25/2020. This is considered the gold standard COVID-19 diagnostic test [31]. For individuals with multiple tests, individuals were considered positive for COVID-19 virus if any of their tests were positive, and negative if all their tests were negative. Our main independent variable was an indicator of Veteran race/ethnicity: White-nH or AI/AN. We determined race/ethnicity from VA administrative data, which was ascertained before the COVID-19 test [32, 33]. We chose White-nH as the comparison group because they consistently had the lowest levels of COVID-19 infections through the pandemic [34], and White-nH individuals largely benefit from systemic racism in medical and healthcare institutions that have put AI/AN individuals at higher risk for COVID-19 [35].
Our moderating variable was a dichotomous county-level indicator of whether Veterans resided in an Indian Health Service (IHS) Contract Health Service Delivery Area (CHSDA) county. IHS defines these counties as those that include all or part of a reservation or any county or counties with a common boundary with a reservation [36]. IHS applies this definition uniformly throughout the USA to determine eligibility for IHS-paid health services. Nationally, nearly two-third of AI/ANs reside in CHSDA counties [37, 38]. CHSDA has been used in other studies to identify areas with a higher concentration of AI/AN residents [15, 37, 39].
Mediating variables included the following neighborhood characteristics from the 2014–2018 US Census: percent overcrowded households (> 1 person per room), percent of households without complete plumbing (lacking one or more of the following: hot/cold running water, flushing toilet, or bathtub/shower), and percent of households without kitchen plumbing (lacking 1 + of the following: sink with a faucet, stove/range, or refrigerator), and neighborhood SES deprivation (n-SES deprivation). We defined n-SES deprivation based on the Agency for Healthcare Research and Quality (AHRQ)’s SES index [40]. This validated index uses a weighted score that combines neighborhood (census tract) measures of median housing value, median household income, and percentages living below the federal poverty line, 25 + years old with at least 4 years of college, 25 + years old with less than a 12th-grade education, unemployed, and overcrowded households. We scaled the score for our sample to a 0–100 range, reverse-coded the score such that higher values indicate greater n-SES deprivation, then created a categorical indicator based on quartiles. A common concern with mediation analyses is the temporal ordering—ensuring that the predictor and mediator variables both precede the outcome variable [41]. In our analysis, both exposure (race/ethnicity) and mediator (neighborhood characteristics) variables preceded the outcome variable (COVID-19 infection).
Control variables included age (< 40 years; 40–59 years; 60–74 years; 75 + years), gender, individual-SES (low SES, high SES, indeterminate/military service-connected), prior diagnosis of one or more CDC-risk factors for severe COVID-19, and time period of COVID test-19 (3/1/2020–5/31/2020 vs. 6/1/2020–8/25/2020). We determined individual-SES from VHA’s enrollment priority group. Individuals with an income below VHA’s threshold for requiring copayment were classified as having low SES. Veterans with military service-connected disability do not have to provide income information to determine their priority group, so they were classified as indeterminate SES. Veterans with prior diagnosis of comorbidities initially identified by the CDC as risk factors for severe COVID-19 (chronic kidney disease stage 5 or end-stage renal disease; chronic pulmonary disease; diabetes; heart disease; immunocompromised state; liver disease; hypertension; and asthma) might alter their behavior to minimize risk of contracting COVID-19; therefore, we included these as covariates. The pandemic, including trends in disparities, evolved over time in response to increased knowledge of the virus and awareness of disparities [34]. For Veterans with multiple COVID-19 tests, we used the date of the first positive test, or first negative test if the Veteran never tested positive, as consistent with VA’s National Surveillance Tool [29].
Statistical Methods
We calculated descriptive statistics of means and proportions for the sample stratified by race/ethnicity and neighborhood characteristics in CHSDA and non-CHSDA counties. We also calculated summary statistics for racial/ethnic and neighborhood area-level characteristics for our sample by IHS region.
Testing moderated mediation involved three steps. First, we estimated the total effect of AI/AN vs. White-nH COVID-19 positivity disparity in both CHSDA and non-CHSDA counties with a logistic regression model that included a race/ethnicity-by-CHSDA residence interaction term and adjusted for potential confounders listed above. The total effects for CHSDA and non-CHSDA residents separately were estimated from the interaction term.
Second, we decomposed each of the total effects into the direct (unmediated) and indirect (mediated by a neighborhood characteristic) effect components. We estimated the direct effect of race/ethnicity for CHSDA and non-CHSDA residents with an inverse-odds-weighted logistic regression model that also included a race/ethnicity-by-CHSDA residence interaction term, while adjusting for the same potential confounders. Before running this logistic regression, it was necessary to derive the inverse-odds weights (IOWs) with Tchetgen Tchetgen’s approach as described by Nguyen 2015’s practical guide [42]. We derived the IOWs by fitting separate logistic regression models (one for each mediator) estimating the relationship between race/ethnicity and a neighborhood mediator in CHSDA and non-CHSDA resident groups with covariate adjustment, and using the resulting coefficients to calculate an IOW for each observation in the AI/AN group (“treatment” group), while each observation in the White-nH group was given an IOW of 1 (“control” group). After this, we estimated the direct effects of race/ethnicity for CHSDA and non-CHSDA residents using the inverse odds-weighted logistic regression model as described above while controlling for the same covariates in the total effect model. We then calculated the indirect effect of race/ethnicity for CHSDA and non-CHSDA residents by subtracting the direct race/ethnicity effect coefficients for CHSDA/non-CHSDA residents from the total race/ethnicity effect coefficients for CHSDA/non-CHSDA residents, and bootstrapping these estimates to obtain standard errors and 95% confidence intervals. We considered there to be evidence of mediation if the indirect effects were statistically significant at p < 0.05. To aid in interpretation, we transformed the total, direct, and indirect effect coefficients into odds ratios and the indirect effect coefficients into the percent of the total effect (i.e., the AI/AN vs. White-nH disparity) that is explained by the mediator of interest (calculated by indirect effect beta coefficient /total effect beta coefficient) [43].
Third, we tested moderated mediation by testing whether the magnitudes of the mediated effects (i.e., indirect effects) for each neighborhood mediator of interest differed between CHSDA and non-CHSDA counties. We considered there to be evidence of moderated mediation if the indirect effect of the neighborhood characteristic of interest was significantly different for CHSDA and non-CHSDA counties at p < 0.05.
All analyses were conducted in Stata version 15.1 (StataCorp, College Station, TX). The work received a Determination of Non-Research from the VA Greater Los Angeles Healthcare System Institutional Review Board.
Results
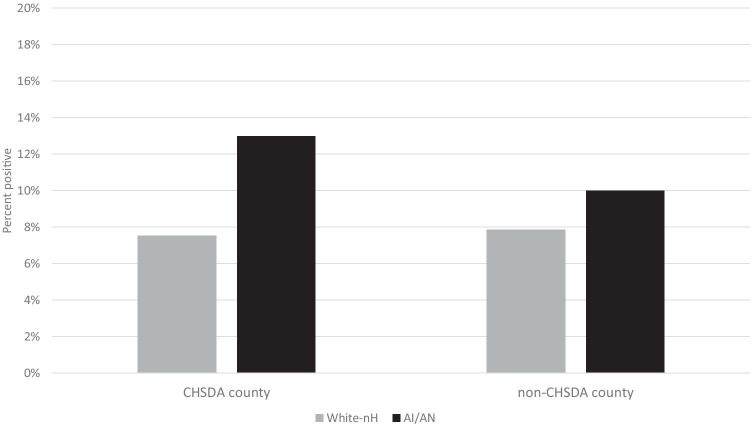
In our sample of 261,981 Veterans, AI/ANs were more likely to be female and younger, and less likely to have high income or any CDC risk factors than White-nHs (Table 1). Approximately 47% of AI/ANs resided in CHSDA counties compared to 25% of White-nHs. Additionally, AI/ANs lived in neighborhoods with a larger proportion of households that lacked complete plumbing, lacked kitchen plumbing, and were overcrowded, and of lower SES. Approximately 8% of our sample tested positive for COVID-19. A larger proportion of AI/ANs tested positive for COVID-19 than Whites-nH overall (11.4% vs 7.8%), and this difference was larger in CHSDA counties (5.5% difference in test positivity) than in non-CHSDA counties (2.2% difference) (Fig. 2).
Table 1.
Sample characteristics by race/ethnicity
| Race/ethnicity | Total (n = 261,981) | |||
|---|---|---|---|---|
| White non-Hispanic (n = 258,936) | AI/AN (n = 3,045) | p-value | ||
| % or mean | % or mean | % or mean | ||
| Sex | ||||
| Female | 9.1% | 15.7% | < 0.001 | 9.2% |
| Male | 90.9% | 84.3% | 90.8% | |
| Age categories | ||||
| < 40 years | 11.4% | 15.0% | < 0.001 | 11.5% |
| 40–59 years | 23.0% | 29.0% | 23.0% | |
| 60–74 years | 44.3% | 42.6% | 44.2% | |
| 75 + years | 21.3% | 13.4% | 21.2% | |
| SES/priority group | ||||
| High income | 11.9% | 8.5% | < 0.001 | 11.9% |
| Low income | 20.0% | 19.5% | 20.0% | |
| Service connected | 68.0% | 72.0% | 68.1% | |
| Any CDC risk factor | ||||
| None | 22.7% | 26.0% | < 0.001 | 22.8% |
| 1 or more risk factors | 77.3% | 74.0% | 77.2% | |
| Date test was conducted | ||||
| March–May, 2020 | 22.3% | 24.3% | 0.007 | 22.3% |
| June–August, 2020 | 77.7% | 75.7% | 77.7% | |
| Neighborhood characteristics | ||||
| Resides in CHSDA county | ||||
| No | 75.3% | 52.7% | < 0.001 | 75.0% |
| Yes | 24.7% | 47.3% | 25.0% | |
| % overcrowded households1, mean (SD) | 2.7 (3.5) | 4.4 (5.3) | < 0.001 | 2.7 (3.5) |
| % households lacking complete plumbing2, mean (SD) | 0.4 (0.4) | 0.8 (1.9) | < 0.001 | 0.4 (0.4) |
| % households lacking kitchen plumbing3, mean (SD) | 0.8 (0.4) | 1.0 (1.3) | < 0.001 | 0.8 (0.4) |
| Neighborhood SES Deprivation Index4 | ||||
| Quartile 1 (highest SES) | 25.1% | 18.6% | < 0.001 | 25.0% |
| Quartile 2 | 25.0% | 20.9% | 25.0% | |
| Quartile 3 | 25.0% | 23.4% | 25.0% | |
| Quartile 4 (lowest SES) | 24.9% | 37.1% | 25.0% | |
| COVID test status | ||||
| Negative | 92.2% | 88.6% | < 0.001 | 92.2% |
| Positive | 7.8% | 11.4% | 7.8% | |
1Overcrowded housing defined as having 1 + person per room
2Lacking complete plumbing defined as households lacking at least one of the following: hot/cold running water, flush toilet, tub/shower
3Lacking kitchen plumbing defined as households lacking at least one of the following: no sink with faucet, stove, refrigerator
4Neighborhood SES (n-SES) deprivation based on AHRQ's neighborhood deprivation index, standardized to 0–100 and reversed coded so that larger numbers indicate greater n-SES deprivation
https://archive.ahrq.gov/research/findings/final-reports/medicareindicators/medicareindicators3.html
Fig. 2.
COVID-19 test positivity by race/ethnicity in CHSDA and non-CHSDA counties from 3/1/2020–8/25/2020
When stratified by CHSDA and non-CHSDA counties (Table 2), differences in neighborhood characteristics between where AI/ANs and non-Hispanic Veterans lived were more pronounced in CHSDA counties. For example, in CHSDA counties, AI/ANs lived in neighborhoods where, on average, 5.6% of households were considered overcrowded, compared to 3.4% for White-nHs. In contrast in non-CSHDA counties, AI/ANs lived in neighborhoods with an average of 3.4% overcrowded households, while White-nHs lived in neighborhoods with an average of 2.5% overcrowded households. While AI/ANs in CHSDA counties lived in neighborhoods with lower SES and a larger proportion of households lacking complete plumbing than White-nHs, these neighborhood characteristics were similar for AI/ANs and White-nHs living in non-CHSDA counties. There were also regional differences in neighborhood characteristics for our sample. In this sample, the mean proportion of overcrowded households was highest in the Pacific Coast followed by Alaska (Appendix Table 4). The mean proportion of households lacking complete and kitchen plumbing was highest in Alaska. Neighborhood SES was lowest in the Southern Plains region. More than 30% of AI/AN and 50% of White-nH Veterans in our sample lived in the East. Alaska had the largest proportion and the East had the smallest proportion of AI/AN Veterans. After Alaska, where all counties are designated as CHSDA counties, the Southwest had the next largest proportion of Veterans residing in CHSDA counties.
Table 2.
Neighborhood characteristics of CHSDA and non-CHSDA counties for AI/AN and White non-Hispanic Veterans
| Neighborhood characteristics | CHSDA counties (n = 65,147) | Non-CHSDA counties (n = 195,394) | ||
|---|---|---|---|---|
| White non-Hispanic Veterans (97.8%) | AI/AN Veterans (2.2%) | White non-Hispanic Veterans (99.2%) | AI/AN Veterans (0.8%) | |
| % overcrowded households1, mean (SD) | 3.4 (3.4) | 5.6 (6.0) | 2.5 (3.3) | 3.4 (4.3) |
| % households lacking complete plumbing2, mean (SD) | 0.4 (0.5) | 1.2 (2.7) | 0.4 (0.3) | 0.4 (0.3) |
| % households lacking kitchen plumbing3, mean (SD) | 0.8 (0.4) | 1.3 (1.8) | 0.8 (0.4) | 0.8 (0.4) |
| Neighborhood SES Deprivation Index4 quartiles, % | ||||
| Quartile 1 (highest SES) | 26.1 | 15.0 | 24.8 | 21.8 |
| Quartile 2 | 25.5 | 18.0 | 24.9 | 23.6 |
| Quartile 3 | 24.4 | 24.8 | 25.2 | 22.2 |
| Quartile 4 (lowest SES) | 24.0 | 42.3 | 25.1 | 32.4 |
1Overcrowded housing defined as having 1 + person per room
2Lacking complete plumbing defined as households lacking at least one of the following: hot/cold running water, flush toilet, tub/shower
3Lacking kitchen plumbing defined as households lacking at least one of the following: no sink with faucet, stove, refrigerator
4Neighborhood SES (n-SES) deprivation based on AHRQ’s neighborhood deprivation index, standardized to 0–100 and reversed coded so that larger numbers indicate lower n-SES deprivation
https://archive.ahrq.gov/research/findings/final-reports/medicareindicators/medicareindicators3.html
Table 4.
Racial ethnic sample composition and neighborhood characteristics by Indian Health Service (IHS) Region1
| Northern Plains | Southern Plains | Southwest | Pacific Coast | East | Alaska | |
|---|---|---|---|---|---|---|
| Racial/ethnic sample characteristic by region | ||||||
| % racial/ethnic sample distribution across regions2 | ||||||
| White-nH | 15.79 | 8.79 | 9.09 | 13.21 | 52.95 | 0.17 |
| AI/AN | 13.22 | 16.67 | 18.00 | 20.21 | 31.30 | 0.59 |
| % of sample that is AI/AN | 0.97 | 2.17 | 2.27 | 1.76 | 0.69 | 3.89 |
| % sample residing in a CHSDA county by race/ethnicity | ||||||
| White-nH | 16.34 | 26.11 | 68.13 | 57.90 | 12.10 | 100.00 |
| AI/AN | 42.40 | 62.48 | 83.49 | 60.92 | 11.75 | 100.00 |
| Neighborhood characteristics by region | ||||||
| % overcrowded households3, mean (SD) | 1.84 (2.18) | 3.42 (3.29) | 3.62 (4.13) | 5.49 (5.99) | 1.99 (2.42) | 5.29 (4.18) |
| % households lacking complete plumbing4, mean (SD) | 0.37 (0.43) | 0.41 (0.27) | 0.41 (0.77) | 0.45 (0.35) | 0.38 (0.28) | 1.93 (2.95) |
| % households lacking kitchen plumbing5, mean (SD) | 0.81 (0.48) | 0.83 (0.33) | 0.76 (0.55) | 0.75 (0.35) | 1.09 (0.52) | 1.69 (2.15) |
| Neighborhood SES Deprivation Index6 quartiles, % | ||||||
| Quartile 1 (highest SES) | 21.52 | 18.69 | 29.56 | 38.12 | 23.11 | 38.12 |
| Quartile 2 | 29.97 | 23.21 | 24.20 | 23.77 | 24.23 | 34.35 |
| Quartile 3 | 29.15 | 26.41 | 20.36 | 18.24 | 25.98 | 17.18 |
| Quartile 4 (lowest SES) | 19.36 | 31.69 | 25.88 | 19.87 | 26.68 | 10.25 |
1States in each of the Indian Health Service regions are as follows: Northern Plains (Illinois, Indiana, Iowa, Michigan, Minnesota, Montana, Nebraska, North Dakota, South Dakota, Wisconsin, Wyoming), Southern Plains (Oklahoma, Kansas, Texas), Southwest (Arizona, Colorado, Nevada, New Mexico, Utah), Pacific Coast (California, Idaho, Oregon, Washington, Hawaii), East (Alabama, Arkansas, Connecticut, Delaware, Florida, Georgia, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Mississippi, Missouri, New Hampshire, New Jersey, New York, North Carolina, Ohio, Pennsylvania, Rhode Island, South Carolina, Tennessee, Vermont, Virginia, West Virginia, District of Columbia), Alaska
2Row percentages for each racial/ethnic group
3Overcrowded housing defined as having 1 + person per room
4Lacking complete plumbing defined as households lacking at least one of the following: hot/cold running water, flush toilet, tub/shower
5Lacking kitchen plumbing defined as households lacking at least one of the following: sink with faucet, stove, refrigerator
6Neighborhood SES (n-SES) deprivation based on AHRQ’s neighborhood deprivation index, standardized to 0–100 and reverse coded so that larger numbers indicate greater n-SES deprivation
https://archive.ahrq.gov/research/findings/final-reports/medicareindicators/medicareindicators3.html
Table 3 presents tests of mediation for those living in CHSDA and non-CHSDA counties and tests of moderated mediation by CHSDA county residence. Overall, we found evidence that the neighborhood characteristics considered in this analysis mediated the AI/AN versus White-nH COVID-19 infection disparities among individuals living in both CHSDA and non-CHSDA counties. In CHSDA counties, three of the four neighborhood characteristics we examined mediated AI/AN disparities. The proportion of households lacking kitchen plumbing had the strongest mediating effect, accounting for nearly 34.0% of the AI/AN vs. White-nH difference in COVID-19 positivity (calculated using beta coefficients from the moderated mediation analysis presented in Appendix Table 5 as follows: 0.236 [indirect effect β]/0.696 [total effect β]; followed by the proportion of households lacking complete plumbing), which accounted for 24.5% of the total effect disparity, and finally n-SES deprivation, accounting for 17.1% of the total effect disparity.
Table 3.
Moderated mediation of neighborhood characteristics on AI/AN vs. White non-Hispanic COVID-19 infection disparities, by CHSDA county residence
| CHSDA counties | Non-CHSDA counties | CHSDA vs non-CHSDA moderated mediation | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Neighborhood characteristic mediators | Total effect OR (95% CI) |
Direct effect OR (95% CI) |
Indirect effect OR (95% CI) |
% explained by mediator | Total effect OR (95% CI) |
Direct effect OR (95% CI) |
Indirect effect OR (95% CI) |
% explained by mediator | Difference in indirect effect OR (95% CI) | p-value |
| % overcrowded households | 1.91 (1.53, 2.10)a | 1.66 (1.36, 1.96)a | 1.09 (0.99, 1.19) | 14.8% | 1.31 (1.10, 1.52)b | 1.20 (0.99, 1.41)c | 1.09 (1.01, 1.18)c | 33.3% | 0.998 (0.88, 1.12) | 0.970 |
| % households lacking complete plumbing | 1.87 (1.58, 2.17)a | 1.61 (1.30, 1.92)a | 1.17 (1.05, 1.28)b | 24.5% | 1.33 (1.11, 1.55)b | 1.23 (1.01, 1.44)c | 1.09 (1.01, 1.16)c | 29.0% | 1.07 (0.94, 1.20) | 0.245 |
| % households lacking kitchen plumbing | 2.00 (1.68, 2.33)a | 1.58 (1.28, 1.99)a | 1.27 (1.13, 1.41)a | 34.0% | 1.33 (1.11, 1.55)b | 1.22 (1.01, 1.44)c | 1.09 (1.01, 1.16)c | 28.6% | 1.17 (1.01, 1.32) | 0.018 |
| Neighborhood deprivation SES | 1.85 (1.56, 2.15)a | 1.67 (1.36, 1.97)a | 1.11 (1.003, 1.23)c | 17.1% | 1.33 (1.12, 1.54)a | 1.20 (0.999, 1.41)c | 1.10 (1.03, 1.18)b | 34.9% | 1.006 (0.88, 1.13) | 0.919 |
ap < 0.001
bp < 0.005
cp < 0.05
Bold denotes statistically significant effects at p < 0.05. Significant indirect effects indicate significant mediation effects. Each neighborhood characteristic was modeled separately. Models controlled for sex, age, individual SES, having a CDC risk factor, and the date test was conducted
Table 5.
Beta coefficients from moderated mediation analysis
| CHSDA counties | Non-CHSDA counties | |||||
|---|---|---|---|---|---|---|
| Neighborhood characteristic mediators | Total effect Β coefficient |
Direct effect Β coefficient | Indirect effect Β coefficient |
Total effect Β coefficient |
Direct effect Β coefficient |
Indirect effect Β coefficient |
| % overcrowded households | 0.594 | 0.507 | 0.088 | 0.271 | 0.181 | 0.090 |
| % households lacking complete plumbing | 0.628 | 0.474 | 0.154 | 0.286 | 0.203 | 0.083 |
| % households lacking kitchen plumbing | 0.696 | 0.459 | 0.236 | 0.288 | 0.206 | 0.082 |
| Neighborhood deprivation SES | 0.617 | 0.511 | 0.105 | 0.283 | 0.184 | 0.099 |
Each neighborhood characteristic was modeled separately. Models controlled for sex, age, individual SES, having a CDC risk factor, and the date test was conducted
In non-CHSDA counties, all four neighborhood characteristics mediated the AI/AN disparity. N-SES deprivation had the strongest mediating effect and accounted for 34.9% of the COVID-19 positivity disparity, followed closely by the proportion of overcrowded households, accounting for 33.3% of the disparity. The proportion of households lacking complete plumbing accounted for 29.0% of the disparity, and lastly, the proportion of household lacking kitchen plumbing’s mediating effect accounted for 28.6% of the disparity.
We found evidence of moderated mediation by CHSDA county residence for one of the neighborhood characteristics (Table 3). The proportion of households lacking kitchen plumbing had a stronger mediating effect on the AI/AN vs. White-nH COVID-19 positivity disparity for those living in CHSDA counties than those who did not (OR difference between CHSDA vs. non-CHSDA indirect effects: 1.17, 95% CI: 1.01, 1.32, p-value = 0.018). Expressed as percentages of the AI/AN vs. White-nH COVID-19 positivity disparity, the mediating effect of the proportion of households lacking kitchen plumbing on the COVID-19 positivity disparity among AI/ANs was 5.4 percentage points larger in CHSDA counties than in non-CHSDA counties. For the other neighborhood characteristics, mediating effects were not statistically significantly different for CHSDA and non-CHSDA counties.
Discussion
In this study, we found disparities in COVID-19 infections for AI/ANs relative to White-nHs among both CHSDA and non-CHSDA county residents. Several neighborhood characteristics, including the proportion of households lacking complete plumbing or kitchen plumbing, and n-SES deprivation, mediated these disparities in both CHSDA and non-CHSDA counties, above and beyond differences in individual characteristics. However, statistically significant differences between AI/AN and White-nH groups remained, with AI/ANs having higher odds of infection than White-nHs. We found evidence of moderated mediation for the neighborhood characteristic proportion of households lacking kitchen plumbing, with a stronger mediating effect on AI/AN vs. White-nH COVID-19 disparities among those who lived in CHSDA counties than those not living in these counties.
We found that some of the neighborhood characteristics previously identified as correlates of higher COVID-19 infections on Indian Reservations [1] also explained higher COVID-19 infections in AI/ANs compared to White-nHs for residents of both CHSDA and non-CHSDA counties. Specifically, neighborhoods with a larger proportion of households that lack complete plumbing and greater n-SES deprivation partially accounted for these disparities, with similar mediating effect sizes in both CHSDA and non-CHSDA counties. Households without complete plumbing, particularly running water, experience challenges to following CDC’s recommendations for COVID-19 prevention, such as frequent handwashing, and may rely on communal bathrooms for personal hygiene. These households also risk exposure when they go to stores to purchase bottled water or haul water from communal wells. This social determinant may similarly play a role in higher AI/AN COVID-19 infections in non-CHSDA counties, as urban Indians are also more likely to live in households that lack plumbing facilities [26]. Living in lower SES communities is associated with worse health, including higher risk of COVID-19 [44]. The COVID-19 infection disparity for AI/ANs may be explained in part by the fact that AI/ANs, both living on reservations or in urban areas, tend to live in more impoverished neighborhoods than White-nHs [26, 45].
We found that living in neighborhoods with more households lacking kitchen plumbing also accounted for the AI/AN vs. White-nH COVID-19 infection disparities. While this neighborhood characteristic had a mediating effect on those living in both CHSDA and non-CHSDA counties, the effect was stronger in CHSDA counties. There are several possible mechanisms through which this neighborhood characteristic may mediate the AI/AN-White-nH disparity. Lacking kitchen plumbing may be an indicator of greater food insecurity. A recent study of low-income adults in the USA found that those experiencing very high food insecurity experienced challenges in following initial public health guidance to stock up on 2 weeks of food to limit grocery store trips and promote social distancing [46]. Households that lack kitchen plumbing may be at higher risk for COVID-19 exposure if they lack the ability to store (without refrigerators) or prepare (without stove/range) food, which requires more trips to acquire food or to rely on neighbors or community members for meals. Additionally, communities with more food-insecure households may rely on food pantries/food banks, which may have challenges in implementing social distancing measures. AI/ANs, in general, are more likely to experience food insecurity compared to other racial/ethnic groups [47]. The effect of multiple disadvantages—being AI/AN, living in neighborhoods with more food insecure households, in CHSDA counties—may put these individuals at even higher risk for COVID-19 infection. CHSDA counties may have greater residential segregation between AI/ANs and White-nHs [15], where AI/ANs may be more likely to live on or very close to reservations with higher levels of food insecurity [48], while White-nHs may live in separate, less food-insecure communities. Moreover, previous research found that AI/ANs living on reservations must travel further to grocery stores compared to other low-income individuals nationally [49], which may suggest fewer grocery stores and other food resources in rural communities on or near reservations. Conversely, AI/AN and White-nH Veterans in non-CHSDA counties may live in more integrated communities with similar neighborhood exposures for both groups.
Prior research has found that living in communities with larger household size is related to higher rates of COVID-19 infections [50], while another study found that on reservations, the proportion of crowded households was not associated with COVID-19 infections [1]. In this sample of VHA users, the proportion of crowded housing in the neighborhood mediated AI/AN vs. White-nH COVID-19 disparities for those living in non-CHSDA counties. Greater mediating effects for AI/AN Veterans of non-CHSDA county residence in neighborhoods with a high percent of crowded households may also be related to lack of geographic proximity to reservations and their cultural and economic resources from other AI/AN individuals.
Limitations to this study include potential race/ethnicity misclassification, especially for AI/ANs living in non-CHSDA counties [38]; this may have biased our comparisons toward the null. Additionally, our study focused on Veteran VHA users, who are generally older and sicker than the general population; however, our analyses adjusted for age and comorbidity. We defined neighborhoods based on census tracts, but this may differ from lived experiences of study participants, especially in rural areas where census tracts may cover large geographic areas. The most recent census tract data came from 2014–2018, but neighborhood characteristics may have changed. We could not disaggregate American Indian and Alaska Native Veterans as these groups are combined in accordance with the Office of Budget and Management’s standards for classifying race and ethnicity [51]. Lastly, our cross-sectional study design precludes a strict causal interpretation.
Public Health Impacts
Our study adds to limited, though growing, evidence that some neighborhood-level social determinants of health explain part of the disparity in COVID-19 infection between AI/AN Veterans and White-nH Veterans. Additional research is needed to identify other social determinants—at both the individual and more macro-levels—that contribute to the increased burden of COVID-19 on AI/ANs. Although research has primarily focused on the COVID-19 pandemic’s effects on AI/ANs living on reservations, we found that some neighborhood-level social determinants also have a detrimental effect on AI/ANs who do not live on or near reservations. While tribe nations have implemented their own COVID-19 mitigation on reservations (e.g., Navajo Nation’s strict safer at home measures, including weekend lockdowns and closing roads to visitors [52], and extensive contact tracing by IHS, tribal leaders, and local hospital leaders [53]), those who do not reside near tribal lands likely do not benefit from these efforts. It is important that VHA, IHS, and state and local health departments provide culturally appropriate messaging to AI/ANs residing away from reservations on how they can protect themselves from COVID-19, including the importance of handwashing and social distancing in crowded, multigenerational households, and following other national public health recommendations. Moreover, national public health strategies for COVID-19 mitigation, testing, and vaccination should focus on AI/AN communities.
More research is needed to better understand underlying mechanisms through which the proportion of households that lack kitchen plumbing in the neighborhood explains AI/AN disparities in COVID-19 infections. We posit one potential underlying mechanism: food insecurity. VA has implemented a clinical reminder for food insecurity screening, and refers those who screen positive to a multidisciplinary team (including social worker, dietician, and clinician) that offers tailored interventions [54]. VA can use clinical reminder information to identify AI/AN Veterans who have previously been identified as food insecure and, through their multidisciplinary and tailored approach, help these Veterans obtain food while protecting themselves from COVID-19. This may be especially important for Veterans who live in non-CHSDA counties.
Appendix
Author Contribution
M. S. W., D. M. U., and D. L. W. conceived of the analysis. A. H. Y. and T. P. H. obtained and managed the data. W. N. S. conducted the analysis. M. S. W. interpreted the results and drafted the manuscript. All authors were involved in the review and editing of the manuscript.
Funding
This work was supported by the VA Office of Health Equity (OHE) and VA Quality Enhancement Research Initiative (QUERI) through grant no. PEC-15–239 to the OHE/QUERI National Partnered Evaluation Center, and by VA HSR&D (no. IIR-17–289 and no. SDR-20–402).
Data Availability
Data from this study are not publicly available due to patient confidentiality.
Declarations
Conflict of Interest
The authors declare no competing interests.
Ethical Approval
The work received a Determination of Non-Research from the VA Greater Los Angeles Healthcare System Institutional Review Board.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rodriguez-Lonebear D, Barceló NE, Akee R, Carroll SR. American Indian Reservations and COVID-19: Correlates of early infection rates in the pandemic. J Public Health Manag Pract. 2020;26(4):371–377. doi: 10.1097/PHH.0000000000001206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hatcher SM, Agnew-Brune C, Anderson M, Zambrano LD, Rose CE, Jim MA, et al. COVID-19 Among American Indian and Alaska Native Persons - 23 States, January 31-July 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(34):1166–1169. doi: 10.15585/mmwr.mm6934e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bryan MS, Sun J, Jagai J, Horton DE, Montgomery A, Sargis R, et al. COVID-19 mortality and neighborhood characteristics in Chicago. Ann Epidemiol. 2020 doi: 10.1016/j.annepidem.2020.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hatef E, Chang HY, Kitchen C, Weiner JP, Kharrazi H. Assessing the impact of neighborhood socioeconomic characteristics on COVID-19 prevalence across seven states in the United States. Front Public Health. 2020;8:571808. doi: 10.3389/fpubh.2020.571808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ingraham NE, Purcell LN, Karam BS, Dudley RA, Usher MG, Warlick CA, et al. Racial/ethnic disparities in hospital admissions from COVID-19 and determining the impact of neighborhood deprivation and primary language. medRxiv. 2020. 10.1101/2020.09.02.20185983. [DOI] [PMC free article] [PubMed]
- 6.Abedi V, Olulana O, Avula V, Chaudhary D, Khan A, Shahjouei S, et al. Racial, economic, and health inequality and COVID-19 infection in the United States. J Racial Ethn Health Disparities. 2020:1–11. 10.1007/s40615-020-00833-4. [DOI] [PMC free article] [PubMed]
- 7.Dalsania AK, Fastiggi MJ, Kahlam A, Shah R, Patel K, Shiau S, et al. The relationship between social determinants of health and racial disparities in COVID-19 mortality. J Racial Ethn Health Disparities. 2021:1–8. 10.1007/s40615-020-00952-y. [DOI] [PMC free article] [PubMed]
- 8.Raine S, Liu A, Mintz J, Wahood W, Huntley K, Haffizulla F. Racial and ethnic disparities in COVID-19 outcomes: social determination of health. Int J Environ Res Public Health. 2020;17(21):8115. doi: 10.3390/ijerph17218115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kakol M, Upson D, Sood A. Susceptibility of Southwestern American Indian tribes to coronavirus disease 2019 (COVID-19). J Rural Health. 2019;2020. 10.1111/jrh.12451. [DOI] [PMC free article] [PubMed]
- 10.Guenzel N, Struwe L. Historical trauma, ethnic experience, and mental health in a sample of urban American Indians. J Am Psychiatr Nurses Assoc. 2020;26(2):145–156. doi: 10.1177/1078390319888266. [DOI] [PubMed] [Google Scholar]
- 11.Gone JP, Hartmann WE, Pomerville A, Wendt DC, Klem SH, Burrage RL. The impact of historical trauma on health outcomes for indigenous populations in the USA and Canada: a systematic review. Am Psychol. 2019;74(1):20–35. doi: 10.1037/amp0000338. [DOI] [PubMed] [Google Scholar]
- 12.John-Henderson NA, Ginty AT. Historical trauma and social support as predictors of psychological stress responses in American Indian adults during the COVID-19 pandemic. J Psychosom Res. 2020;139:110263. doi: 10.1016/j.jpsychores.2020.110263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Warne D, Wescott S. Social determinants of American Indian Nutritional Health. Curr Dev Nutr. 2019;3(Suppl 2):12–18. doi: 10.1093/cdn/nzz054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cobb N, Espey D, King J. Health behaviors and risk factors among American Indians and Alaska Natives, 2000–2010. Am J Public Health. 2014;104(Suppl 3):S481–9. doi: 10.2105/ajph.2014.301879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong MS, Steers WN, Hoggatt KJ, Ziaeian B, Washington DL. Relationship of neighborhood social determinants of health on racial/ethnic mortality disparities in US veterans-Mediation and moderating effects. Health Serv Res. 2020;55(Suppl 2):851–62. doi: 10.1111/1475-6773.13547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deitz S, Meehan K. Plumbing poverty: mapping hot spots of racial and geographic inequality in U.S. household water insecurity. Ann Am Assoc Geogr. 2019;109(4):1092–109. doi: 10.1080/24694452.2018.1530587. [DOI] [Google Scholar]
- 17.Hathaway ED. American Indian and Alaska Native people: social vulnerability and COVID-19. J Rural Health. 2021;37(1):256–259. doi: 10.1111/jrh.12505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hu T, Yue H, Wang C, She B, Ye X, Liu R, et al. Racial segregation, testing site access, and COVID-19 incidence rate in Massachusetts, USA. Int J Environ Res Public Health. 2020;17(24). 10.3390/ijerph17249528. [DOI] [PMC free article] [PubMed]
- 19.Huyser KR, Yang T-C, Yellow Horse AJ. Indigenous peoples, concentrated disadvantage, and income inequality in New Mexico: a ZIP code-level investigation of spatially varying associations between socioeconomic disadvantages and confirmed COVID-19 cases. J Epidemiol Community Health. 2021:jech-2020–215055. 10.1136/jech-2020-215055. [DOI] [PubMed]
- 20.Dubay L, Aarons J, Brown KS, Kenney GM. How risk of exposure to the coronavirus at work varies by race and ethnicity and how to protect the health and well-being of workers and their families. Washington, DC: Urban Institute; 2020. [Google Scholar]
- 21.National Congress of American Indians Policy Researh Center. A place we call home: what is the future of tribal housing? . In: Indians NCoA, editor. 2017.
- 22.Huyser KR, Sakamoto A, Takei I. The persistence of racial disadvantage: the socioeconomic attainments of single-race and multi-race Native Americans. Popul Res Policy Rev. 2010;29(4):541–568. doi: 10.1007/s11113-009-9159-0. [DOI] [Google Scholar]
- 23.Dewees S, Marks B. Research notes - twice invisible: understanding rural native America. Longmont: First Nations Development Institute; 2017. [Google Scholar]
- 24.Brown RA, Dickerson DL, D’Amico EJ. Cultural identity among urban American Indian/Alaska Native Youth: implications for alcohol and drug use. Prev Sci. 2016;17(7):852–861. doi: 10.1007/s11121-016-0680-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnston J. Where water is scarce on Native American reservations Covid-19 spreads more easily. 2020. https://www.circleofblue.org/2020/world/where-water-is-scarce-on-native-american-reservations-covid-19-spreads-more-easily/. Accessed June 2, 2021.
- 26.National Urban Indian Family Coalition. Urban Indian America: the Status of American Indian & Alaskan Native Children & Families Today. 2008.
- 27.U.S. Department of Health and Human Serivces Office of Minority Health. Profile: American Indian/Alaskan Native. 2018. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=62#:~:text=This%20racial%20group%20comprises%201.7,reservations%20or%20other%20trust%20lands. Accessed December 21, 2020.
- 28.DeSimone D. A history of military service: Native Americans in the US. Military Yesterday and Today. 2020. https://www.uso.org/stories/2914-a-history-of-military-service-native-americans-in-the-u-s-military-yesterday-and-today. Accessed June 15, 2021.
- 29.VA Informatics and Computing Infrastructure. VA COVID_19 Shared Data Resource. 2020.
- 30.U.S. Census Bureau. 2014–2018 American Community Survey 5-year Estimates. 2018.
- 31.Karam M, Althuwaikh S, Alazemi M, Abul A, Hayre A, Alsaif A, et al. Chest CT versus RT-PCR for the detection of COVID-19: systematic review and meta-analysis of comparative studies. JRSM Open. 2021;12(5):20542704211011837. doi: 10.1177/20542704211011837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saechao FS, Frayne SM. Veteran Health Equity Report–FY2013. Technical Appendix. Washington, DC: U.S. Department of Veterans Affairs; 2016. [Google Scholar]
- 33.Washington DL. Using VA data to characterize health and healthcare disparities in VA. VA Cyberseminar Series: Using Data and Information Systems in Partnered Research. 2017. p. https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/video_archive.cfm?SessionID=2318.
- 34.Wong MS, Haderlein TP, Yuan AH, Moy E, Jones KT, Washington DL. Time Trends in racial/ethnic differences in COVID-19 infection and mortality. Int J Environ Res Public Health. 2021;18(9). 10.3390/ijerph18094848. [DOI] [PMC free article] [PubMed]
- 35.Sabatello M, Jackson Scroggins M, Goto G, Santiago A, McCormick A, Morris KJ, et al. Structural racism in the COVID-19 pandemic: moving forward. Am J Bioeth. 2021;21(3):56–74. doi: 10.1080/15265161.2020.1851808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Johnson T. Contract Health Services. 2013. https://www.ihs.gov/california/tasks/sites/default/assets/File/BP2013-CHS101-Johnson.pdf. Accessed.
- 37.Perdue DG, Haverkamp D, Perkins C, Daley CM, Provost E. Geographic variation in colorectal cancer incidence and mortality, age of onset, and stage at diagnosis among American Indian and Alaska Native people, 1990–2009. Am J Public Health. 2014;104(Suppl 3):S404–14. doi: 10.2105/ajph.2013.301654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Espey DK, Jim MA, Richards TB, Begay C, Haverkamp D, Roberts D. Methods for improving the quality and completeness of mortality data for American Indians and Alaska Natives. Am J Public Health. 2014;104(Suppl 3):S286–S94. doi: 10.2105/AJPH.2013.301716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jim MA, Arias E, Seneca DS, Hoopes MJ, Jim CC, Johnson NJ, et al. Racial misclassification of American Indians and Alaska Natives by Indian Health Service Contract Health Service Delivery Area. Am J Public Health. 2014;104(Suppl 3):S295–302. doi: 10.2105/ajph.2014.301933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bonito A, Bann C, Eicheldinger C, Carpenter L. Creation of new race-ethnicity codes and socioeconomic status (SES) indicators for Medicare beneficiaries final report. Rockville: Agency for Healthcare Resarch and Quality; 2008.
- 41.Fairchild AJ, McDaniel HL. Best (but oft-forgotten) practices: mediation analysis. Am J Clin Nutr. 2017;105(6):1259–1271. doi: 10.3945/ajcn.117.152546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nguyen QC, Osypuk TL, Schmidt NM, Glymour MM, Tchetgen Tchetgen EJ. Practical guidance for conducting mediation analysis with multiple mediators using inverse odds ratio weighting. Am J Epidemiol. 2015;181(5):349–356. doi: 10.1093/aje/kwu278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nguyen TT, Tchetgen Tchetgen EJ, Kawachi I, Gilman SE, Walter S, Glymour MM. The role of literacy in the association between educational attainment and depressive symptoms. SSM Popul Health. 2017;3:586–593. doi: 10.1016/j.ssmph.2017.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Madhav KC, Oral E, Straif-Bourgeois S, Rung AL, Peters ES. The effect of area deprivation on COVID-19 risk in Louisiana. PLoS One. 2020;15(12):e0243028. doi: 10.1371/journal.pone.0243028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sarche M, Spicer P. Poverty and health disparities for American Indian and Alaska Native children: current knowledge and future prospects. Ann N Y Acad Sci. 2008;1136:126–136. doi: 10.1196/annals.1425.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wolfson JA, Leung CW. Food insecurity and COVID-19: disparities in early effects for US adults. Nutrients. 2020;12(6):1648. doi: 10.3390/nu12061648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jernigan VBB, Huyser KR, Valdes J, Simonds VW. Food insecurity among American Indians and Alaska Natives: a national profile using the Current Population Survey-Food Security Supplement. J Hunger Environ Nutr. 2017;12(1):1–10. doi: 10.1080/19320248.2016.1227750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pindus N, Hafford C. Food security and access to healthy foods in Indian country: learning from the Food Distribution Program on Indian Reservations. J Public Aff. 2019;19(3):e1876. doi: 10.1002/pa.1876. [DOI] [Google Scholar]
- 49.Kaufman P, Dicken C, Williams R. Measuring access to healthful, affordable food in American Indian and Alaska Native Tribal Areas. Economic Information Bulletin Number 1312014.
- 50.Figueroa JF, Wadhera RK, Lee D, Yeh RW, Sommers BD. Community-level factors associated with racial and ethnic disparities in COVID-19 rates in Massachusetts. Health Aff (Millwood) 2020;39(11):1984–1992. doi: 10.1377/hlthaff.2020.01040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Office of Management and Budget. Revisions to the Standards for the Classification of Federal Data on race and ethnicity. Federal Register;1997.
- 52.Navajo Nation Government. Welcome to the Navajo Nation Government - Coronavirus Information. 2021. https://www.navajo-nsn.gov/. Accessed January 15, 2021.
- 53.Close RM, Stone MJ. Contact tracing for Native Americans in Rural Arizona. N Engl J Med. 2020;383(3):e15. doi: 10.1056/NEJMc2023540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cohen AJ, Rudolph JL, Thomas KS, Archambault E, Bowman MM, Going C, et al. Food insecurity among veterans: resources to screen and intervene. Fed Pract. 2020;37(1):16–23. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data from this study are not publicly available due to patient confidentiality.