Abstract
Background
During the COVID-19 pandemic, parents and children have experienced stress and fear, and the attitudes of parents toward COVID-19 need to be explored.
Purpose
This study aimed to develop the Parental Attitude Scale-Protecting Children during COVID-19 (PAS-CV19S) and assess its psychometric properties. This study also aimed to determine the relationship between parental attitudes about COVID-19 and fear of COVID-19.
Design and methods
In this methodological and correlational study, parents of children ages 6 to 18 years old were included (N = 402). The PAS-CV19S was developed for this study. The study collected data using an online sociodemographic form, a fear of COVID-19 scale, and the PAS-CV19S. The Cronbach alpha coefficient, confirmatory factor analysis, and explanatory factor analysis were used to assess the validity and reliability of PAS-CV19S. Pearson correlation analysis was used to examine the relationship between the fear of COVID-19 scale and the PAS-CV19S.
Results
The PAS-CV19S is a valid and reliable scale consisting of three factors (general health, mental health, and preventive behaviors) as subdimensions. The Cronbach alpha of the PAS-CV19S overall was 0.90; the Cronbach alphas for the general health, mental health, and preventive behaviors subdimensions were 0.78, 0.80, and 0.92, respectively. There was a significant negative correlation between fear of COVID-19 and the mental health subdimension.
Conclusion and practice implications
This study sheds light on parental attitudes about protecting their children from COVID-19. The fear of COVID-19 of parents did not affect attitudes other than mental health. Parental concerns and attitudes about COVID-19 need to be discussed to protect children.
Keywords: COVID-19, Parent, Fear, Attitudes, Children
Introduction
Coronaviruses represent a large group of viruses that cause a range of illnesses. The novel coronavirus disease of 2019 (COVID-19) appeared in December 2019 in Wuhan, China, and was seen in Turkey as of March 10, 2020 (Repubic of Turkey Ministry, 2020). More than 11 million cases of COVID-19 have been reported, including more than 2.5 million deaths globally. In Turkey, more than 2.6 million cases of COVID-19 have been confirmed, with more than 28,000 deaths (WHO Coronavirus Disease (COVID-19) Dashboard, 2021). Face-to-face training in schools was suspended as of March 12, 2020, in Turkey (Seker et al., 2020). According to 2019 data from the Ministry of Education in Turkey, 18 million preschool, primary, secondary, and high school students were affected (Repubic of Turkey Ministry of National Education, 2019); since the March lockdown, these students have stayed in their homes. Schools play an important role in social communication for students with their friends and teachers. Also, students who need counseling can access counseling more easily through schools (Wang, Horby, et al., 2020). Because of the epidemic, the daily routines of children have been disturbed, and their access to educational resources has been limited (Lee, 2020). In addition to the school closings, changes in curfew have affected children's routines. During the epidemic, children are restricted to their homes without engaging in activities in open areas and without adequate communication with their peers, and these changes may have negative effects on their health (Wang, Pan, et al., 2020). The quarantine process is a major concern of COVID-19 because of the uncertainty about the individual and environmental effects (Brooks et al., 2020). Children adapt to the emotional state of adults. Unexplainable behavior in adults is perceived by children as a threat and can cause anxiety (Dalton et al., 2019). Children and adolescents may exhibit extroverted behaviors (anger, uneasiness) because of their anxiety (Dalton et al., 2020). Studies on the psychosocial effects of the pandemic are being carried out in children and young people as well as the adults (Cao et al., 2020; Wang, Pan, et al., 2020). In studies was expression most children have experienced anxiety, depression, and fear during COVID-19 (Chang et al., 2020; Liu et al., 2020).
Fear is known to be associated with other psychological disorders, such as anxiety and depression. Fear has caused substantial negative impacts on people's quality of life during previous epidemics (Huang & Zhao, 2020). This is strongly intertwined with social isolation and anxiety, especially during the pandemic (Santini et al., 2020). Parents continued to work (remotely or not) while looking after children, with no clarity about how long the situation would last. For many people, it has been frightening to keep children busy and safe at home. These difficulties are even greater for crowded households. Furthermore, violence against children may increase during school closures. Parents and children can and have experienced stress and fear during the pandemic (Cluver et al., 2020).
In one study of Abuhammad (2021), parents had good protection measures about COVID-19 and were satisfied with governmental measures. COVID-19 is not the first virus to threaten humanity and might not be the last. Effective strategies are needed to evaluate and strengthen familial attitudes to protect, care for, and provide for children. When the literature was reviewed, a scale measuring parental attitudes about COVID-19 was not found. Determining the attitudes of parents with school-aged children and the fear of COVID-19 during the pandemic will contribute to the COVID-19 literature. This study aimed to determine the attitudes of parents about protecting children during COVID-19 and examined the effect of fear of COVID-19 on parental attitudes.
Material and methods
Design and study population
This study was a methodological, correlational exploration conducted to develop the Parental Attitude Scale-Protecting Children during COVID-19 (PAS-CV19S) and assess its psychometric properties. The relationship between the PAS-CV19S and fear of COVID-19 was evaluated.
Inclusion criteria of the study were: a) being a parent with children aged 6 to 18; b) being Turkish parent; c) having internet access; d) uses social media, and e) literate. The sample included all parents with children between the ages of 6 and 18 between June 15, 2020, and July 3, 2020, who resided in Turkey. GPOWER 3.0 statistical program using, the study was set to 80% power, with low effect size, a 95% confidence interval, and the margin of error was 5% for a 0.05 level of significance. The required sample size was determined to be 385. A convenience sampling method was applied in this research, and at least 385 parents planned to be included through social media. The study included 402 parents who were matching including criteria between June 15, 2020, and July 3, 2020. The construct validity analyses were conducted with all 402 parents.
Parents who did not have children between the ages of 6 and 18 years and those who stated that they did not agree to participate in this research on Google forms via social media were not included in the study. Behaviors among parents who have children older than 18 years old could differ, so these parents were not included in the study.
The PAS-CV19S was developed in this study. The final scale consisted of 24 items. The validity of the PAS-CV19S was tested by experts. To test the reliability of the PAS-CV19S, 20 parents were included for a test-retest. The necessary sample size was determined to be at least five times the number of scale items (24 × 5 = 120) (De Vellis, 2012).
Instruments
Sociodemographic data collection form
Age, gender, education level, number of children, profession of the parents, employment status during the pandemic, presence of a chronic disease in the adult, presence of a chronic disease in the child, being positive for COVID-19, and the presence of people who were positive for COVID-19 nearby were recorded.
Parental attitude scale-protecting children during COVID-19 (PAS-CV19S)
The scale included the attitudes of parents about COVID-19 to protect children. The literature on attitudes of parents about the novel coronavirus was reviewed to develop an item pool for the PAS-CV19S (CDC, 2020; Clark et al., 2020; Cluver et al., 2020; Esposito & Principi, 2020; National Association of School Psychologists, 2020; Noori et al., 2020; Zhou et al., 2020). Researchers received support from the literature to develop scale items. Item generation was performed after an extensive literature review (Morgado et al., 2017). The draft scale included items about protection from coronavirus, items about mental health, and items about precautionary behaviors for parents. Expert opinions—including evaluation by pediatricians, psychologists, and linguists—were used to finalize the draft scale. Based on the feedback received from the expert opinions, it was suggested that the items similar to each other should be removed, and the items that were more inclusive should remain. Researchers decided to remove six items in line with expert opinions. A pilot study was conducted on 30 parents. Parents who participated in the pilot study were not included in the sample. The final scale included 24 items using a 5-point Likert ranking: (1) strongly disagree, (2) disagree, (3) undecided, (4) agree, and (5) strongly agree. A minimum of 24 points and a maximum of 120 points could be obtained from the scale. The validity and reliability analyses were applied by reviewing the expert opinion about the scale. The validity and reliability analyses are presented in the Results section. The original Cronbach alpha for the PAS-CV19S was 0.90. The PAS-CV19S included three subdimensions: general health (α = 0.78), mental health (α = 0.80), and precautionary behaviors (α = 0.92). The high attitude score is positive about COVID safety.
Fear of COVID-19 scale (FCV-19S)
The fear of COVID-19 scale is a one-dimensional 7-item, 5-point Likert scale. Ahorsu et al. (2020) determined the factor loadings (0.66–0.74) and the corrected item-total correlation (0.47–0.56) and found the COVID-19 fear scale acceptable. The internal consistency and the test-retest reliability of the scale (α = 0.82 and intraclass correlation coefficient = 0.72) were accepted. The fear of COVID-19 scale positively correlated with perceived vulnerability, hospital anxiety, and depression. The minimum score for each item was 1 (strongly disagree), and the maximum score was 5 (strongly agree). The total score ranged from 7 to 35. A higher score indicated a greater fear of COVID-19. A Turkish validity and reliability study of this scale was performed by Satici et al. (2020). Scale permission was obtained for use in this study.
Data collection
This research was carried out using Google forms via social media. The online sociodemographic form, the PAS-CV19S and the fear of COVID-19 scale were shared through the researchers' Facebook, Instagram, and Twitter accounts. When a person who saw the notice clicked on the link, an informed consent form for the research appeared. Any participant who Turkish parent had children ages 6–18 years and who completed the informed consent was able to fill out the data collection forms. The data were collected between June 15, 2020, and July 3, 2020, after the lockdown ended.
Ethical statement
Permission was obtained from the Republic of Turkey Ministry of Health and the ethics committee of the university hospital. Statements were taken from the participants of this study to attest that they participated in this study and that they met the criteria of participation in this study. After the participants read about the purpose of the research saw a form with the contact addresses of the researchers, they read the following statement: “I know that I have children between the ages of 6-18, I voluntarily participate in this study and I can stop answering whenever I want. I accept the use of the information I provide in scientific publications.” Participants who approved this statement completed the form. Anyone who wanted to leave was able to exit by closing the form. The contact address of the responsible researcher was shared, and detailed information about study was provided so that the participants could call/e-mail.
Analysis
An average and percentage calculations were used to evaluate descriptive data. The significance level was accepted as p < 0.05. Shapiro Wilks test was used for normality of scale means. Regarding the PAS-CV19S, it was used the scope validity index for compatibility analysis of expert opinions. Pearson correlation analysis for item-total score analysis of scale and sub-dimensions, Cronbach Alpha coefficient for determining the internal consistency of scale and sub-dimensions, confirmatory factor analysis whether the items and subdimensions explained the original structure of the scale and explanatory factor analysis to determine the item-factor relationship were used. The data were divided into two halves for factor analysis, EFA was performed with one-half of the data, and CFA was performed with the other-half. The relationship between the PAS-CV19S and the fear of COVID-19 Scale and the items mean scores was evaluated by Pearson correlation analysis. SPSS 22.0 (SPSS Inc., Chicago, IL, USA) and LISREL 8.7 analysis programs were used to evaluate the data (Jöreskog & Sörbom, 1996).
Results
Demographics
Of the 402 parents included in the study, 89.1% (n = 358) were mothers, and parents' mean (±standard deviation) age was 40.24 ± 6.52 years; 72.6% (n = 301) were university or higher-level graduates, and participants had an average two children (mean ± SD = 1.8 ± 0.7; minimum = 1, maximum = 5). Overall, 17.2% of participants (n = 69) had a chronic illness (32.4% had asthma; 22.1%, hypertension; 11.8%, diabetes mellitus; and 33.7%, other). In addition, 8.5% (n = 34) of the children had a chronic illness (47.2% had asthma; 5.6%, allergy; 5.6%, type 1 diabetes mellitus; 41.6%, other). During the pandemic, 37.8% of participants (n = 152) stated that they were actively working; 5.5% (n = 22) had COVID-19; and 22.6% (n = 91) had been near people who were positive for COVID-19 (Table 1 ).
Table 1.
Parents' demographics (n = 402).
| Demographics |
Number (Percantage) |
| Parent Mother Father |
n (%) 358 (89.1) 44 (11.9) |
| Age | M ± SD 40.24 ± 6.52 |
| Parent’ education Primary school High school University/or higher graduates |
n (%) 35 (7) 66 (16.4) 301 (72.6) |
| The number of child parent has | M ± SD (Min, Max) 1.8 ± 0.7 (min = 1, max = 5) |
| Employment status during COVID-19 pandemic Unemployed/Not working Working actively during pandemic/Nothing changed Working remotely/Flexible working |
n (%) 55 (13.7) 152 (37.8) 195 (48.5) |
| Chronic illness Yes/No |
n (%) 69 (17.2) / 333 (82.8) |
| Chronic illness in his/her child Yes/No |
n (%) 34 (8.5) / 368 (91.5) |
| Having COVID-19 (+) Yes/No |
n (%) 22 (5.5) / 380 (94.5) |
| Having COVID-19 (+) people around Yes/No |
n (%) 91 (22.6) / 311 (77.4) |
Validity and reliability analysis of PAS-CV19S
Validity analysis: The experts (with Ph.D. degrees in pediatrics, community health, and psychiatric nursing, and with an M.D. in pediatrics) were identified to test the validity of the PAS-CV19S. Each of the 12 experts ranked each item on a 4-point Likert scale (1 = inappropriate, 2 = some change is needed, 3 = appropriate, 4 = very appropriate). The scale consisted of 24 items. The content validity index was 0.98 (range, 0.97–1.00).
Test-retest reliability: The PAS-CV19S was administered to 20 parents 2 weeks later, and there was a statistically significant positive relationship between the test-retest scores (p < 0.05).
Internal consistency reliability: The reliability coefficient of the PAS-CV19S was α = 0.90. The reliability coefficients for the subdimensions of general health (eight items), mental health (five items), and precautionary behaviors (11 items) were α = 0.78, α = 0.80, and α = 0.92, respectively. The overall item score, subdimension item score, and subdimension/the overall item score correlations for the PAS-CV19S are shown in Table 1. The overall item score correlations ranged from 0.277 to 0.675, and the general health subdimension item score correlations ranged from 0.381 to 0.609. The mental health subdimension item score correlations ranged from 0.411 to 0.637, and those for the precautionary behaviors subdimension ranged from 0.563 to 0.777. Subdimension/total scale score correlations of general health, mental health, and precautionary behaviors were 0.690, 0.715, and 0.738, respectively (p < 0.001; Table 2 ).
Table 2.
Reliability Results of PAS-CV19S (item-total, item-subdimension, and subdimension- total scale score correlations, Cronbach alpha) (n = 402).
| PAS-CV19S Items | M ± SD (Min-Max) | Item total score correlations |
Item-subdimension total score correlations |
Subdimension- total scale scores correlations |
Cronbach alpha |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| r | p | r | p | r | p | α | ||||
| General Health (Factor 1) | Item 1 | I can protect my child from coronavirus. | 3.4 ± 0.9 (1–5) | 0.277 | <0.001 | 0.381 | <0.001 | 0.690 | <0.001 | 0.78 |
| Item 2 | I take the necessary measures to protect my child from coronavirus. | 4.2 ± 0.7 (1–5) | 0.494 | <0.001 | 0.457 | <0.001 | ||||
| Item 3 | I provide a healthy diet to protect my child from coronavirus. | 4.3 ± 0.5 (2–5) | 0.533 | <0.001 | 0.445 | <0.001 | ||||
| Item 4 | I maintain my child's daily routine. | 3.6 ± 1.0 (1–5) | 0.348 | <0.001 | 0.485 | <0.001 | ||||
| Item 5 | I support my child to continue distance education. | 4.2 ± 0.9 (1–5) | 0.405 | <0.001 | 0.452 | <0.001 | ||||
| Item 6 | I support my child to play/spend her/his spare time efficiently. | 4.2 ± 0.6 (1–5) | 0.530 | <0.001 | 0.609 | <0.001 | ||||
| Item 7 | I support my child to exercise at home. | 4.1 ± 0.8 (1–5) | 0.417 | <0.001 | 0.480 | <0.001 | ||||
| Item 8 | I support my child's social development. | 4.2 ± 0.7 (2–5) | 0.530 | <0.001 | 0.547 | <0.001 | ||||
| Mental Health (Factor 2) | Item 9 | I allow my child to express herself/himself. | 4.5 ± 0.5 (1–5) | 0.616 | <0.001 | 0.637 | <0.001 | 0.715 | <0.001 | 0.80 |
| Item 10 | I support my child to keep in touch with her/his friends. | 4.2 ± 0.7 (1–5) | 0.354 | <0.001 | 0.411 | <0.001 | ||||
| Item 11 | I observe behavioral changes in my child. | 4.4 ± 0.5 (2–5) | 0.563 | <0.001 | 0.621 | <0.001 | ||||
| Item 12 | As my child can understand, I talk to her/him about the coronavirus. | 4.4 ± 0.6 (1–5) | 0.587 | <0.001 | 0.636 | <0.001 | ||||
| Item 13 | I observe if my child is worried about coronavirus. | 4.4 ± 0.5 (2–5) | 0.579 | <0.001 | 0.623 | <0.001 | ||||
| Precautionary Behaviors (Factor 3) | Item 14 | For coronavirus protection, I provide that my child is washing her/his hands properly. | 4.6 ± 0.5 (2–5) | 0.639 | <0.001 | 0.648 | <0.001 | 0.738 | <0.001 | 0.92 |
| Item 15 | I tell my child to use the inside the elbow when he/she sneezes/coughs if she/he does not have a handkerchief. | 4.6 ± 0.4 (3–5) | 0.675 | <0.001 | 0.719 | <0.001 | ||||
| Item 16 | I provide my child to wear a mask to cover the mouth and nose in the outside. | 4.5 ± 0.7 (1–5) | 0.489 | <0.001 | 0.592 | <0.001 | ||||
| Item 17 | I tell my child that she/he should stay away from sick people. | 4.7 ± 0.4 (3–5) | 0.647 | <0.001 | 0.777 | <0.001 | ||||
| Item 18 | When my child is sick (when she/he has a fever, cough, etc.), I keep her/his away from other people. | 4.7 ± 0.4 (3–5) | 0.640 | <0.001 | 0.752 | <0.001 | ||||
| Item 19 | I keep my child away from crowded environments as much as possible. | 4.6 ± 0.5 (2–5) | 0.570 | <0.001 | 0.669 | <0.001 | ||||
| Item 20 | I keep my child away from closed and air-conditioned environments as much as possible. | 4.5 ± 0.6 (2–5) | 0.492 | <0.001 | 0.563 | <0.001 | ||||
| Item 21 | I provide my child with pays attention to the hygiene rules that must be followed outside. | 4.6 ± 0.5 (2–5) | 0.660 | <0.001 | 0.796 | <0.001 | ||||
| Item 22 | I provide my child to adapt to the social distance outside. | 4.4 ± 0.7 (1–5) | 0.533 | <0.001 | 0.650 | <0.001 | ||||
| Item 23 | I also protect my health to protect my child's health. | 4.7 ± 0.4 (4–5) | 0.582 | <0.001 | 0.690 | <0.001 | ||||
| Item 24 | I become a role model for my child to protect her/his health. | 4.6 ± 0.4 (3–5) | 0.607 | <0.001 | 0.694 | <0.001 | ||||
| Total | 0.90 | |||||||||
Construct validity: In the exploratory factor analysis (EFA), the KMO coefficient was 0.91.
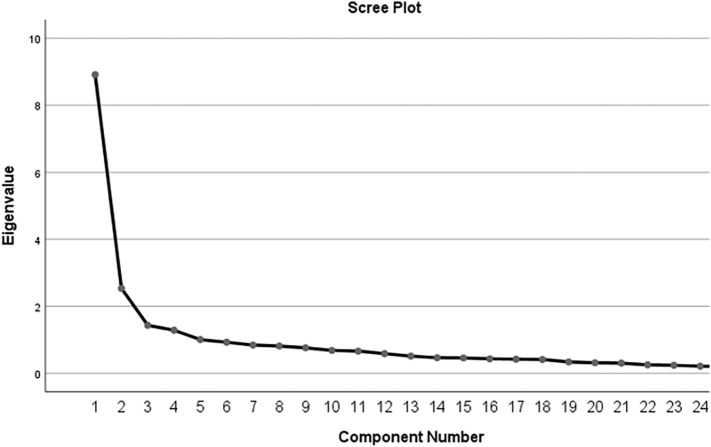
Kaiser (1974) considers a value of 0.9 or greater to be adequate for sampling. The Bartlett test results were chi-square = 4791.20 and p < 0.001. The EFA found that three factors explained 52.67% of the total variance and had eigen values higher than 1.00 (Fig. 1 ). The general health (factor 1), mental health (factor 2), and precautionary behaviors (factor 3) subdimensions explained 13.20%, 13.04%, and 26.43% of the total variance; had factor loadings of 0.41–0.71, 0.60–0.69, and 0.59–0.81, respectively (Table 3 ).
Fig. 1.
Screen plot of exploratory factor analysis.
Table 3.
Exploratory factor analysis results, principal components analysis and the rate of variance explained by factors of PAS-CV19S.
| Factors | PAS-CV19S Items | Factor loading values in principal component analysis | Rate of variances explained by factors | EFA Results |
|---|---|---|---|---|
| General Health (Factor 1) | Item 1 | 0.592 | 13.20% |
KMO = 0.91, Bartlett's test, X2 = 4791.20, p < 0.001 |
| Item 2 | 0.490 | |||
| Item 3 | 0.414 | |||
| Item 4 | 0.666 | |||
| Item 5 | 0.553 | |||
| Item 6 | 0.713 | |||
| Item 7 | 0.623 | |||
| Item 8 | 0.608 | |||
| Mental Health (Factor 2) | Item 9 | 0.676 | 13.04% | |
| Item 10 | 0.600 | |||
| Item 11 | 0.678 | |||
| Item 12 | 0.690 | |||
| Item 13 | 0.675 | |||
| Precautionary Behaviors (Factor 3) | Item 14 | 0.634 | 26.43% | |
| Item 15 | 0.698 | |||
| Item 16 | 0.643 | |||
| Item 17 | 0.799 | |||
| Item 18 | 0.768 | |||
| Item 19 | 0.723 | |||
| Item 20 | 0.598 | |||
| Item 21 | 0.810 | |||
| Item 22 | 0.710 | |||
| Item 23 | 0.737 | |||
| Item 24 | 0.712 | |||
| Total | 52.67% |
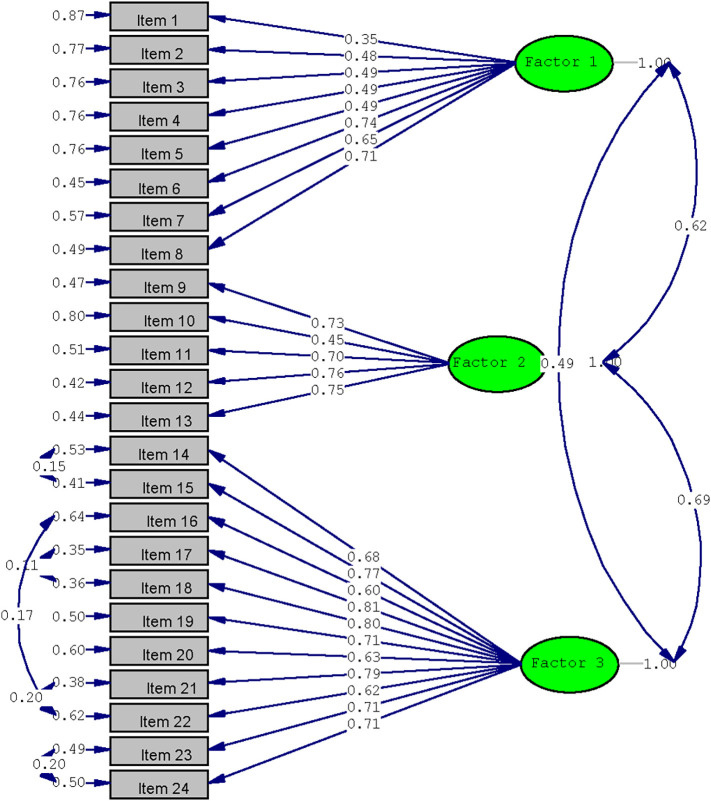
The confirmatory factor analysis (CFA) results were compatible with those of the EFA and are shown in Fig. 2 . The CFA found that the factor loadings of the general health, mental health, and precautionary behaviors subdimensions ranged from 0.35 to 0.71, from 0.45 to 0.75, and from 0.62 to 0.81, respectively. The fit indices of the PAS-CV19S were chi-squared = 759.32, df = 244, chi-squared/df = 3.111, p = 0.000, RMSEA = 0.073, GFI = 0.86, NF I = 0.95, NNFI = 0.96, CFI = 0.96, IFI = 0.96, RFI = 0.94, RMR = 0.031, and AGFI = 0.83. The chi-squared/df value in this study was more than 3, and a maximum of five is considered an acceptable value (Hooper et al., 2008). The PAS-CV19S has 24 items. The minimum and maximum scores on this scale are 24 and 120, respectively. As the scores on the PAS-CV19S increase, parental attitudes about general health, mental health, and precautionary behaviors change more with higher scores.
Fig. 2.
Confirmatory factor analysis of PAS-CV19S.
The scale scores and relationship between PAS-CV19S and FCV-19S
The general health, mental health, and precautionary behaviors subdimensions and the PAS-CV19S total mean scores were 51.0 ± 4.4 (min, 40; max, 55), 32.7 ± 4.1 (min, 18; max, 40), 22.0 ± 2.3 (min, 11; max, 25), and 105.7 ± 8.8 (min, 84; max, 120), respectively.
The mean ± standard deviation scores on the fear of COVID-19 scale were 20.1 ± 5.7 (min, 7; max, 35), mean ± standard deviation scores for individual items were as follows: item 1 (“I am most afraid of coronavirus-19”), 3.5 ± 1.0; item 2 (“It makes me uncomfortable to think about coronavirus-19”), 3.6 ± 1.0; item 3 (“My hands become clammy when I think about coronavirus-19”), 1. 0.9 ± 0.8; item 4 (“I am afraid of losing my life because of coronavirus-19”), 2.9 ± 1.2; item 5 (“When watching news and stories about COVID-19 on social media, I become nervous or anxious”), 3.5 ± 1.1; item 6 (“I cannot sleep because I'm worried about getting coronavirus-19”), 2.1 ± 1.0; and item 7 (“My heart races or palpitates when I think about getting coronavirus-19”), 2.3 ± 1.1.
The correlation between the total PAS-CV19S score or the general health, mental health, and precautionary behaviors subdimension scores and total fear of COVID-19 scale score were examined. There was a significant negative correlation between fear of COVID-19 and the mental health subdimension (r = −0.120, p < 0.05), but no correlation was found between fear and general health, precautionary behaviors, or PAS-CV19S total score (Table 4 ).
Table 4.
Relationship between PAS-CV19S and FCV-19S (n = 402).
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. General Health | |||||
| 2. Mental Health | 0.494** | ||||
| 3. Precautionary Behaviors | 0.411** | 0.566** | |||
| 4. PAS-CV19S | 0.802** | 0.776** | 0.842** | ||
| 5. FCV-19S Total | −0.019 | −0.120* | 0.054 | −0.013 |
Discussion
The PAS-CV19S was developed to evaluate parental behaviors related to COVID-19 in an up-to-date, detailed, and easily applicable way. This scale was developed according to institutional guidelines, and it consists of universal items. Researchers can adapt this scale to their communities and use the scale in related studies. The findings of this study show that the scale has a high level of reliability. Expressions intended to be assessed by the items were measured sufficiently. The total Cronbach alpha value was 0.90, and it was greater than 0.78 for all subdimensions. The Cronbach alpha for the general health subdimension (α = 0.78) was slightly lower than the others. In this study, the subdimension/total scale correlations were statistically significant (p < 0.001) and were greater than 0.69. These findings showed that all items had sufficient correlation with their subdimensions. The items that composed the subdimensions also had a high level of reliability. Furthermore, the scale had high internal consistency (Rattray & Jones, 2007).
The EFA found that the three factors explained 52.67% of the total variance and had eigenvalues greater than 1.00. These findings suggested that the items on the scale explained variance adequately and provided evidence of its construct validity. The EFA found that the factor loadings of all items on the scale were greater than 0.41. It showed that the items on the scale were at moderate and high levels and that its construct validity was acceptable (De Vellis, 2012). The CFA found that the subdimension factor loadings were greater than 0.35. The GFI, CFI, NFI, and NNFI were all greater than 0.90, and the RMSEA was less than 0.080. These results showed that the data are compatible with the model and confirmed the three-factor structure. These values showed that the scale has structural validity, that the scale items are adequately represented in subdimensions, and that the tool is valid (De Vellis, 2012; Johnson & Christensen, 2008). The scale developed in this study, as prepared by current guidelines, has high validity and reliability values. A measurement tool adapted to Turkish culture has not yet been encountered. This scale enabled the determination of the attitudes of parents to protect children from COVID-19. It is a measurement tool that can be easily applied to improve children's health in community-based studies.
The PAS-CV19S scale overall and in subdimension scores were high. These high scores indicated that parents take general health measures to protect their children, are sensitive to protecting their children's mental health, and show precautionary behaviors to avoid COVID-19. In the scale items, the parents scored lower than on the following two items than on other items: “I can protect my child from coronavirus” and “I maintain my child's daily routine.” These need to be addressed: parents have felt that they may not be able to protect their children from coronavirus, and they are also aware that their children's daily routines are disrupted. Parents need to build stronger relationships with their children in times of hardship. Open-access online parenting resources about COVID-19 are available (Cluver et al., 2020). Children often have milder COVID-19 symptoms than adults (Ludvigsson, 2020). It has known that asymptomatic people can transmit the COVID-19 and that children are often asymptomatic, so the universal use of face masks with hand hygiene and safety distancing have seem extremely useful (Esposito & Principi, 2020). Parents need to take universal measures for themselves and their children in their everyday lives. Our purpose in planning this study has been to determine whether fear of COVID-19 influenced their attitudes. It has found that the parental attitude scores were quite high. Studies about parental knowledge and attitudes about COVID-19 are limited (Abuhammad, 2020). In one study, the knowledge of and attitudes about COVID-19 in Jordanian parents demonstrated high score (Abuhammad, 2021). In another study, parents of pediatric patients had high knowledge levels, positive attitudes, and practices about COVID-19 (Noori et al., 2020).
During the COVID-19 pandemic, high levels of anxiety in parents have affected the anxiety levels of children (Saddik et al., 2020). We found average levels of fear. Although the scores of the first, second, and fifth items on the FCV-19S were high, the scores of the other items were low. There was a significant negative correlation between fear of COVID-19 and the mental health subdimension scores of PAS-CV19S. This result suggests that, as the fear of COVID-19 increases, parents are less concerned with protecting their children's mental health.
No correlation was found between fear of COVID-19 and general health or precautionary behaviors subdimensions or between fear of COVID-19 and the PAS-CV19S total score. Parents and children have lived with increased stress and fear during the pandemic (Cluver et al., 2020). The isolation and curfew imposed a complete change of lifestyle, and these measures had the potential to threaten the mental health of children and parents. Numerous mental health threats for all people have been associated with the current pandemic (Fegert et al., 2020). The long-term consequences of the pandemic should be monitored, and the attitudes of the parents during this process should be observed. In this study, we shed light on parental attitudes about protecting their children during COVID-19 pandemic. Although we did not find a relationship between fear of COVID-19 and parental attitudes, we found a relationship between their attitudes toward protecting their children's mental health and fear of COVID-19. Future studies should focus more on this topic and should handle preventive health behaviors for parents. Effective strategies to support parents and children to cope with the challenges of COVID-19 are needed such as providing instructional materials; links to websites that contain current advisories on COVID-19 safeguards; and access to mental health resources (Clark et al., 2020). Studies about COVID-19 and its effect on parents of children with chronic and developmental diseases are needed (Narzisi, 2020), in part because parents with children who have chronic diseases will likely experience more fear and anxiety (Senkalfa et al., 2020).
Practice implications
The general attitudes of parents about protecting children during COVID-19, attitudes about mental health, and precautionary behaviors can be determined by health professionals. During the pandemic, which is predicted to continue in the coming years, health professionals will continue to be called upon to provide anticipatory guidance on COVID-19 protective public health measures to parents and children. In this study, the fear of COVID were evaluated and considered average. Parents may feel unable to protect their children from COVID-19 and may worry about their children's development and education as the daily routines are disrupted. More importantly, parents can project their COVID-19 fears to their children, and the relationship quality between the two generations can change. Health professionals should support parents in matters related to COVID-19 and should approach parents and their children holistically.
Limitations
There are some difficulties and limitations in this study. The findings of the study cannot be generalized for all parents. Studies with larger sample sizes will be required to define the relationship between fear of COVID-19 and parents' attitudes about protecting children during COVID-19 pandemic.
Conclusion
We developed a valid and reliable measurement tool that measures parental attitudes about protecting children during COVID-19; it consists of three subdimensions: general health, mental health, and precautionary behaviors. This scale can be used in descriptive and experimental studies to determine parental attitudes during COVID-19. It is designed according to national and international guidelines, the scale and its items are universal. Adaptive and comparative studies can also be conducted with this scale for cross-cultural studies. Timely and correct determination of attitudes will make it easier to take protective measures. In this study, the attitude scores of parents were quite high, suggesting that parents take general health measures to protect their children, are sensitive to protecting their children's mental health, and show precautionary behaviors to avoid COVID-19. The fear of COVID-19 was considered average and correlated only with the mental health subdimension of the PAS-CV19S. The consequences of fear-induced behaviors related to COVID-19 can reach irreparable levels.
This study can guide clinicians in evaluating the parental attitudes about protecting children during COVID-19 pandemic and evaluating the fear of COVID-19, thus protecting the health of the children. The health professional is in an excellent position to guide parents by making themselves available online and by being an accurate and accessible source of information.
Funding
The authors received no financial support for the study, authorship, and/or publication of this study.
Author contributions
Gülçin Özalp Gerçeker and Murat Bektaş contributed to the study conception and design. Material preparation were performed by Gülçin Özalp Gerçeker and Emine Zahide Özdemir. Data collection were performed by Gülçin Özalp Gerçeker, Emine Zahide Özdemir and Bilge Özdemir. Data analysis were performed by Murat Bektaş. The first draft of the manuscript was written by Gülçin Özalp Gerçeker, Emine Zahide Özdemir and Bilge Özdemir. Gülçin Özalp Gerçeker, Emine Zahide Özdemir, Bilge Özdemir and Murat Bektaş commented on previous versions of the manuscript, read and approved the final manuscript.
Conflict of interest statement
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this study.
Acknowledgments
The authors thanks to all parents in this study.
References
- Abuhammad S. Barriers to distance learning during the COVID-19 outbreak: A qualitative review from parents’ perspective. Heliyon. 2020;6(11) doi: 10.1016/j.heliyon.2020.e05482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abuhammad S. Parents’ knowledge and attitude towards COVID-19 in children: A Jordanian study. International Journal of Clinical Practice. 2021;75(2) doi: 10.1111/ijcp.13671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahorsu D.K., Lin C.-Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The fear of COVID-19 scale: Development and initial validation. International Journal of Mental Health and Addiction. 2020 doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC Coronavirus disease 2019 (COVID-19) 2020. https://www.cdc.gov/coronavirus/2019-ncov/index.html
- Chang J., Yuan Y., Wang D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. Journal of Southern Medical University. 2020;40(2):171–176. doi: 10.12122/j.issn.1673-4254.2020.02.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark H., Coll-Seck A.M., Banerjee A., Peterson S., Dalglish S.L., Ameratunga S.…Costello A. A future for the world’s children? A WHO–UNICEF–Lancet Commission. The Lancet. 2020;395(10224):605–658. doi: 10.1016/S0140-6736(19)32540-1. [DOI] [PubMed] [Google Scholar]
- Cluver L., Lachman J.M., Sherr L., Wessels I., Krug E., Rakotomalala S.…McDonald K. Parenting in a time of COVID-19. The Lancet. 2020;395(10231) doi: 10.1016/S0140-6736(20)30736-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalton L., Rapa E., Stein A. Protecting the psychological health of children through effective communication about COVID-19. The Lancet Child & Adolescent Health. 2020;4(5):346–347. doi: 10.1016/S2352-4642(20)30097-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalton L., Rapa E., Ziebland S., Rochat T., Kelly B., Hanington L.…Richter L. Communication with children and adolescents about the diagnosis of a life-threatening condition in their parent. The Lancet. 2019;393(10176):1164–1176. doi: 10.1016/S0140-6736(18)33202-1. [DOI] [PubMed] [Google Scholar]
- De Vellis R. 3rd ed. Sage Publisher; 2012. Scale development : Theory and applications. [Google Scholar]
- Esposito S., Principi N. To mask or not to mask children to overcome COVID-19. European Journal of Pediatrics. 2020;179(8):1267–1270. doi: 10.1007/s00431-020-03674-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fegert J.M., Vitiello B., Plener P.L., Clemens V. Challenges and burden of the coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry and Mental Health. 2020;14(1):20. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper D., Coughlan J., Michael R., Mullen M. Structural equation modelling: Guidelines for determining model fit. Electronic Journal of Business Research Methods. 2008;6(1):53–60. [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Research. 2020;288(January) doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson B., Christensen L. 3rd ed. Sage Publication; 2008. Educational research: Quantitative, qualitative, and mixed approaches. [Google Scholar]
- Jöreskog K.G., Sörbom D. Scientific Software International; Chicago, IL: 1996. LISREL 8 user’s reference guide. [Google Scholar]
- Kaiser H.F. An index of factorial simplicity. Psychometrika. 1974;39(1):31–36. doi: 10.1007/BF02291575. [DOI] [Google Scholar]
- Lee J. Mental health effects of school closures during COVID-19. The Lancet Child & Adolescent Health. 2020;4(6):421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Liu Y., Liu Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: A cross-sectional survey. Psychiatry Research. 2020;289:113070. doi: 10.1016/j.psychres.2020.113070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludvigsson J.F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatrica. 2020;109(6):1088–1095. doi: 10.1111/apa.15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgado F.F.R., Meireles J.F.F., Neves C.M., Amaral A.C.S., Ferreira M.E.C. Scale development: Ten main limitations and recommendations to improve future research practices. Psicologia: Reflexao e Critica. 2017;30(1):1–20. doi: 10.1186/s41155-016-0057-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narzisi A. Handle the autism spectrum condition during coronavirus (COVID-19) stay at home period: Ten tips for helping parents and caregivers of young children. Brain Sciences. 2020;10(4):207. doi: 10.3390/brainsci10040207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Association of School Psychologists . 2020. Helping children cope with changes resulting from COVID-19. [Google Scholar]
- Noori N.M., Teimouri A., Khalili M., Nakhaee-Moghadam M. Knowledge, attitude, and practice towards COVID-19 among parents or guardians of patient children. Caspian Journal of Health Research. 2020;5(2):39–44. doi: 10.29252/cjhr.5.2.39. [DOI] [Google Scholar]
- Rattray J., Jones M.C. Essential elements of questionnaire design and development. Journal of Clinical Nursing. 2007;16(2):234–243. doi: 10.1111/j.1365-2702.2006.01573.x. [DOI] [PubMed] [Google Scholar]
- Repubic of Turkey Ministry COVID-19 information page. 2020. https://covid19.saglik.gov.tr/?_Dil=2
- Repubic of Turkey Ministry of National Education National education statistics formal education 2018–19. 2019. https://sgb.meb.gov.tr/meb_iys_dosyalar/2019_09/30102730_meb_istatistikleri_orgun_egitim_2018_2019.pdf
- Saddik B., Hussein A., Albanna A., Elbarazi I., Al-Shujairi A., Sharif-Askari F.S.…Halwani R. Assessing the influence of parental anxiety on childhood anxiety during the COVID-19 pandemic in the United Arab Emirates. MedRxiv. 2020 doi: 10.1101/2020.06.11.20128371. [DOI] [Google Scholar]
- Santini Z.I., Jose P.E., York Cornwell E., Koyanagi A., Nielsen L., Hinrichsen C.…Koushede V. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. The Lancet Public Health. 2020;5(1):e62–e70. doi: 10.1016/S2468-2667(19)30230-0. [DOI] [PubMed] [Google Scholar]
- Satici B., Gocet-Tekin E., Deniz M.E., Satici S.A. Adaptation of the fear of COVID-19 scale: Its association with psychological distress and life satisfaction in Turkey. International Journal of Mental Health and Addiction. 2020:1–9. doi: 10.1007/s11469-020-00294-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seker M., Özer A., Tosun Z., Korkut C., Doğrul M. Turkish academy of sciences. 2020. COVID-19 pandemic assessment report. http://www.tuba.gov.tr/files/images/2020/kovidraporu/Covid-19 Raporu-Final+.pdf. [Google Scholar]
- Senkalfa B.P., Sismanlar Eyuboglu T., Aslan A.T., Ramaslı Gursoy T., Soysal A.S., Yapar D., İlhan M.N. Effect of the COVID-19 pandemic on anxiety among children with cystic fibrosis and their mothers. Pediatric Pulmonology. 2020;55(8):2128–2134. doi: 10.1002/ppul.24900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. The Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Coronavirus Disease (COVID-19) Dashboard 2021. https://covid19.who.int/
- Zhou W., Wang Q., Hu K., Zhang Z. 2020. The coronavirus prevention handbook: 101 science-based tips that could save your life (Kindle Edi) (Skyhorse) [Google Scholar]