This article presents a decision framework and companion tool linked to a standard, dynamic state-transition model of SARS-CoV-2 transmission on campus to help residential college administrators make decisions about vaccination programs and policies, infection surveillance with varying frequencies of testing and target populations, and use of nonpharmaceutical interventions (for example, distancing and masking), all considered with the goal of returning to pre–COVID-19 operations for the fall 2021 semester.
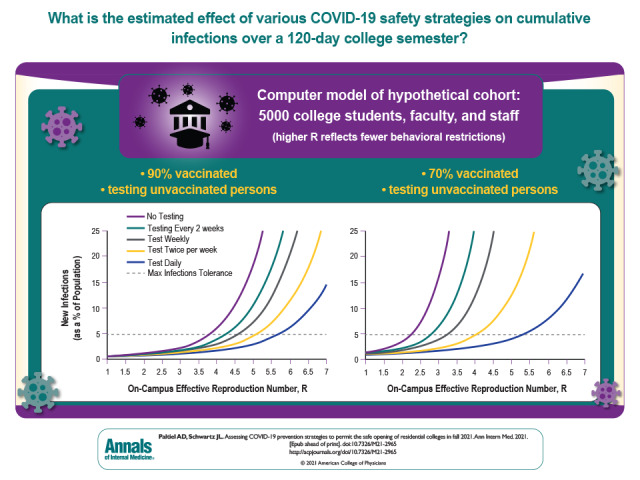
Visual Abstract. Assessing COVID-19 Prevention Strategies to Allow Colleges to Open in Fall.
This article presents a decision framework and companion tool linked to a standard, dynamic state-transition model of SARS-CoV-2 transmission on campus to help residential college administrators make decisions about vaccination programs and policies, infection surveillance with varying frequencies of testing and target populations, and use of nonpharmaceutical interventions (for example, distancing and masking), all considered with the goal of returning to pre–COVID-19 operations for the fall 2021 semester.
Abstract
Background:
Effective vaccines, improved testing technologies, and decreases in COVID-19 incidence prompt an examination of the choices available to residential college administrators seeking to safely resume in-person campus activities in fall 2021.
Objective:
To help college administrators design and evaluate customized COVID-19 safety plans.
Design:
Decision analysis using a compartmental epidemic model to optimize vaccination, testing, and other nonpharmaceutical interventions depending on decision makers' preferences, choices, and assumptions about epidemic severity and vaccine effectiveness against infection, transmission, and disease progression.
Setting:
U.S. residential colleges.
Participants:
Hypothetical cohort of 5000 persons (students, faculty, and staff) living and working in close proximity on campus.
Measurements:
Cumulative infections over a 120-day semester.
Results:
Under base-case assumptions, if 90% coverage can be attained with a vaccine that is 85% protective against infection and 25% protective against asymptomatic transmission, the model finds that campus activities can be resumed while holding cumulative cases below 5% of the population without the need for routine, asymptomatic testing. With 50% population coverage using such a vaccine, a similar cap on cumulative cases would require either daily asymptomatic testing of unvaccinated persons or a combination of less frequent testing and resumption of aggressive distancing and other nonpharmaceutical prevention policies. Colleges returning to pre–COVID-19 campus activities without either broad vaccination coverage or high-frequency testing put their campus population at risk for widespread viral transmission.
Limitation:
Uncertainty in data, particularly vaccine effectiveness (preventive and transmission); no distinguishing between students and employees; and assumes limited community intermixing.
Conclusion:
Vaccination coverage is the most powerful tool available to residential college administrators seeking to achieve a safe return to prepandemic operations this fall. Given the breadth of potential outcomes in the face of uncontrollable and uncertain factors, even colleges with high vaccination rates should be prepared to reinstitute or expand testing and distancing policies on short notice.
Primary Funding Source:
National Institute on Drug Abuse.
Residential colleges throughout the United States are once again confronting the challenges posed by SARS-CoV-2 in their planning for operations during the approaching academic year. As in 2020, the characteristic features of campus life—communal living arrangements with shared dining, sleeping, and bathing spaces; classrooms, performance spaces, and athletic venues of varying size and density; and a population of young adults eager to socialize—raise concerns about superspreading and the safety of neighboring communities (1–3).
This year, however, residential college administrators are presented with a dramatically more favorable context on which to act than they encountered in summer 2020. Chief among the differences is the widespread availability of several, highly effective vaccines. Vaccines in use in the United States have dramatically reduced the incidence of symptomatic disease (4). Additional evidence shows reductions in viral transmission and infections, notably asymptomatic infections (5). Breakthrough infections among vaccinated persons are uncommon and generally minor in severity (6).
Last year's experience also showed the considerable benefits of testing for SARS-CoV-2 and nonpharmaceutical interventions (NPIs) (7). Residential colleges that adhered assiduously to a combination of high-cadence testing, dedensification, masking, hand washing, and social distancing seem to have substantially reduced the transmission of infection on their campuses during the 2020–2021 academic year (8, 9). Routine, asymptomatic screening can now be done effectively and conveniently at marginal costs as low as $2.50 per test (10, 11).
These observations suggest that the question facing residential college officials is not whether there exists a safe approach to bringing students onto campus this fall. Rather, their challenge is how best to design and implement a portfolio of strategies—a combination of vaccination policies, virologic monitoring, and NPIs—that will strike what they consider an appropriate balance between adequate outbreak control and restoration of the residential college experience.
The purpose of this report is to provide evidence and structure to address that challenge. We offer a quantitative framework that supports exploration of policy approaches and evaluates the feasibility and compatibility of different combinations of strategies and performance targets. Because background conditions and risk tolerance will vary among residential colleges and their epidemiologic settings, we have also developed a publicly available spreadsheet implementation of our model-based analysis (Supplement 1). This companion tool permits residential college decision makers not only to reproduce the results reported here but also to design a customized portfolio of strategies that reflects their institution's specific priorities and circumstances.
Methods
Analytic Overview
We developed a decision framework to help residential college administrators make decisions about vaccination programs and policies, infection surveillance with varying frequencies of testing and target populations, and use of NPIs (for example, distancing and masking), all considered with the goal of returning to pre–COVID-19 operations for the fall 2021 semester. We linked this framework to a standard, state-transition model of SARS-CoV-2 transmission on campus (1). This permitted us to capture the dynamic interaction of alterative interventions and measure their combined effect on cumulative infections over a 120-day semester.
Choices and Preferences
Motivating our approach is the contention that those responsible for setting policies for residential colleges—for example, school administrators, state-appointed overseers, government education officials, or governors or other elected officials—express their priorities about campus COVID-19–related health and wellness measures via the choices they make in the following 4 domains:
1. Efforts to promote high vaccination coverage. Rates of vaccination on college campuses this fall will vary widely, mirroring the large differences in both vaccination coverage across U.S. regions and the intensity with which residential college officials have encouraged vaccination (12). Colleges that have elected to do nothing to actively encourage vaccination will nevertheless benefit from ongoing national vaccination efforts and can plausibly anticipate that 50% of their campus population will be vaccinated (13). Colleges that have taken a more active approach have done so with varying degrees of aggressiveness. For purposes of illustration, we have chosen 70% as a mid-range value and 90% as our upper-bound value, one that should be attainable by colleges that are vigorously ensuring adherence to an explicit vaccination requirement.
2. Testing frequency and targeting. Current guidelines differ on both the frequency and targeting of routine, asymptomatic screening for SARS-CoV-2 infection in college settings (11, 14, 15). Some residential colleges may elect to target screening activities solely toward unvaccinated persons; others may test all members of the campus community, regardless of vaccination status; others may test vaccinated and unvaccinated members of the community with different frequencies; and still others may retire their asymptomatic testing programs and test only symptomatic persons. In the illustrative examples that follow, we consider both targeted and untargeted testing using nucleic acid amplification testing with a reverse transcriptase polymerase chain reaction assay at rates ranging from once every 2 weeks to daily. We also consider the option of restricting testing to persons with symptoms.
3. Priority given to restoring the prepandemic college experience. In planning for the fall 2021 semester, decision makers reveal their institutional priorities and preferences when they weigh measures aimed at keeping everyone healthy and minimizing the risks for COVID-19 against measures aimed at restoring the activities of residential college campus life experienced before the pandemic. The balance between these competing objectives may be struck at any point on the continuum that runs between a total lockdown at one extreme and an unrestricted return to pre–COVID-19 college activities at the other extreme. This continuum is not just a conceptual abstraction; one may quantify choice of location on that continuum using the on-campus, effective reproduction number (R*), a measure that takes into account a college's adoption of NPIs before any vaccination or testing interventions against the background epidemiology of the pandemic in the surrounding community (16).
In fall 2020, choices on some of the nation's campuses tilted heavily toward reducing COVID-19 cases and transmission—with little-to-no in-person instruction; minimal athletics, performances, or other extracurriculars; dedensified dormitories; large-scale asymptomatic screening programs; distancing; masking; and other measures. The R* on these campuses may have been close to 0. On other campuses, attention to NPIs was less aggressive and the on-campus R* likely exceeded its off-campus analog. Statewide estimates of the effective reproduction number in the United States range from roughly 0.5 to 1.5 (17). However, recent reports suggest that new viral variants may have reproduction numbers as high as 7 (18). In the illustrative examples that follow, we adopt a conservative baseline value of R* of 3, reflecting the desire of many college decision makers to return to the intimacy of pre–COVID-19 residential campus activities without physical distancing but also accounting for the threat of new variants (11).
4. Tolerance for campus infections. It is unrealistic to expect that all pre–COVID-19 activities can be resumed this fall while simultaneously eliminating all viral transmission on campus. A more reasonable expectation is that the cumulative number of infections on campus may be held below some ceiling that has been deemed “tolerable.” College administrators may object to the notion of specifying an explicit threshold. However, the degree to which “acceptable campus infections” constitutes at the very least an implicit, if not explicit, choice—one that reflects decision makers' preferences and institutional priorities—can be inferred from the widely divergent responses to outbreaks seen during the 2020–2021 academic year (19, 20). For purposes of illustration, we use a ceiling of 5%, noting that this value includes both asymptomatic and symptomatic cases.
In articulating these 4 domains of residential college responses to COVID-19 for fall 2021, we make no value judgments. Rather, we treat each as an independent choice that reveals useful information about decision makers' preferences, priorities, and constraints. Our aim is to assemble these choices and to report on their mutual compatibility, given current knowledge about the virus, its epidemiology, and the effect of vaccines and NPIs. If a set of choices is not feasible, the epidemic model can point to the additional concessions or responses that may be required.
Analytic Model
We updated the standard compartmental epidemic model first developed for our July 2020 analysis of campus screening options (1). A full description of the model and input data assumptions is provided in Supplement 2. This model captures many of the essential features of the situation facing college decision makers: the epidemiology of SARS-CoV-2; the natural history of COVID-19 illness; and the availability of testing technologies to detect, isolate, and contain the presence of SARS-CoV-2 in a residential college setting (Supplement Figure). The updated model adds functionality to account for the presence of persons who have achieved antibody protection, either as the result of prior infection with SARS-CoV-2 or via vaccination. The model permits users to specify 3 kinds of antibody protection: protection from infection (measured as a percentage reduction in susceptibility to so-called “breakthrough infections”), protection from transmission (measured as a percentage reduction in the probability of transmission of infection to others), and disease modification (measured as a percentage reduction in the risk for progression to hospitalization and death). To account for waning protection over time, the model also permits users to specify a rate of decay for the first 2 of these forms of protection.
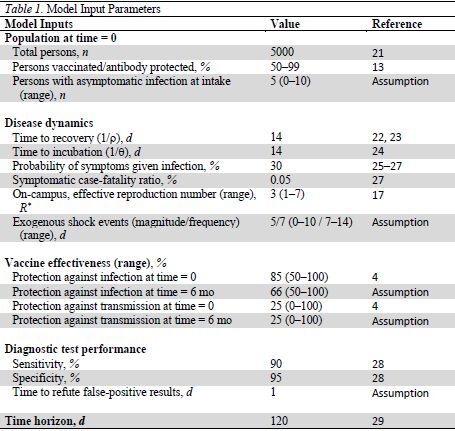
Input data for the illustrative results reported below were obtained from various published sources (4, 13, 17, 21–29) (Table 1 and Supplement 2), adhering whenever possible to the data guidance for modelers issued by the Centers for Disease Control and Prevention (27). Interested readers may explore alternative input data assumptions using the publicly available spreadsheet implementation of the model.
Table 1.
Model Input Parameters
Sensitivity Analysis
Beyond the 4 domains of decision making described earlier, there are a host of factors and uncertainties over which college administrators have no influence. To help decision makers understand how the consequences of their choices may vary in the face of variation in these uncontrollable factors, we conducted illustrative sensitivity analysis on vaccine effectiveness (preventive and transmission); the rate of decay in effectiveness; the frequency and magnitude of imported infections (such as those that may arise as a result of mixing between a campus community and surrounding, off-campus communities); and the presence of undetected, asymptomatic persons on campus at the start of the semester. Additional explorations may be done using the publicly accessible implementation of the model (Supplement 1).
This analysis adheres to the Consolidated Health Economic Evaluation Reporting Standards reporting guideline, where applicable (30). Because this study used only aggregate, published data, the institutional review board of the Yale School of Medicine (protocol ID 2000030998) determined that this research did not involve human participants and did not require its review or approval.
Role of the Funding Source
The funder had no role in the design, conduct, or data analysis of the study or the decision to submit the manuscript for publication.
Results
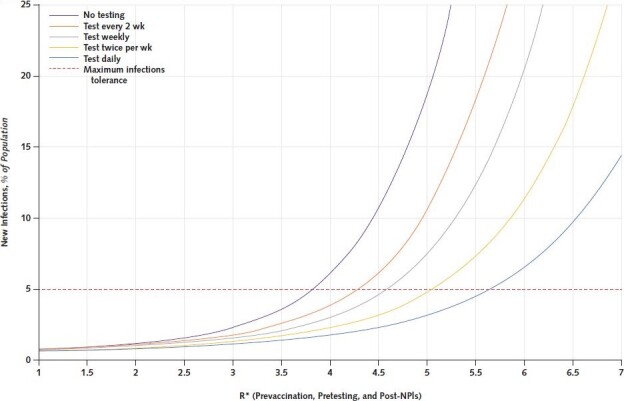
Figure 1 reports the findings of the model under baseline input data assumptions, assuming 50% coverage with a vaccine that is 85% protective against infection and 25% protective against asymptomatic transmission. In the absence of any testing, cumulative infections could be held below 5% of the campus population but only if R* less than 1.5 were maintained, consistent with the resumption of aggressive distancing and other NPI prevention policies. With increasingly frequent testing of the unvaccinated population (weekly, twice a week, or daily), a 5% cap on cumulative infections may be achieved at progressively higher levels of R* (2.5, 3.5, and 5.25, respectively). Of note, without either testing or distancing policies, a return to pre–COVID-19 campus life and activities could result in the infection of virtually all unvaccinated members of the population before the end of the semester (extending the purple curve beyond the boundaries of Figure 1).
Figure 1. Cumulative infections with 50% vaccination coverage and testing targeted to the unvaccinated population alone.
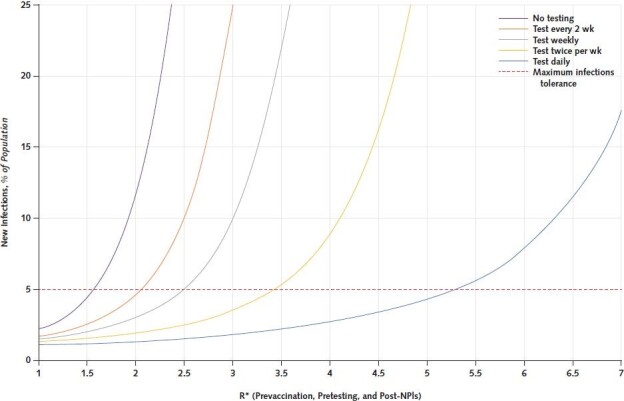
The figure illustrates the findings of the model under baseline input data assumptions, assuming 50% vaccination coverage. The curves report the expected cumulative infections in the population over a 120-day semester (y-axis) under alternative frequencies of routine, asymptomatic testing of unvaccinated persons (ranging from no testing to testing every day). The R* is inversely related to the aggressiveness of NPI measures, such as masking and distancing. In the absence of any testing (purple curve), cumulative infections may be held below 5% of the campus population (horizontal red dashed line) if R* is < 1.5 (that is, implementation of aggressive NPIs). With testing twice a week (yellow curve), that level of cumulative infections could be achieved at R* values of < 3.5; with daily testing (blue curve), it could be achieved at R* values of < 5.25. NPI = nonpharmaceutical intervention; R* = on-campus, effective reproduction number.
Increasing vaccination coverage to 70% produces small improvements in the model's predicted outcomes (Figure 2). Without any testing, holding R* less than 2.25 could keep cumulative infections below 5%; with increasingly frequent testing (weekly, twice a week, or daily) of the unvaccinated population, that same 5% level of cumulative infections could be achieved at R* of 3.25, 4.1, and 5.4, respectively. Cumulative infections could be held below 10% by testing every 2 weeks while implementing distancing and other NPIs to keep R* less than 3.4.
Figure 2. Cumulative infections with 70% vaccination coverage and testing targeted to the unvaccinated population alone.
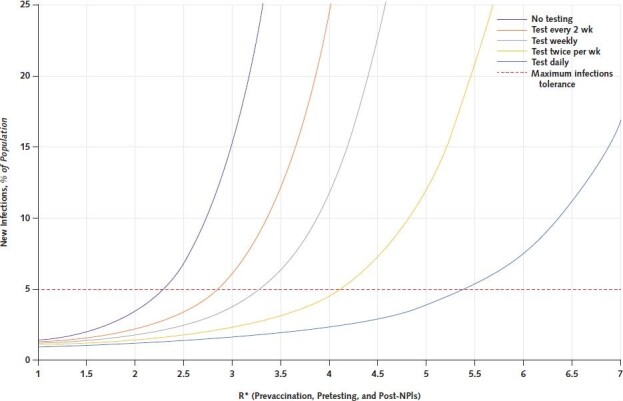
The figure illustrates the findings of the model under baseline input data assumptions, assuming 70% vaccination coverage. The curves report the expected cumulative infections in the population over a 120-day semester (y-axis) under alternative frequencies of routine, asymptomatic testing of unvaccinated persons (ranging from no testing to testing every day). The R* is inversely related to the implementation of NPI measures, such as masking and distancing. In the absence of any testing (purple curve), cumulative infections may be held below 5% of the campus population (horizontal red dashed line) if R* is <2.25 (that is, implementation of aggressive NPIs). With testing twice a week (yellow curve), that level of cumulative infections could be achieved at R* values of <4.2; with daily testing (blue curve), it could be achieved at R* values of <5.4. NPI = nonpharmaceutical intervention; R* = on-campus, effective reproduction number.
The model suggests that under baseline input data assumptions, the need for any asymptomatic testing would be eliminated at colleges that can achieve vaccination coverage levels of 90% while holding R* less than 3.75 (Figure 3).
Figure 3. Cumulative infections with 90% vaccine coverage and testing targeted to the unvaccinated population alone.
The figure reports the findings of the model under baseline input data assumptions, assuming 90% vaccination coverage. The curves denote the expected cumulative infections in the population over a 120-day semester (y-axis) under alternative frequencies of routine, asymptomatic testing of unvaccinated persons (ranging from daily testing to no asymptomatic testing). The R* is inversely related to the aggressiveness of NPI measures, such as masking and distancing. In the absence of any testing (purple curve), cumulative infections may be held below 5% of the campus population (horizontal red dashed line) if R* is kept <3.75. With testing twice a week (yellow curve), that level of cumulative infections could be achieved at R* values of <5.0; with daily testing (blue curve), it could be achieved at R* values of <5.6. NPI = nonpharmaceutical intervention; R* = on-campus, effective reproduction number.
Sensitivity Analysis
Vaccine Effectiveness
In general, less optimistic assumptions about vaccine effectiveness necessitate greater attention to both screening and distancing options. The Appendix Figure reports findings with vaccine preventive effectiveness lowered to 75% (decreasing to 50% at 6 months) and transmission effectiveness set to 0%. The effects of lower vaccination effectiveness are most pronounced at higher vaccination coverage rates. With vaccination coverage of 90%, for example, the model suggests that R* less than 2.75 may be required to hold cumulative case rates below 5%, even with frequent testing of the unvaccinated population (Appendix Figure, C).
Appendix Figure. Sensitivity to vaccine effectiveness.
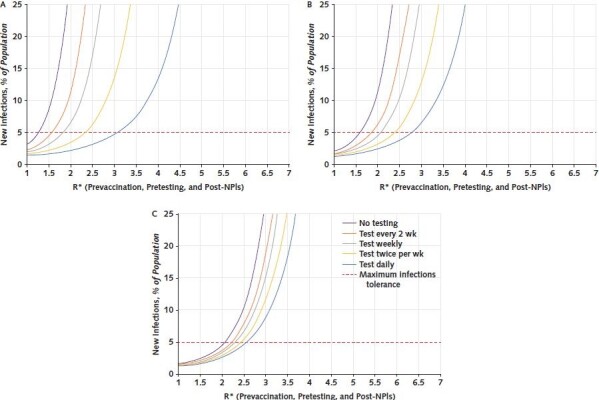
The figure reports cumulative infections under baseline input data assumptions but with vaccine preventive effectiveness lowered to 75% (decreasing to 50% at 6 months) and transmission effectiveness set to 0%. Asymptomatic testing is targeted to the unvaccinated population at frequencies ranging from no testing to daily testing. NPI = nonpharmaceutical intervention; R* = on-campus, effective reproduction number. A. With 50% vaccination coverage and in the absence of any testing (purple curve), the R* to hold cumulative infections below 5% (horizontal red dashed line) must now be <1.25 (from 1.5 under baseline conditions); with testing twice a week (yellow curve), the R* must remain below 2.4 (previously 3.5). The effects of lower vaccination effectiveness are more pronounced at higher vaccination coverage rates. B. At 70% coverage, in the absence of any testing (purple curve), the R* to hold cumulative infections below 5% (horizontal red dashed line) must now be <1.6 (from 2.25 under baseline conditions); with testing twice a week (yellow curve), the R* must remain below 2.3 (previously 4.5). C. At 90% coverage, in the absence of any testing (purple curve), the R* to hold cumulative infections below 5% (horizontal red dashed line) must now be <2.1 (from 3.75 under baseline conditions); with testing twice a week (yellow curve), the R* must remain below 2.4 (previously 5.0).
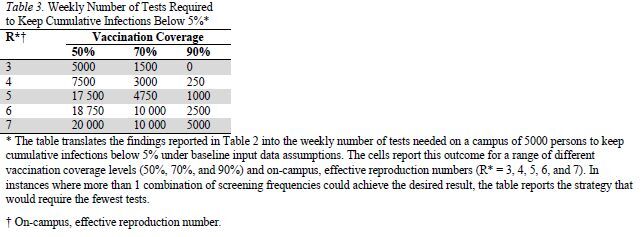
Differential Testing Based On Vaccination Status
Table 2 reports the screening frequencies (for unvaccinated and vaccinated persons, respectively) that would be required to hold cumulative infections below 5% for a range of different vaccination coverage and R* levels. At schools that can achieve higher vaccination levels or lower values of R*, it may be optimal to target testing activities to the unvaccinated population; as coverage or vaccine effectiveness levels decrease or R* increases, testing of both vaccinated and unvaccinated members of the population may be needed. In several instances, more than 1 combination of screening frequencies could achieve the desired result. Table 3 translates these findings into the weekly number of tests that would be needed on a campus of 5000 persons and shows the nonlinearly increasing marginal benefits of both greater vaccination coverage and reduced R*.
Table 2.
Screening Frequencies Required to Keep Cumulative Infections Below 5%*
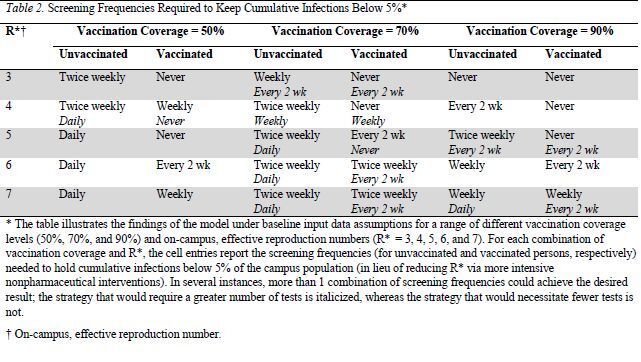
Table 3.
Weekly Number of Tests Required to Keep Cumulative Infections Below 5%*
Discussion
As residential colleges prepare for the fall 2021 semester, several conclusions with implications for their planning emerge from this modeling exercise, including the paradigmatic scenarios presented earlier and the countless alternative designs that can be examined using the publicly available companion tool.
First, one size does not fit all. No single, “optimal” plan for college reopening captures the breadth of institutional circumstances and priorities on campuses nationwide. The curves presented in the Results section are highly malleable and dependent on idiosyncratic choices that fall within the control of decision makers. These interdependent choices include the degree to which they seek a resumption of the pre–COVID-19 campus experience through the relaxation of NPIs (for example, masking and social distancing); the efforts they undertake to promote or ensure very high vaccination rates, including through the use of requirements; and the number of cases they deem to be within acceptable levels. Therefore, residential college administrators can and should tailor their public health strategies to their particular settings, conditions, and concerns, recognizing the tradeoffs inherent in any policy approach. The spreadsheet implementation of our analysis is available to support such an exercise (Supplement 1).
Second, an adaptive contingency plan must be developed. Just as there is considerable uncertainty with respect to the trajectory of the COVID-19 pandemic in the months ahead, so too is there uncertainty about the suitability of any static approach intended to facilitate the safe return to on-campus college life over a months-long time horizon. The curves presented in the Results section are highly sensitive to the uncertainties in the underlying data. Plausible variation in factors beyond the control of decision makers—the preventive effectiveness of the vaccine, the emergence of new viral variants, an unexpected death, or legal action, to cite just a few possibilities—can produce greatly divergent outcomes. Given that some of these uncertain factors can change rapidly, even residential colleges that enter fall 2021 in an apparent favorable position should remain vigilant and prepared to quickly alter their approaches if conditions warrant. The emergence of the Delta variant during summer 2021 illustrates the speed with which the trajectory of the pandemic can change and the corresponding need for residential college officials to reevaluate their plans and responses just as rapidly. The Delta variant has also prompted many colleges to reinstate indoor masking policies in an effort to hold down the R* when students return to campus this fall. Masks were a highly effective NPI during the 2020–2021 academic year and are less disruptive to the campus experience and environment than NPIs, such as distancing or dedensification (for example, hybrid or fully remote learning). Unlike those NPIs, mask use can also be suspended or reinstated on short notice as conditions change.
Third, vaccine coverage should be maximized. Of the many factors within the control of residential college decision makers planning for fall 2021, the level of vaccination in the campus community is likely to be the single most powerful determinant of safety, as measured through the number of cases occurring among students, faculty, and staff. Residential colleges with high vaccination rates—particularly those exceeding 90%—can insulate themselves against most of the threats that will otherwise prompt widespread or frequent testing and a return to more intensive or disruptive NPIs. Vaccination also offers the most reliable envelope of protection in the face of potential worsening public health conditions leading to increased R*. Colleges will enter the fall 2021 semester with widely varying vaccination rates, in part a result of the presence or absence of requirements for students, faculty, or staff. Beginning the semester with a very high vaccination rate is clearly more desirable, but all colleges—especially those with moderate or low vaccination rates as the fall begins—should support ongoing efforts to maximize vaccination coverage throughout the semester given its clear individual and community benefits.
Fourth, emerging data on vaccine effectiveness should be monitored. Of the many factors that lie beyond the control of decision makers planning for fall 2021, none is as worrisome as a potential decrease in vaccine effectiveness. Students, faculty, and staff will arrive on campus having been vaccinated using any number of vaccines—1 of the 3 authorized by the U.S. Food and Drug Administration or 1 of the several other vaccines in use internationally. Although the U.S.-authorized vaccines all show high levels of protection against severe outcomes, their overall effectiveness varies, and evidence about their performance against variants like Delta continues to emerge. Less is known about the effectiveness of international vaccines authorized by the World Health Organization, particularly the protection they provide against variants. Although evidence suggests that vaccines have largely remained resilient against the challenges presented by current variants—particularly against severe outcomes—even modest reductions in overall vaccine effectiveness in the months ahead could substantially alter the degree to which a campus reopening plan is adequate to provide the level of community protection sought by decision makers. Careful attention by residential college officials to new evidence about vaccine effectiveness and related guidance from local, state, and health officials will be essential to a sustainable fall 2021 semester on campus.
Fifth, the targeting of testing activities should be carefully considered. Decision makers have the option not only to institute a program of routine asymptomatic testing for SARS-CoV-2 but also to determine whether that program should be applied to all members of the campus community or only those who remain unvaccinated. Our exploratory investigations suggest that the benefits of extending routine testing to the broader population may be greatest when campus vaccination rates are very low (that is, about 50% or lower) or the vaccine is found to be much less effective than evidence has indicated. In addition to those limited benefits of widespread testing, such programs are financially costly to colleges and increase the risk for false-positive results, which can lead to disruptions and confusion. Residential colleges that limit required, routine testing only to unvaccinated members of their community also gain the opportunity for that policy to serve as an incentive for persons to be vaccinated.
The simple model underlying this analysis has notable limitations. We assumed a homogeneous population encompassing all persons—students, faculty, and staff—living and working in close, regular physical proximity to one another in a campus setting. We did not explicitly take into account nonrandom mixing patterns, age-dependent transmission, or any of the other evident differences between students and university employees, although nonstudent members of the college community include a higher proportion of older, more medically vulnerable persons. Also, we do not distinguish between students living in dormitories and those living in off-campus settings. Thus, this model may not work well for colleges with large percentages of commuting students. These are important distinctions deserving further exploration, but they are beyond the scope of this analysis. Finally, we remind readers that the outputs of any model-based analysis are only as reliable as the input data assumptions that produced them. Our deterministic model reports crude averages only and does not account for any stochastic variation. Ideally, we would have done a calibration exercise and provided confidence ranges, not only for the parameter values in Table 1 but also for the curves presented in the figures; such an exercise is beyond both the scope of this analysis and the current state of the evidence base. We urge readers to note the absence of these important features, to interpret our results with caution, and to avail themselves of the companion spreadsheet (Supplement 1) to reassess decisions as better input data become available.
Recent guidance documents for institutions of higher education have been released by the Centers for Disease Control and Prevention, the American College Health Association, the Massachusetts Higher Education Testing Group, and other organizations (11, 14, 15). Each strives to support decision making by residential college officials preparing for a safe reopening for the fall 2021 semester while restoring as much of the pre–COVID-19 on-campus experience as possible. Our analysis aims to inform and enhance that work, providing a tool that illuminates the complex interplay of choices available to decision makers as they consider their institutional circumstances, priorities, and needs in the face of an ongoing and uncertain public health threat.
Supplementary Material
Footnotes
This article was published at Annals.org on 31 August 2021.
References
- 1.Paltiel AD , Zheng A , Walensky RP . Assessment of SARS-CoV-2 screening strategies to permit the safe reopening of college campuses in the United States. JAMA Netw Open. 2020;3:e2016818. [PMID: ] doi: 10.1001/jamanetworkopen.2020.16818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chang JT , Crawford FW , Kaplan EH . Repeat SARS-CoV-2 testing models for residential college populations. Health Care Manag Sci. 2021;24:305-318. [PMID: ] doi: 10.1007/s10729-020-09526-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Losina E , Leifer V , Millham L , et al. College campuses and COVID-19 mitigation: clinical and economic value. Ann Intern Med. 2021;174:472-483. [PMID: ] doi: 10.7326/M20-6558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. COVID-19 vaccines work. Accessed at www.cdc.gov/coronavirus/2019-ncov/vaccines/effectiveness/work.html on 25 August 2021.
- 5.Levine-Tiefenbrun M , Yelin I , Katz R , et al. Initial report of decreased SARS-CoV-2 viral load after inoculation with the BNT162b2 vaccine. Nat Med. 2021;27:790-792. [PMID: ] doi: 10.1038/s41591-021-01316-7 [DOI] [PubMed] [Google Scholar]
- 6.CDC COVID-19 Vaccine Breakthrough Case Investigations Team.. COVID-19 vaccine breakthrough infections reported to CDC - United States, January 1-April 30, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:792-793. [PMID: ] doi: 10.15585/mmwr.mm7021e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haug N , Geyrhofer L , Londei A , et al. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat Hum Behav. 2020;4:1303-1312. [PMID: ] doi: 10.1038/s41562-020-01009-0 [DOI] [PubMed] [Google Scholar]
- 8.Fox MD , Bailey DC , Seamon MD , et al. Response to a COVID-19 outbreak on a university campus - Indiana, August 2020. MMWR Morb Mortal Wkly Rep. 2021;70:118-122. [PMID: ] doi: 10.15585/mmwr.mm7004a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schultes O, Clarke V, Paltiel AD, et al. COVID-19 in Connecticut institutions of higher education during the 2020-2021 academic year. medRxiv Preprint posted online 13 August 2021. doi:10.1101/2021.08.11.21261732
- 10.Centers for Disease Control and Prevention. Overview of testing for SARS-CoV-2 (COVID-19). Accessed at www.cdc.gov/coronavirus/2019-ncov/hcp/testing-overview.html on 25 August 2021.
- 11.Massachusetts Higher Education Testing Group. Report and recommendations of the Massachusetts Higher Education Testing Group. 4 May 2021. Accessed at https://covid.risd.edu/wp-content/uploads/2021/05/2021-Higher-Ed-Testing-Group-Report-and-Broad-Institute-Proposal-Final-2.pdf on 25 August 2021.
- 12.Thomason A, O'Leary B. Here's a list of colleges that require students or employees to be vaccinated against Covid-19. The Chronicle of Higher Education. 24 August 2021. Accessed at www.chronicle.com/blogs/live-coronavirus-updates/heres-a-list-of-colleges-that-will-require-students-to-be-vaccinated-against-covid-19 on 25 August 2021.
- 13.Centers for Disease Control and Prevention. COVID data tracker: COVID-19 vaccinations in the United States. Accessed at https://covid.cdc.gov/covid-data-tracker/#vaccinations on 25 August 2021.
- 14.Centers for Disease Control and Prevention. Considerations for institutions of higher education. Accessed at www.cdc.gov/coronavirus/2019-ncov/community/colleges-universities/considerations.html on 25 August 2021.
- 15.American College Health Association. Considerations for reopening institutions of higher education for the fall semester 2021. Accessed at www.acha.org/documents/resources/guidelines/ACHA_Considerations_for_Reopening_IHEs_for_Fall_2021_5.25.21.pdf on 25 August 2021.
- 16.Gostic KM , McGough L , Baskerville EB , et al. Practical considerations for measuring the effective reproductive number, Rt. PLoS Comput Biol. 2020;16:e1008409. [PMID: ] doi: 10.1371/journal.pcbi.1008409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Covidestim: COVID-19 nowcasting. Accessed at https://covidestim.org/ on 25 August 2021.
- 18.Rigby J, Newey S, Nuki P, et al. Delta variant Q&A: are the symptoms different, and do vaccines protect against it? The Telegraph. 16 July 2021. Accessed at https://www.telegraph.co.uk/global-health/science-and-disease/delta-variant-symptoms-signs-different-do-vaccines-protect/ on 25 August 2021.
- 19.Fausset R. Outbreaks drive U.N.C. Chapel Hill online after a week of classes. The New York Times. 17 August 2020. Accessed at www.nytimes.com/2020/08/17/us/unc-chapel-hill-covid.html?smid=url-share on 25 August 2021.
- 20.University of Wisconsin–Madison. COVID-19 response dashboard. Accessed at https://covidresponse.wisc.edu/dashboard/ on 25 August 2021.
- 21.Moody J. 10 colleges with the most undergraduate students. U.S. News & World Report. 29 September 2020. Accessed at www.usnews.com/education/best-colleges/the-short-list-college/articles/colleges-with-the-most-undergraduates on 25 August 2021.
- 22.Lauer SA , Grantz KH , Bi Q , et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172:577-582. [PMID: ] doi: 10.7326/M20-0504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Quarantine if you might be sick. Accessed at www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/quarantine-isolation.html on 25 August 2021.
- 24.He X , Lau EHY , Wu P , et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26:672-675. [PMID: ] doi: 10.1038/s41591-020-0869-5 [DOI] [PubMed] [Google Scholar]
- 25.Sah P , Fitzpatrick MC , Zimmer CF , et al. Asymptomatic SARS-CoV-2 infection: A systematic review and meta-analysis. Proc Natl Acad Sci U S A. 2021;118. [PMID: ] doi: 10.1073/pnas.2109229118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Subramanian R , He Q , Pascual M . Quantifying asymptomatic infection and transmission of COVID-19 in New York City using observed cases, serology, and testing capacity. Proc Natl Acad Sci U S A. 2021;118. [PMID: ] doi: 10.1073/pnas.2019716118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention. COVID-19 pandemic planning scenarios. Accessed at www.cdc.gov/coronavirus/2019-ncov/hcp/planning-scenarios.html on 25 August 2021.
- 28.Infectious Diseases Society of America. IDSA guidelines on the diagnosis of COVID-19: molecular diagnostic testing. Accessed at www.idsociety.org/practice-guideline/covid-19-guideline-diagnostics/ on 25 August 2021. [DOI] [PMC free article] [PubMed]
- 29.Yale University. Academic calendar. Accessed at https://yalecollege.yale.edu/academics/academic-calendar/2021-2022-academic-calendar on 25 August 2021.
- 30.Husereau D , Drummond M , Petrou S , et al; ISPOR Health Economic Evaluation Publication Guidelines-CHEERS Good Reporting Practices Task Force. Consolidated health economic evaluation reporting standards (CHEERS)—explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Health. 2013;16:231-50. [PMID: ] doi: 10.1016/j.jval.2013.02.002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


