Abstract
Background:
Lipofilling is currently a fundamental component of rhytidoplasty and fat harvesting has become a common procedure. Tonnard introduced the concept of nanofat grafting, a revolutionary milestone, in which adipocytes are mechanically separated from the stromal vascular fraction and the latter is injected, adding the possibility of cellular therapies to the surgical field. Later, Verpaele et al. published a report using a new device to apply this nanofat in a uniform manner, which they termed nanofat needling. The device has 24 microneedles of 1.5 mm length and is applied as a stamp, in a tapping motion. The same manufacturer offers a similar model with 64 microneedles, 1.0 mm length, and available as a roller.
Objectives:
We sought to evaluate the combination of the above-mentioned microneedling devices to achieve faster nanofat delivery.
Materials and Methods:
A prospective evaluation of patients undergoing a combined nanofat microneedling approach for skin rejuvenation and scar revision, using both a stamp device as well as a roller, was performed in a private practice setting, from January 2019 to January 2020. Patient satisfaction, complications, and surgical time were evaluated.
Results:
We applied this combination treatment to over 100 treatment areas in 86 patients over a 12-month period, with a short operative time, no increase in complications, consistent results, and good patient satisfaction.
Conclusions:
We recommend the use of this new device in association with the original one, in order to decrease the procedure time. We designate this strategy “fast nanofat microneedling.”
Keywords: Collagen induction, facial rejuvenation, fat grafting, microneedling, nanofat
BACKGROUND
Lipofilling is currently a fundamental component of rhytidoplasty and fat harvesting has become a common procedure. Tonnard et al.[1] introduced the concept of nanofat grafting, a revolutionary milestone, in which adipocytes are mechanically separated from the stromal vascular fraction and the latter is injected, adding the possibility of cellular therapies to the surgical field. Later, Verpaele et al.[2] published a report using a new device to apply this nanofat in a uniform manner, which they termed nanofat needling. The device has 24 microneedles of 1.5 mm length and is applied as a stamp, in a taping motion. The same manufacturer offers a similar model with 64 microneedles, 1.0 mm length, available as a roller; therefore, speed of injection is higher and allows a multidirectional distribution, which has been found to be a fundamental factor for adequate percutaneous collagen induction via microneedling.
MATERIALS AND METHODS
This was a prospective assessment of the senior author: Ronaldo Righesso (RR) private practice patients submitted to microneedling plus nanofat either for skin rejuvenation or scar revision, either as a standalone procedure or in combination with other operations. Patients treated between January 2019 and January 2020 were included. All patients gave written informed consent for surgery and publication. STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines were followed for manuscript preparation. The study was performed in accordance with the Declaration of Helsinki for Research in Human Subjects and subsequent amendments.
To prepare the nanofat, the same mechanical protocol as suggested by Tonnard et al.[3] was adopted. The fat is harvested from the lower abdomen after infiltration with a modified Klein solution with a multiport 3-mm cannula with sharp side holes 1 mm in diameter. The fat is rinsed and filtered through a sterile nylon cloth with 0.5 mm pore size mounted over a sterile canister. Next, the fat undergoes a two-step emulsification process. The first step is performed by shuffling of the microfat from a full 10mL syringe to an empty one through a 2.4 mm female-to-female Luer-Lok connector. After 30 passes, the same process is repeated with a 1.2-mm female-to-female Luer-Lok connector for another 30 passes. At the end of this emulsification process, a whitish discoloration of the fat is seen. The fat is now passed through a 600-µm filter. Once the process is concluded, the resultant nanofat fills the micro bottle attached to the device [Figure 1]. If necessary, local infiltration of the target area is done with Lidocaine 1%. After allowing for adequate anesthesia, nanofat needling is done.
Figure 1.
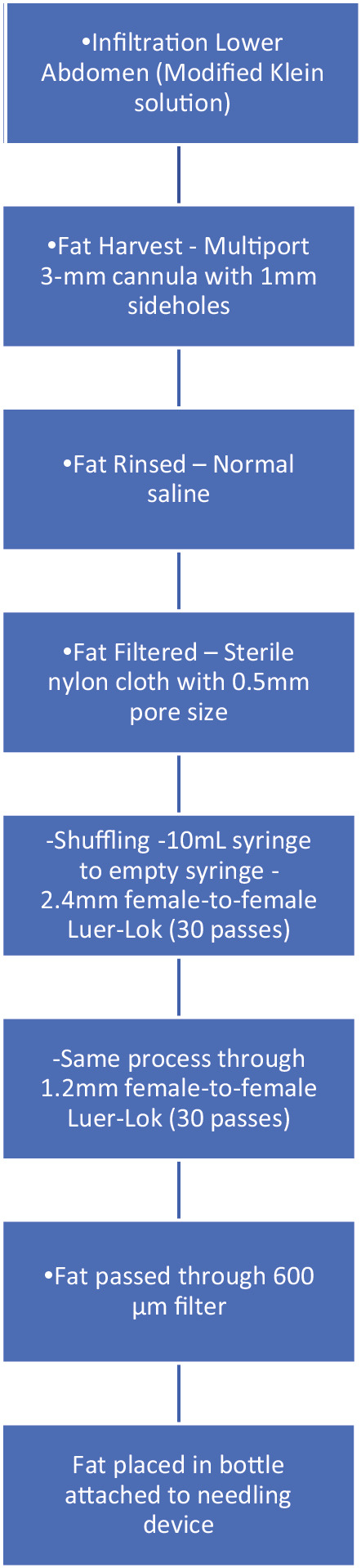
Flow chart—nanofat preparation
Verpaele et al.[2] reported the use of a microneedle device called HydraNeedle 20® (Guangzhou Ekai Eletronic Technology Co Ltd, Guangzhou, China). It contains 20 gold titanium needles, each 0.13 mm in diameter and 1.5 mm in length. It works by repetitive tapping motions to create the microchannels. The same manufacturer offers a similar device, called HydraRoller®, with 64 microneedles, 1 mm length each. This device has a different application: working as a roller, turning the needles, and delivering the content.
Our first contact with this technique was during an ISAPS (International Society of Aesthetic Plastic Surgery) meeting in September 2018, in Porto Alegre, where Dr. Tonnard presented his use of the HydraNeedle device. We incorporated the device immediately, performing our first cases in October 2018, prior to Dr. Tonnard’s April 2019 publication in Plastic and Reconstructive Surgery. After initial experience with 10 patients, we sought alternatives to expedite the procedure without losing efficiency. We found the Hydra Roller, which has more needles, but of a shorter length, of up to 1 mm, on the manufacturer’s website. We began by using this on 10 patients, on the décolletage; one side was treated with the Hydra Roller and one side with the Hydra Needle. At 2 months post-procedure, we did not see a clinically apparent difference between either device, although it was our perception that the roller allowed for a more homogeneous application. In January 2019, we decided to pair the devices, using Hydra Needle after the application of Hydra Roller, since there is no 1.5 mm needle length version of the latter; therefore, more superficial application would not be detrimental. We recommend the use of both devices, starting with the roller, delivering about 90% of the estimated nanofat, followed by delivery of the remaining 10% with the stamp. The roller is used, with passes made at a 90-degree angle, first vertically and then horizontally, and posteriorly using the stamp device. The endpoint is punctate bleeding.
Once needling is concluded, the nanofat is left on the skin surface for 10 min to allow penetration through the microchannels, after which the treated area is cleaned using normal saline, followed by application of nanofat cream (9mL of nanofat, 1mL of methylcellulose powder, and 10mL of 0.9% normal saline. Patients are advised to use the nanofat cream 5 to 6 times a day, for 3 days.[2] The nanofat cream should be kept in the refrigerator, between 8 and 16°C, during this period.[3]
Patients classified their aesthetic results after at least 4 months post-procedure, on a scale of 1 to 4, with the following scores: 1, very good; 2, good; 3, slight improvement; 4, no difference.
RESULTS
This strategy saves a considerable amount of time, delivering 8mL of nanofat in approximately 6 to 7 min.
We started to apply this method in January 2019 and have used it in 86 patients, treating 112 areas, without any complications [Table 1]. The average patient age was 58.7 years. Videos 1 and 2 present each device in action, demonstrating the difference between the methods. Figures 2–4 show pre- and postoperative results of different patients who underwent fast nanofat microneedling, either as a standalone procedure or in association with face- and necklift. Table 2 shows patient evaluations of results, with the majority (84.8%) considering their result very good or good. Only three patients (3.48%) considered that there was no difference.
Table 1.
Procedures and treatment regions
| Procedure | Patients (n) | Treatment regions | Treatments performed (n) |
|---|---|---|---|
| Facelift | 29 | Frontal | 20 |
| Décolletage | 15 | ||
| Hands | 8 | ||
| Periorbital and/or Perioral | 7 | ||
| Endoscopic browlift + blepharoplasty | 12 | Frontal | 8 |
| Periorbital and/or Perioral | 18 | ||
| Décolletage | 6 | ||
| Scar revision | 3 | Face | 2 |
| Abdomen | 1 | ||
| Liposuction (torso) | 8 | Frontal | 5 |
| Periorbital and/or Perioral | 3 | ||
| Décolletage | 4 | ||
| Lipoabdominoplasty | Frontal | 7 | |
| Periorbital and/or Perioral | 6 | ||
| Décolletage | 3 | ||
| Hands | 2 | ||
| Blepharoplasty | 9 | Frontal | 4 |
| Periorbital and/or Perioral | 4 | ||
| Décolletage | 3 | ||
| Total | 86 | 112 |
Figure 2.
Preoperative (A,C) and 1 year postoperative views of a 58-year-old female who underwent fast nanofat microneedling in association with face- and necklift. Improvement in skin pigmentation and texture, as well as improvement of fine rhytides, are noted
Figure 4.
(A,C) Preoperative and (B,D) 1 year postoperative images of a 73-year-old female who underwent face and necklift as well as fast nanofat microneedling. Close-up views show improvement of the perioral and chin regions, with decreased fine rhytides and pigmentation (this area medially to the nasolabial folds is not undermined or otherwise treated by facelift)
Table 2.
Patient evaluation of results of microneedling
| Very good | n = 18 | 20.9% |
| Good | n = 55 | 63.9% |
| Slight improvement | n = 10 | 11.62% |
| No difference | n = 3 | 3.48% |
| Total | 86 | 100% |
Figure 3.
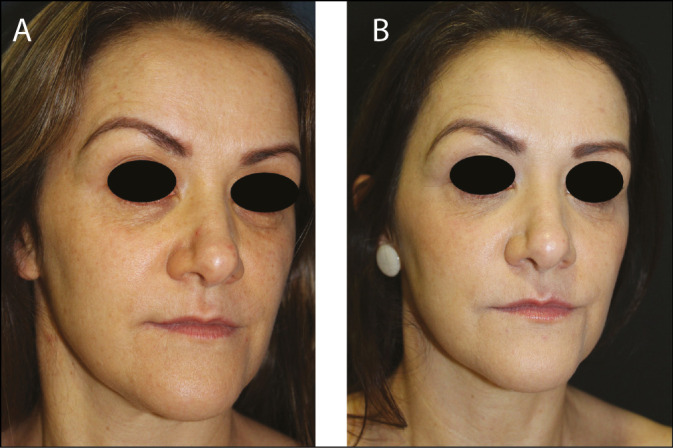
(A) Preoperative and (B) postoperative images of a 44-year-old female who underwent fast nanofat microneedling as a standalone procedure. Improvement in fine rhytides and pigmentation, especially in the infraorbital area, can be noted
The 15.1% of patients who reported a slight improvement or none at all were over the age of 65, with greater photodamage, and with complaints relating to areas of thicker epidermis and dermis, such as the hands [Figure 5] and décolletage [Figures 6 and 7]. However, we did not perform an evaluation of results by specific treatment area, but rather the overall result.
Figure 5.
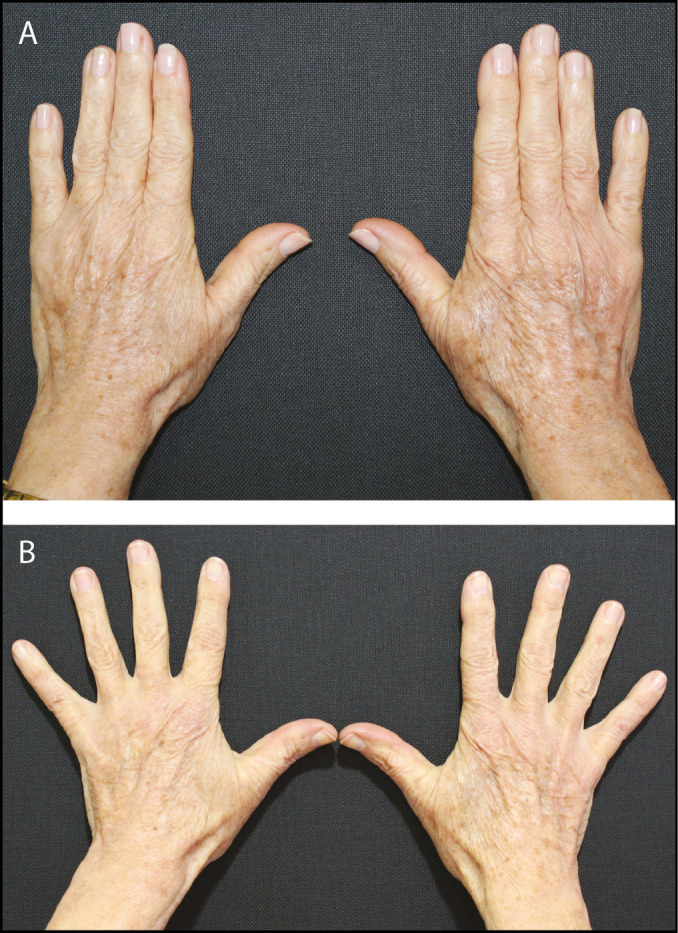
(A) Preoperative and (B) 14-month postoperative views of fast nanofat microneedling performed to the dorsal hands of a 68-year-old female demonstrating improvement in skin quality and turgor. No structural (volumetric) fat grafting was performed
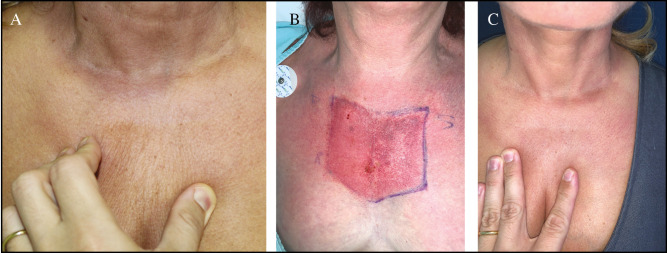
Figure 6.
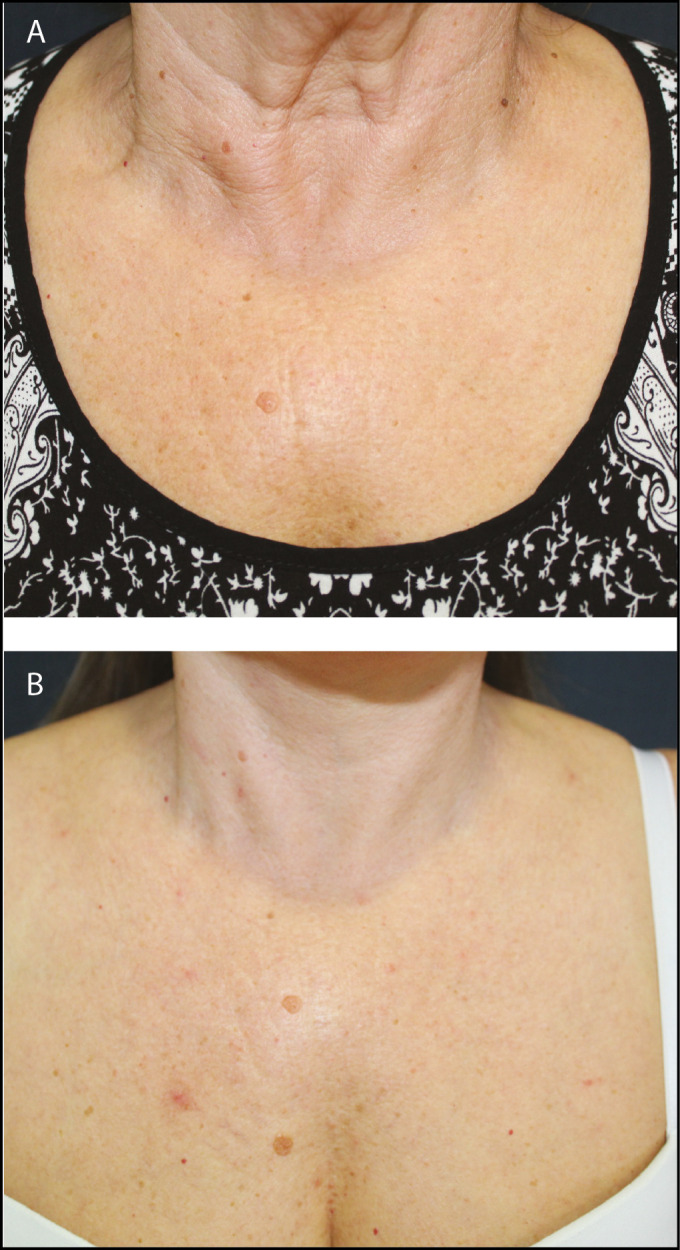
Décolletage area of a 54-year-old Caucasian woman who underwent facelift, necklift with medial platysmaplasty and fast nanofat needling. (A) Preoperative; (B) 12-month postoperative, showing improvement in skin texture and fine rhytides
Figure 7.
Décolletage area of a 47-year-old Caucasian woman who underwent fast nanofat needling. She did not undergo additional facial or neck procedures. (A) Preoperative view demonstrating loss of elasticity when pinching the skin; (B) view at end of procedure, with the goal of diffuse pinpoint bleeding; (C) postoperative view at 14 months showing improvement of elasticity, with decreased fine rhytides on skin pinch
Six patients had prolonged erythema, which lasted on average 10 days, resolving completely between 15 and 20 days. An additional four patients who underwent lower blepharoplasty had prolonged periorbital edema which resolved after 2 weeks. Pruritus which persisted beyond 30 days was present in two patients who underwent treatment of the hands and one patient who underwent treatment of the décolletage. This resolved within 5 days with topical corticosteroid cream (betamethasone dipropionate 0.05%).
DISCUSSION
Microneedling has become an increasingly popular minimally invasive resurfacing procedure, with the goal of controlled dermal damage—the clinical endpoint being a pinpoint uniform bleeding—which in turn stimulates regeneration of treated areas of skin.[4,5] Clinical results are similar to other noninvasive methods such as laser, but with lower cost, less risk of hyperpigmentation, potentially making it a better option for darker skin types,[6] and potentially less downtime.[7]
Manual, motorized, and radiofrequency coupled devices are available, with no clear clinical superiority of one device over the others, however, with increased costs associated with motorized and radiofrequency coupled devices.
Microneedling is thought to work via stimulation of a controlled injury with subsequent healing and collagen remodeling.[8] In animal models, the TGF (transforming growth factor) family of factors may play a role; specifically, a preferential stimulation of anti-fibrogenic TGF-β3 may be responsible for the rearrangement and deposit of collagen fibers in a lattice pattern, as in normal skin, as opposed to a parallel arrangement, as seen in scars. Additionally, VEGF (vascular endothelial growth factor) is upregulated after microneedling and may have a role in neoangiogenesis and keratinocyte function.[9] Microneedling has also been shown to play a role in regulation of abnormal pigmentation by altering melanocyte-stimulating hormone and interleukin-10 secretion, and this has been demonstrated clinically in burn scar therapy.[10] In summary, animal studies show an increased epidermal thickness of up to 112% at 8 weeks, with fewer gaps in the stratum corneum; upregulation of type 1 collagen; increased glycosaminoglycans in the dermis; increased fibronectin expression, a marker of fibroblast differentiation and a mediator for collagen alignment.[11,12]
Microneedling increases skin permeability, allowing for increased transdermal penetration[13,14] of medications and other substances.[15] Preclinical studies point to possible benefits in fat retention rates with microneedling in association with fat grafting.[16,17] Results by Sezgin and Özmen[18] suggest that facial skin quality is improved when performing microneedling in addition to fat grafting for both cosmetic and reconstructive indications (revision of scars and burns).
Studies by Lee et al.[19] on skin aging, using secretory factors derived from human embryonic stem cells, showed a statistically significant improvement when microneedling was performed to enhance epidermal penetration.
As the previous reports[1,2,3] state, it takes about 15 to 20 min to deliver the full content of the container (8mL) and sometimes extra volume is needed if an area beyond the face is to be treated.[3]
The original device, named HydraNeedle®, has 20 microneedles (1.5 mm length); considering an average of 3 taps per second,[2,3] each tap creates 20 microchannels, 3600 channels per minute. Thus, 72,000 microchannels are created during the 20-min treatment. From this, one can estimate a delivery rate of 1mL every 150 seconds or 0.4mL per minute. On the other hand, the HydraRoller® device possesses 64 microneedles (maximum length is 1.0 mm) and, considering an average of 3 complete rotations per second, produces a total of 11520 microchannels per minute, 230,400 microchannels during the same 20 min, delivering the 8 cc in 6 min, at an estimated injection speed of 1mL every 45s or 1.3mL per minute. Therefore, the HydraRoller® device seems to be about 3.2 times faster than the HydraNeedle®.
The shorter length of the HydraRoller® needles can be a drawback in areas of thicker skin, potentially leading to more superficial penetration and creation of less effective microchannels; skin thickness varies greatly throughout different treatment areas.[20] According to Fernandes[21] and Zeitter et al.,[11] 1 mm needles show similar results to 3 mm needles, with an advantage of less downtime, swelling, and pain.[7] On the other hand, Lima and Lima[22] state that the roller microneedles only penetrate 50 to 70% of their length, so microneedles of 1 mm barely reach the superficial dermis, possibly promoting less collagen induction.
To surpass this inconvenient of shorter needles and shallow penetration, we suggest using a mixed technique, starting with the HydraRoller®, delivering about 90% of estimated nanofat volume, and concluding the procedure with the HydraNeedle®, applying the last 10%. This strategy saves a considerable amount of time, delivering 8mL in approximately 6 to 7 min.
From January 2019 to January 2020, we used this technique on 86 patients, treating 112 areas, without any complications and with minimal patient complaints. No patients had delayed healing, hypertrophic or visible scarring, nor granuloma or nodule formation.
When using the HydraRoller®, the device should move in all directions: horizontal, vertical, and oblique, covering evenly all areas. The HydraNeedle® should be applied gently, covering all surfaces. The stamp delivers the nanofat by puncturing the skin, solely in a vertical direction. The roller makes distribution of fat in any direction possible.
The needles in a roller initially penetrate at an angle and then go deeper as the roller turns. Finally, the needle is extracted at the convex angle and therefore the tracts are curved, reflecting the path of the needle as it rolls into and then out of the skin. The epidermis and particularly the stratum corneum remain intact, except for these tiny holes, which are about four cells in diameter.[23] Lima and Lima[22] also classified the inflicted injury as mild (0.5 mm needles), moderate (1.0 and 1.5 mm needles), and deep (2.0 to 2.5 mm needles), showing a direct relationship between the inflicted trauma and needle length. Needles of 0.25 mm and 0.5 mm are used for drug delivery in fine wrinkles and to improve texture and shine of skin; 1 mm and 1.5 mm needles are used for improvement in skin laxity and medium-depth wrinkles, while 2 mm and 2.5 mm needles are used for distensible depressed scars, striae, and wavy, retractable scars.[24]
The skin should be needled as densely as possible. Usually, as the needle holes get too close to each other, the needle “slips” into an established hole and so it seems impossible to over treat the skin. The higher number of microchannels can result in a higher injury, promoting a superior release of growth factors and infiltration of fibroblasts, resulting in more collagen and elastin.[5] The endpoint of the procedure is diffuse transient punctate bleeding, an uncertain parameter that turns the technique operator dependent.
Additional studies are needed, including biopsy and histological analysis, in order to define the ideal depth of microneedling and the role of nanofat in cutaneous rejuvenation. Additionally, there may be differences in both needle penetration and mechanical trauma leading to differences in subsequent skin repair and regeneration. Due to the variable skin thickness of the face, striae and scars, devices with longer needles (such as conventional rollers which achieve a depth of up to 3 mm) may provide improved results and expand indications for needling.
CONCLUSIONS
We have been using the mixed protocol, roller plus stamp, for over 18 months. The combination of nanofat grafting with needling appears to be a smart strategy, since both techniques are effective and synergistic. Combining two different needling devices, stamp and roller, in order to speed up the procedure, seems to save surgical time without any drawbacks. Future research should analyze the best manner to maximize the benefits of nanofat microneedling. Questions regarding ideal needle length, injected nanofat volume and type of device still need to be answered.
Compliance with ethical standards
All procedures were performed in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments. All patients gave written informed consent for surgery, publication of data and photos.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflict of interest
The authors declare that they have no conflicts of interest to disclose.
All videos available online www.jcasonline.com
REFERENCES
- 1.Tonnard P, Verpaele A, Peeters G, Hamdi M, Cornelissen M, Declercq H. Nanofat grafting: Basic research and clinical applications. Plast Reconstr Surg. 2013;132:1017–26. doi: 10.1097/PRS.0b013e31829fe1b0. [DOI] [PubMed] [Google Scholar]
- 2.Verpaele A, Tonnard P, Jeganathan C, Ramaut L. Nanofat needling: A novel method for uniform delivery of adipose-derived stromal vascular fraction into the skin. Plast Reconstr Surg. 2019;143:1062–5. doi: 10.1097/PRS.0000000000005455. [DOI] [PubMed] [Google Scholar]
- 3.Tonnard P, Verpaele A, Carvas M. Fat grafting for facial rejuvenation with nanofat grafts. Clin Plast Surg. 2020;47:53–62. doi: 10.1016/j.cps.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 4.Alster TS, Graham PM. Microneedling: A review and practical guide. Dermatol Surg. 2018;44:397–404. doi: 10.1097/DSS.0000000000001248. [DOI] [PubMed] [Google Scholar]
- 5.Majid I. Microneedling therapy in atrophic facial scars: An objective assessment. J Cutan Aesthet Surg. 2009;2:26–30. doi: 10.4103/0974-2077.53096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liebl H, Kloth LC. Skin cell proliferation stimulated by microneedles. J Am Coll Clin Wound Spec. 2012;4:2–6. doi: 10.1016/j.jccw.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ramaut L, Hoeksema H, Pirayesh A, Stillaert F, Monstrey S. Microneedling: Where do we stand now? A systematic review of the literature. J Plast Reconstr Aesthet Surg. 2018;71:1–14. doi: 10.1016/j.bjps.2017.06.006. [DOI] [PubMed] [Google Scholar]
- 8.Schmitt L, Marquardt Y, Amann P, Heise R, Huth L, Wagner-Schiffler S, et al. Comprehensive molecular characterization of microneedling therapy in a human three-dimensional skin model. PLoS One. 2018;13:e0204318. doi: 10.1371/journal.pone.0204318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aust MC, Reimers K, Kaplan HM, Stahl F, Repenning C, Scheper T, et al. Percutaneous collagen induction-regeneration in place of cicatrisation? J Plast Reconstr Aesthet Surg. 2011;64:97–107. doi: 10.1016/j.bjps.2010.03.038. [DOI] [PubMed] [Google Scholar]
- 10.Busch KH, Aliu A, Walezko N, Aust M. Medical needling: Effect on skin erythema of hypertrophic burn scars. Cureus. 2018;10:e3260. doi: 10.7759/cureus.3260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zeitter S, Sikora Z, Jahn S, Stahl F, Strauß S, Lazaridis A, et al. Microneedling: Matching the results of medical needling and repetitive treatments to maximize potential for skin regeneration. Burns. 2014;40:966–73. doi: 10.1016/j.burns.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 12.Iosifidis C, Goutos I. Percutaneous collagen induction (microneedling) for the management of non-atrophic scars: Literature review. Scars Burn Heal. 2019;5:2059513119880301. doi: 10.1177/2059513119880301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wermeling DP, Banks SL, Hudson DA, Gill HS, Gupta J, Prausnitz MR, et al. Microneedles permit transdermal delivery of a skin-impermeant medication to humans. Proc Natl Acad Sci USA. 2008;105:2058–63. doi: 10.1073/pnas.0710355105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fabbrocini G, De Vita V, Fardella N, Pastore F, Annunziata MC, Mauriello MC, et al. Skin needling to enhance depigmenting serum penetration in the treatment of melasma. Plast Surg Int. 2011;2011:158241. doi: 10.1155/2011/158241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schoenberg E, O’Connor M, Wang JV, Yang S, Saedi N. Microneedling and PRP for acne scars: A new tool in our arsenal. J Cosmet Dermatol. 2020;19:112–4. doi: 10.1111/jocd.12988. [DOI] [PubMed] [Google Scholar]
- 16.Sezgin B, Ozmen S, Bulam H, Omeroglu S, Yuksel S, Cayci B, et al. Improving fat graft survival through preconditioning of the recipient site with microneedling. J Plast Reconstr Aesthet Surg. 2014;67:712–20. doi: 10.1016/j.bjps.2014.01.019. [DOI] [PubMed] [Google Scholar]
- 17.Samdal F, Skolleborg KC, Berthelsen B. The effect of preoperative needle abrasion of the recipient site on survival of autologous free fat grafts in rats. Scand J Plast Reconstr Surg Hand Surg. 1992;26:33–6. doi: 10.3109/02844319209035180. [DOI] [PubMed] [Google Scholar]
- 18.Sezgin B, Özmen S. Fat grafting to the face with adjunctive microneedling: A simple technique with high patient satisfaction. Turk J Med Sci. 2018;48:592–601. doi: 10.3906/sag-1711-42. [DOI] [PubMed] [Google Scholar]
- 19.Lee HJ, Lee EG, Kang S, Sung JH, Chung HM, Kim DH. Efficacy of microneedling plus human stem cell conditioned medium for skin rejuvenation: A randomized, controlled, blinded split-face study. Ann Dermatol. 2014;26:584–91. doi: 10.5021/ad.2014.26.5.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chopra K, Calva D, Sosin M, Tadisina KK, Banda A, De La Cruz C, et al. A comprehensive examination of topographic thickness of skin in the human face. Aesthet Surg J. 2015;35:1007–13. doi: 10.1093/asj/sjv079. [DOI] [PubMed] [Google Scholar]
- 21.Fernandes D. Minimally invasive percutaneous collagen induction. Oral Maxillofac Surg Clin North Am. 2005;17:51–63, vi. doi: 10.1016/j.coms.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 22.Lima EVA, Lima MA, Takano D. Microneedling experimental study and classification of the resulting injury. Surg Cosmet Dermatol. 2013;5:110–4. [Google Scholar]
- 23.Kalluri H, Kolli CS, Banga AK. Characterization of microchannels created by metal microneedles: Formation and closure. Aaps J. 2011;13:473–81. doi: 10.1208/s12248-011-9288-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lima EVA, Lima MA, Takano D. Microagulhamento: Estudo experimental e classificação da injúria provocada. Surg Cosmet Dermatol. 2013;5:110–4. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.