Abstract
Background
Homelessness continues to be a pressing public health concern in many countries, and mental disorders in homeless persons contribute to their high rates of morbidity and mortality. Many primary studies have estimated prevalence rates for mental disorders in homeless individuals. We conducted a systematic review and meta-analysis of studies on the prevalence of any mental disorder and major psychiatric diagnoses in clearly defined homeless populations in any high-income country.
Methods and findings
We systematically searched for observational studies that estimated prevalence rates of mental disorders in samples of homeless individuals, using Medline, Embase, PsycInfo, and Google Scholar. We updated a previous systematic review and meta-analysis conducted in 2007, and searched until 1 April 2021. Studies were included if they sampled exclusively homeless persons, diagnosed mental disorders by standardized criteria using validated methods, provided point or up to 12-month prevalence rates, and were conducted in high-income countries. We identified 39 publications with a total of 8,049 participants. Study quality was assessed using the JBI critical appraisal tool for prevalence studies and a risk of bias tool. Random effects meta-analyses of prevalence rates were conducted, and heterogeneity was assessed by meta-regression analyses. The mean prevalence of any current mental disorder was estimated at 76.2% (95% CI 64.0% to 86.6%). The most common diagnostic categories were alcohol use disorders, at 36.7% (95% CI 27.7% to 46.2%), and drug use disorders, at 21.7% (95% CI 13.1% to 31.7%), followed by schizophrenia spectrum disorders (12.4% [95% CI 9.5% to 15.7%]) and major depression (12.6% [95% CI 8.0% to 18.2%]). We found substantial heterogeneity in prevalence rates between studies, which was partially explained by sampling method, study location, and the sex distribution of participants. Limitations included lack of information on certain subpopulations (e.g., women and immigrants) and unmet healthcare needs.
Conclusions
Public health and policy interventions to improve the health of homeless persons should consider the pattern and extent of psychiatric morbidity. Our findings suggest that the burden of psychiatric morbidity in homeless persons is substantial, and should lead to regular reviews of how healthcare services assess, treat, and follow up homeless people. The high burden of substance use disorders and schizophrenia spectrum disorders need particular attention in service development. This systematic review and meta-analysis has been registered with PROSPERO (CRD42018085216).
Trial registration
PROSPERO CRD42018085216.
In an updated systematic review and meta analysis, Stefan Gutwinski, Stefanie Schreiter, and colleagues examine the prevalence of mental disorders among individuals who are homeless in high income countries.
Author summary
Why was this study done?
Homelessness continues to affect a large number of people in high-income countries and is associated with an increased risk of mental disorders.
To guide service development, further research, and public policy, reliable estimates on the prevalence of mental disorders among homeless individuals are needed.
Many primary investigations into rates of mental disorders have been published since a previous comprehensive quantitative synthesis in 2008.
What did the researchers do and find?
We performed a systematic database search, extracted data from primary reports, and assessed their risk of bias, resulting in a sample of 39 studies including information from over 8,000 homeless individuals in 11 countries.
We conducted random effects meta-analyses of 7 common diagnostic categories. Prevalence estimates were all increased in homeless individuals compared with those in the general population. Alcohol use disorders had the highest absolute rate, at 37%, with substantially elevated proportional excesses compared to the general population for schizophrenia spectrum disorders and drug use disorders as well.
There was substantial between-study variation in prevalence estimates, and meta-regression analyses found that sampling method, participant sex distribution, and study country explained some of the heterogeneity.
What do these findings mean?
The high burden of substance use disorders and severe mental illness in homeless people represents a unique challenge to public health and policy.
Future research should prioritize quantification of unmet healthcare needs, and how they can be identified and effectively treated. Research on subgroups, including younger people and immigrant populations, is a priority for prevalence work.
Introduction
Homelessness is recognized by the United Nations Economic and Social Council as an issue of global importance [1]. In high-income countries, around 2 million people have been homeless over the past decade [2]. In the US, the lifetime prevalence of homelessness is estimated at 4.2% [3], with around 550,000 individuals lacking fixed, regular, and adequate residence on any given night [4]. Patterns over time have differed by country, although homelessness has increased in many high-income countries in recent years, including in the US and UK since 2017 [2].
There has been an increasing recognition of the public health importance of homeless persons, with many studies reporting high rates of acute hospitalization, chronic diseases, and mortality [5–13]. Comorbidities increase these risks, particularly mental disorder comorbidities. For example, in a Danish population study, comorbidity of psychiatric disorders increased mortality rates by 70% [14]. Furthermore, mental illness among homeless individuals has been associated with elevated rates of criminal behavior and victimization [15,16], prolonged courses of homelessness [17,18], and perceived discrimination [19]. Mental disorders among homeless individuals are mostly treatable and represent an important opportunity to address health inequalities.
Information on the overall extent and pattern of mental disorders among homeless people is necessary to inform resource allocation and service development, and to allow researchers, clinicians, and policymakers to consider evidence gaps. The large number of primary studies, of varying quality and samples, means that systematic reviews are required to clarify and synthesize the evidence, underscore main findings, and consider implications. According to a recent umbrella review, there have been at least 7 systematic reviews with quantitative data synthesis in the past 2 decades [20]; however, most of them focused on individual diagnostic categories [21–24], examined specific age bands [24,25], or were limited to a single country [26]. The last meta-analysis to our knowledge that provided a comprehensive account of the prevalence of major mental disorders in homeless adults in high-income countries completed its search in 2007 [27], and since then, a considerable number of primary studies have been published [28,29]. Thus, we conducted an updated systematic review and meta-analysis on the prevalence of mental disorders among homeless people in high-income countries, and added the diagnostic categories of any mental disorder and bipolar disorder.
Methods
Search strategy
We searched for studies that determined prevalence rates for at least 1 of the following disorders among homeless persons: (1) schizophrenia spectrum disorders, (2) major depressive disorder, (3) bipolar disorder, (4) alcohol use disorders, (5) drug use disorders, (6) personality disorders, and (7) any current mental disorder (Axis I disorders in the Diagnostic and Statistical Manual of Mental Disorders [DSM] multiaxial system [30]).
We have updated an earlier review [27] that was based on a search for articles published up until December 2007, so we targeted new primary studies published between 1 January 2008 and 1 April 2021. We searched Embase via OvidSP, Medline via OvidSP and via PubMed, and PsycInfo via EBSCOhost. Additionally, we searched Google Scholar using a search query and screened all literature citing the previous review. Finally, we screened reference lists of relevant publications. Each search employed a specific combination of search terms designed to fit the databases’ respective syntaxes and thesaurus systems (S1 Table). Articles written in languages other than English or German were translated by professional translators. The protocol for this systematic review and meta-analysis has been published (PROSPERO CRD42018085216). We followed Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines for extracting and assessing data [31]. This systematic review adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (see S2 Table) [32].
Eligibility criteria and study selection
Inclusion criteria were as follows: (1) homelessness status of study participants was validated by an operationalized definition or a sampling method that specifically targeted homeless population; (2) standardized criteria for the psychiatric disorders specified above, based on the International Classification of Diseases (ICD) or DSM, were applied; (3) psychiatric diagnoses were made by clinical examination or interviews using validated semi-structured diagnostic instruments; (4) for any psychiatric disorders except for personality disorders (where lifetime rates were used), prevalence rates were reported within 12 months; and (5) study location was a high-income country according to the classification of the World Bank [33].
Surveys that reported a response rate of less than 50% or exclusively sampled from selected subpopulations (such as elderly homeless, homeless youth, or homeless single parents) were excluded.
In order to assess all results from the bibliographic search process, researchers SS, SG, and KD each carried out a multilevel screening process independently from one another. Any differences between results were resolved by consensus between all the authors.
Data collection and quality assessment
Information from included surveys was extracted on study location, year of diagnostic assessment, operational definition of homelessness status, sampling method, diagnostic procedures, diagnostic criteria, professional qualification of interviewers, response rate, dropout rate, number of participants by sex, sample mean age, current accommodation of participants, sample mean duration of homelessness, and number of participants diagnosed with schizophrenia spectrum disorders, major depressive disorder, bipolar disorder, alcohol- and drug-related disorders, personality disorders, and any primary diagnosis of a mental disorder apart from personality and developmental disorders (i.e., Axis I disorders in DSM). If data regarding any of these categories were unclear in the published study, we corresponded with the primary study authors.
Each included publication was rated on methodological quality by 2 sets of criteria specifically designed to assess prevalence studies: the JBI critical appraisal tool for prevalence studies [34] and a risk of bias tool [35]. This process was carried out by SS, SG, and KD independently, and any differences were resolved by discussion.
Statistical analysis
Random effects meta-analyses and meta-regression analyses were performed on each diagnostic category independently—prevalence data for alcohol misuse/abuse and alcohol dependence were both entered into the single category of alcohol use disorders, in accordance with current diagnostic approaches. All analyses were done in R, version 4.0.4 [36]. The package “metafor,” version 2.4–0, was utilized for meta-analysis and meta-regression analysis, supplemented by “glmulti,” version 1.0.8, for multivariable model selection and “mice”, version 3.13.0, for multivariate imputation [37–39].
Prevalence estimates were transformed on the double arcsine function in order to avoid variance instability and confidence intervals (CIs) exceeding the interval (0 ≤ x ≤ 1) in which prevalence proportions can be meaningfully defined [40]. We calculated random effects models, which we deemed appropriate considering sampling differences. The Paule–Mandel estimator was chosen to measure between-study variance due to its reliability for different types of models [41]. A Q-test for heterogeneity was conducted. To quantify measures of between-study heterogeneity, we report the test statistic QE and corresponding p-value as well as the I2 statistic. Additionally, we calculated 95% prediction intervals (PIs) for all meta-analytical models [42]. Because the “metafor::predict.rma” function unrealistically assumed that the model variance τ2 was a known value [43], we instead implemented a method proposed by Higgins and colleagues that accounts for τ2 being an estimate with limited precision ([44], expression 12).
Additional meta-analyses were carried out in each diagnostic category for low-risk-of-bias studies, assigned during quality assessment [35]. Subgroup analyses comparing low-risk-of-bias and moderate-risk-of-bias studies were performed through a Q-test. In cases of significant between-subgroup difference, a meta-regression model with risk of bias assessment as a single independent variable was computed to estimate the proportion of variance explained by disparities in methodological quality.
For each diagnostic category, meta-regression analyses were performed to investigate potential sources of heterogeneity. Continuous independent variables for single factor meta-regression were number of participants, sex distribution (female/all), and final year of diagnostic assessments. Categorial independent factors were diagnostic method (structured/semi-structured interview versus non-structured clinical evaluation), sampling method (randomized versus non-randomized sampling methods), and study location (US, UK, or Germany). The 3 study locations were prespecified as predictor variables due to a preponderance of primary studies in each of these countries.
Multivariable meta-regression models were also calculated. The respective independent variables were chosen through automated, information-criterion-based model selection with generalized linear models [38]. For models with 20 or more included studies, the Akaike information criterion (AIC) was used; for models with fewer than 20 included studies, we utilized the corrected version for small sample sizes (AICC) to avoid over-fitting.
The proportion of variance of prevalence estimates explained by any meta-regression model was estimated by the R2 statistic [45].
We assumed that missingness was at random [46], so missing values in independent variables (that were missing despite requests for additional information to primary study authors) were replaced through multiple imputation by chained equations [47]. For models including incomplete predictor variables, results of meta-regression on imputed data are presented as the primary analysis; meta-regression results on only complete cases are provided as sensitivity analyses [48].
Results
Description of included studies
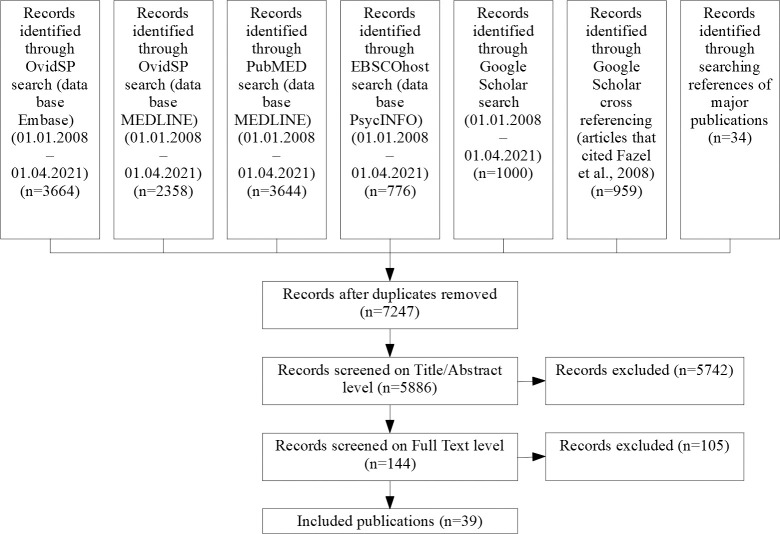
The systematic literature search returned 5,886 distinct records, of which 144 full texts were assessed (see S3 Table for reasons for exclusion). We identified a total of 39 studies comprising data on 8,049 homeless individuals [28,29,49–85] (see Fig 1 for flow chart of screening process). This included 10 additional studies for this update [28,29,53–55,57,59,62,75,76], and 2 previous investigations were further clarified [81,83].
Fig 1. Screening process.
Out of the 39 included studies, 27 publications reported age (mean of 41.1 years) [28,49–57,59,64,65,67,70–73,75,76,78–82,84,85], and the proportion of women was 22.3% (based on 38 studies) [28,29,49–65,67–85]. Eleven studies [52,56,68,71–74,80,82,83,85] investigated male-only samples, and 5 studies [59,65,78,81,84] solely women. Of the 39 studies, 27 were from 3 countries: 11 from the US (n = 2,694 participants) [57,59,60,64,69,75,77,79,83–85], 7 from the UK (n = 1,390 participants) [49,61,66,67,70,78,82], and 9 from Germany (n = 936 participants) [28,50,51,56,65,71–73,80,81]. Six studies were from other European countries (n = 2,301 participants) [29,52,55,58,62,76], 1 study was from Canada (n = 60 participants) [69], 2 were from Japan (n = 194 participants) [53,54], and 2 were from Australia (n = 667 participants) [63,74]. Fourteen studies reported a response rate of 85% or above [49,60,65,66,69–73,78,81,82,84,85], 20 studies reported a response rate below 85% [28,29,50–52,54–56,58,59,61–64,68,74,76,79,80,83], and 5 did not report participation rate [53,57,67,75,77]. In 13 studies, participants were accommodated in shelters, hostels, or residential care when assessed [28,49,63,66,70,72,74,76–78,81–83] while in 3 they were rough sleeping [54,62,67]; 22 studies had mixed samples regarding accommodation or provided incomplete information [29,50–53,55–61,64,65,68,69,71,73,75,79,80,84,85]. S4 Table provides further information on methodological and sample characteristics. For quality ratings, see S5 and S6 Tables. S7 Table provides all extracted data that meta-analyses and meta-regression analyses were based on.
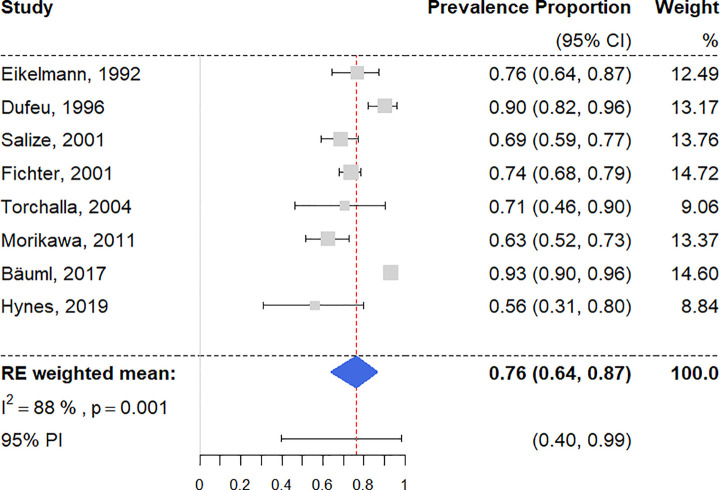
Any current mental disorders
There were 8 surveys reporting on homeless people having at least 1 diagnosis of a current mental disorder [28,51,54,62,71–73,81], with a random effects pooled prevalence estimated at 76.2% (95% CI 64.0% to 86.6%) (Fig 2). Individual study prevalence rates ranged from 56.3% to 93.3%, with substantial heterogeneity (I2 = 88% [95% CI 72% to 97%]). The 95% PI was 40% to 99%. Univariable meta-regression analysis revealed that studies with randomized sampling procedures reported significantly higher prevalence estimates than ones with other sampling procedures, accounting for a large proportion of heterogeneity (R2 = 59%) (see S8 Table). Sampling procedure was chosen as the only predictor variable by multivariable model selection (see Table 1).
Fig 2. Forest plot of prevalence estimates of any current mental disorder.
Analytic weights are from random effects meta-analysis. Grey boxes represent study estimates; their size is proportional to the respective analytical weight. Lines through the boxes represent the 95% CIs around the study estimates. The blue diamond represents the mean estimate and its 95% CI. The vertical red dashed line indicates the mean estimate. CI, confidence interval; PI, prediction interval.
Table 1. Study-level factors associated with between-study heterogeneity in multivariable meta-regression.
| Model | β (standard error) and p-value, by factor | ||||||
|---|---|---|---|---|---|---|---|
| Any current mental disordera,b | Schizophrenia spectrum disorders | Major depression | Bipolar disorder | Alcohol use disordersb | Drug use disorders | Personality disordersa,b | |
| Imputed model | — | With R 2 = 16% | With R 2 = 32% | With R 2 = 54% | — | With R 2 = 42% | — |
| — | Sample size (continuous): >−0.01 (<0.01) p = 0.04 |
Randomized sampling versus other: 0.17 (0.07) p = 0.03 |
Randomized sampling versus other: −0.11 (0.04) p = 0.03 |
— | Randomized sampling versus other: −0.39 (0.12) p < 0.01 |
— | |
| Sex distribution (female/all): 0.13 (0.07) p = 0.09 |
Sex distribution (female/all): 0.14 (0.09) p = 0.15 |
Sex distribution (female/all): 0.15 (0.06) p = 0.04 |
UK versus other locations: −0.48 (0.18) p = 0.01 |
||||
| Germany versus other locations: −0.09 (0.05) p = 0.11 |
|||||||
| Complete case analysis | With R 2 = 59% | With R 2 = 13% | With R 2 = 32% | With R 2 = 50% | With R 2 = 27% | With R 2 = 51% | With R 2 = 15% |
| Randomized sampling versus other: 0.23 (0.08) p = 0.03 |
Sample size (continuous): >−0.01 (<0.01) p = 0.07 |
Randomized sampling versus other: 0.18 (0.08) p = 0.03 |
Randomized sampling versus other: −0.12 (0.04) p = 0.03 |
Germany versus other locations: 0.33 (0.10) p < 0.01 |
Randomized sampling versus other: −0.39 (0.10) p < 0.01 |
North America versus other locations: 0.30 (0.17) p = 0.10 |
|
| Sex distribution (female/all): 0.14 (0.08) p = 0.08 |
Sex distribution (female/all): 0.18 (0.10) p = 0.10 |
Sex distribution (female/all): 0.12 (0.06) p = 0.09 |
North America versus other locations: 0.20 (0.10) p = 0.04 |
UK versus other locations: −0.72 (0.20) p < 0.01 |
|||
| Germany versus other locations: −0.09 (0.05) p = 0.11 |
|||||||
Statistically significant values given in bold.
aA univariable model was chosen in model selection, so only 1 variable is presented.
bAll variables in the multivariable model were complete, so no imputation was needed.
In a subgroup analysis of 4 low-risk-of-bias studies [62,71,73,81], the random effects prevalence was 75.3% (95% CI 50.2% to 93.6%; I2 = 81% [95% CI 32% to 99%]). There was no significant difference between quality subgroups (Q = 0.03, p = 0.87).
Schizophrenia spectrum disorders
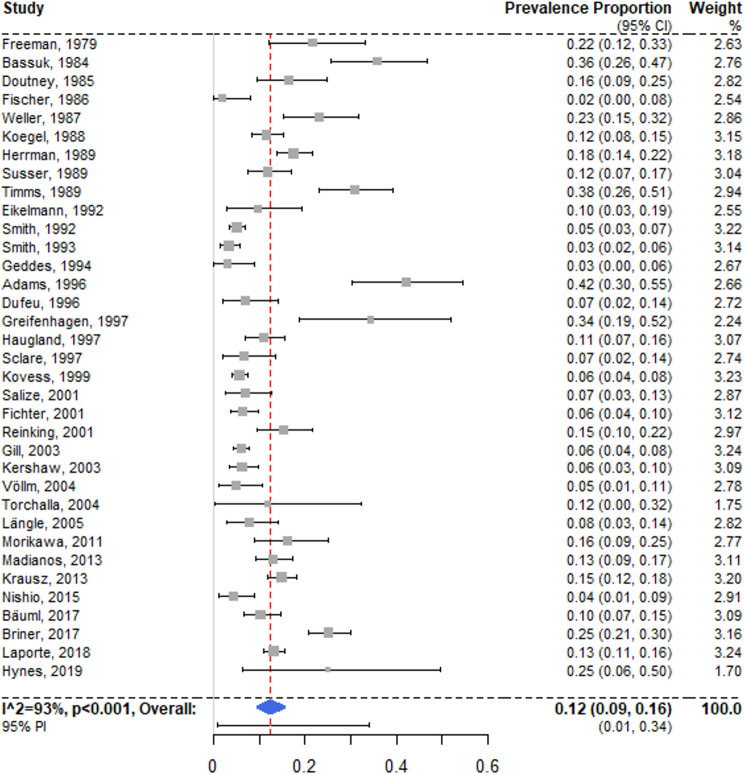
There were 35 surveys reporting on any schizophrenia spectrum disorder [28,29,49,51–58,60–74,76–78,80–85], and the random effects prevalence was 12.4% (95% CI 9.5% to 15.7%) (Fig 3), with substantial heterogeneity (I2 = 93% [95% CI 89% to 96%]; 95% PI 0% to 34%). Primary investigation estimates ranged between 2.0% and 42.2%. No single model coefficient in univariable meta-regression was statistically significant. A multivariable model with sample size, proportion of female participants, and study location in Germany accounted for a small share of the heterogeneity (R2 = 16%). The latter model indicated that studies with smaller samples had significantly higher prevalence rates, but only when based on imputed values (see Table 1).
Fig 3. Forest plot of prevalence estimates of schizophrenia spectrum disorders.
Analytic weights are from random effects meta-analysis. Grey boxes represent study estimates; their size is proportional to the respective analytical weight. Lines through the boxes represent the 95% CIs around the study estimates. The blue diamond represents the mean estimate and its 95% CI. The vertical red dashed line indicates the mean estimate. CI, confidence interval; PI, prediction interval; RE, random effects.
A subgroup analysis of 17 low-risk-of-bias studies [29,49,52,55,58,60,62,65,67,69,71,73,78,80,81,84,85] revealed a random effects pooled prevalence of 10.5% (95% CI 6.2% to 15.7%; I2 = 94% [95% CI 88% to 98%]). The subgroup difference between low-risk-of-bias and moderate-risk-of-bias studies was non-significant, with the low-risk group resulting in a marginally lower weighted mean (Q = 1.59, p = 0.21).
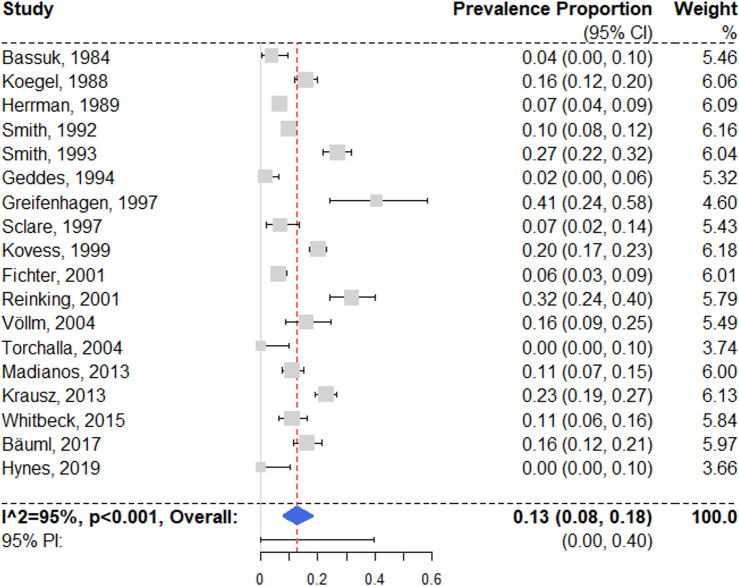
Major depression
We identified 18 studies reporting prevalence estimates on major depressive disorder [28,49,52,55,57–60,62,63,65,67,71,77,80,81,84,85], with a random effects pooled prevalence of 12.6% (95% CI 7.9% to 18.2%) (Fig 4). Individual study estimates ranged between 0% and 40.6% and showed substantial heterogeneity (I2 = 95% [95% CI 90% to 98%]; 95% PI 0% to 40%). Univariable meta-regression analysis produced no significant models (see S8 Table). For multivariable regression, independent variable sampling procedure and proportion of female participants were selected; the model indicated that studies with randomized sampling reported significantly higher prevalence rates (see Table 1).
Fig 4. Forest plot of prevalence estimates of major depression.
Analytic weights are from random effects meta-analysis. Grey boxes represent study estimates; their size is proportional to the respective analytical weight. Lines through the boxes represent the 95% CIs around the study estimates. The blue diamond represents the mean estimate and its 95% CI. The vertical red dashed line indicates the mean estimate. CI, confidence interval; PI, prediction interval; RE, random effects.
In a subgroup analysis of 13 low-risk-of-bias studies [49,52,55,58,60,62,65,67,71,80,81,84,85], the random effects pooled prevalence was 13.0% (95% CI 6.7% to 20.9%; I2 = 96% [95% CI 90% to 99%]). There were no significant differences in between risk of bias subgroups (Q = 0.09, p = 0.76).
Bipolar disorder
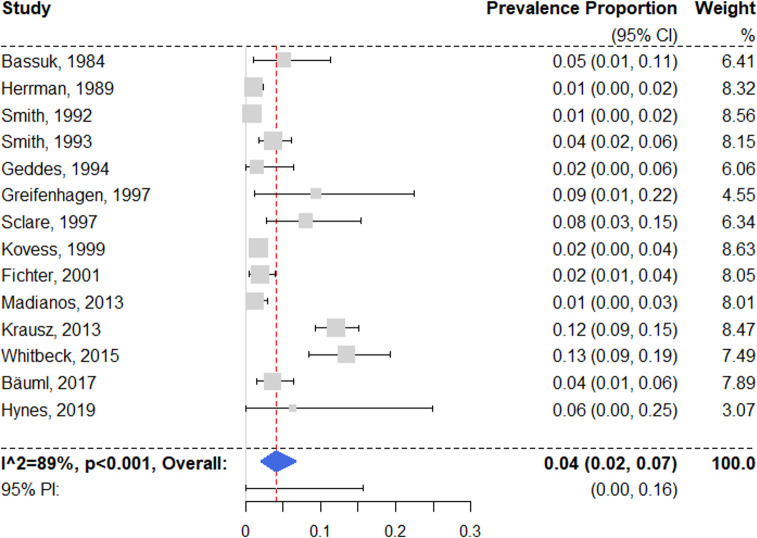
Fourteen surveys with prevalence estimates on bipolar disorder were identified [28,49,55,57–59,62,63,65,67,71,77,84,85]. Three studies reported on solely type I bipolar disorder [49,57,85], 4 examined all bipolar disorder subtypes [28,59,65,71], and 7 did not specify [55,58,62,63,67,77,84]. The random effects pooled prevalence was 4.1% (95% CI 2.0% to 6.7%) (Fig 5), with substantial heterogeneity (I2 = 89% [95% CI 77% to 96%]; 95% PI 0% to 16%). Individual estimates ranged from 1.0% to 13.5%. Univariable regression models indicated that studies with higher proportions of female participants reported significantly higher rates of bipolar disorder (see S8 Table). In the multivariable model, prevalence estimates from studies with randomized sampling were significantly lower than those from studies with other sampling methods (see Table 1).
Fig 5. Forest plot of prevalence estimates of bipolar disorder.
Analytic weights are from random effects meta-analysis. Grey boxes represent study estimates; their size is proportional to the respective analytical weight. Lines through the boxes represent the 95% CIs around the study estimates. The blue diamond represents the mean estimate and its 95% CI. The vertical red dashed line indicates the mean estimate. CI, confidence interval; PI, prediction interval; RE, random effects.
A subgroup analysis of 9 low-risk-of-bias surveys [49,55,58,62,65,67,71,84,85] resulted in a random effects pooled prevalence of 2.6% (95% CI 1.0% to 4.9%), with moderate heterogeneity (I2 = 78% [95% CI 29% to 96%]). The difference between low-risk-of-bias and moderate-risk-of-bias studies was non-significant (Q = 2.29, p = 0.13).
Findings for any affective disorder (which included depression and bipolar disorder) are reported in S1 Text and S6 Table.
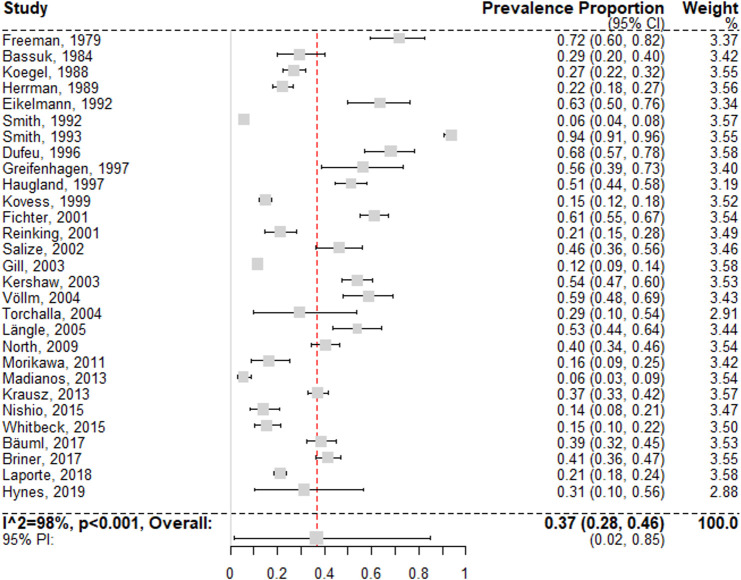
Alcohol use disorders
Estimates on alcohol use disorders could be extracted from 29 surveys [28,29,51–66,68,71–73,76,77,79–81,84,85]. The random effects pooled prevalence was 36.7% (95% CI 27.7% to 46.2%) (Fig 6), with individual study estimates ranging from 5.5% to 71.7%, and with substantial between-study heterogeneity (I2 = 98% [95% CI 97% to 99%]; 95% PI 2% to 85%). Univariable meta-regression models indicated that studies with smaller samples and studies from Germany (compared to other locations) reported significantly higher rates of alcohol use disorders (see S8 Table). In multivariable analysis, the best selected model included only study location as a predictor variable, with higher prevalences reported in Germany and North America (see Table 1).
Fig 6. Forest plot of prevalence estimates of alcohol use disorders.
Analytic weights are from random effects meta-analysis. Grey boxes represent study estimates; their size is proportional to the respective analytical weight. Lines through the boxes represent the 95% CIs around the study estimates. The blue diamond represents the mean estimate and its 95% CI. The vertical red dashed line indicates the mean estimate. CI, confidence interval; PI, prediction interval; RE, random effects.
In a subgroup analysis of 14 low-risk-of-bias studies [29,52,55,58,60,62,65,71,73,79–81,84,85], the random effects pooled prevalence was 36.9% (95% CI 21.1% to 54.3%; I2 = 99% [95% CI 98% to 100%]). There was no significant difference between risk of bias subgroups (Q < 0.01, p = 0.96).
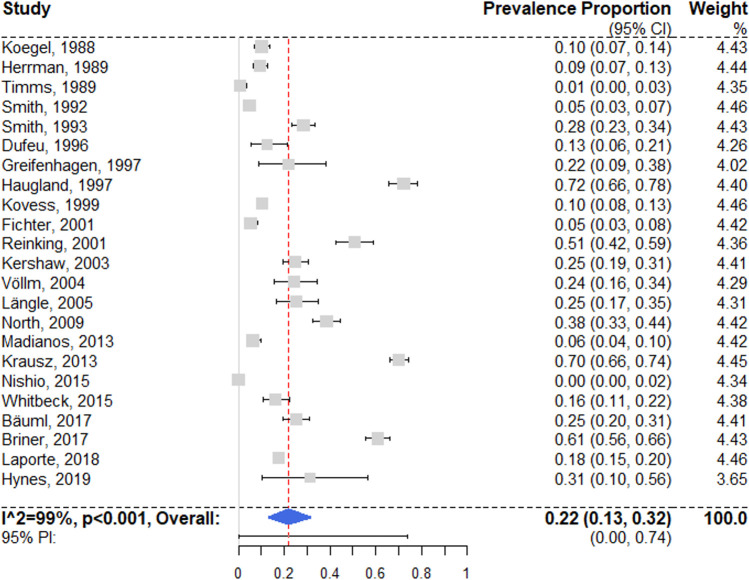
Drug use disorders
We identified 23 surveys reporting prevalence estimates on drug use disorders [28,29,52,53,55–65,71,73,76,79,80,82,84,85] (Fig 7). A random effects pooled prevalence of 21.7% (95% CI 13.1% to 31.7%) was found, with very high heterogeneity (I2 = 99% [95% CI 98% to 99%]; 95% PI 0% to 74%); individual estimates ranged between 0% and 72.1%. According to univariable meta-regression, studies with randomized sampling (as opposed to other sampling methods) estimated significantly lower prevalence rates (see S8 Table). The selected multivariable model showed that studies from the UK reported lower prevalence rates. These results were confirmed by a secondary complete case analysis.
Fig 7. Forest plot of prevalence estimates of drug use disorders.
Analytic weights are from random effects meta-analysis. Grey boxes represent study estimates; their size is proportional to the respective analytical weight. Lines through the boxes represent the 95% CIs around the study estimates. The blue diamond represents the mean estimate and its 95% CI. The vertical red dashed line indicates the mean estimate. CI, confidence interval; PI, prediction interval; RE: random effects.
A subgroup analysis of 13 low-risk-of-bias studies [29,52,55,58,60,62,65,71,73,79,80,84,85] resulted in a random effects pooled prevalence of 18.1% (95% CI 10.5% to 27.2%), with substantial heterogeneity (I2 = 97% [95% CI 94% to 99%]). The difference between subgroups was not significant (Q = 0.65, p = 0.42).
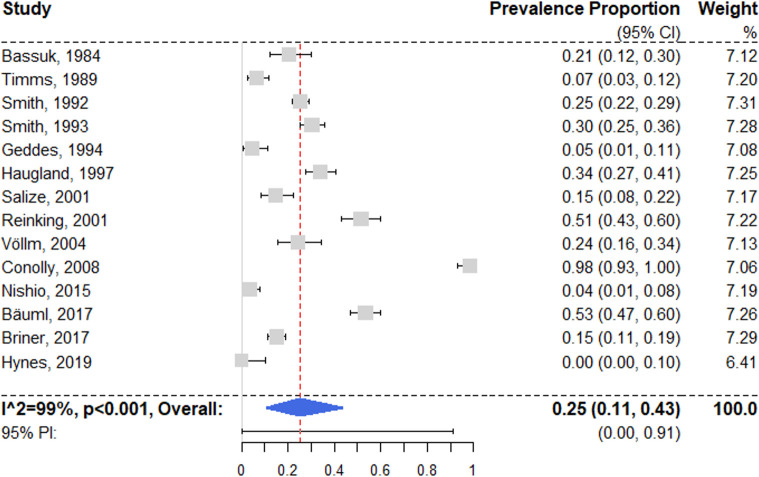
Personality disorders
Fourteen studies reported prevalence estimates on lifetime personality disorders [28,51–53,62,64,67,75–77,80,82,84,85], with a random effects pooled prevalence of 25.4% (95% CI 10.9% to 43.6%) (Fig 8). Individual estimates ranged between 0% and 98.3%, resulting in substantial heterogeneity (I2 = 99% [95% CI 97% to 99%]; 95% PI 0% to 91%). Univariable regression models did not yield significant results (see S8 Table), and neither did the selected multivariable model (see Table 1).
Fig 8. Forest plot of prevalence of personality disorders.
Analytic weights are from random effects meta-analysis. Grey boxes represent study estimates; their size is proportional to the respective analytical weight. Lines through the boxes represent the 95% CIs around the study estimates. The blue diamond represents the mean estimate and its 95% CI. The vertical red dashed line indicates the mean estimate. CI, confidence interval; PI, prediction interval; RE, random effects.
In a subgroup analysis of 6 low-risk-of-bias studies [52,62,67,80,84,85], the random effects pooled prevalence was 21.0% (95% CI 4.7% to 44.5%), with substantial heterogeneity (I2 = 97% [95% CI 92% to 100%]). The difference between subgroups was not significant (Q = 0.32, p = 0.57).
Discussion
This systematic review and meta-analysis of the prevalence of mental illness among homeless people in high-income countries included 39 studies comprising a total of 8,049 participants. We investigated 7 common psychiatric diagnoses, and examined possible explanations for the between-study heterogeneity. We report 3 main findings.
With a pooled prevalence of around 37%, alcohol-related disorders were the most prevalent diagnostic category. This prevalence estimate is around 10-fold greater than general population estimates: An EU study reported a 12-month prevalence of 3.4% in the general population [86]. Correspondingly, drug-related disorders were the second most common current mental disorder, with a pooled prevalence of 22% (which can be compared with the 12-month prevalence in the US general population of 2.5% [87]). We found substantial variation between the individual studies contributing to these estimates, with individual study estimates ranging from 5.5% to 71.7% for alcohol-related disorders; this variation was partially accounted for by study location. Particularly, German-based samples typically had higher prevalence rates of alcohol use disorders than those from other nations. This might highlight geographical differences regarding the affordability and availability of substances, including a comparatively low alcohol tax in Germany [88]. Irrespective of this moderating factor, the strong association between homelessness and substance abuse reflects a bidirectional relationship: Alcohol and drug use represent possible coping strategies in marginalized housing situations. At the same time, substance abuse and other psychiatric disorders precede the onset of homelessness in many people, with alcohol use disorders in particular emerging at an earlier point in life compared to age-matched non-homeless comparisons [89], suggesting that substance use might contribute to the deterioration of an individual’s housing situation. Such deterioration is consistent with the links between substance use disorders and excess mortality in homeless people [11], homelessness chronicity, psychosocial problems [90], and poorer long-term housing stability [91].
A second main finding was that some study characteristics consistently explained the variations in prevalence. In 5 diagnostic groups, methods were important, specifically the number of included participants and the sampling procedure. Unexpectedly, the latter had differential effects by diagnostic group. In bipolar disorder and drug use disorders, randomization was associated with lower prevalence estimates, whereas for any current mental disorder and major depression, it was associated with higher estimates. These findings underline the importance of standardized methodological procedures for homelessness research. We recommend that new research studies should base their inclusion criteria on a standardized definition of homelessness based on ETHOS criteria [92] and use randomized sampling, standardized diagnostic instruments, and trained interviewers with clinical backgrounds (including nurses, psychologists, and medical doctors).
Our third main finding was high prevalence rates for treatable mental illnesses, with 1 in 8 homeless individuals having either major depression (12.6%) or schizophrenia spectrum disorders (12.4%). This represents a high rate of schizophrenia spectrum disorders among homeless people, and a very large excess compared to the 12-month prevalence in the general population, which for schizophrenia is estimated around 0.7% in high-income countries [86]. For major depression, the difference from the general population is not marked, as the 12-month prevalence in the US general population is estimated at 10% [93], although comparisons would need to account for the differences in age and sex structure between the samples contributing to this review and the general population. Depression remains important because it is modifiable, and because of its effects on adverse outcomes. In addition, a recent cohort study based in Vancouver, Canada, found that substance use disorders were associated with worsening of psychosis in homeless people, underscoring the links between these mental disorders, and the importance of treatment in mitigating their effects directly and indirectly [13]. This study also found elevated risks of mortality in those with psychosis and alcohol use disorders [13].
Overall, our findings underscore the importance of mental health problems among homeless individuals. This review is complemented by other research on the often precarious financial and housing situation of psychiatric patients, for whom high rates of homelessness, indebtedness, and lack of bank account ownership have been reported [94–97]. Being homeless and having mental disorders are therefore closely interrelated. Fragmented and siloed services will therefore be typically unable to address these linked psychosocial and health problems. The mental disorders reported in this study are typically associated with unmet needs in the homeless population [51,98–100], which further indicates the need for integrated approaches. Many different initiatives to address these needs have been researched over the last decade, among them Housing First, Intensive Case Management, Assertive Community Treatment, and Critical Time Intervention. Randomized controlled studies using these approaches have generally resulted in positive effects on housing stability, but only moderate or no effects on most indicators of mental health in comparison to usual care, including for substance use [101–104]. Therefore, further improvements in management and treatment are necessary that focus on these common mental disorders.
The COVID-19 pandemic has put homeless people at particular risk of infection and further marginalization [105]. But it has shown what is possible—government agencies and charity organizations managed to quickly provide accommodation to a large number of rough-sleeping homeless people in some European regions [106,107].
Some limitations to this review need to be considered. We searched a limited number of databases, so it is possible that we missed certain primary reports, although this possibility was minimized by searching through reference lists and Google Scholar citations. Furthermore, despite the high rate of multimorbidity in homeless populations [108,109], included studies lacked information on comorbidity. With most of the primary studies reporting prevalence rates of more than 1 of the investigated diagnostic categories, effects from the same sample were in many cases entered into multiple meta-analytical models. This may have led to measurement error and overestimation if diagnostic criteria overlap, but without diagnostic validity studies specific to homeless persons, this remains uncertain. We limited the number of demographic variables that we conducted heterogeneity analyses on, because of variations in measurement and reporting detail. Future work, including individual participant meta-analysis, could standardize information on age, socioeconomic background, and ethnicity, for example.
The present review focuses on high-income countries because sample and diagnostic heterogeneity would presumably increase if a wider range of countries was included. It is important to note, however, that homeless populations in low- and middle-income countries need investigation, and may have higher rates of trauma-related symptoms [110,111]. The prevalence of the mental disorders reported in the current review does not consider unmet healthcare needs or treatment provision, which are additional elements to consider in developing services. Finally, several subpopulations were underrepresented: migrants and refugees (individuals who did not speak the local language were excluded from some study samples), the “hidden homeless” population (e.g., “couch-surfers”) [112] (sampling procedures were often not able to identify this group), and, importantly, homeless women. Twenty-two percent of participants in the included studies were female, lower than most estimates of the proportion of women among homeless populations, which range between 25% and 40% [4,113].
In summary, we found high prevalence of mental disorders among homeless people in high-income countries, with around three-quarters having any mental disorder and a third having alcohol use disorders. Future research should focus on integrated service models addressing the identified needs of substance use disorders, schizophrenia spectrum disorders, and depression in homeless individuals as a priority. In addition, new work could consider focusing on underrepresented subpopulations like homeless women and migrants. Furthermore, longitudinal studies could examine mechanisms linking homelessness and mental disorders in order to develop more effective preventive measures.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Results of meta-analysis and meta-regression analysis.
(DOCX)
Acknowledgments
We are grateful to authors of included and non-included publications who provided additional details about their studies: C. Adams, H.-J. Salize, A. Greifenhagen, C. Vazquez, U. Beijer, C. Siegel, and G. Gilchrist. We are also grateful to the professional translator N. Spennemann for assistance with Japanese studies.
Abbreviations
- CI
confidence interval
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- PI
prediction interval
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The Wellcome Trust (https://wellcome.org) granted the submission fee for this review to SF (grant number 202836/Z/16/Z). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.United Nations Commission for Social Development. Affordable housing and social protection systems for all to address homelessness. Report of the Secretary-General. E/CN.5/2020/3. New York: United Nations Commission for Social Development; 2019Nov27 [cited 2020 May 10]. Available from: https://undocs.org/en/E/CN.5/2020/3. [Google Scholar]
- 2.Directorate of Employment, Labour and Social Affairs. HC3.1 Homeless population. Paris: Organisation for Economic Co-operation and Development; 2020. [cited 2020 May 3]. Available from: https://www.oecd.org/els/family/HC3-1-Homeless-population.pdf. [Google Scholar]
- 3.Tsai J. Lifetime and 1-year prevalence of homelessness in the US population: results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. J Public Health (Oxf). 2018;40(1):65–74. doi: 10.1093/pubmed/fdx034 [DOI] [PubMed] [Google Scholar]
- 4.Henry M, Mahathey A, Morrill T, Robinson A, Shivji A, Watt R. The 2018 Annual Homeless Assessment Report (AHAR) to Congress. Part 1: point-in-time estimates of homelessness. Washington (DC): US Department of Housing and Urban Development; 2018Dec [cited 2020 May 10]. Available from: https://www.huduser.gov/portal/sites/default/files/pdf/2018-AHAR-Part-1.pdf. [Google Scholar]
- 5.Willliams SP, Bryant K. Sexually transmitted infection prevalence among homeless adults in the United States: a systematic literature review. Sex Transm Dis. 2018;45(7):494–504. doi: 10.1097/OLQ.0000000000000780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Topolovec-Vranic J, Ennis N, Colantonio A, Cusimano MD, Hwang SW, Kontos P, et al. Traumatic brain injury among people who are homeless: a systematic review. BMC Public Health. 2012;12(1):1059. doi: 10.1186/1471-2458-12-1059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nusselder WJ, Slockers MT, Krol L, Slockers CT, Looman CWN, van Beeck EF. Mortality and life expectancy in homeless men and women in Rotterdam: 2001–2010. PLoS ONE. 2013;8(10):e73979. doi: 10.1371/journal.pone.0073979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fazel S, Geddes JR, Kushel M. The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. 2014;384(9953):1529–40. doi: 10.1016/S0140-6736(14)61132-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bernstein RS, Meurer LN, Plumb EJ, Jackson JL. Diabetes and hypertension prevalence in homeless adults in the United States: a systematic review and meta-analysis. Am J Public Health. 2014;105(2):46–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beijer U, Wolf A, Fazel S. Prevalence of tuberculosis, hepatitis C virus, and HIV in homeless people: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(11):859–70. doi: 10.1016/S1473-3099(12)70177-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baggett TP, Hwang SW, O’Connell JJ, Porneala BC, Stringfellow EJ, Orav EJ, et al. Mortality among homeless adults in Boston: shifts in causes of death over a 15-year period. JAMA Intern Med. 2013;173(3):189–95. doi: 10.1001/jamainternmed.2013.1604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aldridge RW, Story A, Hwang SW, Nordentoft M, Luchenski SA, Hartwell G, et al. Morbidity and mortality in homeless individuals, prisoners, sex workers, and individuals with substance use disorders in high-income countries: a systematic review and meta-analysis. Lancet. 2018;391(10117):241–50. doi: 10.1016/S0140-6736(17)31869-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jones AA, Gicas KM, Seyedin S, Willi TS, Leonova O, Vila-Rodriguez F, et al. Associations of substance use, psychosis, and mortality among people living in precarious housing or homelessness: a longitudinal, community-based study in Vancouver, Canada. PLoS Med. 2020;17(7):e1003172. doi: 10.1371/journal.pmed.1003172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nielsen SF, Hjorthøj CR, Erlangsen A, Nordentoft M. Psychiatric disorders and mortality among people in homeless shelters in Denmark: a nationwide register-based cohort study. Lancet. 2011;377(9784):2205–14. doi: 10.1016/S0140-6736(11)60747-2 [DOI] [PubMed] [Google Scholar]
- 15.Perron BE, Alexander-Eitzman B, Gillespie DF, Pollio D. Modeling the mental health effects of victimization among homeless persons. Soc Sci Med. 2008;67(9):1475–9. doi: 10.1016/j.socscimed.2008.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roy L, Crocker AG, Nicholls TL, Latimer EA, Ayllon AR. Criminal behavior and victimization among homeless individuals with severe mental illness: a systematic review. Psychiatr Serv. 2014;65(6):739–50. doi: 10.1176/appi.ps.201200515 [DOI] [PubMed] [Google Scholar]
- 17.Caton CLM, Dominguez B, Schanzer B, Hasin DS, Shrout PE, Felix A, et al. Risk factors for long-term homelessness: findings from a longitudinal study of first-time homeless single adults. Am J Public Health. 2005;95(10):1753–9. doi: 10.2105/AJPH.2005.063321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patterson ML, Somers JM, Moniruzzaman A. Prolonged and persistent homelessness: multivariable analyses in a cohort experiencing current homelessness and mental illness in Vancouver, British Columbia. Ment Health Subst Use. 2012;5(2):85–101. [Google Scholar]
- 19.Skosireva A, O’Campo P, Zerger S, Chambers C, Gapka S, Stergiopoulos V. Different faces of discrimination: perceived discrimination among homeless adults with mental illness in healthcare settings. BMC Health Serv Res. 2014;14(1):376. doi: 10.1186/1472-6963-14-376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hossain MM, Sultana A, Tasnim S, Fan Q, Ma P, McKyer ELJ, et al. Prevalence of mental disorders among people who are homeless: an umbrella review. Int J Soc Psychiatry. 2020;66(6):528–41. doi: 10.1177/0020764020924689 [DOI] [PubMed] [Google Scholar]
- 21.Ayano G, Tesfaw G, Shumet S. The prevalence of schizophrenia and other psychotic disorders among homeless people: a systematic review and meta-analysis. BMC Psychiatry. 2019;19(1):370. doi: 10.1186/s12888-019-2361-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ayano G, Tsegay L, Abraha M, Yohannes K. Suicidal ideation and attempt among homeless people: a systematic review and meta-analysis. Psychiatr Q. 2019;90(4):829–42. doi: 10.1007/s11126-019-09667-8 [DOI] [PubMed] [Google Scholar]
- 23.Depp CA, Vella L, Orff HJ, Twamley EW. A quantitative review of cognitive functioning in homeless adults. J Nerv Ment Dis. 2015;203(2):126–31. doi: 10.1097/NMD.0000000000000248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Embleton L, Mwangi A, Vreeman R, Ayuku D, Braitstein P. The epidemiology of substance use among street children in resource‐constrained settings: a systematic review and meta‐analysis. Addiction. 2013;108(10):1722–33. doi: 10.1111/add.12252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bassuk EL, Richard MK, Tsertsvadze A. The prevalence of mental illness in homeless children: a systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2015;54(2):86–96. doi: 10.1016/j.jaac.2014.11.008 [DOI] [PubMed] [Google Scholar]
- 26.Schreiter S, Bermpohl F, Krausz M, Leucht S, Rössler W, Schouler-Ocak M, et al. The prevalence of mental illness in homeless people in Germany. Dtsch Arztebl Int. 2017;114(40):665–72. doi: 10.3238/arztebl.2017.0665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5(12):e225. doi: 10.1371/journal.pmed.0050225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bäuml J, Brönner M, Baur B, Pitschel-Walz GG, Jahn T, Bäuml J. Die SEEWOLF-Studie: seelische Erkrankungsrate in den Einrichtungen der Wohnungslosenhilfe im Großraum München. Archiv für Wissenschaft und Praxis der sozialen Arbeit. Freiburg im Breisgau: Lambertus-Verlag; 2017. [Google Scholar]
- 29.Laporte A, Vandentorren S, Detrez M-A, Douay C, Le Strat Y, Le Mener E, et al. Prevalence of mental disorders and addictions among homeless people in the greater Paris area, France. Int J Environ Res Public Health. 2018;15(2):241. doi: 10.3390/ijerph15020241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Williams JBW. The multiaxial system of DSM-III: where did it come from and where should it go?: II. Empirical studies, innovations, and recommendations. Arch Gen Psychiatry. 1985;42(2):181–6. doi: 10.1001/archpsyc.1985.01790250075010 [DOI] [PubMed] [Google Scholar]
- 31.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008–12. doi: 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 32.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Bank. World Bank country and lending groups. Washington (DC): World Bank; 2020. [cited 2020 Sep 11]. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. [Google Scholar]
- 34.JBI. Critical appraisal tools. Adelaide: University of Adelaide; 2021 [cited 2021 Aug 12]. Available from: https://jbi.global/critical-appraisal-tools.
- 35.Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–9. doi: 10.1016/j.jclinepi.2011.11.014 [DOI] [PubMed] [Google Scholar]
- 36.Bates D, Chambers J, Dalgaard P, Gentleman R, Hornik K, Ihaka R, et al. R-4.0.4. Comprehensive R Archive Network; 2021. [cited 2021 Apr 21]. Available from: https://cran.r-project.org/. [Google Scholar]
- 37.Van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011Dec12. doi: 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- 38.Calcagno V, de Mazancourt C. glmulti: an R package for easy automated model selection with (generalized) linear models. J Stat Softw. 2010May31. doi: 10.18637/jss.v034.i12 [DOI] [Google Scholar]
- 39.Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010Aug5. doi: 10.18637/jss.v036.i03 [DOI] [Google Scholar]
- 40.Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Community Health. 2013;67(11):974–8. doi: 10.1136/jech-2013-203104 [DOI] [PubMed] [Google Scholar]
- 41.Veroniki AA, Jackson D, Viechtbauer W, Bender R, Bowden J, Knapp G, et al. Methods to estimate the between-study variance and its uncertainty in meta-analysis. Res Synth Methods. 2016;7(1):55–79. doi: 10.1002/jrsm.1164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Riley RD, Higgins JPT, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011;342:964–7. doi: 10.1136/bmj.d549 [DOI] [PubMed] [Google Scholar]
- 43.Viechtbauer W. Package ‘metafor.’ Version 2.4–0. Comprehensive R Archive Network; 2020 [cited 2021 Apr 21]. Available from: https://cran.r-project.org/web/packages/metafor/metafor.pdf.
- 44.Higgins JPT, Thompson SG, Spiegelhalter DJ. A re-evaluation of random-effects meta-analysis. J R Stat Soc Ser A Stat Soc. 2009;172(1):137–59. doi: 10.1111/j.1467-985X.2008.00552.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Anderson-Sprecher R. Model comparisons and R^2. Am Stat. 1994;48(2):113–7. [Google Scholar]
- 46.Little RJ, D’Agostino R, Cohen ML, Dickersin K, Emerson SS, Farrar JT, et al. The prevention and treatment of missing data in clinical trials. N Engl J Med. 2012;367(14):1355–60. doi: 10.1056/NEJMsr1203730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res. 2011;20(1):40–9. doi: 10.1002/mpr.329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jakobsen JC, Gluud C, Wetterslev J, Winkel P. When and how should multiple imputation be used for handling missing data in randomised clinical trials—a practical guide with flowcharts. BMC Med Res Methodol. 2017;17(1):162. doi: 10.1186/s12874-017-0442-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sclare PD. Psychiatric disorder among the homeless in Aberdeen. Scott Med J. 1997;42(6):173–7. doi: 10.1177/003693309704200605 [DOI] [PubMed] [Google Scholar]
- 50.Salize HJ, Dillmann-Lange C, Stern G, Kentner-Figura B, Stamm K, Rossler W, et al. Alcoholism and somatic comorbidity among homeless people in Mannheim, Germany. Addiction. 2002;97(12):1593–600. doi: 10.1046/j.1360-0443.2002.00235.x [DOI] [PubMed] [Google Scholar]
- 51.Salize HJ, Horst A, Dillmann-Lange C, Killmann U, Stern G, Wolf I, et al. Needs for mental health care and service provision in single homeless people. Soc Psychiatry Psychiatr Epidemiol. 2001;36(4):207–16. doi: 10.1007/s001270170065 [DOI] [PubMed] [Google Scholar]
- 52.Reinking DP, Wolf JR, Kroon H. Hoge prevalentie van psychische stoornissen en verslavingsproblemen bij daklozen in de stad Utrecht. Ned Tijdschr Geneeskd. 2001;145(24):1161–6. [PubMed] [Google Scholar]
- 53.Nishio A, Yamamoto M, Horita R, Sado T, Ueki H, Watanabe T, et al. Prevalence of mental illness, cognitive disability, and their overlap among the homeless in Nagoya, Japan. PLoS ONE. 2015;10(9):e0138052. doi: 10.1371/journal.pone.0138052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Morikawa S, Uehara R, Okuda K, Shimizu H, Nakamura Y. [Prevalence of psychiatric disorders among homeless people in one area of Tokyo.] Nihon Koshu Eisei Zasshi. 2011;58(5):331–9. [PubMed] [Google Scholar]
- 55.Madianos MG, Chondraki P, Papadimitriou GN. Prevalence of psychiatric disorders among homeless people in Athens area: a cross-sectional study. Soc Psychiatry Psychiatr Epidemiol. 2013;48(8):1225–34. doi: 10.1007/s00127-013-0674-2 [DOI] [PubMed] [Google Scholar]
- 56.Längle G, Egerter B, Albrecht F, Petrasch M, Buchkremer G. Prevalence of mental illness among homeless men in the community. Soc Psychiatry Psychiatr Epidemiol. 2005;40(5):382–90. doi: 10.1007/s00127-005-0902-5 [DOI] [PubMed] [Google Scholar]
- 57.Krausz RM, Clarkson AF, Strehlau V, Torchalla I, Li K, Schuetz CG. Mental disorder, service use, and barriers to care among 500 homeless people in 3 different urban settings. Soc Psychiatry Psychiatr Epidemiol. 2013;48(8):1235–43. doi: 10.1007/s00127-012-0649-8 [DOI] [PubMed] [Google Scholar]
- 58.Kovess V, Mangin Lazarus C. The prevalence of psychiatric disorders and use of care by homeless people in Paris. Soc Psychiatry Psychiatr Epidemiol. 1999;34(11):580–7. doi: 10.1007/s001270050178 [DOI] [PubMed] [Google Scholar]
- 59.Whitbeck LB, Armenta BE, Welch-Lazoritz ML. Borderline personality disorder and Axis I psychiatric and substance use disorders among women experiencing homelessness in three US cities. Soc Psychiatry Psychiatr Epidemiol. 2015;50(8):1285–91. doi: 10.1007/s00127-015-1026-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Koegel P, Burnam MA, Farr RK. The prevalence of specific psychiatric disorders among homeless individuals in the inner city of Los Angeles. Arch Gen Psychiatry. 1988;45(12):1085–92. doi: 10.1001/archpsyc.1988.01800360033005 [DOI] [PubMed] [Google Scholar]
- 61.Kershaw A, Singleton N, Meltzer H. Survey of the health and well-being of homeless people in Glasgow. Int Rev Psychiatry. 2003;15(1–2):141–3. doi: 10.1080/0954026021000046065 [DOI] [PubMed] [Google Scholar]
- 62.Hynes F, Kilbride K, Fenton J. A survey of mental disorder in the long-term, rough sleeping, homeless population of inner Dublin. Ir J Psychol Med. 2019;36(1):19–22. doi: 10.1017/ipm.2018.23 [DOI] [PubMed] [Google Scholar]
- 63.Herrman H, McGorry P, Bennett P, van Riel R, Singh B. Prevalence of severe mental disorders in disaffiliated and homeless people in inner Melbourne. Am J Psychiatry. 1989;146(9):1179–84. doi: 10.1176/ajp.146.9.1179 [DOI] [PubMed] [Google Scholar]
- 64.Haugland G, Siegel C, Hopper K, Alexander MJ. Mental illness among homeless individuals in a suburban county. Psychiatr Serv. 1997;48(4):504–9. doi: 10.1176/ps.48.4.504 [DOI] [PubMed] [Google Scholar]
- 65.Greifenhagen A, Fichter M. Mental illness in homeless women: an epidemiological study in Munich, Germany. Eur Arch Psychiatry Clin Neurosci. 1997;247(3):162–72. doi: 10.1007/BF03033070 [DOI] [PubMed] [Google Scholar]
- 66.Gill B, Meltzer H, Hinds K. The prevalence of psychiatric morbidity among homeless adults. Int Rev Psychiatry. 2003;15(1–2):134–40. doi: 10.1080/0954026021000046056 [DOI] [PubMed] [Google Scholar]
- 67.Geddes J, Newton R, Young G, Bailey S, Freeman C, Priest R. Comparison of prevalence of schizophrenia among residents of hostels for homeless people in 1966 and 1992. BMJ. 1994;308(6932):816–9. doi: 10.1136/bmj.308.6932.816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Freeman SJ, Formo A, Alampur AG, Sommers AF. Psychiatric disorder in a skid-row mission population. Compr Psychiatry. 1979;20(5):454–62. doi: 10.1016/0010-440x(79)90031-2 [DOI] [PubMed] [Google Scholar]
- 69.Fischer PJ, Shapiro S, Breakey WR, Anthony JC, Kramer M. Mental health and social characteristics of the homeless: a survey of mission users. Am J Public Health. 1986;76(5):519–24. doi: 10.2105/ajph.76.5.519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Weller BG, Weller MP, Coker E, Mahomed S. Crisis at Christmas 1986. Lancet. 1987;1(8532):553–4. doi: 10.1016/s0140-6736(87)90187-5 [DOI] [PubMed] [Google Scholar]
- 71.Fichter MM, Quadflieg N. Prevalence of mental illness in homeless men in Munich, Germany: results from a representative sample. Acta Psychiatr Scand. 2001;103(2):94–104. doi: 10.1034/j.1600-0447.2001.00217.x [DOI] [PubMed] [Google Scholar]
- 72.Eikelmann B, Inhester ML, Reker T. Psychische Störungen bei nichtsesshaften Männern. Defizite in der psychiatrischen Versorgung. Sozialpsychiatr Informationen. 1992;29–32. [Google Scholar]
- 73.Dufeu P, Podschus J, Schmidt LG. Alkoholabhängigkeit bei männlichen Wohnungslosen. Häufigkeit, Ausprägung und Determinanten. Nervenarzt. 1996;67(11):930–4. [DOI] [PubMed] [Google Scholar]
- 74.Doutney CP, Buhrich N, Virgona A, Cohen A, Daniels P. The prevalence of schizophrenia in a refuge for homeless men. Aust N Z J Psychiatry. 1985;19(3):233–8. doi: 10.3109/00048678509158828 [DOI] [PubMed] [Google Scholar]
- 75.Conolly AJ, Cobb-Richardson P, Ball SA. Personality disorders in homeless drop-in centre clients. J Pers Disord. 2008;22(6):573–88. doi: 10.1521/pedi.2008.22.6.573 [DOI] [PubMed] [Google Scholar]
- 76.Briner D, Jäger M, Kawohl W, Baumgartner-Nietlisbach G. Mental disorder and self-rated health among homeless people in Zurich: first epidemiological data from Switzerland. Psychiatr Prax. 2017;44(6):339–47. doi: 10.1055/s-0042-111742 [DOI] [PubMed] [Google Scholar]
- 77.Bassuk EL, Rubin L, Lauriat A. Is homelessness a mental health problem? Am J Psychiatry. 1984;141(12):1546–50. doi: 10.1176/ajp.141.12.1546 [DOI] [PubMed] [Google Scholar]
- 78.Adams CE, Pantelis C, Duke PJ, Barnes TRE. Psychopathology, social and cognitive functioning in a hostel for homeless women. Br J Psychiatry. 1996;168(1):82–6. doi: 10.1192/bjp.168.1.82 [DOI] [PubMed] [Google Scholar]
- 79.North CS, Eyrich-Garg KM, Pollio DE, Thirthalli J. A prospective study of substance use and housing stability in a homeless population. Soc Psychiatry Psychiatr Epidemiol. 2009;45(11):1055–62. doi: 10.1007/s00127-009-0144-z [DOI] [PubMed] [Google Scholar]
- 80.Völlm B, Becker H, Kunstmann W. Psychiatrische Morbidität bei allein stehenden wohnungslosen Männern. Psychiatr Prax. 2004;31(5):236–40. doi: 10.1055/s-2003-815014 [DOI] [PubMed] [Google Scholar]
- 81.Torchalla I, Albrecht F, Buchkremer G, Längle G. Wohnungslose Frauen mit psychischer Erkrankung—eine Feldstudie. Psychiatr Prax. 2004;31(05):228–35. [DOI] [PubMed] [Google Scholar]
- 82.Timms PW, Fry AH. Homelessness and mental illness. Health Trends. 1989;21(3):70–1. [PubMed] [Google Scholar]
- 83.Susser E, Struening EL, Conover S. Psychiatric problems in homeless men. Lifetime psychosis, substance use, and current distress in new arrivals at New York City shelters. Arch Gen Psychiatry. 1989;46(9):845–50. doi: 10.1001/archpsyc.1989.01810090087012 [DOI] [PubMed] [Google Scholar]
- 84.Smith EM, North CS, Spitznagel EL. Alcohol, drugs, and psychiatric comorbidity among homeless women: an epidemiologic study. J Clin Psychiatry. 1993;54(3):82–7. [PubMed] [Google Scholar]
- 85.Smith EM, North CS, Spitznagel EL. A systematic study of mental illness, substance abuse, and treatment in 600 homeless men. Ann Clin Psychiatry. 1992;4(2):111–20. [Google Scholar]
- 86.Wittchen H-U, Jacobi F. Size and burden of mental disorders in Europe—a critical review and appraisal of 27 studies. Eur Neuropsychopharmacol. 2005;15(4):357–76. doi: 10.1016/j.euroneuro.2005.04.012 [DOI] [PubMed] [Google Scholar]
- 87.Merikangas KR, McClair VL. Epidemiology of substance use disorders. Hum Genet. 2012;131(6):779–89. doi: 10.1007/s00439-012-1168-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Adams M, Effertz T. Effective prevention against risky underage drinking—the need for higher excise taxes on alcoholic beverages in Germany. Alcohol Alcohol. 2010;45(4):387–94. doi: 10.1093/alcalc/agq031 [DOI] [PubMed] [Google Scholar]
- 89.North CS, Pollio DE, Smith EM, Spitznagel EL. Correlates of early onset and chronicity of homelessness in a large urban homeless population. J Nerv Ment Dis. 1998;186(7):393–400. doi: 10.1097/00005053-199807000-00002 [DOI] [PubMed] [Google Scholar]
- 90.Stein JA, Dixon EL, Nyamathi AM. Effects of psychosocial and situational variables on substance abuse among homeless adults. Psychol Addict Behav. 2008;22(3):410–6. doi: 10.1037/0893-164X.22.3.410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Aubry T, Duhoux A, Klodawsky F, Ecker J, Hay E. A longitudinal study of predictors of housing stability, housing quality, and mental health functioning among single homeless individuals staying in emergency shelters. Am J Community Psychol. 2016;58(1–2):123–35. doi: 10.1002/ajcp.12067 [DOI] [PubMed] [Google Scholar]
- 92.Amore K, Baker M, Howden-Chapman P. The ETHOS definition and classification of homelessness: an analysis. Eur J Homelessness. 2011;5(2):19–37. [Google Scholar]
- 93.Hasin DS, Sarvet AL, Meyers JL, Saha TD, Ruan WJ, Stohl M, et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry. 2018;75(4):336–46. doi: 10.1001/jamapsychiatry.2017.4602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Schreiter S, Bermpohl F, Schouler-Ocak M, Krausz R, Rössler W, Heinz A, et al. Bank account ownership and access among in-patients in psychiatric care in Berlin, Germany—a cross-sectional patient survey. Front Psychiatry. 2020;11:508. doi: 10.3389/fpsyt.2020.00508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Schreiter S, Fritz FD, Rössler W, Majić T, Schouler-Ocak M, Krausz MR, et al. [Housing Situation Among People with Substance Use Disorder in a Psychiatric Centre in Berlin, Germany—A Cross-Sectional Patient Survey.] Psychiatr Prax. 2021;48:156–60. doi: 10.1055/a-1290-5091 [DOI] [PubMed] [Google Scholar]
- 96.Schreiter S, Heidrich S, Heinz A, Rössler W, Krausz RM, Schouler-Ocak M, et al. [Debts, loans and unpaid bills among day patients and inpatients in psychiatric care in Berlin, Germany.] Nervenarzt. 2020Oct14. doi: 10.1007/s00115-020-01013-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Schreiter S, Heidrich S, Zulauf J, Saathoff U, Brückner A, Majic T, et al. Housing situation and healthcare for patients in a psychiatric centre in Berlin, Germany: a cross-sectional patient survey. BMJ Open. 2019;9(12):e032576. doi: 10.1136/bmjopen-2019-032576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Currie LB, Patterson ML, Moniruzzaman A, McCandless LC, Somers JM. Examining the relationship between health-related need and the receipt of care by participants experiencing homelessness and mental illness. BMC Health Serv Res. 2014;14:404. doi: 10.1186/1472-6963-14-404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Desai MM, Rosenheck RA. Unmet need for medical care among homeless adults with serious mental illness. Gen Hosp Psychiatry. 2005;27(6):418–25. doi: 10.1016/j.genhosppsych.2005.06.003 [DOI] [PubMed] [Google Scholar]
- 100.Chondraki P, Madianos MG, Dragioti E, Papadimitriou GN. Homeless mentally ill in Athens area: a cross-sectional study on unmet needs and help-seeking. Int J Soc Psychiatry. 2013;60(6):544–53. doi: 10.1177/0020764013503150 [DOI] [PubMed] [Google Scholar]
- 101.Clarke GN, Herinckx HA, Kinney RF, Paulson RI, Cutler DL, Lewis K, et al. Psychiatric hospitalizations, arrests, emergency room visits, and homelessness of clients with serious and persistent mental illness: findings from a randomized trial of two ACT programs vs. usual care. Ment Health Serv Res. 2000;2(3):155–64. doi: 10.1023/a:1010141826867 [DOI] [PubMed] [Google Scholar]
- 102.Stergiopoulos V, Hwang SW, Gozdzik A, Nisenbaum R, Latimer E, Rabouin D, et al. Effect of scattered-site housing using rent supplements and intensive case management on housing stability among homeless adults with mental illness: a randomized trial. JAMA. 2015;313(9):905–15. doi: 10.1001/jama.2015.1163 [DOI] [PubMed] [Google Scholar]
- 103.Rosenheck R, Kasprow W, Frisman L, Liu-Mares W. Cost-effectiveness of supported housing for homeless persons with mental illness. Arch Gen Psychiatry. 2003;60(9):940–51. doi: 10.1001/archpsyc.60.9.940 [DOI] [PubMed] [Google Scholar]
- 104.Herman D, Opler L, Felix A, Valencia E, Wyatt RJ, Susser E. A critical time intervention with mentally iII homeless men: Impact on psychiatric symptoms. J Nerv Ment Dis. 2000;188(3):135–40. doi: 10.1097/00005053-200003000-00002 [DOI] [PubMed] [Google Scholar]
- 105.Perri M, Dosani N, Hwang SW. COVID-19 and people experiencing homelessness: challenges and mitigation strategies. CMAJ. 2020;192(26):e716–9. doi: 10.1503/cmaj.200834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ministry of Housing, Communities & Local Government, Jenrick R. 6,000 new supported homes as part of landmark commitment to end rough sleeping. London: Ministry of Housing, Communities & Local Government; 2020May24 [cited 2021 Jan 1]. Available from: https://www.gov.uk/government/news/6-000-new-supported-homes-as-part-of-landmark-commitment-to-end-rough-sleeping. [Google Scholar]
- 107.Deutsche Welle. Berlin opens first hostel for the homeless amid coronavirus pandemic. Deutsche Welle. 2020 Mar 31 [cited 2021 Jan 2]. Available from: https://www.dw.com/en/berlin-opens-first-hostel-for-the-homeless-amid-coronavirus-pandemic/a-52972263.
- 108.Bowen M, Marwick S, Marshall T, Saunders K, Burwood S, Yahyouche A, et al. Multimorbidity and emergency department visits by a homeless population: a database study in specialist general practice. Br J Gen Pract. 2019;69(685):e515–25. doi: 10.3399/bjgp19X704609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Raphael R-W, Caroline S, Dan L, Megan A, Briony H. Premature frailty, geriatric conditions and multimorbidity among people experiencing homelessness: a cross-sectional observational study in a London hostel. Housing Care Support. 2020;23(3–4):77–91. [Google Scholar]
- 110.Abdu L, Withers J, Habib AG, Mijinyawa MS, Yusef SM. Disease pattern and social needs of street people in the race course area of Kano, Nigeria. J Health Care Poor Underserved. 2013;24(1):97–105. doi: 10.1353/hpu.2013.0010 [DOI] [PubMed] [Google Scholar]
- 111.Mathebula SD, Ross E. Realizing or relinquishing rights? Homeless youth, their life on the streets and their knowledge and experience of health and social services in Hillbrow, South Africa. Soc Work Health Care. 2013;52(5):449–66. doi: 10.1080/00981389.2012.742483 [DOI] [PubMed] [Google Scholar]
- 112.Agans RP, Jefferson MT, Bowling JM, Zeng D, Yang J, Silverbush M. Enumerating the hidden homeless: Strategies to estimate the homeless gone missing from a point-in-time count. J Off Stat. 2014;30(2):215–29. [Google Scholar]
- 113.Neupert P. Statistikbericht 2017. Berlin: Bundesarbeitsgemeinschaft Wohnungslosenhilfe. 2018. [cited 2020 Jul 18]. Available from: https://www.bagw.de/fileadmin/bagw/media/Doc/STA/STA_Statistikbericht_2017.pdf. [Google Scholar]