Abstract
Background
Circulatory failure frequently occurs after out-of-hospital cardiac arrest (OHCA) and is part of post-cardiac arrest syndrome (PCAS). The aim of this study was to investigate circulatory disturbances in PCAS by assessing the circulatory trajectory during treatment in the intensive care unit (ICU).
Methods
This was a prospective single-center observational cohort study of patients after OHCA. Circulation was continuously and invasively monitored from the time of admission through the following five days. Every hour, patients were classified into one of three predefined circulatory states, yielding a longitudinal sequence of states for each patient. We used sequence analysis to describe the overall circulatory development and to identify clusters of patients with similar circulatory trajectories. We used ordered logistic regression to identify predictors for cluster membership.
Results
Among 71 patients admitted to the ICU after OHCA during the study period, 50 were included in the study. The overall circulatory development after OHCA was two-phased. Low cardiac output (CO) and high systemic vascular resistance (SVR) characterized the initial phase, whereas high CO and low SVR characterized the later phase. Most patients were stabilized with respect to circulatory state within 72 h after cardiac arrest. We identified four clusters of circulatory trajectories. Initial shockable cardiac rhythm was associated with a favorable circulatory trajectory, whereas low base excess at admission was associated with an unfavorable circulatory trajectory.
Conclusion
Circulatory failure after OHCA exhibits time-dependent characteristics. We identified four distinct circulatory trajectories and their characteristics. These findings may guide clinical support for circulatory failure after OHCA.
Trial registration
ClinicalTrials.gov: NCT02648061
Supplementary Information
The online version contains supplementary material available at 10.1186/s12871-021-01434-2.
Keywords: Out-of-hospital cardiac arrest, Post-cardiac arrest syndrome, Circulation, Hemodynamic, Cluster, Sequence analysis
Introduction
Circulatory failure frequently occurs after out-of-hospital cardiac arrest (OHCA) and is part of the post-cardiac arrest syndrome (PCAS). It is believed to be secondary to myocardial dysfunction and systemic inflammation due to global ischemia–reperfusion injury [1].
Three studies provided detailed descriptions of circulatory patterns in subgroups of OHCA patients by measuring cardiac output (CO) and systemic vascular resistance (SVR) at specific time points [2–4]. The circulatory instability was characterized by a low cardiac index and filling pressures, and the median time to onset was approximately seven hours [2]. After 24 h, the cardiac index increased, but superimposed vasodilatation delayed the discontinuation of vasopressors and fluid treatment [2].
The American Heart Association (AHA) guidelines for resuscitation and post cardiac arrest treatment recommend tailoring treatment to the specific subgroups of patients who most likely benefit from the interventions [5]. Sequence analysis is a method to describe and analyze patient development over time and to identify clusters of patients with similar trajectories [6, 7]. Three cohort studies of patients with sepsis have utilized this method to identify patients with similar “clinical phenotypes” [8–10]. To date, no studies have used sequence analysis in patients after OHCA.
The International Liaison Committee on Resuscitation (ILCOR) indicates several knowledge gaps concerning the optimal treatment of PCAS. One of these knowledge gaps is how to best deliver circulatory support after cardiac arrest [11].
The aim of this study was to analyze circulatory development after OHCA. To better understand the different “circulatory phenotypes” in PCAS, we identified clusters of patients with similar trajectories and potential predictors for cluster membership.
Methods
Study design
This was a prospective single-center observational cohort study including patients with OHCA who were admitted to the hospital with return of spontaneous circulation (ROSC). Patients were included between January 2016 and November 2017.
Setting
St. Olav’s University Hospital is a 938-bed tertiary hospital in Trondheim, Norway, serving a population of approximately 700,000 [12].
Eligibility
Both comatose and awake adults admitted to the ICU with ROSC after OHCA were assessed for eligibility. Exclusion criteria were age < 18 years, pregnancy, assumed septic or anaphylactic etiology of cardiac arrest, transfer from another hospital, decision to limit life-sustaining therapy upon arrival, acute cardiothoracic surgery, intervention with extracorporeal membranous oxygenation (ECMO) or a ventricular assist device (VAD) before arrival in the ICU.
Study period
Patients followed the study protocol from the time of admission and the subsequent five days, or until the patient died, underwent ECMO/VAD/acute cardiothoracic surgery, life-prolonging therapies were limited, or were transferred to a general ward or another hospital. Day zero had variable length depending on the time of inclusion, whereas day one started the following morning at 06:00.
Study procedure
All comatose patients without contraindications received a pulmonary artery catheter (PAC) (Swan-Ganz CCombo, Edwards Lifesciences, USA) for continuous central hemodynamic measurements. Twice daily, we calibrated the PAC oxygen saturation sensors and measured wedge pressure.
The electronic critical care management system (Picis CareSuite, Optum Inc., USA) recorded heart rate, blood pressure, peripheral transcutaneous oxygen saturation, fluid balance, medications and respiratory support. In patients with PAC, the system collected cardiac output, pulmonary artery pressure, mixed venous saturation, and calculated systemic vascular resistance. From the prehospital report and hospital record, we registered data according to the Utstein template [13], Charlson Comorbidity Index [14], and information on assessment and treatment.
We calculated the Simplified Acute Physiology Score 2 (SAPS-2) 24 h after admission and Sequential Organ Failure Assessment (SOFA) scores daily [15, 16]. After 30 and 180 days, we obtained survival status and cerebral performance category (CPC) from the hospital records [17].
Thrombocyte count and creatinine and bilirubin serum concentrations were measured at inclusion and every day at 06:00 during the study period. Every six hours, we obtained an arterial blood gas sample.
Post-cardiac arrest care and cardiovascular support
Comatose patients were cooled (36 °C) for 24 h. Patients with a suspected ischemic etiology of cardiac arrest received coronary angiography and percutaneous revascularization.
In the presence of hypotension and clinical signs of tissue hypoperfusion, circulation was optimized through fluid and vasopressor administration based on the department’s guidelines on circulatory support. A detailed description of the post-cardiac arrest care in this study has been published [18].
Circulatory state classification
Patients’ circulatory measurements were classified every hour into one of three circulatory states: ‘undisturbed’, ‘disturbed’ or ‘severely disturbed’, based upon the least favorable measurement. We used predefined values of mean blood pressure, heart rate, lactate concentrations, fluid resuscitation, vasoactive medications and the need for mechanical circulatory support (Table 1) [18]. There is no consensus on the definition or classification of circulatory instability. For this reason, hemodynamic variables and corresponding cutoff values were based upon general guidelines, clinical relevance and availability during routine monitoring of critically ill patients. Central venous oxygen saturation was initially included in the classification but was omitted because therapeutic infusions hindered sufficiently frequent measurements [18].
Table 1.
Circulatory statesa
| Variables | Undisturbed | Disturbed | Severely disturbed |
|---|---|---|---|
| Mean arterial pressure, mmHg | ≥ 65 | 45–64 | < 45 |
| Heart rate, beats per minute | 51–100 | < 50, 101–130 | ≤ 40, > 130 |
| Lactate, mmol/l | < 2 | 2–4 | > 4 |
| Fluid resuscitation, l/hours | < 0.5 | 0.5–1.9 | ≥ 2 |
| Norepinephrine, μg·kg−1·min−1 | < 0.1 | 0.1–0.29 | ≥ 0.3 |
| Dobutamine, μg·kg−1·min−1 | No | < 10 | ≥ 10 |
| Vasopressin | No | No | Yes |
| Epinephrine | No | No | Yes |
| Levosimedan | No | No | Yes |
| Aorta balloon pump | No | No | Yes |
aEvery hour a patient was classified as having undisturbed, disturbed or severely disturbed circulation according to the least favorable measurement at that time (e.g., isolated mean arterial pressure of 40 mmHg is sufficient to classify a patient as having severely disturbed circulation)
Statistical analysis
We assessed patients’ transitions among the circulatory states of ‘undisturbed’, ‘disturbed’ or ‘severely disturbed’ using a multistate model [19]. For instance, a patient in a ‘disturbed’ state may transition to either an ‘undisturbed’ or ‘severely disturbed’ state [20]. Furthermore, the state transitions also describe a sequence of states, i.e., a “trajectory”, for each patient. In addition, if the patient did not complete the study period, we considered the reason for incompletion to be informative and coded it into one of three “absorbing states”, i.e., ‘death’, ‘still treated in ICU’ or ‘transferred to ward in stable circulatory condition’.
We used sequence and cluster analysis to analyze patient trajectories. In this process, an algorithm uses pairwise optimal matching and Ward’s minimal variance method to group the sequences hierarchically into clusters of similar trajectories [6]. In optimal matching, similarity between trajectories is measured by the penalty cost for editing a sequence into another, and the result of all pairwise matches is recorded in a matrix. As recommended, the penalty cost of insertion or deletion was set to 1, and the cost of substitution was based on the transition rate [6]. Ward’s method evaluates all possible cluster combinations to build a hierarchy of clusters with the least variance bottom-up until the preset number of clusters is identified [6]. Based on previous studies on intensive care populations, we aimed to identify four clusters [9, 21].
We used ordered logistic regression to estimate the odds ratio for cluster membership based on independent factors related to patient demographics, resuscitation episode and status at hospital admission. In ordered logistic regression, the odds ratios among clusters are equal, and the odds ratio is interpreted as the odds of a higher (here: worse) cluster membership. Based on predictors from previous studies, we included age, comorbidity, shockable initial rhythm, time to ROSC, base deficit at admission and circulatory shock at admission to predict cluster membership and the anticipated circulatory trajectory [22, 23].
Data were extracted and analyzed using MATLAB software (Mathworks Inc., USA). Statistical analyses were performed using Stata version 16.0 (StataCorp LCC, USA) and R version 3.6.0 [24]. The R package “TraMineR” was used for sequence analysis and visualization of both individual sequences of circulatory states and transversal distributions of circulatory states during the ICU period [6].
Sample size
This is a descriptive study, and no formal sample size calculation was performed [25].
Ethics approval and consent to participate
The Regional Committee for Medical and Health Research Ethics, Central Norway Health Region (REK Midt, No. 2015/1807) approved this study. Written informed consent was obtained from either the patient or next-of-kin if the patient was unable to consent.
Results
Demographics
Among 71 patients admitted with ROSC after OHCA during the study period, 65 were assessed for eligibility, and 50, 42 of which were comatose, were included in the study (Supplementary Figure 1). Fifteen patients were excluded for the following reasons: seven because life-sustaining treatment was withdrawn upon arrival at the hospital, two had septic causes of cardiac arrest, two were not in need of intensive care treatment, two patients received VAD, one received ECMO and one patient underwent immediate cardiothoracic surgery. PAC was inserted in 30 of the included comatose patients. The primary contraindications were bleeding diastasis after percutaneous coronary intervention, implantable cardioverter-defibrillator or technical difficulties.
Baseline demographic data are presented in Table 2. Mean patient age was 62.7 (standard deviation (SD) 15.3) years, 40 (80%) were males, and the median Charlson Comorbidity Index score was 3 points (first to third quartiles (Q1–Q3): 2–4). In 42 (84%) patients, cardiac arrest was of cardiac etiology, and ventricular fibrillation was the initial rhythm in 37 (74%) patients. Forty-four (88%) patients received bystander cardiopulmonary resuscitation. The median ambulance response time was 9.5 (Q1–Q3: 5–13.5) minutes. ROSC was achieved after a median of 24 (Q1–Q3: 14–32) minutes from the time of the emergency call.
Table 2.
Demographics and outcomes
| Patient characteristics and outcomes | All | Comatose | Awake |
|---|---|---|---|
| N = 50 | n = 42 (84%) | n = 8 (16%) | |
| Demographics | |||
| Age, years, mean (sd) | 62.7 (15.3) | 64.8 (14.5) | 51.8 (14.5) |
| Male sex, no. (%) | 40 (80) | 35 (83) | 5 (62) |
| Body mass index, mean (sd) | 27.5 (6.6) | 27.7 (7) | 26.4 (2.3) |
| Medical history | |||
| Charlson comorbidity index, median (Q1–Q3) | 3 (2–4) | 3 (2–5) | 2 (1–3) |
| Cerebral performance category, median (Q1–Q3) | 1 (1–1) | 1 (1–1) | 1 (1–1) |
| Cardiac arrest | |||
| Location, no. (%) | |||
| Place of residence | 19 (38) | 16 (38) | 3 (37) |
| Public place | 21 (42) | 16 (38) | 5 (63) |
| Other | 10 (20) | 10 (24) | 0 (0) |
| Bystander witnessed, no. (%) | 42 (84) | 34 (80) | 8 (100) |
| Bystander performed CPR, no. (%) | 44 (88) | 37 (88) | 7 (87) |
| First monitored rhythm, no. (%) | |||
| Shockable | |||
| Ventricular fibrillation | 37 (74) | 30 (71) | 7 (88) |
| Ventricular tachycardia | 2 (4) | 1 (2) | 1 (12) |
| Nonshockable | |||
| Asystole | 4 (8) | 4 (10) | 0 (0) |
| Pulseless electric activity | 7 (14) | 7 (17) | 0 (0) |
| Number of defibrillations, median (Q1–Q3) | 2 (1–4) | 2 (1–4) | 1 (1–2) |
| Time from cardiac arrest to event, median (Q1–Q3) | |||
| Start of basic life support—min | 1 (1–2) | 1 (1–2) | 1 (1–2) |
| Start of advanced life support—min | 9 (5–13) | 10 (5–15) | 5 (2–7) |
| Return of spontaneous circulation—min | 24 (14–32) | 26 (19–35) | 8 (4–14) |
| Adrenaline—mg, median (Q1–Q3) | 0 (0–2) | 1 (0–3) | 0 (0–0) |
| Presumed etiology, no. (%) | |||
| Cardiac | 42 (84) | 34 (81) | 8 (100) |
| Asphyxia | 5 (10) | 5 (12) | 0 (0) |
| Other | 3 (6) | 3 (7) | 0 (0) |
| Certain pulmonary aspiration, no. (%) | 9 (18) | 9 (21) | 0 (0) |
| At admission | |||
| Body temperature, °C, mean (sd) | 35.3 (1.1) | 35.2 (1.0) | 36.5 (0.6) |
| In circulatory shocka, no. (%) | 18 (36) | 18 (42) | 0 (0) |
| Arterial blood gas, mean (sd) | |||
| pH | 7.18 (0.14) | 7.17 (0.15) | 7.28 (0.05) |
| pCO2, kPa | 6.2 (1.8) | 6.4 (1.9) | 5.2 (0.7) |
| Base excess, mmol/l | -9.4 (7.4) | -9.7 (7.7) | -7.6 (5.2) |
| HCO3, mmol/l | 17.9 (4.5) | 17.7 (4.4) | 19.1 (4.7) |
| Lactate, mmol/l | 6.7 (4.2) | 6.9 (4.5) | 5.9 (2.7) |
| Oxygen saturation, % | 92.1 (9.4) | 91.5 (10.1) | 95.2 (3.1) |
| Acute intervention, no. (%) | |||
| Angiography | 26 (52) | 21 (50) | 5 (63) |
| Percutaneous coronary intervention | 21 (42) | 17 (40) | 4 (50) |
| Computer tomography scan | 18 (36) | 16 (38) | 2 (25) |
| Pulmonary artery catheter | 30 (60) | 30 (71) | 0 (0) |
| Therapeutic hypothermia protocol initiated | 28 (56) | 28 (67) | 0 (0) |
| Prone position, no. (%) | 2 (4) | 2 (5) | 0 (0) |
| Simplified Acute Physiology Score II b, mean (sd) | 62 (19) | 68 (12) | 28 (9) |
| Length of stay | |||
| ICU, days, median (Q1–Q3) | 6 (3–12) | 8 (4–12) | 2 (2–3) |
| Ventilator time, hours, median (Q1–Q3) | 64 (12–162) | 93 (28–173) | 0 (0–0) |
| Hospital, days, median (Q1–Q3) | 14 (7–20) | 14,5 (7–20) | 13 (6–16) |
| Outcome, 180 days | |||
| Mortality, n (%) | 16 (32) | 16 (38) | 0 (0) |
| Cerebral | 10 (20) | 10 (23) | - |
| Circulatory | 2 (4) | 2 (5) | - |
| Respiratory | 0 (0) | 0 (0) | - |
| Multiorgan failure c | 3 (6) | 3 (7) | - |
| Other/unknown | 1 (2) | 1 (2) | - |
| Cerebral performance category, n (%) | |||
| I—Normal | 22 (44) | 22 (52) | 8 (100) |
| II—Moderate disability | 2 (4) | 2 (5) | 0 (0) |
| III—Severe disability | 2 (4) | 2 (5) | 0 (0) |
| IV—Coma or vegetative state | 0 (0) | 0 (0) | 0 (0) |
| V—Brain death | 16 (32) | 16 (38) | 0 (0) |
Comatose indicates patients who were intubated and gave no contact (GCS < 8). Awake patients were responsive and followed instructions
ICU Intensive care unit, GCS Glasgow coma scale, SD Standard deviation, Q1–Q3 first to third quartiles
aSystolic blood pressure < 90 mmHg or in need of fluids and/or vasopressors to maintain systolic blood pressure > 90 mmHg
bAfter 24 h
cIf failure of two or more organ systems led to death
Clinical circulatory variables
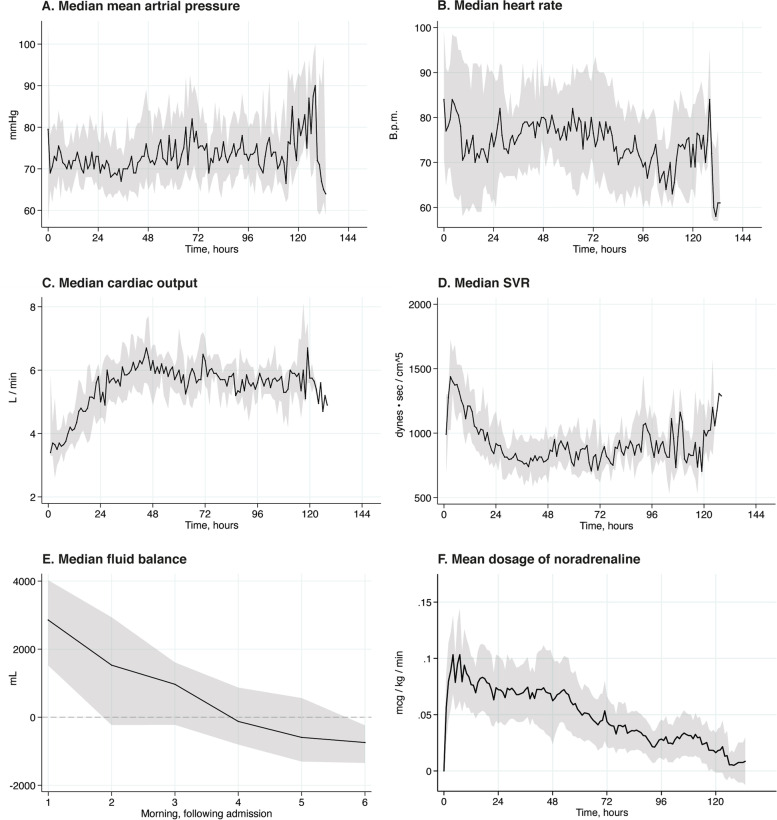
The median mean arterial pressure (MAP) was stable at approximately 70 mmHg and increased slightly after 24 h, whereas the median heart rate varied between 70 and 80 beats per minute (Fig. 1A and B). Mean pulmonary artery wedge pressure was stable between 11 and 13 mmHg, whereas median mean pulmonary arterial pressure (MPAP) was stable between 23 and 25 mmHg. The initial median CO was 2.8 L·min−1, with a median SVR of 1400 dynes·sec−1·cm−5 (Fig. 1C and D). Thereafter, the median CO increased, and the median SVR decreased until 48 h, when the median CO stabilized at approximately 6 L·min−1 and the SVR stabilized at approximately 800 dynes·sec−1·cm−5. Fluid administration was highest from admission to the following morning, and by the fourth morning, the median fluid balance was negative (Fig. 1E). The mean noradrenaline dose was initially 0.08 μg·kg−1·min−1 and decreased to 0.02 μg·kg−1·min−1 during the study period (Fig. 1F).
Fig. 1.
Clinical circulatory variables. A Median value of the mean arterial pressure with interquartile range indicated by the shaded area. B Median heart rate with interquartile range indicated by the shaded area. C Median cardiac output with interquartile range indicated by the shaded area. D Median systemic vascular resistance with interquartile range indicated by the shaded area. E Median fluid balance with interquartile range indicated by the shaded area. Fluid balance was calculated every morning. F Mean dose of noradrenaline with 95% confidence interval indicated by the shaded area. B.p.m: beats per minute. SVR: Systemic vascular resistance
Circulatory state sequences and distribution
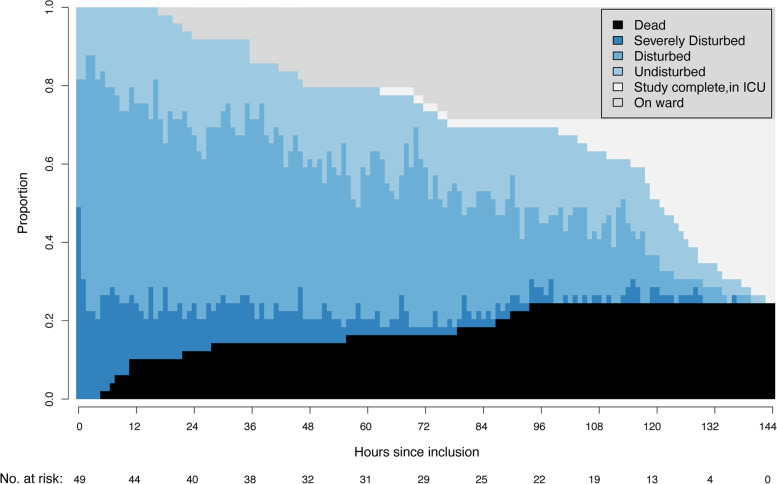
During the study period, 869 circulatory state transitions were recorded and analyzed. One patient was excluded from this analysis due to problems with data sampling. The hourly distributions of patients in each circulatory state, together with patients who died or were transferred out of the ICU, are shown in Fig. 2.
Fig. 2.
Distribution plot. Hourly distribution of circulatory states, including number at risk for state transition and coded absorbing states (i.e., death, discharge to the ward and still in the ICU but out of study). ICU: Intensive care unit
At hospital admission, approximately half of the patients were in a state of ‘severely disturbed’ circulation. Over time, circulation improved for most patients (Fig. 2). More patients entered the state of ‘disturbed’ circulation during the first 72 h than after. At the end of the study period, 14 (28%) patients had been transferred to the ward, 23 (46%) were still in ICU care, and 12 (24%) died (Fig. 2).
Hypotension, heart rate and dose of noradrenaline were the variables that most frequently “triggered” a change to a worse circulatory state (Supplementary Figure 2).
Circulatory trajectories
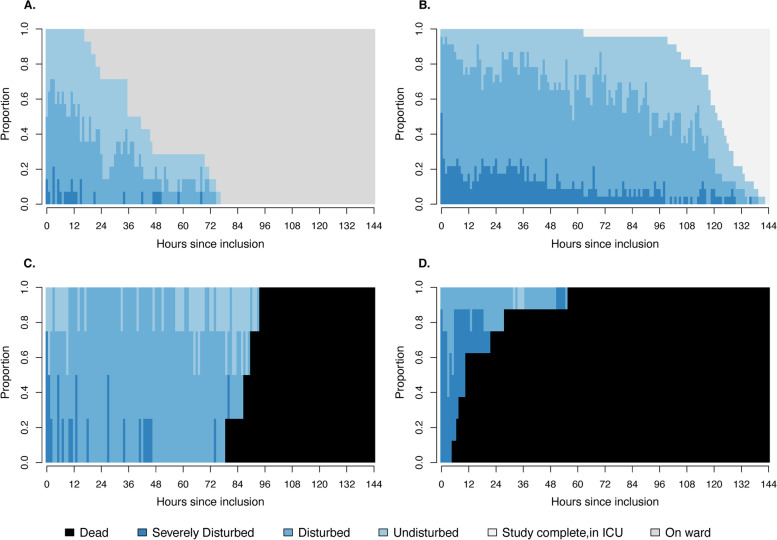
We identified four typical clusters of circulatory trajectories after OHCA. ‘Cluster 1’ (28% of patients) describes a circulatory trajectory where most patients were stabilized within 48 h and transferred to a general ward (Fig. 3a). ‘Cluster 2’ was the dominant cluster (46% of patients) and showed a trajectory where the patients were mostly in the disturbed circulatory state and remained sedated and ventilated during the study period (Fig. 3b).
Fig. 3.
Distribution plot for clusters 1 to 4. Hourly distribution of circulatory states, including death, discharge to the ward and still in the ICU but out of study. A Cluster 1. B Cluster 2. C Cluster 3. D Cluster 4. ICU: Intensive care unit
‘Cluster 3’ (8% of patients) describes a trajectory in predominantly disturbed circulatory states that ends in death within 96 h (Fig. 3c), whereas ‘Cluster 4’ (16% of patients) shows a more dramatic trajectory with patients in severe circulatory state until death, typically within 24 h (Fig. 3d).
In the multivariable analysis, base deficit at admission (OR 1.18 per mmol·L−1) was significantly associated with a less favorable cluster and thus a worse circulatory trajectory (Table 3). An initial shockable cardiac rhythm (ventricular fibrillation or tachycardia) was associated with a more favorable cluster (OR 0.07). Characteristics and sequence plots of the clusters are presented in Supplementary Table 1 and Supplementary Figure 3, respectively. The model did not violate the proportional odds assumption between the clusters (Χ2 = 0.15).
Table 3.
Ordered logistic regression analysis of the association between cluster membership and demographic variables
| Demographic variables | Univariable analysis | Multivariable analysis |
|---|---|---|
| Odds ratio (95% CI) | Odds ratio (95% CI) | |
| Age, per 5 years | 1.06 (0.88—1.28) | 1.17 (0.84—1.63) |
| Charlson Comorbidity Index, point | 0.97 (0.76—1.23) | 1.06 (0.70—1.61) |
| Initial shockable rhythm, yes | 0.02 (0.004—0.14) | 0.07 (0.01—0.46) |
| Time to ROSC, per 5 min | 1.04 (1.01—1.09) | 1.12 (0.88—1.42) |
| Base deficit at admission, per mmol/L | 1.23 (1.10—1.37) | 1.18 (1.03—1.35) |
| Circulatory shocka in the ER, yes | 5.64 (1.71—18.62) | 1.93 (0.47—7.85) |
In ordered logistic regression, the odds ratios among clusters are equal, and the odds ratio should be interpreted as the odds of a higher cluster than the compared cluster when the explanatory variable is increased by one unit and all other variables are held constant. Pseudo R2 = 0.30
CI Confidence interval, ER Emergency room, ROSC Return of spontaneous circulation
aSystolic blood pressure < 90 mmHg or in need of fluids and/or vasopressors to maintain systolic blood pressure > 90 mmHg
Morbidity and mortality
During the first four days, the patients had median SOFA scores between 10 and 11 points, which improved on the fifth day to a median of 7.5 points. The most frequent organ system failures were circulatory, neurologic and respiratory (Supplementary Table 2).
Sixteen patients died within 180 days (Table 2). Six patients died within 48 h, predominantly from refractory circulatory shock or multiorgan failure (4 of 6 patients), while ten patients died later, mostly due to irreversible brain injury (8 of 10 patients). All eight patients who were awake at admission survived with good neurologic outcomes (defined as CPC 1). Twenty-two of the 26 patients who were comatose at admission and discharged alive from the hospital had good neurologic outcomes (CPC 1) after 180 days.
Discussion
We found that after out-of-hospital cardiac arrest, patients had an overall two-phase circulatory development. Low CO and high SVR characterized the initial phase, whereas high CO and low SVR characterized the later phase. We identified four clusters of circulatory trajectories after OHCA. Multivariable analysis revealed that initial shockable rhythm was significantly associated with a favorable circulatory trajectory, while metabolic acidosis at admission was associated with an unfavorable circulatory trajectory.
Current AHA guidelines recommend MAP > 65 mmHg [5]. Patients included in our study had a median MAP between 70 and 75 mmHg during the study period. This was achieved by fluid and vasopressor administration. After liberal fluid resuscitation for the first 12 h, the need for fluids was gradually reduced in the following days. A similar pattern was evident for norepinephrine, where the mean dose was reduced after a few hours of intensive care. During the first 48 h, the CO increased concomitantly with a decrease in the calculated SVR. This pattern has previously been interpreted as resolving myocardial stunning, followed by peripheral vasodilatation due to systemic inflammation [2]. However, in this study, the median MAP and filling pressure were stable in the higher normal range, and the decrease in median SVR did not lead to an increase in vasopressor support or fluid resuscitation. Because CO and SVR are reciprocal values given constant arterial to venous pressure differences, the reduced calculated SVR might not be clinically relevant but rather an artifact due to increasing CO.
Seventy-two hours was found to be a “turning point” in circulatory stabilization. First, the majority of patients had reached a state of ‘undisturbed’ circulation by this time. Second, the majority of patients in this study achieved negative daily fluid balance between 72 and 96 h after cardiac arrest. In critically ill patients, persistent positive daily fluid balance beyond day four is associated with higher mortality [26, 27]. These observations suggest a stabilizing circulatory status within three days and are in accordance with findings by Laurent and coworkers [2].
We identified four clusters of circulatory trajectories. Three of the four clusters reached a finite state after 72 h: either stable and transferred to the ward (‘Cluster 1’) or dead (‘Cluster 3’ and ‘Cluster 4’). ‘Cluster 2’ remained in intensive care after 72 h. SOFA scores showed that most patients who remained in the ICU experienced multiorgan failure. However, 20 of 23 patients in ‘Cluster 2’ ultimately survived, and 18 of 23 patients had good neurologic outcomes (CPC 1). This observation supports that long-term intensive care treatment of OHCA patients is usually indicated, as the majority of patients, although critically ill, survived with a good cerebral outcomes.
Base deficit at admission was associated with an unfavorable circulatory trajectory, whereas initial shockable cardiac rhythm was associated with a favorable circulatory trajectory. Time to ROSC is a strong predictor for outcome [22], as seen in the univariable analysis. However, there is a high degree of collinearity between the initial shockable cardiac rhythm (i.e., ventricular tachycardia or fibrillation) and time to ROSC, and only the former was included in the final multivariable model [28, 29]. Bro-Jeppesen and coworkers have shown that increased lactate at admission is a strong predictor of vasopressor need [23]. This observation agrees with our findings, as both high lactate and metabolic acidosis at admission are indicative of “stressed metabolism” during the prehospital phase. Signs of stressed metabolism in combination with nonshockable rhythm, alternatively long time to ROSC, are suggestive of a high “ischemia–reperfusion burden” and thus a worse circulatory trajectory.
To make the result more clinically generalizable and to have a larger variability in independent predictors, thereby increasing the potential for identifying potential predictors, we included both awake and comatose patients. Awake patients usually experienced cardiac arrest, a short time to ROSC and excellent outcomes after hospital admission.
Age and comorbidities are usually associated with organ failure and mortality in an intensive care population [30] but were not significantly associated with a less favorable circulatory trajectory in our study. We observed a similar pattern of organ failure after OHCA as described by Roberts et al., with severe circulatory, respiratory and cerebral failures (SOFA score 3–4) and milder coagulation and kidney dysfunctions (SOFA score 1–2) [31]. Liver dysfunction was rare.
Sixteen of 42 (38%) patients who were comatose at hospital admission died within 180 days after OHCA. This is in line with previously reported mortality rates [32]. Furthermore, we found the same two-phase death pattern as previously described [33]; the early deaths were dominated by circulatory collapse and multiorgan failure, whereas later deaths were dominated by severe brain injury.
Strengths and limitations
The strengths of this study are its prospective design, consecutive inclusion of patients, and data including central hemodynamic measurements being obtained continuously and frequently. We also recognize some potential limitations. First, this was a single-center study with a limited number of patients, which might limit the generalizability of the results and increase the probability of making a type-2 error. However, the number of circulatory state transitions was high (869 transitions) and was sufficient to perform analyses regarding circulatory trajectories. Second, the variables and thresholds used to define the circulatory categories have not been validated. However, no consensus exists on how to define circulatory instability; therefore, we utilized measurements that are routinely available in ICU patients and thresholds based on general guidelines. Finally, sequence analysis is a complex procedure. The penalty cost of sequence editing is debatable, and a different value could have resulted in a different pairwise matching and perhaps cluster membership. However, the four clusters described in this study seem clinically reasonable.
Conclusions
Low CO and high SVR characterized the initial circulatory failure after OHCA. During the first 48 h, this pattern reversed to a high CO and low SVR. The majority of patients experienced circulatory stabilization within 72 h after cardiac arrest. We identified four clusters of patients with different severities of circulatory failure. Initial shockable cardiac rhythm was associated with a favorable circulatory trajectory, and low base excess at admission was associated with an unfavorable circulatory trajectory.
Supplementary Information
Additional file 1: Supplementary Figure 1. Flowchart summarizing patient enrollment and exclusion. CA: Cardiac arrest. ICU: Intensive care unit. ECMO: Extracorporeal membranous oxygenation. OHCA: Out-of-hospital cardiac arrest. PAC: Pulmonary artery catheter. VAD: Ventricular assist device.
Additional file 2: Supplementary Figure 2. Heat-map showing which of the variables in the circulatory state model that categorizes the patient in a worse circulatory state. IABP: Intra-aortic balloon pump. MAP: Mean arterial pressure.
Additional file 3: Supplementary Figure 3. Sequence plot for cluster 1 to 4, showing sequences of longitudinal succession of circulatory states, i.e. trajectory, for every patient in the respective cluster. A. Cluster 1. B. Cluster 2. C. Cluster 3. D. Cluster 4. ICU: Intensive care unit.
Additional file 4: Supplementary Table 1. Demographic and mortality for cluster 1 to 4. * Systolic blood pressure <90 mmHg or in need of fluids and/or vasopressors to maintain systolic blood pressure >90 mmHg. † Comatose were patients that were intubated and gave no contact (GCS <8). ER: Emergency room. GCS: Glasgow coma scale. ROSC: Return of spontaneous circulation. SD: Standard deviation. SAPS: Simplified Acute Physiology Score.
Additional file 5: Supplementary Table 2. Sequential Organ Failure Assessment score. * In sedated patients daily Glasgow Coma Scale is based on pre-sedation score. SOFA: Sequential Organ Failure Assessment. Q1–Q3: first to third quartiles.
Acknowledgements
We would like to thank the ICU staff for their excellent support.
Abbreviations
- AHA
American Heart Association
- CA
Cardiac arrest
- CO
Cardiac output
- CPC
Cerebral performance category
- ECMO
Extracorporeal membranous oxygenation
- ICU
Intensive care unit
- ILCOR
International Liaison Committee on Resuscitation
- MAP
Mean arterial pressure
- MPAP
Mean pulmonary arterial pressure
- OHCA
Out-of-hospital cardiac arrest
- PAC
Pulmonary artery catheter
- PCAS
Post-cardiac arrest syndrome
- ROSC
Return of spontaneous circulation
- SAPS-2
Simplified Acute Physiology Score 2
- SD
Standard deviations
- SOFA
Sequential Organ Failure Assessment
- SVR
Systemic vascular resistance
- VAD
Ventricular assist device
- Q1–Q3
First to third quartiles
Authors’ contributions
HL, DB, NKS and PK included patients, initiated treatment and placed all pulmonary artery catheters in accordance with the study protocol. HL, DB, NKS, PK, TS and KB supervised the study and patient care daily. ØG retrieved all patient files from the electronic critical care management system. HL, ML and TN contributed extensively to the statistical analysis. All authors contributed to interpreting the data and writing the manuscript. All authors have read and approved the final manuscript.
Funding
This work was funded by a research grant from the Norwegian University of Science and Technology and St. Olav’s University Hospital (Samarbeidsorganet HMN-NTNU).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The Regional Committee for Medical and Health Research Ethics, Central Norway Health Region (REK Midt, No. 2015/1807) approved this study. Written informed consent was obtained from either the patient or next-of-kin if the patient was unable to consent. This study was performed in accordance with the ethical standards of the Declaration of Helsinki (1964) and its subsequent amendments.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Anderson RJ, Jinadasa SP, Hsu L, Ghafouri TB, Tyagi S, Joshua J, et al. Shock subtypes by left ventricular ejection fraction following out-of-hospital cardiac arrest. Crit Care. 2018;22:162. doi: 10.1186/s13054-018-2078-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Laurent I, Monchi M, Chiche J-D, Joly L-M, Spaulding C, Bourgeois B, et al. Reversible myocardial dysfunction in survivors of out-of-hospital cardiac arrest. J Am Coll Cardiol. 2002;40:2110–2116. doi: 10.1016/S0735-1097(02)02594-9. [DOI] [PubMed] [Google Scholar]
- 3.Hovdenes J, Laake JH, Aaberge L, Haugaa H, Bugge JF. Therapeutic hypothermia after out-of-hospital cardiac arrest: experiences with patients treated with percutaneous coronary intervention and cardiogenic shock. Acta Anaesthesiol Scand. 2007;51:137–142. doi: 10.1111/j.1399-6576.2006.01209.x. [DOI] [PubMed] [Google Scholar]
- 4.Bro-Jeppesen J, Hassager C, Wanscher M, Østergaard M, Nielsen N, Erlinge D, et al. Targeted temperature management at 33°C versus 36°C and impact on systemic vascular resistance and myocardial function after out-of-hospital cardiac arrest: a sub-study of the target temperature management trial. Circ Cardiovasc Interv. 2014;7:663–672. doi: 10.1161/CIRCINTERVENTIONS.114.001556. [DOI] [PubMed] [Google Scholar]
- 5.Callaway CW, Donnino MW, Fink EL, Geocadin RG, Golan E, Kern KB, et al. Part 8: post-cardiac arrest care: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S465–482. doi: 10.1161/CIR.0000000000000262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gabadinho A, Ritschard G, Müller NS, Studer M. Analyzing and visualizing state sequences in R with TraMineR. J Stat Softw. 2011;40:1–37. doi: 10.18637/jss.v040.i04. [DOI] [Google Scholar]
- 7.Gabadinho A, Ritschard G. Searching for typical life trajectories applied to childbirth histories. In: Levy R, Widmer E, editors. Gendered life courses - between individualization and standardization. A European approach applied to Switzerland. Vienna: Lit; 2013. pp. 287–312. [Google Scholar]
- 8.Geri G, Vignon P, Aubry A, Fedou A-L, Charron C, Silva S, et al. Cardiovascular clusters in septic shock combining clinical and echocardiographic parameters: a post hoc analysis. Intensive Care Med. 2019;45:657–667. doi: 10.1007/s00134-019-05596-z. [DOI] [PubMed] [Google Scholar]
- 9.Guilamet MCV, Bernauer M, Micek ST, Kollef MH. Cluster analysis to define distinct clinical phenotypes among septic patients with bloodstream infections. Medicine. 2019;98:e15276. doi: 10.1097/MD.0000000000015276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Souza-Dantas VC, Dal-Pizzol F, Tomasi CD, Spector N, Soares M, Bozza FA, et al. Identification of distinct clinical phenotypes in mechanically ventilated patients with acute brain dysfunction using cluster analysis. Medicine. 2020;99:e20041. doi: 10.1097/MD.0000000000020041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neumar RW, Nolan JP, Adrie C, Aibiki M, Berg RA, Böttiger BW, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation. 2008;118:2452–83. doi: 10.1161/CIRCULATIONAHA.108.190652. [DOI] [PubMed] [Google Scholar]
- 12.St. Olav University Hospital: Key figures from 2016. St. Olav’s University Hospital; 2017. https://stolav.no/en/about-the-hospital/key-figures-from-2016.
- 13.Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update of the Utstein Resuscitation Registry templates for out-of-hospital cardiac arrest: A statement for healthcare professionals from a Task Force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Resuscitation. 2015;96:328–340. doi: 10.1016/j.resuscitation.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 14.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–1251. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 15.Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957–2963. doi: 10.1001/jama.1993.03510240069035. [DOI] [PubMed] [Google Scholar]
- 16.Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–10. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 17.Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet Lond Engl. 1975;1:480–484. doi: 10.1016/S0140-6736(75)92830-5. [DOI] [PubMed] [Google Scholar]
- 18.Langeland H, Bergum D, Løberg M, Bjørnstad K, Damås JK, Mollnes TE, et al. Transitions between circulatory states after out-of-hospital cardiac arrest: Protocol for an observational, prospective cohort study. JMIR Res Protoc. 2018;7:e17. doi: 10.2196/resprot.8558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schulz J, Kvaløy JT, Engan K, Eftestøl T, Jatosh S, Kidanto H, et al. State transition modeling of complex monitored health data. J Appl Stat. 2019;47:1–21. doi: 10.1080/02664763.2019.1698523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Putter H, Fiocco M, Geskus RB. Tutorial in biostatistics: competing risks and multi-state models. Stat Med. 2007;26:2389–2430. doi: 10.1002/sim.2712. [DOI] [PubMed] [Google Scholar]
- 21.Jouan Y, Grammatico-Guillon L, Teixera N, Hassen-Khodja C, Gaborit C, Salmon-Gandonnière C, et al. Healthcare trajectories before and after critical illness: population-based insight on diverse patients clusters. Ann Intensive Care. 2019;9:126. doi: 10.1186/s13613-019-0599-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martinell L, Nielsen N, Herlitz J, Karlsson T, Horn J, Wise MP, et al. Early predictors of poor outcome after out-of-hospital cardiac arrest. Crit Care Lond Engl. 2017;21:96. doi: 10.1186/s13054-017-1677-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bro-Jeppesen J, Annborn M, Hassager C, Wise MP, Pelosi P, Nielsen N, et al. Hemodynamics and vasopressor support during targeted temperature management at 33°C Versus 36°C after out-of-hospital cardiac arrest: a post hoc study of the target temperature management trial*. Crit Care Med. 2015;43:318–327. doi: 10.1097/CCM.0000000000000691. [DOI] [PubMed] [Google Scholar]
- 24.R Core Team . R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2019. [Google Scholar]
- 25.Norman G, Monteiro S, Salama S. Sample size calculations: should the emperor’s clothes be off the peg or made to measure? BMJ. 2012;345:e5278. doi: 10.1136/bmj.e5278. [DOI] [PubMed] [Google Scholar]
- 26.Acheampong A, Vincent J-L. A positive fluid balance is an independent prognostic factor in patients with sepsis. Crit Care Lond Engl. 2015;19:251. doi: 10.1186/s13054-015-0970-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shen Y, Huang X, Zhang W. Association between fluid intake and mortality in critically ill patients with negative fluid balance: a retrospective cohort study. Crit Care. 2017;21:104. doi: 10.1186/s13054-017-1692-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tanguay-Rioux X, Grunau B, Neumar R, Tallon J, Boone R, Christenson J. Is initial rhythm in OHCA a predictor of preceding no flow time? Implications for bystander response and ECPR candidacy evaluation. Resuscitation. 2018;128:88–92. doi: 10.1016/j.resuscitation.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 29.Wibrandt I, Norsted K, Schmidt H, Schierbeck J. Predictors for outcome among cardiac arrest patients: the importance of initial cardiac arrest rhythm versus time to return of spontaneous circulation, a retrospective cohort study. BMC Emerg Med. 2015;15:3. doi: 10.1186/s12873-015-0028-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haas B, Wunsch H. How does prior health status (age, comorbidities and frailty) determine critical illness and outcome? Curr Opin Crit Care. 2016;22:500–505. doi: 10.1097/MCC.0000000000000342. [DOI] [PubMed] [Google Scholar]
- 31.Roberts BW, Kilgannon JH, Chansky ME, Mittal N, Wooden J, Parrillo JE, et al. Multiple organ dysfunction after return of spontaneous circulation in postcardiac arrest syndrome. Crit Care Med. 2013;41:1492–1501. doi: 10.1097/CCM.0b013e31828a39e9. [DOI] [PubMed] [Google Scholar]
- 32.Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, et al. Targeted temperature management at 33°C versus 36°C after cardiac arrest. N Engl J Med. 2013;369:2197–2206. doi: 10.1056/NEJMoa1310519. [DOI] [PubMed] [Google Scholar]
- 33.Lemiale V, Dumas F, Mongardon N, Giovanetti O, Charpentier J, Chiche J-D, et al. Intensive care unit mortality after cardiac arrest: the relative contribution of shock and brain injury in a large cohort. Intensive Care Med. 2013;39:1972–1980. doi: 10.1007/s00134-013-3043-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary Figure 1. Flowchart summarizing patient enrollment and exclusion. CA: Cardiac arrest. ICU: Intensive care unit. ECMO: Extracorporeal membranous oxygenation. OHCA: Out-of-hospital cardiac arrest. PAC: Pulmonary artery catheter. VAD: Ventricular assist device.
Additional file 2: Supplementary Figure 2. Heat-map showing which of the variables in the circulatory state model that categorizes the patient in a worse circulatory state. IABP: Intra-aortic balloon pump. MAP: Mean arterial pressure.
Additional file 3: Supplementary Figure 3. Sequence plot for cluster 1 to 4, showing sequences of longitudinal succession of circulatory states, i.e. trajectory, for every patient in the respective cluster. A. Cluster 1. B. Cluster 2. C. Cluster 3. D. Cluster 4. ICU: Intensive care unit.
Additional file 4: Supplementary Table 1. Demographic and mortality for cluster 1 to 4. * Systolic blood pressure <90 mmHg or in need of fluids and/or vasopressors to maintain systolic blood pressure >90 mmHg. † Comatose were patients that were intubated and gave no contact (GCS <8). ER: Emergency room. GCS: Glasgow coma scale. ROSC: Return of spontaneous circulation. SD: Standard deviation. SAPS: Simplified Acute Physiology Score.
Additional file 5: Supplementary Table 2. Sequential Organ Failure Assessment score. * In sedated patients daily Glasgow Coma Scale is based on pre-sedation score. SOFA: Sequential Organ Failure Assessment. Q1–Q3: first to third quartiles.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.