Abstract
Objectives
To examine associations between preoperative fear-avoidance model (FAM) risk subgroup status and patient expectation of surgical success with postoperative outcomes at 6 and 12 months after anterior cruciate ligament reconstruction (ACLR).
Design
Cohort study.
Setting
Academic medical center.
Participants
54 patients (25 females) undergoing unilateral ACLR.
Main Outcome Measures
Cluster analysis distinguished FAM risk subgroups based on preoperative fear of movement/reinjury, self-efficacy, and pain catastrophizing. Preoperative expectation for surgical success was assessed with a numeric rating scale. Six and 12-month outcomes included Subjective Patient Outcomes for Return to Sport, Knee Injury and Osteoarthritis Outcome Score (KOOS) sports/recreation and quality of life, and International Knee Documentation Committee (IKDC) Subjective Knee Form.
Results
Thirteen (24%) patients were “moderate-to-high FAM risk.” Moderate-to-high FAM risk patients had lower odds of return to sport at 12 months (OR=.3, p=.05) and lower KOOS sports/recreation at 6 months (st. beta=−.27, p=.05), KOOS quality of life at 12 months (st. beta=−.42, p=.007), and IKDC at 6 (st. beta=−.29, p=.04) and 12 months (st. beta=−.47, p=.001). Higher expectation was associated with lower 6-month IKDC (st. beta=−.36, p=.008) and 12-month KOOS quality of life (st. beta=−0.29, p=.05).
Conclusions
Preoperative FAM risk influences patient-reported outcomes and return to sport at 6 and 12 months.
Keywords: Knee injuries, patient expectations, psychological adaptation, return to sport
INTRODUCTION
Psychosocial characteristics are risk factors for poor rates of return to sport and patient-reported outcomes after anterior cruciate ligament reconstruction (ACLR) (Ardern, 2015; Ardern, Taylor, Feller, & Webster, 2013; Forsdyke, Smith, Jones, & Gledhill, 2016; Hsu, Meierbachtol, George, & Chmielewski, 2017). Several authors have highlighted fear-avoidance model (FAM) factors such as fear of movement/reinjury, pain catastrophizing, and self-efficacy for their associations with recovery after ACLR (Ardern, 2015; Chmielewski & George, 2019; Nwachukwu et al., 2019; te Wierike, van der Sluis, van den Akker-Scheek, Elferink-Gemser, & Visscher, 2013). The majority of ACLR studies investigating psychosocial factors have been cross-sectional (Beischer, Hamrin Senorski, Thomee, Samuelsson, & Thomee, 2019; Lentz et al., 2009; Lentz et al., 2012; Tripp, Stanish, Ebel-Lam, Brewer, & Birchard, 2007) or examined associations over the postoperative period (Ardern, Taylor, Feller, Whitehead, & Webster, 2015; Chmielewski et al., 2011; Hamrin Senorski et al., 2017; Langford, Webster, & Feller, 2009; Lentz et al., 2015; McCullough et al., 2012; Nwachukwu et al., 2019; Paterno, Flynn, Thomas, & Schmitt, 2018), which limits conclusions related to preoperative screening or prognosis. Additionally, few studies have examined preoperative FAM risk factors and their relationship with return to sport or activity (Ardern, Taylor, Feller, Whitehead, & Webster, 2013; Thomee et al., 2008). Ardern et al. (2013) found preoperative fear of movement/reinjury and psychological readiness were significant predictors of return to sport, while Thomee et al. (2008) found significant associations between preoperative self-efficacy and 1-year physical activity. There remains a significant knowledge gap regarding preoperative risk based on FAM factors for return to sport after ACLR. Individual self-report measures representing single psychosocial constructs are often used to determine relationships between preoperative FAM factors and postoperative outcomes. Examining more complex profiles may provide additional insight into FAM risk factor influence. Clustering methods consider the composite influence of multiple psychosocial factors through subgrouping based on similar cohort characteristics. An empirically-derived psychosocial cluster approach has been undertaken in patients with low back pain (Beneciuk, Robinson, & George, 2012, 2015; Nisenzon et al., 2014; Rabey, Smith, Beales, Slater, & O’Sullivan, 2016) and chronic pain (Boersma & Linton, 2006; Larsson, Gerdle, Bernfort, Levin, & Dragioti, 2017; Widerstrom-Noga, Felix, Cruz-Almeida, & Turk, 2007). Examining the influence of a preoperative FAM risk subgroup rather than only single FAM measures on ACLR outcomes has the potential to provide a more comprehensive prognostic assessment.
A related and rarely studied contextual factor is preoperative expectation of surgical recovery. While not a central tenet within the FAM, patient expectations predict functional outcomes in various orthopaedic surgery populations (Bialosky, Bishop, & Cleland, 2010; Coronado, Seitz, Pelote, Archer, & Jain, 2018; Yee, Adjei, Do, Ford, & Finkelstein, 2008). A greater understanding of the relative influence of preoperative FAM factors and expectation for surgical success on ACLR recovery can potentially form optimal screening methods for identifying athletes at risk for not returning to sport. Such screening methods can also inform risk mitigation strategies.
The primary objective of this study was to examine the association between preoperative composite FAM risk (fear of movement/reinjury, self-efficacy, pain catastrophizing) and patient-reported ACLR outcomes at 6 and 12 months using a cluster-based approach. Our secondary objective was to examine the association of preoperative patient expectation for surgical success and 6- and 12-month patient-reported outcomes. We hypothesized that higher FAM risk status and patient expectation for surgical success would be associated with poor return to sport, sports participation, knee function, and quality of life after ACLR.
MATERIAL AND METHODS
Study Design
This was a prospective cohort study of patients undergoing primary unilateral ACLR. The Institutional Review Board of Vanderbilt University Medical Center approved the study.
Patients
Consecutive English-speaking patients, between the ages of 12 and 33 years, were recruited preoperatively over a 14-month period from a single academic medical center. Inclusion criteria were: 1) enrollment into the parent Multicenter Orthopaedic Outcomes Network (MOON) study (Wright et al., 2007); 2) undergoing primary unilateral ACLR; 3) injured while playing a sport; and 4) no history of prior surgery to either knee. Patients undergoing simultaneous bilateral ACLR, revision ACLR, or surgical repair of additional knee ligaments were excluded.
Procedures
After obtaining written informed consent (or assent with parental consent for minors), patients completed a questionnaire for age, sex, race, height and weight, years of education, depression (scores greater than 10 on the 9-item Patient Health Questionnaire (Kroenke, Spitzer, Williams, & Lowe, 2010; Richardson et al., 2010; Spitzer et al., 1994)), preoperative activity level (Marx Activity Rating Scale (Marx, Stump, Jones, Wickiewicz, & Warren, 2001)), expectation for surgical success, and primary type of sport and sport level. Preoperative fear of movement/reinjury, self-efficacy, and pain catastrophizing were assessed using the Tampa Scale for Kinesiophobia (TSK) (Roelofs, Goubert, Peters, Vlaeyen, & Crombez, 2004), Knee Self-Efficacy Scale (K-SES) (Thomee et al., 2006), and Pain Catastrophizing Scale (PCS) (Sullivan, Bishop, & Pivik, 1995), respectively. Preoperative outcomes of sports participation and quality of life were assessed with Knee Injury and Osteoarthritis Outcome Score (KOOS) (Roos, Roos, Lohmander, Ekdahl, & Beynnon, 1998) sports/recreation and quality of life subscales, and knee function with the International Knee Documentation Committees (IKDC) Subjective Knee Form (Irrgang et al., 2001). Follow-up assessment was conducted by mail on printed forms at 6 and 12 months following surgery using the same validated outcome measures. Return to sport was assessed at 6 and 12 months with the Subjective Patient Outcome for Return to Sports (SPORTS) score (Blonna, Lee, & O’Driscoll, 2010).
Surgical and Rehabilitation Procedures
Surgery was performed by a single board-certified orthopaedic surgeon (K.P.S.) Surgeon discretion was used for graft choice and concurrent meniscal procedures. Articular cartilage pathology in the medial, lateral, and patellofemoral compartments was documented. Surgical data were extracted using a questionnaire and the medical record. Following surgery, all patients underwent the same prescribed physical therapy protocol using MOON ACLR rehabilitation guidelines (Wright et al., 2015). These published guidelines were informed by best evidence and content experts. The phased approach followed functional progression criteria. The duration of physical therapy was estimated to involve a total of 16 to 24 visits (minimum of 6 visits), with most visits occurring within the first 6 weeks. Compliance to postoperative physical therapy was not documented.
FAM Measures
Fear of movement/reinjury
The TSK is a valid and reliable measure of fear of movement/reinjury in surgical patients and patients with various musculoskeletal conditions (Archer et al., 2012; French, France, Vigneau, French, & Evans, 2007; Kori, Miller, & Todd, 1990; Roelofs et al., 2004; Swinkels-Meewisse et al., 2006). The TSK has been used in adolescent and adult patients with knee injuries, including ACLR (Chmielewski & George, 2019; Selhorst, Fernandez-Fernandez, Schmitt, & Hoehn, 2020). We used the 17-item version, with scores ranging from 17 to 68. Higher TSK scores indicate higher fear of movement/reinjury.
Self-Efficacy
The K-SES is a valid and reliable measure that assesses four domains of self-efficacy (daily activities, sports activities, knee function activities, knee function in future) (Thomee et al., 2006, 2007). The K-SES has been used as a measure of self-efficacy in adolescent patients after ACLR (Beischer et al., 2019). We used the 6-item subscale for knee function activities. The K-SES knee function activities subscale assesses how confident patients are about performing functional activities at that moment in time, despite knee pain/discomfort. K-SES knee function subscale scores range from 0 to 10, with higher scores indicating greater confidence in knee function.
Pain Catastrophizing
The PCS is a valid and reliable measure that assesses unhelpful catastrophic thoughts or emotions about pain (Sullivan et al., 1995). PCS scores have shown associations with pain intensity, patient-reported disability, negative affect, and pain-related fear (Osman et al., 2000; Sullivan et al., 1995). The PCS has been assessed in adolescent and adult patients with knee injuries, including ACLR (Chmielewski & George, 2019; Selhorst et al., 2020; Tripp, Stanish, Reardon, Coady, & Sullivan, 2003). The PCS contains 13 items with scores ranging from 0 to 52. Higher PCS scores indicate greater pain catastrophizing.
Expectation for Surgical Success
Patients rated their preoperative expectation of having a successful surgery on a scale from 1 to 10, with 1 indicating low expectation and 10 indicating high expectation. We used a modified scale similar to previously reported expectation assessments of overall surgical success (Haanstra et al., 2012).
Outcome Measures
Return to sport
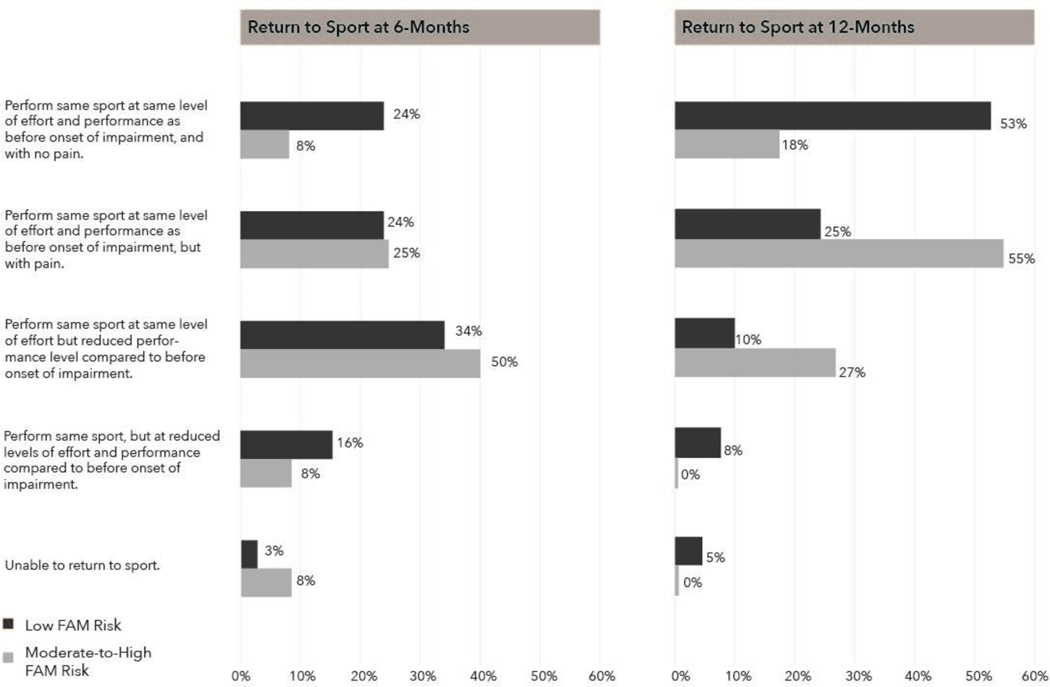
The single-item SPORTS score was used to assess a participant’s return to sport status (Blonna et al., 2010). The SPORTS score has excellent test-retest reliability and good concurrent validity with moderately high correlations with the KOOS sports/recreation subscale and Lysholm scale in patients after ACLR (Blonna et al., 2012). For the SPORTS score, patients select whether they can 1) perform same sport at same level of effort and performance as before onset of impairment, and with no pain; 2) perform same sport at same level of effort and performance as before onset of impairment, but with pain; 3) perform same sport at same level of effort but reduced performance level compared to before onset of impairment; 4) perform same sport, but at reduced levels of effort and performance compared to before onset of impairment; or 5) unable to return to the same sport.
Sports Participation and Quality of Life
The KOOS was used to assess sports participation and quality of life (Roos et al., 1998). The KOOS consists of five subscales and was developed for use in a young, highly active population with knee injuries (Roos et al., 1998). KOOS subscales have good reliability and validity in patients with knee injuries (Roos & Lohmander, 2003; Roos et al., 1998; Roos & Toksvig-Larsen, 2003). For this study, we considered the 5-item sports/recreation and 4-item quality of life subscales as outcomes. KOOS subscale scores range from 0 to 100, with higher scores indicating higher sports participation or quality of life. The minimum clinically important difference (MCID) for the KOOS subscales is 8 points (Roos & Lohmander, 2003).
Knee Function
The 18-item IKDC was used to assess patient-reported perceptions of knee pain, stiffness, swelling, joint locking and instability, and function (Irrgang et al., 2001). The IKDC demonstrates good internal consistency and test-retest reliability in patients with various knee problems, including ACLR (Greco et al., 2010; Higgins et al., 2007; Irrgang et al., 2001). IKDC scores range from 0 to 100, with higher scores indicating better knee function. The MCID for the IKDC is 9 points (Nwachukwu et al., 2017).
Data Analysis
We performed a two-step cluster analysis to identify preoperative FAM risk subgroups based on fear of movement/reinjury, self-efficacy, and pain catastrophizing. Cluster analysis differentiates cases based on homogenous structures within the data. We did not specify the number of clusters a priori. Cluster subgrouping was assessed with a silhouette coefficient and measure of variable contribution. We repeated the cluster analysis with cases randomly sorted to ensure subgroup stability (IBM Corporation, 2016). Independent samples t-tests were used to confirm subgroup differences in FAM variables.
Descriptive statistics were used for generating mean [SD] and proportion (frequency) for continuous and categorical variables, respectively. Multivariable proportional odds regression with odds ratio [95% CI] was used to examine the association between preoperative FAM risk subgroups and expectation for surgical success and 6- and 12-month return to sport. Multivariable linear regression with unstandardized beta [95% CI] and standardized beta were used for 6- and 12-month sports participation, knee function, and quality of life. Separate models were generated for each outcome and time point, and included a priori covariates of age, sex, and preoperative outcome score. Marx score was used as a baseline covariate for return to sport and sports participation models (Spindler et al., 2018).
We used IBM SPSS Statistics version 26.0 software (IBM Corporation, Armonk, NY) for cluster subgrouping and linear models and R software (R Foundation for Statistical Computing, Vienna, Austria) using the rms package for proportional odds models (R Core Team). Only complete cases were analyzed. Data from 50 (93%) and 51 (94%) patients were available at 6 months and 12 months, respectively. Alpha was set at the .05 level or lower for statistical significance.
RESULTS
Patient Sample
Fifty-four consecutive patients (mean [95% CI] age = 19.1 [17.7; 20.5] years, 29 (54%) males) were enrolled (Table 1). All patients reported a high preoperative level of activity. Most patients were involved in contact sports (soccer, basketball, football) and sports at the high school level. Preoperative expectation for surgical success was high, where 46 (83%) patients rated their expectation as a 9 or higher (median [IQR] = 9.0 [9.0; 10.0]). All patients had bone-patellar tendon-bone autografts. Six (11%) patients had concomitant grade 2 medial collateral ligament (MCL) injury and 1 (2%) patient had a grade 1 MCL injury. No patients had a concomitant lateral collateral ligament involvement. Surgical management of medial and lateral meniscus tears occurred in 13 (24%) and 23 (43%) patients, respectively.
Table 1.
Sociodemographic, Surgical, and Psychosocial Characteristics (N=54). Abbreviations: BMI = body mass index, BTB = bone-patellar tendon-bone, TSK = Tampa Scale for Kinesiophobia, PCS = Pain Catastrophizing Scale, K-SES = Knee Self-Efficacy Scale Values are mean [SD] or count (%) unless otherwise noted.
| Moderate-to-High | Low | ||
|---|---|---|---|
| Characteristic | All (N=54) | FAM Risk (n=13) | FAM Risk (n=41) |
|
| |||
| Sociodemographic | |||
| Age, in years | 19.1 [5.1] | 17.6 [3.8] | 19.6 [5.4] |
| Sex, Male | 29 (54 %) | 6 (46 %) | 23 (56 %) |
| Race, White | 46 (85 %) | 9 (69 %) | 37 (90 %) |
| BMI, in kg/cm2 | 24.6 [4.6] | 24.0 [3.5] | 24.9 [4.9] |
| Education, in years | 12.0 [3.2] | 11.5 [2.8] | 12.1 [3.3] |
| Depression, yes | 2 (4 %) | 1 (8 %) | 1 (2 %) |
| Marx score, median [IQR] | 16 [16; 16] | 16 [16; 16] | 16 [13; 16] |
| Sport | |||
| Basketball | 14 (26 %) | 5 (38 %) | 9 (22 %) |
| Football | 13 (24 %) | 1 (8 %) | 12 (29 %) |
| Soccer | 18 (33 %) | 7 (54 %) | 11 (27 %) |
| Other | 9 (17 %) | 0 (0 %) | 9 (22 %) |
| Level of Sport | |||
| High School | 31 (57 %) | 10 (77 %) | 21 (51 %) |
| Recreation | 8 (15 %) | 1 (8 %) | 7 (17 %) |
| Amateur | 6 (11 %) | 1 (8 %) | 5 (12 %) |
| College | 9 (17 %) | 1 (8 %) | 8 (20 %) |
| Surgical | |||
| BTB autograft | 54 (100 %) | 13 (100 %) | 41 (100 %) |
| Medial meniscus treatment | |||
| No tear | 33 (61 %) | 8 (62 %) | 25 (61 %) |
| Untreated tear | 8 (15 %) | 2 (15 %) | 6 (15 %) |
| Repair | 9 (17 %) | 2 (15 %) | 7 (17 %) |
| Excision | 4 (7 %) | 1 (8 %) | 3 (7 %) |
| Lateral meniscus treatment | |||
| No tear | 22 (41 %) | 7 (54 %) | 15 (37 %) |
| Untreated tear | 9 (17 %) | 1 (8 %) | 8 (20 %) |
| Repair | 3 (6 %) | 1 (8 %) | 2 (5 %) |
| Excision | 20 (37 %) | 4 (31 %) | 16 (39 %) |
| Articular cartilage chondrosis | |||
| Medial compartment - grade 2 | 8 (15 %) | 1 (8 %) | 7 (17 %) |
| Medial compartment - grade 3 | 1 (2 %) | 1 (8 %) | 0 (0 %) |
| Lateral compartment - grade 2 | 4 (7 %) | 2 (15 %) | 2 (5 %) |
| Lateral compartment - grade 3 | 1 (2 %) | 0 (0 %) | 1 (2 %) |
| Patellofemoral compartment - grade 2 | 1 (2 %) | 0 (0 %) | 1 (2 %) |
| Medial collateral ligament injury | |||
| Grade 1 | 1 (2 %) | 1 (8 %) | 0 (0 %) |
| Grade 2 | 6 (11%) | 0 (0 %) | 6 (15%) |
| Preoperative Psychosocial | |||
| Fear of movement/reinjury (TSK) | 39.4 [6.2] | 44.4 [5.5] | 37.8 [5.6] |
| Self-efficacy (K-SES) | 28.8 [9.5] | 17.6 [9.3] | 31.9 [6.6] |
| Pain catastrophizing (PCS) | 8.7 [7.8] | 17.9 [8.5] | 5.8 [4.9] |
| Expectation of surgical success | 9.3 [1.0] | 8.7 [1.3] | 9.4 [0.8] |
FAM Risk Subgroups
Two subgroups were identified based on a good cluster solution (silhouette coefficient = .5). Thirteen (24%) patients fit within a “moderate-to-high FAM risk” group with higher preoperative scores for fear of movement/reinjury (mean difference = 6.6 [3.1 to 10.2], p < .001) and pain catastrophizing (mean difference = 12.0 [8.3 to 15.8], p < .001), and lower preoperative scores for self-efficacy (mean difference [95% CI] = −14.3 [−18.9 to −9.6], p < .001) compared to the “low FAM risk” group. The order of importance for differentiating subgroups was pain catastrophizing (relative importance = 1.0), self-efficacy (relative importance = .95), and fear of movement/reinjury (relative importance = .45). Characteristics of the subgroups are presented in Table 1. Patients in the moderate-to-high FAM risk group had lower preoperative expectation for surgical success (mean difference [95% CI] = - .7 [−1.4 to −.1], p < .05). There were no other differences between groups.
Multivariable Associations between FAM Subgroup and Outcomes
One (8%) patient in the moderate-to-high FAM risk group returned to their same sport at the same level of effort and performance as before onset of impartment and without pain at 6 months, compared to 9 (24%) patients in the low FAM risk group (Figure 1). Although not statistically significant, the odds of returning to sport at 6 months at each subsequent level of the SPORTS score was 70% lower in the moderate-to-high FAM risk group (p = .07) (Table 2).
Figure 1.
Return to sport at 6 (n =50) and 12 months (n = 51) by preoperative FAM risk subgroup.
Table 2.
Multivariable Proportional Odds Regression Analyses for SPORTS Score at 6 and 12 Months. Abbreviations: FAM = fear-avoidance model, SPORTS = Subjective Patient Outcome for Return to Sports.
| 6 Months | 12 Months | |||
|---|---|---|---|---|
|
|
||||
| Odds Ratio [95% CI] | p | Odds Ratio [95% CI] | p | |
|
| ||||
| SPORTS Score | ||||
| Moderate-to-high FAM risk | .3 [.1 to 1.1] | .07 | .3 [.1 to 1.0] | .05 |
| Expectation of surgical success | .7 [.4 to 1.3] | .28 | .8 [.4 to 1.5] | .51 |
Models controlled for age, sex, and preoperative Marx score
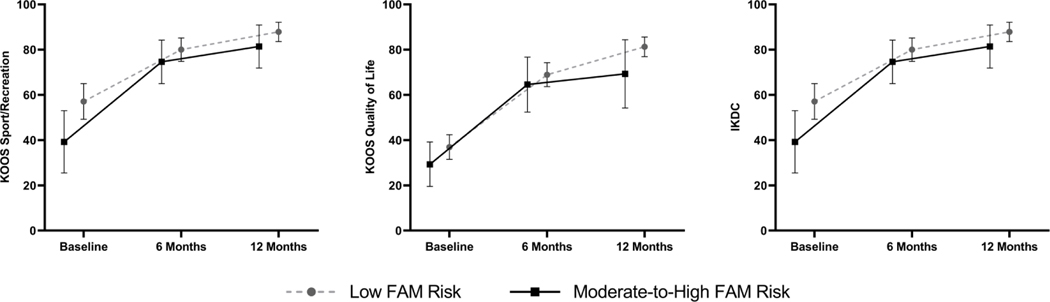
At 12 months, 2 (18%) patients in the moderate-to-high FAM risk group and 21 (53%) patients in the low FAM risk group were able to return to their same sport at the same level of effort and performance as before onset of impartment and without pain. The odds of returning to sport at 12 months at each subsequent level of the SPORTS score was marginally significant, with 70% lower odds in the moderate-to-high FAM risk group (p = .05) (Table 2). Patients in the moderate-to-high FAM risk group reported lower knee function at 6 months (p = .04) and 12 months (p = .001) and lower quality of life at 12 months (p = .007) (Table 3 and Figure 2). Patients in the moderate-to-high FAM risk group also reported marginally lower sports participation at 6 months (p = .05). The magnitude of outcome score difference (unstandardized beta in Table 3) between subgroups for 6- and 12-month KOOS subscales and 12-month IKDC exceeded MCID values.
Table 3.
Multivariable Linear Regression Analyses for the KOOS and IKDC at 6 and 12 Months. Abbreviations: FAM = fear-avoidance model, KOOS = Knee Injury and Osteoarthritis Outcome Score, IKDC = International Knee Documentation Committee
| 6 Months | 12 Months | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Unstandardized Beta [95% CI] | Standardized Beta | p | Unstandardized Beta [95% CI] | Standardized Beta | p | |
|
| ||||||
| KOOS Sport/Recreation | ||||||
| Moderate-to-high FAM risk | −9.9 [−20.0 to .2] | −.27 | .05 | −7.1 [−16.7 to 2.5] | −.21 | .15 |
| Expectation of surgical success | −3.7 [−8.1 to .6] | −.23 | .09 | .4 [−3.6 to 4.4] | .03 | .85 |
| KOOS Quality of Life | ||||||
| Moderate-to-high FAM risk | −9.4 [−21.0 to 2.2] | −.24 | .11 | −17.5 [−29.9 to −5.0] | −.42 | .007 |
| Expectation of surgical success | −3.9 [−8.8 to 1.0] | −.23 | .12 | −5.1 [−10.1 to .01] | −.29 | .05 |
| IKDC | ||||||
| Moderate-to-high FAM risk | −7.6 [−14.6 to −.5] | −.29 | .04 | −13.0 [−20.7 to −5.4] | −.47 | .001 |
| Expectation of surgical success | −4.1 [−7.1 to −1.1] | −.36 | .008 | −2.5 [−5.6 to .6] | −.22 | .11 |
Regression models controlled for age, sex, and preoperative outcome score (*Marx used for KOOS Sport/Recreation)
Figure 2.
Unadjusted scores for Knee Injury and Osteoarthritis Outcome Score (KOOS) Sports and Recreation and Quality of Life subscales and International Knee Documentation Committee (IKDC) by preoperative FAM risk subgroup. Mean scores are marked, with error bars representing 95% confidence intervals.
Multivariable Associations between Expectation for Surgical Success and Outcomes
Patients with higher preoperative expectation for surgical success had lower knee function at 6 months (p = .008) and marginally lower quality of life at 12 months (p = .05) (Table 3). Preoperative expectation was not associated with quality of life at 6 months or return to sport and sports participation at 6 or 12 months (p > .05).
DISCUSSION
We examined the association of preoperative FAM risk subgroup status and patient expectation for surgical success and 6- and 12-month outcomes after ACLR. Patients with moderate-to-high FAM risk (24% of sample) had lower odds of return to sport and poorer 6-month sports participation, 6- and 12-month knee function, and 12-month quality of life. We observed an association between preoperative expectation and 6-month knee function and 12-month quality of life. While preliminary, these results suggest preoperative FAM characteristics and expectation are important risk factors to consider in estimating recovery and may suggest a need for targeted strategies.
Overall, 20% of our sample returned to sport at their same effort or performance level and without pain at 6 months, while 45% returned to their sport at this level at 12 months. Return to preinjury sport is estimated between 33% and 66% at or before one year post-operatively (Ardern, Taylor, Feller, & Webster, 2014; Ardern, Webster, Taylor, & Feller, 2011). In another study using the SPORTS score, 32% of participants were able to return to sport at the same level of effort or performance without pain at 5–10 years post-ACLR (Blonna et al., 2012). The SPORTS score is designed to assess not only return to sport, but also the level of performance and associated degree of residual impairment. This level of return to sport appraisal provides a more specific assessment of the athlete’s return to sport status, however, makes direct comparison with prior reported return to sport rates difficult.
We found 24% of patients exhibited moderate-to-high preoperative FAM risk. Direct comparison to prior ACLR literature is challenging as few studies have reported the proportion meeting high-risk status based on the FAM model. In a small study by Burland et al. (2020), 29% of patients reported high fear of movement/reinjury (TSK scores > 37) at an average of 3.6 years after surgery. The moderate-to-high and low FAM risk subgroups showed improvement in patient-reported outcomes from baseline to 12-months, with significantly less outcome improvement noted in the moderate-to-high risk group over time. This is especially notable when examining the magnitude of difference in outcome scores for the KOOS subscales and IKDC.
Preoperative FAM risk status was an important predictor of 1-year return to sport, knee function, and quality of life. These findings are in line with studies examining independent associations between preoperative fear of movement/reinjury and self-efficacy and postoperative ACLR outcomes (Ardern, Taylor, Feller, Whitehead, et al., 2013; Thomee et al., 2008). Our study demonstrates that a preoperative composite FAM risk subgroup that includes pain catastrophizing is related to multiple outcomes relevant to recovery. Pain catastrophizing and self-efficacy were the most distinguishing subgroup factors. The sports literature frequently highlights the importance of fear (Nwachukwu et al., 2019), especially for return to sport. Fear of movement/reinjury appears as a common preoperative emotion, while elevated pain catastrophizing is less prevalent and, perhaps, a unique state or trait characteristic among a subset of patients (George, Lentz, Zeppieri, Lee, & Chmielewski, 2012). Conflicting evidence exists for the relationship of pain catastrophizing to post-ACLR outcomes (Baranoff, Hanrahan, & Connor, 2015; Chmielewski & George, 2019; Chmielewski et al., 2011; Jochimsen et al., 2020; Pavlin, Sullivan, Freund, & Roesen, 2005; Tichonova, Rimdeikiene, Petruseviciene, & Lendraitiene, 2016; Tripp et al., 2007). Some studies have shown early postoperative pain catastrophizing (i.e., at 2 to 4 weeks after ACLR) predicted subsequent knee impairment resolution (e.g. 12 weeks) (Chmielewski & George, 2019) and post-rehabilitation pain, function, and quality of life (Tichonova et al., 2016), while other studies did not show significant relationships (Baranoff et al., 2015; Chmielewski et al., 2011). Pavlin et al. (2005) found preoperative pain catastrophizing predicted acute postoperative pain, while Jochimsen et al. (2020) reported preoperative pain catastrophizing was not associated with 6-month pain or KOOS subscale scores. Additional work is needed to confirm the importance of pain catastrophizing as a psychosocial risk factor relative to other established constructs.
Over 80% of patients expected their surgery to be a success. Prior literature has highlighted a similar proportion who expect nearly normal to normal knee function and a return to their pre-injury sport (Feucht et al., 2016; Webster & Feller, 2019). We did not observe an association between preoperative expectation and return to sport as hypothesized. Sonesson et al. (2017) reported no differences between patients who returned or did not return to sport in their preoperative expectation of length of rehabilitation, time to running/jumping, or time to return to sport. In contrast, Ardern et al. (2013) found athletes who expected a longer time to return to sport had a lower chance of returning to sport. We did find preoperative expectation was associated with the IKDC at 6 months and KOOS quality of life subscale at 12 months. However, the association with 12-month quality of life was marginal and should be interpreted with caution.
Psychosocial factors are important considerations within the decision-making process. Preoperative screening may help identify patients at risk for poor outcomes. Based on our study, subgroup classification using multidimensional screening tools rather than single questionnaires may be useful for predicting poor recovery. Multidimensional measures such as the STarTBack and Optimal Screening for Prediction of Referral and Outcome (OSPRO) tools represent clinically feasible composite risk assessments of multiple psychosocial domains for patients with musculoskeletal pain (Hill et al., 2008; Lentz et al., 2016). Use of multidimensional tools can direct more precise management or tailored screening processes to establish prognosis (Van Wyngaarden, Noehren, & Archer, 2019). Similar work is needed investigating the most important screening questions across FAM domains for determining outcomes or management after ACLR. Currently, most preoperative ACLR programs focus on range of motion or strength impairments, and it is unknown whether a preoperative psychosocial intervention can enhance return to sport. Postoperative psychosocial interventions can improve postoperative quality of life, anxiety, and fear of reinjury (Coronado, Bird, et al., 2018; Cupal & Brewer, 2001; Zaffagnini, Russo, Marcheggiani Muccioli, & Marcacci, 2013). Future efforts examining the efficacy of a combined preoperative and postoperative intervention on return to sport are warranted (Coronado et al., 2020).
Our study is limited by the small sample, which influences the precision of our findings (i.e., width of 95% CIs) and our ability to account for more covariates (e.g., including concurrent meniscal or articular cartilage pathology). Although some of the effect estimates suggest clinically meaningful associations, our results should be considered preliminary and require more robust evidence for validation. All outcomes were patient-reported, and none involved objective physical function or performance measures. Additionally, all patients underwent surgery by a single surgeon and may not generalize to other settings. While all patients were prescribed the same evidence-based physical therapy program, we are unable to report on compliance or details regarding postoperative rehabilitation. Thus, we are unable to account for rehabilitation factors as potential confounders to return to sport or patient-reported outcomes. Additionally, most of our patients reported a high preoperative activity level. We focused on preoperative factors because of our interest in at-risk patient screening before surgery. We did not examine changes in subgroup membership or FAM scores. Future work should examine whether change in subgroup membership may influence postoperative recovery.
CONCLUSION
Twenty-four percent of participants were moderate-to-high risk based on preoperative FAM factor scores. The moderate-to-high FAM risk subgroup showed lower odds of return to sport and poorer patient-reported outcomes up to 12 months. Preoperative expectation was an important predictor of knee function and quality of life. These findings highlight the importance of preoperative multidimensional screening for patients at-risk for poor ACLR outcomes.
HIGHLIGHTS.
24% of patients were moderate-to-high risk based on fear-avoidance model (FAM) factors.
Moderate-to-high FAM risk patients had poorer return to sport and patient-reported outcomes.
Expectation of surgical success was an important predictor of 6-month knee function.
Acknowledgments:
Dr. Coronado was supported by a Vanderbilt Faculty Research Scholars Award during manuscript development and submission.
Ethical approval: This study was approved by the Institutional Review Board of Vanderbilt University Medical Center
Funding: Research reported in this publication was partially supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number R01 AR053684 and by CTSA award No. UL1 TR002243 from the National Center for Advancing Translational Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Institutes of Health or the National Center for Advancing Translational Sciences.
Footnotes
Declaration of interest: The authors acknowledge that this manuscript has not been previously published nor under consideration for publication elsewhere. If accepted, the manuscript will not be published elsewhere. All authors have approved the final version of this manuscript.
Conflict of interest: None declared
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Archer KR, Phelps KD, Seebach CL, Song Y, Riley LH 3rd, & Wegener ST (2012). Comparative study of short forms of the Tampa Scale for Kinesiophobia: fear of movement in a surgical spine population. Arch Phys Med Rehabil, 93(8), 1460–1462. doi: 10.1016/j.apmr.2012.03.024 [DOI] [PubMed] [Google Scholar]
- Ardern CL (2015). Anterior Cruciate Ligament Reconstruction-Not Exactly a One-Way Ticket Back to the Preinjury Level: A Review of Contextual Factors Affecting Return to Sport After Surgery. Sports Health, 7(3), 224–230. doi: 10.1177/1941738115578131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardern CL, Taylor NF, Feller JA, & Webster KE (2013). A systematic review of the psychological factors associated with returning to sport following injury. Br J Sports Med, 47(17), 1120–1126. doi: 10.1136/bjsports-2012-091203 [DOI] [PubMed] [Google Scholar]
- Ardern CL, Taylor NF, Feller JA, & Webster KE (2014). Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med, 48(21), 1543–1552. doi: 10.1136/bjsports-2013-093398 [DOI] [PubMed] [Google Scholar]
- Ardern CL, Taylor NF, Feller JA, Whitehead TS, & Webster KE (2013). Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med, 41(7), 1549–1558. doi: 10.1177/0363546513489284 [DOI] [PubMed] [Google Scholar]
- Ardern CL, Taylor NF, Feller JA, Whitehead TS, & Webster KE (2015). Sports participation 2 years after anterior cruciate ligament reconstruction in athletes who had not returned to sport at 1 year: a prospective follow-up of physical function and psychological factors in 122 athletes. Am J Sports Med, 43(4), 848–856. doi: 10.1177/0363546514563282 [DOI] [PubMed] [Google Scholar]
- Ardern CL, Webster KE, Taylor NF, & Feller JA (2011). Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med, 39(3), 538–543. doi: 10.1177/0363546510384798 [DOI] [PubMed] [Google Scholar]
- Baranoff J, Hanrahan SJ, & Connor JP (2015). The roles of acceptance and catastrophizing in rehabilitation following anterior cruciate ligament reconstruction. J Sci Med Sport, 18(3), 250–254. doi: 10.1016/j.jsams.2014.04.002 [DOI] [PubMed] [Google Scholar]
- Beischer S, Hamrin Senorski E, Thomee C, Samuelsson K, & Thomee R. (2019). How Is Psychological Outcome Related to Knee Function and Return to Sport Among Adolescent Athletes After Anterior Cruciate Ligament Reconstruction? Am J Sports Med, 47(7), 1567–1575. doi: 10.1177/0363546519843073 [DOI] [PubMed] [Google Scholar]
- Beneciuk JM, Robinson ME, & George SZ (2012). Low back pain subgroups using fear-avoidance model measures: results of a cluster analysis. Clin J Pain, 28(8), 658–666. doi: 10.1097/AJP.0b013e31824306ed [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beneciuk JM, Robinson ME, & George SZ (2015). Subgrouping for patients with low back pain: a multidimensional approach incorporating cluster analysis and the STarT Back Screening Tool. J Pain, 16(1), 19–30. doi: 10.1016/j.jpain.2014.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bialosky JE, Bishop MD, & Cleland JA (2010). Individual expectation: an overlooked, but pertinent, factor in the treatment of individuals experiencing musculoskeletal pain. Phys Ther, 90(9), 1345–1355. doi: 10.2522/ptj.20090306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blonna D, Castoldi F, Delicio D, Bruzzone M, Dettoni F, Bonasia DE, & Rossi R. (2012). Validity and reliability of the SPORTS score. Knee Surg Sports Traumatol Arthrosc, 20(2), 356–360. doi: 10.1007/s00167-011-1608-8 [DOI] [PubMed] [Google Scholar]
- Blonna D, Lee GC, & O’Driscoll SW (2010). Arthroscopic restoration of terminal elbow extension in high-level athletes. Am J Sports Med, 38(12), 2509–2515. doi: 10.1177/0363546510376727 [DOI] [PubMed] [Google Scholar]
- Boersma K, & Linton SJ (2006). Psychological processes underlying the development of a chronic pain problem: a prospective study of the relationship between profiles of psychological variables in the fear-avoidance model and disability. Clin J Pain, 22(2), 160–166. doi: 10.1097/01.ajp.0000159582.37750.39 [DOI] [PubMed] [Google Scholar]
- Burland JP, Howard JS, Lepley AS, DiStefano LJ, Lepley LK, & Frechette L. (2020). What Are Our Patients Really Telling Us? Psychological Constructs Associated With Patient-Reported Outcomes After Anterior Cruciate Ligament Reconstruction. J Athl Train, 55(7), 707–716. doi: 10.4085/1062-6050-120-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chmielewski TL, & George SZ (2019). Fear avoidance and self-efficacy at 4 weeks after ACL reconstruction are associated with early impairment resolution and readiness for advanced rehabilitation. Knee Surg Sports Traumatol Arthrosc, 27(2), 397–404. doi: 10.1007/s00167-018-5048-6 [DOI] [PubMed] [Google Scholar]
- Chmielewski TL, Zeppieri G Jr., Lentz TA, Tillman SM, Moser MW, Indelicato PA, & George SZ (2011). Longitudinal changes in psychosocial factors and their association with knee pain and function after anterior cruciate ligament reconstruction. Phys Ther, 91(9), 1355–1366. doi: 10.2522/ptj.20100277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coronado RA, Bird ML, Van Hoy EE, Huston LJ, Spindler KP, & Archer KR (2018). Do psychosocial interventions improve rehabilitation outcomes after anterior cruciate ligament reconstruction? A systematic review. Clin Rehabil, 32(3), 287–298. doi: 10.1177/0269215517728562 [DOI] [PubMed] [Google Scholar]
- Coronado RA, Seitz AL, Pelote E, Archer KR, & Jain NB (2018). Are Psychosocial Factors Associated With Patient-reported Outcome Measures in Patients With Rotator Cuff Tears? A Systematic Review. Clin Orthop Relat Res, 476(4), 810–829. doi: 10.1007/s11999.0000000000000087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coronado RA, Sterling EK, Fenster DE, Bird ML, Heritage AJ, Woosley VL, . . . Archer KR (2020). Cognitive-behavioral-based physical therapy to enhance return to sport after anterior cruciate ligament reconstruction: An open pilot study. Phys Ther Sport, 42, 82–90. doi: 10.1016/j.ptsp.2020.01.004 [DOI] [PubMed] [Google Scholar]
- Cupal DD, & Brewer BW (2001). Effects of relaxation and guided imagery on knee strength, reinjury anxiety, and pain following anterior cruciate ligament reconstruction. Rehabilitation Psychology, 46(1), 28–43. doi:Doi 10.1037/0090-5550.46.1.28 [DOI] [Google Scholar]
- Feucht MJ, Cotic M, Saier T, Minzlaff P, Plath JE, Imhoff AB, & Hinterwimmer S. (2016). Patient expectations of primary and revision anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc, 24(1), 201–207. doi: 10.1007/s00167-014-3364-z [DOI] [PubMed] [Google Scholar]
- Forsdyke D, Smith A, Jones M, & Gledhill A. (2016). Psychosocial factors associated with outcomes of sports injury rehabilitation in competitive athletes: a mixed studies systematic review. Br J Sports Med, 50(9), 537–544. doi: 10.1136/bjsports-2015-094850 [DOI] [PubMed] [Google Scholar]
- French DJ, France CR, Vigneau F, French JA, & Evans RT (2007). Fear of movement/(re)injury in chronic pain: a psychometric assessment of the original English version of the Tampa scale for kinesiophobia (TSK). Pain, 127(1–2), 42–51. doi: 10.1016/j.pain.2006.07.016 [DOI] [PubMed] [Google Scholar]
- George SZ, Lentz TA, Zeppieri G, Lee D, & Chmielewski TL (2012). Analysis of shortened versions of the tampa scale for kinesiophobia and pain catastrophizing scale for patients after anterior cruciate ligament reconstruction. Clin J Pain, 28(1), 73–80. doi: 10.1097/AJP.0b013e31822363f4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greco NJ, Anderson AF, Mann BJ, Cole BJ, Farr J, Nissen CW, & Irrgang JJ (2010). Responsiveness of the International Knee Documentation Committee Subjective Knee Form in comparison to the Western Ontario and McMaster Universities Osteoarthritis Index, modified Cincinnati Knee Rating System, and Short Form 36 in patients with focal articular cartilage defects. Am J Sports Med, 38(5), 891–902. doi: 10.1177/0363546509354163 [DOI] [PubMed] [Google Scholar]
- Haanstra TM, van den Berg T, Ostelo RW, Poolman RW, Jansma EP, Cuijpers P, & de Vet HC (2012). Systematic review: do patient expectations influence treatment outcomes in total knee and total hip arthroplasty? Health Qual Life Outcomes, 10, 152. doi: 10.1186/1477-7525-10-152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamrin Senorski E, Samuelsson K, Thomee C, Beischer S, Karlsson J, & Thomee R. (2017). Return to knee-strenuous sport after anterior cruciate ligament reconstruction: a report from a rehabilitation outcome registry of patient characteristics. Knee Surg Sports Traumatol Arthrosc, 25(5), 1364–1374. doi: 10.1007/s00167-016-4280-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins LD, Taylor MK, Park D, Ghodadra N, Marchant M, Pietrobon R, . . . International Knee Documentation, C. (2007). Reliability and validity of the International Knee Documentation Committee (IKDC) Subjective Knee Form. Joint Bone Spine, 74(6), 594–599. doi: 10.1016/j.jbspin.2007.01.036 [DOI] [PubMed] [Google Scholar]
- Hill JC, Dunn KM, Lewis M, Mullis R, Main CJ, Foster NE, & Hay EM (2008). A primary care back pain screening tool: identifying patient subgroups for initial treatment. Arthritis Rheum, 59(5), 632–641. doi: 10.1002/art.23563 [DOI] [PubMed] [Google Scholar]
- Hsu CJ, Meierbachtol A, George SZ, & Chmielewski TL (2017). Fear of Reinjury in Athletes. Sports Health, 9(2), 162–167. doi: 10.1177/1941738116666813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corporation. (2016). TwoStep Cluster Analysis. IBM SPSS Statistics V24 Documentation. Retrieved from https://www.ibm.com/support/knowledgecenter/SSLVMB_24.0.0/spss/base/idh_twostep_main.html [Google Scholar]
- Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, . . . Shelborne KD (2001). Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med, 29(5), 600–613. doi: 10.1177/03635465010290051301 [DOI] [PubMed] [Google Scholar]
- Jochimsen KN, Pelton MR, Mattacola CG, Huston LJ, Reinke EK, Spindler KP, . . . Jacobs CA (2020). Relationship Between Pain Catastrophizing and 6-Month Outcomes Following Anterior Cruciate Ligament Reconstruction. J Sport Rehabil, 29(6), 808–812. doi: 10.1123/jsr.2018-0431 [DOI] [PubMed] [Google Scholar]
- Kori SH, Miller RP, & Todd DD (1990). Kinesiophobia: a new region of chronic pain behavior. Pain Manage, 3, 35–43. [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB, & Lowe B. (2010). The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry, 32(4), 345–359. doi: 10.1016/j.genhosppsych.2010.03.006 [DOI] [PubMed] [Google Scholar]
- Langford JL, Webster KE, & Feller JA (2009). A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. Br J Sports Med, 43(5), 377–381. doi: 10.1136/bjsm.2007.044818 [DOI] [PubMed] [Google Scholar]
- Larsson B, Gerdle B, Bernfort L, Levin LA, & Dragioti E. (2017). Distinctive subgroups derived by cluster analysis based on pain and psychological symptoms in Swedish older adults with chronic pain - a population study (PainS65+). BMC Geriatr, 17(1), 200. doi: 10.1186/s12877-017-0591-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lentz TA, Beneciuk JM, Bialosky JE, Zeppieri G Jr., Dai Y, Wu SS, & George SZ (2016). Development of a Yellow Flag Assessment Tool for Orthopaedic Physical Therapists: Results From the Optimal Screening for Prediction of Referral and Outcome (OSPRO) Cohort. J Orthop Sports Phys Ther, 46(5), 327–343. doi: 10.2519/jospt.2016.6487 [DOI] [PubMed] [Google Scholar]
- Lentz TA, Tillman SM, Indelicato PA, Moser MW, George SZ, & Chmielewski TL (2009). Factors associated with function after anterior cruciate ligament reconstruction. Sports Health, 1(1), 47–53. doi: 10.1177/1941738108326700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lentz TA, Zeppieri G Jr., George SZ, Tillman SM, Moser MW, Farmer KW, & Chmielewski TL (2015). Comparison of physical impairment, functional, and psychosocial measures based on fear of reinjury/lack of confidence and return-to-sport status after ACL reconstruction. Am J Sports Med, 43(2), 345–353. doi: 10.1177/0363546514559707 [DOI] [PubMed] [Google Scholar]
- Lentz TA, Zeppieri G Jr., Tillman SM, Indelicato PA, Moser MW, George SZ, & Chmielewski TL (2012). Return to preinjury sports participation following anterior cruciate ligament reconstruction: contributions of demographic, knee impairment, and self-report measures. J Orthop Sports Phys Ther, 42(11), 893–901. doi: 10.2519/jospt.2012.4077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marx RG, Stump TJ, Jones EC, Wickiewicz TL, & Warren RF (2001). Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med, 29(2), 213–218. doi: 10.1177/03635465010290021601 [DOI] [PubMed] [Google Scholar]
- McCullough KA, Phelps KD, Spindler KP, Matava MJ, Dunn WR, Parker RD, . . . Reinke EK. (2012). Return to high school- and college-level football after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Am J Sports Med, 40(11), 2523–2529. doi: 10.1177/0363546512456836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nisenzon AN, George SZ, Beneciuk JM, Wandner LD, Torres C, & Robinson ME (2014). The role of anger in psychosocial subgrouping for patients with low back pain. Clin J Pain, 30(6), 501–509. doi: 10.1097/AJP.0000000000000019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nwachukwu BU, Adjei J, Rauck RC, Chahla J, Okoroha KR, Verma NN, . . . Williams RJ 3rd. (2019). How Much Do Psychological Factors Affect Lack of Return to Play After Anterior Cruciate Ligament Reconstruction? A Systematic Review. Orthop J Sports Med, 7(5), 2325967119845313. doi: 10.1177/2325967119845313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nwachukwu BU, Chang B, Voleti PB, Berkanish P, Cohn MR, Altchek DW, . . . Williams RJR. (2017). Preoperative Short Form Health Survey Score Is Predictive of Return to Play and Minimal Clinically Important Difference at a Minimum 2-Year Follow-up After Anterior Cruciate Ligament Reconstruction. Am J Sports Med, 45(12), 2784–2790. doi: 10.1177/0363546517714472 [DOI] [PubMed] [Google Scholar]
- Osman A, Barrios FX, Gutierrez PM, Kopper BA, Merrifield T, & Grittmann L. (2000). The Pain Catastrophizing Scale: further psychometric evaluation with adult samples. J Behav Med, 23(4), 351–365. doi: 10.1023/a:1005548801037 [DOI] [PubMed] [Google Scholar]
- Paterno MV, Flynn K, Thomas S, & Schmitt LC (2018). Self-Reported Fear Predicts Functional Performance and Second ACL Injury After ACL Reconstruction and Return to Sport: A Pilot Study. Sports Health, 10(3), 228–233. doi: 10.1177/1941738117745806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavlin DJ, Sullivan MJ, Freund PR, & Roesen K. (2005). Catastrophizing: a risk factor for postsurgical pain. Clin J Pain, 21(1), 83–90. doi: 10.1097/00002508-200501000-00010 [DOI] [PubMed] [Google Scholar]
- R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. ISBN 3–9000051-07–0, URL http://www.R-project.org/. Retrieved from http://www.R-project.org [Google Scholar]
- Rabey M, Smith A, Beales D, Slater H, & O’Sullivan P. (2016). Differing Psychologically Derived Clusters in People With Chronic Low Back Pain are Associated With Different Multidimensional Profiles. Clin J Pain, 32(12), 1015–1027. doi: 10.1097/AJP.0000000000000363 [DOI] [PubMed] [Google Scholar]
- Richardson LP, McCauley E, Grossman DC, McCarty CA, Richards J, Russo JE, . . . Katon W. (2010). Evaluation of the Patient Health Questionnaire-9 Item for detecting major depression among adolescents. Pediatrics, 126(6), 1117–1123. doi: 10.1542/peds.2010-0852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roelofs J, Goubert L, Peters ML, Vlaeyen JW, & Crombez G. (2004). The Tampa Scale for Kinesiophobia: further examination of psychometric properties in patients with chronic low back pain and fibromyalgia. Eur J Pain, 8(5), 495–502. doi: 10.1016/j.ejpain.2003.11.016 [DOI] [PubMed] [Google Scholar]
- Roos EM, & Lohmander LS (2003). The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes, 1, 64. doi: 10.1186/1477-7525-1-64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roos EM, Roos HP, Lohmander LS, Ekdahl C, & Beynnon BD (1998). Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther, 28(2), 88–96. doi: 10.2519/jospt.1998.28.2.88 [DOI] [PubMed] [Google Scholar]
- Roos EM, & Toksvig-Larsen S. (2003). Knee injury and Osteoarthritis Outcome Score (KOOS) - validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes, 1, 17. doi: 10.1186/1477-7525-1-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selhorst M, Fernandez-Fernandez A, Schmitt L, & Hoehn J. (2020). Adolescent psychological beliefs, but not parent beliefs, associated with pain and function in adolescents with patellofemoral pain. Phys Ther Sport, 45, 155–160. doi: 10.1016/j.ptsp.2020.07.003 [DOI] [PubMed] [Google Scholar]
- Sonesson S, Kvist J, Ardern C, Osterberg A, & Silbernagel KG (2017). Psychological factors are important to return to pre-injury sport activity after anterior cruciate ligament reconstruction: expect and motivate to satisfy. Knee Surg Sports Traumatol Arthrosc, 25(5), 1375–1384. doi: 10.1007/s00167-016-4294-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spindler KP, Huston LJ, Chagin KM, Kattan MW, Reinke EK, Amendola A, . . . Wright RW (2018). Ten-Year Outcomes and Risk Factors After Anterior Cruciate Ligament Reconstruction: A MOON Longitudinal Prospective Cohort Study. Am J Sports Med, 46(4), 815–825. doi: 10.1177/0363546517749850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Kroenke K, Linzer M, deGruy FV 3rd, Hahn SR, . . . Johnson JG (1994). Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA, 272(22), 1749–1756. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/7966923 [PubMed] [Google Scholar]
- Sullivan MJL, Bishop SR, & Pivik J. (1995). The Pain Catastrophizing Scale: Development and validation. Psychological Assessment, 7(4), 524–532. doi:Doi 10.1037/1040-3590.7.4.524 [DOI] [Google Scholar]
- Swinkels-Meewisse IE, Roelofs J, Schouten EG, Verbeek AL, Oostendorp RA, & Vlaeyen JW (2006). Fear of movement/(re)injury predicting chronic disabling low back pain: a prospective inception cohort study. Spine (Phila Pa 1976), 31(6), 658–664. doi: 10.1097/01.brs.0000203709.65384.9d [DOI] [PubMed] [Google Scholar]
- te Wierike SC, van der Sluis A, van den Akker-Scheek I, Elferink-Gemser MT, & Visscher C. (2013). Psychosocial factors influencing the recovery of athletes with anterior cruciate ligament injury: a systematic review. Scand J Med Sci Sports, 23(5), 527–540. doi: 10.1111/sms.12010 [DOI] [PubMed] [Google Scholar]
- Thomee P, Wahrborg P, Borjesson M, Thomee R, Eriksson BI, & Karlsson J. (2006). A new instrument for measuring self-efficacy in patients with an anterior cruciate ligament injury. Scand J Med Sci Sports, 16(3), 181–187. doi: 10.1111/j.1600-0838.2005.00472.x [DOI] [PubMed] [Google Scholar]
- Thomee P, Wahrborg P, Borjesson M, Thomee R, Eriksson BI, & Karlsson J. (2007). Self-efficacy, symptoms and physical activity in patients with an anterior cruciate ligament injury: a prospective study. Scand J Med Sci Sports, 17(3), 238–245. doi: 10.1111/j.1600-0838.2006.00557.x [DOI] [PubMed] [Google Scholar]
- Thomee P, Wahrborg P, Borjesson M, Thomee R, Eriksson BI, & Karlsson J. (2008). Self-efficacy of knee function as a pre-operative predictor of outcome 1 year after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc, 16(2), 118–127. doi: 10.1007/s00167-007-0433-6 [DOI] [PubMed] [Google Scholar]
- Tichonova A, Rimdeikiene I, Petruseviciene D, & Lendraitiene E. (2016). The relationship between pain catastrophizing, kinesiophobia and subjective knee function during rehabilitation following anterior cruciate ligament reconstruction and meniscectomy: A pilot study. Medicina (Kaunas), 52(4), 229–237. doi: 10.1016/j.medici.2016.07.005 [DOI] [PubMed] [Google Scholar]
- Tripp DA, Stanish W, Ebel-Lam A, Brewer BW, & Birchard J. (2007). Fear of reinjury, negative affect, and catastrophizing predicting return to sport in recreational athletes with anterior cruciate ligament injuries at 1 year postsurgery. Rehabilitation Psychology, 52(1), 74–81. doi: 10.1037/0090-5550.52.1.74 [DOI] [Google Scholar]
- Tripp DA, Stanish WD, Reardon G, Coady C, & Sullivan MJ (2003). Comparing Postoperative Pain Experiences of the Adolescent and Adult Athlete After Anterior Cruciate Ligament Surgery. J Athl Train, 38(2), 154–157. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/12937527 [PMC free article] [PubMed] [Google Scholar]
- Van Wyngaarden JJ, Noehren B, & Archer KR (2019). Assessing psychosocial profile in the physical therapy setting. Journal of Applied Biobehavioral Research. doi: 10.1111/jabr.12165 [DOI] [Google Scholar]
- Webster KE, & Feller JA (2019). Expectations for Return to Preinjury Sport Before and After Anterior Cruciate Ligament Reconstruction. Am J Sports Med, 47(3), 578–583. doi: 10.1177/0363546518819454 [DOI] [PubMed] [Google Scholar]
- Widerstrom-Noga EG, Felix ER, Cruz-Almeida Y, & Turk DC (2007). Psychosocial subgroups in persons with spinal cord injuries and chronic pain. Arch Phys Med Rehabil, 88(12), 1628–1635. doi: 10.1016/j.apmr.2007.09.013 [DOI] [PubMed] [Google Scholar]
- Wright RW, Dunn WR, Amendola A, Andrish JT, Bergfeld J, Kaeding CC, . . . Spindler KP. (2007). Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med, 35(7), 1131–1134. doi: 10.1177/0363546507301318 [DOI] [PubMed] [Google Scholar]
- Wright RW, Haas AK, Anderson J, Calabrese G, Cavanaugh J, Hewett TE, . . . Group, M. (2015). Anterior Cruciate Ligament Reconstruction Rehabilitation: MOON Guidelines. Sports Health, 7(3), 239–243. doi: 10.1177/1941738113517855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yee A, Adjei N, Do J, Ford M, & Finkelstein J. (2008). Do patient expectations of spinal surgery relate to functional outcome? Clin Orthop Relat Res, 466(5), 1154–1161. doi: 10.1007/s11999-008-0194-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaffagnini S, Russo RL, Marcheggiani Muccioli GM, & Marcacci M. (2013). The Videoinsight(R) method: improving rehabilitation following anterior cruciate ligament reconstruction--a preliminary study. Knee Surg Sports Traumatol Arthrosc, 21(4), 851–858. doi: 10.1007/s00167-013-2392-4 [DOI] [PubMed] [Google Scholar]