Abstract
Background:
Stretch marks (SM) are nowadays the most common aesthetic pathology of the body; in the XX century, it mainly affected pregnant women, while today it also affects teenagers during puberty, boys and girls without distinction. The aim of this study was to evaluate possible variations in the histological structure of the skin—in terms of quality/quantity of the extracellular matrix and of the collagen and elastic fibers—following the electromagnetic fields and negative pressure (V-EMF) treatment as regards hypotonia and SMs.
Materials and Methods:
For the current study, 60 women, aged between 25 and 45, were examined. All of them presented deep, white or pearly white colored SMs having had them for between 12 and 25 years. These were documented, asking patients their level of satisfaction, through pictures and biopsies. All patients underwent a cycle of 6 or 8 weekly sessions; everyone was highly satisfied with the results obtained.
Results:
Biopsies proved that the tissue was reorganized and restored to the original volume, characterized by the production of new, high-quality collagen and elastin molecules, by the reorganization of the basement membrane and by the correct positioning of the melanocytes. No side effects were observed during the treatments. This synergy stands as the most suitable treatment of striae rubra and alba.
Conclusion:
V-EMF enhances the keratinocyte migration base, melanocytes, and promotes neoangiogenesis with the result of improvement in the SM.
Keywords: Electromagnetic fields, negative pressure, skin aging, stretch marks
INTRODUCTION
Stretch marks (SM) are nowadays the most common aesthetic pathology of the body; in the XX century, it mainly affected pregnant women, whereas today it also affects teenagers during puberty, boys and girls without distinction. Microdermabrasion, needling therapy, and various types of lasers have been used for the treatment of SM, but to date none is able to deal with this aesthetic pathology with certain, satisfactory and systematic outcomes on all patients, both from the point of view of reducing the depth of the line and the typical hypopigmentation of the mature striae.[1,2,3] No current therapeutic option offers complete treatment, although there are a few emerging new modalities that are encouraging.[1] Microdermabrasion was probably the first instrumental method applied to SM and yet it does not have a significant bibliographical reference. Anyhow, the therapy showed an improvement in only the stria rubra and limited or nil improvement of the stria alba.[4,5] Histological analysis documents an increase in procollagen I.[4] Lasers have become the most common technology in the treatment of striae; these include pulsed-day laser (PDL), excimer lasers (ELs), the short-pulsed carbon dioxide fractional lasers (CO2FLs), Nd: YAG lasers, the non-ablative Er:Glass fractional lasers (NAFL), diode lasers, and fractional photothermolysis. Below we analyze what emerges from the published studies.
Magnets have been used in clinical practice since ancient times by Egyptians, Greeks, and Chinese.[6] Electromagnetic fields and negative pressure is a new treatment for hypotonia and SM. The aim of this study was to evaluate the effectiveness of the electromagnetic fields and negative pressure in the treatment of SM through a clinical and histological evaluation of variations of quality/quantity of the extracellular matrix and of the collagen and elastic fibers.
MATERIALS AND METHODS
This study was conducted in a private office of Verona (Italy), in full accordance with ethical principles, including the World Medical Association Declaration of Helsinki (https://www.wma.net/wp-content/uploads/2018/07/DoH-Oct2008.pdf) and the additional requirements of Italian law. The sample included 60 healthy adult Caucasian female patients, suffering simultaneously from cutaneous hypotonia and SM. The selected patients were between 25 and 45 years of age, and body mass index (BMI) was between 21 and 27 and historically healthy.
The subjects were normal-weight or slightly overweight without complications of any diagnosis of degenerative diseases and lifestyle habits that would have favored aging, such as smoking, alcohol abuse, etc.
Each patient signed informed consent on the adopted procedure, but none of the patients knew which pathology the treatment was aimed at.
The diagnosis for all was a simultaneous presence of cutaneous hypotonia, cellulite, and white SM (whose onset time has not been documented).
The exclusion criteria for patients were as follows:
pacemaker carriers,
surgery or cancer treatment in the last 5 years,
epilepsy,
vascular insufficiency located in the area to be treated (thrombosis, thrombophlebitis, varicose veins),
skin inflammation of the area to be treated,
open wounds in the area to be treated,
ongoing anticoagulant therapy,
pregnancy or breastfeeding,
incidents of anorexia or bulimia in the last 2 years,
previous treatment of SM with other therapies.
The patients belonging to the study group underwent a cycle of six to eight sessions, with weekly treatments, without the addition of any active ingredients. The patients were all in the phototypes II and III of the Fitzpatrick scale with skin areas affected with white SM, hypotonia, and cellulite. The treatments were administered between March 18 and May 2019 with follow-up of 90 days. The clinical study, developed in an observational and microscopic manner using histology, followed the double-blind control procedure randomized in parallel groups.
At the end of the course of treatment, all the patients expressed a rate of satisfaction on the result achieved.
Electromagnetic fields and negative pressure device therapy (V-EMF)
The device that generates the V-EMF (Expo Italia Srl, Florence, Italy) was used in the present study.
The device was equipped with a generator of electromagnetic fields, an electron flow generator, a pair of vacuum pumps, and a series of handpieces. The apparatus acts through the use of magnetic fields. The electromagnetic field, fundamental for this technology, which is based on the synergy between the electromagnetic field, vacuum effect, and low-intensity electrical stimulation, is generated with an electric signal with a variable frequency between 500 and 1000 Hz, projected toward handpieces that are completely covered with a dielectric material. Even the passage of the electrical signal, from the device toward the handpiece, takes place inside a special electric cable covered with a high-density metal mesh, destined to create a real Faraday cage that prevents the signal from being dispersed in the environment. The part of the handpiece in contact with the skin of the patient is covered with a dielectric material of very high electrical resistance, intended to constitute an insulating barrier. The insulating structure thus created is placed in contact with the patient’s skin with which it interacts, creating an effect similar to that of a capacitor.
The dielectric coating prevents the passage of the electrical signal from the device to the patient’s skin, but, instead, allows the stimulation of the electric charges present inside the biological tissue.
The charges move in relation to the electric potential supplied by the device, which acts by rejecting the similar ones and attracting the opposites. The continuous polarity change leads to a continuous flow of endogenous electric charges, which move inside these tissues, with particular attention to the activity of sodium Na+ and potassium K+ ions whose action of permeability of cell membranes increases per unit of time. The continuous kinetic activity of the ions and the rapid rotation of the dipoles present cause a partial transformation of the motion kinetic energy into stabilized thermal energy, never below 39°C and never above 40°C utilizing the biofeedback system provided in the device. The brushless vacuum pumps allow the delivery of negative pressure with absolute precision and stability, with a maximum value of ‒0.35 atm.
Histology processing
Each patient underwent biopsies at different times during the therapeutic procedure before and after treatment.
The biopsies were carried out to document:
epithelial basal cells;
epithelial thickness;
number of melanocytes;
vessel number;
qualitative evaluation of type III collagen with multiple stained histology;
qualitative evaluation of elastic fibers with multiple stained histology.
The treated area and site of the biopsy was the culotte de cheval.
Each patient underwent two biopsies, before and after treatment; a total 120 biopsies were performed. These were performed with a circular punch biopsy of 2 mm diameter (KAI Industries, Oyana, Japan).
The histological tests were performed and validated at the Department of Neuroscience, Biomedicine, and Movement, Anatomy and Histology Section, University of Verona, Italy.
The specimens were stained with hematoxylin and eosin, Masson’s trichrome, and Van Gieson. Four fields of 2000 μm in diameter and 4000 μm long were evaluated for each sample.
Statistical analysis
A power analysis was performed using clinical software for determining the number of samples needed to achieve statistical significance for quantitative analyses of cell numbers for:
epithelial basal cells;
epithelial thickness;
number of melanocytes;
vessel number.
A calculation model was adopted for dichotomous variables (yes/no effect) by using the incidence effect designed to discern the reasons (80% for the test group and 20% for the control group), with alpha = 0.05 and power = 95%.
The optimal number of samples for analysis was 60 patients per group.
Numerical results are presented as means±SD for all the experiments.
The data outcome was collected and statistically evaluated by the software package GraphPad 6 (Prism, San Diego, CA, USA). The normal distribution of the study data was evaluated by the Kolmogorov–Smirnov test to evaluate the normal distribution. The Wilcoxson signed-rank test was performed to compare the study variables’ means in each group. The level of significance was set at P < 0.05.
RESULTS
Patients were questioned at the end of the study on any changes of the skin: of the total 60 patients, 57 responded that they had observed considerable changes especially in the brightness of the skin in the treated area, and three responded that they noticed only a slight change but that the skin was different.
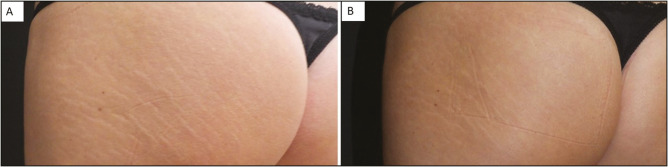
However, all 60 patients expressed a positive judgment of skin compactness and tactile sensation. The objective results are shown with photographic images before and after the completed treatment in some of the patients treated [Figure 1]. We observed decreased striae and initial tanning, leading to a reorganization of the skin layers and to a restoration of the melanocytes.
Figure 1.
Before (A) and after (B) 9 V-EMF treatment. The evident and deep striae appear now filled, soft to touch and their color is much more similar to the surrounding normal skin, all this due to a better vascularization
Histological analysis
After an initial objective evaluation using photographic images before and after treatment, an associated histological evaluation was performed with different staining, to highlight the ultrastructural aspects of the epidermis and dermis.
The histological results of the slides were read by two pathologists working in two different medical universities, Verona and Modena Reggio Emilia, to minimize the possibility of misinterpretation.
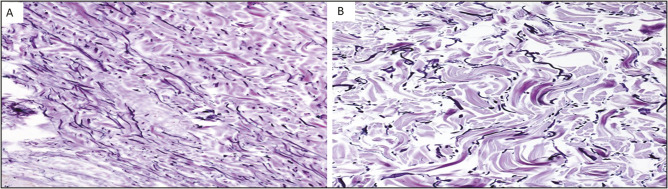
Before treatment
The epidermis of the SM demonstrated loss of the rete ridge pattern and collagen bundles perpendicular to the surface, which appeared disorderly spaced [Figures 1–5]. Additionally, alteration of the microcirculation was evident before treatment. Few melanocytes were observed. No inflammatory cells were observed in the epithelium or epidermis. The histomorphometric results are shown in Figure 6 and Table 1.
Figure 5.
A. Before treatment. Disorganized collagen fibers with differing volumes, with this staining the alteration of the microcirculation is more evident. Masson Gold Trichrome. ×40. B. After treatment. Well-organized collagen fibers of constant volume. Masson Gold Trichrome. ×60
Figure 6.
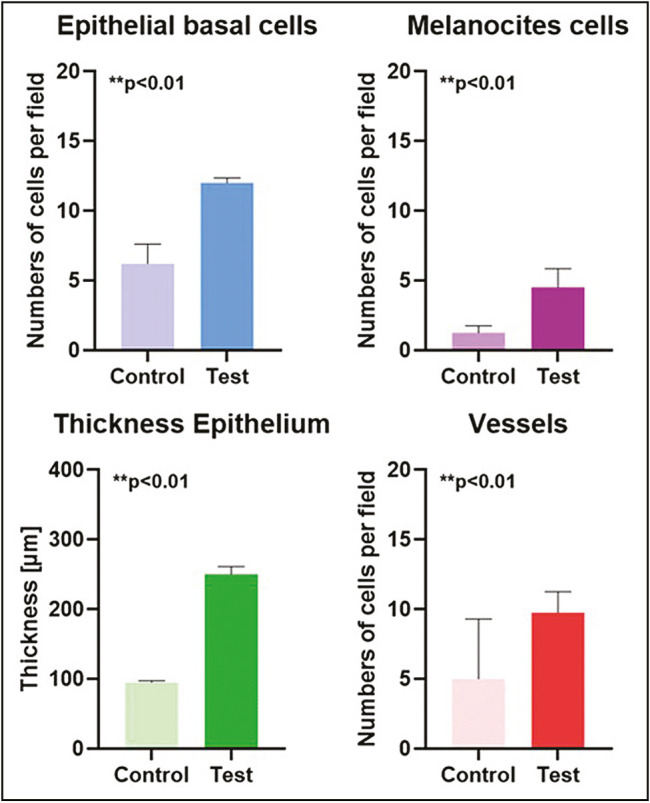
The bar graphs show the epithelial basal cells, epithelial thickness, melanocytes, and vessel number (mean, standard deviation)
Table 1.
Summary of the means count of Epithelial Basal Cells, Thickness Epithelial, Melanocites, Number Vessel
| Groups | Epithelial basal cells | Epithelial thickness (µm) | Number of melanocytes | Vessel number | ||||
|---|---|---|---|---|---|---|---|---|
| Control | Test | Control | Test | Control | Test | Control | Test | |
| Average (SD) | 6.21 ± 1.4 | 12.01 ± 0.4 | 95.5 ± 2.22 | 250 ± 11.77 | 1.25 ± 0.7 | 4.52 ± 0.33 | 5 ± 4.4 | 9.75 ± 1.5 |
| P-value | P < 0.01 | P < 0.01 | P < 0.01 | P < 0.01 | ||||
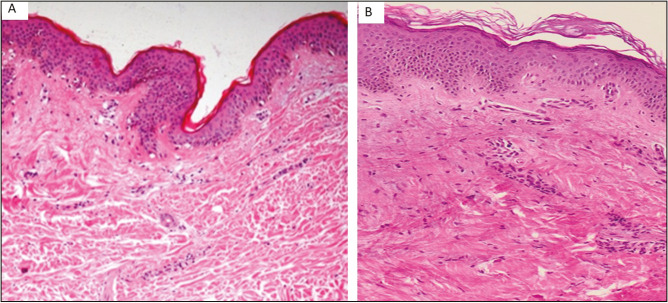
Figure 2.
A. Section of skin including epidermis and dermis. Before treatment. Hematoxylin and eosin. ×10. White SM. B. After treatment. The epidermis shows up with increased thickness; moreover, the visible collagen appears reorganized and the microcirculation is present. Hematoxylin and eosin. ×10. White SM
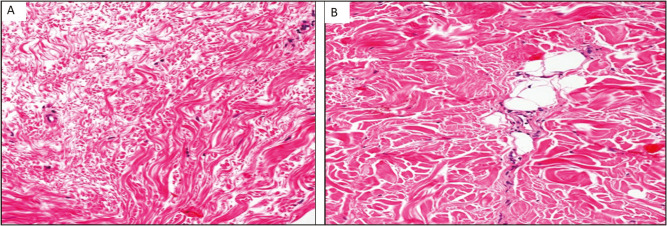
Figure 3.
A. Skin section, specific to the dermis, before treatment. Disorganized collagen fibers with different volumes. Hematoxylin and eosin. ×40. B. After treatment. Collagen fibers increased in volume and reorganized. Hematoxylin and eosin. ×40
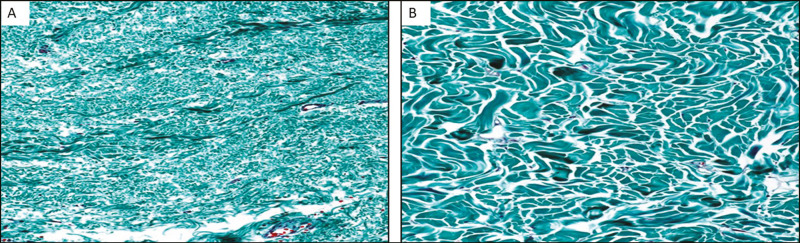
Figure 4.
A. Before treatment. Elastic fibers disorganized. Weigert. ×40. B. After treatment. White SM. Elastic fibers, well-formed, long, and stretched. Weigert. ×40
After treatment
the epidermis showed increased thickness; moreover, the visible collagen appeared reorganized and the microcirculation was present. The epidermis had a basket weave appearance and well-formed rete ridges. Additionally, normal dermis demonstrated collagen bundles parallel to the surface, which were evenly spaced. There was a clear increase in epidermal thickness and the presence of melanocytes; no inflammatory cells were observed in the epithelium or epidermis [Figures 1–5]. The histomorphometric results are shown in the table and [Figure 6] (Table).
DISCUSSION
The results of the present study indicate that the treatment adopted is associated with an increased and structural regulation of collagen in the dermis, increase in cellular replication of the epidermis with increased thickness, and repositioning with the regulation of melanocytic cells, with considerable synthesis of elastic fibers that lose their point-like structure.
In addition to the general reorganization of the treated tissue, good angiogenesis with good microcirculation architecture was evident. Patients’ statements on improved skin brightness and compactness are linked to the aforementioned: improvement of the quality of hyaluronic acid, increase in type 3 collagen concentration, and regularization of epidermis metabolism.
In addition to the clinical evidence of the results, it was observed that the treatment was considered pleasant and relaxing by all patients, who could maintain their normal lifestyle. Furthermore, no side effects nor down time occurred. The choice of the range of frequencies adopted, i.e. low frequencies, allows a real activity of crossing of the cell membranes by the Na+ and K+ ions due to an effective action of induced ionic migration, unlike what happens with higher frequencies with which one obtains at most an ionic vibration and therefore only a thermal effect but not the action of Na+ and K+ carriers on cells and fibroblasts. This difference is essential in the histological evaluation, which allows us to understand the regeneration obtained, or rather the increase in the presence of collagen and elastic fibers and the greater cellular mitosis, a consequence of the cellular nutrition induced by the Na+ and K+ pumps and not by the induced thermal effect.
The stimulation induced by the V-EMF device determines a series of clinically appreciable benefits in the cutaneous areas affected by various pathological conditions, such as relaxation, micro-wrinkles, spots, acne, cellulite, and SM.
The benefits can be attributable to the combined effect of three mechanisms:
-
(a)
the increase of the blood microcirculation, which facilitates the oxygenation of the treated tissues;
-
(b)
stimulation of tissue cellular metabolism which, among other things, favors the transmission of any active ingredients;
-
(c)
stimulation of fibroblasts (both mechanical and respiratory), which induces the production of collagen and elastin.
Starting from these assumptions, the present study aims to evaluate the effect of the V-EMF treatment on the histological framework of the skin, in order to help clarify the efficacy detected, from a clinical point of view, in the different conditions in which the technique is indicated.
The choice of this experimental approach seems to be the most suitable to document the observed clinical effectiveness in an objective way, so as to make both the doctor and the patient confident, also in terms of safety and risk/benefit ratio.
Similar results were achieved by Artigiani et al.[7] This technology has already shown a great potential in the regeneration of the striae, claiming to witness a “real restructuring of the stretch mark without any side effects,” documenting the outcomes on white SM aged between 7 and 35 years, also on patients with high levels of skin phototypes. The researchers also state that the therapy was found to be effective on all treated patients. The most interesting aspect of this article is the abundant bioptic documentation, which demonstrates a real cutaneous repair of the striated tissue, with the reorganization of the basement membrane and multiplication of collagen and elastic fibers.
In a similar way, Nicoletti et al.[8] documented a significant reparative action in the treatment of post-surgical and burn scars, stating that the combined sequential local treatment of hypertrophic scars, with low-intensity electromagnetic and electric stimulation in association with negative pressure, demonstrated a favorable synergic effect on the scar collagen and remodeling of the elastic fibers network. An amplification of the effects of three different well-known physical energies was therefore obtained without any side effects.
Analyzing the results obtained, we see that after three sessions two out of 10 patients left the study, three out of 10 patients reported no results (no improvement) and five reported little result (poor). The same patients after a 3-month follow-up declared the following: no result in 2 out of 10 and little result in 6 out of 10. The photos document a poor outcome. In addition to the dubious outcomes encountered by the authors, the NAFL is characterized by a moderate pain during therapy,[9,10,11] micro-crusting,[10] recurrent edema, and hyperpigmentation,[9,11,12] which is generally reabsorbed in 5/10 days, with a maximum duration of hyperpigmentation of 8 weeks.[13]
de Angelis et al.[14] recommend prophylaxis to patients in the month before the treatments and in the following 6 months. Therefore, the limitations due to the heterogeneity of the laser trials (wavelength, protocols) have an unclear effect on the SM. There is evidence that EMF promotes bone formation and therefore can be used in regenerative applications aimed at bone fracture healing[15] and bone augmentation procedure.[16] EMF has positive effects during cartilage regeneration[17] and can be used for its positive impact on epidermal stem cell proliferation which may result in beneficial effects.[18] Many clinical practice guidelines recommended that NP can be used for reducing the healing time of surgical wounds.[19]
In conclusion, the results of the present study show that V-EMF enhanced an increased rate of the epithelium thickening, the number of melanocytes, and vascularization with improved color of the SM.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Elsaie ML, Baumann LS, Elsaaiee LT. Striae distensae (stretch marks) and different modalities of therapy: An update. Dermatol Surg. 2009;35:563–73. doi: 10.1111/j.1524-4725.2009.01094.x. [DOI] [PubMed] [Google Scholar]
- 2.Hague A, Bayat A. Therapeutic targets in the management of striae distensae: A systematic review. J Am Acad Dermatol. 2017;77:559–68.e18. doi: 10.1016/j.jaad.2017.02.048. [DOI] [PubMed] [Google Scholar]
- 3.Keen MA. Striae distensae: What’s new at the horizon? Br J Med Practition. 2016;9:a919. [Google Scholar]
- 4.FAAD DSSM. Therapeutic update on the treatment of striae distensae. J Drugs Dermatol. 2015;14:11–2. [PubMed] [Google Scholar]
- 5.Ali M, Basma M, El-Tatawy RA, Elfar NN, Ali M, Dareen A. A comparative clinical and histopathological study of microneedling versus microdermabrasion (aluminum oxide crystals) in the treatment of striae distensae. J Egypt Women’s Dermatol Soc. 2017;14:92–9. [Google Scholar]
- 6.Null G. Healing with magnets. New York, NY: Carroll & Graf Publishers, Inc.; 1998. [Google Scholar]
- 7.Artigiani A, Cervadoro G, Loggini B, Paolocchi A. Biodermogenesi: La soluzione non invasiva al trattamento delle smagliature. La Medicina Estetica. 2012;1:543–52. [Google Scholar]
- 8.Nicoletti G, Perugini P, Bellino S, Capra P, Malovini A, Jaber O, et al. Scar remodeling with the association of monopolar capacitive radiofrequency, electric stimulation, and negative pressure. Photomed Laser Surg. 2017;35:246–58. doi: 10.1089/pho.2016.4180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim BJ, Lee DH, Kim MN, Song KY, Cho WI, Lee CK, et al. Fractional photothermolysis for the treatment of striae distensae in Asian skin. Am J Clin Dermatol. 2008;9:33–7. doi: 10.2165/00128071-200809010-00003. [DOI] [PubMed] [Google Scholar]
- 10.Stotland M, Chapas AM, Brightman L, Sukal S, Hale E, Karen J, et al. The safety and efficacy of fractional photothermolysis for the correction of striae distensae. J Drugs Dermatol. 2008;7:857–61. [PubMed] [Google Scholar]
- 11.Malekzad F, Shakoei S, Ayatollahi A, Hejazi S. The safety and efficacy of the 1540 nm non-ablative fractional XD probe of Star Lux 500 device in the treatment of striae alba: Before-after study. J Lasers Med Sci. 2014;5:194–8. [PMC free article] [PubMed] [Google Scholar]
- 12.Yang YJ, Lee G-Y. Treatment of striae distensae with nonablative fractional laser versus ablative CO2 fractional laser: a randomized controlled trial. Ann Dermatol. 2011;23:481–9. doi: 10.5021/ad.2011.23.4.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tretti Clementoni M, Lavagno R. A novel 1565 nm non-ablative fractional device for stretch marks: A preliminary report. J Cosmet Laser Ther. 2015;17:148–55. doi: 10.3109/14764172.2015.1007061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Angelis F, Kolesnikova L, Renato F, Liguori G. Fractional nonablative 1540-nm laser treatment of striae distensae in Fitzpatrick skin types II to IV: Clinical and histological results. Aesthet Surg J. 2011;31:411–9. doi: 10.1177/1090820X11402493. [DOI] [PubMed] [Google Scholar]
- 15.Luo F, Hou T, Zhang Z, Xie Z, Wu X, Xu J. Effects of pulsed electromagnetic field frequencies on the osteogenic differentiation of human mesenchymal stem cells. Orthopedics. 2012;35:e526–31. doi: 10.3928/01477447-20120327-11. [DOI] [PubMed] [Google Scholar]
- 16.Scarano A, Carinci F, Assenza B, Piattelli M, Murmura G, Piattelli A. Vertical ridge augmentation of atrophic posterior mandible using an inlay technique with a xenograft without miniscrews and miniplates: Case series. Clin Oral Implant Res. 2011;22:1125–30. doi: 10.1111/j.1600-0501.2010.02083.x. [DOI] [PubMed] [Google Scholar]
- 17.Mayer-Wagner S, Passberger A, Sievers B, Aigner J, Summer B, Schiergens TS, et al. Effects of low frequency electromagnetic fields on the chondrogenic differentiation of human mesenchymal stem cells. Bioelectromagnetics. 2011;32:283–90. doi: 10.1002/bem.20633. [DOI] [PubMed] [Google Scholar]
- 18.Bai WF, Zhang MS, Huang H, Zhu HX, Xu WC. Effects of 50 Hz electromagnetic fields on human epidermal stem cells cultured on collagen sponge scaffolds. Int J Radiat Biol. 2012;88:523–30. doi: 10.3109/09553002.2012.692496. [DOI] [PubMed] [Google Scholar]
- 19.Webster J, Liu Z, Norman G, Dumville JC, Chiverton L, Scuffham P, et al. Negative pressure wound therapy for surgical wounds healing by primary closure. Cochrane Database Syst Rev. 2019;3:CD009261. doi: 10.1002/14651858.CD009261.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]