Abstract
Lassa arenavirus (LASV) is the cause of Lassa Fever in humans in West Africa. The multimammate mouse (Mastomys natalensis) is a reservoir host of LASV and the primary source of human infections. Humans are assumed to become infected due to contact with this animal or its excretions. Thus far, the available literature does not describe the sampling of feces as a means to detect LASV in M. natalensis populations. More evidence is needed to know if feces of naturally infected M. natalensis can be LASV-positive and an exposure risk to humans. This study sampled feces deposits in households from three villages in the LASV-endemic region of Faranah, Guinea. PCR analysis found 10 out of 88 samples to be positive for LASV, and sequencing showed clustering to previously identified Yarawelia and Dalafilani strains. We conclude that feces sampling is a viable, non-invasive method for the determination and sequencing of LASV strains.
Keywords: Lassa virus, Feces, Environmental sampling, Rodent, M. natalensis, Africa, Guinea
1. Introduction
Lassa arenavirus (LASV) is endemic to West Africa that causes up to 300,000 human Lassa Fever (LF) infections with approximately 5000 to 10,000 fatalities annually [1,2]. These numbers are likely underestimations as gaps in diagnostic tools, surveillance systems and access to health services in remote areas are frequent [2]. Misdiagnosis of cases was exemplified in 2019 when a Guinean man died of LF after being mistakenly diagnosed with malaria, typhoid fever and Ebola [3]. Mathematical models estimate that 897,700 human infections occur annually [4]. LASV has a case-fatality rate as high as 50% during epidemics [5]. LF has an incubation period of 6–21 days, with 80% of infected persons being asymptomatic. Symptoms may present as sore throat and fever, with rapid onset of congestion, vomiting, diarrhea, seizures and death [1]. The multimammate mouse (Mastomys natalensis) is the primary reservoir of LASV contributing to human infection. This rodent is widely distributed throughout sub-Saharan Africa where it lives in houses and agricultural fields [6]. Cohabitation of M. natalensis and humans presents opportunity for viral spillover, as studies show that the rodent sheds viral titers in its urine for up to seven days in laboratory conditions [7].
Detection methods of LASV within M. natalensis described throughout available literature primarily detail rodent biopsies and viral extraction from organ tissue or blood [8]. The literature has not described sampling of feces for LASV in natural conditions, but does show successful feces sampling of coronavirus RNA [9], rodent parvoviruses [10] and Morogoro arenavirus (MORV) in laboratory rodents. Genetic similarities between MORV and LASV suggest that the latter can be detected in M. natalensis feces as long as sampling occurs within 3 to 29 days post-infection [11]. Furthermore, LASV can survive outside the rodent host for several days in laboratory conditions [12]. In this study, we explored the possibility of detecting LASV in feces of naturally infected M. natalensis by sampling and testing feces in dwellings of an endemic area.
2. Methods
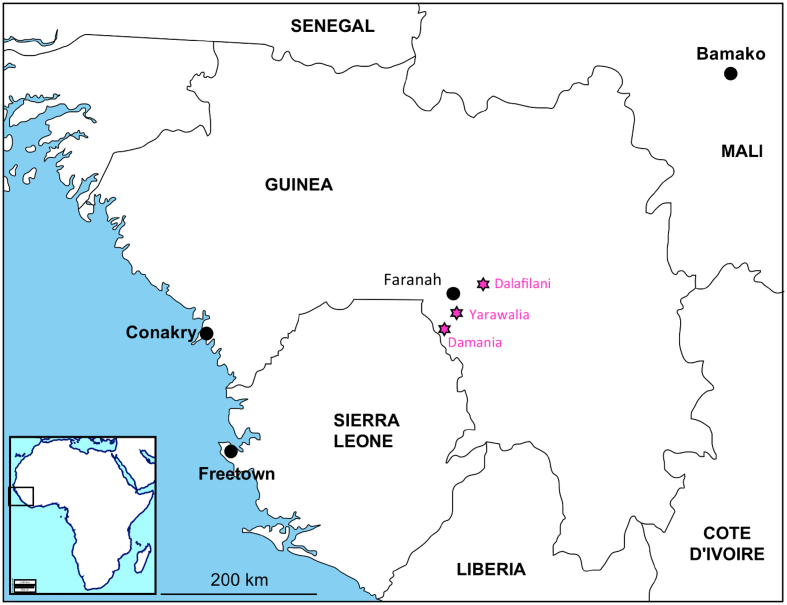
This study was conducted in the endemic region of Faranah (Guinea), where the LASV prevalence and seroprevalence in the rodent population were 5–10% and 20–40%, respectively. The occupancy of houses with rodents was ±60% at the beginning of the dry season (November) [6]. All participating house owners gave informed and written consent prior to sampling. The first 26–32 houses with droppings and a consenting owner along a transect were included. Sampling took place in 88 rooms, dispatched in three villages (32 in Yarawalia, 30 in Dalafilani, and 26 in Damania) (Fig. 1). Usually, the sampler took 2–3 droppings from each deposit. As such, a single sample contained feces from more than one rodent if possible. The feces samples were immediately stored in 1 ml DNA/RNA Shield (Zymo Research, California, USA) and placed in a dark, cold box for transportation to a − 20 °C freezer [13,14].
Fig. 1.
Map of Guinea showing the sampled villages in the vicinity of Faranah. Dalafilani (10.143158 N, 10.605512 W), Damania (9.806699 N, 10.863339 W), Yarawalia (9.954588 N, 10.732534 W). The maps of Africa and West Africa were downloaded from http://d-maps.com/carte.php?num_car=728&lang=fr and http://d-maps.com/carte.php?num_car=752&lang=fr, and then modified in using the software EazyDraw v 5.3.0 (http://eazydraw.com).
RNA was extracted from feces samples in pools of three using the QIAamp Viral RNA extraction kit (Qiagen, Hilden, Germany). The pooled extractions were then analyzed via quantitative real time RT-PCR (RT-qPCR) in a Rotorgene using the RealStar Lassa Virus RT-PCR Kit 2.0 (altona Diagnostics, Hamburg, Germany). Pools detected to be LASV-positive were then split, extracted and re-analyzed. Positive feces samples were subsequently tested by conventional RT-PCR targeted on glycoprotein (GP) using the primers LVS 36+ 5´-ACC GGG GAT CCT AGG CAT TT-3′ and OWS 1000–5´-AGCATGTCACAGAAYTCYTCATCATG-3′. The PCR products were sequenced using Sanger technology.
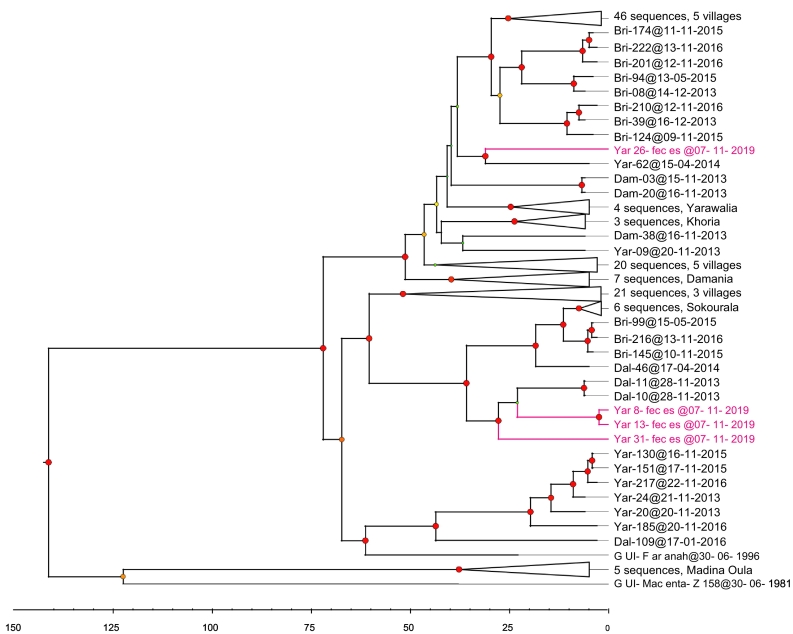
Sequences were then analyzed for their phylogenetic origin. The nucleotide sequences of partial GPC were aligned with others from the Faranah area in using MacVector, version 16.0.10. The analysis was inferred by using the Bayesian Markov Chain Monte Carlo (MCMC) method, implemented in BEAST software [15]. The parameters were set in BEAUTI as follows: the tip-date at the day level, the substitution model as GTR + gamma, the codon partition with positions 1, 2, 3, the clock model as strict, and the coalescent tree with a constant size population. The chain length was 50 million, with echo states and log parameters every 50,000 steps. The xml files issued from BEAUTI were run in BEAST and checked in TRACER. The consensus tree was obtained in Tree Annotator, and then visualized through FigTree (BEAST packages, https://beast.community/programs).
3. Results and discussion
This study detected LASV in ten feces samples (Table 1). Four sequences of the glycoprotein 1 kb were identified with subsequent phylogenetic analyses suggesting clustering to previously identified Yarawalia and Dalafilani strains (Fig. 2). The sequences belong to lineage IV, which comprises all isolates of Guinea, Sierra Leone and Liberia [16,17]. Identification of unique sequences suggests that the four positive samples belonged to different rodents. Clustering of sequences between Yarawalia and Damania provides further evidence for frequent viral importation and circulation between villages [6,8].
Table 1.
Cycle threshold (Ct) values of the RT-qPCRs targeted on glycoprotein (GP) and polymerase genes, and results of the conventional RT-PCR targeted on the GP 1 kb.
| Sample ID | Ct (GP) | GP 1 kb | Ct (polymerase) |
|---|---|---|---|
| Positive control | 32.85 | – | 32.59 |
| Yar 4 | 25.43 | NEG | 28.34 |
| Yar 8 | 28.91 | POS (MW776596) | 26.45 |
| Yar 10 | 25.70 | NEG | 28.56 |
| Yar 11 | 36.06 | NEG | 37.79 |
| Yar 13 | 22.93 | POS (MW776597) | 24.80 |
| Yar 16 | 24.86 | NEG | 28.77 |
| Yar 26 | 21.45 | POS (MW776598) | 23.29 |
| Yar 28 | 28.66 | NEG | 30.93 |
| Yar 31 | 25.10 | POS (MW776599) | 25.25 |
| Dam 13 | 25.31 | NEG | 30.78 |
The GP 1 kb RT-PCR is less sensitive than the RT-qPCR, explaining lower positive samples. Only the lowest Ct values (high viral load) obtained for the polymerase test gave signals in the conventional RT-PCR, and provided subsequent sequencing. Accession numbers are given between parentheses.
Fig. 2.
Time-calibrated phylogeny of the Lassa virus strains, gathering 144 sequences belonging to lineages IV described in Guinea. The tree shows the partial glycoprotein precursor (888 nt). Posterior probabilities are coded as follows: 0.7, green dots; 0.80 to <0.85, purple-blue dots; > 0.97, red dots. Scale axis represents the time in years. The sequences are deposited in GenBank under the accession numbers MW776596-MW776599 (see Table 1). Detailed information about the sequence names is available in the supplementary table. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Compared to standard trapping methods for rodent sampling (e.g. necropsies, capture-recapture), feces sampling is simpler, less time-consuming, and safer as it removes risks associated with animal contact. Furthermore, using DNA/RNA shield as buffer solution ensures the safe handling of samples as the product inactivates and preserves RNA at room temperature. The ease of this sampling method creates the possibility to make broad surveys by sampling an entire village in less than one day.
One village had predominate detection of LASV, with nine of the positive samples coming from Yarawalia (out of 32 samples, 28.1% LASV-prevalence), only one coming from Damania (out of 30 samples, 3.3% LASV-prevalence), and none from Dalafilani (out of 26 samples, 0% LASV-prevalence) (Table 1). This unequal distribution does not match the known LASV prevalence of >20% in the three villages. Furthermore, Dalafilani had no positive samples, but trappings in the same month during a previous year (2013) found a 26.7% LASV-prevalence (8/39) in rodents in Dalafilani. Trappings from the same study also found higher prevalence in Damania during the same month: 20.0% (10/50 in 2013), 10.7% (3/28 in 2015), and 8.9% (4/45 in 2016). Conversely, trappings out of Yarawalia had lower prevalence: 18.2% (8/44 in 2013) and 12.0% (3/25 in 2016). However, spatial clustering of LASV positive M. natalensis is known to occur and it might be that we picked-up such a cluster in Yarawalia [6]. The Mariën et al. 2020 study had more success in capturing positive rodents because their study had a doubled sample size compared to this one. Furthermore, feces found and sampled in Yarawalia appeared fresh and moist, whereas droppings in the other two villages appeared old and dry. This difference could have affected the detection of LASV as older feces likely had longer exposure to high temperatures inside houses leading to viral decay [18,19].
The detection of LASV-positive feces further suggests that humans cohabitating with M. natalensis are at risk of exposure to LASV, not only while the rodent is physically in the communal space but also after the rodent leaves via exposure to feces. In these villages, feces are found everywhere in the houses: on the floor, in the bed, in bowls, uncovered water and food. It is common for women to remove feces from the rice with their fingertips during cooking, an intimate contact potentially representing a risk for LASV exposure. Safe removal of rodent feces should therefore be encouraged to reduce LASV-exposure.
4. Limitations
A primary limitation of the study methodology was its small sample size, which is potentially why there was a wide variance in detected LASV positive feces between villages. A second limitation was the variation in freshness of feces, which might have impacted the detection of the viral RNA. Viral RNA is likely to have degraded in older feces and thus less likely to be picked-up by PCR. A last limitation of this study was that PCR analysis could only show LASV RNA presence within a certain period. Detecting antibodies from previous infection was not possible, nor could infectiousness be determined in cell culture as the DNA/RNA shield buffer solution inactivates all viral activity.
5. Recommendations
To conduct a broad investigation on the presence of the Lassa virus in a territory, we believe that feces sampling is a fast and cost-efficient method. While it is clear that rodent trapping and dissecting is a more sensitive approach, feces sampling is a compelling alternative for research groups that do not have the capacity or the knowledge for this expensive and laborious fieldwork. This sampling approach could be especially useful in epidemiological and anthropological studies because researchers can gather information from the villagers during safer environmental sampling. According to our pilot study, we recommend increasing the sample size to ensure that feces from clusters of LASV-infected rodents are sampled and not missed by chance. Furthermore, we recommend that clustering be explored by mapping out the coordinates of all houses within a sampled village. Working with participants to ensure that rodent feces are cleaned from dwellings the day before sampling would substantially improve the sampling method by ensuring that feces are fresh. Additionally, we recommend cultivation of LASV positive samples to explore infectiousness and exposure risks further. Implementing this simple method on a large scale would extend the possibilities of investigating rodent-borne diseases in general.
Ethics
Approval to conduct the study was granted by the National Ethics Committee of Guinea under the permit 129/CNERS/16. Informed, written consent was obtained from each dwelling owner prior to sampling.
Declaration of interest
The authors of this article have no conflicts of interest with the contents of this manuscript.
Funding
This work was supported by the German Research Foundation (DFG, ref. FI1781/2-1). Joachim Marien is currently a research assistant of Research Foundation Flanders (FWO).
Acknowledgments
This study would not have been possible without the contribution of many gracious individuals. We want to acknowledge Dr. Almudena Mari-Saez for sharing her invaluable knowledge and experience with Guinean Lassa Fever studies; Dr. N’Faly Magassouba for facilitating the screening of the Lassa virus in his laboratory in Conakry; Pimrapat Gebert for her statistical advice; the Guinean field team who assisted with sample collection logistics; and all study participants who graciously offered their valuable time and trust.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.onehlt.2021.100317.
Contributor Information
Rebekah Wood, Email: rebekah.r.wood@gmail.com, woodr@rki.de.
Elisabeth Fichet-Calvet, Email: fichet-calvet@bnitm.de.
Appendix A. Supplementary data
List of the 144 LASV sequences from rodents and humans used in the analysis.
References
- 1.McCormick J., Fisher-Hoch S. Arenaviruses I. Springer; 2002. Lassa fever; pp. 75–109. [Google Scholar]
- 2.Fischer W.A., II, Wohl D.A. Moving Lassa fever research and care into the 21st century. J. Infect. Dis. 2017;215(12):1779–1781. doi: 10.1093/infdis/jix206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Magassouba N.F., et al. A sporadic and lethal Lassa fever case in Forest Guinea, 2019. Viruses. 2020;12(10):1062. doi: 10.3390/v12101062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basinski A.J., et al. Bridging the gap: using reservoir ecology and human serosurveys to estimate Lassa virus spillover in West Africa. PLoS Comput. Biol. 2021;17(3) doi: 10.1371/journal.pcbi.1008811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bausch D.G., et al. Lassa fever in Guinea: I. Epidemiology of human disease and clinical observations. Vector Borne Zoonotic Dis. 2001;1(4):269–281. doi: 10.1089/15303660160025903. [DOI] [PubMed] [Google Scholar]
- 6.Mariën J., et al. Households as hotspots of Lassa fever? Assessing the spatial distribution of Lassa virus-infected rodents in rural villages of Guinea. Emerg. Microb. Infect. 2020;9(1):1055–1064. doi: 10.1080/22221751.2020.1766381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Walker D., et al. Comparative pathology of Lassa virus infection in monkeys, guinea-pigs, and Mastomys natalensis. Bull. World Health Organ. 1975;52(4–6):523. [PMC free article] [PubMed] [Google Scholar]
- 8.Fichet-Calvet E., et al. Spatial and temporal evolution of Lassa virus in the natural host population in upper Guinea. Sci. Rep. 2016;6(1):1–6. doi: 10.1038/srep21977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berto A., et al. Detection of potentially novel paramyxovirus and coronavirus viral RNA in bats and rats in the Mekong Delta region of southern Viet Nam. Zoonoses Public Health. 2018;65(1):30–42. doi: 10.1111/zph.12362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Compton S.R., Riley L.K. Detection of infectious agents in laboratory rodents: traditional and molecular techniques. Comp. Med. 2001;51(2):113–119. [PubMed] [Google Scholar]
- 11.Borremans B., et al. Shedding dynamics of Morogoro virus, an African arenavirus closely related to Lassa virus, in its natural reservoir host Mastomys natalensis. Sci. Rep. 2015;5:10445. doi: 10.1038/srep10445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sagripanti J.-L., Rom A.M., Holland L.E. Persistence in darkness of virulent alphaviruses, Ebola virus, and Lassa virus deposited on solid surfaces. Arch. Virol. 2010;155(12):2035–2039. doi: 10.1007/s00705-010-0791-0. [DOI] [PubMed] [Google Scholar]
- 13.Tan S.K., et al. Stability of Zika virus in urine: specimen processing considerations and implications for the detection of RNA targets in urine. J. Virol. Methods. 2017;248:66–70. doi: 10.1016/j.jviromet.2017.04.018. [DOI] [PubMed] [Google Scholar]
- 14.Camacho-Sanchez M., et al. Preservation of RNA and DNA from mammal samples under field conditions. Mol. Ecol. Resour. 2013;13(4):663–673. doi: 10.1111/1755-0998.12108. [DOI] [PubMed] [Google Scholar]
- 15.Drummond A.J., et al. Bayesian phylogenetics with BEAUti and the BEAST 1.7. Mol. Biol. Evol. 2012;29(8):1969–1973. doi: 10.1093/molbev/mss075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li Y., Tian H. Adaptive genetic diversification of Lassa virus associated with the epidemic split of north-central Nigerian and non-Nigerian lineages. Virology. 2020;545:10–15. doi: 10.1016/j.virol.2020.03.002. [DOI] [PubMed] [Google Scholar]
- 17.Wiley M.R., et al. Lassa virus circulating in Liberia: a retrospective genomic characterisation. Lancet Infect. Dis. 2019;19(12):1371–1378. doi: 10.1016/S1473-3099(19)30486-4. [DOI] [PubMed] [Google Scholar]
- 18.Walker A.T., et al. Effect of time at temperature on wild poliovirus titers in stool specimens. Virology. 2015;482:28–31. doi: 10.1016/j.virol.2015.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ahmed W., et al. Comparative decay of culturable faecal indicator bacteria, microbial source tracking marker genes, and enteric pathogens in laboratory microcosms that mimic a sub-tropical environment. Sci. Total Environ. 2021;751:141475. doi: 10.1016/j.scitotenv.2020.141475. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
List of the 144 LASV sequences from rodents and humans used in the analysis.