Abstract
Background: Nursing students who suffer from co-occurring anxiety experience added difficulties when communicating and interacting with others in a healthy, positive, and meaningful way. Previous studies have found strong positive correlations between Internet addiction (IA) and anxiety, suggesting that nursing students who report severe IA are susceptible to debilitating anxiety as well. To date, however, network analysis (NA) studies exploring the nature of association between individual symptoms of IA and anxiety have not been published.
Objective: This study examined associations between symptoms of IA and anxiety among nursing students using network analysis.
Methods: IA and anxiety symptoms were assessed using the Internet Addiction Test (IAT) and the Generalized Anxiety Disorder Screener (GAD-7), respectively. The structure of IA and anxiety symptoms was characterized using “Strength” as a centrality index in the symptom network. Network stability was tested using a case-dropping bootstrap procedure and a Network Comparison Test (NCT) was conducted to examine whether network characteristics differed on the basis of gender and by region of residence.
Results: A total of 1,070 nursing students participated in the study. Network analysis showed that IAT nodes, “Academic decline due to Internet use,” “Depressed/moody/nervous only while being off-line,” “School grades suffer due to Internet use,” and “Others complain about your time spent online” were the most influential symptoms in the IA-anxiety network model. Gender and urban/rural residence did not significantly influence the overall network structure.
Conclusion: Several influential individual symptoms including Academic declines due to Internet use, Depressed/moody/nervous only while being off-line, School grades suffering due to Internet use and Others complain about one's time spent online emerged as potential targets for clinical interventions to reduce co-occurring IA and anxiety. Additionally, the overall network structure provides a data-based hypothesis for explaining potential mechanisms that account for comorbid IA and anxiety.
Keywords: internet addiction, anxiety, nursing students, network analysis, symptoms
Introduction
In recent decades, Internet addiction (IA) has become a common problem among adolescent and young adults. IA refers to an inability to control Internet use and a maladaptive pattern of Internet use that may result in clinically significant impairment or distress (1, 2). IA is associated with a range of negative health outcomes including poor mental health (e.g., anxiety and depression), reduced physical activity, changed eating habits, impaired cognition, poor academic performance, and increased risk for obesity and diabetes (3–6); in light of its prevalence and consequences, the treatment and prevention of IA have generated increased attention in psychiatry research and practice.
IA is comprised of heterogeneous signs and symptoms such as excessive Internet use, withdrawal symptoms (e.g., feelings of anger, tension, and/or depression) when a computer is inaccessible, tolerance (e.g., the need for advanced computer equipment and software, or increased hours of use to feel satisfied) and negative repercussions (e.g., arguments, lying, poor achievement, social isolation, and fatigue) due to excessive Internet use (7).
Traditionally, researchers have weighed individual symptoms of IA equally and evaluated IA severity on the basis of calculating total scores from responses to items on associated measures, Unfortunately, this approach obscures meaningful associations between individual symptoms and the identification of individual symptoms that may be more critical to the onset and or maintenance of comorbid experiences of distress such as anxiety (8). Network analysis (NA) has emerged as a novel approach to conceptualizing psychological phenomena in a manner that addresses these limitations of traditional approaches. NA has the potential to map specific relationships among individual symptoms of a disorder and identify targets for treatment (9). Furthermore, NA tools can be used to extract the structure of psychiatric disturbances from clinical data (10, 11) that highlights only meaningful associations between individual symptoms within and/or between disorders (12).
In network theory, central symptoms are more likely to activate other symptoms; thus central symptoms are thought to play a major role in causing the onset and/or maintenance of a syndrome. NA has been implemented in studying several psychiatric disorders, including depression (13–16), anxiety (17, 18), and IA symptoms among adolescents with autism spectrum disorders (19).
As a profession, nursing is expected to have an important role in health promotion as well as the reduction of IA and its negative health outcomes. However, if nursing students suffer from IA, this may act as a barrier to effective learning and the capacity to deliver health services effectively. Individuals with heightened anxiety often seek recreational activities to relieve their stress (20); thus, many people turn to the Internet when they suffer from anxiety symptoms due, in part, to the anonymous nature of online activities (21). Previous studies have found strong positive correlations between IA and anxiety, suggesting that nursing students who report severe IA are susceptible to debilitating anxiety as well (22–24). In order to reduce the co-occurrence of IA and anxiety, prevent associated negative outcomes, and develop specific treatments that are effective for those in need, it would be useful to understand particular symptoms of anxiety and IA that are most important in fostering each problem and their co-occurrence. To date, however, NA studies exploring the nature of association between individual symptoms of IA and anxiety have not been published.
Toward redressing this gap in the literature, this study examined item-level relationships between IA and anxiety among nursing students based on NA. In particular, the focus was upon identifying those symptoms that were most central within the IA-anxiety network model in tandem with evaluating the potential impact of gender and region of residence as sociodemographic influences on the observed network model.
Methods
Study Design
This was an online, multi-center, cross-sectional study conducted between September 14 and October 7, 2020. All nursing students registered in nursing schools of five universities (Peking University, Capital Medical University, Jilin University, Lanzhou University, and Wuhan University) in China were consecutively invited to participate in this study. The survey was conducted using the WeChat-based “QuestionnaireStar” program. WeChat is a widely used social communication application with 1.2 billion users in China. Participants who met the following criteria were included: (1) undergraduate nursing students in participating nursing schools, (2) ability to understand Chinese and willingness to provide written informed consent. To reduce missing values in the questionnaire, following other peer-reviewed, published studies (25, 26) all questions were set to require a mandatory response, though participants could provide an out-of-range values if they preferred not to answer specific items. The local research ethics committee permitted this approach, as long as the response requirements were mentioned clearly, at the outset, in the informed consent, the survey was conducted on a voluntary basis, and participants could withdraw from the study at any time, for any reason (e.g., they do not want to answer particular items). The study protocol was approved by IRBs of the participating nursing schools.
Measurement Tools
IA was measured using the Chinese version of the self-report Internet Addiction Test (IAT) (27, 28). The IAT comprises 20 items, each of which includes “1 = rarely” and “5 = always” as anchors. A higher total score indicates more severe IA. Anxiety symptoms were measured with the Chinese version of the seven-item Generalized Anxiety Disorder scale (GAD-7) (29, 30). Items were rated between “0= not at all” and “3= almost every day,” with a higher score indicating more severe anxiety symptoms.
Network Estimation
All analyses were conducted using R (Version 4.0.3) (31). The network structure of IAT and GAD data was estimated by using the Enhanced Least Absolute Shrinkage and Selection Operator (eLASSO) method (11). To estimate and visualize the network, R-package qgraph (Version 1.6.5) (32) and bootnet (Version 1.4.3) (33) were used. The algorithm used the penalty parameter to obtain sparsity and the Extended Bayes Information Criterion (EBIC) (i.e., a measure of goodness of fit) to select the best set of neighbor factors for each node (symptom). When each node (a node represents a symptom) is connected to a number of other nodes through edges (an edge represents specific links between two symptoms) with different weights, the final network is constructed automatically and indicates the strength of direct associations between nodes (11). The network was visualized using the Fruchterman-Reingold algorithm (33). In the network layout, edge thickness was used to indicate the strength of an association between nodes. The edge color indicated the direction of an association (i.e., green edges indicated positive associations, and red edges indicated negative associations) (32). Symptoms with stronger and more frequent associations with other nodes were placed closer to each other and more concentrated in the network.
NA provides quantitative centrality indicators for each node based on the unique configuration of a network. In NA, network centrality measures include Strength, Betweenness, and Closeness. Strength is the sum of the weight of all direct connections between a specific symptom and others. Betweenness indicates how often a symptom lies on the shortest indirect path with another node. Closeness indicates how strongly a node is indirectly connected to other nodes in a network (i.e., the inverse of the sum of the distances). Centrality measures are reported as standardized values (z-scores). Given that recent studies (34) concluded that Betweenness and Closeness centrality are unsuitable in psychological networks, Strength was the only centrality index used in this study. In addition, the predictability of each node was estimated using the package “mgm.” Predictability was defined as the variance in a node that is explained by all other nodes in the network (35).
Estimation of Network Accuracy and Stability
The stability of node attributes was estimated using the case dropping bootstrap procedure. If most samples can be excluded from the dataset without observing significant changes in the centrality index of the node, the network is considered to be stable. Stability is represented graphically and quantified by calculating the relevant stability coefficient (CS-C). The accuracy of an edge weight is estimated using a non-parametric bootloader to calculate its confidence interval (CI). Observations are randomly resampled to create multiple new data sets from which a 95% CI can be calculated. In this NA, we performed 1,000 permutations and used a bootstrap differential test to evaluate differences in network properties (15).
Comparisons of Network Characteristics by Gender and Region of Residence
We used Network Comparison Tests (NCT) to conduct exploratory analyses examining whether network characteristics differ as a function of gender and region of residence (rural vs. urban). First, we compared the distribution of edge weights in each network to characterize the network structure. Then, we compared differences in strength for each edge of networks between women vs. men and rural vs. urban areas, after controlling for multiple tests using a Holm-Bonferroni correction.
Results
Study Sample
A total of 1,070 nursing students (805 women, 265 men) completed the GAD and IAT; of these, 42.7% were from rural areas while 47.3% were from urban regions. The mean GAD-7 total score was 3.1 (SD = 3.9) and mean IAT total score was 40 (SD = 12.8) (Table 1).
Table 1.
Sample characteristics.
| Age, mean (SD) | 19.7(1.4) |
| Female Gender, % | 75.2% |
| Only child, % | 42.7% |
| Rural residence, % | 42.7% |
| School grade, % | |
| First year | 26.8% |
| Second year | 22.1% |
| Third year | 23.3% |
| Fourth year | 27.8% |
| GAD-7 total, mean (SD) | 3.1(3.9) |
| IAT total, mean (SD) | 40.1(12.8) |
Network Structure and Centrality Measure Analysis
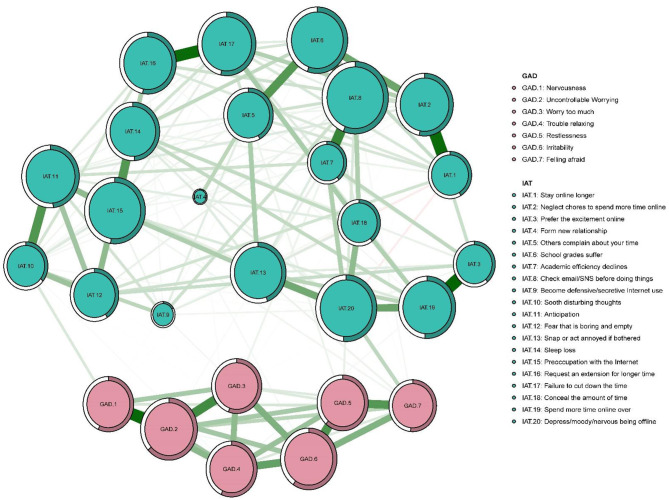
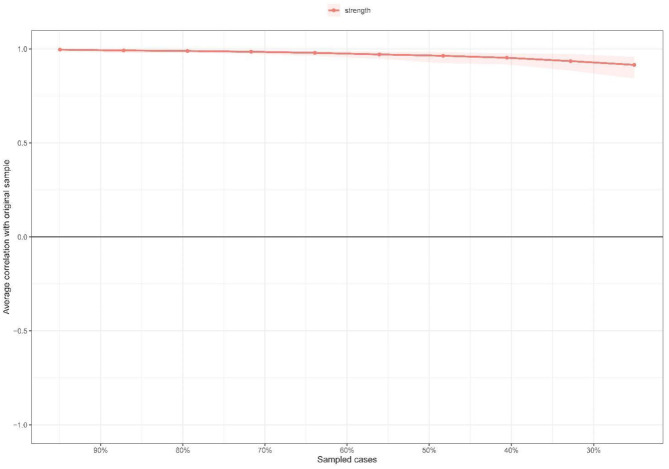
The IA network was estimated with an EBICglasso model (Figure 1). The predictability of symptoms is shown as ring-shaped pie charts in Figure 1. The mean predictability was 0.47 in nursing students. Figure 2 shows the network centrality index of strength. We also investigated the stability of the network analysis, and found an excellent level of stability (i.e., CS-coefficient = 0.75), indicating that 75% of the sample could be dropped without the network structure changing to a significant extent compared to the original structure (Figure 3).
Figure 1.
Estimated network model for Internet addiction in nursing students (n = 1,070). Symptom network of Internet addiction and anxiety symptoms in nursing students in post-COVID-19 pandemic era in China. The survey was conducted between September 14 and October 7, 2020. Ring-shaped pie charts represent predictability (a fully filled dark ring would indicate that 100% of the symptom's variance is explained by its intercorrelations with the other symptoms in the network). In the diagram symptom node with stronger connections are closer to each other. The green node denotes the IAT items; the pink node denote the GAD-7 items. The dark green lines represent positive correlations. The red lines represent negative correlations. The edge thickness represents the strength of the association between symptom nodes.
Figure 2.
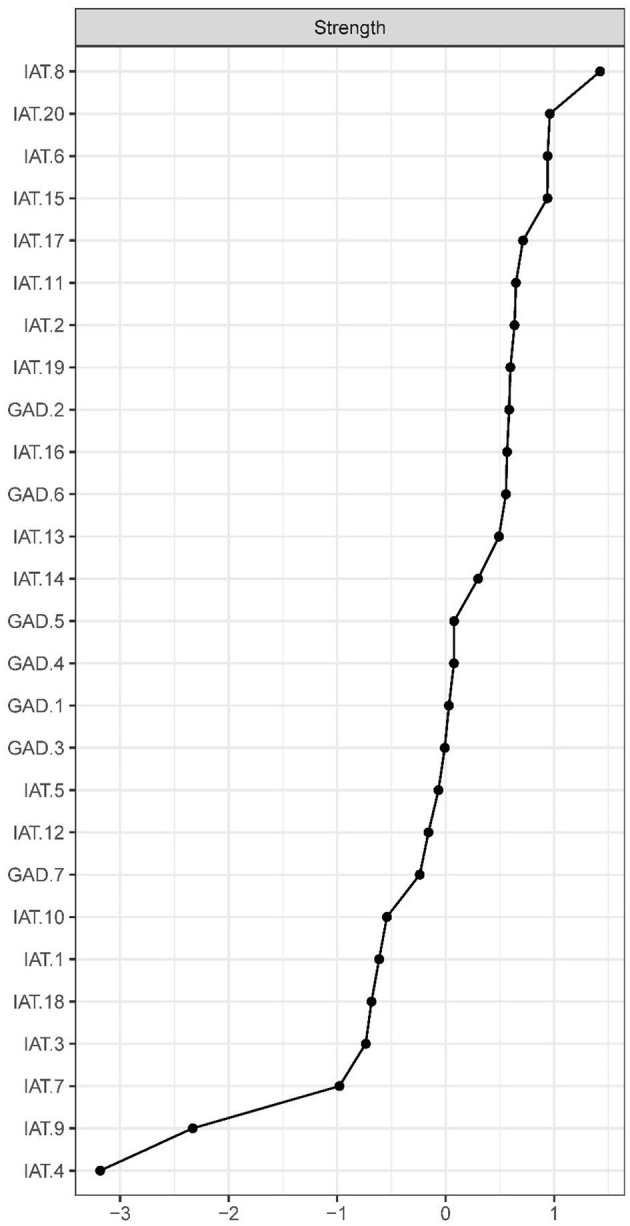
Centrality indices of Internet addiction, shown as standardized values z scores.
Figure 3.
Stability of centrality indices by case dropping subset bootstrap. The x-axis represents the percentage of cases of original sample used at each step. The y-axis represents the average of correlations between the centrality indices from the original network and the centrality indices from the networks that were re-estimated after dropping increasing percentages of cases. Each line indicates the correlations of strength and bridge strength, while areas indicate 95% CI.
With the IA-anxiety model, the node IAT-2 (“Neglect chores to spend more time online”) had the strongest connections with IAT-1 (“Stay online longer than intended”), and IAT-6 (“School grades suffer due to Internet use”). Although nodes IAT-16 (“Request to extension for longer time spent online”) and IAT-17 (“Failure to cut down the time spent online”) were situated at the periphery of the network, these two items were directly connected. Node IAT-19 (“Spend more time online over going out with others”) was connected with IAT-13 (“Prefer to excitement online to the time with others”) and IAT-20 (“Depressed/moody/nervous only while being off-line”). Nodes IAT-11 (“Anticipate for future online activities”) and IAT-10 (“Sooth disturbing about your Internet use”) were highly interconnected. Nodes IAT-7 (“Check email/SNS before doing things you need to do”) and IAT-8 (“Academic decline due to Internet use”) were also strongly interconnected and had a “U” shape relationship with IAT-6 (“School grades suffer due to Internet use”) and IAT-5 (“Others complain about your time spend online”). Moreover, node IAT-1 (“Stay online longer than intended”) was negatively associated with IAT-18 (“Conceal the amount of time spent online”) and IAT-20 (“Depressed/moody/nervous only while being off-line”). Within the IA-anxiety network model, node GAD-2 (“Uncontrollable worrying”) had the strongest, most direct connections with GAD-1 (“Nervousness”) and GAD-3 (“Worry too much”). Nodes GAD-5 (“Restlessness”) and GAD-7 (“feeling afraid”) were strongly interconnected and were placed within a cluster that comprised GAD-4 (“Trouble relaxing”) and GAD-6 (“Irritability”).
In the IA and anxiety network model, node IAT-20 (“Depressed/moody/nervous only while being off-line”) was most strongly related to node GAD-7 (“feeling afraid”) (average edge weight = 0.094), followed by the connection between nodes IAT-10 (“Sooth disturbing about your Internet use”) and GAD-1 (“Nervousness”) (average edge weight = 0.056), and the connection between nodes IAT-13 (“Prefer to excitement online to the time with others”) and GAD-7 (“feeling afraid”) (average edge weight = 0.029).
In terms of strength, node IAT-8 (“Academic decline due to Internet use”) was most influential (Figure 2), followed by nodes IAT-20 (“Depressed/moody/nervous only while being off-line”), IAT-6 (“School grades suffer due to Internet”), and IAT-5 (“Others complain about your time spend online”) (Figure 2), all of which emerged as central symptoms in understanding the IA-anxiety network model in nursing students. In contrast, several other symptoms were marginal, such as IAT-7 (“Check email/SNS before doing things you need to do”), IAT-4 (“Form new relationship with online users”), and IAT-9 (“Become defensive/secretive about your Internet use”).
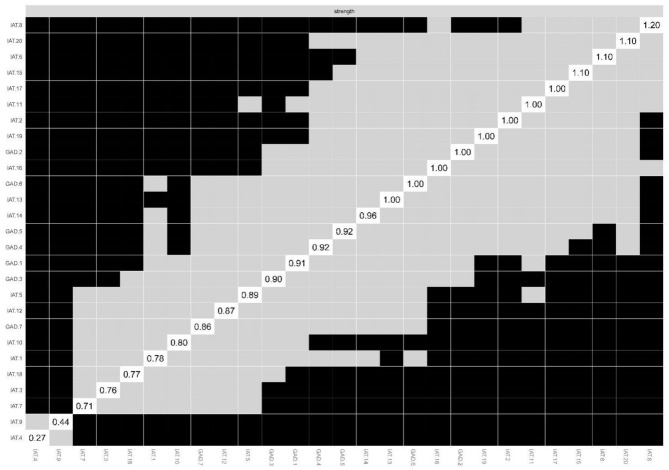
Network Accuracy and Stability
Bootstrapped 95%CIs for estimated edge-weights suggested that the network model was reliable and stable. The bootstrap difference test showed most of the comparisons between edge weights were statistically significant (Figure 4).
Figure 4.
Non-parametric bootstrapped difference test for strength. Gray boxes indicate no difference between nodes, whereas black boxes indicate significant difference (α = 0.05). Values reported in the diagonal represent the strength values of each node.
Gender and Residence Effects
In the comparison of network models between female and male nursing students, there were no significant differences in network global strength (p = 0.865) or the distribution of edge weights (p = 0.652; Supplementary Figures 1–3). Subdividing the sample according to urban vs. rural residence, no significant differences were found in network global strength (p = 0.301) or the distribution of edge weights (p = 0.484). Plots are shown in Supplementary Figures 4–6.
Discussion
To the best of our knowledge, this study is the first to use NA as a means of examining associations between IA and anxiety at individual symptom level among nursing students. Analyses indicated nodes IAT-8 (“Academic decline due to Internet use”), IAT-20 (“Depressed/moody/nervous only while being off-line”), IAT-6 (“School grades suffer due to Internet use”), and IAT-5 (“Others complain about your time spend online”) were the most influential symptoms within the IA-anxiety network. Additionally, neither gender nor urban vs. rural residence had a significant impact on the overall network structure.
The NA revealed nodes IAT-8 (“Academic performance decline due to Internet use”) and IAT-6 (“School grades suffer due to Internet use”) as the most central symptoms in the IA-anxiety network, which is consistent with previous findings in both research on autism spectrum disorder patients and the general population (19). Previous studies have found bidirectional relations between poor academic performance and IA (36, 37), which could account for our findings. On the one hand, in order to avoid facing academic demands and reduce stress related to academic work, students with greater academic challenges may be at a higher risk for increasing Internet usage (38, 39). On the other hand, increasing Internet usage may lead to declines in academic performance (40). As such, academic performance declines may be a critical intervention target for educators and health professionals treating students who experience co-occurring IA and anxiety.
Node IAT-20 (“Depressed/moody/nervous only while being offline”) was identified as one of the most central symptoms in the IA-anxiety network of nursing students, consistent with previous NA findings in college student and adolescent samples (19). Also, this finding dovetails with the identification of withdrawal symptoms such as feelings of anger, tension, and/or depression when the computer is inaccessible as a widely accepted criterion in assessing IA syndrome (41). When college students experience stress or depression due to high levels of academic pressure, they may be susceptible to accessing the Internet in order to escape from such demands (42). When they can no longer use the Internet as an avoidant coping strategy, risk for loneliness, depressed mood, and/or anxiety symptoms may increase (42, 43).
A major clinical feature of IA is the loss of control (41, 44). In this IA-anxiety network control was a prominent theme in the IA-anxiety symptom network of nursing students. For instance, node IAT-5 (“Others complain about your time spend online”) emerged as a central symptom in the IA-anxiety network. Other important strong edges identified in this study were the connections between IAT-16 (“Request an extension for longer time spent online”) and IAT-17 (“Failure to cut down the time spent online”) as well as between IAT-2 (“Neglect chores to spend more time online”) and IAT-1 (“Stay online longer than you intend”); both of these connections underscore excessive Internet use and/or increased hours of Internet use as important criteria for IA (7, 41, 44). Previous NA findings on problematic smartphone use showed that excessive screen time on smartphones was likely to trigger problematic smartphone use though students with high self-control may be less likely to develop problematic smartphone use (45), in line with our IA results in this study. As such, reducing students' excessive Internet use and strengthening their self-control should be incorporated within programs designed to prevent and treat comorbid IA and anxiety.
The IA-anxiety network revealed strong edges that serve as hypotheses for understanding mechanisms that contribute to comorbid IA and anxiety among nursing students. For example, it can be hypothesized that the edge connecting IAT-3 (“Prefer the excitement online to the time with others”) and IAT-9 (“Spend more time online over going out with others”) reflects a bi-directional relationship between increased digital social engagements and decreased real-world social engagements. A possible reason for this complementary relationship is that students who prefer online social networks experience more real-world interpersonal problems such as conflicts with parents (46). In addition, the Internet may provide those who have experienced social interaction difficulties with opportunities to avoid these challenges (47). Our results highlighted potential associations between poor social skills and excessive Internet use (43). Consequently, social skills training could be helpful in increasing at-risk nursing students' involvement in offline social activities (48) and reducing the severity of IA-anxiety comorbidity.
Previous studies found the co-occurrence of IA and anxiety symptoms is common (43, 49). In this NA, node GAD-7 (“Feeling afraid”) had a strong connection with node IAD-20 (“Depressed/moody/nervous only while being offline”). It may be that nursing students who display excessive Internet use are more neurotic, less extraverted, and more socially anxious and lonely than peers who do not show these excesses and gain more support from online social networks (23, 24). Furthermore, nursing students who feel more afraid may spend more time online to escape from real world demands (50) in line with evidence that socially anxious individuals often prefer to online rather than face-to-face communications (43).
A unique aspect of this study was its data collection phase during the Coronavirus disease (COVID-19) pandemic. The pandemic has led to many sudden, dramatic changes in lifestyle, teaching and learning as well as corresponding elevations in psychological distress experiences including anxiety and IA (5, 22, 51, 52). Within this context, our findings may have clinical significance in developing appropriate interventions to reduce co-occurring anxiety and IA among nursing students during pandemics or other societal upheavals. For example, establishing a reasonable activity schedule each day, a regular sleep routine, and opportunities for recreation and relaxation during the pandemic may help to reduce risks for anxiety and IA (53). In addition, self-monitoring and regulating one's time and use of the Internet may facilitate self-control and time management (53). Reducing access to the Internet and/or placing smartphones/devices in inconvenient settings that reduce their immediacy and availability may aid in alleviating co-occurring IA and anxiety (53) among nursing students who have less self-control over Internet use.
This study has several strengths. First, because the study sample was large and featured a multi-center design, findings may be more generalizable to nursing students in China than smaller, single site research would. Second, analyses supported both the stability and accuracy of the observed IA-anxiety network. In addition, NCT analyses explicitly tested both gender and urban vs. rural residence as sociodemographic influences on the IA-anxiety network structure of nursing students. Associated analyses indicated that the observed network does not vary on the basis of these factors.
This study also has several limitations. First, for logistical reasons, following other studies (54–56) anxiety and IA symptoms were measured via self-report responses on questionnaires during the post COVID-19 pandemic period; as such, it is possible that associations between item responses were magnified due to common method variance. Therefore, our findings may not be generalizable to interview-based assessments or non-pandemic contexts. Second, due to the non-experimental, cross-sectional study design, causal relations between symptoms of IA and anxiety could not be determined. Future longitudinal studies are needed to assess changes in IA-anxiety symptom patterns over time. Third, given the current research focus, participants were recruited from nursing schools, rather than psychiatric settings. Thus, NA findings from nursing students in this research may not be applicable to psychiatric samples diagnosed with IA and/or anxiety disorders. Finally, although mandatory responses were required in completing the online survey, participants were able to provide out of range values (which would be treated as missing values) if they encountered a question they did not want to answer. However, this limitation was not a function of the current survey set-up and can occur when interviews or surveys involve non-mandatory responses.
In conclusion, this NA study revealed (1) academic declines due to Internet use, (2) depression/moodiness/nervousness only while being off-line, (3) school grades suffering due to Internet use and (4) others' complaints about one's time spent online as the most prominent nodes and potentially useful targets for curriculum and/or clinical interventions designed to help nursing students who are struggling with co-occurring IA and anxiety. On this basis, interventions involving additional academic support and/or cognitive behavioral therapy for internet addiction (CBT-IA) may have utility in addressing academic declines, poor time management, distress related to being offline, and internet preoccupation among at-risk or distressed nursing students (57–59). Additionally, analyses of the IA-anxiety network structure provided an empirically based foundation for future studies investigating the development and maintenance of comorbid IA and anxiety symptoms among nursing students.
Data Availability Statement
The Institutional Review Boards (IRB) that approved the study prohibit the authors from making the research data set publicly available. Readers and all interested researchers may contact Dr. Yu-Tao Xiang (xyutly@gmail.com) for details. Dr. Xiang could apply to the Institutional Review Board (IRB)s for the release of the data.
Ethics Statement
The study protocol was approved by IRBs of the participating nursing schools. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
HC, WB, ZW, LH, LC, B-XY, and Y-TX: conceptualization, methodology, and software. HC, WB, and Y-TX: data curation and writing original draft preparation. H-TX, SL, QZ, Z-MG, MJ, and HZ: visualization and investigation. FA and Y-TX: supervision. HC, Y-JZ, and PC: software and validation. TC, TJ, and Y-LT: writing—reviewing and editing. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
Funding. The study was supported by the National Science and Technology Major Project for investigational new drug (2018ZX09201-014), the Beijing Municipal Science & Technology Commission (No. Z181100001518005), the 2020 Higher Education Teaching Achievement Cultivation Project of Gansu Province, the Fundamental Research Funds for the Central Universities (2020YJ065), and the University of Macau (MYRG2019-00066-FHS).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.723355/full#supplementary-material
References
- 1.Laconi S, Rodgers RF, Chabrol H. The measurement of Internet addiction: a critical review of existing scales and their psychometric properties. Comput Human Behav. (2014) 41:190–202. 10.1016/j.chb.2014.09.026 [DOI] [Google Scholar]
- 2.Young KS. Internet addiction: a new clinical phenomenon and its consequences. Am Behav Sci. (2004) 48:402–15. 10.1177/0002764204270278 [DOI] [Google Scholar]
- 3.Cheng C, Li AY. Internet addiction prevalence and quality of (real) life: a meta-analysis of 31 nations across seven world regions. Cyberpsychol Behav Soc Netw. (2014) 17:755–60. 10.1089/cyber.2014.0317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Colizzi M, Sironi E, Antonini F, Ciceri ML, Bovo C, Zoccante L. Psychosocial and behavioral impact of COVID-19 in autism spectrum disorder: an online parent survey. Brain Sci. (2020) 10:341. 10.3390/brainsci10060341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dubey S, Biswas P, Ghosh R, Chatterjee S, Dubey MJ, Chatterjee S, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr. (2020) 14:779–88. 10.1016/j.dsx.2020.05.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mamun MA, Hossain MS, Moonajilin MS, Masud MT, Misti JM, Griffiths MD. Does loneliness, self-esteem and psychological distress correlate with problematic internet use? A Bangladeshi survey study. Asia-Pacific Psychiatry. (2020) 12:e12386. 10.1111/appy.12386 [DOI] [PubMed] [Google Scholar]
- 7.Block JJ. Issues for DSM-V: internet addiction. Am J Psychiatry. (2008) 165:306–7. 10.1176/appi.ajp.2007.07101556 [DOI] [PubMed] [Google Scholar]
- 8.Beard C, Millner AJ, Forgeard MJ, Fried EI, Hsu KJ, Treadway M, et al. Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychol Med. (2016) 46:3359–69. 10.1017/S0033291716002300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fried EI, Nesse RM, Zivin K, Guille C, Sen S. Depression is more than the sum score of its parts: individual DSM symptoms have different risk factors. Psychol Med. (2014) 44:2067–76. 10.1017/S0033291713002900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Borsboom D.C. A. O. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. (2013) 9:91–121. 10.1146/annurev-clinpsy-050212-185608 [DOI] [PubMed] [Google Scholar]
- 11.van Borkulo CD, Borsboom D, Epskamp S, Blanken TF, Boschloo L, Schoevers RA, et al. A new method for constructing networks from binary data. Sci Rep. (2014) 4:5918. 10.1038/srep05918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Epskamp S, Kruis J, Marsman M. Estimating psychopathological networks: be careful what you wish for. PLoS ONE. (2017) 12:e0179891. 10.1371/journal.pone.0179891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Belvederi Murri M, Amore M, Respino M, Alexopoulos GS. The symptom network structure of depressive symptoms in late-life: results from a European population study. Mol Psychiatry. (2020) 25:1447–56. 10.1038/s41380-018-0232-0 [DOI] [PubMed] [Google Scholar]
- 14.Galimberti C, Bosi MF, Caricasole V, Zanello R, Dell'Osso B, Vigano CA. Using network analysis to explore cognitive domains in patients with unipolar versus bipolar depression: a prospective naturalistic study. CNS Spectr. (2020) 25:380–91. 10.1017/S1092852919000968 [DOI] [PubMed] [Google Scholar]
- 15.Mullarkey MC, Marchetti I, Beevers CG. Using network analysis to identify central symptoms of adolescent depression. J Clin Child Adolesc Psychol. (2019) 48:656–68. 10.1080/15374416.2018.1437735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang Y, Hu Z, Feng Y, Wilson A, Chen R. Changes in network centrality of psychopathology symptoms between the COVID-19 outbreak and after peak. Mol Psychiatry. (2020) 25:3140–9. 10.1038/s41380-020-00881-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Price M, Legrand AC, Brier ZMF, Hebert-Dufresne L. The symptoms at the center: examining the comorbidity of posttraumatic stress disorder, generalized anxiety disorder, and depression with network analysis. J Psychiatr Res. (2019) 109:52–8. 10.1016/j.jpsychires.2018.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith KE, Mason TB, Crosby RD, Cao L, Leonard RC, Wetterneck CT, et al. A comparative network analysis of eating disorder psychopathology and co-occurring depression and anxiety symptoms before and after treatment. Psychol Med. (2019) 49:314–24. 10.1017/S0033291718000867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hirota T, McElroy E, So R. Network analysis of internet addiction symptoms among a clinical sample of Japanese adolescents with autism spectrum disorder. J Autism Dev Disord. (2020) 51:2764–772. 10.1007/s10803-020-04714-x [DOI] [PubMed] [Google Scholar]
- 20.Bryant J, Zillmann D. Using television to alleviate boredom and stress: selective exposure as a function of induced excitational states. J Broadcast Electr Media. (1984) 28:1–20. 10.1080/08838158409386511 [DOI] [Google Scholar]
- 21.Young KS, Rogers RC. The relationship between depression and Internet addiction. Cyberpsychol Behav. (1998) 1:25–8. 10.1089/cpb.1998.1.25 [DOI] [Google Scholar]
- 22.Ghosh A. COVID-19 pandemic and an early career mental health researcher from a low and middle income country: is there any light at the end of the tunnel? Asia-Pacific Psychiatry. (2020). 10.1111/appy.12424. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Javaeed A, Zafar MB, Iqbal M, Ghauri SK. Correlation between Internet addiction, depression, anxiety and stress among undergraduate medical students in Azad Kashmir. Pak J Med Sci. (2019) 35:506–9. 10.12669/pjms.35.2.169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Younes F, Halawi G, Jabbour H, El Osta N, Karam L, Hajj A, et al. Internet addiction and relationships with insomnia, anxiety, depression, stress and self-esteem in university students: a cross-sectional designed study. PLoS ONE. (2016) 11:e0161126. 10.1371/journal.pone.0161126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Leeuw ED, Hox JJ, Boeve A. Handling do-not-know answers: exploring new approaches in online and mixed-mode surveys. Soc Sci Comput Rev. (2016) 34:116–132. 10.1177/0894439315573744 [DOI] [Google Scholar]
- 26.Lund E, Gram IT. Response rate according to title and length of questionnaire. Scand J Soc Med. (1998) 26:154–60. 10.1177/14034948980260020401 [DOI] [PubMed] [Google Scholar]
- 27.Chin F, Leung CH. The concurrent validity of the Internet Addiction Test (IAT) and the Mobile Phone Dependence Questionnaire (MPDQ). PLoS ONE. (2018) 13:e0197562. 10.1371/journal.pone.0197562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lai CM, Mak KK, Watanabe H, Ang RP, Pang JS, Ho RC. Psychometric properties of the internet addiction test in Chinese adolescents. J Pediatr Psychol. (2013) 38:794–807. 10.1093/jpepsy/jst022 [DOI] [PubMed] [Google Scholar]
- 29.He XY, Li CB, Qian J, Cui HS. Wu WY. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatient. Shanghai Arch Psychiatry. (2010) 22:3. [Google Scholar]
- 30.Lowe B, Decker O, Muller S, Brahler E, Schellberg D, Herzog W, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. (2008) 46:266–74. 10.1097/MLR.0b013e318160d093 [DOI] [PubMed] [Google Scholar]
- 31.R Core Team . R: A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing; (2020). [Google Scholar]
- 32.Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D. qgraph: network visualizations of relationships in psychometric data. J Stat Softw. (2012) 48:1–18. 10.18637/jss.v048.i04 [DOI] [Google Scholar]
- 33.Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods. (2018) 50:195–212. 10.3758/s13428-017-0862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bringmann LF, Elmer T, Epskamp S, Krause RW, Schoch D, Wichers M, et al. What do centrality measures measure in psychological networks? J Abnorm Psychol. (2019) 128:892. 10.1037/abn0000446 [DOI] [PubMed] [Google Scholar]
- 35.Haslbeck JMB, Waldorp LJ. mgm: estimating time-varying mixed graphical models in high-dimensional data. J Stat Softw. (2020) 93:1–49. 10.18637/jss.v093.i08 [DOI] [Google Scholar]
- 36.Grant JE, Lust K, Chamberlain SR. Problematic smartphone use associated with greater alcohol consumption, mental health issues, poorer academic performance, and impulsivity. J Behav Addict. (2019) 8:335–342. 10.1556/2006.8.2019.32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Samaha M, Hawi NS. Relationships among smartphone addiction, stress, academic performance, and satisfaction with life. Comput Human Behav. (2016) 57:321–5. 10.1016/j.chb.2015.12.045 [DOI] [Google Scholar]
- 38.Jones S, Johnson-Yale C, Millermaier S, Pérez FS. Academic work, the Internet and US college students. Internet High Educ. (2008) 11:165–77. 10.1016/j.iheduc.2008.07.001 [DOI] [Google Scholar]
- 39.Turner K, McCarthy VL. Stress and anxiety among nursing students: a review of intervention strategies in literature between 2009 and (2015). Nurse Educ Pract. (2017) 22:21–9. 10.1016/j.nepr.2016.11.002 [DOI] [PubMed] [Google Scholar]
- 40.Odaci H. Academic self-efficacy and academic procrastination as predictors of problematic internet use in university students. Comput Educ. (2011) 57:1109–13. 10.1016/j.compedu.2011.01.005 [DOI] [Google Scholar]
- 41.Young K. Internet addiction: diagnosis and treatment considerations. J Contemp Psychother. (2009) 39:241–6. 10.1007/s10879-009-9120-x [DOI] [Google Scholar]
- 42.Whang LS-M, Lee S, Chang G. Internet over-users' psychological profiles: a behavior sampling analysis on internet addiction. Cyberpsychol Behav. (2003) 6:143–50. 10.1089/109493103321640338 [DOI] [PubMed] [Google Scholar]
- 43.Weinstein A, Dorani D, Elhadif R, Bukovza Y, Yarmulnik A, Dannon P. Internet addiction is associated with social anxiety in young adults. Ann Clin Psychiatry. (2015) 27:4–9. 10.1093/med/9780199380183.003.0001 [DOI] [PubMed] [Google Scholar]
- 44.Young KS. Internet addiction: the emergence of a new clinical disorder. Cyberpsychol Behav. (1998) 1:237–44. 10.1089/cpb.1998.1.237 [DOI] [Google Scholar]
- 45.Huang S, Lai X, Xue Y, Zhang C, Wang Y. A network analysis of problematic smartphone use symptoms in a student sample. J Behav Addict. (2020) 9:1032-3. 10.1556/2006.2020.00098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yucens BUA. The relationship between internet addiction, social anxiety, impulsivity, self-esteem, and depression in a sample of Turkish undergraduate medical students. Psychiatry Res. (2018) 267:313–8. 10.1016/j.psychres.2018.06.033 [DOI] [PubMed] [Google Scholar]
- 47.Fioravanti G, Dettore D, Casale S. Adolescent Internet addiction: testing the association between self-esteem, the perception of Internet attributes, and preference for online social interactions. Cyberpsychol Behav Soc Netw. (2012) 15:318–23. 10.1089/cyber.2011.0358 [DOI] [PubMed] [Google Scholar]
- 48.Chou WJ, Huang MF, Chang YP, Chen YM, Hu HF, Yen CF. Social skills deficits and their association with Internet addiction and activities in adolescents with attention-deficit/hyperactivity disorder. J Behav Addict. (2017) 6:42–50. 10.1556/2006.6.2017.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Andreassen CS, Billieux J, Griffiths MD, Kuss DJ, Demetrovics Z, Mazzoni E, et al. The relationship between addictive use of social media and video games and symptoms of psychiatric disorders: a large-scale cross-sectional study. Psychol Addict Behav. (2016) 30:252. 10.1037/adb0000160 [DOI] [PubMed] [Google Scholar]
- 50.Glaser P, Liu JH, Hakim MA, Vilar R, Zhang R. Is social media use for networking positive or negative? Offline social capital and internet addiction as mediators for the relationship between social media use and mental health. N Z J Psychol. (2018) 47:11–7. [Google Scholar]
- 51.Alheneidi H, AlSumait L, AlSumait D, Smith AP. Loneliness and problematic internet use during COVID-19 lock-down. Behav Sci (Basel). (2021) 11:5. 10.3390/bs11010005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE. (2020) 15:e0231924. 10.2139/ssrn.3541120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Király O, Potenza MN, Stein DJ, King DL, Hodgins DC, Saunders JB, et al. Preventing problematic internet use during the COVID-19 pandemic: consensus guidance. Compr Psychiatry. (2020) 100:152180. 10.1016/j.comppsych.2020.152180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dalbudak E, Evren C. The relationship of Internet addiction severity with attention deficit hyperactivity disorder symptoms in turkish university students; impact of personality traits, depression and anxiety. Compr Psychiatry. (2014) 55:497–503. 10.1016/j.comppsych.2013.11.018 [DOI] [PubMed] [Google Scholar]
- 55.McNicol ML, Thorsteinsson EB. Internet addiction, psychological distress, and coping responses among adolescents and adults. Cyberpsychol Behav Soc Netw. (2017) 20:296–304. 10.1089/cyber.2016.0669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wu C-Y, Lee M-B, Liao S-C, Chang L-R. Risk factors of internet addiction among internet users: an online questionnaire survey. PLoS ONE. (2015) 10:e0137506. 10.1371/journal.pone.0137506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Putri APS, Poerwandari EK, Rusli E. Social anxiety and internet addiction: CBT intervention module development based on self-reflection. Adv Soc Sci Educ Human Res. (2018) 135:397–409. 10.2991/iciap-17.2018.38 [DOI] [Google Scholar]
- 58.Szász-Janocha C, Vonderlin E, Lindenberg K. Treatment outcomes of a CBT-based group intervention for adolescents with Internet use disorders. J Behav Addict. (2021) 9:978–89. 10.1556/2006.2020.00089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Young KS. Treatment outcomes using CBT-IA with Internet-addicted patients. J Behav Addict. (2013) 2:209–15. 10.1556/JBA.2.2013.4.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The Institutional Review Boards (IRB) that approved the study prohibit the authors from making the research data set publicly available. Readers and all interested researchers may contact Dr. Yu-Tao Xiang (xyutly@gmail.com) for details. Dr. Xiang could apply to the Institutional Review Board (IRB)s for the release of the data.