Abstract
Vaccination has become one of the most effective ways of controlling the spread of COVID-19. Consequently, revealing the evolutionary and cognitive antecedents of COVID-19 vaccine hesitancy and vaccination intention has become crucial. Drawing on the theory of behavioral immune system (BIS), we investigate whether perceived vulnerability to disease (PVD) is associated with vaccination intentions through the need for cognitive closure (NCC) and vaccine hesitancy. The data was collected from 525 adults from Turkey. The structural equation modeling results indicate that of the two dimensions of PVD, germ aversion predicts COVID-19 vaccination intention through sequential mediation of NCC and vaccine hesitancy. Perceived infectability, on the other hand, is directly and positively related to vaccination intention. By showing the mediating role of NCC, our results offer an insight as to why germ aversion translates into vaccine hesitancy, and low vaccination intention. We discuss the potential benefits of considering the roles of BIS and NCC in campaigns and policies targeted at increasing COVID-19 vaccine uptake and suggest implications for such practices.
Keywords: COVID-19 vaccines, Behavioral immune system, Need for cognitive closure, Vaccine hesitancy, Vaccination intention
1. Introduction
Since December 2019, the world has been challenged by a global health crisis, a new coronavirus pandemic (COVID-19), which brought many problems that people and governments had to manage. One of them pertains to the uncertainty and hesitancy that surround the vaccination decisions. Shortly after the initial ideas of vaccination to fight COVID-19 had been voiced, public debates have been sparked worldwide on whether to get vaccinated or not. Consequently, vaccine hesitancy has become a prominent issue that poses a threat to public health (Freeman et al., 2020; Salali & Uysal, 2020). Behavioral immune system (BIS) has been theorized as an antecedent of positive health-related behaviors (Shook et al., 2020), including vaccine attitudes and vaccination intention (Karlsson et al., 2021b). However, a number of studies have documented a negative relationship between BIS and vaccine-related outcomes (Clay, 2017; Luz et al., 2019; Reuben et al., 2020). This study aimed to address this finding by examining need for cognitive closure (NCC) as an intermediary variable in the relationship between BIS and COVID-19 vaccine hesitancy. In confirming the proposed relationships, this study extends past research on the BIS and vaccination by uncovering a process through which a heightened BIS would translate into hesitancy about vaccination, and consequently reluctance to get vaccinated.
1.1. The behavioral immune system and health behaviors
Throughout the evolution of humans, parasites and infectious diseases have been serious threats to survival and reproduction, which caused the physiological defense mechanisms to evolve. However, fighting against pathogens with such mechanisms may be metabolically costly. Thus, scholars (e.g., Murray & Schaller, 2016; Schaller & Park, 2011) theorized that a BIS, specialized in avoiding pathogen threats in the environment, might have evolved. BIS is assumed to detect pathogens that have perceivable cues and to keep the organism away from infection threats. It is considered to have affective, cognitive, and behavioral mechanisms in which people vary at trait and state level (Duncan et al., 2009). Avoidance of pathogen sources (e.g., disgust sensitivity, germ/contamination aversion) and differences in perception of oneself's vulnerability to diseases are commonly known facets of BIS.
The protective functions of BIS have received support in past research investigating the relationship of BIS with health-related behaviors. Individuals who feel vulnerable to infections are more likely to overestimate the pathogen risks (Miller & Maner, 2012), and engage more in preventative health behaviors (Shook et al., 2020). Related to the COVID-19, germ aversion increases by reading information about the COVID-19 pandemic (Bacon & Corr, 2020), and pathogen avoidance predicts anxiety and protective practices such as social distancing during the COVID-19 pandemic (Makhanova & Shepherd, 2020).
However, even though the recent evidence indicates a positive association between BIS and vaccination intention (Karlsson et al., 2021b), a considerable number of studies found a somewhat surprising negative relationship between BIS and favorable attitudes towards vaccination. For example, people with high disgust sensitivity were more skeptical about the efficacy and safety of vaccines (Clifford & Wendell, 2016). Similarly, contamination aversion was positively correlated with negative attitudes towards vaccines (Clay, 2017; Luz et al., 2019), and vaccine-hesitant individuals had higher disgust sensitivity (Reuben et al., 2020). This surprising negative relationship between BIS and vaccination attitudes has been explained by the possibility that BIS treats vaccines as contamination cues. It was argued that a mechanism evolved to detect the probable sources of pathogens and contamination which would otherwise tax the immune system is likely to operate against vaccines because they contain substances that elicit an immune response (Clay, 2017).
The findings on the negative BIS–vaccination relationship raise the possibility that specific intermediary processes exist in the relationship between BIS and vaccination-related outcomes (e.g., vaccine hesitancy, vaccination intentions). A cognitive construct that is strongly involved in decision-making may be relevant to the BIS–vaccination relationship considering the uncertainties and skepticism surrounding the COVID-19 vaccines (Karlsson et al., 2021a). We consider NCC as such and present our reasoning by which we formed expectations about the mediating role of NCC in the relationship between BIS and vaccination intention as follows.
1.2. The mediating role of need for cognitive closure
NCC refers to “the desire for a firm answer to a question and an aversion towards ambiguity” (Kruglanski & Webster, 1996, p. 264). It is involved in decision-making such that it alludes to the motivational tendency towards getting a definite answer to reduce uncertainty (Raglan et al., 2014). High NCC has been associated with ambiguity intolerance, rapid decision making (Kruglanski, 2004), limited information searching (Choi et al., 2008), and reduced preference for new options (Mannetti et al., 2007). People with high NCC do not favor uncertain situations and situations that require a decision as opposed to those in which people have freedom to abstain from deciding (Kruglanski, 2004). Consequently, people with high NCC may make hasty decisions based on insufficient evidence to alleviate the unease incited by uncertainties and decision-making (Webster & Kruglanski, 1994). Such a motivational disposition can work hand in hand with an active BIS and underlie the link between the BIS and vaccine hesitancy. Heightened BIS makes individuals sensitive to the disease and contamination cues (e.g., COVID-19 vaccines) and directs cognitive and behavioral tendencies to eliminate sources of such cues. NCC would complement this relationship with a decision-making process based on simplistic information processing (for a review see Kruglanski, 2004), at the expense of thorough and careful consideration about COVID-19 vaccines. Supporting the association between NCC and vaccine hesitancy, Cole et al. (2015) revealed that individuals with high NCC are more resistant to getting vaccinated than their low NCC counterparts. This line of argument is further solicited by how people with high dispositional NCC react to risky situations. Schumpe et al. (2017) showed that when confronted with risky choices, high NCC people tend to make less risky decisions. Thus, the heightened BIS would be associated with a decisional tendency (i.e., NCC) towards reducing the uncertainty and avoiding a salient risky circumstance, which in turn translates into hesitancy about COVID-19 vaccines, and consequently leads to lower intentions about getting vaccinated.
1.3. Overview of the current study
Our arguments thus far outline a process from BIS to vaccination intention through NCC and vaccine hesitancy. BIS generates various affective and cognitive mechanisms that guide behaviors when contextual cues point out potential pathogens (Schaller & Park, 2011). Infectious diseases create contexts characterized by risk perceptions and uncertainty that drive people to seek a definite answer and safer behavioral patterns to manage their behaviors (Kruglanski, 2004). The COVID-19 pandemic might amplify the behavioral immune responses and inclinations (Karlsson et al., 2021b). A heightened BIS (Bacon & Corr, 2020; Karlsson et al., 2021b) would be related to the need for closure because both the motivational tendencies instigated by BIS and the characteristics of the pandemic may incline people to arrive at a decision on the matter at hand. In the context of COVID-19 vaccines, a heightened BIS would lead to hesitancy about the vaccines through a motivational tendency (i.e., NCC) that drives prompt decision-making. Finally, hesitancy about the vaccines relates to lower intention to get vaccinated, as documented by past research (Karlsson et al., 2021a; Luz et al., 2019). Thus, we expect that (1) BIS is positively associated with NCC, (2) that NCC is positively associated with vaccine hesitancy, (3) and that vaccine hesitancy is negatively associated with intention to get vaccinated. Taken together, we hypothesize that BIS is associated with COVID-19 vaccination intention through sequential mediation of NCC and vaccine hesitancy.
2. Method
2.1. Participants and procedure
The sample consisted of 525 people from Turkey who volunteered to participate in an online survey. Their age ranged between 18 and 74 (M = 32.18, SD = 10.22). Other demographic information is presented in Table 1 . Participants were informed about the purpose and method of the research via an informed consent form. The data was collected between January 5 and 24, 2021. In this period, the first COVID-19 vaccine was administered in Turkey (January 14, 2021) and vaccination was not available for the public except for health care workers and pharmacists.
Table 1.
Participant demographics.
| Demographics | Frequency | Percentage |
|---|---|---|
| Sex | ||
| Men | 199 | 37.9 |
| Women | 321 | 61.1 |
| Other | 5 | 1 |
| Education | ||
| Primary school | 21 | 4.0 |
| High school | 173 | 32.9 |
| Undergraduate | 265 | 50.5 |
| Post–graduate | 66 | 12.6 |
| Past vaccine experience | ||
| Yes | 178 | 33.9 |
| No | 347 | 66.1 |
2.2. Measures
In addition to the measurements of the demographic information, we used four scales. Unless otherwise stated, all scale items were rated on a 5-point scale (1 = completely disagree, 5 = completely agree).
2.2.1. Need for cognitive closure
Individual differences in NCC were measured with the Turkish version (Yılmaz, 2015) of the 15-item Need for Cognitive Closure–Short Form (Roets & Van Hiel, 2011). All the subscales were combined into a single score (α = 0.86).
2.2.2. Perceived vulnerability to disease
Individual differences in BIS were measured with the Turkish version (Sevi, 2017) of the 14-item PVD scale (Duncan et al., 2009), which consisted of a 7-item Perceived Infectability (PI) subscale (α = 0.81), and a 7-item Germ Aversion (GA) subscale (α = 0.72). One item of GA (“I avoid using public telephones because of the risk that I may catch something from the previous user.”) was discarded because of the low frequency of usage of public telephones in Turkey (Sevi, 2017).
2.2.3. Vaccine hesitancy
To measure COVID-19 vaccine hesitancy, we generated three items following studies that operationalized vaccine hesitancy through common reasons that instigate hesitancy (see Luyten et al., 2019; Shapiro et al., 2018). The items were: “I am afraid of the side–effects of the vaccine”, “I am afraid that the vaccine will have permanent effects on my body”, and “Since COVID-19 vaccines are developed very quickly, I do not trust them”.
2.2.4. Vaccine intention
To measure vaccine intention, we used a single question–item (“Will you get a COVID-19 vaccine?”) rated on a 5-point scale (1 = I will definitely not get vaccinated; 5 = I will definitely get vaccinated).
2.2.5. Control variables
We controlled for age, sex, and past flu vaccine experience of the participants based on past research showing their significant relationship with vaccine intention (Freeman et al., 2020; Malik et al., 2020). However, age and sex were not correlated with COVID-19 vaccine intention in our data, and the analyses with and without them were identical. Thus, we omitted them from further analyses. Past flu vaccine experience was related to COVID-19 vaccine intention; thus, it was retained.
3. Results
Table 2 shows means, standard deviations, correlations among variables, and reliability estimates of the scales. We used structural equation modeling to test our hypotheses and created three parcels for PVD dimensions and four parcels for NCC scale by considering their item-to-construct relationships (Little et al., 2002). We used the items as indicators of COVID-19 vaccine hesitation since it was measured with three items. COVID-19 vaccine intention was measured with a single item. We set its reliability to 0.85 (Jöreskog & Sörbom, 1982) and followed the procedure for the single-item constructs recommended by Anderson and Gerbing (1988) by constraining the factor loading to the square root of reliability score and error variance to one minus reliability multiplied by the observed item variance.
Table 2.
Descriptive statistics, correlations between variables and reliability estimates.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Sexa | – | |||||||
| 2. Past vaccination experienceb | −0.03 | – | ||||||
| 3. Age | −0.20⁎⁎ | −0.09⁎ | – | |||||
| 4. Perceived infectability | 0.06 | 0.05 | 0.01 | (0.81) | ||||
| 5. Germ aversion | 0.05 | −0.01 | 0.08 | 0.11⁎ | (0.72) | |||
| 6. Need for cognitive closure | 0.06 | 0.06 | 0.15⁎⁎ | 0.07 | 0.36⁎⁎ | (0.85) | ||
| 7. COVID-19 vaccine hesitancy | 0.13⁎⁎ | −0.04 | −0.08 | −0.01 | 0.15⁎⁎ | 0.18⁎⁎ | (0.78) | |
| 8. COVID-19 vaccine intention | −0.02 | 0.10⁎ | 0.05 | 0.11⁎ | −0.08 | −0.10⁎ | −0.54⁎⁎ | – |
| Mean | – | – | 32.18 | 4.10 | 5.48 | 5.04 | 3.28 | 3.41 |
| SD | – | – | 10.22 | 1.27 | 1.10 | 0.91 | 0.96 | 1.12 |
Note. N = 525. Reliability estimates were reported in parentheses on the diagonal. 1 = past vaccination experience.
0 = male, 1 = female.
0 = No past vaccination experience.
p < .05.
p < .01.
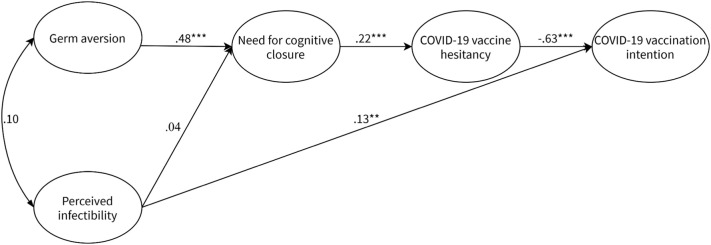
We first tested the measurement model with Mplus 8 (Muthén & Muthén, 1998–2017) which provided a good fit to the data. The details are provided in the online supplementary materials. Next, we tested the hypothesized structural model. The model provided good fit to the data, χ 2 (86, N = 525) = 204.77, p < .001, RMSEA = 0.051, TLI = 0.944, CFI = 0.954, SRMR = 0.043. We compared this model with an alternative model that estimated the direct paths between the study variables (i.e., the direct relationship of PVD dimensions with vaccine hesitancy and intention, and the direct relationship between NCC and vaccine intention). The model fit improved significantly, χ 2 (81, N = 525) = 192.02, p < .001, RMSEA = 0.051, TLI = 0.944, CFI = 0.957, SRMR = 0.041. ∆χ 2 (5) = 12.75, p < .05. However, inspection of the results revealed that the only significant path that contributed to chi-square reduction was PI predicting vaccine intention. Consequently, we retained this path only and constituted our final model, χ 2 (85, N = 525) = 196.06, p < .001, RMSEA = 0.050, TLI = 0.947, CFI = 0.957, SRMR = 0.044 (see Fig. 1 ), which was significantly better than the initial model, ∆χ 2 (1) = 8.71, p < .01.
Fig. 1.
Path estimates of the final model note: N = 525. Standardized estimates were reported. Past vaccination experience was not included in the figure for brevity. It significantly predicted COVID-19 vaccination intention (β = 0.09, p = .03). *p < .05, **p < .01, ***p < .001.
The results showed that GA (β = 0.48, p < .001) significantly predicted NCC while PI did not (β = 0.04, p = .49). NCC significantly predicted vaccine hesitancy (β = 0.22, p < .001) and vaccine hesitancy significantly predicted vaccine intention, (β = −0.63, p = .001). The model explained 42% variance in vaccine intention, 5% variance in vaccine hesitancy, and 24% variance in NCC.
We investigated the mediated relationships for GA using the bootstrap analysis. Specifically, we estimated bias-corrected confidence intervals of three indirect effects using 5000 bootstrapped resamples. The indirect relationship between GA and vaccine hesitancy through NCC was significant, coefficient = 0.10, SE = 0.03, p = .001, 95% CI [0.05, 0.16]. The indirect relationship between NCC and vaccine intention through vaccine hesitancy was also significant, coefficient = −0.22, SE = 0.06, p < .001, 95% CI [−0.35, −0.11]. Lastly, the results showed that GA was significantly related to vaccine intention through sequential mediation of NCC and vaccine hesitancy, coefficient = −0.11, SE = 0.03, p = .001, 95% CI [−0.18, −0.05]. Overall, these results confirm our hypotheses for GA dimension, but not for PI dimension of PVD.
4. Discussion
In the present study, we aimed to investigate cognitive factors that might affect the COVID-19 vaccination intentions in a sample from Turkey. We predicted that BIS is associated with lower intentions to get vaccinated through NCC and COVID-19 vaccine hesitancy. The results have confirmed our predictions for GA. PI, on the other hand, was directly related to COVID-19 vaccination intentions.
The results showed that GA had a strong relationship with NCC. The risk of disease resulting from pathogens has always created uncertainty in the ancestral environment as it does today because people cannot know for sure who is sick in a group and how diseases could be transmitted. For our minds, which evolved in this social niche, seeking for certainty and dislike of ambiguity seems to be adaptive (for a review, see Rosen et al., 2014). The finding that people with high GA were also inclined to be high in NCC revealed that the mechanism that drives cognitive and behavioral tendencies towards detecting and avoiding pathogens may operate in conjunction with a cognitive structure characterized by a desire for closure and avoidance of risks. This result is consistent with the past research showing both BIS and NCC have a significant relation to structures such as risk tolerance (Prokosch et al., 2019; Schumpe et al., 2017), and being more open to new experiences (Kupfer & Tybur, 2017; Onraet et al., 2011).
Our model indicated that GA was related to the vaccine hesitancy through the mediation of NCC. These findings demonstrate that cognitive processes involved in decision-making may have a role in why aversion of germs drives feelings of hesitancy towards vaccines. It seems that once heightened, GA is inclined to take action against any cue that it deems dangerous, including COVID-19 vaccines. This initial inclination drives the hesitancy about vaccines through a simplistic decision-making process, motivated towards a prompt closure (Kruglanski, 2004), and avoiding risks (e.g., Schumpe et al., 2017).
PI, on the other hand, was not significantly associated with NCC and vaccine hesitancy. Despite this unexpected result, previous research (e.g., Bacon & Corr, 2020; Clay, 2017; Luz et al., 2019) reported the distinct relationships of the two facets of BIS with the tested constructs, as was the case in our model. However, PI was directly and positively associated with participants' intention of vaccination. Those who perceive themselves at more risk of contamination and believe that the effects of the disease will be more severe for them may see the vaccine as a more reliable method of protection. In line with this finding, it was found that perceived vulnerability to COVID-19 is one of the predictors of intention to get vaccinated (Ruiz & Bell, 2021), higher PI is related to accepting the influenza vaccine (Luz et al., 2019), and negatively correlated with anti-vaccination attitudes (Kempthorne & Terrizzi, 2021). In this regard, the extent of people's confidence in their immunity seems to be related to their risk perception for COVID-19, and consequently considerations about vaccination.
Even though the tested relationships were significant, the explained variances in vaccine hesitancy (5%) and vaccination intention (24%) were low to moderate. Thus, factors not tested in the model may account for the unexplained variance. Prior research has demonstrated that social and cognitive factors such as social dominance, authoritarianism, religiousness, and conspiratorial beliefs are related to vaccine hesitancy (Murphy et al., 2021). These factors may be of relevance to our study because they are also associated with NCC (Kossowska & Sekerdej, 2015; Leman & Cinnirella, 2013).
Our study findings have valuable implications for practices aimed at fighting off hesitation towards vaccination and increasing vaccination rates. First, the significant involvement of NCC in the relationship between GA and vaccine hesitation suggests that campaigns can benefit from strategies that aim to reduce NCC. For example, theory and research on NCC indicate that making costs of a quick decision salient and presenting the appeal of the alternatives may reduce the need for closure (Kruglanski & Fishman, 2009). Thus, campaigns that promote COVID-19 vaccination can target costs of not getting vaccinated and spotlight the benefits of vaccines. These strategies may also shift the attention of BIS from vaccine-related threat cues to disease-related cues, disrupt the link between a heightened GA and NCC, and thus drive people to consider their attitudes and behavioral inclinations about vaccination more thoroughly. The clarity of the messages and the adverse influence of misinformation can be another point of focus for such campaigns. Individuals with a high NCC are intolerant of uncertain and risky situations which makes them prone to the negative influence of misinformation. For example, during the COVID-19 pandemic, people with high NCC did more food stockpiling than their low NCC counterparts due to perceived uncertainty and risk of being without food (Brizi & Biraglia, 2021). Thus, messages that reduce risk and uncertainty perceptions about the vaccines and policies enacted to fight misinformation about vaccines are particularly important and potentially beneficial to overcome COVID-19 vaccine hesitation and increase vaccination rates. Lastly, PI was positively and directly related to the vaccination intention, which indicates that the preventive health campaigns would benefit from highlighting the effectiveness of vaccines and the severity of COVID-19 disease.
The findings and contributions should be interpreted by taking the limitations of the study into account. The cross-sectional design and single-source data of the study bring about two issues that should be noted. First, causal interpretations cannot be made based on current data. Even though the causal ordering of the study variables was supported by theoretical reasoning, we cannot rule out the alternative bidirectional or reverse relationships. Second, single-source and single-method data is prone to common method bias. Although the measurement model tests indicated that the study variables are distinct constructs, care should be taken in interpreting the results. Future research with longitudinal designs will be helpful to confirm our results and extend them by establishing causality of the relationships. The online data collection method is another limitation of the current study. Such a method may limit the generalizability of the findings as the recruited participants may not represent the population well and the data is susceptible to skewed participant demographics.
CRediT authorship contribution statement
Çağlar Solak: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. Hilal Peker-Dural: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. Sercan Karlıdağ: Methodology, Writing – original draft, Writing – review & editing. Mehmet Peker: Formal analysis, Writing – original draft, Writing – review & editing.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.paid.2021.111245.
Appendix A. Supplementary materials
Supplementary materials
References
- Anderson J.C., Gerbing D.W. Structural equation modeling in practice: A review and recommended two–step approach. Psychological Bulletin. 1988;103(3):411–423. doi: 10.1037/0033-2909.103.3.411. [DOI] [Google Scholar]
- Bacon A.M., Corr P.J. Behavioral immune system responses to coronavirus: A reinforcement sensitivity theory explanation of conformity, warmth toward others and attitudes toward lockdown. Frontiers in Psychology. 2020;11:1–13. doi: 10.3389/fpsyg.2020.566237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brizi A., Biraglia A. “Do I have enough food?” How need for cognitive closure and gender impact stockpiling and food waste during the COVID-19 pandemic: A cross–national study in India and the United States of America. Personality and Individual Differences. 2021;168 doi: 10.1016/j.paid.2020.110396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J.A., Koo M., Choi I., Auh S. Need for cognitive closure and information search strategy. Psychology & Marketing. 2008;25:1027–1042. doi: 10.1002/mar.20253. [DOI] [Google Scholar]
- Clay R. The behavioral immune system and attitudes about vaccines: Contamination aversion predicts more negative vaccine attitudes. Social Psychological and Personality Science. 2017;8(2):162–172. doi: 10.1177/1948550616664957. [DOI] [Google Scholar]
- Clifford S., Wendell D.G. How disgust influences health purity attitudes. Political Behavior. 2016;38(1):155–178. doi: 10.1007/s11109-015-9310-z. [DOI] [Google Scholar]
- Cole A.P., Gill J.M., Fletcher K.D., Shivers C.A., Allen L.C., Mwendwa D.T. Understanding African American college students’ H1N1 vaccination decisions. Health Psychology. 2015;34(12):1185–1190. doi: 10.1037/hea0000232. [DOI] [PubMed] [Google Scholar]
- Duncan L.A., Schaller M., Park J.H. Perceived vulnerability to disease: Development and validation of a 15–item self–report instrument. Personality and Individual Differences. 2009;47(6):541–546. doi: 10.1016/j.paid.2009.05.001. [DOI] [Google Scholar]
- Freeman D., Loe B.S., Chadwick A., Vaccari C., Waite F., Rosebrock L.…Lambe S. COVID-19 vaccine hesitancy in the UK: The Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychological Medicine. 2020:1–15. doi: 10.1017/S0033291720005188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jöreskog K.G., Sörbom D. Recent developments in structural equation modeling. Journal of Marketing Research. 1982;19(4):404–416. doi: 10.2307/3151714. [DOI] [Google Scholar]
- Karlsson L.C., Soveri A., Lewandowsky S., Karlsson L., Karlsson H., Nolvi S.…Antfolk J. Fearing the disease or the vaccine: The case of COVID-19. Personality and Individual Differences. 2021;172 doi: 10.1016/j.paid.2020.110590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson L.C., Soveri A., Lewandowsky S., Karlsson L., Karlsson H., Nolvi S.…Antfolk J. The behavioral immune system and vaccination intentions during the coronavirus pandemic. PsyArXiv. 2021 doi: 10.31234/osf.io/r8uaz. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempthorne J.C., Terrizzi J.A. The behavioral immune system and conservatism as predictors of disease–avoidant attitudes during the COVID-19 pandemic. Personality and Individual Differences. 2021;178 doi: 10.1016/j.paid.2021.110857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kossowska M., Sekerdej M. Searching for certainty: Religious beliefs and intolerance toward value–violating groups. Personality and Individual Differences. 2015;83:72–76. doi: 10.1016/j.paid.2015.03.053. [DOI] [Google Scholar]
- Kruglanski A.W. Psychology Press; New York: 2004. The psychology of closed–mindedness. [Google Scholar]
- Kruglanski A.W., Fishman S. Psychological factors in terrorism and counterterrorism: Individual, group, and organizational levels of analysis. Social Issues and Policy Review. 2009;3(1):1–44. doi: 10.1111/j.1751-2409.2009.01009.x. [DOI] [Google Scholar]
- Kruglanski A.W., Webster D.M. Motivated closing of the mind: “Seizing” and “freezing”. Psychological Review. 1996;103(2):263–283. doi: 10.1037/0033-295X.103.2.263. [DOI] [PubMed] [Google Scholar]
- Kupfer T.R., Tybur J.M. Pathogen disgust and interpersonal personality. Personality and Individual Differences. 2017;116:379–384. doi: 10.1016/j.paid.2017.05.024. [DOI] [Google Scholar]
- Leman P.J., Cinnirella M. Beliefs in conspiracy theories and the need for cognitive closure. Frontiers in Psychology. 2013;4:378. doi: 10.3389/fpsyg.2013.00378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little T.D., Cunningham W.A., Shahar G., Widaman K.F. To parcel or not to parcel: Exploring the question, weighing the merits. Structural Equation Modeling: A Multidisciplinary Journal. 2002;9(2):151–173. doi: 10.1207/s15328007sem0902_1. [DOI] [Google Scholar]
- Luyten J., Bruyneel L., van Hoek A.J. Assessing vaccine hesitancy in the UK population using a generalized vaccine hesitancy survey instrument. Vaccine. 2019;37(18):2494–2501. doi: 10.1016/j.vaccine.2019.03.041. [DOI] [PubMed] [Google Scholar]
- Luz P.M., Brown H.E., Struchiner C.J. Disgust as an emotional driver of vaccine attitudes and uptake? A mediation analysis. Epidemiology and Infection. 2019;147 doi: 10.1017/S0950268819000517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makhanova A., Shepherd M.A. Behavioral immune system linked to responses to the threat of COVID-19. Personality and Individual Differences. 2020;167(110221) doi: 10.1016/j.paid.2020.110221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik A.A., McFadden S.A.M., Elharake J., Omer S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26 doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannetti L., Pierro A., Kruglanski A. Who regrets more after choosing a non–status–quo option? Post decisional regret under need for cognitive closure. Journal of Economic Psychology. 2007;28:186–196. [Google Scholar]
- Miller S.L., Maner J.K. Overperceiving disease cues: The basic cognition of the behavioral immune system. Journal of Personality and Social Psychology. 2012;102(6):1198–1213. doi: 10.1037/a0027198. [DOI] [PubMed] [Google Scholar]
- Murphy J., Vallières F., Bentall R.P., Shevlin M., McBride O., Hartman T.K.…Hyland P. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nature Communications. 2021;12(29):1–15. doi: 10.1038/s41467-020-20226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray D.R., Schaller M. In: Advances in experimental social psychology. Olson J.M., Zanna M.P., editors. Vol. 53. Academic Press; 2016. The behavioral immune system: Implications for social cognition, social interaction, and social influence; pp. 75–129. [Google Scholar]
- Muthén L.K., Muthén B.O. 8th ed. Muthén & Muthén; Los Angeles, CA: 1998–2017. Mplus user’s guide. [Google Scholar]
- Onraet E., Van Hiel A., Roets A., Cornelis I. The closed mind: ‘Experience’ and ‘cognition’ aspects of openness to experience and need for closure as psychological bases for right–wing attitudes. European Journal of Personality. 2011;25:184–197. doi: 10.1002/per.775. [DOI] [Google Scholar]
- Prokosch M.L., Gassen J., Ackerman J.M., Hill S.E. Caution in the time of cholera: Pathogen threats decrease risk tolerance. Evolutionary Behavioral Sciences. 2019;13(4):311–334. doi: 10.1037/ebs0000160. [DOI] [Google Scholar]
- Raglan G.B., Babush M., Farrow V.A., Kruglanski A.W., Schulkin J. Need to know: The need for cognitive closure impacts the clinical practice of obstetrician/gynecologists. BMC Medical Informatics and Decision Making. 2014;14:122. doi: 10.1186/s12911-014-0122-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuben R., Aitken D., Freedman J.L., Einstein G. PLoS ONE. 2020. Mistrust of the medical profession and higher disgust sensitivity predict parental vaccine hesitancy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roets A., Van Hiel A. Item selection and validation of a brief, 15–item version of the Need for Closure Scale. Personality and Individual Differences. 2011;50(1):90–94. doi: 10.1016/j.paid.2010.09.004. [DOI] [Google Scholar]
- Rosen N.O., Ivanova E., Knäuper B. Differentiating intolerance of uncertainty from three related but distinct constructs. Anxiety, Stress and Coping. 2014;27(1):55–73. doi: 10.1080/10615806.2013.815743. [DOI] [PubMed] [Google Scholar]
- Ruiz J.B., Bell R.A. Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine. 2021;39(7):1080–1086. doi: 10.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salali G.D., Uysal M.S. COVID-19 vaccine hesitancy is associated with beliefs on the origin of the novel coronavirus in the UK and Turkey. Psychological Medicine. 2020:1–3. doi: 10.1017/S0033291720004067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaller D.R., Park J. The behavioral immune system (and why it matters) Current Directions in Psychological Science. 2011;20(2):99–103. doi: 10.1177/0963721411402596. [DOI] [Google Scholar]
- Schumpe B.M., Brizi A., Giacomantonio M., Panno A., Kopetz C., Kosta M., Mannetti L. Need for cognitive closure decreases risk taking and motivates discounting of delayed rewards. Personality and Individual Differences. 2017;107:66–71. doi: 10.1016/j.paid.2016.11.039. [DOI] [Google Scholar]
- Sevi B. The Council of Higher Education – National Thesis Center; Turkey: 2017. Effects of behavioral immune system on risk taking: The case of framing effect. (Publication No. 481977) [Master Thesis, Koç University] [Google Scholar]
- Shapiro G.K., Tatar O., Dube E., Amsel R., Knauper B., Naz A.…Rosberger Z. The vaccine hesitancy scale: Psychometric properties and validation. Vaccine. 2018;36(5):660–667. doi: 10.1016/j.vaccine.2017.12.043. [DOI] [PubMed] [Google Scholar]
- Shook N.J., Sevi B., Lee J., Oosterhoff B., Fitzgerald H.N. Disease avoidance in the time of COVID-19: The behavioral immune system is associated with concern and preventative health behaviors. PLoS One. 2020;15(8 August):1–15. doi: 10.1371/journal.pone.0238015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster D.A., Kruglanski A.W. Individual differences in need for cognitive closure. Journal of Personality and Social Psychology. 1994;67(6):1049–1062. doi: 10.1037//0022-3514.67.6.1049. [DOI] [PubMed] [Google Scholar]
- Yılmaz O. The Council of Higher Education – National Thesis Center; Turkey: 2015. An investigation of the reciprocal relationship between analytic thinking and political ideology. (Publication No. 414517) [Master Thesis, Boğaziçi University] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary materials