This editorial refers to ‘Association between adiposity and cardiovascular outcomes: an umbrella review and meta-analysis of observational and Mendelian randomization studies’, by M.S. Kim et al., doi:10.1093/eurheartj/ehab454.
During the last decades of the 20th century and up to now the human phenotype has undergone a rapid change from being predominantly normal weight or underweight to an increasing and large proportion being overweight or obese.1,2 These massive changes over a comparatively short period are probably mostly driven by changes in the global food system, with more processed, affordable, and effectively marketed food than ever before, together with automation of many jobs and more motorized transport.3 It has been claimed that body mass index (BMI) would need to revert to what it was in the 1980s in order to prevent unsustainable health consequences4 but, so far, public health efforts to monitor and control population weight have been inadequate almost everywhere. Although underweight still poses a major public health problem, which may potentially be increasing in response to the economic consequences of the ongoing coronavirus disease 2019 (COVID-19) pandemic, the number of people globally with obesity is unprecedented in human history. Currently, the prevalence of obesity globally has surpassed that of underweight in both men and women, and, in 2014, 2.3% of men and 5.0% of women were severely obese, with a BMI of 35 kg/m2 or higher.1 In particular, the increasing proportion with obesity and severe obesity in adolescence and youth, and/or massive weight gain over adult life, will probably have marked consequences for future population health, resulting in a potential surge of cardiometabolic disorders worldwide.
Roughly a third of all deaths globally are due to cardiovascular disease (CVD). In the large Prospective Urban Rural Epidemiology (PURE) study5 that examined modifiable risk factors for a composite of cardiovascular death, myocardial infarction, stroke, and heart failure, abdominal obesity, present in about half of the 155 722 participants from 21 countries displayed an adjusted hazard ratio of 1.26 (95% confidence interval 1.18–1.34), implying a relatively modest effect. This effect, however, will have been attenuated by adjustment for several other factors that, in turn, are part of the causal chain leading to obesity, such as hypertension and diabetes. Additionally, findings from composite outcomes may be difficult to interpret because their separate components, for example heart failure and coronary heart disease, have not only different pathophysiology, but also different risk factor patterns. As an example, despite the fact that LDL cholesterol has a strong causal effect with respect to coronary heart disease, which, in turn, is one of the most important risk factors for heart failure, LDL cholesterol seems to play little or no role as a risk factor for heart failure.6 Elevated non-fasting triglyceride concentration, on the other hand, linearly associated with BMI, was shown to be a very strong risk factor for future heart failure. Accordingly, variations in effect sizes for various risk factors on specific cardiovascular disorders is of major interest in the understanding of trends in CVD mortality and incidence in response to changes in risk factors.
Because of the multiple studies investigating overweight and obesity in relation to various cardiovascular disorders, which in turn have different risk factor patterns, it is difficult to discern exactly which role elevated body weight plays in separate outcomes, particularly given the huge number of individual studies on the subject. Systematic reviews and meta-analyses, collecting and evaluating associations between obesity-related indices and CVD risk, have been published, but it is still difficult to obtain an overview of effect sizes and reliability of the information provided on the association between overweight and obesity in relation to cardiovascular outcomes. Aggregating data in meta-analyses has been done multiple times, but usually only for a single outcome, or a limited number only.
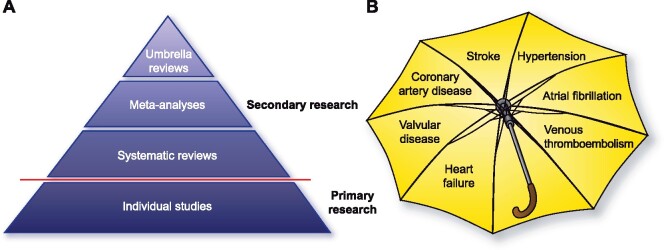
An umbrella review uses previously published reviews and meta-analyses on exposures and clinical outcomes, synthesizing them according to a pre-defined protocol, involving extensive statistical replication and updating of the previous meta-analyses (Graphical Abstract). One strength of the umbrella review is that it assesses multiple biases for relevant outcomes as well as the stratification of findings into distinct levels of evidence. A multitude of umbrella reviews have been carried out over the last few years covering widely varying clinical disorders; however, none so far on obesity and multiple cardiovascular outcomes. In their study published in this issue of the European Heart Journal, Kim et al.7 conducted an umbrella review of 12 systematic reviews, where they identified 53 results from meta-analyses from altogether 501 cohorts, and 12 Mendelian randomization (MR) studies.
Graphical Abstract.
Schematic representation of hierarchy of scientific evidence (left) and of the umbrella review by M.S. Kim et al. (right).
Observational epidemiological studies suffer from many potential biases, including confounding and reverse causation. This limits their ability to identify causal associations. Because data from long-term randomized controlled trials of interventions against overweight and obesity are rare or non-existent, and only available in selected populations, causality between elevated indices of body weight and outcomes is difficult to establish. As a novel feature of this study, the authors incorporated MR studies into the body of evidence from observational studies.
MR refers to the use of genetic variants as a proxy for environmentally modifiable exposures and can be implemented within observational epidemiological studies. The method can be considered as analogous to randomized controlled trials.8 In this instance, genetically predicted higher BMI and central adiposity can be regarded as randomly distributed with potential confounders equally distributed, and therefore there will be no need to consider reverse causation, which is particularly relevant with respect to obesity. For example, a J-shaped or U-shaped relationship between adiposity and outcomes is common, particularly in older and sicker populations, reflecting the influence of ageing and disease on body weight, and not that a higher weight in itself is protective.
This is the first umbrella review on the topic of obesity and several types of fatal and incident cardiovascular outcomes, in this case hypertension, stroke, atrial fibrillation, venous thrombo-embolism, heart failure, valvular disease, and coronary heart disease. The authors performed a search for systematic reviews and meta-analyses of observational and MR studies that were published up to January 2021; the former in order to estimate the size of the effect and the latter to determine evidence of causality. About half of the associations were supported by high-level evidence. Associations were consistent between sexes and across global regions. The evidence level was assessed through MR studies, and graded at four levels (very low, low, moderate, and high). The net results are shown in a graphical abstract.7
The effect size in risk for every 5 kg/m2 increase in incidence varied from 10% increase for haemorrhagic stroke (low evidence) to 49% for hypertension (high evidence). The corresponding effect sizes for heart failure and coronary heart disease (CHD) were 41% and 15%, respectively (both high evidence). Similarly, among conditions with supported moderate or high level causality for obesity (BMI between 30 and 35 kg/m2) were pulmonary embolism, venous thrombo-embolism, atrial fibrillation, as well as CVD and CHD mortality. In the MR studies, the effect size per 1 kg/m2 was 12% for heart failure and 7% for CHD, both with high evidence for causality. Among disorders with low or very low evidence levels for associations and/or weak evidence of causality were all-cause and haemorrhagic stroke, stroke and heart failure mortality, and sudden cardiac death.
Accordingly, with respect to heart disease, collective evidence suggests that rising BMI is a risk factor for both CHD and heart failure, although the evidence concerning the link between categories (overweight, obese, and severely obese) and heart failure was weak. The authors note specifically that these heterogeneous results across adiposity categories complicate the interpretation of the association. Still, many studies will not have included a very large number of severely obese, which is the fastest growing category. Also, only adults were studied; we know from studies of very large populations of adolescents undergoing medical evaluation before military service that the increase in risk for several outcomes associated with rising BMI is much steeper than that usually seen for adults.9,10
The massive work undertaken in the study by Kim et al. is of particular interest for our understanding of current trends in heart disease incidence, and potentially also of what to expect in the future when increasing numbers of overweight, obese, and severely obese people who are now young or adolescent become middle aged and older. In a recent study from the USA, heart failure and hypertensive heart disease accounted for major increases in premature deaths and offset declines in ischaemic heart disease mortality.11 Similarly, in Sweden, a shift in young-onset CVD events (before the age of 40) in men demonstrated a marked shift from incident acute myocardial infarction to incident heart failure.12 The much lower effect size by continuous BMI on CHD relative to that of heart failure could help explain these emerging trends and provide some indication of what might happen in the future when heart failure, already a huge global issue in the elderly, will be likely to surpass acute myocardial infarction as a major problem also among the young and middle-aged.
Funding
A.R. acknowledges support from the Swedish Research Council [2018-02527, VRREG 2019-00193], the Swedish Heart and Lung Foundation, and AFA Insurance.
Conflict of interest: none declared.
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.
References
- 1.NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet 2016;387:1377–1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017;390:2627–2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, Gortmaker SL.. The global obesity pandemic: shaped by global drivers and local environments. Lancet 2011;378:804–814. [DOI] [PubMed] [Google Scholar]
- 4.McPherson K.Reducing the global prevalence of overweight and obesity. Lancet 2014;384:728–730. [DOI] [PubMed] [Google Scholar]
- 5.Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, Brauer M, Kutty VR, Gupta R, Wielgosz A, AlHabib KF, Dans A, Lopez-Jaramillo P, Avezum A, Lanas F, Oguz A, Kruger IM, Diaz R, Yusoff K, Mony P, Chifamba J, Yeates K, Kelishadi R, Yusufali A, Khatib R, Rahman O, Zatonska K, Iqbal R, Wei L, Bo H, Rosengren A, Kaur M, Mohan V, Lear SA, Teo KK, Leong D, O’Donnell M, McKee M, Dagenais G.. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet 2020;395:795–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Varbo A, Nordestgaard BG.. Nonfasting triglycerides, low-density lipoprotein cholesterol, and heart failure risk: two cohort studies of 113 554 individuals. Arterioscler Thromb Vasc Biol 2018;38:464–472. [DOI] [PubMed] [Google Scholar]
- 7.Kim MS, Kim WJ, Khera AV, Kim JY, Yon DK, Lee SW, Shin JI, Won HH.. Association between adiposity and cardiovascular outcomes: an umbrella review and meta-analysis of observational and Mendelian randomization studies. Eur Heart J 2021;42:3388–3403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lawlor DA, Harbord RM, Sterne JA, Timpson N, Davey Smith G.. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med 2008;27:1133–1163. [DOI] [PubMed] [Google Scholar]
- 9.Twig G, Yaniv G, Levine H, Leiba A, Goldberger N, Derazne E, Ben-Ami Shor D, Tzur D, Afek A, Shamiss A, Haklai Z, Kark JD.. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N Engl J Med 2016;374:2430–2440. [DOI] [PubMed] [Google Scholar]
- 10.Rosengren A, Åberg M, Robertson J, Waern M, Schaufelberger M, Kuhn G, Åberg D, Schiöler L, Torén K.. Body weight in adolescence and long-term risk of early heart failure in adulthood among men in Sweden. Eur Heart J 2017;38:1926–1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shah NS, Molsberry R, Rana JS, Sidney S, Capewell S, O’Flaherty M, Carnethon M, Lloyd-Jones DM, Khan SS.. Heterogeneous trends in burden of heart disease mortality by subtypes in the United States, 1999–2018: observational analysis of vital statistics. BMJ 2020;370:m2688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Åberg ND, Adiels M, Lindgren M, Nyberg J, Georg Kuhn H, Robertson J, Schaufelberger M, Sattar N, Åberg M, Rosengren A.. Diverging trends for onset of acute myocardial infarction, heart failure, stroke and mortality in young males: role of changes in obesity and fitness. J Intern Med 2021;doi: 10.1111/joim.13285. [DOI] [PubMed] [Google Scholar]