Highlights
-
•
First study to examine equality in coverage of COVID-19 vaccination across Wales.
-
•
Overall vaccination coverage for COVID-19 vaccination is high.
-
•
Vaccination coverage is lower in more deprived areas and among ethnic minority groups.
-
•
First vaccine study to use census linkage providing high data coverage on ethnic group.
-
•
Closing the vaccination equity gap before further waves of infection should be a priority.
Keywords: COVID-19 Vaccines, Vaccination, Immunisation, Socioeconomic factors, Ethnic groups
Abstract
The COVID-19 pandemic has highlighted existing health inequalities for ethnic minority groups and those living in more socioeconomically deprived areas in the UK. With higher levels of severe outcomes in these groups, equitable vaccination coverage should be prioritised. The aim of this study was to identify inequalities in coverage of COVID-19 vaccination in Wales, UK and to highlight areas which may benefit from routine enhanced surveillance and targeted interventions.
Records within the Wales Immunisation System (WIS) population register were linked to the Welsh Demographic Service Dataset (WDSD) and central list of shielding patients, held within the Secure Anonymised Information Linkage (SAIL) Databank. Ethnic group was derived from the 2011 census and over 20 administrative electronic health record (EHR) data sources. Uptake of first dose of any COVID-19 vaccine was analysed over time, with the odds of being vaccinated as at 25th April 2021 by sex, health board of residence, rural/urban classification, deprivation quintile and ethnic group presented. Using logistic regression models, analyses were adjusted for age group, care home resident status, health and social care worker status and shielding status.
This study included 1,256,412 individuals aged 50 years and over. Vaccine coverage increased steadily from 8th December 2020 until mid-April 2021. Overall uptake of first dose of COVID-19 vaccine in this group was 92.1%. After adjustment the odds of being vaccinated were lower for individuals who were male, resident in the most deprived areas, resident in an urban area and an ethnic group other than White. The largest inequality was seen between ethnic groups, with the odds of being vaccinated 0.22 (95 %CI 0.21–0.24) if in any Black ethnic group compared to any White ethnic group.
Ongoing monitoring of inequity in uptake of vaccinations is required, with better targeted interventions and engagement with deprived and ethnic communities to improve vaccination uptake.
1. Introduction
As at 14th May 2021 the COVID-19 pandemic has led to 3,339,002 deaths worldwide with a total of 160,813,869 confirmed cases and an unmeasurable impact on peoples wellbeing [1]. A number of licenced vaccines are providing hope for all that the pandemic may to come to an end and livelihoods can return to a sense of normality. The World Health Organization (WHO) Europe Health 2020 policy framework highlighted reducing health inequity both between and within countries, including equitable access to vaccinations, as a priority [2]. Equitable access to vaccination is of particular importance given more severe outcomes from COVID-19 disease has been seen in Black and Asian ethnic groups and individuals resident in more deprived areas [3], [4], [5].
Wales is a nation of the UK with a population of approximately 3.1 million and devolved responsibility for the National Health Service (NHS), which provides free health care to the population. As at 6th May 2021 there had been a total of 211,827 confirmed COVID-19 cases and 5,552 related deaths in Wales [6]. The COVID-19 vaccination programme in Wales started on 8th December 2020, and followed the Joint Committee on Vaccination and Immunisation (JCVI) guidance on groups to prioritise [7]. Those at highest risk of severe outcomes or at occupational risk were vaccinated first, this included older adults in care homes, front-line health and social care staff, adults aged 80 years and older, and those with clinical risks. Vaccinations were then rolled-out to the adult general population in decreasing age order. NHS services in Wales, including access to vaccinations, are provided by seven health boards, which cover different geographical regions. Each health board led its own roll-out of the COVID-19 mass vaccination programme, with central provision of vaccines and oversight from a multi-organisation COVID-19 Vaccination Board (CVB) chaired by Welsh Government. A national, patient-level vaccination register, the all Wales Immunisation System (WIS), was developed by Digital Health Care Wales (DHCW) working alongside delivery and surveillance stakeholders. The WIS vaccination register was built on experiences and infrastructure of the pre-existing national child health data system. WIS primary functions include: scheduling vaccination clinics, providing patient invitations by written letter and SMS text, recall of patients to missed appointments, and providing a national repository of timely vaccination data. The denominator spine of WIS was the national list of those registered for NHS care in Wales (the Welsh Demographics Service dataset). Within WIS there is the ability to manually add those not previously registered for NHS care. To identify those who were a priority for vaccination due to clinical or occupational risks, WIS denominator data were supplemented with additional information from general practices, the national shielded patient list and health and social care employers. Invitation letters generated using WIS were posted to individuals with the date and time of their appointment at a local mass-vaccination centre, general practice or community pharmacy, individuals were encouraged to contact a telephone helpline to rearrange their appointment if they could not attend. Appointments for the second dose were scheduled at the nationally recommended interval after administration of the first dose.
Pfizer-BioNTech BNT162b2 vaccine was the first to be offered. Due to the logistics of handling the refrigeration requirements for this vaccine, the main method of delivery for the early part of the programme was via mass vaccination clinics, with many front-line health and social care workers amongst the first to be vaccinated. Vaccination coverage in care home residents and older adults increased rapidly throughout January as the Oxford-AstraZeneca ChAdOx1 vaccine became available, which due to better stability at 2–8 °C was more suited to smaller vaccination clinics in a wider number of settings. Moderna mRNA-1273 COVID-19 vaccine was supplied for use in Wales from 7th April 2021 in one health board. As at 15th April 2021 a first dose had been offered to all individuals aged 50 years and older.
The Public Health Wales (PHW) Vaccine Preventable Disease Programme (VPDP) provide daily updates on vaccination uptake through the PHW rapid COVID-19 surveillance dashboard [6]. This includes a monthly report, showing breakdown of uptake by sex, social deprivation quintile and ethnic group, with data suggesting inequity in vaccine uptake exists within the country. However, the interaction between these factors has not been explored. There are a number of published studies looking at factors associated with low vaccination uptake in both children and adults [8], [9], [10], [11], [12]. However, large studies covering whole populations are limited [13], [14], [15]. The majority of studies in adults focus on influenza vaccination, with low uptake associated with socioeconomic status, ethnicity, sex, urban/rural residence, income, educational status, household size, living alone, co-morbidities, alcohol consumption and smoking status [9], [10], [11], [12].
Reasons for not being vaccinated can be numerous and complex, related to access barriers and challenges in attending appointments, awareness of reliable information and health literacy, vaccine hesitancy or anti-vaccine views [16]. Prior to the COVID-19 vaccine roll out, hesitancy had been identified as a potential challenge amongst Black and Pakistani ethnic groups, and also in those with lower levels of education attainment in the UK [17]. In the US, acceptance was lower in females, younger adults, Black/African Americans and those without a college degree [18]. It is important to recognise that equitable access acknowledges that some population groups will need special consideration, such as tailored method of invitation and access to suitable vaccination venues.
The aim of this study was to look at the equality of coverage of COVID-19 vaccination in Wales over the first five months of the mass vaccination programme, and to highlight inequalities which may benefit from routine enhanced surveillance and targeted interventions.
2. Methods
All analyses were completed via the Secure Anonymised Information Linkage (SAIL) Databank, hosted by Swansea University, as part of the Con-COV project [19]. All individuals aged 50 years and over as at 31st March 2021 alive, resident and registered for NHS care in Wales as at 25th April 2021 were included.
Uptake of first dose of (any) COVID-19 vaccine type was analysed and is presented by sex, health board of residence, rural/urban classification, deprivation quintile and ethnic group. Additional characteristics including: age group, care home resident status, health and social care worker status and shielding status were added as covariates to allow adjustment for differing characteristics of those prioritised in the vaccine roll out. Odds of being vaccinated with at least one dose of COVID-19 vaccine as at 25th April 2021 was estimated using univariable and multivariable logistic regression.
Sex and Lower-layer Super Output Area (LSOA) of residence was obtained from the Welsh Demographic Service Dataset (WDSD) (which is based on individuals registered for NHS care in Wales) and includes address history, date of birth and date of death. Date of vaccination, health board of residence, care home resident status and health and social care worker status were taken from the Wales Immunisation System (WIS) data, as at 25th April 2021. WIS contains information on vaccination status, vaccination dates, vaccination priority/risk group information and limited demographic information based on all WDSD registered individuals. The use of WIS, the national person-level vaccine registry, ensures that analyses are representative of the population of Wales. There will be small numbers of Welsh residents who are not registered with the NHS, including unregistered recent migrants, those whose residency status changes frequently, and those experiencing homelessness. However, outreach services are actively offering vaccination services to groups where possible, including manually registering unregistered individual with WIS and the wider NHS.
LSOA of residence for an individual’s most recent address was linked to the Welsh Index of Multiple Deprivation (WIMD) 2019 estimated deprivation scores [20]. Deprivation scores at ecological (LSOA) level were then ranked and divided in to quintiles to categorise the most (group 1) and least deprived (group 5) LSOA areas. Urban/Rural location of residence was assigned by joining LSOA to the 2011 census rural/urban classification data provided by the Office for National Statistics (ONS) [21]. Shielding status, was sourced from the national list of individuals for whom additional social restrictions were recommended at the start of the COVID-19 pandemic due to high clinical risk, based on clinician assessment and general practice records, a copy of which is held in SAIL (CVSP). A standardised set of ethnicity groups were used based on harmonised ethnicity data from 20 electronic health record (EHR) data sources across primary and secondary care, as well as administrative and specialist services data sources available in the SAIL Databank, and the ONS Census 2011 into a standard set of categories [22].
Analysis were carried out using R version 4.0.4.
3. Results
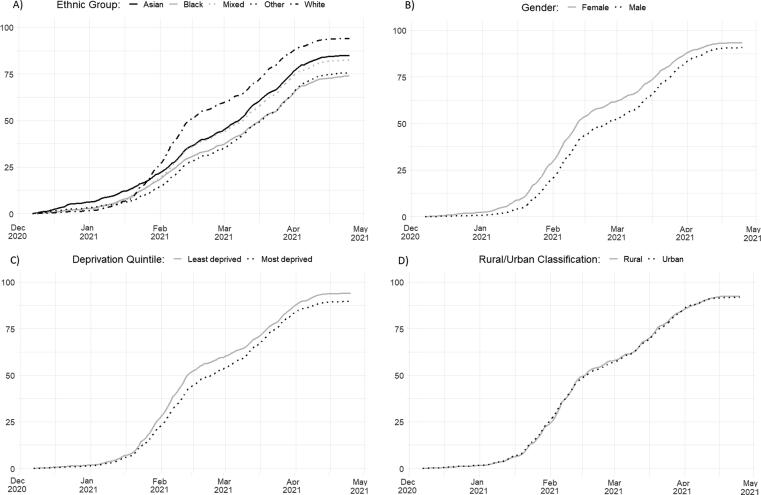
The study population included 1,256,412 individuals aged 50 years and over. Overall uptake of the first dose of COVID-19 vaccine was 92.1% as at 25th April 2021. Coverage in this age group increased steadily across age deciles until around the 10th April when it began to plateau [Fig. 1]. As at 25th April 2021 the largest inequality in coverage was seen by ethnic group, with a gap of 20.2 percentage points between those in any White ethnic group and those in any Black ethnic group, a gap of 9.1 percentage points between those in any White ethnic group and those in any Asian ethnic group, and gap of 11.6 percentage points between those in any White ethnic group and those with a Mixed ethnic background (Table 1). Significant differences were seen across all characteristics, with gaps of 4.3, 4.3, 2.7 and 0.6 percentage points when comparing the most and least deprived quintile, health board of residence with higher and lowest coverage, sex and rural/urban classification respectively. The gap in coverage observed between ethnic groups widened over the first five months of the programme as additional priority groups became eligible [Fig. 1]. However, the sex gap has narrowed compared to 12.2 percentage points as at 5th February 2021.
Fig. 1.
Cumulative uptake of one dose of COVID-19 vaccine (any type) by ethnic group, sex, urban/rural residence classification and social quintile of deprivation Wales 2020–21 a,b. a Data sourced from the all Wales Immunisation System (WIS) in SAIL within the COVID Vaccination Data (CVVD) as at 25th April 2021. b To define the most and least deprived areas of Wales small area geography Lower-layer Super Output Area (LSOA) of residence were ranked by Welsh Index of Multiple Deprivation (WIMD) score and the populations divided in to quintiles.
Table 1.
Uptake of one dose of COVID-19 vaccine (any type) and odds of being vaccinated, Wales; April 25, 2021.a,b,c
| Univariable |
Multivariable |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Category | Population (n) | Uptake (%) | OR | 95% CI | P-value | AOR | 95% CI | P-value |
| Ethnicity | White | 1,134,610 | 94.1 | ||||||
| Black | 3,954 | 73.9 | 0.18 | (0.17–0.19) | <0.01 | 0.22 | (0.21–0.24) | <0.01 | |
| Asian | 14,001 | 85.0 | 0.36 | (0.34–0.37) | <0.01 | 0.41 | (0.39–0.43) | <0.01 | |
| Mixed | 7,657 | 82.5 | 0.30 | (0.28–0.32) | <0.01 | 0.36 | (0.34–0.38) | <0.01 | |
| Other | 2,815 | 75.6 | 0.20 | (0.18–0.21) | <0.01 | 0.24 | (0.22–0.27) | <0.01 | |
| Unknown | 93,348 | 72.0 | 0.16 | (0.16–0.17) | <0.01 | 0.20 | (0.19–0.20) | <0.01 | |
| Health Board | HB 1 | 236,013 | 93.1 | ||||||
| HB 2 | 291,589 | 91.1 | 0.75 | (0.74–0.77) | <0.01 | 0.66 | (0.65–0.68) | <0.01 | |
| HB 3 | 170,399 | 91.0 | 0.75 | (0.73–0.77) | <0.01 | 0.81 | (0.79–0.83) | <0.01 | |
| HB 4 | 176,381 | 93.5 | 1.06 | (1.04–1.09) | <0.01 | 1.03 | (1.01–1.06) | 0.01 | |
| HB 5 | 167,622 | 92.7 | 0.93 | (0.91–0.96) | <0.01 | 0.80 | (0.78–0.82) | <0.01 | |
| HB 6 | 59,962 | 89.3 | 0.61 | (0.59–0.63) | <0.01 | 0.52 | (0.50–0.54) | <0.01 | |
| HB 7 | 154,419 | 92.7 | 0.94 | (0.92–0.96) | <0.01 | 0.86 | (0.84–0.88) | <0.01 | |
| Sex | Male | 605,751 | 90.8 | ||||||
| Female | 650,632 | 93.4 | 1.45 | (1.43–1.47) | <0.01 | 1.18 | (1.16–1.19) | <0.01 | |
| Location | Rural | 434,525 | 92.5 | ||||||
| Classification | Urban | 821,860 | 91.9 | 0.92 | (0.90–0.93) | <0.01 | 0.86 | (0.84–0.87) | <0.01 |
| Deprivation | Least deprived | 276,237 | 94.0 | ||||||
| Quintile | 4 | 273,049 | 92.5 | 0.78 | (0.76–0.80) | <0.01 | 0.81 | (0.79–0.83) | <0.01 |
| 3 | 257,936 | 92.1 | 0.74 | (0.72–0.75) | <0.01 | 0.78 | (0.76–0.79) | <0.01 | |
| 2 | 239,753 | 91.8 | 0.72 | (0.70–0.73) | <0.01 | 0.71 | (0.70–0.73) | <0.01 | |
| Most deprived | 209,410 | 89.7 | 0.55 | (0.54–0.56) | <0.01 | 0.59 | (0.57–0.60) | <0.01 | |
Data sourced from the all Wales Immunisation System (WIS) as at 25th April 2021.
Multivariate regression model estimates adjusted for ethnic group, health board, sex, urban/rural classification, deprivation quintile of residence, age group, health and social care worker status, care home resident status, shielding status.
To assign deprivation quintile, small area geography Lower-layer Super Output Area (LSOA) of residence were ranked by Welsh Index of Multiple Deprivation (WIMD) score and the populations divided in to quintiles.
After adjusting for age group, health and social care worker status, care home resident status and shielding status the odds of being vaccinated were lower if from a Black (0.22 95 %CI 0.21–0.24), Asian (0.41 95 %CI 0.39–0.43), Mixed ethnic background (0.36 95 %CI 0.34–0.38) or Other (0.24 95 %CI 0.22–0.27) ethnic group compared to the aggregated White ethnic group and also, if resident in the most deprived quintile compared to the least deprived quintile (0.59 95% CI 0.57–0.60). (Table 1). The odds of being vaccinated also varied by health board of residence. The odds of being vaccinated were lower if resident in an urban area compared to a rural area (0.86 95% CI 0.84–0.87).
4. Discussion
Coverage of the first dose in the population aged 50 years and older is high and suggests that at a population level, new vaccinations against COVID-19 have been positively received. However, as with other vaccinations focused at older adults, a number of significant social inequities in coverage are evident. Despite adjusting for age, care home resident status, occupation and shielding status, adults (over 50 years) in Wales are, so far, less likely to be vaccinated if they live in a more deprived area or belong to an ethnic group other than White. Given the media attention, levels of disease and mortality in older adult age-groups, and the disruption the COVID-19 pandemic has caused to livelihoods, the overall high uptake in the population may be unsurprising. This study shows that, on the whole, for all aged 50 years and over, gaps in coverage do not appear to be reducing with time, with a risk of increasing the disproportionate impact of the pandemic on these populations during future waves [23]. Many administrative health datasets have large amounts of missing data on ethnicity, with coding completeness in primary care records <50% in England [22], [24]. To our knowledge this is the first study to include census linkage to look at vaccine coverage, enabling a population-scale analysis of inequalities.
It cannot be assumed that these results are generalizable to other nations but they highlight the importance of ensuring surveillance is in place to make sure no one is left behind in terms of access to health care and being able to make accurately informed decisions. Limitations of this study mainly relate to misclassification of data. Information may be entered incorrectly in to WIS and appearing on the shielding list relies on the accurate recording of clinical risk factors in general practice records. Data completeness was generally good, although small numbers of individuals did not have sex information available (<5) and, although it was possible to attain ethnic group information for the majority of the study population it was unknown for 7.4% of individuals. Vaccination uptake in the population with unknown ethnic group is low and this is a group that need further investigation. Sociodemographic data in this study are at ecological level rather than individual level, while this demonstrates inequality according to the overall status of a small area of residence (mean population size of 1,500), it may be prone to ecological fallacy at individual level. Ethnic grouping used in this study is broad and further work is needed to look into minority groups where coverage could be comparatively low but it is not apparent when looking at the data aggregated in this way.
Existing interventions to minimise inequalities include active invitation by letter, phone or text for all those on the WIS database, and engagement with underserved communities. Due to the stepwise roll-out of the vaccination programme to incremental risk groups, it will be important to track the gap in coverage for specific age and risk groups, which may show a differed pattern of widening or narrowing inequality over time.
This study identifies inequality in coverage and further targeted work is required to ascertain whether the root-causes may be inequities in service provision or other factors. Geographical clustering of risk groups are potential hotspots for virus transmission and can be identified in linked databases and prioritised in targeted intervention. It is important not to assume that inequalities in coverage are due to differing levels of vaccine hesitancy and further analysis of opt out/ decliner information would help determine whether this is the case in Wales, as has been shown elsewhere [17], [18], [25], [26].
Additional factors such as access to vaccination clinics for the elderly who live alone need to be explored [11]. The use of a population register alongside data linkage enables representative analysis of vaccination inequalities in the population who have registered for health care. Consideration also needs to be taken to identify minority groups such as asylum seekers, refugees, the homeless and travelling population who may face barriers in accessing health care or registering with services which would ensure they are invited for vaccination [27], [28], [29]. This study has identified significant inequality in coverage of vaccination, which is the first step in tailoring services to address underlying causative factors. Further work is needed to identify the barriers to vaccination which may be related to accessibility, awareness or acceptability. Specific needs of groups who are currently poorly served by vaccination services will need to be considered. The impact of publicity and awareness of rare adverse events following vaccination and perceived safety concerns on uptake of vaccination should also be taken in to consideration.
Developing robust surveillance systems, utilising data linkage resources, reducing these inequities and understanding underlying reasons will benefit the future rollout of COVID-19 vaccination booster programmes and control of other vaccine preventable diseases such as influenza and pneumococcal disease.
5. Conclusions
This analysis highlights the need for ongoing monitoring of inequity in uptake of vaccinations. In addition to existing interventions to mitigate inequalities, further engagement should be undertaken with those in ethnic minority groups and in more socially deprived areas, including the development of tailored vaccination approaches as appropriate to minimise observed inequities in vaccination coverage to prevent severe outcomes from COVID-19, utilising available resources [30]. Closing the vaccination equity gap before further waves of infection occur should be a priority.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: MP, AA, SC, RR, RL and LG sit on the Wales COVID-19 Vaccination Board (CVB) and/or subgroups of the CVB.
Acknowledgments
Acknowledgements
This work was led by MP as part of her PhD at Swansea University contributing to the enhanced COVID-19 vaccination surveillance activities led by Public Health Wales VPDP and CDSC. Enhanced surveillance of COVID-19 vaccination equity is carried out in collaboration with members of the Wales COVID-19 Vaccination Board Data and Epidemiology Sub-Group, including: Public Health Wales (VPDP and CDSC), DHCW and Swansea University (SAIL). Authors of this report would like to thank the DHCW WIS, Data Warehouse and IS teams, the WIS Data Quality Group and all those carrying out data entry for vaccinations into WIS and associated QA work.
We wish to acknowledge the collaborative partnership that enabled acquisition and access to the de-identified data, which contributed to this analysis. The collaboration was led by the Swansea University Health Data Research UK team under the direction of the Welsh Government Technical Advisory Cell (TAC) and includes the following groups and organisations: the Secure Anonymised Information Linkage (SAIL) Databank, Administrative Data Research (ADR) Wales, NHS Wales Informatics Service (NWIS), Public Health Wales, NHS Shared Services Partnership and the Welsh Ambulance Service Trust (WAST). All research conducted has been completed under the permission and approval of the SAIL independent Information Governance Review Panel (IGRP) project number 0911. The team at Swansea University who support and maintain the One Wales collaboration, Con-COV project and associated COVID-19 e-cohorts not listed as authors are, Gareth Davies, Rowena Griffiths, Jane Lyons, Laura North.
Authors’ contributions
MP led the conception and design of this work with input from LG and SC. MP performed the analysis with AA completing the linkage and analysis to derive ethnic group. RL and FT are members of the Con-COV group that created of the linked data cohort that enabled these analyses to be undertaken. MP drafted the first iteration of the manuscript. All authors critically reviewed the manuscript, provided important intellectual input, approved the final version and agreed to be accountable for their contributions.
Data statement
The data used in this study is available from the Secure Anonymised Information Linkage (SAIL) Databank at Swansea University, Swansea, UK, which is part of the national e-health records research infrastructure for Wales. All proposals to use SAIL data are subject to review by an independent Information Governance Review Panel (IGRP). Before any data can be accessed, approval must be given by the IGRP. The IGRP gives careful consideration to each project to ensure proper and appropriate use of SAIL data. When access has been approved, it is gained through a privacy protecting safe haven and remote access system referred to as the SAIL Gateway. SAIL has established an application process to be followed by anyone who would like to access data via SAIL at: www.saildatabank.com/application-process.
Funding sources
The data used for this research were made available through Con-COV collaboration. Controlling COVID-19 through enhanced population surveillance and intervention (Con-COV): a platform approach, funded by the UKRI Medical Research Council, grant reference: MR/V028367/1. This work was supported by Health Data Research (HDR) UK [HDR-9006] which receives its funding from the UK Medical Research Council, Engineering and Physical Sciences Research Council, Economic and Social Research Council, Department of Health and Social Care (England), Chief Scientist Office of the Scottish Government Health and Social Care Directorates, Health and Social Care Research and Development Division (Welsh Government), Public Health Agency (Northern Ireland), British Heart Foundation (BHF) and the Wellcome Trust; Administrative Data Research (ADR) UK which is funded by the Economic and Social Research Council [grant ES/S007393/1].
Contributor Information
Malorie Perry, Email: Malorie.Perry@wales.nhs.uk.
Ashley Akbari, Email: A.Akbari@swansea.ac.uk.
Simon Cottrell, Email: Simon.Cottrell@wales.nhs.uk.
Michael B. Gravenor, Email: m.b.gravenor@swansea.ac.uk.
Richard Roberts, Email: Richard.Roberts3@wales.nhs.uk.
Ronan A. Lyons, Email: R.A.Lyons@Swansea.ac.uk.
Stuart Bedston, Email: stuart.bedston@swansea.ac.uk.
Fatemah Torabi, Email: Fatemah.Torabi@swansea.ac.uk.
Lucy Griffiths, Email: Lucy.Griffiths@swansea.ac.uk.
References
- 1.World Health Organisation. WHO Coronavirus (COVID-19) Dashboard. https://covid19.who.int/: 2021 [Accessed 14.05.2021].
- 2.WHO Europe. Health 2020 A European policy framework and strategy for the 21st century, https://www.euro.who.int/__data/assets/pdf_file/0011/199532/Health2020-Long.pdf; 2013 [accessed 24.04.21].
- 3.Public Health England. Beyond the data: Understanding the impact of COVID-19 on BAME groups. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/892376/COVID_stakeholder_engagement_synthesis_beyond_the_data.pdf: 2020 [accessed 24.04.21].
- 4.Bambra C., Riordan R., Ford J., Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health. 2020;74(11):964–968. doi: 10.1136/jech-2020-214401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Katikireddi S.V., Lal S., Carrol E.D., Niedzwiedz C.L., Khunti K., Dundas R. Unequal impact of the COVID-19 crisis on minority ethnic groups: a framework for understanding and addressing inequalities. J Epidemiol Community Health. 2021 doi: 10.1136/jech-2020-216061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Public Health Wales. Rapid COVID-19 Surveillance, https://public.tableau.com/profile/public.health.wales.health.protection#!/vizhome/RapidCOVID-19virology-Public/Headlinesummary: 2021 [accessed 24.04.21].
- 7.Public Health England. COVID-19 – SARS-CoV-2: the green book chapter 14a, https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/978508/Green_book_chapter_16April2021.pdf; 2021 [accessed 24.04.21].
- 8.Bocquier A., Ward J., Raude J., Peretti-Watel P., Verger P. Socioeconomic differences in childhood vaccination in developed countries: a systematic review of quantitative studies. Expert Rev Vaccines. 2017;16(11):1107–1118. doi: 10.1080/14760584.2017.1381020. [DOI] [PubMed] [Google Scholar]
- 9.Coupland C., Harcourt S., Vinogradova Y., Smith G., Joseph C., Pringle M. Inequalities in uptake of influenza vaccine by deprivation and risk group: time trends analysis. Vaccine. 2007;25(42):7363–7371. doi: 10.1016/j.vaccine.2007.08.032. [DOI] [PubMed] [Google Scholar]
- 10.Endrich M.M., Blank P.R., Szucs T.D. Influenza vaccination uptake and socioeconomic determinants in 11 European countries. Vaccine. 2009;27(30):4018–4024. doi: 10.1016/j.vaccine.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 11.Jain A., van Hoek A.J., Boccia D., Thomas S.L. Lower vaccine uptake amongst older individuals living alone: A systematic review and meta-analysis of social determinants of vaccine uptake. Vaccine. 2017;35(18):2315–2328. doi: 10.1016/j.vaccine.2017.03.013. [DOI] [PubMed] [Google Scholar]
- 12.Lee K.C., Han K., Kim J.Y., Nam G.E., Han B.D., Shin K.E. Socioeconomic status and other related factors of seasonal influenza vaccination in the South Korean adult population based on a nationwide cross-sectional study. PLoS One. 2015;10(2) doi: 10.1371/journal.pone.0117305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hull B.P., Mclntyre P.B., Sayer G.P. Factors associated with low uptake of measles and pertussis vaccines–an ecologic study based on the Australian Childhood Immunisation Register. Aust N Z J Public Health. 2001;25(5):405–410. [PubMed] [Google Scholar]
- 14.Slåttelid Schreiber S.M., Egebjerg Juul K., Dehlendorff C., Krüger Kjær.S. Socioeconomic predictors of human papillomavirus vaccination among girls in the Danish childhood immunization program. J Adolesc Health. 2015;56(4):402–407. doi: 10.1016/j.jadohealth.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 15.Perry M., McGowan A., Roberts R., Cottrell S. Timeliness and equity of infant pertussis vaccination in wales: Analysis of the three dose primary course. Vaccine. 2020;38(6):1402–1407. doi: 10.1016/j.vaccine.2019.12.001. [DOI] [PubMed] [Google Scholar]
- 16.MacDonald N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 17.Robertson E., Reeve K.S., Niedzwiedz C.L., Moore J., Blake M., Green M. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav Immun. 2021;94:41–50. doi: 10.1016/j.bbi.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Malik A.A., McFadden S.AM., Elharake J., Omer S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lyons J., Akbari A., Torabi F., Davies G.I., North L., Griffiths R. Understanding and responding to COVID-19 in Wales: protocol for a privacy-protecting data platform for enhanced epidemiology and evaluation of interventions. BMJ Open. 2020;10(10):e043010. doi: 10.1136/bmjopen-2020-043010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Welsh Government. Welsh index of multiple deprivation 2019. 2020. http://gov.wales/statistics-and-research/welsh-index-multiple-deprivation/?lang=en [accessed 24.04.21].
- 21.Office for National Statistics. 2011 rural/urban classification. 2016. https://www.ons.gov.uk/methodology/geography/geographicalproducts/ruralurbanclassifications/2011ruralurbanclassification [accessed 24.04.21].
- 22.Khunti K., Routen Am Bangerjee A., Pareek M. The need for improved collection and coding of ethnicity in health research. J Public Health (Oxf) 2020 doi: 10.1093/pubmed/fdaa198. [DOI] [PubMed] [Google Scholar]
- 23.Osama T., Razai M.S., Majeed A. COVID-19 vaccine allocation: addressing the United Kingdom’s colour-blind strategy. J R Soc Med. 2021;114(5):240–243. doi: 10.1177/01410768211001581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tippu Z., Correa A., Liyanage H., Burleigh D., McGovern A., Van Vlymen J. Ethnicity Recording in Primary Care Computerised Medical Record Systems: An Ontological Approach. J Innov Health Inform. 2017;23(4):799. doi: 10.14236/jhi.v23i4.920. [DOI] [PubMed] [Google Scholar]
- 25.Sallam M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines (Basel) 2021;9(2):160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nguyen L H, Joshi A D, Drew D A, Merino J, Ma W, Lo W-H et al. Racial and ethnic differences in COVID-19 vaccine hesitancy and uptake. medRxiv. 2021; 2021.02.25.21252402. doi: 10.1101/2021.02.25.21252402. Preprint.
- 27.Knights F., Carter J., Deal A., Crawshaw A.F., Hayward S.E., Jones L. Impact of COVID-19 on Migrants' Access to Primary Care and Implications for Vaccine Roll Out: A National Qualitative Study. Br J Gen Pract. 2021;71(709):e583–e595. doi: 10.3399/BJGP.2021.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Crawshaw A.F., Deal A., Rustage K., Forster A.S., Campos-Matos I., Vandrevala T. What must be done to tackle vaccine hesitancy and barriers to COVID-19 vaccination in migrants? J Travel Med. 2021 doi: 10.1093/jtm/taab048. taab048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Babando J., Quesnel D.A., Woodmass K., Lomness A., Graham J.R. Responding to pandemics and other disease outbreaks in homeless populations: A review of the literature and content analysis. Health Soc Care Commun. 2021 doi: 10.1111/hsc.13380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.NHS England and NHS Improvement. COVID-19 vaccine programme: Maximising vaccine uptake in underserved communities: a framework for systems, sites and local authorities leading vaccination delivery. https://www.england.nhs.uk/coronavirus/publication/maximising-vaccine-uptake-in-underserved-communities-a-framework/: 2021 [Accessed 08.05.2021].