Abstract
Introduction:
The DIEP flap is considered the gold standard in autologous breast reconstruction. Despite the benefit of a lifelong natural reconstruction, some argue that the potential drawbacks, specifically operative time and recovery, are significant. We recently focused specifically on process analysis in our DIEP flap practice and present a comprehensive analysis in efficient DIEP flap breast reconstructions.
Methods:
Fifty consecutive bilateral DIEP flaps were prospectively tracked (100 flaps). The procedure was divided into segments (recipient site preparation, DIEP flap dissection/harvest, microsurgery, breast shaping, and abdominal closure). All individual step times were recorded for each team member. Relevant patient characteristics, intraoperative details and postoperative outcomes were recorded.
Results:
Average surgical time was 3 hours and 58 minutes (the fastest time recorded was 2 h and 14 min). There were no immediate postoperative complications. The anastomotic revision rate was 6%. Four surgeons contributed 34.7% of the time, three surgeons 32.2% of the time, two surgeons 23.6% of the time, and one surgeon 4.8% of total time. In procedures under 4 hours, four surgeons contributed simultaneously 36.7% of the time compared to 21.8% in the longer procedures (P = 0.004). Four surgeons contributed 45.4% of the time (P = 0.01) in the sub-three-hour bilateral DIEP flap procedures.
Conclusions:
Efficient DIEP flap breast reconstruction can be accomplished with a well-trained and coordinated team approach involving like-minded surgeons with extensive experience working together. The synergistic map shows constant movement with utilization of hidden time, without sacrificing education, outcomes, or innovation.
INTRODUCTION
The gold standard procedure for natural, lifelong breast reconstruction is the deep inferior epigastric perforator flap (DIEP flap). The DIEP flap is a complex procedure with innumerable critical yet subtle steps in achieving success and historically some of the drawbacks have been a much longer operative time, increase in morbidity, pain, longer hospital stay and longer convalescence for the patient. Along with other surgeons,1–3 we have sought to optimize this operation to increase patient access.4–8 Process analysis remains an important aspect to reduce complacency and provide the opportunity for continued progression in the field of microsurgical breast reconstruction.
When improving a procedure as complex as a DIEP flap, we can focus on multiple aspects, ranging from operative setup, decision-making, technical aspects, donor site management, and finally the aesthetic outcome. The operative setup has been discussed in previous works, and there is no question that efficiency can be increased with streamlined instrument trays.9 Decision-making has been improved with experience and confidence on perforator selection,4 as well as the increased use of technology for perforator mapping.8 The physical movement of hands and specific aspects of surgical technique are difficult to standardize, or study, without one-on-one interaction.10 As success has increased with microsurgical procedures, many focus on limiting donor site morbidity in autologous breast reconstruction.5,11 Although the aesthetic outcome is commonly the center of discussion at meetings and carries a paramount importance to the patient, it is difficult to standardize and tends to be less tangible to assess in large series. Of all the facets in DIEP flap breast reconstruction, the aesthetic outcome is the most subjective.
In our standard DIEP flap breast reconstruction, we maintain aesthetic outcome at center focus, without sacrificing other goals of efficiency and safety. To better accomplish the primary goal, we continue to evaluate the overall logistics and operational flow. We previously studied our process on what we considered to be the more standard technical steps of this operation.6 We focused specifically on how experience impacts the execution of DIEP flap harvest and microsurgery. We are now expanding our focus to map the entire operation. Our current goal is to expand this analysis to encompass our entire procedure using a co-surgery model12 and show the operative flow in a highly efficient DIEP flap breast reconstruction without being fast.
METHODS
An IRB approved study was performed using a REDCap (Research Electronic Data Capture) database.13,14 Fifty consecutive bilateral delayed DIEP flap breast reconstruction patients were evaluated. Demographic data, surgical characteristics, and postoperative course were all recorded and analyzed.
Using a detailed process mapping, 50 consecutive bilateral DIEP flaps were prospectively tracked. The procedure was divided into five overall segments with multiple subsegments. The overall segments include recipient site preparation, DIEP flap dissection and harvest, microsurgery, aesthetic breast inset and shaping, and abdominal closure (Figs. 1–5). All reconstructions were delayed (11 breasts) or delayed-immediate (89 breasts) bilateral breast reconstructions. Throughout each procedure, the start and stop times of all tasks were recorded. The performance of every individual and their experience level was tracked and recorded. The two attendings were consistently the same but the other two surgeons were not. We did not track surgeons that were not physically using their hands but might be supervising and guiding a portion of the procedure. This data was placed into a flow schematic, or map, to allow operational evaluation.
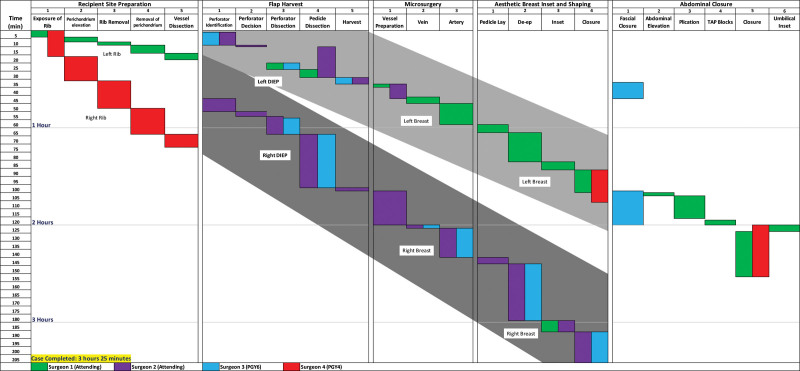
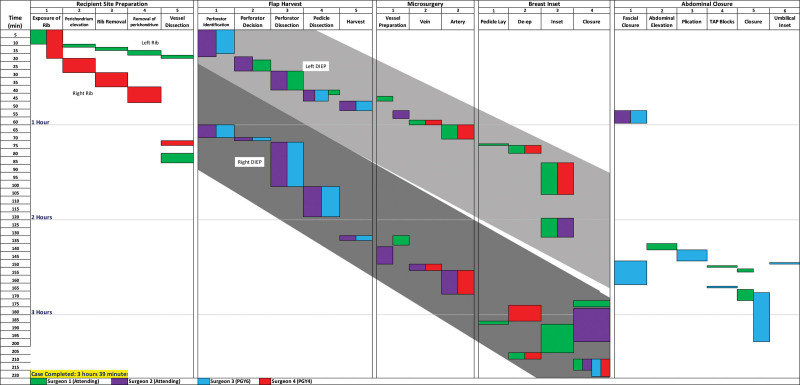
Fig. 1.
Mapping diagram of a delayed bilateral DIEP flap breast reconstruction in a 58-year-old patient with BMI of 25.6. The first DIEP flap had one intermediate perforator and the second DIEP flap had three lateral perforators. There were no revisions. The procedure was completed in 3 hours and 25 minutes.
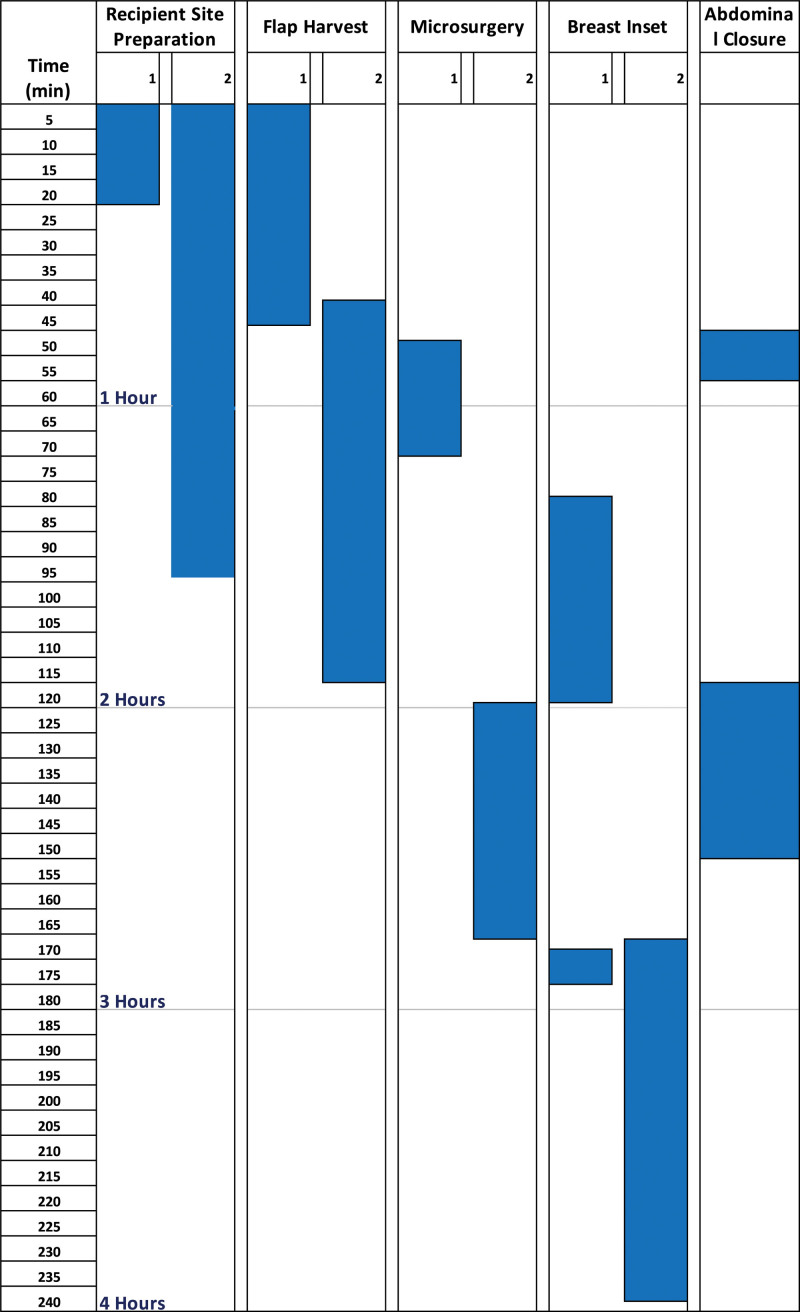
Fig. 5.
Mapping diagram of a delayed bilateral DIEP flap breast reconstruction in a 49-year-old patient with BMI of 25.2. The first DIEP flap had two lateral perforators and the second DIEP flap had two lateral perforators. There were no revisions. The procedure was completed in 2 hours and 14 minutes.
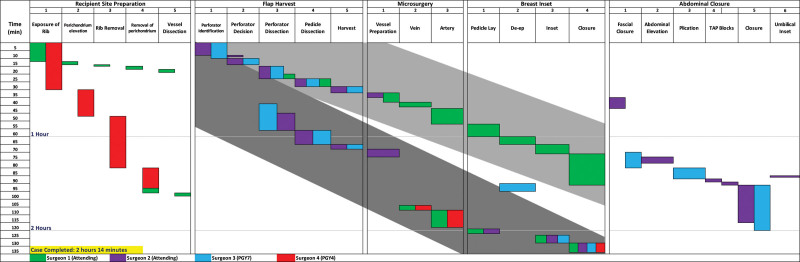
Fig. 2.
Mapping diagram of a delayed bilateral DIEP flap breast reconstruction in a 62-year-old patient with BMI of 23.7. The first DIEP flap had two lateral perforators and the second DIEP flap had two lateral perforators. There were revisions of both arterial anastomoses. The procedure was completed in 3 hours and 36 minutes.
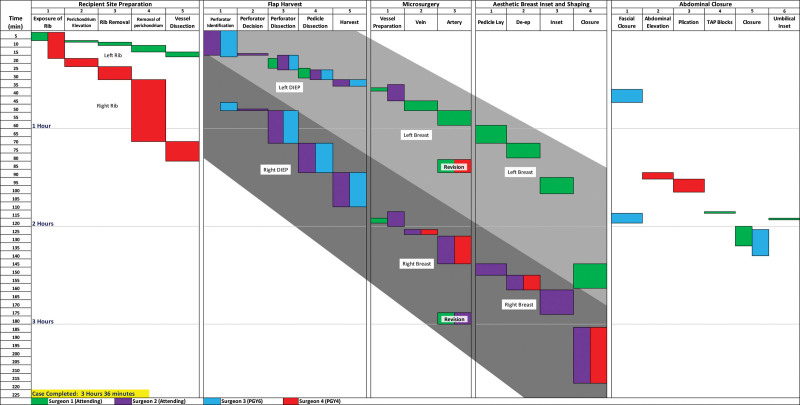
Fig. 3.
Mapping diagram of a delayed bilateral DIEP flap breast reconstruction in a 41-year-old patient with BMI of 24.4. The first DIEP flap had one intermediate perforator and the second DIEP flap had one intermediate perforator. There were no revisions. The procedure was completed in 3 hours and 33 minutes.
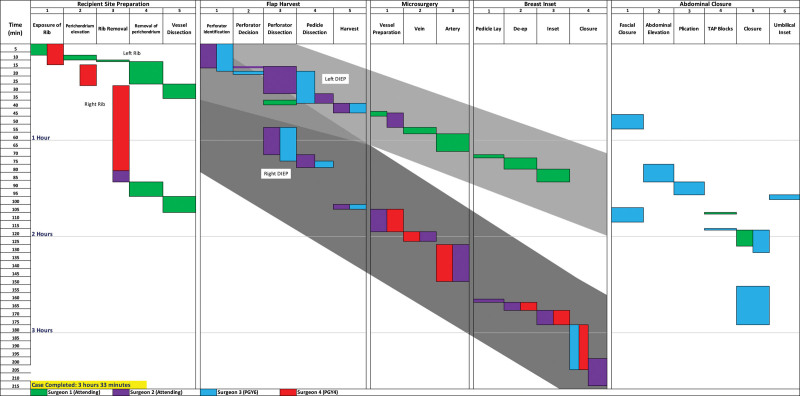
Fig. 4.
Mapping diagram of a delayed bilateral DIEP flap breast reconstruction in a 42-year-old patient with BMI of 36.5. The first DIEP flap had one medial perforator as well as two lateral perforators and the second DIEP flap had one medial perforator. There were no revisions. The procedure was completed in 3 hours and 39 minutes.
Statistical analysis was performed using Microsoft Excel (2020, Microsoft Corporation, Redmond, Wash.).
RESULTS
Fifty consecutive patients undergoing delayed bilateral DIEP flaps were included in this prospective study (100 flaps). This study was conducted during the initial lockdown secondary to COVID-19, from January 2020 until August 2020. Patient demographics are shown in Table 1. The average total surgical time (skin incision to skin closure completion) was 3 hours and 58 minutes (maximum time 6 h and 36 min, minimum 2 h 14 min, SD 48.5 min). All flaps were completed successfully without immediate postoperative complication. There was a total anastomotic revision rate of 6%, with 75% of these being arterial. The total length of stay for this patient series was 2.5 days. If excluding patients that stayed for social reasons (out of town patients, limited family support), the length of stay was decreased to 2.16 days. Patient complications included two abdominal wounds that ultimately required operative treatment, and one breast wound in the remaining radiated tissue that was revised at a secondary phase surgery. There were no immediate returns to the operating room or flap losses. There were no clinical signs of fat necrosis in this series. All flaps were evaluated with indocyanine green15 at time of inset. Intraoperative details and postoperative course is shown in Tables 2 and 3.
Table 1.
Patient Characteristics Divided by Those Procedures that Took More Than, and Less Than, 4 Hours
| Under 4 h DIEPs | Over 4 h DIEPs | Total DIEPs | ||||
|---|---|---|---|---|---|---|
| 30 | 20 | 50 | ||||
| Average | SD | Average | SD | Average | SD | |
| Age, y | 50.2 | 8 | 52 | 8.2 | 50.9 | 8.2 |
| Radiation | 10 | 33% | 9 | 45% | 19 | 38% |
| Chemo | 20 | 67% | 9 | 45% | 29 | 58% |
| Body mass index | 28.7 | 5.3 | 31.9 | 7.2 | 30 | 6.2 |
| High | 39.8 | 48.1 | 48.1 | |||
| Low | 22.1 | 22.3 | 22.1 | |||
| Former smoker | 5 | 16.7% | 6 | 30.0% | 11 | 22.0% |
| Autoimmune | 5 | 16.7% | 2 | 10.0% | 7 | 14.0% |
| Clotting history | 1 | 3.3% | 0 | 0.0% | 1 | 2.0% |
| Hypertension | 7 | 23.3% | 5 | 25.0% | 12 | 24.0% |
| Diabetes mellitus | 1 | 3.3% | 1 | 5.0% | 2 | 4.0% |
Table 2.
Intraoperative Characteristics and Hospital Course Divided by Those Procedures that Took More Than, and Less Than, 4 Hours
| Under 4 h | Over 4 hs | Total DIEPs | |
|---|---|---|---|
| Flap weight (initial) | 825 | 1176 | 972 |
| Flap weight (final) | 774 | 1000 | 865 |
| 1 perforator | 44.4% | 39.5% | 42.4% |
| 2 perforators | 38.9% | 44.7% | 41.3% |
| 3 perforators | 14.8% | 10.5% | 13.0% |
| 4 perforators | 1.9% | 5.3% | 3.3% |
| Medial only | 26.4% | 36.1% | 30.3% |
| Lateral only | 62.3% | 52.8% | 58.4% |
| Intermediate only | 5.7% | 8.3% | 6.7% |
| Multiple | 5.7% | 2.8% | 4.5% |
| LOS (excluding social) | 2.17 | 2.15 | 2.16 |
| LOS (all) | 2.4 | 2.65 | 2.49 |
LOS, length of stay.
Table 3.
Patient Complications Divided by Those Procedures that Took Greater Than, and More Than, 4 Hours
| Under 4 h | Over 4 h | Total DIEPs | ||||
|---|---|---|---|---|---|---|
| Abdominal wounds | 1 | 3.3% | 1 | 5.0% | 2 | 4.0% |
| Seromas | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Vessel revisions | 3 | 2.5% | 9 | 11.3%* | 12 | 6.0% |
| Blood transfusions | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| DVT | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| PE | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Return to OR | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Flap losses | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
*Statistically significant (P = 0.01). DVT, deep vein thrombosis; PE, pulmonary embolism; OR, operating room.
Our typical procedure is completed with a three- or four-person team. In this series, it was always a four-person team. There was significant overlap and assistance with each step. This allows multiple surgeons to simultaneously work. During this series, on average for each individual procedure, four surgeons were contributing 34.7% of the time, three surgeons were contributing 32.2% of the time, two surgeons were contributing 23.6% of the time, and one surgeon was contributing 4.8% of total time. Idle time was 4.6% of the procedure with no surgeons physically working. The number of surgeons contributing simultaneously had a direct impact on total operative time. In the more efficient procedures (under 4 h), four surgeons were contributing simultaneously 36.7% of the total time compared to 21.8% in the longer procedures (P = 0.004). Four surgeons contributed 45.4% of the total time (P = 0.01) in the sub-three-hour bilateral DIEP flap procedures.
The procedural flow was diagramed in representative maps for each surgery. (Figs. 1–5) Each surgeon (two attendings and two trainees) is given a color and their contribution to individual surgical steps is recorded and shown in the diagrams. Critical analysis was performed for each procedure that contributed to specific rate limiting steps or surgical pauses.
The recipient site preparation included the pocket preparation as well as vessel exposure and preparation.7 In our series, the left chest was always prepared (average 19.9 min) before completion of the first DIEP flap dissection and harvest (43.7 min). This allowed the surgeon that initially worked in the chest to contribute to the first DIEP flap dissection and harvest in 100% of cases. Expeditious completion of the recipient site allowed this surgeon to perform on average of 2.2 steps over 18.5 minutes of flap dissection and harvest (most commonly perforator and pedicle dissection).
The first flap anastomosis was performed with loupe magnification to avoid obstruction of the contralateral chest and resulting pause of internal mammary vessel preparation. The second chest preparation (average time 94.3 min) still delayed harvest of the second flap in 35% of procedures.
The DIEP flap harvest includes the five critical steps to flap procurement. The first flap was harvested by 43.7 ± 12.7 minutes while the second flap was harvested by 115.3 ± 30.4 minutes. From start to finish, the average flap harvest time was 59.8 ± 24.9 minutes (flap one 43.7 ± 12.7 min and flap two 76.6 ± 23.5 min) (P < 0.001). This statistically significant difference was likely secondary to the fact that more surgeons were involved in the first flap harvest.
Microsurgery included three steps (microsurgical preparation, venous anastomoses, and arterial anastomoses). Average ischemia time for all flaps was 34.5 ± 15.6 minutes. The first harvested flap had a significantly lower ischemia time (23.1 ± 5.2 compared to 47.7 ± 12.5, P < 0.001). The average setup and flap preparation was 17.8 minutes, the venous anastomosis was 3.8 minutes, and the arterial anastomosis was 13.7 minutes. The setup and preparation time is skewed by the fact that we routinely complete a portion of the abdominal closure (abdominal elevation, plication, fascial closure, and transversus abdominis plane blocks) before initiating microsurgery on the second flap. This allows complete closure of the abdomen, whereas the anastomoses are completed. This discrepancy is seen when the first preparation time is compared to the second preparation time (8.3 ± 4.5 versus 25.7 ± 12.6 min) (P < 0.001).
Anastomotic revisions occurred in 12 flaps. Despite a relatively small direct delay of 17.6 ± 7.7 minutes, there is likely a larger impact that is not completely accounted for. When revision is required, two surgeons are removed from continued progress and potentially other portions of the procedure are placed on hold as a result. Procedures that took less than 4 hours were less likely to require an anastomotic revision in comparison to those that took more than 4 hours (5% versus 22.5%, P = 0.01).
The aesthetic inset and shaping consisted of four steps. This portion of the procedure took 47.3 ± 16.4 minutes on average with 2.48 surgeons contributing. The first flap inset always overlapped with other portions of the procedure, whereas the second flap inset typically did not. The second flap inset is a rate limiting step for completion of the procedure. To help expedite inset of the secondary flap, more surgeons are involved then in the first flap inset (3.28 versus 1.68, P < 0.001). The aesthetic result is likely the most critical portion of the procedure to the overall outcome (Figs. 6 and 7).
Fig. 6.
A 44-year-old woman treated with mastectomy and radiation at an outside facility. She ultimately had wound complications requiring a skin graft. We treated her with delayed bilateral DIEP flaps followed by one additional surgery for slight revision and nipple reconstruction.
Fig. 7.
A 42-year-old woman that underwent bilateral mastectomy for an invasive breast cancer. She was initially treated with expanders followed by radiation. She returned for bilateral DIEP flaps followed by one additional surgery for slight revision and nipple reconstruction.
The abdominal closure included six steps. Fascia is closed with a combination of interrupted sutures and running sutures. The mesh is used only when fascia appears weak.16 Plication is performed with interrupted figure of eight sutures. TAP blocks are performed with ultrasound. The abdominal skin flap is closed in three layers (interrupted sutures in the superficial fascial system and dermis and running subcuticular). The umbilicus is inset with tacking sutures to the abdominal wall or removed based on stalk height, obesity, and positioning.5 As we transitioned to positioning the patient for abdominal closure before starting the second microsurgery, the abdominal closure is always completed before the completion of the second flap. The closure is also completed before the final closure of the first flap in 47.1% of procedures. On average, the abdominal closure was completed with 56 minutes remaining in the overall procedure.
The overall average flow of our efficient DIEP is shown in Figure 8.
Fig. 8.
Mapping diagram of average efficient DIEP flap breast reconstruction
DISCUSSION
As our experience with autologous tissue breast reconstruction increased, it was natural to begin evaluating our process to achieve improved outcomes. Ultimately, without fully understanding the concepts, we applied deliberate practice, a term coined by Anders Ericsson,17 and introduced to us by Dr Evan S. Garfein.18 We started with subsections of this multistep, complex operation. We published a paper on chest preparation7 and a video description of our typical technique. This has been used as a model to train our team and standardize the process. DIEP flap harvest and microsurgery6 were next divided into steps to help the team create a standard mental map of the critical steps and maneuvers. We now present a more comprehensive analysis. With focus on efficiency and process mapping, we have experienced a drastic decrease in operative times. In 2015, our average bilateral DIEP flap breast reconstruction took 8 hours and 34 minutes, whereas in 2020, we present 50 consecutive procedures with an average time that is reduced by over half (3 h and 58 min). Our most efficient time during this study was 2 hours and 14 minutes, with several under 3 hours, and a more recent bilateral DIEP was completed in 1 hour and 47 minutes. Previous work with national datasets (that admittedly did not have a matched group to our series) presents similar times to our earlier experience (8 h and 44 min).19 This advancement has come with a significant increase in experience; in 2015, we had completed approximately 700 autologous tissue breast reconstructions, and in 2020, we have completed over 2000.
Our current total operative times are now significantly lower than what we published in our analysis focused on DIEP flap harvest and microsurgery only.6 It was rightfully pointed out that we were not including critical portions of this highly technical, yet ultimately aesthetically minded, procedure.20 In that study, we did not include the aesthetic portions of both the breast inset and the donor site closure. In the current study, we provide a different and more comprehensive look at our surgical process in DIEP flap breast reconstruction.
Our approach to breast reconstruction has evolved over the years and we have more recently implemented significant process analysis. Our initial goal was focused on enhancing efficiency and allowing a more direct compartmentalized educational experience. We now look at our operation in a more global manner, recording from start to completion. With this analysis, one can appreciate that our approach uses two attendings and allows all critical steps to happen simultaneously instead of in-sequence. One example of this is the incorporation of loupe microsurgery for the first set of anastomoses.21 There was a slight learning curve related to this modified technique, and as a result an early increase in intraoperative revisions. Although these revisions did produce a significant change in operative time, it had a limited overall impact toward time. Ultimately, we found that the use of loupe microsurgery allows continued contralateral recipient site preparation as well as contralateral flap harvest without interference.
An additional point of efficiency utilizing constant motion is that when a task is completed by one surgeon, that person nearly immediately moves to start, or assist, with another task. With this work we introduce the “hidden” or “buried time concept.” Rather than let other team members scrub out and leave the operating room while microsurgery is being done, we utilize this approach to take back the “hidden or buried time” to reduce the overall length of the operation. In all procedures, the abdomen was closed as much as possible before completion of microsurgery. Having effectively more than one team allows a continued progress without compromise of the ultimate outcome.
Although we believe strongly in the idea that shorter operative times can lead to improvement in results, decreased morbidity, and quicker recovery, we do not focus on efficiency at the expense of aesthetic outcome. In fact, our primary goal is an aesthetic outcome and we believe this is still possible in much reduced operative times. As is displayed in the flow diagrams, instead of walking away after the first microsurgery is completed, the attending involved will routinely perform the aesthetic flap inset, whereas other portions of the procedure are completed by other team members. In modern breast reconstruction, patients seek and often expect superior aesthetic outcomes. Therefore, the inset is the most important portion of the DIEP flap procedure from a patient’s perspective. With a consistent team, including similar experience and aesthetic philosophy, and extensive communication, this can still be accomplished simultaneously to other portions of the procedure without compromise. When two experienced surgeons routinely work together and are capable of setting ego aside to allow suggestions and potential criticisms, it is certainly possible that the aesthetic outcome is improved and not jeopardized as one might assume with an extremely efficient operative time.
We are not advocating this as an assembly line operative management of DIEP flap breast reconstruction. Instead, we provide an engineered approach for the vascular components, the artistic inset components, as well as the logistical and operational components that make breast reconstruction with DIEP flaps viable. Others evaluated the DIEP flap as a 100-step procedure.1 This is incredibly detailed, and while useful, we find this difficult to implement and track. We have therefore, categorized portions of DIEP flap breast reconstruction and divided each category into a few individual steps, which in our mind simplifies our process analysis.
This report accounts for a four-member team, but there are scenarios where we perform this same operation with a three-member or even a two-member team. Certainly, in other practices, this may also be the norm. The modeling would be different in these approaches but ultimately requires an optimal usage of the individual skills balanced with the lead surgeon, or surgeons, comfort, and experience. The goal is to create synergies and use each individual to their fullest capability while providing a safe and superior aesthetic outcome. These levels of efficiency are only possible with a team approach. It is also critical to have well-trained operative team. In our practice, we have a core group of approximately eight people that work with us in breast microsurgery. In any given procedure, we typically have one scrub tech and one circulator.
We are still attempting to focus the outcome of surgery that is unique to every patient and delivering a personal and individualized result. This model allows for creativity and continued innovation. What we are attempting, and hopefully have shown, is efficient time allocation and skill disbursement toward providing a unique result for a patient, all the while still routinely providing complex options ranging from stacked flaps,22–24 four flaps,25 double-pedicle DIEPs,26 dual-flow flaps, profunda artery perforator flaps,27,28 and lumbar artery perforator flaps.29,30 We do not cut corners or focus on speed directly as an end to itself, but instead advocate for avoiding wasted movement and encourage constant progress balanced by educating the next generation of plastic surgeons in an academic setting.
CONCLUSIONS
Efficient bilateral DIEP flap breast reconstruction can be accomplished with a well-trained and coordinated team approach involving like-minded surgeons with extensive experience working together. The synergistic map shows constant movement with utilization of hidden time, without sacrificing education, patient outcomes, or innovation.
ACKNOWLEDGMENT
Evan Garfein, MD: Dr. Garfein has provided much inspiration for our process analysis and exposed us to Anders Ericsson’s concept of deliberate practice. Kabrina Ishmael CST, Erica Donker, RN, Abby Weaver, RN Soni Matthews, RN and Regina Smith, RN: Our surgical team played a critical role in routinely documenting intraoperative details and improving surgical flow.
Footnotes
Published online 7 September 2021.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Sharma HR, Rozen WM, Mathur B, et al. 100 steps of a DIEP flap-A prospective comparative cohort series demonstrating the successful implementation of process mapping in microsurgery. Plast Reconstr Surg Glob Open. 2019;7:e2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Canizares O, Mayo J, Soto E, et al. Optimizing efficiency in deep inferior epigastric perforator flap breast reconstruction. Ann Plast Surg. 2015;75:186–192. [DOI] [PubMed] [Google Scholar]
- 3.Lee BT, Tobias AM, Yueh JH, et al. Design and impact of an intraoperative pathway: a new operating room model for team-based practice. J Am Coll Surg. 2008;207:865–873. [DOI] [PubMed] [Google Scholar]
- 4.Hembd A, Teotia SS, Zhu H, et al. Optimizing perforator selection: a multivariable analysis of predictors for fat necrosis and abdominal morbidity in DIEP flap breast reconstruction. Plast Reconstr Surg. 2018;142:583–592. [DOI] [PubMed] [Google Scholar]
- 5.Cho MJ, Teotia SS, Haddock NT. Predictors, classification, and management of umbilical complications in DIEP flap breast reconstruction. Plast Reconstr Surg. 2017;140:11–18. [DOI] [PubMed] [Google Scholar]
- 6.Haddock NT, Teotia SS. Deconstructing the reconstruction: evaluation of process and efficiency in deep inferior epigastric perforator flaps. Plast Reconstr Surg. 2020;145:717e–724e. [DOI] [PubMed] [Google Scholar]
- 7.Haddock NT, Teotia SS. Five steps to internal mammary vessel preparation in less than 15 minutes. Plast Reconstr Surg. 2017;140:884–886. [DOI] [PubMed] [Google Scholar]
- 8.Haddock NT, Dumestre DO, Teotia SS. Efficiency in DIEP flap breast reconstruction: the real benefit of computed tomographic angiography imaging. Plast Reconstr Surg. 2020;146:719–723. [DOI] [PubMed] [Google Scholar]
- 9.Buchel E. How to simplify the DIEP flap and optimize or efficiency. Paper presented at: Breast Reconstruction: State of the Art 2019. November 23, 2019; New York, NY. [Google Scholar]
- 10.Berger AJ, Gaster RS, Lee GK. Development of an affordable system for personalized video-documented surgical skill analysis for surgical residency training. Ann Plast Surg. 2013;70:442–446. [DOI] [PubMed] [Google Scholar]
- 11.Cho MJ, Teotia SS, Haddock NT. Classification and management of donor-site wound complications in the profunda artery perforator flap for breast reconstruction. J Reconstr Microsurg. 2020;36:110–115. [DOI] [PubMed] [Google Scholar]
- 12.Haddock NT, Kayfan S, Pezeshk RA, et al. Co-surgeons in breast reconstructive microsurgery: what do they bring to the table? Microsurgery. 2018;38:14–20. [DOI] [PubMed] [Google Scholar]
- 13.Harris PA, Taylor R, Minor BL, et al. ; REDCap Consortium. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hembd AS, Yan J, Zhu H, et al. Intraoperative assessment of DIEP flap breast reconstruction using indocyanine green angiography: reduction of fat necrosis, resection volumes, and postoperative surveillance. Plast Reconstr Surg. 2020;146:1e–10e. [DOI] [PubMed] [Google Scholar]
- 16.Haddock NT, Culver AJ, Teotia SS. Abdominal weakness, bulge, or hernia after DIEP flaps: an algorithm of management, prevention, and surgical repair with classification. J Plast Reconstr Aesthet Surg. 2020. (E-pub ahead of print). [DOI] [PubMed] [Google Scholar]
- 17.Ericsson KA. Acquisition and maintenance of medical expertise: a perspective from the expert-performance approach with deliberate practice. Acad Med. 2015;90:1471–1486. [DOI] [PubMed] [Google Scholar]
- 18.Garfein ES. Discussion on deliberate pracrtice and mental representations. In: Haddock N, ed. 2020. (Personal Communication).
- 19.Chen AD, Kamali P, Chattha AS, et al. The national surgical quality improvement program 30-day challenge: microsurgical breast reconstruction outcomes reporting reliability. Plast Reconstr Surg Glob Open. 2018;6:e1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Daar D, Salibian A, Frey J, et al. Reply: flap inset and tailoring are critical steps in process-mapping DIEP flap breast reconstruction. Plast Reconstr Surg. 2021;147:559e–560e. [DOI] [PubMed] [Google Scholar]
- 21.Pannucci CJ, Basta MN, Kovach SJ, et al. Loupes-only microsurgery is a safe alternative to the operating microscope: an analysis of 1,649 consecutive free flap breast reconstructions. J Reconstr Microsurg. 2015;31:636–642. [DOI] [PubMed] [Google Scholar]
- 22.Haddock NT, Cho MJ, Gassman A, et al. Stacked profunda artery perforator flap for breast reconstruction in failed or unavailable deep inferior epigastric perforator flap. Plast Reconstr Surg. 2019;143:488e–494e. [DOI] [PubMed] [Google Scholar]
- 23.Teotia SS, Cho MJ, Haddock NT. Salvaging breast reconstruction: profunda artery perforator flaps using thoracodorsal vessels. Plast Reconstr Surg Glob Open. 2018;6:e1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haddock NT, Cho MJ, Teotia SS. Comparative analysis of single versus stacked free flap breast reconstruction: a single-center experience. Plast Reconstr Surg. 2019;144:369e–377e. [DOI] [PubMed] [Google Scholar]
- 25.Haddock N, Suszynski TM, Teotia S. Consecutive bilateral stacked breast reconstruction using abdominally-based and posterior thigh free flaps. Plast Reconstr Surg. 2020. [DOI] [PubMed] [Google Scholar]
- 26.Cho MJ, Haddock NT, Teotia SS. Clinical decision making using CTA in conjoined, bipedicled DIEP and SIEA for unilateral breast reconstruction. J Reconstr Microsurg. 2020;36:241–246. [DOI] [PubMed] [Google Scholar]
- 27.Haddock NT, Gassman A, Cho MJ, et al. 101 consecutive profunda artery perforator flaps in breast reconstruction: lessons learned with our early experience. Plast Reconstr Surg. 2017;140:229–239. [DOI] [PubMed] [Google Scholar]
- 28.Haddock NT, Teotia SS. Consecutive 265 profunda artery perforator flaps: refinements, satisfaction, and functional outcomes. Plast Reconstr Surg Glob Open. 2020;8:e2682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Haddock N, Teotia S. Lumbar artery perforator flap: video surgical sequence. Plast Reconstr Surg Glob Open. 2020;8:e2680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haddock NT, Teotia SS. Lumbar artery perforator flap: initial experience with simultaneous bilateral flaps for breast reconstruction. Plast Reconstr Surg Glob Open. 2020;8:e2800. [DOI] [PMC free article] [PubMed] [Google Scholar]