Abstract
The potential mental health consequences of the coronavirus disease 2019 (COVID-19) pandemic are widely acknowledged; however, limited research exists regarding the nature and patterns of stress responses to COVID-19-related potentially traumatic events (PTEs) and the convergence/divergence with responses to other (non-COVID-19-related) PTEs. Network analysis can provide a useful method for evaluating and comparing these symptom structures. The present study includes 7034 participants from 86 countries who reported on mental health symptoms associated with either a COVID-19-related PTE (n = 1838) or other PTE (n = 5196). Using network analysis, we compared the centrality and connections of symptoms within and between each group. Overall, results show that the COVID-19-related network includes transdiagnostic symptom associations similar to networks tied to PTEs unrelated to the pandemic. Findings provide evidence for a shared centrality of depression across networks and theoretically consistent connections between symptoms. Network differences included stronger connections between avoidance-derealization and hypervigilance-depression in the COVID-19 network. Present findings support the conceptualization of psychological responses to pandemic-related PTEs as a network of highly interconnected symptoms and support the use of a transdiagnostic approach to the assessment and treatment of mental health challenges related to the COVID-19 pandemic.
Keywords: COVID-19, Global mental health, Stress responses, Network analysis
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic represents a potentially traumatic event (PTE) that is, in many ways, unique from other large-scale stressors. Specifically, the current pandemic is both a personally impactful event, shaped by numerous individual factors (e.g., economic and social resources, occupation, age, and health status) and a globally shared experience. In addition to the prolonged physical threats related to the virus, the potential for secondary traumatic and stressful events stemming from pandemic-related circumstances, such as lockdown measures, is far-reaching (e.g., heightened levels of intimate partner violence (Ertan et al., 2020, Usher et al., 2020), poverty (Laborde, Martin, Swinnen, & Vos, 2020), and separation from hospitalized family members (Montauk & Kuhl, 2020)). Importantly, these threats, including the direct health risks, are ongoing and without a determinable ending, creating the potential for psychological reactions to the anticipation of a stressor, in addition to past or current stressful events (Horesh & Brown, 2020).
The mental health consequences of the pandemic are becoming increasingly well-documented in scientific literature and include symptoms of anxiety, depression, insomnia, trauma-related symptoms, and substance use (Rajkumar, 2020, Xiong et al., 2020). Recent research has also provided evidence of a COVID Stress Syndrome ( Taylor et al., 2020b, Taylor et al., 2020c), which includes five domains of distress tied specifically to COVID-19: fears related to contamination, fears related to economic consequences, xenophobic fears about foreigners spreading the virus, compulsive checking and reassurance seeking, and traumatic stress symptoms. In addition to distress related to specific traumatic or stressful events, psychological reactions to the pandemic can include both over- and under-responses (excessive fear and downplaying the seriousness of COVID-19, respectively) that can lead to similarly maladaptive behaviors such as excessive avoidance and disregard for social distancing, respectively (Taylor, Landry, Paluszek, & Asmundson, 2020a). The observed mental health consequences of the COVID-19 pandemic are supported by research from prior mass trauma events, including the SARS outbreak, and might develop into chronic conditions (Ko et al., 2006, Lam et al., 2009, Mak et al., 2010, McAlonan et al., 2007, Wu et al., 2009). While it is evident that the pandemic has caused and continues to cause significant mental health issues, the underlying patterns and connections between symptoms requires additional evaluation and replication. Furthermore, given the unique qualities of the COVID-19 pandemic, it is unclear if/how the psychological reactions to this PTE may differ from PTEs unrelated to the pandemic.
One promising method for assessing symptom-level connections is through network analysis. This method represents an alternative to the latent variable approach (i.e., symptoms contribute equally and independently to an underlying disorder) and positions psychopathology as a network of symptoms (nodes) with causal links (edges) between them. Within a network, certain symptoms may be more or less central to the overall presentation and may activate each other to different degrees and in different ways (Borsboom, 2008, Borsboom, 2017, McNally et al., 2015). Although most frequently used with cross-sectional data, which does not allow for inferences about causal links between symptoms, researchers have advocated for the use of the network approach for the study of psychopathology (Fried, 2015), noting its implicit appreciation for the interdependent nature of psychological processes.
Network analysis has become especially prominent in the field of traumatic stress and has been used in numerous studies to map the symptom structure and assess cross-cluster connections of PTSD, as well as compare networks tied to different PTEs (Armour et al., 2017, Weems, 2020). Synthesized findings have noted inconsistency of both the centrality of symptoms and symptom associations and suggest that this may support an idiographic approach to the network structure of PTSD based on particular populations (Birkeland et al., 2020, Isvoranu et al., 2020). For example, in a comparison of different PTE networks, the sexual assault network showed the most consistency with the DSM-5 symptom clusters, while the sudden accidental or violent death network appeared theoretically inconsistent (conceptually related symptoms were negatively associated, and clusters were not clearly retained; Benfer et al., 2018). Separate studies have found that among earthquake survivors, re-experiencing and arousal symptoms were most central (McNally et al., 2014), whereas among survivors of mass shootings, intrusive thoughts, anger, and feeling detached were most central (Sullivan, Smith, Lewis, & Jones, 2018). Given the uniqueness of the pandemic as a global stressor and the range of stress-inducing events, which may or may not reflect Criteria A specifications (Asmundson & Taylor, 2021), it is possible that symptom networks may differ from PTEs unrelated to an ongoing global crisis.
Several recent studies have applied network analysis to psychological responses to COVID-19. Specifically, within a sample of recovered COVID-19 patients in China, networks were estimated containing COVID-19-related variables (e.g., illness severity) and symptoms of anxiety, depression, and PTSD (Liu, Epskamp, & Isvoranu, 2020). In this study, severity of illness was associated with nervousness and the inability to relax in the anxiety-focused network, anhedonia and reduced energy in the depression-focused network, and sleep difficulties in the PTSD-focused network. More recently, Taylor, Landry, Paluszek, Rachor, and Asmundson (2020d) used network analysis to examine connections between the five domains of COVID-19-related distress identified in the COVID Stress Scales (Taylor et al., 2020b), as well as minimizing and conspiratorial beliefs about COVID-19, and engagement in or disregard for safety and prosocial behaviors. Worry related to the dangerousness of the virus was central to the network and closely connected to compulsive checking and reassurance seeking, which was, in turn, connected to re-experiencing symptoms (Taylor, Landry, Paluszek, Rachor, & Asmundson, 2020). In a subsequent network analysis including substance use in a network of COVID-19-related distress and disregard for social distancing, both alcohol and drug abuse were closely related to traumatic stress symptoms tied to COVID-19 (Taylor, Paluszek, Rachor, McKay, & Asmundson, 2021). In addition to further highlighting the mental health impacts of the pandemic, the latter two studies demonstrate the implications of these psychological responses for engagement in harmful behaviors and attitudes, such as panic buying, anti-science beliefs, non-compliance with safety precautions (e.g., social distancing), and stigmatization of health care workers and foreigners.
The present research used network analysis to explore the underlying transdiagnostic symptom network resulting from PTEs identified as being related to COVID-19 and compare the network to that of PTEs unrelated to the pandemic. COVID-19-relatedness represents a number of risk factors for prolonged and more severe events, which may result in potential differences between PTEs identified as being related versus unrelated to the pandemic. For example, in the case of abuse experienced in relationships, COVID-19 can be used as a means of coercive control, including partners providing misinformation about lockdown measures and using fear of contagion to increase isolation and deter their partners from seeking medical or other support (Usher et al., 2020). Some have argued that experiencing the COVID-19 pandemic (independent of contracting the virus) represents a PTE in itself (Karatzias et al., 2020, Shevlin et al., 2020). From this perspective, experiencing an event that is also related to COVID-19 may represent a compounding burden. However, it may also be the case that because the events are in essence the same, responses would be parallel (e.g., the unexpected death of a loved one would be experienced similarly whether it was due to COVID-19 or not). Given the uniqueness of PTEs related to the pandemic and limited research on the topic, the authors have no prior hypotheses as to how this symptom network may compare to PTEs with no reported connection to COVID-19. This study used the Global Psychotrauma Screen (GPS) to assess trauma-related symptoms among those reporting either a COVID-19-related PTE or a non-COVID-19-related (Other) PTE from a geographically diverse sample.
2. Method
2.1. Participants and procedure
Seven thousand thirty-four individuals (74.00% female-identifying) from around the world were recruited through online advertising by members of the GC-TS. Data was collected from April 25, 2020 to November 30, 2020. Nonprobability sampling of the general population was used to maximize participation worldwide. Participation was voluntary and no financial or material compensation was offered. The short online study was offered in 21 languages and open to anyone 16 years or older (14 respondents were excluded for not meeting this criteria) who reported experiencing a “difficult or frightening event”. Participants ranged in age from 16 to 100 years old (Mage = 38.46, SDage = 14.36).
2.2. Measures
Participants were presented with the following prompt, “Sometimes things happen to people that are unusually or especially frightening, horrible, or traumatic. This can be Corona virus (COVID-19) related events, or other events such as a serious accident or fire, physical or sexual assault or abuse, earthquake or flood, war [.]” And asked to think of a “difficult or frightening event” that they have experienced. Participants were then asked if their event was related to COVID-19. After making this specification, additional information about the event (nature of event, time since event, whether it was job-related) was collected prior to completion of the GPS. More specifically, participants indicated whether their identified PTE involved physical violence, sexual violence, emotional abuse, serious injury, life-threat, sudden death of a loved one, and/or causing harm to someone. Demographic information (age, identified gender, and country of residence) was also collected prior to completion of the GPS.
2.2.1. Global Psychotrauma Screen (GPS)
The GPS is a self-report measure consisting of 22 yes/no items (included in the Supplemental Material) and available in 21 languages (Frewen et al., 2021, Oe et al., 2020, Olff et al., 2020, Rossi et al., 2021). After identifying a PTE, participants are asked to consider the identified event and report whether or not they have experienced 17 psychological symptoms within the past month; symptoms can be categorized into subdomains relating to PTSD, complex PTSD, anxiety, depression, insomnia, self-harm, dissociation, substance use, and other stress-related problems. The five remaining items relate to risk/resilience factors: lack of support, psychiatric history, other stressful events, childhood trauma, and resilience; these five items were not included in the network analysis.
2.3. Data analysis
R code for all analyses is provided in the Supplemental Material. Missing data for age (2.0%), onset of the event (5.3%), work-relatedness of the event (14.7%) and trauma frequency (18.2%) was imputed using R package Missforest (normalized root mean squared error = 0.33 and proportion of falsely classified entries = 0.11; Stekhoven & Bühlmann, 2012). Participants were divided into two groups: those who identified their most stressful experience as being related to the COVID-19 pandemic (n = 1838), and those whose most stressful experience was reported as being unrelated to the pandemic (n = 5196). Due to the low endorsement of self-harm, we excluded this item from the network analysis to decrease the likelihood of estimation errors.
2.3.1. Network analysis and comparison test
Simulation studies provide guidance on appropriate sample sizes for network estimation using binary data and suggest that for networks including up to 30 nodes, a sample size of 500 is typically acceptable (van Borkulo et al., 2014). Both networks estimated in the current study, each containing 16 nodes, are based on samples well above this recommendation.
Networks were estimated with eLasso using the IsingFit package in R version 4.0.3 (van Borkulo & Epskamp, 2016), which generates maximally sparse networks by reducing potentially spurious associations to zero. This method uses Extended Bayesian Information Criterion (EBIC) for model selection and is appropriate for binary data. In the estimated networks, nodes represent symptom items on the GPS and edges indicate the magnitude of the association (logistic regression coefficient) between every pair of items, controlling for the associations with all other items. Weighting of edges in the network plot corresponds to the strength of each pairwise association. To estimate the differing interconnectedness of nodes and determine their communities, we used the walktrap algorithm (Pons & Latapy, 2005) in the igraph R package (Csardi & Nepusz, 2006). This community analysis is not intended to reduce the dimensionality of the data, rather to provide a visual aid for highlighting closely connected nodes.
Node centrality for both networks were estimated using three indices: strength (each node’s direct connections to other nodes in the network, calculated by summing the absolute values of the node’s edges), closeness (the extent to which information from each node passes through the rest of the network, calculated from the inverse of the sum of all shortest paths between each node and all other nodes), and betweenness (each node’s ability to control/alter the flow between other nodes in the network, calculated by summing the number of times the node appears on the shortest path).
The accuracy of the estimated networks was evaluated in two ways. The stability of edge weights in each network was assessed by computing non-parametric bootstrapped confidence intervals and observing the differences in strength between samples (bootnet R package) (Epskamp, Borsboom, & Fried, 2018). To assess the stability of the centrality indices, we used the correlation stability coefficient (CS-coefficient), which indicates the proportion of cases that can be dropped while maintaining at least a .7 correlation between the centrality indices of the full sample and those of the subsamples. Interpretation of centrality indices with a CS-coefficient of less than .25 is not recommended (Epskamp et al., 2018).
Lastly, quantitative comparisons of the two networks were completed using the Network Comparison Test (NCT; van Borkulo, Boschloo, Kossakowski, & Tio, 2017). NCT is an invariance test of global strength (overall degree of connectivity), network structure (distribution of edge weights), and edge strength (strength of connections between specific node pairs). There is evidence to suggest that using the NCT with groups of different sample sizes results in a loss of power (van Borkulo et al., 2017). As a follow up to the NCT results of the current study, we calculated 10 bootstrapped subsamples of the larger (Other) group with sample size equal to the smaller (COVID-19) group and present the averaged invariance statistics and p values.
3. Results
3.1. Descriptive statistics
Characteristics of the two PTE groups, including frequencies of item endorsement, are presented in Table 1. The types of trauma reported by each group are reported in Table 2. Both groups included a disproportionately higher number of female-identified participants, which mirrors gender differences observed in prevalence rates of trauma exposure. 482 (26.22%) of the COVID-19-related group and 1756 (33.80%) of the Other (non-COVID-19-related) group reported having received a psychiatric diagnosis or been treated for psychological problems. The recency of the reported PTE differed substantially between groups; not surprisingly, the COVID-19-related PTEs were more recent (80.09% occurring within the past 12 months) than the Other group (35.01% occurring within the past 12 months); additionally, a higher proportion of COVID-19-related events were identified as work-related (34.33% compared to 29.54%).
Table 1.
Characteristics and Symptom Frequencies of PTE Group (COVID-19-related and Other).
| Variable | COVID-19 (n = 1838) | Other (n = 5196) |
|---|---|---|
| Age | 39.65 (15.15) | 38.04 (14.05) |
| Gender (Female) | 1345 (73.18) | 3863 (74.35) |
| Psychiatric History (Yes) | 482 (26.22) | 1756 (33.80) |
| UN Region | ||
| Africa | 94 (5.52) | 174 (3.44) |
| Latin America and Caribbean | 334 (18.62) | 496 (9.82) |
| North America | 118 (6.58) | 399 (7.90) |
| Eastern Asia | 164 (9.14) | 460 (9.10) |
| South-Eastern Asia | 270(15.05) | 234 (4.63) |
| Southern Asia | 64 (3.57) | 106 (2.10) |
| Western Asia | 194 (10.81) | 513 (10.15) |
| Eastern Europe | 133 (7.41) | 612 (12.11) |
| Northern Europe | 24 (1.34) | 213 (4.22) |
| Southern Europe | 194 (10.81) | 859 (17.00) |
| Western Europe | 185 (10.31) | 890 (17.61) |
| Australia and New Zealand | 20 (1.11) | 97 (1.92) |
| GPS symptoms (endorsed) | ||
| Nightmares | 854 (46.46) | 2348 (45.19) |
| Avoidance | 1037 (56.42) | 2781 (53.52) |
| Hypervigilance | 1083 (58.92) | 2288 (44.03) |
| Numbing | 943 (51.31) | 2375 (45.71) |
| Guilt | 722 (39.28) | 2319 (44.63) |
| Worthlessness | 769 (41.84) | 2243 (44.17) |
| Anger | 682 (37.11) | 1923 (37.01) |
| Anxiety | 1365 (74.27) | 3476 (66.90) |
| Worry | 1068 (58.11) | 2672 (51.42) |
| Depression | 1154 (62.79) | 3072 (59.12) |
| Anhedonia | 1072 (58.32) | 2638 (50.77) |
| Insomnia | 1037 (58.42) | 2778 (53.46) |
| Self-harm | 133 (7.24) | 481 (9.26) |
| Derealization | 630 (34.28) | 1346 (25.90) |
| Depersonalization | 278 (15.13) | 856 (16.47) |
| Substance use | 473 (25.73) | 1529 (29.43) |
| Other problems | 963 (52.39) | 2684 (51.66) |
Note. Age presented as M (SD); all other variables presented as n (%).
Table 2.
Characteristics of Trauma Type by PTE Group (COVID-19-related and Other).
| Variable | COVID-19 (n = 1838) | Other (n = 5196) |
|---|---|---|
| Time since PTE | ||
| Past year | 1472 (80.09) | 1819 (35.01) |
| Work-related | 631 (34.33) | 1535 (29.54) |
| Single event | 1334 (72.58) | 3342 (64.32) |
| Trauma Type | ||
| Physical violence | 427 (23.23) | 1352 (26.02) |
| Sexual violence | 303 (16.49) | 920 (17.71) |
| Emotional abuse | 623 (33.90) | 2178 (41.92) |
| Serious injury | 114 (6.20) | 527 (10.14) |
| Life-threat | 625 (34.00) | 1773 (34.12) |
| Sudden death of loved one | 302 (16.43) | 1149 (22.11) |
| Causing harm | 59 (3.21) | 154 (2.96) |
Note. Presented as n (%). Participants could select multiple trauma types.
3.2. Network estimations
Out of a possible 120 edges, the COVID-19 network contained 87 non-zero positive edges (72.50% density), while the Other network contained 101 non-zero positive edges (84.17% density).
3.2.1. Community detection
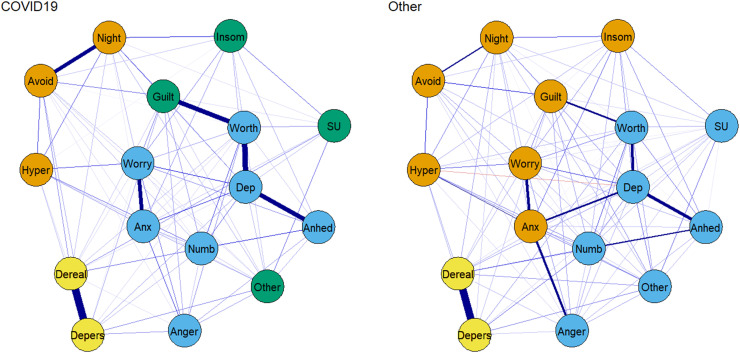
Similar patterns of communities were detected across both networks ( Fig. 1), with some exceptions. Within the Other network, symptoms formed an affective (blue) and an anxiety/arousal (orange) cluster, whereas in the COVID-19 network, hypervigilance, avoidance, and nightmares were less connected to related symptoms (i.e., anxiety and insomnia) and formed their own community. In both networks, the two dissociative symptoms (depersonalization and derealization) formed a distinct community (yellow).
Fig. 1.
Estimated Networks of GPS Symptoms for COVID-19-related and Other PTEs. Note. Edge width and density indicate strength of connections. Node colors represent communities detected in each network. Night – nightmares; Avoid – avoidance; Hyper – hypervigilance; Numb – numbing; Guilt – guilt; Worth – worthlessness; Anger – anger; Anx – anxiety; Worry – worry; Dep – depression; Anhed – anhedonia; Insom – insomnia; Dereal – derealization; Depers – depersonalization; SU – substance use; Other – other physical, emotional or social problems. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3.2.2. Edge strength and accuracy
Edge weights represent the relative strength of connections between symptoms and risk factors in the network; however, the accuracy of the observed ranking of associations can be highly variable. Accuracy tests revealed considerable overlap among CIs for the bootstrapped edge weights in both networks; however, the strongest edge weights remained significantly stronger than the weakest ones. For example, the strongest edge across both networks, derealization – depersonalization was still significantly stronger than all other significant edges in the Other network and 95.35% of the other significant edges in the COVID-19 network; in addition, in the COVID-19 network, depression-anhedonia, depression-worthlessness, guilt-worthlessness, and nightmares-avoidance remained significantly stronger than 88.37% of other significant edges. Edge weight accuracy plots and matrixes comparing significant edge differences are available in the Supplementary materials.
3.2.3. Node centrality
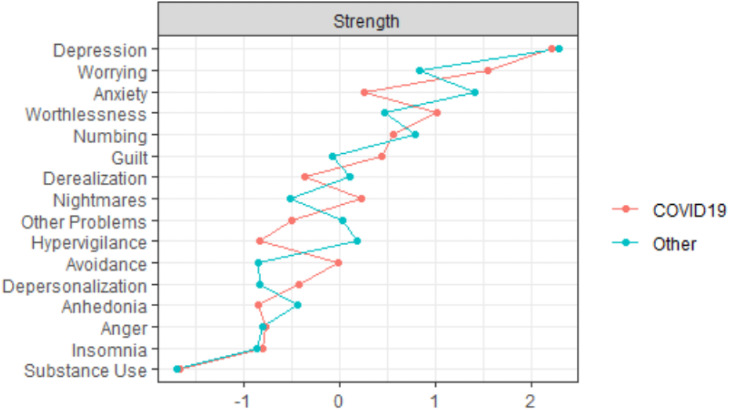
The centrality stability analysis suggested high stability for strength in both the COVID-19 (CS(cor = 0.7) = 0.52) and Other (CS(cor = 0.7) = 0.75) networks. Closeness was stable in the Other network (CS(cor = 0.7) = 0.75), and, to a lesser extent, in the COVID-19 network (CS(cor = 0.7) = 0.36). Betweenness was stable in the Other network (CS(cor = 0.7) = 0.44), but not so in the COVID-19 network (CS(cor = 0.7) = 0.05). These results suggest that inter network comparisons of relative node centrality should be based primarily on strength (centrality stability plots available in the Supplementary material).
Within both the COVID-19 and Other network, depression demonstrated the highest strength centrality, indicating that it has many and/or strong connections to other nodes in the network. Conversely, in both networks, substance use appeared the least central ( Fig. 2).
Fig. 2.
Degree Centrality (strength) of the Two Networks. Note. Centrality indices are plotted using standardized z-scores for interpretability and ordered from highest (top) to lowest (bottom) strength.
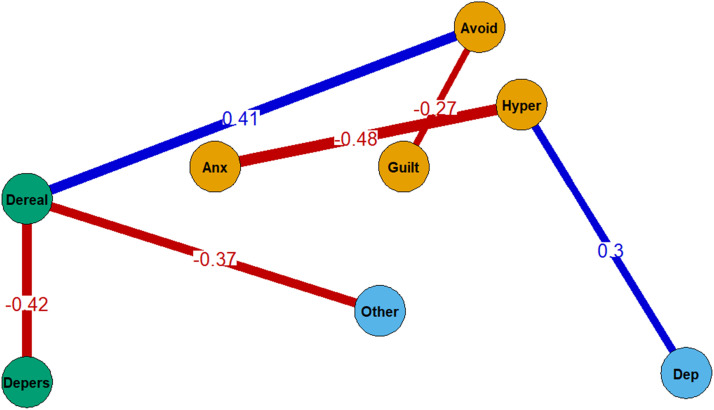
3.3. Network comparisons
Results of the NCT revealed that the global strength (overall level of connectivity) of the Other PTE network was significantly higher than the COVID-19 network (S = 6.12, p < .001); the global structures of the networks (maximum difference in edge weights) was not significantly different (M = 0.48, p = .253). Centrality difference tests suggest that anxiety has significantly higher strength (more/stronger direct connections) within the Other network, compared to the COVID-19 network (p < .001). Six edge weights differed significantly between networks: the connection between avoidance-derealization and hypervigilance-depression was stronger in the COVID-19 network, while hypervigilance-anxiety, avoidance-guilt, derealization-depersonalization, and derealization-other problems were stronger in the Other network ( Fig. 3). The follow-up sensitivity test provided support for the stability of the two invariance metrics: global strength remained significantly different across all the bootstrapped samples (S ave = 3.89 p ave = 0.015) and the difference in global structure reached significance in only 20% of the samples (M ave = 0.61, p ave = 0.193).
Fig. 3.
Edges that Differ Significantly Between the COVID-19 and Other Networks. Note. Values indicate the difference between the edges across networks. Blue lines indicate edges that had a higher value and red lines indicate edges that had a lower value in the COVID-19 network compared to the Other network. Node colors are consistent with community membership in the COVID-19 network. Avoid – avoidance; Hyper – hypervigilance; Anx – anxiety; Dep – depression; Dereal – derealization; Depers – depersonalization; Other – other problems. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
4. Discussion
Understanding the ways in which COVID-19-related traumatic events are similar to and different from PTEs unrelated to COVID-19 is crucial in the development of mental health prevention and intervention efforts. The multilingual GPS provided a rapid and globally accessible screening tool for a range of psychological reactions to PTEs. Network analysis represents an effective approach to mapping the structure of psychopathology and the Network Comparison Test provides a novel analytic method for making direct quantitative comparisons between networks. The results of the present paper are primarily exploratory, serving to expand the literature on mental health symptom networks by including transdiagnostic stress reactions, which provides information about cross-diagnosis symptom interactions and highlights the pathways that activate and maintain psychological distress. More specifically, this research provides the first (to our knowledge) network analysis of mental health responses to COVID-19-related PTEs and offers a preliminary comparison to PTEs identified as being unrelated to the pandemic. Existing research on trauma-related symptom networks highlights the importance of replication and assessment of networks with different samples and in different contexts. The ways in which individuals experience traumatic or stressful events related to the COVID-19 pandemic are still unfolding; however, given the still ongoing and unpredictable nature of COVID-19, it is beneficial to investigate the symptom structure of PTEs perceived as being related to the pandemic, and compare this to PTEs experienced as unrelated to the pandemic. Importantly, the large geographically diverse sample and multilingual symptom measure allows for increased reliability of the estimated network and generalizability of the results.
Findings offer several key takeaways that can be used to improve understanding and inform action related to the mental health consequences of the COVID-19 pandemic. Specifically, depression showed the highest strength centrality in both networks, which highlights the benefit of a transdiagnostic approach (i.e., including symptoms outside of traditional PTSD criteria) to the assessment of PTE-related distress and is consistent with existing research showing negative affect as the most influential symptom in networks containing trauma-related symptoms (Birkeland et al., 2020, Price et al., 2019). As noted by Asmundson and Taylor (2021), research and discussion related to traumatic-stress responses to the pandemic are often conflated with assessments of PTSD, which requires not only specific symptom criteria, but a substantiated index (Criteria A) event. In the present study, although participants’ symptoms are anchored to their reported experience of a "difficult or frightening event" related to the COVID-19 pandemic (or other situation), these PTEs cannot be equated with a Criteria A event. Furthermore, the symptoms assessed represent transdiagnostic stress reactions, not specific PTSD symptom criteria.
Differences in node strength centrality between the two networks was noted for anxiety, which was a more central symptom for the Other PTE group. Importantly, this finding does not indicate that anxiety is more commonly experienced in response to non-COVID-19-related PTEs, rather it suggests that the symptom anxiety has less/weaker direct associations to other symptoms of distress among those experiencing a COVID-19-related PTE. The use of symptom centrality to guide targeted interventions has been challenged in recent years (Bringmann et al., 2019, Spiller et al., 2020). Therefore, it may be most useful to interpret the relative prominence of certain symptoms as one piece in the dynamic structure of each network, with anxiety activating and being activated in different ways in response to different pandemic related/unrelated PTEs.
The edges that could most reliably be considered strongest included the same two symptom connections across networks: depersonalization-derealization and worthlessness-depression, both of which are theoretically consistent. The global strength of the two networks were significantly different, though the stability of these differences should be replicated in other samples. The significant differences in edge weights between networks suggest potential differences in symptom relatedness. Specifically, in the Other network, anxiety was more strongly connected to hypervigilance, avoidance to guilt, and derealization and depersonalization; in the COVID-19 network, derealization had a stronger connection to avoidance and hypervigilance to depression. The reason for (and stability of) these observed differences remains an empirical question; however, it may relate to the relative differences in centrality of anxiety and hypervigilance in the non-pandemic-related PTE group (both symptoms have more/stronger connections in general).
On a broader level, the networks shared several similarities, including comparable communities that reflect logical relationships in terms of item content. The additional fractioning of communities in the COVID-19 network should be interpreted with caution, as it is possible that observed differences are the result of sampling variation, rather than meaningful group differences. The present research provides preliminary insight into the experience of and interplay between psychological reactions to COVID-19-related stressors, as well as potential similarities and differences to PTEs not related to COVID-19. However, there are several limitations that should be addressed in future research. The nature of PTEs within each group are heterogeneous and, therefore, the dichotomized split is a blunt method for comparing the psychological profiles of different trauma types. Specific to the current study, the range of potentially stressful events related to the pandemic is vast and this lack of specificity regarding the nature of the event limits interpretation (Asmundson & Taylor, 2021). Importantly, we cannot be sure of the specific reasons as to why events were identified as COVID-19-related; however, because participants are tying the event to COVID-19, we reason that factors specific to the pandemic (e.g., uncertainty, ongoing reminders, etc.) are playing a role in the interpretation of and reaction to the events. That said, depending on the nature of the event, it may share similarities with existing trauma types; for example, infecting someone else or being unable to provide adequate care to patients may have features similar to a moral injury in other settings (Williamson, Murphy, & Greenberg, 2020), whereas exposure to illness/death in a frontline position may resemble other vicarious trauma experiences. Further investigation is needed with respect to the qualitative aspects of pandemic-related traumas to better understand the nature and nuances of psychological responses to such an extraordinary global event. Moreover, it is important to acknowledge the high prevalence of polytrauma histories among trauma-exposed individuals. Isolating and classifying traumas is not always realistic and does not account for the additive and interactive effects of other PTEs, which can impact symptom presentation. An additional limitation of the present study is the between-group differences, which may impact the networks: participants reporting a COVID-19-related PTE differed from participants reporting a non-pandemic related PTE on several aspects including trauma characteristics (recency of the trauma and work relatedness of the trauma) and demographics (age). Since some of these characteristics might change over time (e.g. COVID-19-related events might become “less recent”), replication of the current results is important. Cross-sectional data does not allow for inferences related to the direction of symptom edges. Additionally, as noted in Benfer et al. (2018), the regularization procedures used in network analysis to account for multiple testing can result in the exclusion of true connections, which may limit the accuracy of the estimated networks (Benfer et al., 2018). Lastly, online research limits participation to those with internet access, leading to the exclusion of vulnerable groups.
Despite these limitations, the current study is the first to assess the network of transdiagnostic stress symptoms in response to COVID-19 and to provide a direct comparison with other PTEs in a global sample. Results can support subsequent research on the psychological consequences of the pandemic and may help inform prevention and treatment efforts. Consistent with previous studies, findings suggest that depression plays a prominent role in psychological reactions to stressful events and changes to this symptom may have a substantial impact on multiple feedback loops of distress. Future studies are needed to assess the impact of different interventions (e.g., cognitive based vs. emotion regulation focused) on the symptom network and their effectiveness at reducing overall distress. Accounting for cultural and geographic differences in symptom presentation would also be beneficial. In addition, more empirical studies are needed that directly anchor reported symptoms to a COVID-19-specific experience and address vulnerabilities to psychological distress.
Funding
This study was financed in part by the Indonesian Endowment Fund for Education (Lembaga Pengelola Dana Pendidikan/LPDP) Ref: S-395/LPDP.3/2019, the Chinese Scholarship Council (NO. 201504910771), the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001 and the Cassa di Risparmio di Padova e Rovigo Foundation Research Fellowship - Italy (CARIPARO).
Acknowledgements
We thank all ambassadors of the Global Psychotrauma Screen – Cross-Cultural responses to COVID-19 versus other traumatic events (GPS-CCC) study who helped include participants around the world, in particular: Helene Aakvaag, Dean Ajdukovic, Zafer Altunbezel, Xenia Anastassiou-Hadjicharalambous, Vittoria Ardino, Anne Bakker, Sara Belquaid, Jonathon Bisson, Erine Bröcker, Lucia Cantoni, Ruby Charak, Marylene Cloitre, Aida Dias, Malgorzata Dragan, Atle Dyregrov, Julian Ford, Sarah Gallo, Paul Frewen, Wissam El Hage, Juanita Haagsma, Jackie June ter Heide, Danielle Hett, Maryke Hewett, Jana Javakhishvili, Nancy Kassam-Adams, Yoshiharu Kim, Christian Kristensen, Rachel Langevin, Juliana Lanza, Patrick Lorenz, Weili Lu, Brigitte Lueger-Schuster, Sam Manickam, Marcelo Mello, Gladys Mwiti, Natallia Nalyvaiko, Angela Nickerson, Misari Oe, Heval Özgen, Janaina Pinto, Daniela Rabellino, Luisa Sales, Carolina Salgado, Julia Schellong, Ulrich Schnyder, Soraya Seedat, Nadejda Semenova, Andrew Smith, Sjacko Sobczak, Erik de Soir, Zhonglin Tan, Keerthana Thatavarthi, Carmelo Vazquez, Anne Wagner, Li Wang, Irina Zrnic.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.janxdis.2021.102476.
Appendix A. Supplementary material
Supplementary material.
.
Supplementary material.
.
Supplementary material.
.
Data availability
Raw data were generated through the Global Collaboration on Traumatic Stress (GC-TS). Derived data supporting the findings of this study are available on the GC-TS website: www.global-psychotrauma.net.
References
- Armour C., Fried E.I., Olff M. PTSD symptomics: network analyses in the field of psychotraumatology. European Journal of Psychotraumatology. 2017;8 doi: 10.1080/20008198.2017.1398003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asmundson G.J., Taylor S. Garbage in, garbage out: The tenuous state of research on PTSD in the context of the COVID-19 pandemic and infodemic. Journal of Anxiety Disorders. 2021;78 doi: 10.1016/j.janxdis.2021.102368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benfer N., Bardeen J.R., Cero I., Kramer L.B., Whiteman S.E., Rogers T.A., Weathers F.W. Network models of posttraumatic stress symptoms across trauma types. Journal of Anxiety Disorders. 2018;58:70–77. doi: 10.1016/j.janxdis.2018.07.004. [DOI] [PubMed] [Google Scholar]
- Birkeland M.S., Greene T., Spiller T.R. The network approach to posttraumatic stress disorder: A systematic review. European Journal of Psychotraumatology. 2020;11(1) doi: 10.1080/20008198.2019.1700614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D. Psychometric perspectives on diagnostic systems. Journal of Clinical Psychology. 2008;64(9):1089–1108. doi: 10.1002/jclp.20503. [DOI] [PubMed] [Google Scholar]
- Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16(1):5–13. doi: 10.1002/wps.20375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bringmann L.F., Elmer T., Epskamp S., Krause R.W., Schoch D., Wichers M.…Snippe E. What do centrality measures measure in psychological networks? Journal of Abnormal Psychology. 2019;128:892–903. doi: 10.1037/abn0000446. [DOI] [PubMed] [Google Scholar]
- Csardi G., Nepusz T. The igraph software package for complex network research. InterJournal Complex Systems. 2006;1695(5):1–9. [Google Scholar]
- Epskamp S., Borsboom D., Fried E.I. Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods. 2018;50(1):195–212. doi: 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ertan D., El-Hage W., Thierrée S., Javelot H., Hingray C. COVID-19: urgency for distancing from domestic violence. European Journal of Psychotraumatology. 2020;11(1) doi: 10.1080/20008198.2020.1800245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frewen P., McPhail I., Schnyder U., Oe M., Olff M. Global Psychotrauma Screen (GPS): Psychometric properties in two internet-based studies. European Journal of Psychotraumatology. 2021;12(1) doi: 10.1080/20008198.2021.1881725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried E.I. Problematic assumptions have slowed down depression research: Why symptoms, not syndromes are the way forward. Frontiers in Psychology. 2015;6 doi: 10.3389/fpsyg.2015.00309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horesh D., Brown A.D. Covid-19 response: Traumatic stress in the age of Covid-19: a call to close critical gaps and adapt to new realities. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12(4):331–335. doi: 10.1037/TRA0000592. [DOI] [PubMed] [Google Scholar]
- Isvoranu, A.-M., Epskamp, S., & Cheung, M. (2020). Network models of post-traumatic stress disorder: A meta-analysis. https://doi.org/10.31234/OSF.IO/8K4U6.
- Karatzias T., Shevlin M., Murphy J., McBride O., Ben-Ezra M., Bentall R.P.…Hyland P. Posttraumatic stress symptoms and associated comorbidity during the COVID-19 pandemic in Ireland: a population-based study. Journal of Traumatic Stress. 2020;33(4):365–370. doi: 10.1002/jts.22565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko C.H., Yen C.F., Yen J.Y., Yang M.J. Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry and Clinical Neurosciences. 2006;60(4):397–403. doi: 10.1111/j.1440-1819.2006.01522.x. [DOI] [PubMed] [Google Scholar]
- Laborde D., Martin W., Swinnen J., Vos R. COVID-19 risks to global food security. Science. 2020;369(6503):500–502. doi: 10.1126/science.abc4765. [DOI] [PubMed] [Google Scholar]
- Lam M.H.B., Wing Y.K., Yu M.W.M., Leung C.M., Ma R.C.W., Kong A.P.S.…Lam S.P. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors long-term follow-up. Archives of Internal Medicine. 2009;169(22):2142–2147. doi: 10.1001/archinternmed.2009.384. [DOI] [PubMed] [Google Scholar]
- Liu D., Epskamp S., Isvoranu A.-M. Network analysis of physical and psychiatric symptoms of hospital discharged patients infected with COVID-19. Journal Affective Disorder. 2020 doi: 10.31219/OSF.IO/VZAWG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak I.W.C., Chu C.M., Pan P.C., Yiu M.G.C., Ho S.C., Chan V.L. Risk factors for chronic post-traumatic stress disorder (PTSD) in SARS survivors. General Hospital Psychiatry. 2010;32(6):590–598. doi: 10.1016/j.genhosppsych.2010.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAlonan G.M., Lee A.M., Cheung V., Cheung C., Tsang K.W.T., Sham P.C.…Wong J.G.W.S. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Canadian Journal of Psychiatry. 2007;52(4):241–247. doi: 10.1177/070674370705200406. [DOI] [PubMed] [Google Scholar]
- McNally R.J., Robinaugh D.J., Wu G.W.Y., Wang L., Deserno M.K., Borsboom D. Mental disorders as causal systems. Clinical Psychological Science. 2015;3(6):836–849. doi: 10.1177/2167702614553230. [DOI] [Google Scholar]
- Montauk T.R., Kuhl E.A. COVID-related family separation and trauma in the intensive care unit. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12(S1):S96. doi: 10.1037/tra0000839. [DOI] [PubMed] [Google Scholar]
- Oe M., Kobayashi Y., Ishida T., Chiba H., Matsuoka M., Kakuma T.…Olff M. Screening for psychotrauma related symptoms: Japanese translation and pilot testing of the Global Psychotrauma Screen. European Journal of Psychotraumatology. 2020;11(1) doi: 10.1080/20008198.2020.1810893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olff M., Bakker A., Frewen P., Aakvaag H., Ajdukovic D., Brewer D.…Schnyder U. Screening for consequences of trauma – an update on the global collaboration on traumatic stress. European Journal of Psychotraumatology. 2020;11(1) doi: 10.1080/20008198.2020.1752504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pons P., Latapy M. Vol. 3733. Springer; Berlin, Heidelberg: 2005. Computing communities in large networks using random walks; pp. 284–293. (Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics)). (LNCS) (LNCS) [DOI] [Google Scholar]
- Price M., Legrand A.C., Brier Z.M.F., Hébert-Dufresne L. The symptoms at the center: examining the comorbidity of posttraumatic stress disorder, generalized anxiety disorder, and depression with network analysis. Journal of Psychiatric Research. 2019;109:52–58. doi: 10.1016/j.jpsychires.2018.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar R.P. COVID-19 and mental health: A review of the existing literature. Asian Journal of Psychiatry. 2020;52 doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi R., Socci V., Talevi D., Niolu C., Pacitti F., Di Marco A., Olff M. Trauma-spectrum symptoms among the Italian general population in the time of the COVID-19 outbreak. European Journal of Psychotraumatology. 2021;12(1) doi: 10.1080/20008198.2020.1855888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shevlin M., Hyland P., Karatzias T. Is posttraumatic stress disorder meaningful in the context of the COVID-19 pandemic? A response to Van Overmeire’s Commentary on Karatzias et al. (2020) Journal of Traumatic Stress. 2020;33(5):866–868. doi: 10.1002/jts.22592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiller T.R., Levi O., Neria Y., Suarez-Jimenez B., Bar-Haim Y., Lazarov A. On the validity of the centrality hypothesis in cross-sectional between-subject networks of psychopathology. BMC Medicine. 2020;18(1):297. doi: 10.1186/s12916-020-01740-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stekhoven D.J., Bühlmann P. Missforest-Non-parametric missing value imputation for mixed-type data. Bioinformatics. 2012;28(1):112–118. doi: 10.1093/bioinformatics/btr597. [DOI] [PubMed] [Google Scholar]
- Sullivan C.P., Smith A.J., Lewis M., Jones R.T. Network analysis of PTSD symptoms following mass violence. Psychological Trauma: Theory, Research, Practice, and Policy. 2018;10(1):58–66. doi: 10.1037/tra0000237. [DOI] [PubMed] [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Asmundson G.J.G. Reactions to COVID-19: differential predictors of distress, avoidance, and disregard for social distancing. Journal of Affective Disorders. 2020;277:94–98. doi: 10.1016/j.jad.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Fergus T.A., McKay D., Asmundson G.J.G. Development and initial validation of the COVID stress scales. Journal of Anxiety Disorders. 2020;72 doi: 10.1016/j.janxdis.2020.102232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Fergus T.A., McKay D., Asmundson G.J.G. COVID stress syndrome: Concept, structure, and correlates. Depression and Anxiety. 2020;37:706–714. doi: 10.1002/da.23071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Rachor G.S., Asmundson G.J. Worry, avoidance, and coping during the COVID-19 pandemic: A comprehensive network analysis. Journal of Anxiety Disorders. 2020;76 doi: 10.1016/j.janxdis.2020.102327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., Paluszek M.M., Rachor G.S., McKay D., Asmundson G.J. Substance use and abuse, COVID-19-related distress, and disregard for social distancing: A network analysis. Addictive Behaviors. 2021;114 doi: 10.1016/j.addbeh.2020.106754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usher K., Bhullar N., Durkin J., Gyamfi N., Jackson D. Family violence and COVID‐19: Increased vulnerability and reduced options for support. International Journal of Mental Health Nursing. 2020;29(4):549–552. doi: 10.1111/inm.12735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Borkulo C., Boschloo L., Kossakowski J., Tio P. Comparing network structures on three aspects: A permutation test. Researchgate.Net. 2017 doi: 10.13140/RG.2.2.29455.38569. [DOI] [PubMed] [Google Scholar]
- van Borkulo C.D., Borsboom D., Epskamp S., Blanken T.F., Boschloo L., Schoevers R.A., Waldorp L.J. A new method for constructing networks from binary data. Scientific Reports. 2014;4(1):1–10. doi: 10.1038/srep05918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Borkulo, C.D., & Epskamp, S. (2016). Type Package Title Fitting Ising Models Using the ELasso Method. https://doi.org/10.1038/srep05918.
- Weems C.F. Commentary on the special issue on network analysis: assessment, intervention, theory, and the nature of reality: Actualizing the potential of network perspectives on posttraumatic stress disorder. Journal of Traumatic Stress. 2020;33(1):116–125. doi: 10.1002/jts.22482. [DOI] [PubMed] [Google Scholar]
- Williamson V., Murphy D., Greenberg N. COVID-19 and experiences of moral injury in front-line key workers. Occupational Medicine. 2020;70(5):317–319. doi: 10.1093/occmed/kqaa052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z.…Hoven C.W. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Canadian Journal of Psychiatry. 2009;54(5):302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L.…McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material.
Supplementary material.
Supplementary material.
Data Availability Statement
Raw data were generated through the Global Collaboration on Traumatic Stress (GC-TS). Derived data supporting the findings of this study are available on the GC-TS website: www.global-psychotrauma.net.