Abstract
This study aimed to explore the association between perceived isolation and symptoms of distress in people with GI disorders at the time of the pandemic; and to examine factors which moderate this relationship. This online cross-sectional survey was advertised in May–September 2020 via patient organisations and associated social media. Overall, 831 people (82% female, mean age 49 years) from 27 countries participated. A significant relationship between social isolation and psychological distress was noted (r = .525, p < .001). GI symptoms moderated the association between isolation and distress (B = .047, t = 2.47, p = .015). Interventions targeting these factors may help to reduce distress in people with GI disorders at the time of major stressors such as the COVID-19 pandemic.
Keywords: COVID-19 pandemic, Gastrointestinal disorders, Isolation, Psychological distress
Introduction
Gastrointestinal (GI) disorders are highly prevalent throughout the world, with up to 40% of the adult population reporting symptoms of a gastrointestinal condition (Sperber et al., 2020) In particular, irritable bowel syndrome (IBS) affects at least 5% of the population while close to 1% of western populations experience inflammatory bowel disease (IBD) or coeliac disease (Chaparro et al., 2019; GBD, 2017IBDCollaborators, 2020; Ng et al., 2018; Sperber et al., 2020). GI disorders can be debilitating and costly to treat (Canavan et al., 2014; Park et al., 2020). The disorders are characterized by altered brain-gut communication (Holtmann et al., 2016), with notable vulnerability to anxiety and depression, which, in turn, can aggravate GI symptom frequency and severity (Clappison, Hadjivassiliou, & Zis, 2020; Gracie et al., 2018; N. Koloski et al., 2020; N. A. Koloski et al., 2012; N. A. Koloski et al., 2016).
The coronavirus (COVID-19) pandemic, which to date has resulted in over 4 million deaths worldwide (ECDC, 2021), has proven to be a significant and ongoing stressor, increasing the burden of mental illness. High levels of distress (i.e., stress, anxiety and depression) in the general population, as compared to the pre-pandemic period, have been observed in large studies from China (C. Wang et al., 2020a, 2020b), New Zealand (Sibley et al., 2020) and the United States (Prout et al., 2020), and are proposed to result from fears of contracting the virus, unemployment, increased domestic violence, and prolonged isolation (IASC, 2020).
Mandatory and voluntary self-isolation has been a major feature of the COVID-19 pandemic, with governments around the world implementing temporary lockdowns of varied severity, shutting down businesses, services, schools, and travel, promoting working from home and enforcing physical distancing. While effective in reducing the spread of the virus, prolonged isolation has been linked with poor mental health during the COVID-19 pandemic (Lee et al., 2020; Smith & Lim, 2020; Wong et al., 2020). Distress and sleep problems have also increased during the pandemic (Hossain et al., 2020; S. Wang et al., 2020a, 2020b), with studies demonstrating that pre-existing mental health difficulties likely predispose individuals to increased risk of clinically significant distress during the pandemic (Murphy et al., 2020). However, studies examining self-isolation and mental distress have to date paid limited attention to adults with chronic health problems.
Populations living with chronic GI disorders may be at significant risk of deteriorating mental health during major life challenges such as the present pandemic. While GI disorders have different aetiologies, treatment, and consequently perceived COVID-19 risks, anxiety and depression are generally more prevalent for those with chronic GI disorders compared to healthy controls (Clappison et al., 2020; Mikocka-Walus et al., 2016; Zamani, Alizadeh-Tabari, & Zamani, 2019), thus increasing their vulnerability in the context of a stressor such as the pandemic (Murphy et al., 2020; Rahman et al., 2020). In addition, secondary impacts of the pandemic such as decreased access to routine medical care (Bernstein et al., 2020(in press); Czeisler et al., 2020), and supply chain disruptions of medication (Ann Pulk et al., 2020), certain foods and personal hygiene products (Davis, Jasper, & McCarthy, 2020; Truu, 2020; Wright, 2020) may interfere with everyday life for those with GI disorders, further escalating distress levels. Isolation, subsequent to reduced social support as well as a sense of loneliness, can lead to deterioration in mental health (Kamp et al., 2019). Self-imposed social isolation due to embarrassment and stigma has been documented pre-COVID-19 in GI populations and was associated with poorer mental health outcomes (Fourie et al., 2018). Therefore, COVID-19 pandemic-related isolation could further reduce options for social contact in a population that is already limiting those interactions. On the other hand, the imposed social isolation for the general population related to public health orders during the pandemic (Smith & Lim, 2020) may have reduced distress for those with GI disorders by addressing dilemmas around social invitations through requiring restricted social interactions for all.
While the reviewed literature suggests that the current isolation experienced by people living with GI disorders would affect their overall psychosocial wellbeing, other factors such as the degree to which they may fear the new pathogen, how well they are able to live with these uncomfortable experiences, and how severe their GI symptoms are could influence this relationship. The present study, therefore, aimed to:
1) Explore the association between perceived isolation and symptoms of distress in people with GI disorders in the context of the pandemic; and.
2) Examine factors which may moderate this relationship.
Methods
Design
This cross-sectional study, which collected data from May to September 2020, is part of an ongoing longitudinal study of wellbeing in people with GI disorders during the COVID-19 pandemic (Ferreira et al., 2021).
Setting
The study was undertaken online using the Qualtrics platform. Completion of the survey indicated consent to participation.
Recruitment
The study was advertised internationally via social media and patient organisations (e.g. Coeliac Australia, Crohn’s and Colitis Canada, Crohn’s & Colitis Association Denmark, International Foundation of Functional GI disorders USA, Maag Lever Darm Stichting (MLDS) from the Netherlands).
Inclusion / Exclusion Criteria
In order to be eligible for the study, participants needed to be age 18 and older, diagnosed by a physician with a GI disorder (self-reported), and able to provide informed consent. The questionnaire was provided in English only.
Measures
Demographics
Patient demographics and health characteristics were collected using an investigator-developed questionnaire, which incorporated validated measures where available. To account for socioeconomic status (SES) as a metric of household resource, we combined the reported variables of highest education level attained and pre-tax household income. Educational attainment was given a value from one to ten, ascending from completion of primary/elementary school to completion of a doctoral degree. Annual pre-tax household income was requested from participants in their local currency, and for those who responded (n = 424), ranked one to five according to quintile of household income relative to each geographical region using online data tools (EuroStat, 2021; OECD, 2021). These two values were then summed to create a composite SES metric. We have converted the descriptive statistics into a common metric of USD using the mean conversion rate for each currency in 2020 (OzForex, 2020). Regarding job loss during COVID, participants recorded their employment status (full time, part time, casual, self-employed or unemployed, student, retired, pension) prior to the global emergence of COVID (circa January 2020), and again in the two weeks prior to completing the survey. Participants were then categorised into those who had recorded employed in the former but not the latter as having lost employment during COVID.
Psychological Distress
Distress, collectively including stress, anxiety and depression, was measured on the Depression, Anxiety and Stress Scale (DASS-21). The DASS-21 is a 21-item scale of symptoms of depression, anxiety and stress over the past week, with questions rated on a 4-point Likert scale, ranging from 0 (did not apply to me at all) to 3 (applied to me very much or most of the time). A higher total score indicates higher levels of psychological distress. The DASS-21 has been shown to possess adequate construct validity and reliability to measure the dimensions of depression, anxiety and stress separately and of distress overall (Henry & Crawford, 2005). The DASS total score ranges from 0 to 63 which are doubled for comparison with published norms. Reliability for the overall scale was good; α = 0.95.
Isolation During COVID
COVID isolation was measured utilizing two items created for the present study: Due to COVID-19, how much do you feel you are isolated? Due to COVID-19, how much does isolation affect you emotionally? Two items were created by the research team to assess isolation. While isolation-based scales are available (for overview, see Veazie, Gilbert, and Winchell (2019)), they are not COVID-19 specific and take more time to complete due to their length. Given this, we created two items based upon the style and response formation of the Brief illness Perceptions Questionnaire. These two items assessed the perceived extent and emotional impact of isolation associated with the COVID-19 pandemic. Respondents rated each item on a scale from 0 (no concern) to 10 (extremely concerned) that best corresponds to their views. Higher scores indicate greater sense of isolation. The responses were summed and divided by two. Correlational analysis of the isolation measure suggested good construct validity. We have performed statistical evaluation of the COVID isolation measure used, through simple bivariate correlation analysis. We observed that the two items used to measure isolation significantly correlated with lower quality of life, worse depressive, anxious, and stress symptoms, but were entirely unrelated to living situation. We further identified that the total isolation measure increased the strength of those correlations. Given the strong face validity of the item, and the convergent validity with wellbeing but orthogonality with living situation, we interpret the isolation score as predictive of a construct that measures the psychological aspects of isolation regardless of physical isolation. Living with others: R = -0.011, p = 0.750. Quality of life: R = -0.414, p < 0.001. Depression: R = 0.424, p < 0.001. Anxiety: R = 0.530, p < 0.001. Stress: R = 0.486, p < 0.001.
Experiential Avoidance
Experiential avoidance was measured on the Acceptance and Action Scale (AAQ-II) (Bond et al., 2011). The AAQ-II is a 7-item measure aiming to evaluate attempts to avoid potentially unpleasant internal experiences of thoughts and feelings, even though doing so can create harm in the long-run (S.C. Hayes et al., 1999). An example item is “I worry about not being able to control my thoughts and feelings”. Ratings are from 1 (“Never true”) to 7 (“Always true”), and higher scores correspond to higher levels of experiential avoidance. Scores greater than 24 have been found to correlate with clinically meaningful symptoms of anxiety or depression (S. C. Hayes, 2019). Reliability for the AAQ-II was good in the current sample; α = 0.94.
COVID Fear
COVID fear was measured on the Fear Relating to COVID-19 Scale, adapted from the Fear of AIDS Scale (Arrindell et al., 1989) and recently validated in gastroenterology (Trindade & Ferreira, 2020). This 9-item measure rates level of fear and concern experienced regarding different situations (e.g. contracting COVID; having contact with health professionals). All items are rated on a 5-point scale from 1 (no fear) to 5 (very much fear) with higher scores indicating greater fear about COVID-19. Reliability for COVID fear was good in the current sample; α = 0.93.
GI Symptom Severity
Gastrointestinal symptom severity was measured with the Gastrointestinal Symptom Rating Scale (GSRS), a widely used and reliable tool which can be used across a range of GI conditions (Dimenäs et al., 1995). The measure has 15 items which rate groups of GI symptoms (reflux, constipation, diarrhoea, abdominal pain and indigestion) on the level of discomfort over the past week. The GSRS uses a 7-point Likert-scale, ranging from ‘no discomfort at all’ to ‘very severe discomfort’. The total score ranges from 15 to 105, with higher scores reflecting more severe symptoms. Reliability for the GSRS was good; α = 0.91.
Statistical Analysis
Missing Data and Data Integrity
We examined for missing data with two approaches. First, we performed Littles’ MCAR (missing completely at random) on the included variables and failed to reject the null hypothesis (χ2 (57) = 67.39, p = 0.163. We then performed a visual pattern analysis to examine monotonicity. We concluded that our missing data were likely MCAR, and so missing values were excluded listwise from analyses. Data met assumptions of linearity, independence of errors and fell within acceptable ranges of normal distribution. We failed to reject the null hypothesis for the Kolmogorov–Smirnov test in each model.
Descriptive Statistics
Descriptive statistics were presented as means, standard deviations, medians, ranges, frequencies and percentages, as appropriate.
Correlations
Bivariate correlations were performed for all variables in the model, using Pearson’s r for continuous variables and Spearman’s rho for ordinal variables.
Regression Model
A linear regression model using the packages car (Fox & Weisberg, 2018), and emmeans (Lenth, 2018), in R (Arrindell et al., 1989) and Jamovi (jamovi, 2020) was prepared to explore whether potential moderators of the association between COVID related isolation and distress; experiential avoidance, COVID fear and GI symptoms. COVID isolation, experiential avoidance, COVID Fear, GI symptoms, and sociodemographic variables were entered into the model as main effects. DASS-21 distress was the dependent variable. We also examined simple slopes to compare levels of moderators. Simple effects were examined at one standard deviation above and below the mean values of the moderator.
Results
Overall, 831 respondents from 27 countries participated in the survey. The mean age was 49 years old (SD = 16.1, range 18–94). The majority were female (82%), married (56%), and had a university degree (60%), and the greatest uptake came from the United Kingdom (n = 44%) (Table 1). The most common GI disorders included IBD (n = 322), coeliac disease (n = 273) and IBS (n = 260). Other conditions included: colonic inertia (n = 9), diverticulitis (n = 54), functional dyspepsia (n = 20), gallstones (n = 35), gastroparesis (n = 18), GERD (n = 96), globus (n = 5), haemorrhoids (n = 74), and other (n = 129). Average duration of disease across types was 16.91 years.
Table 1.
Descriptive statistics and frequencies
| N | Missing | Mean | SD | Min | Max | |
|---|---|---|---|---|---|---|
| Age | 793 | 38 | 49.1 | 16.1 | 18 | 94 |
| GSRS | 831 | 0 | 36.2 | 16.6 | 15 | 97 |
| Distress | 831 | 0 | 26.9 | 25.4 | 0 | 126 |
| Experiential Avoidance | 831 | 0 | 19 | 9.85 | 7 | 49 |
| COVID Fear | 831 | 0 | 26.5 | 8.51 | 9 | 45 |
| Isolation | 831 | 0 | 4.73 | 2.79 | 0 | 10 |
| USD Income | 424 | 407 | $75,015 | $84,456 | 0 | $1,103,832 |
| SES | 424 | 407 | 8.45 | 3.47 | 0 | 18 |
| Years with GI | 830 | 0 | 16.91 | 15 | 0 | 92 |
| Gender | Immunomodulating medication | ||||
|---|---|---|---|---|---|
| Levels | Counts | % | Levels | Counts | % |
| Male | 142 | 17.1% | Not currently taking | 766 | 92.2% |
| Female | 684 | 82.3% | Currently taking | 65 | 7.8% |
| Equally / neither / unsure | 3 | 0.4% | |||
| Other (please specify): | 2 | 0.2% | |||
| Highest Education | Income level (in USD) | ||||
|---|---|---|---|---|---|
| Levels | Counts | % | Levels* | Counts | % |
| Elementary school to 8th grade | 7 | 0.8% | 1, < $28,035 | 45 | 10.8% |
| Some high school, no diploma | 39 | 4.7% | 2, < $53,431 | 44 | 10.6% |
| High school degree or equivalent (e.g. GED) | 84 | 10.1% | 3, < $86,402 | 67 | 16.1% |
| Some college credit, no degree | 75 | 9.0% | 4, < $142,400 | 84 | 20.1% |
| Trade/technical/vocational training | 89 | 10.7% | 5, > $142,400 | 177 | 42.5% |
| Associate degree (e.g., AA, AS) | 39 | 4.7% | Employment during COVID | ||
| Bachelor’s degree (e.g., BA, BS, BBA) | 279 | 33.6% | Levels | Counts | % |
| Master’s degree | 150 | 18.1% | Maintained | 785 | 94.5% |
| Professional degree (e.g., MD, JD, DVM) | 36 | 4.3% | Loss | 46 | 5.5% |
| Doctorate degree (e.g., PhD) | 33 | 4.0% | |||
| Living Status | |||||
|---|---|---|---|---|---|
| Levels | Counts | % | |||
| Living alone | 139 | 16.7% | |||
| Living with partner | 512 | 61.6% | |||
| Living with parents | 68 | 8.2% | |||
| Living with friends | 14 | 1.7% | |||
| Other living situation (e.g. share house, dormitory) | 98 | 11.8% |
*Quintiles of household pre-tax annual income in USD
The mean scores overall for distress were within the normal range (≤ 28; M = 26.9, SD = 25.4). To more closely examine those with elevated distress levels, the sum of the maximum cut-off scores for each subscale was used to infer a full scale cut off score of 64 or greater as indicative of severe distress (Lovibond & Lovibond, 1995). A total of 31.5% (n = 262) exceeded this level on the DASS-21. The mean severity of GI symptoms was low (M = 36.2, SD = 16.6). For the GI symptom severity scale (GSRS), 72.9% (n = 606) exceed the maximum cut-off mean response thresholds of 1.53 for males and 1.59 for female participants (Dimenäs et al., 1996). Finally, the mean score for experiential avoidance for the sample overall was also low (M = 19, SD = 9.85). The AAQ2 indicates that scores > 28 are problematic (Bond et al., 2011), which corresponds to approximately one-fifth of the present sample (n = 172, 20.7%).
Aim 1: Explore the Association Between Perceived Isolation and Symptoms of Distress in People with GI Disorders
A moderate-to-strong positive association was observed between isolation and distress (r = 0.525, p < 0.001). Younger age and female gender were significantly associated with lower levels of distress; all other variables were positively associated with distress (Table 2). Several variables were significantly correlated with isolation. Living with others was unrelated to feelings of isolation. Female gender was a significant indicator of lower isolation scores, all other variables were positively correlated. The observed bivariate correlations ranged from trivially small to strong, and despite many statistically significant results most associations were weak. Other than the correlation between isolation and distress, the strongest correlations were positive associations between experiential avoidance and distress (r = 0.734, p < 0.001) and GI symptom severity and distress (r = 0.484, p < 0.001).
Table 2.
Bivariate correlations
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 Distress | – | |||||||||
| 2 SES | −.055 | – | ||||||||
| 3 Age | −.198† | −.166† | – | |||||||
| 4 GSRS | .484† | −.117* | −.133† | – | ||||||
| 5 Experiential Avoidance | .734† | −.117* | −.214† | .358† | – | |||||
| 6 COVID Fear | .307† | −.074 | −.03 | .249† | .263† | – | ||||
| 7 Isolation | .525† | .008 | −.069 | .322† | .441† | .421† | – | |||
| 8 Immunomodulators | −.011 | .001 | −.104** | .008 | .01 | .05 | .011 | – | ||
| 9 Female Gender | −.145† | .021 | .022 | −.108** | −.124† | −.081** | −.167† | -.041 | – | |
| 10 Job loss during COVID | .046 | −.066 | −.016 | .029 | .013 | .1** | .074* | .027 | −.085* | |
| 11 Living with others | .089* | −.024 | −.149† | .139† | .052 | .053 | .02 | −.006 | −.023 | -.01 |
*p < .05, ** p < .01
† p < .001
Aim 2: Examine Factors which May Moderate the Relationship Between Perceived Isolation and Symptoms of Distress
The model accounted for a substantial amount of variance in distress, each explaining around two-thirds of the variance in reported distress (Table 3).
Table 3.
Adjusted moderation model
| ANOVA Omnibus tests | Regression | 95% Confidence Interval | ||||||
|---|---|---|---|---|---|---|---|---|
| F | P | η2p | Estimate | SE | Lower | Upper | β | |
| Model/Intercept | 68.573 | < .001 | .661 | 29.397 | 1.790 | 25.877 | 32.917 | |
| Acceptance | 208.256 | < .001 | .622 | 1.338 | .093 | 1.156 | 1.521 | .538 |
| COVID Isolation | 43.767 | < .001 | .141 | 2.195 | .332 | 1.543 | 2.848 | .245 |
| COVID Fear | .234 | .629 | .002 | .048 | .099 | −0.147 | 0.244 | .016 |
| GSRS | 18.528 | < .001 | .073 | .227 | .053 | 0.123 | 0.331 | .151 |
| Female gender | 1.671 | .197 | .006 | 2.614 | 2.023 | −1.362 | 6.592 | .104 |
| Lost job during COVID | 1.241 | .266 | .002 | 3.467 | 3.113 | −2.652 | 9.587 | .138 |
| SES | 1.038 | .309 | .005 | .304 | .299 | −0.283 | 0.892 | .031 |
| Age | 2.806 | .095 | .004 | −.084 | .05 | −0.182 | 0.014 | -.053 |
| Living with others | .004 | .970 | − | .048 | .711 | −3.071 | .645 | .243 |
| COVID Isolation * Experiential Avoidance | 1.751 | .187 | .022 | .041 | .031 | −0.019 | 0.101 | .046 |
| COVID Isolation * COVID Fear | 1.007 | .316 | .006 | .035 | .035 | −0.033 | 0.102 | .033 |
| COVID Isolation * GSRS | 6.017 | .015 | .015 | .047 | .019 | 0.009 | 0.084 | .088 |
Adj. R2 = .651
p < .001
Sociodemographic-Adjusted Moderation Model of COVID Isolation, Experiential Avoidance, GI Symptoms, COVID Fear, and Distress.
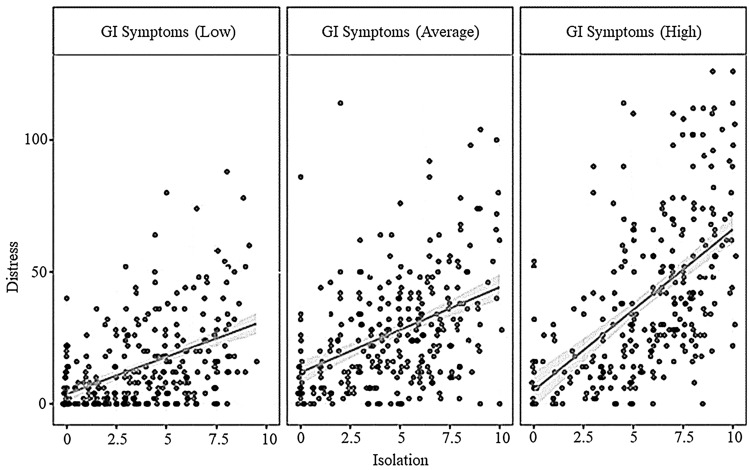
Isolation, experiential avoidance, and GI symptoms were significantly and positively associated with distress (p < 0.001, Table 3), while COVID Fear and each of the sociodemographic covariates were non-significant. We identified a small but robust moderation effect between isolation and GI symptoms, whereby increasing values on either of these independent variables strengthened the association with distress. Analysis of the simple slopes provides the regression coefficients for isolation predicting distress when experiential avoidance is at different levels around the mean. We observed that the association between isolation and distress was significantly positive, but the steepness of the slope increased as reported severity of GI symptoms increased. That is, those reporting higher severity of GI symptoms and higher isolation reported higher levels of distress. For example, when participants reported GI symptom severity at above-average levels, the regression coefficient between COVID isolation and distress was B = 2.98, SE = 0.448, t = 6.65, p < 0.001. See Fig. 1.
Fig. 1.
Moderation effect between isolation, G1 symptoms and distress. Note: G1 symptoms high, low and average panels reflect ranges < 1 standard deviation above and below the mean, and the mean
Discussion
This is the first study to explore the associations between perceived isolation and distress in people with GI disorders during the COVID-19 pandemic, examining potential factors which moderated this relationship.
Isolation was clearly associated with elevated distress for those with GI disorders in the context of the pandemic. This finding is not surprising, as social isolation can be highly correlated with loneliness and both are predictors of poorer physical and mental outcomes as well as all-cause mortality in chronic illness (Hodgson et al., 2020; Leigh-Hunt et al., 2017; Valtorta et al., 2016). However, since many with GI disorders may be particularly prone to curtail social interactions due to embarrassment around their symptoms, it is important to understand the pandemic impact for individuals with these types of chronic conditions. The COVID-19 pandemic has increased social isolation due to the community efforts to reduce spread of the virus by such measures as limiting physical proximity and closing venues often used for social connection such as sports facilities, schools, and work offices. Studies conducted early in the COVID-19 pandemic found an association between an increase in loneliness and decrease in mental health among the general population (Lee et al., 2020; Smith & Lim, 2020; Wong et al., 2020), and our study affirmed that distress was strongly associated with pandemic-related isolation for those with chronic GI disorders. Consideration of activities or mechanisms to mitigate the isolation whether during events such as the pandemic or at other times, may be warranted. The present evidence is low for the efficacy of digital technology interventions (Shah et al., 2021) such as video calls for prolonged isolation (Noone et al., 2020). More promising in tackling social isolation and loneliness are interventions featuring physical activity (Shvedko et al., 2018), meditation (Saini et al., 2021), cognitive modification and supported socialisation (Ma et al., 2020), albeit more high quality trials are needed.
Experiential avoidance, the inability to remain in contact with difficult internal experiences and modulate behaviour per one’s values, is commonly associated with poorer mental health outcomes (Kashdan & Rottenberg, 2010). In the present analysis, experiential avoidance and distress were strongly correlated even in the absence of the isolation variable, suggesting some overlap of these two psychological states (with moderate multicollinearity noted). In particular, the items used to measure experiential avoidance refer to psychological vulnerability and susceptibility to mood changes. In the fully adjusted moderation model, we observed that experiential avoidance was the strongest predictor of distress even when sociodemographic covariates were included, and we observed no moderation effect between experiential avoidance and isolation. This lack of a moderation effect indicates that while feelings of isolation contribute to distress above and beyond that of experiential avoidance, the effect did not exacerbate distress in the sample. These results contrast those of recent studies where experiential avoidance was identified as significant moderator of the relationship between psychological experiences (e.g. health anxiety, pandemic adversity) and indicators of mental health concerns (e.g. depression, anxiety, traumatic stress) (Kroska et al., 2020; Landi et al., 2020; Pakenham et al., 2020). One potential explanation for the lack of a moderation effect between experiential avoidance and isolation is that the elevated levels of self-imposed social isolation in GI populations pre-COVID-19 (Fourie et al., 2018) may have mitigated the potential additive impact of pandemic isolation otherwise present in the community. Further, changes such as consistent access to bathrooms and reliance on home-cooked meals (Bertram et al., 2001; Zysk, Głąbska, & Guzek, 2019) due to stay at home orders could have reduced some of the stress that is commonly encountered by this patient population outside their homes, although that level of detail around daily function was not obtained in this study. This aligns with a previous population-based study which showed that patients with inactive GI disorder have higher rates of mastery than community controls and may therefore cope better when experiencing an event that requires positive coping (Graff et al., 2009). To test the possibility that previous experience with social isolation could inoculate against mental health deterioration, future research should directly measure history of isolation and include comparisons with non-GI samples.
Our expectation that distress would be elevated in a relatively universal manner during the pandemic led us to examine the moderating effect of COVID fear. It seems reasonable that participants with greater fears of COVID-19 might increase their level of isolation to protect themselves and others, or, for those for whom isolation was not an option (such as front-line workers), fear would greatly exacerbate feelings of distress. Indeed, our assumptions about this relationship were corroborated somewhat in a recent study of COVID-19, anxiety and GI symptom perception in a sample with IBD (Trindade & Ferreira, 2020). In our current study however, and despite a significant bivariate correlation, fear of COVID-19 did not predict distress once it was included in the fully adjusted model. Overall, distress levels in the sample were generally low, and even in isolation COVID-19 fear was an unimpressive correlate of distress, and had the weakest coefficient of the three proposed moderators. We interpret these findings as suggestive that whatever the mental health impact of COVID-19 in general, fear of the virus is a minor contributor for GI populations.
Gastrointestinal symptoms significantly moderated the association between isolation and distress, with the association increasing in magnitude in accordance with increasing level of GI symptom severity. Holding feelings of isolation constant, participants reporting a higher level of symptoms reported a doubled rate of change to distress compared to those with lower levels of symptoms. This effect is not unexpected. Symptoms of stress, anxiety and depression strongly correlate with GI and other physical symptoms (Marrie, Graff, & Fisk JD, 2020(in press)), and psychological distress is a common co-morbidity in GI disorders, with at least 25% and 20% of patients with GI presentations reporting elevated symptoms of anxiety and depression, respectively (Mikocka-Walus, Emerson, Olive, & Knowles, 2019). Brain-gut interactions, as exemplified by the bi-directional links between the course of a GI disorder and mental health (Gracie et al., 2018; N. Koloski et al., 2020; N. A. Koloski et al., 2012; N. A. Koloski et al., 2016), are implicated in the causality and presentation of GI disorders (Knowles et al., 2019), and may explain the moderation effect. When GI symptoms are severe, the putative brain-gut interaction would increase the vulnerability to psychological stressors, such as experience of increased isolation. This is consistent with our observation that GI symptoms and isolation predicted distress levels even in the full model, demonstrating that both factors made unique contributions unexplained by covariates.
Limitations
The current study provided cross-sectional findings, which cannot lead to any directional, causal conclusions. Once longitudinal data are available from the project, there will be an opportunity to carefully examine relationships prospectively as well. It is acknowledged that the data collection methodology to obtain multi-country participants (online, English language only) may have resulted in bias in sampling, disproportionally representing a narrower segment of the population living with GI disorders, with respondents predominantly from Western countries. Further, we recruited via disease-specific websites and social media and this might have contributed not only to the higher SES but also, potentially, to a higher level of health literacy. The latter may translate into better knowledge and coping and consequently better mental health. In addition, we did not determine if respondents were living in rural or urban centres, and there may be a discrepancy in how those based in urban versus rural areas would handle the social isolation or perceive the distress of the pandemic.
Our sample was predominantly female, middle-aged, with a high proportion of respondents with a university education. Our finding that female respondents were less distressed than male respondents may reflect sample bias towards more distressed males participating in the study, as typically distress in GI conditions is higher in females (Greuter et al., 2020). In addition, our study showed lower distress among younger people relative to older participants, which contrasts with pandemic research in the general population (Msherghi et al., 2021; Saita et al., 2021). While a previous smaller IBD-related study documented greater distress among young people in a younger sample (Cheema et al., 2021), we propose that our current findings could be interpreted as reasonable given a likely higher number of co-morbidities, polypharmacy, and greater hesitation to utilise technology as a means to maintain social networks. In addition, we did not identify whether respondents had a known diagnosis of depression or anxiety which may have impacted on their response to the stress of the pandemic. To define job loss, we asked about employment pre- and post-COVID-19. This technique is less sensitive than a direct item regarding employment or income reduction. However, the operationalisation as described should reliably distinguish between currently employed, recently unemployed, recently employed, and chronically unemployed, and the comparison between recently unemployed and all others provides a useful contrast for participants whose employment situation has likely changed for the worse since COVID. Finally, the study utilized self-reported GI diagnosis, which has its disadvantages, but was seen as the most feasible approach given challenges in accessing patients in clinics during the early, acute phases of the pandemic. While there were participants with a variety of GI conditions, small numbers in most groups meant it was not feasible to compare among conditions or generalize findings to a specific type of GI condition (e.g. globus).
Conclusion
This international survey showed that in people with GI disorders sense of isolation was associated with greater distress. Isolation and mental health were closely linked in those with high experiential avoidance, elevated GI symptoms and COVID-19 fears. Interventions targeting these factors may help to reduce distress (i.e., symptoms of anxiety, depression and stress) in people with GI disorders at the time of major stressors such as the COVID-19 pandemic.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Simon Knowles, David Skvarc and Antonina Mikocka-Walus. The first draft of the manuscript was written by Antonina Mikocka-Walus and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
No funds, grants, or other support was received.
Data Availability
The data that support the findings of this study are available on request from the senior author, SK. The data are not publicly available due to restrictions.
Code Availability
Not applicable.
Declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article. Outside the present work, A. Mikocka-Walus served as an invited speaker at IBD-related conferences co-organized by Crohn's & Colitis Australia (a charity), Janssen and Ferring and received a speaker's fee. M. Barreiro-de Acosta has served as a speaker, consultant and advisory member for or has received research funding from MSD, AbbVie, Janssen, Kern Pharma, Celltrion, Takeda, Gillead, Pfizer, Ferring, Faes Farma, Shire Pharmaceuticals, Dr. Falk Pharma, Chiesi, Gebro Pharma, Adacyte and Vifor Pharma. Ch. Bernstein has served on advisory Boards for AbbVie Canada, Amgen Canada, Bristol Myers Squibb Canada, Janssen Canada, Roche Canada, Sandoz Canada, Takeda Canada, and Pfizer Canada; Consultant for Mylan Pharmaceuticals and Takeda; Educational grants from Abbvie Canada, Pfizer Canada, Takeda Canada, and Janssen Canada. Speaker’s panel for Abbvie Canada, Janssen Canada, Takeda Canada, and Medtronic Canada. Received research funding from Abbvie Canada and Pfizer Canada. J. Burisch reports personal fees from AbbVie, personal fees from Janssen-Cilag, personal fees from Celgene, grants and personal fees from MSD, personal fees from Pfizer, grants and personal fees from Takeda, grants and personal fees from Tillots Pharma, personal fees from Samsung Bioepis, grants from Bristol Myers Squibb, grants from Novo Nordisk, outside the submitted work. L. Graff has served as a consultant for Roche Canada. R. Gearry has served on advisory boards for AbbVie New Zealand and Australia, Janssen New Zealand. Speaker’s panel for AbbVie New Zealand and Australia, Janssen New Zealand, Takeda Australia, Educational grants from AbbVie, New Zealand. A. Stengel has worked as consultant for a + r Berlin, Boehringer Ingelheim, Dr. Wilmar Schwabe, Microbiotica and Takeda. I. A. Trindade has received consultancy fees from Pfizer Inc. M van Tilburg has served as a consultant for Mahana Therapeutics, inc. S.R Knowles served as an invited speaker at IBD-related conferences co-organized by Crohn's & Colitis Australia (a charity) and Coeliac Australia (a charity), is a member of the Medical Advisory Committee for Glutagen Pty Ltd, and has received consultancy fees from AbbVie Pty Ltd and Janssen-Cilag Pty Ltd.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Swinburne University of Technology Human Research Ethics Committee on 25th May 2020 (Ref: 20202978–4430) as well as the local Human Research Ethics Committees of the participating collaborators, as required.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- EuroStat. (2021). Database - Income and living conditions - Eurostat. Retrieved from: https://ec.europa.eu/eurostat/web/income-and-living-conditions/data/database
- Ann Pulk R, Leber M, Tran L, Ammar M, Amin N, Miller L, Yazdi M. Dynamic pharmacy leadership during the COVID-19 crisis: optimizing patient care through formulary and drug shortage management. American Journal of Health System Pharmacy. 2020 doi: 10.1093/ajhp/zxaa219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arrindell WA, Ross MW, Bridges R, Hout W, Hofman A, Sanderman R. Fear of aids: are there replicable, invariant questionnaire dimensions? Advances in Behaviour Research and Therapy. 1989;11:69–115. doi: 10.1016/0146-6402(89)90015-5. [DOI] [Google Scholar]
- Bernstein, C. N., Ng, S. C., Banerjee, R., Steinwurz, F., Shen, B., Carbonnel, F., ., . . . Gearry, R. B. (2020(in press)). Worldwide management of inflammatory bowel disease during the COVID-19 pandemic: An international survey. Inflamm Bowel Dis. [DOI] [PMC free article] [PubMed]
- Bertram S, Kurland M, Lydick E, Locke GR, 3rd, Yawn BP. The patient's perspective of irritable bowel syndrome. Journal of Family Practice. 2001;50(6):521–525. [PubMed] [Google Scholar]
- Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, Zettle RD. Preliminary psychometric properties of the acceptance and action questionnaire-II: a revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy. 2011;42(4):676–688. doi: 10.1016/j.beth.2011.03.007. [DOI] [PubMed] [Google Scholar]
- Canavan C, West J, Card T. Review article: the economic impact of the irritable bowel syndrome. Alimentary Pharmacology & Therapeutics. 2014;40(9):1023–1034. doi: 10.1111/apt.12938. [DOI] [PubMed] [Google Scholar]
- Chaparro M, Barreiro-de Acosta M, Benítez JM, Cabriada JL, Casanova MJ, Ceballos D, Gisbert JP. EpidemIBD: rationale and design of a large-scale epidemiological study of inflammatory bowel disease in Spain. Therap Adv Gastroenterol. 2019;12:1756284819847034. doi: 10.1177/1756284819847034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheema M, Mitrev N, Hall L, Tiongson M, Ahlenstiel G, Kariyawasam V. Depression, anxiety and stress among patients with inflammatory bowel disease during the COVID-19 pandemic: Australian national survey. BMJ Open Gastroenterol. 2021 doi: 10.1136/bmjgast-2020-000581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clappison E, Hadjivassiliou M, Zis P. Psychiatric manifestations of coeliac disease, a systematic review and meta-analysis. Nutrients. 2020 doi: 10.3390/nu12010142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler MÉ, Marynak K, Clarke KE. Delay or avoidance of medical care because of COVID-19–related concerns — United States, june 2020. MMWR. Morbidity and Mortality Weekly Report. 2020;69:1250–1257. doi: 10.15585/mmwr.mm6936a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis, J., Jasper, C., & McCarthy, M. (2020, 4th August 2020). Shoppers urged to be patient as Victorian coronavirus restrictions impact food supply. ABC Rural. Retrieved from https://www.abc.net.au/news/2020-08-04/victorian-coronavirus-restrictions-impact-on-food-supply/12518136
- Dimenäs E, Carlsson G, Glise H, Israelsson B, Wiklund I. Relevance of norm values as part of the documentation of quality of life instruments for use in upper gastrointestinal disease. Scandinavian Journal of Gastroenterology. Supplement. 1996;221:8–13. doi: 10.3109/00365529609095544. [DOI] [PubMed] [Google Scholar]
- Dimenäs E, Glise H, Hallerbäck B, Hernqvist H, Svedlund J, Wiklund I. Well-being and gastrointestinal symptoms among patients referred to endoscopy owing to suspected duodenal ulcer. Scandinavian Journal of Gastroenterology. 1995;30(11):1046–1052. doi: 10.3109/00365529509101605. [DOI] [PubMed] [Google Scholar]
- ECDC. (2021). Download today’s data on the geographic distribution of COVID-19 cases worldwide. Retrieved from https://www.ecdc.europa.eu/en/publications-data/download-todays-data-geographic-distribution-covid-19-cases-worldwide
- Ferreira N, Mikocka-Walus A, van Tilburg MAL, Graff LA, Apputhurai P, Barreiro-de Acosta M, Knowles SR. The impact of the coronavirus (COVID-19) pandemic on individuals with gastrointestinal disorders: a protocol of an international collaborative study. Journal of Psychosomatic Research. 2021;148:110561. doi: 10.1016/j.jpsychores.2021.110561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fourie S, Jackson D, Aveyard H. Living with inflammatory bowel disease: a review of qualitative research studies. International Journal of Nursing Studies. 2018;87:149–156. doi: 10.1016/j.ijnurstu.2018.07.017. [DOI] [PubMed] [Google Scholar]
- Fox, J., & Weisberg, S. (2018). car: Companion to Applied Regression. [R package]. Retrieved from https://cran.r-project.org/package=car
- GBD2017IBDCollaborators. (2020). The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol, 5(1), 17-30. doi:10.1016/s2468-1253(19)30333-4 [DOI] [PMC free article] [PubMed]
- Gracie DJ, Guthrie EA, Hamlin PJ, Ford AC. Bi-directionality of brain-gut interactions in patients with inflammatory bowel disease. Gastroenterology. 2018;154(6):1635–1646.e1633. doi: 10.1053/j.gastro.2018.01.027. [DOI] [PubMed] [Google Scholar]
- Graff LA, Walker JR, Clara I, Lix L, Miller N, Rogala L, Bernstein CN. Stress coping, distress, and health perceptions in inflammatory bowel disease and community controls. American Journal of Gastroenterology. 2009;104(12):2959–2969. doi: 10.1038/ajg.2009.529. [DOI] [PubMed] [Google Scholar]
- Greuter T, Manser C, Pittet V, Vavricka SR, Biedermann L. Gender differences in inflammatory bowel disease. Digestion. 2020;101(Suppl 1):98–104. doi: 10.1159/000504701. [DOI] [PubMed] [Google Scholar]
- Hayes, S. C. (2019). The Acceptance and Action Questionnaire (AAQ-2).
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and Commitment Therapy: An Experiential Approach to Behavior Change. Guilford Press; 1999. [Google Scholar]
- Henry JD, Crawford JR. The short-form version of the depression anxiety stress scales (DASS-21): Construct validity and normative data in a large non-clinical sample. British Journal of Clinical Psychology. 2005;44(Pt 2):227–239. doi: 10.1348/014466505x29657. [DOI] [PubMed] [Google Scholar]
- Hodgson S, Watts I, Fraser S, Roderick P, Dambha-Miller H. Loneliness, social isolation, cardiovascular disease and mortality: a synthesis of the literature and conceptual framework. Journal of the Royal Society of Medicine. 2020;113(5):185–192. doi: 10.1177/0141076820918236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtmann GJ, Ford AC, Talley NJ. Pathophysiology of irritable bowel syndrome. Lancet Gastroenterol Hepatol. 2016;1(2):133–146. doi: 10.1016/s2468-1253(16)30023-1. [DOI] [PubMed] [Google Scholar]
- Hossain MM, Sultana A, Purohit N. Mental health outcomes of quarantine and isolation for infection prevention: a systematic umbrella review of the global evidence. Epidemiol Health. 2020;42:e2020038. doi: 10.4178/epih.e2020038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IASC. (2020). ADDRESSING MENTAL HEALTH AND PSYCHOSOCIAL ASPECTS OF COVID-19 OUTBREAK Version 1.5. Retrieved from Geneva:
- jamovi. (2020). The jamovi project [Computer Software] (Version Version 1.1). Retrieved from https://www.jamovi.org
- Kamp KJ, West P, Holmstrom A, Luo Z, Wyatt G, Given B. Systematic review of social support on psychological symptoms and self-management behaviors among adults with inflammatory bowel disease. Journal of Nursing Scholarship. 2019;51(4):380–389. doi: 10.1111/jnu.12487. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review. 2010;30(7):865–878. doi: 10.1016/j.cpr.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowles S, Keefer L, Mikocka-Walus A. Psychogastroenterology for Adults: a Handbook for Mental Health Professionals. 1. Routledge; 2019. [Google Scholar]
- Koloski N, Holtmann G, Talley NJ. Is there a causal link between psychological disorders and functional gastrointestinal disorders? Expert Review of Gastroenterology & Hepatology. 2020;14(11):1047–1059. doi: 10.1080/17474124.2020.1801414. [DOI] [PubMed] [Google Scholar]
- Koloski NA, Jones M, Kalantar J, Weltman M, Zaguirre J, Talley NJ. The brain–gut pathway in functional gastrointestinal disorders is bidirectional: a 12-year prospective population-based study. Gut. 2012;61(9):1284–1290. doi: 10.1136/gutjnl-2011-300474. [DOI] [PubMed] [Google Scholar]
- Koloski NA, Jones M, Talley NJ. Evidence that independent gut-to-brain and brain-to-gut pathways operate in the irritable bowel syndrome and functional dyspepsia: a 1-year population-based prospective study. Alimentary Pharmacology & Therapeutics. 2016;44(6):592–600. doi: 10.1111/apt.13738. [DOI] [PubMed] [Google Scholar]
- Kroska EB, Roche AI, Adamowicz JL, Stegall MS. Psychological flexibility in the context of COVID-19 adversity: associations with distress. Journal of Contextual Behavioral Science. 2020;18:28–33. doi: 10.1016/j.jcbs.2020.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landi G, Pakenham KI, Boccolini G, Grandi S, Tossani E. Health anxiety and mental health outcome during COVID-19 lockdown in Italy: the mediating and moderating roles of psychological flexibility. Frontiers in Psychology. 2020;11:2195. doi: 10.3389/fpsyg.2020.02195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CM, Cadigan JM, Rhew IC. Increases in loneliness among young adults during the COVID-19 pandemic and association with increases in mental health problems. Journal of Adolescent Health. 2020;67(5):714–717. doi: 10.1016/j.jadohealth.2020.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, Caan W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–171. doi: 10.1016/j.puhe.2017.07.035. [DOI] [PubMed] [Google Scholar]
- Lenth, R. (2018). emmeans: Estimated Marginal Means, aka Least-Squares Means. [R package]. Retrieved from https://cran.r-project.org/package=emmeans
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2. Psychology Foundation; 1995. [Google Scholar]
- Ma R, Mann F, Wang J, Lloyd-Evans B, Terhune J, Al-Shihabi A, Johnson S. The effectiveness of interventions for reducing subjective and objective social isolation among people with mental health problems: a systematic review. Social Psychiatry and Psychiatric Epidemiology. 2020;55(7):839–876. doi: 10.1007/s00127-019-01800-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marrie, R. A., Graff, L. A., & Fisk JD, P. S., Bernstein CN (2020(in press)). The relationship between symptoms of depression and anxiety and disease activity in IBD over time. Inflamm Bowel Dis. [DOI] [PMC free article] [PubMed]
- Mikocka-Walus, A., Emerson, C., Olive, L., & Knowles, S. R. (2019). Common psychological issues in gastrointestinal conditions. In S. R. Knowles, L. Keefer, & A. Mikocka-Walus (Eds.), Psychogastroenterology for Adults: A Handbook for Mental Health Professionals. London: Routledge.
- Mikocka-Walus A, Knowles SR, Keefer L, Graff L. Controversies revisited: a systematic review of the comorbidity of depression and anxiety with inflammatory bowel diseases. Inflammatory Bowel Diseases. 2016;22(3):752–762. doi: 10.1097/mib.0000000000000620. [DOI] [PubMed] [Google Scholar]
- Msherghi A, Alsuyihili A, Alsoufi A, Ashini A, Alkshik Z, Alshareea E, Elhadi M. Mental health consequences of lockdown during the COVID-19 pandemic: a cross-sectional study. Frontiers in Psychology. 2021;12:605279. doi: 10.3389/fpsyg.2021.605279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy D, Williamson C, Baumann J, Busuttil W, Fear NT. Exploring the impact of COVID-19 and restrictions to daily living as a result of social distancing within veterans with pre-existing mental health difficulties. BMJ Mil Health. 2020 doi: 10.1136/bmjmilitary-2020-001622. [DOI] [PubMed] [Google Scholar]
- Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, Kaplan GG. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2018;390(10114):2769–2778. doi: 10.1016/s0140-6736(17)32448-0. [DOI] [PubMed] [Google Scholar]
- Noone C, McSharry J, Smalle M, Burns A, Dwan K, Devane D, Morrissey EC. Video calls for reducing social isolation and loneliness in older people: a rapid review. Cochrane Database System Review. 2020 doi: 10.1002/14651858.Cd013632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OECD. (2021). OECD Income Distribution Database (IDD): Gini, poverty, income, Methods and Concepts. Retrieved from: https://www.oecd.org/social/income-distribution-database.htm
- OzForex. (2020). Yearly Average Rates.
- Pakenham KI, Landi G, Boccolini G, Furlani A, Grandi S, Tossani E. The moderating roles of psychological flexibility and inflexibility on the mental health impacts of COVID-19 pandemic and lockdown in Italy. Journal of Contextual Behavioral Science. 2020;17:109–118. doi: 10.1016/j.jcbs.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park KT, Ehrlich OG, Allen JI, Meadows P, Szigethy EM, Henrichsen K, Heller CA. The cost of inflammatory bowel disease: an initiative from the Crohn's & Colitis foundation. Inflammatory Bowel Diseases. 2020;26(1):1–10. doi: 10.1093/ibd/izz104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prout TA, Zilcha-Mano S, Aafjes-van Doorn K, Békés V, Christman-Cohen I, Whistler K, Di Giuseppe M. Identifying predictors of psychological distress during COVID-19: a machine learning approach. Frontiers in Psychology. 2020;11:586202. doi: 10.3389/fpsyg.2020.586202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman MA, Hoque N, Alif SM, Salehin M, Islam SMS, Banik B, Cross W. Factors associated with psychological distress, fear and coping strategies during the COVID-19 pandemic in Australia. Global Health. 2020;16(1):95. doi: 10.1186/s12992-020-00624-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saini GK, Haseeb SB, Taghi-Zada Z, Ng JY. The effects of meditation on individuals facing loneliness: a scoping review. BMC Psychol. 2021;9(1):88. doi: 10.1186/s40359-021-00585-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saita E, Facchin F, Pagnini F, Molgora S. In the eye of the Covid-19 storm: a web-based survey of psychological distress among people living in Lombardy. Frontiers in Psychology. 2021;12:566753. doi: 10.3389/fpsyg.2021.566753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah SGS, Nogueras D, van Woerden HC, Kiparoglou V. Evaluation of the effectiveness of digital technology interventions to reduce loneliness in older adults: systematic review and meta-analysis. Journal of Medical Internet Research. 2021;23(6):e24712. doi: 10.2196/24712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shvedko A, Whittaker AC, Thompson JL, Greig CA. Physical activity interventions for treatment of social isolation, loneliness or low social support in older adults: a systematic review and meta-analysis of randomised controlled trials. Psychology of Sport & Exercise. 2018;34:128–137. doi: 10.1016/j.psychsport.2017.10.003. [DOI] [Google Scholar]
- Sibley CG, Greaves LM, Satherley N, Wilson MS, Overall NC, Lee CHJ, Barlow FK. Effects of the COVID-19 pandemic and nationwide lockdown on trust, attitudes toward government, and well-being. American Psychologist. 2020 doi: 10.1037/amp0000662. [DOI] [PubMed] [Google Scholar]
- Smith BJ, Lim MH. How the COVID-19 pandemic is focusing attention on loneliness and social isolation. Public Health Research Practice. 2020 doi: 10.17061/phrp3022008. [DOI] [PubMed] [Google Scholar]
- Sperber, A. D., Bangdiwala, S. I., Drossman, D. A., Ghoshal, U. C., Simren, M., Tack, J., . . . Palsson, O. S. (2020). Worldwide Prevalence and Burden of Functional Gastrointestinal Disorders, Results of Rome Foundation Global Study. Gastroenterology Doi:10.1053/j.gastro.2020.04.014 [DOI] [PubMed]
- Trindade IA, Ferreira NB. COVID-19 Pandemic's effects on disease and psychological outcomes of people with inflammatory bowel disease in portugal: a preliminary research. Inflammatory Bowel Diseases. 2020 doi: 10.1093/ibd/izaa261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truu, M. (2020, 28th May 2020). Half of Australian women were impacted by period product shortages during coronavirus. SBS News. Retrieved from https://www.sbs.com.au/news/half-of-australian-women-were-impacted-by-period-product-shortages-during-coronavirus
- Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. 2016;102(13):1009–1016. doi: 10.1136/heartjnl-2015-308790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veazie, S., Gilbert, J., & Winchell, K. (2019). Addressing Social Isolation To Improve the Health of Older Adults: A Rapid Review. Appendix F, Social Isolation and Loneliness Definitions and Measures. Retrieved from Rockville (MD): https://www.ncbi.nlm.nih.gov/books/NBK537897/ [PubMed]
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal Environmental Research Public Health. 2020 doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S, Zhang Y, Ding W, Meng Y, Hu H, Liu Z, Wang M. Psychological distress and sleep problems when people are under interpersonal isolation during an epidemic: a nationwide multicenter cross-sectional study. European Psychiatry. 2020;63(1):e77. doi: 10.1192/j.eurpsy.2020.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong SYS, Zhang D, Sit RWS, Yip BHK, Chung RY, Wong CKM, Mercer SW. Impact of COVID-19 on loneliness, mental health, and health service utilisation: a prospective cohort study of older adults with multimorbidity in primary care. British Journal of General Practice. 2020;70(700):e817–e824. doi: 10.3399/bjgp20X713021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright, P. (2020, 25th March 2020). Coronavirus COVID-19: Why is everyone buying toilet paper? ABC Life. Retrieved from https://www.abc.net.au/life/coronavirus-covid-19-why-is-everyone-buying-toilet-paper/12024738
- Zamani M, Alizadeh-Tabari S, Zamani V. Systematic review with meta-analysis: the prevalence of anxiety and depression in patients with irritable bowel syndrome. Alimentary Pharmacology & Therapeutics. 2019;50(2):132–143. doi: 10.1111/apt.15325. [DOI] [PubMed] [Google Scholar]
- Zysk W, Głąbska D, Guzek D. Food neophobia in celiac disease and other gluten-free diet individuals. Nutrients. 2019 doi: 10.3390/nu11081762. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the senior author, SK. The data are not publicly available due to restrictions.
Not applicable.