Abstract
Industry 4.0 has transformed manufacturing industry into a new paradigm. In a manner similar to manufacturing, health care delivery is at the dawn of a foundational change into the new era of smart and connected health care, referred to as Health Care 4.0. In this paper, we discuss the historical evolution of Health Care 1.0 to 4.0, describe the characteristics of smart and connected care in Health Care 4.0, identify multiple research challenges and opportunities of Health Care 4.0 in terms of data, model, dynamics, and integration, and outline the implications of people, process, system and health outcomes. Finally, conclusions and recommendations are presented in the areas of (1) involvement of multiple disciplines and perspectives, (2) development of technologies and methodologies with combination of quantitative and qualitative approaches, (3) closed-loop integration of sociotechnical system, and (4) design of person-centered system with specific attention to human needs and health equity.
Keywords: Health Care 4.0, Industry 4.0, smart and connected health care
1. Introduction
Worldwide, we have seen growing interest in engineering approaches to health care delivery in a context of rapid development in medical devices, clinical advancement, data analytics, and information technology. Recent breakthroughs in digital health technologies (e.g., electronic health records, health monitoring and wearable devices) are not only transformative for reengineering care processes and improving health care outcomes such as care quality and patient safety, but can also have major socio-economic impact, as almost 20% of the US GDP is dedicated to health expenditures. These technological developments have generated numerous innovation opportunities as well as substantial challenges for care delivery, and are offering a chance to move beyond the traditional scope of health care engineering, such as process improvement and technology implementation. There has been a growing realization that information technology, systems engineering tools, and organizational innovations play critical roles to address the interrelated quality and productivity crises faced by health care systems around the world (Kaplan et al. 2013, Cassel et al. 2014, Reid et al. 2005). Such technologies and tools can support health care systems in achieving the Quadruple Aim of improving the patient experience, population health, cost control and clinician satisfaction (Sikka et al. 2015). The Healthcare Systems Engineering (HSE) community has a critical role to play in addressing these challenges.
Industry 4.0 has transformed manufacturing industry into a new paradigm (Lasi et al. 2014, Rubmann et al. 2015, Liao et al. 2017) – the smart, cybernized, and sustainable manufacturing era, and has produced substantial improvements in productivity, quality, and/or customer satisfaction of processes, products, and services. Such revolutionary changes can bring about significant impact not only on manufacturing, but also on every aspect of our society, including health care, which has started to embrace these technological innovations. In a manner similar to manufacturing, health care delivery is at the dawn of a paradigm change to reach the new era, referred to as Health Care 4.0. Various diagnosis and treatment options are continuously and exponentially being introduced, extensive data are generated and reported, numerous wired and wireless equipment, sensors, and devices have been installed in hospitals, clinics, home, pharmacies, and many other care environments. In addition, revolutionary updates on computation power have been achieved, novel machine learning, statistics, and artificial intelligence (AI) algorithms are becoming more widespread, new and complex modeling and optimization techniques have been developed, and cognitive impacts are increasingly considered and human factors methods are integrated in the design of technological innovations. These innovations will significantly expand the social and technical capabilities of care delivery, and have the potential, if well designed, implemented and used, to improve care quality, patient experience and outcomes, population health, and clinician satisfaction; therefore, leading to significant benefits to communities and society at large.
Although we have seen progress in smart and connected health care, more research innovation, dissemination and impact are needed to achieve Health Care 4.0. The goal of this paper is to discuss the transition to Health Care 4.0, identify its elements, and propose opportunities and challenges for research on Health Care 4.0.
The remainder of the paper is structured as follows: sections 2 and 3 introduce the history and evolution of Industry 1.0 to 4.0 and of Health Care 1.0 to 4.0, respectively. The elements of Health Care 4.0 are presented in section 4, while challenges and implications for research are summarized in section 5. Finally, conclusions are formulated in section 6.
2. Transition from Industry 1.0 to Industry 4.0
Industry 1.0 represents the first industrial revolution, starting in the 18th century all the way to the mid- and late 19th century. Along with the emerging technologies of steam engine, sewing machines, steel making, and railroads, a mechanization revolution facilitated the societal move from agriculture to industrialization.
From the end of the 19th century to the beginning of the 20th century, the second industry revolution, so-called Industry 2.0, introduced a paradigm change from individual or small-scale manufacturing to large-volume mass production, due to the paramount usage of electricity. The Henry Ford assembly lines enabled systematic allocation and connection of numerous operations and machines efficiently, which completely changed manufacturing processes.
During the last few decades of the 20th century, the rapid development of electronics, computer, and robotic technology has led to massive applications of automation systems, characterized by digitalization and networking of manufacturing and business processes. Computer-integrated and flexible manufacturing systems, manufacturing executive systems, as well as material resource planning and enterprise resource planning, have been widely adopted, which marked the third industry revolution, i.e., Industry 3.0, and also led to the dawn of the fourth revolution.
Stepping into the 21st century, Industry 4.0 represents the fourth industry revolution and aims to integrate cyber-physical systems with information, process, equipment, and operation technologies. The Internet of Things (IoT) and associated services are extensively distributed and used in conjunction with big data analytics and artificial intelligence techniques. Through internet-enabled and cloud-based diagnosis, operation, control, and maintenance of facilities, products, and business processes, we can achieve a smart, sustainable, and cost-effective connection (i.e., integration) of supply, manufacturing, and service. The historical evolution from Industry 1.0 to 4.0 is illustrated in Figure 1.
Figure 1.
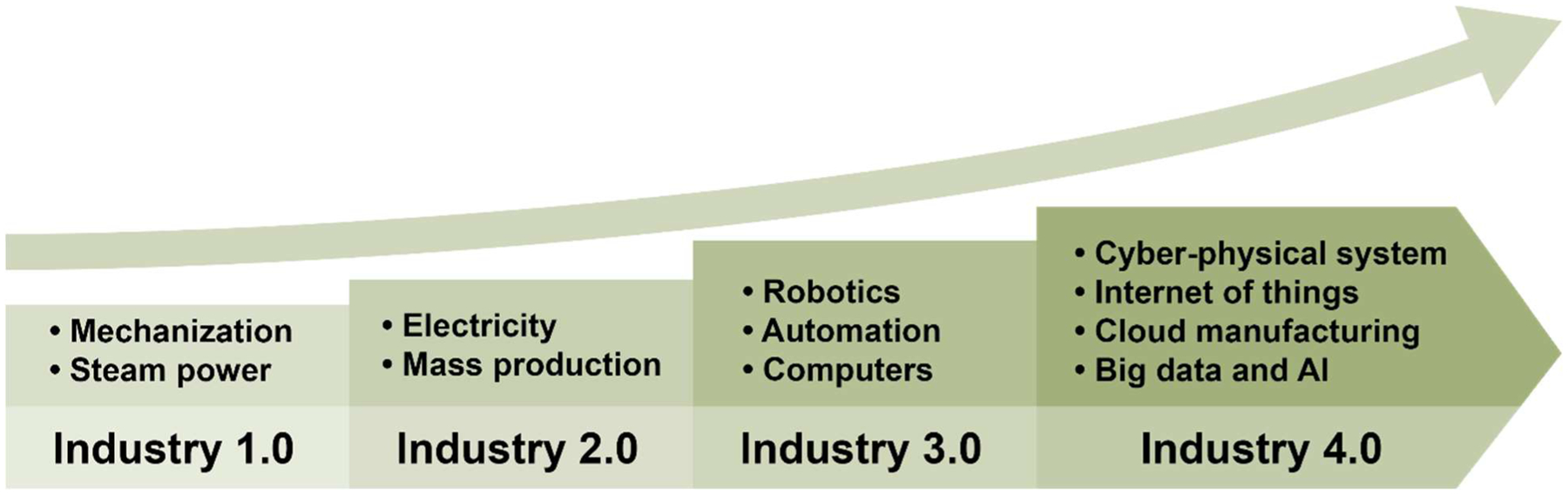
Historical Evolution of Industry 1.0 to Industry 4.0
By looking at the evolution from Industry 1.0 to Industry 4.0 (see Figure 2), we observe initially simple manufacturing devices and technologies, which were then upgraded to more complex and intelligent processes and techniques. We began with a single and small group of machines and equipment and extended to multiple machines, cells and groups, and now to a large-scale manufacturing network. Initially there was only one manufacturing facility; then, we expanded to multiple lines, shops, plants, and finally to enterprise and beyond, to integrate manufacturers with suppliers, service providers, and customers, into a manufacturing community. The data used in manufacturing also grew from a small set, to big data, and to giant data sets with different volumes, varieties, and variations. During this evolution from Industry 1.0 to 4.0, more and more automation components have been included and increasingly less worker/operator involvement has been required.
Figure 2:
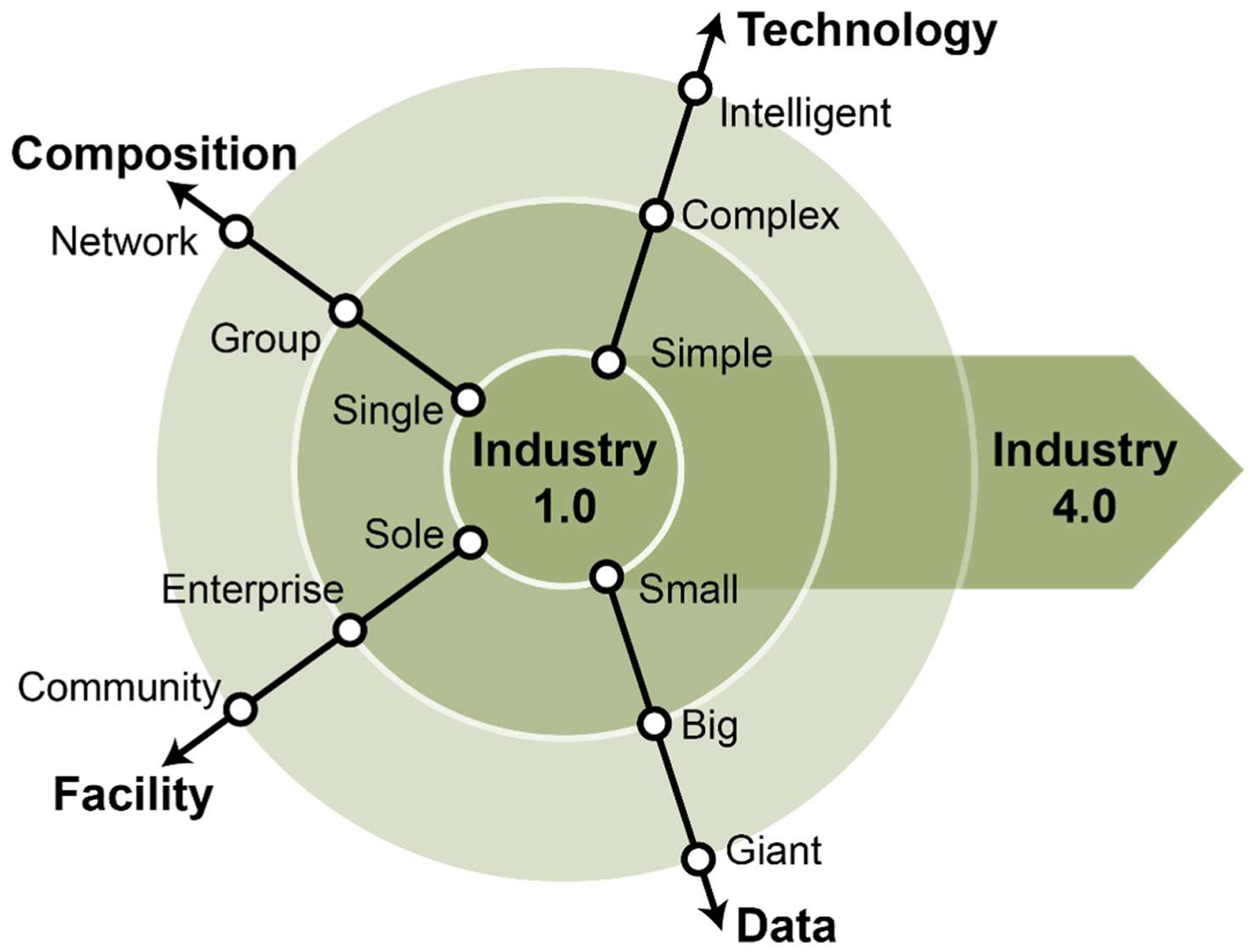
Characteristics of Industry 1.0 to 4.0
3. Transition from Health Care 1.0 to Health Care 4.0
Health care systems share a lot of common features with manufacturing systems (Zhong et al. 2017). Similar to manufacturing or other industry sectors, health care delivery has experienced a long history of evolutions and revolutions. Using our knowledge of the evolution from Industry 1.0 to 4.0 (see above), we describe similar multiple stages to represent the evolution from Health Care 1.0 to Health Care 4.0.
Health Care 1.0 refers to the basic patient-clinician encounter. During such an encounter, a patient visits a clinic and meets with a physician and other members of the care team. Through consultation, testing and diagnosis, the clinician (or care team) provides prescription for medications and a care plan for treating a disease, as well as follow-up plans (e.g. order to get a lab test or an imaging test, referral to a specialist). This model has been prevalent in health care practice for hundreds of years.
Along with major development in health, life science and biotechnology, numerous new medical equipment and devices have been invented, developed and tested, and are increasingly used in health care delivery. For instance, imaging test equipment (e.g. MRI, ultrasound, CT scan), monitoring devices (e.g. pulse oximeter, arterial lines), and surgical and life support equipment (e.g. da Vinci robot, chest tubes) are increasingly used in hospitals and other care settings to support diagnosis, treatment, and monitoring. We refer to this development as Health Care 2.0.
Since last decade, in conjunction with the development of information systems, electronic health or medical records (EHR or EMR) have been implemented to manage care of patients across units and departments of health care organizations; these health information technologies have had major impact on clinical and operational processes. Numerous activities are time-stamped and recorded in the EHR, and many manual processes have been computerized (e.g. order entry in CPOE or computerized provider order entry) and digitalized (e.g. electronic AVS or after visit summary). In addition, using available computer networks, remote care and telehealth have become possible, and electronic visits (e.g. communication between a patient and their physician through a patient portal) are beginning to replace some face-to-face encounters. The current COVID-19 pandemic has increased demand for telehealth and virtual visits. All of these have led to multifarious revolutionary changes in health care delivery. We categorize this revolution as Health Care 3.0.
The fourth health care revolution is now emerging in parallel with Industry 4.0. In such a context, the health care delivery process becomes a cyber-physical system equipped by IoT, RFID (radio-frequency identification), wearables, and all kinds of medical devices, intelligent sensors, medical robots, etc., which are integrated with cloud computing, big data analysis, artificial intelligence, and decision support techniques to achieve smart and interconnected health care delivery. In such a system, not only the health care organizations and facilities (e.g. hospital, clinics, and long-term care facilities) are connected; but also all the equipment and devices, as well as the patients’ home and communities are linked together. Patient-related information, e.g. medication history, diagnostic notes, lab results, treatment plans, pharmacy refills, billing, and insurance claims, can be potentially shared through adequate protocols. In addition, through AI techniques, we can envision proactive treatment, disease prediction and prevention, personalized medicine, and enhanced patient-centered care. Thus, a pervasive, smart, and interconnected health care community emerges, which leads to the paradigm of Health Care 4.0. The transitions from Health Care 1.0 to 4.0 are illustrated in Figure 3.
Figure 3.
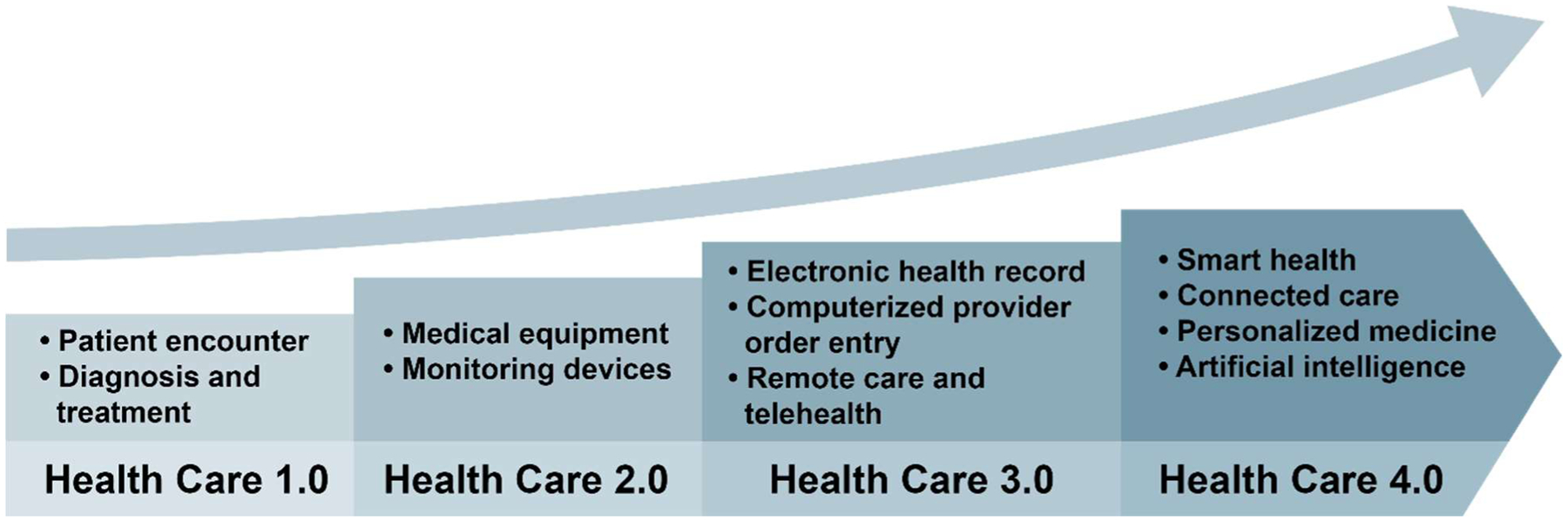
Historical Evolution of Health Care 1.0 to Health Care 4.0
By studying the evolution from Health Care 1.0 to Health Care 4.0 (see Figure 4), we observe that health care delivery has gone from simple medication to more complex and intelligent disease treatment. Patient care was primarily delivered through interactions of a patient with a single clinician, and then expanded by including multiple clinicians, teams, and communities. Initially patient care focused on one facility or discipline, and then expanded to include multiple disciplines, units, and organizations. Now patient care involves large networks and communities of people and organizations. With few data being used at the beginning of the health care transformation, now big and giant data streams with large variations in dimension, quality, format, and characteristic are available in Health Care 4.0. Similar to the evolution of Industry 4.0, Health Care 4.0 includes increasing automation. The most distinctive and critical difference between Industry 4.0 and Health Care 4.0 is about people engagement. In Health Care 4.0, patients (and caregivers) and clinicians are increasingly involved and share responsibilities for monitoring their health, reporting symptoms, and participating in shared decision making for treatment and care planning. As they play more significant roles, patients (and caregivers), as well as clinicians, will be at the center of Health Care 4.0.
Figure 4:
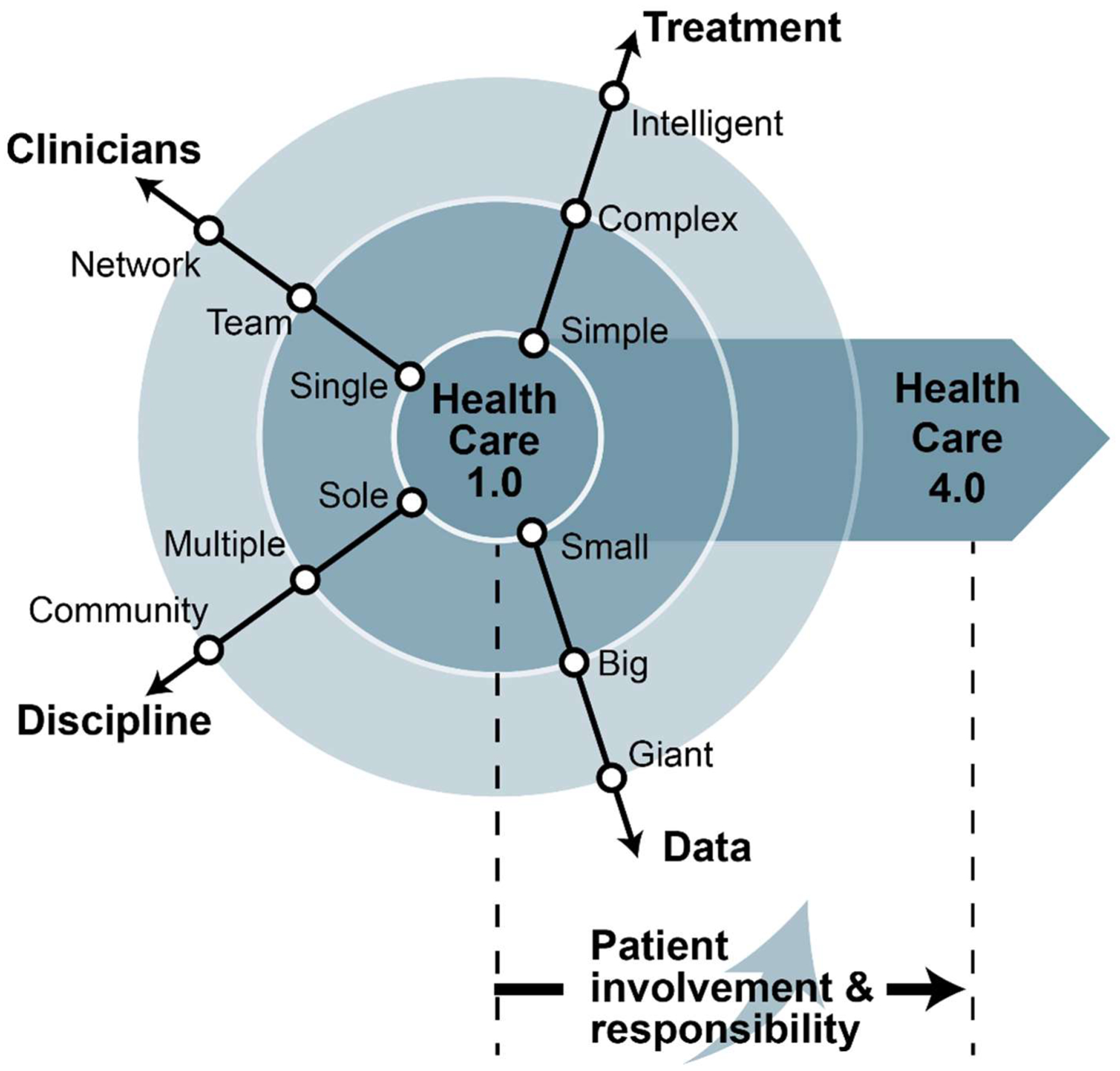
Characteristics of Health Care 1.0 to 4.0
4. Elements of Health Care 4.0
There are two major elements of Health Care 4.0:
- Smartness, i.e., using AI techniques to improve diagnosis, treatment, coordination and communication between patients, clinicians, and other stakeholders, to achieve individualized and patient-centered smart health care management, which includes the following perspectives:
- Stratification and classification. To achieve individualized or personalized care, patient needs and characteristics need to be further understood so that patients can be stratified into different classes (for instance, risk stratification tools for stroke, cancer, and delirium (Stroke Risk in Atrial Fibrillation Working Group 2008, Rodrigues et al. 2012, Newman et al. 2015)). Using stratification and classification tools, important factors correlated to a specific disease can be identified. We can go beyond studying this association, and discover the causal relationship between patient factors and a specific disease, which can help clinicians create patient-specific intervention plans targeting those factors. This can provide the foundation for developing clinical decision support for diagnosis and treatment that can meet specific individual patient needs.
- Prediction analysis. For each patient, accurate predictions of disease development and outcomes based on stratification and classification can be made to help diagnosis and prognosis (for example, prediction of hospital readmission, cardiovascular disease, and COVID-19 infection diagnosis (Kansagara et al. 2011, Damen et al. 2016, Wynants et al. 2020)). Such models should not only provide predicted risk values, but also rank and interpret the factors significantly involved in the prediction. The ranking importance of correlated factors and the potential impact of causal factors can be further investigated to provide recommendations and guidelines for medical decision making.
- Preventive and proactive care. Outputs from prediction analyses can be used to create preventive and proactive care plans (Vlaeyen et al. 2017, Struckmann et al. 2018, Hendry et al. 2019). In addition to preventing or slowing down disease development, we can better address how to prevent medication errors and improve patient safety (Wetterneck et al. 2011, Carayon et al. 2015). Investigation of critical factors affecting patient outcomes and response to treatment can provide recommendations for developing care plans.
- Monitoring, intervention and optimal treatment. To improve patient outcomes, close monitoring of vital signs and other patient-specific critical factors (e.g. Zois et a. 2016, Shah et al. 2016, Correl et al. 2018), and continuous analysis and prediction of patient status are needed to dynamically update care interventions and treatment plans and support optimal medical decision making for each patient. Wireless sensors, wearable devices, as well as edge computing, and patient portals, provide the possibility for self or remote monitoring. Advanced data analysis and optimization models can help develop suitable, individualized intervention and treatment plans.
-
Closed loop. All the elements in Health Care 4.0 are dynamically connected in a closed loop. In other words, the results of medication and treatment decisions need to feed back to the prediction analysis model to dynamically update the predictions and important factors, as well as the care and intervention plan in a timely manner.Natural language processing, deep learning and statistical inference, virtual reality and augmented reality, modeling and optimization techniques play key roles to create a smart health care system. Like in Industry 4.0, IoT, RFID, wearable devices, robotics, and block chain technologies in cyber-physical systems create a mechanism for data collection, monitoring, analysis, intervention, and feedback. Linking these to personalized medicine can help to implement genetic-based diagnosis and treatment approaches and improve the effectiveness of patient therapy.An illustrative example of smart health care is shown in Figure 5, where personalized medicine is targeted to different patient groups, and the results are then fed back to reevaluate and design the smart care iteratively.
- Interconnection, i.e., integrating all aspects of health care to construct an effective information network by connecting the following system elements:
- Interactions between patients, caregivers, and other care team members. Communication between patients and care teams is critical for health care quality and patient safety (Rodin et al. 2009, Thompson et al. 2012, Kelly et al. 2014). Not only the diagnosis results, treatment plans, and clinical outcomes should be communicated to patients, but also engagement of patients and their caregivers in the care and treatment process should become the norm. Thus, patients will better understand what is needed to implement their care plan and be more actively involved in the care process. Such engagement is even more critical when patients have chronic and complex diseases. The judicious development, implementation and use of information technology, patient portals, phone calls, video conferences, and Apps, etc., can help facilitate patient (and caregiver) communication and engagement, particularly during a pandemic or in a remote environment.
- Communications within the professional care team. All health professionals involved in patient care should communicate and coordinate efficiently and effectively (Hewett et al. 2009, Wu et al. 2012, Nguyen et al. 2015). Fragmented care delays delivery of care and leads to substantial waste and patient harm. Advanced information technology and new equipment or devices have the potential to facilitate team communication and care coordination. In particular, a coordinated patient hub can help achieve effective and efficient coordination by supporting information sharing and communication among all team members. This would go a long way to support shared mental model and awareness among the care team, which is critical for quality and safety of patient care (Schultz et al., 2007).
- Equipment and devices. The widespread use of complex and intelligent equipment and numerous wearable devices, sensors, IoT, and different kinds of connecting functions (e.g. Scanaill et al. 2006, Patel et al. 2012, Vegesna et al. 2017) can help to continuously and comprehensive collect information about patient care regardless of the location of care. Cloud and edge computing functions enable these devices to provide additional analysis, diagnosis, and prediction capabilities locally and globally.
- Organizations and community. All health care organizations and community stakeholders, including individual practitioners, small group practices, clinics, hospitals, pharmacies, community health centers, long-term care facilities, individual, regional and public health systems, as well as the broad community will be connected. Care quality improvement requires significant collaboration between all of these health care organizations and the larger community. Information available at each entity needs to be accessible by other entities through appropriate protocols and processes.
- Insurance, billing and costs. Using cutting-edge information technology and management tools, reimbursement practices, regulatory frameworks and desired outcomes can be better aligned to remove barriers and reduce cost. Connections through insurance selection and coverage, streamlining coding, billing, and reimbursement, with health IT advancement in billing systems are important.
- Care transitions across time and space. Care transitions exist across the patient’s lifetime, such as pediatric, adult and senior care, or across space, such as out-patient, in-patient, home or long-term care. Each care phase or location has its unique characteristics as well as universal features. In addition to addressing the specific issues within each phase or location, we need to pay close attention to the transitions between the care phases and locations (Naylor and Keating 2008, Peter et al. 2009, Gabriel et al. 2017). Particularly problems related to information transfer and consistency, patient safety, chronic disease management and continuity of care, are of significant importance and need to be addressed in Health Care 4.0.
- Closed loops. Again, all the connected entities are dynamically linked in multiple closed loops entangled together. Information at the population-, group- and individual-levels can be integrated with all of the other system elements and effectively aligned in the patient journey.
Figure 5.
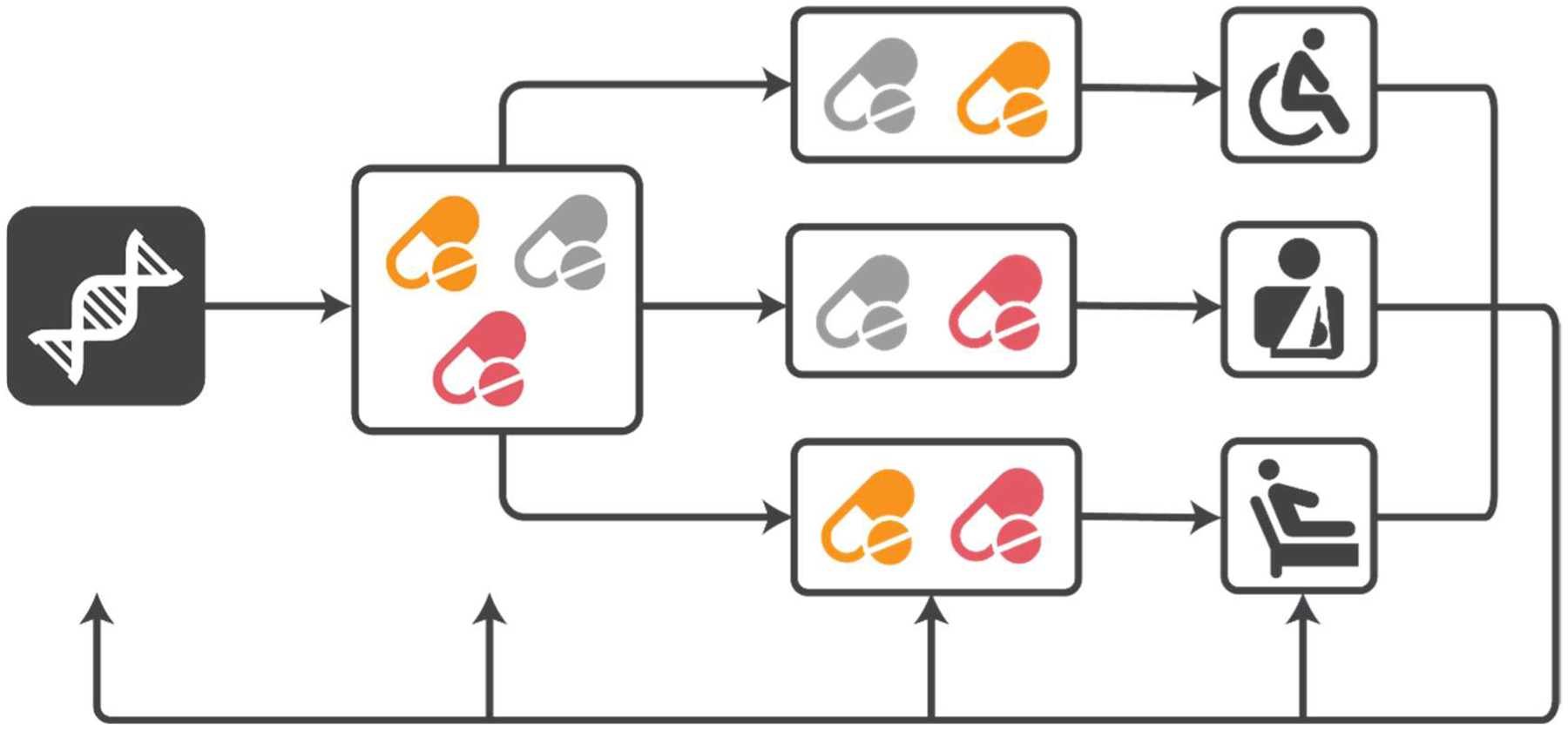
Smart and Personalized Health Care
We not only need information connection in each aspect, but also integration of information along all phases of the patient journey. Secure and authorized information sharing among stakeholders can lead to substantial improvement in health care delivery. The information flow between stakeholders occurs across the patient journey, i.e. the “spatio-temporal distribution of patients’ interactions with multiple care settings over time” (Carayon and Wooldridge 2020). During their journey, a patient may visit multiple health care organizations, including primary care clinic, specialists, hospital, emergency room, rehabilitation facility, and long-term care (Carayon et al. 2020). Health Care 4.0 aims to develop technologies that support information flow and coordination among the various stakeholders involved in the patient journey. Figure 6 provides an illustrative example of such connected care, where the patients are the center of the whole network.
Figure 6.

Connected Health Care
In summary, smart and interconnected health care systems represent the new paradigm of future health care delivery in Health Care 4.0. Making Health Care 4.0 a reality requires multiple research fields and disciplines, such as cyber-physical systems, information technology, artificial intelligence, robotics, computing, security, modeling and optimization, in addition to health sciences (e.g. medicine, nursing, pharmacy), health informatics, bioinformatics, and human factors and systems engineering. Moreover, the interactions between people (patients, caregivers, clinicians) and machines (devices, technology) in a complex sociotechnical system are extremely important to consider. Patients should be the central feature of the smart and interconnected health care system and supported by all other system elements, interactions and activities.
5. Challenges and Implications for Technology and Research
What challenges do we need to address to achieve the Health Care 4.0 vision of smart and connected health care? From the technology development perspective, numerous challenges exist:
-
Data
The smartness of the system depends on data. In addition to the well-known challenges in data availability and privacy issues, data compatibility becomes critical as health care entities use different databases with various formats: how to unify them to make them compatible and communicate is not easy. In health care systems, although a huge amount of data has been collected, the fundamental nature of diseases and humans is still unknown; therefore, it is unclear what will be the most critical data or component in each system. This will certainly affect data collection and subsequent analyses. Furthermore, current AI and machine learning technologies rely on large volume dataset and clear marking or deterministic rules. But many health care problems have unique or specific features related to a disease, a person, or an environment, which means small datasets. The rules or mechanisms (or the “physics”) controlling the process or human behavior are not known. Moreover, health disparities, inequities and human behavior may affect the availability and use of advanced technology, which could lead to unbalanced data across groups. Challenges remain on how to use such small and incomplete datasets with limited domain knowledge to make accurate and meaningful predictions and subsequent analyses.
-
Model
To formulate models for each health care problem, process or system, various levels of details and complexities should be considered. Insufficient details may lead to low confidence in the models and could also result in inadequate outcomes. In addition, higher-level process models are dependent on detailed configurations of lower-level models, and coupled to other process or system models. For instance, a change in the number of medical assistants or rooming time in a primary care clinic pod model will result in variations in service time in the patient flow model, which can lead to updates in appointment schedule and changes in clinician workflow model, and further impact the clinic’s accessibility to the patient panel. On the other hand, models with too much detail may not be feasible in practice due to computation and implementation issues. In addition, data imbalance caused by disparities, inequalities, and behaviors may result in insufficient inputs to the models. Research on smart and connected care is needed to systematically and effectively deal with the tradeoff between process complexity and methodological feasibility, which is extremely challenging.
-
Dynamics
Many of the available models and methods deal with static or long-term behaviors. However, the time dynamics are critical in health care systems, in particular for patient safety, such as transient behaviors in patient rescue, infection prevention, and surgical processes (Vincent & Amalberti 2016). In addition, many current analyses focus on issues with high probabilities. But health care events with very small probabilities may have substantial impact. How to support real-time decision making to address the dynamic behavior with small probabilities while still achieving good outcomes for long-term general performance is challenging.
-
Integration
The successful system connectivity relies on integration of data, model, and methodologies. Each connected element has its own model, with their own focus, objectives, and priorities, which can be different, and sometimes, even conflicting. The models and methodologies can be quantitative (e.g. stochastic analysis and optimization, Brandeau et al. 2004, Denton 2013, Hall 2013, Li et al. 2017), qualitative (e.g. human factors approach, Holden et al. 2013, Carayon 2016, Carayon et al. 2020a, b), empirical (e.g. Worthington 2004, Irving et al. 2009), and experimental (such as medical simulations, e.g., Gaba 2004, McGaghie et al. 2010). How to integrate them with appropriate datasets, and how to take advantage of their complementarity (i.e. using their respective strengths while mitigating their weaknesses) to achieve convergence towards patient care goals while still satisfying each objective, certainly is challenging. In this integration, it is critical to address underlying issues of health disparities and inequities. We need to put the issue of health equity at the center of our technological development and research effort. This should, for instance, involve focused effort on vulnerable patient populations such as those with socioeconomic disadvantages and limited access to technologies. Figure 7 presents an example of such integration, where different approaches, methods, data, and outcomes are integrated to form a closed loop study.
Figure 7:
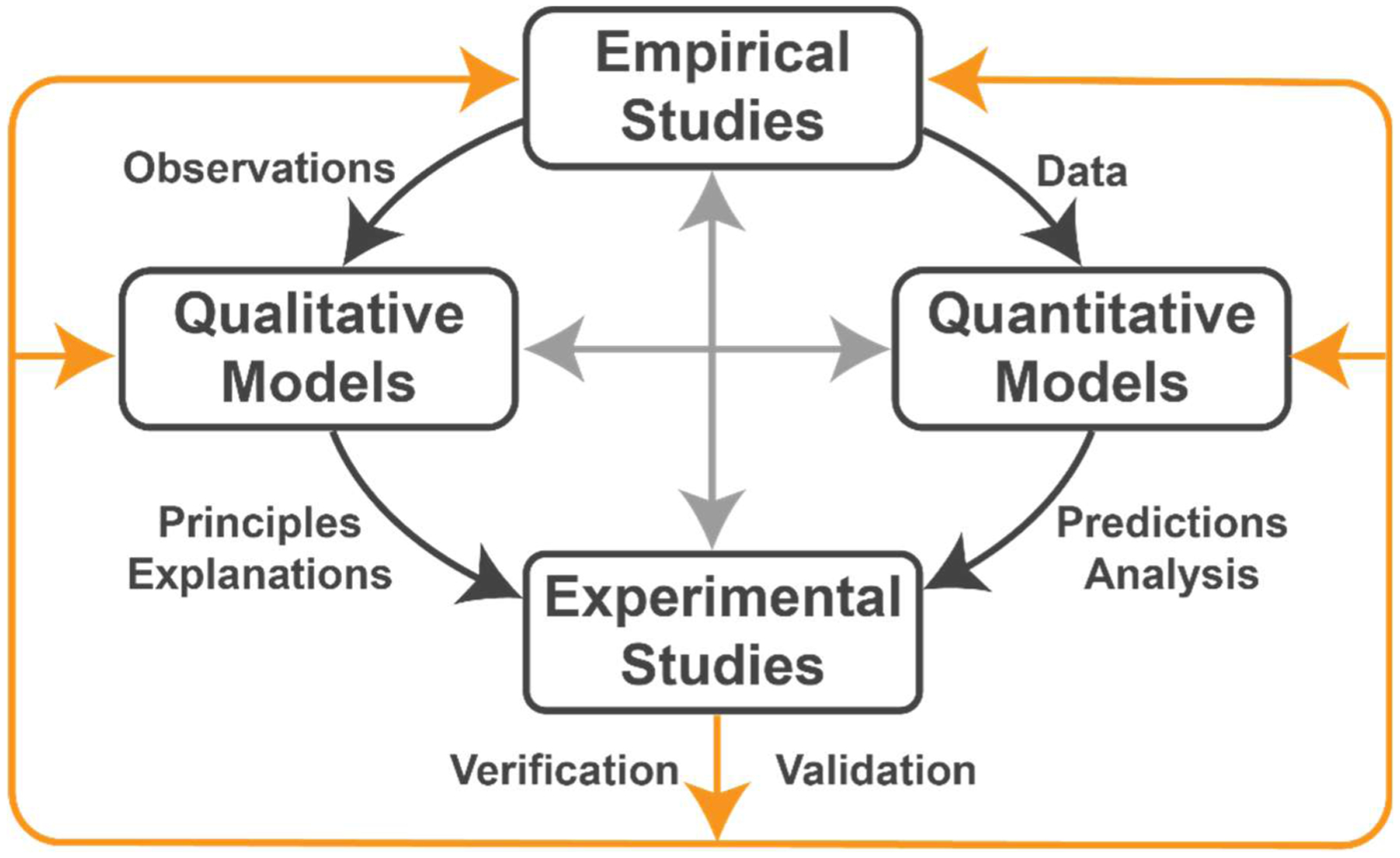
Example of an Integration Study
The integration illustrated in Figure 7 can benefit from an overall conceptual framework, such as the SEIPS (Systems Engineering Initiative for Patient Safety) model (Carayon et al., 2006, 2014). According to the SEIPS model, patient outcomes such as patient safety or health care quality depend on the “appropriate” design of various elements of the work system, and their integration in care processes. We need to further understand how to quantify and qualify the work system elements and their interactions; this will require access to representative, high-quality data that are used to develop analytical and predictive models (see above). In the integration study example of Figure 7, the SEIPS model could be used to ensure that empirical studies provide data on all work system elements, whether they are observational, objective, subjective, quantitative or qualitative. These inputs are then used to develop qualitative models (e.g. cognitive model for a technology interface) and quantitative models (e.g. stochastic model of process performance). Qualitative and quantitative models can then be mixed and integrated. This may, for instance, occur in the development of a technology or process mock-up that can be tested experimentally before its implementation in a care setting. The SEIPS model puts people at the center, including patients, caregivers and clinicians. Given the key role of people in Health Care 4.0 (see above), this emphasis on people is critical and can help to achieve optimal outcomes for both patients and clinicians (see below discussion of the Quadruple Aim).
From the research perspective, the following implications are of significant importance:
-
Need to focus on people: e.g. patients, caregivers and health care professionals
When comparing the evolution between Industry 1.0 to 4.0 and Health Care 1.0 to 4.0, we observe that in both domains, new technologies, equipment and data are being developed and utilized. In Industry 4.0, the participation of people becomes less significant along with increasing automation. However, in Health Care 4.0, with more automation and use of technology, the participation and importance of people actually become more critical. Not only patients, clinicians, and supporting and relevant staff are included in the system, but also their responsibilities are increasing. For instance, patients will have an increasingly proactive role to monitor and adjust their health through feedback provided by wearable devices and online information. The work by health care organizations is not limited to office or regular hours, and needs to integrate continuous analysis and regular response to patients’ requests. From the health technology professional’s perspective, individualized characteristics and needs (from both patients and clinicians) should be considered in their products’ design and service. The way we design systems and processes for Health Care 4.0 will have critical impact on the behavior of patients, caregivers and health care workers.
-
Need to focus on system and process: team, team of teams, caregiving network, process spread across organizational boundaries, involvement of community.
Health care delivery is about “team” work. Even a standard clinic visit involves many different team members: patients, sometimes caregivers, and multiple clinicians and health care workers, e.g. physicians, nurses, medical assistants, pharmacist, lab technicians, etc. Multiple processes can be involved as well, such as patient visit process, caregiver work process, information management process, document and billing process, etc. Such teams and processes expand rapidly when the system becomes larger; therefore including outreach to other organizations, the community, various social networks, and expanding the physical boundaries of the system. Not only the health community, but also other parts of society and various industries (such as manufacturing, service, transportation, finance) will be involved in Health Care 4.0. For example, the COVID-19 pandemic has affected everyone and all the businesses, industries, and communities.
-
Need to ensure that we focus on key health care outcomes: Quadruple Aim (4)
The Quadruple Aim is about designing and optimizing health care system performance through (1) revolutionizing patient experience, (2) improving population health, (3) controlling health care costs, and (4) enhancing clinician satisfaction. The four aims are interconnected and serve as a compass to point the direction for a smart and connected health care system. Health Care 4.0 needs to focus on these key outcomes to balance the positive and negative dependence of the aims and integrate them systematically.
6. Conclusions and Recommendations
Health Care 4.0 provides numerous opportunities and challenges to health care systems engineering. To take advantage of the opportunities and address the challenges to achieve smart and connected health care, we propose the following recommendations:
First, many stakeholders need to get involved, including all fields from engineering, health sciences and education, health care delivery improvement, and health and health care technologies. The multiple expertise domains address different perspectives of the health care systems; their different views and objectives need to converge to achieve a universal vision and the Quadruple Aim. This requires a significant effort of mutual engagement, communication, coordination, and compromise among disciplines and perspectives.
Second, many technologies and methodologies need to get involved. In addition to using quantitative methods, such as modeling, simulation, computation and optimization techniques, qualitative approaches, including survey, human-centered design, evaluation, and field observations, should also be utilized. Preference should be given to combination of quantitative and qualitative methods and the mixing of various methods and data. Moreover, empirical studies and experimental projects, such as medical simulation, virtual reality, and pilot studies, are an essential complement to modeling; especially before, during and after implementation of new practices. This will allow for continuous learning and improvement of care processes and outcomes.
Third, both hardware (medical equipment, devices, and tools) and software (modeling, computation, evaluation, etc.) should be connected in the loop. In the proposed sociotechnical approach, human-machine or human-technology interactions become critical to ensure effective connections and safe implementation of smart technologies.
Finally, humans, including patients, caregivers and health care workers, should be at the center of smart and connected health care, in both research and practice. It is important to consider their characteristics, needs, abilities and constraints when designing and implementing smart and interconnected health care. It is critical to address the issue of disparities and inequities and ensure that Health Care 4.0 is designed to mitigate and reduce such inequities and allow all individuals access to high-quality, safe care. Moreover, the potential negative impact of technologies on sociotechnical systems, like the digital divide, should be addressed, which might need efforts from the public health sector and increased recognition of the role of social determinants of health.
Acknowledgments
Professors Li and Carayon are funded in part by the Agency for Healthcare Research and Quality (R18HS026624), the National Science Foundation (1840358-EEC), and the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS) (UL1TR002373).
They are grateful to the anonymous reviewers for their valuable comments and to the graphic designers at the Grainger Institute of Engineering of the University of Wisconsin-Madison for their contribution to the figures.
References
- Brandeau ML, Sainfort F, Pierskalla WP, editors. Operations research and health care: a handbook of methods and applications. Springer Science & Business Media; 2004. [Google Scholar]
- Carayon P, editor. Handbook of human factors and ergonomics in health care and patient safety. CRC Press; 2016. [Google Scholar]
- Carayon PA, Hundt AS, Karsh BT, Gurses AP, Alvarado CJ, Smith M, Brennan PF. Work system design for patient safety: the SEIPS model. BMJ Quality & Safety. 2006;15(suppl 1):i50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Ju F, Cartmill R, Hoonakker P, Wetterneck TB, Li J. Medication error propagation in intensive care units. In Proceedings of the Human Factors and Ergonomics Society Annual Meeting 2015. (Vol. 59, No. 1, pp. 518–521). Sage CA: Los Angeles, CA: SAGE Publications. [Google Scholar]
- Carayon P, Wooldridge A. Improving patient safety in the patient journey: Contributions from human factors engineering. In: Smith AE, editor. Women in Industrial and Systems Engineering: Key Advances and Perspectives on Emerging Topics. Cham, Switzerland: Springer Nature; 2020. p. 275–99. [Google Scholar]
- Carayon P, Wooldridge A, Hoonakker P, Hundt AS, Kelly MM. SEIPS 3.0: Human-centered design of the patient journey for patient safety. Applied Ergonomics. 2020;84:103033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, Hundt AS, Hoonakker P, Holden R, Gurses AP. Human factors systems approach to healthcare quality and patient safety. Applied ergonomics. 2014;45(1):14–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Wooldridge A, Hoonakker P, Hundt AS and Kelly M SEIPS 3.0: Human-centered design of the patient journey. Applied Ergonomics. 2020; 84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassel CK, Saunders RS. Engineering a better health care system: a report from the President’s Council of Advisors on Science and Technology. The Journal of the American Medical Association. 2014;312(8):787–8. [DOI] [PubMed] [Google Scholar]
- Correll CU, Galling B, Pawar A, Krivko A, Bonetto C, Ruggeri M, Craig TJ, Nordentoft M, Srihari VH, Guloksuz S, Hui CL. Comparison of early intervention services vs treatment as usual for early-phase psychosis: a systematic review, meta-analysis, and meta-regression. JAMA psychiatry. 2018;75(6):555–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damen JA, Hooft L, Schuit E, Debray TP, Collins GS, Tzoulaki I, Lassale CM, Siontis GC, Chiocchia V, Roberts C, Schlüssel MM. Prediction models for cardiovascular disease risk in the general population: systematic review. bmj. 2016;353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denton BT. Handbook of healthcare operations management. New York: Springer. 2013;10(978–1):9. [Google Scholar]
- Gaba DM. The future vision of simulation in health care. BMJ Quality & Safety. 2004;13(suppl 1):i2–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabriel P, McManus M, Rogers K, White P. Outcome evidence for structured pediatric to adult health care transition interventions: a systematic review. The Journal of pediatrics. 2017;188:263–9. [DOI] [PubMed] [Google Scholar]
- Hall R Patient flow. AMC. 2013;10:12. [Google Scholar]
- Hendry A, Vanhecke E, Carriazo AM, López-Samaniego L, Espinosa JM, Sezgin D, O’Donovan M, Hammar T, Ferry P, Vella A, Bacaicoa OA. Integrated care models for managing and preventing frailty: a systematic review for the European Joint Action on Frailty Prevention (ADVANTAGE JA). Translational Medicine@ UniSa. 2019;19:5. [PMC free article] [PubMed] [Google Scholar]
- Hewett DG, Watson BM, Gallois C, Ward M, Leggett BA. Intergroup communication between hospital doctors: implications for quality of patient care. Social science & medicine. 2009;69(12):1732–40. [DOI] [PubMed] [Google Scholar]
- Holden RJ, Carayon P, Gurses AP, Hoonakker P, Hundt AS, Ozok AA, Rivera-Rodriguez AJ. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics. 2013;56(11):1669–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irving JA, Dobkin PL, Park J. Cultivating mindfulness in health care professionals: A review of empirical studies of mindfulness-based stress reduction (MBSR). Complementary therapies in clinical practice. 2009;15(2):61–6. [DOI] [PubMed] [Google Scholar]
- Kansagara D, Englander H, Salanitro A, Kagen D, Theobald C, Freeman M, Kripalani S. Risk prediction models for hospital readmission: a systematic review. Jama. 2011;306(15):1688–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan GS, Bo-Linn G, Carayon P, Pronovost P, Rouse W, Reid P, et al. Bringing a systems approach to health. Washington, DC: Institute of Medicine and National Academy of Engineering; 2013. [Google Scholar]
- Kelley JM, Kraft-Todd G, Schapira L, Kossowsky J, Riess H. The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PloS one. 2014. Apr 9;9(4):e94207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasi H, Fettke P, Kemper HG, Feld T, Hoffmann M. Industry 4.0. Business & Information Systems Engineering. 2014;6(4):239–42. [Google Scholar]
- Li J, Kong N, Xie X. Stochastic Modeling and Analytics in Healthcare Delivery Systems. World Scientific Publishing. 2017. [Google Scholar]
- Liao Y, Deschamps F, Loures ED, Ramos LF. Past, present and future of Industry 4.0-a systematic literature review and research agenda proposal. International Journal of Production Research. 2017;55(12):3609–29. [Google Scholar]
- McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ. A critical review of simulation-based medical education research: 2003–2009. Medical education. 2010;44(1):50–63. [DOI] [PubMed] [Google Scholar]
- Newman MW, O’Dwyer LC, Rosenthal L. Predicting delirium: a review of risk-stratification models. General hospital psychiatry. 2015;37(5):408–13. [DOI] [PubMed] [Google Scholar]
- Nguyen C, McElroy LM, Abecassis MM, Holl JL, Ladner DP. The use of technology for urgent clinician to clinician communications: a systematic review of the literature. International journal of medical informatics. 2015;84(2):101–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel S, Park H, Bonato P, Chan L, Rodgers M. A review of wearable sensors and systems with application in rehabilitation. Journal of neuroengineering and rehabilitation. 2012;9(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peter NG, Forke CM, Ginsburg KR, Schwarz DF. Transition from pediatric to adult care: internists’ perspectives. Pediatrics. 2009;123(2):417–23. [DOI] [PubMed] [Google Scholar]
- Reid PR, Compton WD, Grossman JH, Fanjiang G. Building a Better Delivery System. A New Engineering/Health Care Partnership. Washington, D.C.: The National Academies Press; 2005 [PubMed] [Google Scholar]
- Rodin G, Mackay JA, Zimmermann C, Mayer C, Howell D, Katz M, Sussman J, Brouwers M. Clinician-patient communication: a systematic review. Supportive Care in Cancer. 2009;17(6):627–44 [DOI] [PubMed] [Google Scholar]
- Rodrigues G, Warde P, Pickles T, Crook J, Brundage M, Souhami L, Lukka H. Pre-treatment risk stratification of prostate cancer patients: A critical review. Canadian Urological Association Journal. 2012;6(2):121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubmann M, Lorenz M, Gerbert P, Waldner M, Justus J, Engel P, Harnisch M. Industry 4.0: The future of productivity and growth in manufacturing industries. Boston Consulting Group. 2015;9(1):54–89. [Google Scholar]
- Scanaill CN, Carew S, Barralon P, Noury N, Lyons D, Lyons GM. A review of approaches to mobility telemonitoring of the elderly in their living environment. Annals of biomedical engineering. 2006;34(4):547–63. [DOI] [PubMed] [Google Scholar]
- Schultz K, Carayon P, Hundt AS and Springman SR Care transitions in the outpatient surgery preoperative process: Facilitators and obstacles to information flow and their consequences. Cognition, Technology and Work. 2007, 9(4): 219–231. [Google Scholar]
- Shah C, Arthur DW, Wazer D, Khan A, Ridner S, Vicini F. The impact of early detection and intervention of breast cancer-related lymphedema: a systematic review. Cancer medicine. 2016;5(6):1154–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikka R, Morath JM, Leape L. The Quadruple Aim: Care, health, cost and meaning in work. BMJ Quality & Safety. 2015;24(10):608–10. [DOI] [PubMed] [Google Scholar]
- Stroke Risk in Atrial Fibrillation Working Group. Comparison of 12 risk stratification schemes to predict stroke in patients with nonvalvular atrial fibrillation. Stroke. 2008;39(6):1901–10. [DOI] [PubMed] [Google Scholar]
- Struckmann V, Leijten FR, van Ginneken E, Kraus M, Reiss M, Spranger A, Boland MR, Czypionka T, Busse R, Rutten-van Mölken M. Relevant models and elements of integrated care for multi-morbidity: Results of a scoping review. Health Policy. 2018;122(1):23–35. [DOI] [PubMed] [Google Scholar]
- Thompson L, McCabe R. The effect of clinician-patient alliance and communication on treatment adherence in mental health care: a systematic review. BMC psychiatry. 2012. Dec 1;12(1):87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vegesna A, Tran M, Angelaccio M, Arcona S. Remote patient monitoring via non-invasive digital technologies: a systematic review. Telemedicine and e-Health. 2017;23(1):3–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent C and Amalberti R Safer Healthcare - Strategies for the Real World. 2016; Springer Open. [PubMed] [Google Scholar]
- Vlaeyen E, Stas J, Leysens G, Van der Elst E, Janssens E, Dejaeger E, Dobbels F, Milisen K. Implementation of fall prevention in residential care facilities: A systematic review of barriers and facilitators. International journal of nursing studies. 2017;70:110–21. [DOI] [PubMed] [Google Scholar]
- Wetterneck TB, Walker JM, Blosky MA, Cartmill RS, Hoonakker P, Johnson MA, Norfolk E, Carayon P. Factors contributing to an increase in duplicate medication order errors after CPOE implementation. Journal of the American Medical Informatics Association. 2011;18(6):774–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worthington AC. Frontier efficiency measurement in health care: a review of empirical techniques and selected applications. Medical care research and review. 2004;61(2):135–70. [DOI] [PubMed] [Google Scholar]
- Wu RC, Tran K, Lo V, O’Leary KJ, Morra D, Quan SD, Perrier L. Effects of clinical communication interventions in hospitals: a systematic review of information and communication technology adoptions for improved communication between clinicians. International journal of medical informatics. 2012;81(11):723–32. [DOI] [PubMed] [Google Scholar]
- Wynants L, Van Calster B, Bonten MM, Collins GS, Debray TP, De Vos M, Haller MC, Heinze G, Moons KG, Riley RD, Schuit E. Prediction models for diagnosis and prognosis of covid-19 infection: systematic review and critical appraisal. bmj. 2020;369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong X, Lee HK, Li J. From production systems to health care delivery systems: a retrospective look on similarities, difficulties and opportunities. International Journal of Production Research. 2017;55(14):4212–27. [Google Scholar]
- Zois DS. Sequential decision-making in healthcare IoT: Real-time health monitoring, treatments and interventions. In2016 IEEE 3rd World Forum on Internet of Things (WF-IoT) 2016. (pp. 24–29). IEEE [Google Scholar]


