Abstract
This study aimed to evaluate the sleep-related problems and predictors of probable clinical insomnia among college students during the COVID-19 remission period in China. 146,102 college students from 22 colleges/universities in Guangdong province participated in this study from 1th to 15th June, 2020. Self-administered questionnaires were used to assess demographic characteristics. Sleep-related problems, depression and anxiety symptoms were measured by Youth Self-Rating Insomnia Scale, Patient Health Questionnaire-9 and Generalized Anxiety Disorder Scale-7, respectively. The prevalence of difficulty in initiating sleep, difficulty in maintaining sleep, early morning awakening, sleep insufficiency, unrefreshing sleep and daytime functioning impairment were 7.2%, 3.4%, 3.5%, 9.6%, 14.6%, and 7.6%, respectively. 16.9% students had varying degrees of insomnia and 6.3% were considered as displaying probable clinical insomnia. Moreover, being urban residents, having a history of physical or mental illness, and probable clinical depression or anxiety were significant risk factors of probable clinical insomnia, while college senior degree and 7-8 hours’ sleep duration per day was the protective factor for probable clinical insomnia. Unrefreshing sleep was the most prominent sleep problem among college students during COVID-19 remission in China. Good sleep hygiene practices are strongly suggested to develop in the time of prolonged home isolation.
Keywords: Sleep-related problems, COVID-19, Predictors, College students
1. Introduction
The coronavirus disease 2019 (COVID-19) outbreak in late December during 2019, have exerted adverse effects on individuals such as fear, anger and insomnia (Kang et al., 2020). Due to the characteristics of human-to-human transmission and potentially fatality of COVID-19 (Rothe et al., 2020), many countries, including China, have taken confinement measures to limit the spread of the coronavirus, such as contact restrictions, self-isolation, and closure of schools, and colleges/universities (Bedford et al., 2020). College students, as a group, have potentially experienced a greater psychological impact from the pandemic (Wang et al., 2020), which could be attributed to the increased concerns on academic performance and decreased social interactions (Son et al., 2020).
Social distancing was necessary to control the spread of the pandemic, however, it also negatively affected the sleep quality (Lewis, 2020; Son et al., 2020) and sleep behaviors in students (Wright et al., 2020). Recent studies revealed high prevalence of sleep problems in college students (13.5-25.7%) during the COVID-19 pandemic (Ge et al., 2020; Wang et al., 2020; Zhou et al., 2020). Studies have shown that demographic factors, such as gender, age, residence, and the perceptions of the COVID-19 (Li et al., 2020; Lin et al., 2020) and psychological factors, including emotional disturbance could compromise sleep quality (Zhou et al., 2020). Furthermore, because of the fundamental role sleep plays in emotion regulation, sleep disturbance can have direct consequences upon next day emotional functioning (Altena et al., 2020). Therefore, monitoring the sleep problems of college students, providing tailored and timely sleep interventions to college students during the COVID-19 are necessary.
Starting from the beginning of May, there has been very low newly confirmed cases per day in China, with a clear downward trend nationwide, the situation is gradually normalized and brought under control. Thus, a small proportion of college students are permitted to return to school (The State Council Information Office of the People's Republic of China, 2020). Some social restrictions were still in place, for example, social gatherings were limited to 10 people, people were required to wear masks, maintain a safe social distance and register to travel in public places. Evidence suggests that individuals who have experienced public health emergencies still suffering from different levels of psychological problems even after the situation enhances (Cheng et al., 2004; Fan et al., 2015). However, few studies have considered sleep-related problems among college students during the remission period of the COVID-19.
Therefore, we conducted this study to evaluate the sleep-related problems in college students, and potential risk and protective factors related to clinical insomnia during the remission period in China from June 1st to June 15th 2020. Having a more comprehensive understanding of sleep-related problems among college students during the remission period is of great importance to provide practitioners with suggestion when all students return to schools.
2. Methods
2.1. Participants
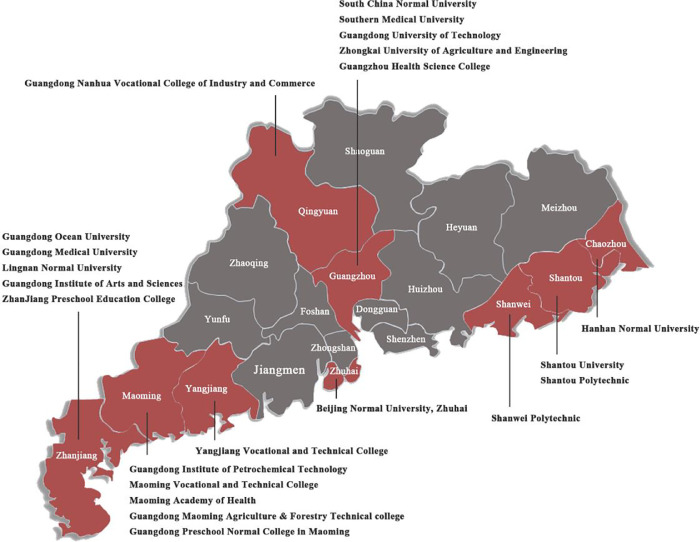
Based on the geographical distribution of the Guangdong Province and types of colleges and universities, we selected 22 colleges and universities in the province by convenient sampling for this survey. Geographical distribution of participating colleges and universities was shown in Fig. 4. The data of this cross-sectional study was collected online from June 1 to 15, 2020. 166,052 students finished the questionnaires via the online platform which our team designed specifically for this COVID-19 project. Finally, about 88% of them (n = 146,102) provided valid data and were included in the current analysis.
Fig. 4.
Geographical distribution of participating colleges and universities.
The study was approved by the Ethics Committees of South China Normal University (Ethics_No._SCNU-PSY-2020-01-001). Participants were informed that their responses were confidential when we transferred the invitation letter to them. Meanwhile, all participants provided informed consent and they could withdraw freely from the study at any time during data collection.
2.2. Procedures
Online questionnaire was adopted in this survey. We use the information website we built and the official WeChat account to push the questionnaire to target universities, the questionnaire was distributed to college students through the psychological counseling center of each university. All students were required to provide their anonymized student number, which was assigned based on their registration status at school, to complete the test. Prior to completing the survey, participants should submit an online informed consent. To ensure the quality of the data, strict quality control was carried out. Exclusion criteria included: completion time <5min, missing information >25%, and inconsistent survey contents.
2.3. Measures
2.3.1. Demographics
Demographic information included gender (male, female), age, grade (freshman, sophomore, junior, senior, postgraduate), residence location (rural, urban), number of siblings in the family (1, ≥2), history of physical illness (with or without a history of physical illness), history of mental illness (with or without a history of mental illness), the severity of COVID-19 in their areas (severe, moderate, mild), and whether to return to school (yes, no).
2.3.2. Sleep-related problems
The Youth Self‑Rating Insomnia Scale (YSIS) was used to measure students’ sleep-related problems in the past two weeks (Liu et al., 2019). The symptoms assessed include: difficulty in initiating sleep (DIS), difficulty in maintaining sleep (DMS), early morning awakening (EMA), sleep insufficiency, unrefreshing sleep, daytime functioning impairment, poor sleep quality, and sleep dissatisfaction. Sleep quality is rated from 1 (Very good) to 5 (Very poor) and sleep satisfaction is rated from 1 (Very satisfied) to 5 (Very unsatisfied). The remaining 6 items are rated from 1 = Never, 2 = < 1 time/week, 3 = 1–2 times/week, 4 = 3–5 times/ week, to 5 = 6–7 times/week. Example items are “During the past two weeks, how often would you say you feel unrested and unrestored upon waking?”. If this item was rated as response 4 (3-5 times/week) or above, the participants were classified as having difficulties in initiating sleep (Chen et al., 2020; Liu et al., 2017). The summing score of the 8 items indicates the severity of insomnia during the past two weeks, ranging from 8 to 40. The cutoffs for insomnia severity were: normal (<22), mild insomnia (22-25), moderate insomnia (26-29), and severe insomnia (≥30). In the current study, a cutoff score of 26 was used to identify whether a student had probable clinical insomnia or not (Liu et al., 2019). The Cronbach's α for YSIS was 0.90 in the current sample.
Besides, sleep quantity was asked using the additional question “During the past two weeks, how much time do you sleep every day?”, score of which range from 1 = <5 hours, 2 = 5-6 hours, 3 = 6-7 hours, 4 = 7-8 hours, to 5 = >8hours.
2.3.3. Depressive and anxiety symptoms
The Patient Heath Questionnaire (PHQ-9) (Kroenke et al., 2001) and Generalized Anxiety Disorder Scale (GAD-7) (Spitzer et al., 2006) were used to measure the severity of depressive and anxiety symptoms, respectively. The PHQ-9 consists of 9 items and the GAD-7 consists of 7 items, and both are rated on a 4-point Likert scale ranging from 0 (not at all) to 3 (nearly every day), with a higher score indicating more severe depressive or generalized anxiety symptoms. A total score of 7 indicates the probable clinical depression (Wang et al., 2014) and anxiety (Tong et al., 2016). In this study, Cronbach's α for PHQ-9 was 0.91 and 0.94 for GAD-7.
2.4. Statistical analyses
Analyses were conducted using SPSS Statistics version 23.0 (IBM Corp., released 2015). Descriptive analysis was applied to describe socio-demographic variables and sleep-related problems. Quantitative data were summarized with mean (M) and standard deviation (SD), while categorical data were represented as frequency (N) and percentage (%). Chi-square tests were used to compare differences between students with and without probable clinical insomnia. We conducted binary logistic regression to explore the predictors of probable clinical insomnia, with all variables significant in the Chi-square tests as covariates. The enter LR method was adopted. The strength of associations between variables and probable clinical insomnia were reflected by the odds ratio (OR) with a 95% confidence interval (CI). Due to the large sample size of this study, the threshold of statistical significance was set as p < 0.01.
3. Results
3.1. Description of the sample
A total of 146,102 college students were enrolled in analysis in our survey. The proportions of male and female were 37.9% and 62.1%, respectively. 9,518 (6.5%) college students have returned to school. Detailed sample demographic characteristics are shown in Table 1 .
Table 1.
Socio-demographic variables of this sample (N = 146,102).
| Variables | N | % |
| Gender | ||
| Female | 90,701 | 62.1 |
| Male | 55,401 | 37.9 |
| Age(years) | ||
| 16-18 | 8,163 | 5.6 |
| 19-21 | 93,713 | 64.1 |
| 22-24 | 39,012 | 26.7 |
| ≥25 | 5,214 | 3.6 |
| Grade | ||
| Freshman | 46,101 | 31.6 |
| Sophomore | 41,012 | 28.1 |
| Junior | 32,717 | 22.4 |
| Senior | 17,824 | 12.2 |
| Postgraduate | 8,448 | 5.8 |
| Residence location | ||
| Rural | 95,388 | 65.3 |
| Urban | 50,714 | 34.7 |
| No. of siblings in the family | ||
| 1 | 32,417 | 22.2 |
| ≥2 | 113,685 | 77.8 |
| History of physical illness | ||
| Yes | 476 | 0.3 |
| No | 145,626 | 99.7 |
| History of mental illness | ||
| Yes | 1,170 | 0.8 |
| No | 144,932 | 99.2 |
| The severity of the COVID-19 in your areaθ | ||
| Severe | 619 | 0.4 |
| Moderate | 133,031 | 91.1 |
| Mild | 12,452 | 8.5 |
| Whether to return to school | ||
| Yes | 9,518 | 6.5 |
| No | 136,584 | 93.5 |
Note: θThe severity of the COVID-19 in the area: Severe areas have more than 10,000 cumulative confirmed cases (e.g. Hubei province); moderate areas have 1,000 to 9,999 cumulative confirmed cases (e.g. Guangdong province), and the remaining provinces in China are mild areas with less than 1,000 cumulative confirmed cases (e.g. Sichuan province).
3.2. Sleep-related problems and sleep quantity among college students
Table 2 presented the rates of self-reported poor sleep quality, sleep dissatisfaction and weekly frequency of sleep-related problems. A total of 67.9% college students self-reported good/very good sleep quality, and a total of 65.1% college students were satisfied/very satisfied with their sleep.
Table 2.
The prevalence of sleep-related problems (N = 146,102).
| Items | Response (%) | ||||
| I1: poor sleep quality | Very good | Good | Fair | Poor | Very poor |
| 29.3 | 38.6 | 27.4 | 3.7 | 0.9 | |
| I2: sleep dissatisfaction | Very satisfied | Satisfied | Fair | Unsatisfied | Very unsatisfied |
| 25.2 | 39.9 | 26.8 | 6.8 | 1.3 | |
| Sleep related symptoms | Never | <1time/ week | 1-2 time/ week | 3-5 time/ week | 5-7 time/ week |
| I3: difficulty initiating sleep | 40.8 | 32.3 | 19.7 | 5.5 | 1.7 |
| I4: difficulty maintaining sleep | 57.8 | 26.6 | 12.2 | 2.7 | 0.7 |
| I5: early morning awakening | 63.5 | 22.5 | 10.4 | 2.7 | 0.8 |
| I6: sleep insufficiency | 42.7 | 27.1 | 20.7 | 7.1 | 2.5 |
| I7: unrefreshing sleep | 32.8 | 27.6 | 25.1 | 10.4 | 4.2 |
| I8: daytime functioning impairment | 48.0 | 26.4 | 18.0 | 5.8 | 1.8 |
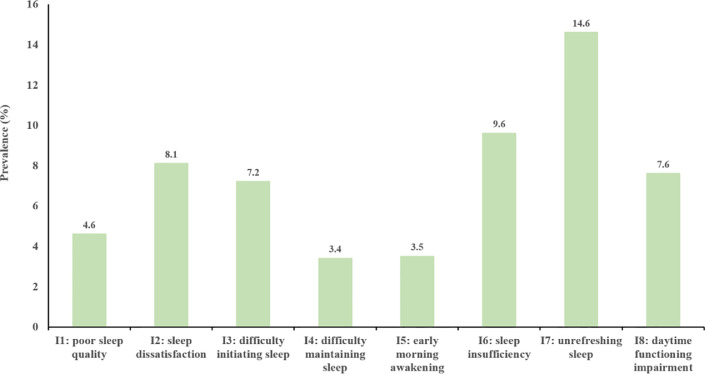
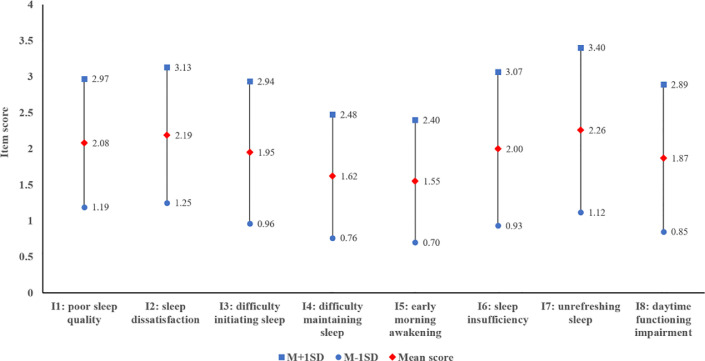
Fig. 1, Fig. 2 showed prevalence and mean scores of sleep-related problems in college students over the past two weeks respectively. The prevalence of DIS, DMS, EMA, sleep insufficiency, unrefreshing sleep and daytime functioning impairment were 7.2%, 3.4%, 3.5%, 9.6%, 14.6%, and 7.6%, respectively.
Fig. 1.
Prevalence of sleep-related problems in college students over the past two weeks.
Note: The prevalence (%) is obtained through response 4 and 5.
Fig. 2.
Scores of sleep-related problems in college students over the past two weeks.
Note: M: mean score; SD: standard deviation.
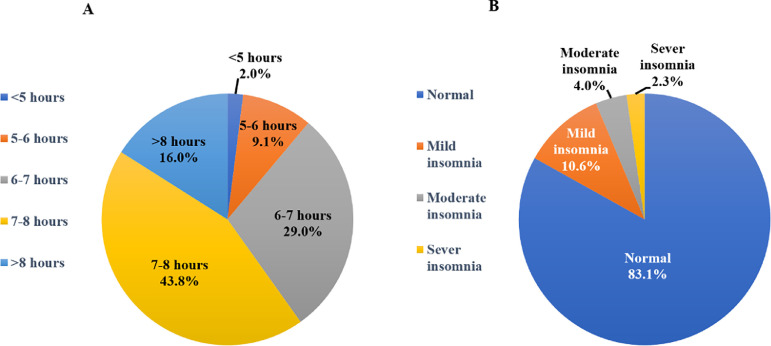
Fig. 3 presented sleep quantity and insomnia symptoms among college students over the past two weeks. 43.8% of college students reported sleeping periods of 7-8 hours per day. Sleeping for less than 5 hours every day was reported by 2% college students (Fig. 3A). 16.9% of students had various degrees of insomnia. Specifically, 4% of college students had moderate insomnia and 2.3% had severe insomnia (Fig. 3B), these two groups of college students were considered as experiencing probable clinical insomnia (n = 9,169).
Fig. 3.
Sleep quantity and insomnia symptoms in college students over the past two weeks.
Note: Fig. 3A shows the students’ sleep time every day; Fig. 3B shows the students’ prevalence of different severity of insomnia.
3.3. Comparison of sample characteristics
The comparisons between students with and without probable clinical insomnia across different factors were depicted in Table 3 . As shown, those in the probable clinical insomnia group were generally female (χ²=11.10, p<0.01), sophomore and junior students (χ²=148.46, p<0.001), urban residents (χ²=48.18, p<0.001), living in areas of moderate severity of the COVID-19 (χ²=11.14, p<0.01), and with less sleep quantity (χ²=5090.78, p<0.001). Higher proportion of having history of physical illness (χ²=66.65, p<0.001), history of mental illness (χ²=1136.76, p<0.001), depressive symptoms (χ²=11603.22, p<0.001) and anxiety symptoms (χ²=10794.12, p<0.001) was reported in probable clinical insomnia group.
Table 3.
Comparison of sample characteristics between no insomnia group and probable clinical insomnia group (N = 146,102).
| Variables | None N(%) |
Probable clinical insomnia* N(%) |
χ² | Cramer's V |
| Gender | 11.10⁎⁎ | 0.009 | ||
| Female | 84,859(93.6) | 5,842(6.4) | ||
| Male | 52,074(94.0) | 3,327(6.0) | ||
| Grade | 148.46⁎⁎⁎ | 0.032 | ||
| Freshman | 43,255(93.8) | 2,846(6.2) | ||
| Sophomore | 38,244(93.2) | 2,768(6.8) | ||
| Junior | 30,421(93.0) | 2,296(7.0) | ||
| Senior | 17,002(95.4) | 822(4.6) | ||
| Postgraduate | 8,011(94.8) | 437(5.2) | ||
| Residence location | 48.18⁎⁎⁎ | 0.018 | ||
| Rural | 47,225(93.1) | 3,489(6.9) | ||
| Unban | 89,708(94.0) | 5,680(6.0) | ||
| No. of siblings in the family | 0.854 | 0.002 | ||
| 1 | 30,347(93.6) | 2,070(6.4) | ||
| ≥2 | 106,586(93.8) | 7,099(6.2) | ||
| History of physical illness | 66.65⁎⁎⁎ | 0.021 | ||
| Yes | 403(84.7) | 73(15.3) | ||
| No | 136530(93.8) | 9096(6.2) | ||
| History of mental illness | 1136.76⁎⁎⁎ | 0.088 | ||
| Yes | 818(70.0) | 352(30.0) | ||
| No | 136,115(93.9) | 8,817(6.1) | ||
| The severity of the COVID-19 in your area | 11.14⁎⁎ | 0.009 | ||
| Severe | 590(95.3) | 29(4.7) | ||
| Moderate | 124,598(93.7) | 8,433(6.3) | ||
| Mild | 11,745(94.3) | 707(5.7) | ||
| Whether to return to school | 0.003 | 0.001 | ||
| Yes | 8,922(93.7) | 596(6.3) | ||
| No | 128,011(93.7) | 8,573(6.3) | ||
| Daily sleep quantity | 5090.78⁎⁎⁎ | 0.187 | ||
| <5h | 2386(81.5) | 543(18.5) | ||
| 5-6h | 10911(82.0) | 2389(18.0) | ||
| 6-7h | 39213(92.5) | 3169(7.5) | ||
| 7-8h | 61892(96.6) | 2150(3.4) | ||
| >8h | 22531(96.1) | 918(3.9) | ||
| Depressive symptoms | 11603.22⁎⁎⁎ | 0.282 | ||
| Yes | 44,006(84.5) | 8,049(15.5) | ||
| No | 92,927(98.8) | 1,120(1.2) | ||
| Anxiety symptoms | 10794.12⁎⁎⁎ | 0.272 | ||
| Yes | 23,953(80.7) | 5,739(19.3) | ||
| No | 112,980(97.1) | 3,430(2.9) |
Insomnia is defined as a YSIS score ≥26
p<0.01
p<0.001
3.4. Factors associated with probable clinical insomnia
The predictors of probable clinical insomnia were shown in Table 4 . The results showed that being female [AOR = 1.08, 95% CI = 1.03-1.13], living in urban [AOR = 1.14, 95% CI = 1.09-1.20], having a history of physical illness [AOR = 1.59, 95% CI = 1.19-2.13], a history of mental illness [AOR = 3.53, 95% CI = 3.04-4.09], or suffering depressive [AOR = 8.41, 95% CI = 7.82-9.04] and anxiety symptoms [AOR = 2.14, 95% CI = 2.03-2.25] were all potential risk factors for developing probable clinical insomnia. College senior degree [AOR = 0.78, 95% CI = 0.72-0.85] and 7-8 hours’ sleep duration per day [AOR = 0.78, 95% CI = 0.72-0.85] served as a protective factor for probable clinical insomnia. Nevertheless, the severity of the COVID-19 in living area was not found to significantly predict probable clinical insomnia.
Table 4.
The predictors of clinical insomnia in the logistic regression (N = 146,102).
| Variables | OR (95%CI) | AOR (95%CI) |
| Gender | ||
| Male | 1 | 1 |
| Female | 1.08⁎⁎ (1.03,1.13) | 1.08⁎⁎ (1.03,1.13) |
| Grade | ||
| Freshman | 1 | 1 |
| Sophomore | 1.10⁎⁎ (1.04,1.14) | 1.05 (0.99,1.11) |
| Junior | 1.15⁎⁎⁎ (1.08,1.21) | 1.02 (0.96,1.09) |
| Senior | 0.74⁎⁎⁎ (0.68,0.80) | 0.79⁎⁎⁎ (0.72,0.86) |
| Postgraduate | 0.83⁎⁎⁎ (0.75,0.92) | 0.93 (0.83,1.04) |
| Residence location | ||
| Rural | 1 | 1 |
| Urban | 1.17⁎⁎⁎ (1.12,1.22) | 1.14⁎⁎⁎ (1.09,1.20) |
| History of physical illness | ||
| No | 1 | 1 |
| Yes | 2.72⁎⁎⁎ (2.12,3.49) | 1.59⁎⁎ (1.19,2.13) |
| History of mental illness | ||
| No | 1 | 1 |
| Yes | 6.64⁎⁎⁎ (5.85,7.54) | 3.53⁎⁎⁎ (3.04,4.09) |
| The severity of the COVID-19 in your area# | ||
| Severe | 1 | 1 |
| Moderate Mild |
1.38 (0.95,2.00) | 1.24 (0.83,1.86) |
| 1.23 (0.84,1.79) | 1.09 (0.72,1.63) | |
| Daily sleep quantity | ||
| >8h | 1 | 1 |
| 7-8h | 0.85⁎⁎⁎ (0.79,0.92) | 0.78⁎⁎⁎ (0.72,0.85) |
| 6-7h | 1.98⁎⁎⁎ (1.84,2.14) | 1.39⁎⁎⁎ (1.28,1.50) |
| 5-6h | 5.37⁎⁎⁎ (4.96,5.82) | 2.70⁎⁎⁎ (2.48,2.93) |
| <5h | 5.59⁎⁎⁎ (4.98,6.26) | 4.80⁎⁎⁎ (4.22,5.45) |
| Depressive symptoms | ||
| No | 1 | 1 |
| Yes | 15.18⁎⁎⁎ (14.24,16.17) | 8.41⁎⁎⁎ (7.82,9.04) |
| Anxiety symptoms | ||
| No | 1 | 1 |
| Yes | 7.89⁎⁎⁎ (7.55,8.25) | 2.14⁎⁎⁎ (2.03,2.25) |
Note: 95% CI, 95% confidence interval. OR, odds ratio; each independent variable was analyzed one by one; AOR, adjusted odds ratio; all independent variables were simultaneously entered into a logistic regression model.
Severe as the reference
p<0.01
p<0.001
4. Discussion
The present study is the first large-scale cross-sectional study to investigate sleep-related problems among college students during the remission stage of the COVID-19 in China. Our main findings revealed that most students had enough hours of sleep, and the prevalence of insomnia did not get higher after the lifting of quarantine in China (Zhou et al., 2020). The sleep-related problems found with highest prevalence was unrefreshing sleep (14.6%), followed by sleep insufficiency (9.6%), daytime functioning impairment (7.6%), DIS (7.2%), EMA (3.5%), and DMS (3.4%). Moreover, being urban residents, having a history of physical or mental illness, and probable clinical depression or anxiety were significant risk factors of probable clinical insomnia, while college senior degree was the protective factor for probable clinical insomnia.
43.8% college students slept for 7-8 hours per day. As for insomnia, 16.9% of students reported mild or more severe insomnia symptoms and 6.3% college students were probably experiencing clinical insomnia. Although insomnia prevalence rates among college students increased significantly during the COVID-19 outbreak in China (Wang et al., 2020; Zhou et al., 2020), our research did not find a significant higher prevalence rate of insomnia during the COVID-19 remission period compared with the outbreak period. The gradually relieving social distancing and returning back to school life might contribute to this result. Those are tentative explanations, thus, this finding should be explained with cautions.
It was worth noting that unrefreshing sleep was the most prominent sleep problem during COVID-19 remission in China. Unrefreshing sleep is characterized by waking up with tired feelings in the morning (Ohayon and Roth, 2001). It is suggested that individuals who obtained enough sleep but still suffered unrefreshing sleep complaints could be considered as having nonrestorative sleep (NRS) (Wilkinson and Shapiro, 2012). This result echoes with previous studies showing that college students sleep more and wake up later during the periods of quarantine, however, their sleep quality decreased (Benham, 2020; Li et al., 2020; Wright et al., 2020). COVID-19 has restricted students' social activities, leaving them with more spare time, which has worsened the sleep hygiene habits, such as the inconsistent sleep-wake schedules and more possibilities to use electronic products before sleep (Cellini et al., 2020). The situation that self-isolation deteriorates sleep hygiene has been found in other studies (Bahkir & Grandee, 2020; Lin et al., 2020), it may result in prolonged sleep latency and decreased sleep quality (Salehinejad et al., 2020). Furthermore, worries about academic performance and lacking of physical activities were also associated with unrefreshing sleep (Cvejic et al., 2018; Zhang et al., 2020). COVID-19 limited ones’ physical activities and disrupted regular academic arrangements of some college students. As a result, these people tended to report fatigue in the morning, which led to greater unsatisfaction with sleep quality and quantity, ultimately affecting their mood and impairing daytime functioning the next day. However, we have to also consider the possibility that sleep quality would also be improved during lockdown. A Study in Finland found that almost a third of people reported better sleep quality during the lockdown than before (Pesonen et al., 2020). It suggests that there are also some protective factors for sleep during lockdown, such as alleviated pressure in scheduling and better sleep environment.
Our findings showed that DIS, DMS, and EMA were not the major sleep problems among college students during the COVID-19 remission period in China. The results were comparable to that before the pandemic (Liu et al., 2017). However, a study from Italy showed that the percentages of DIS, DMS and EMA in college students were much higher than the incidence reported in the absence of pandemic (DIS, 55.4% vs 38.9%; EMA, 30% vs 21.4%; DMS, 33.7% vs 19.5%) (Marelli et al., 2021). These results could be explained that people's panic about the pandemic gradually subsided as the pandemic eased, and their sleep quality were improved with it.
In examining the risk and protective factors related to clinical insomnia, we found that being in senior grade was a protective factor to it. In addition to that, being female, urban residents, having a history of physical or mental illness, and probable clinical depression or anxiety were significantly associated with the risk of probable clinical insomnia. Previous study showed that senior students were the predominant sub-group of students with poor sleep quality (Xie et al., 2020), which contrasted to our finding. It is possible that senior students had high levels of concern about the negative impact of COVID-19 on their academic achievement and/or the employment prospect of this year in the early stage of the COVID-19. Gradually, the improving situation of the COVID-19 and associated employment supports from the government and universities might contribute to the decrease in insomnia. Female was found to have a higher risk of clinical insomnia, which is consistent with previous studies showing that among those suffering from insomnia, females predominated (de Zambotti et al., 2018; Zhou et al., 2020). Students who live in cities were also more likely to experience clinical insomnia. Previous studies have confirmed that city dwellers suffered more insomnia symptoms (Lahiri et al., 2020; Zhai et al., 2018), mainly because the pandemic originated from densely populated areas and urban population flows increased during the remission period. All of these might exacerbate urban residents’ concerns and uncertainty. In addition, shortened sleep duration lead to an increase in student insomnia symptoms, which also has an impact on daytime function (Chan et al., 2018).
We also found that people with a history of somatic diseases had a significantly increased risk of probable clinical insomnia, which is in line with the prior research (Liu et al., 2020). There are some tentative explanations. Firstly, people with a history of somatic diseases may worry more about infection, leading to more insomnia symptom Secondly, patients with physical illness often suffered comorbid insomnia symptoms, which is usually the result of multiple effects, including direct impairment of sleep-wake mechanisms, ache, medication hangover, or depression and anxiety in reaction to the illness (Sateia and Nowell, 2004).
Meanwhile, mental illnesses, especially depression and anxiety, are strong associated with clinical insomnia. Poor mental health status may be one reason for developing insomnia (Boehm et al., 2016; Morin et al., 2015; Taylor et al., 2003). Additionally, studies on natural disasters showed that that traumatic events may exacerbate anxiety and depression, and thus exacerbate insomnia (Liu et al., 2020). Quarantine measures against the COVID-19 have reportedly increased anxiety and depression among college students (Du et al., 2020; Li et al., 2021), which may be an important potential risk factor for subsequent insomnia. We suggest that it is necessary to pay attention to both emotional problems and sleep-related problems when providing intervention to students who exposed to the COVID-19. Furthermore, future studies with multiple follow-ups are highly suggested to explore whether insomnia symptoms are caused by anxiety, depression, and/or their comorbidity.
In addition to the factors included in this study, the COVID-19 pandemic related stressors could also affect sleep, for example, infection fears and inadequate supplies have been confirmed to be closely related to sleep (Brooks et al., 2020). Furthermore, high rates of sleep disturbances have also been found in people infected with COVID-19 (Taquet et al., 2021). The main mediators through which contracting COVID-19 affects sleep quality may be the fear for death, especially in the absence of a vaccine (Lin et al., 2020).
Insomnia symptoms, primarily due to environmental stress or psychological disorders, may be an acute or short-term cindition in the early period of the outbreak. In such cases, emphasizing sleep hygiene and using hypnotics when necessary are suggested (Sateia and Nowell, 2004). Nonetheless, individuals with persistent insomnia after the acute stress period might need to be considered for probable chronic insomnia. They were more likely to show more worries, anxiety or maladaptive sleep-regulating strategies (Roberts et al., 2008; Sidani et al., 2019). Excessive negative cognitions along with sleep insufficiency will enhance individual perception of the threat of insomnia, further exacerbating the insomnia (Harvey, 2002). Therefore, we suggest that colleges and universities should continue paying attention to students’ sleep problems after they fully return to school. Providing students with sleep intervention information and necessary psychotherapy services (e.g., cognitive-behavioral therapy (Hood et al., 2014)) to help improve their sleep quality and develop good sleep hygiene habits are necessary.
Although this study recruited a large sample to investigate in the sleep status of college students in the post-pandemic period, there are some limitations that need considering. First, due to the sudden nature of COVID-19 pandemic, we did not conduct surveys at the point in time prior to the outbreak, resulting in limited information on effects of COVID-19 to sleep quality. Second, participants evaluated their insomnia symptoms with the self-reported questionnaire, thus, strict clinical diagnoses are recommended for future studies to confirm our current findings. Third, we will continue to follow up and supplement the measurements of college students' sleep habits.
To sum up, unrefreshing sleep was the most prominent sleep problem among college students after the lifting of quarantine in China. We suggest to develop good sleep hygiene habits, as it may result in a potentially positive impact on sleep later in life. Furthermore, differences in different sub-groups of the population need to be taken into account to setting out targeted policies. These findings also indicated that the government and colleges should continue keeping a watchful eye on the sleep problems of college students, especially unrefreshing sleep, and providing them with necessary psychological services pandemic.
Acknowledgments
Acknowledgements
The authors want to express their sincere appreciation to all people who involved in the study and the partner schools.
Contributors
Yifan Zhang: Writing-Original draft preparation, Writing – review & editing
Dongfang Wang: Methodology, Formal analysis, Visualization, Writing – review
Jingbo Zhao: Resources, Investigation
Xiao-Yan CHEN: Writing – Reviewing
Huilin Chen: Writing – Reviewing
Zijuan Ma: Writing - Reviewing
Qian Yu: Investigation
Tong Wang: Investigation
Zihao Chen: Investigation
Jiaqi Jiang: Investigation
Zhiyi Zhu: Investigation
Shuiqing Huang: Investigation
Fang Fan: Supervision, Resources, Project administration, Funding acquisition,
Writing- Reviewing and Editing
Xianchen Liu: Supervision, Project administration, Writing- Reviewing
Role of the Founding Source
The current study was funded by National Natural Science Foundation of China (Grant No.31271096, 31900789, 31871129); Research on the Processes and Repair of Psychological Trauma in Youth, Project of Key Institute of Humanities and Social Sciences, MOE (Grant No.16JJD190001); Guangdong Province Universities and Colleges Pearl River Scholar Funded Scheme, (GDUPS 2016); Graduate Research and Innovation Project of School of Psychology, South China Normal University (PSY-SCNU202017), and Special Funds for the Cultivation of Guangdong College Students’ Scientific and Technological Innovation. (“Climbing Program” Special Funds: pdjh2021a0131).
References
- Altena E., Baglioni C., Espie C.A., Ellis J., Gavriloff D., Holzinger B., Schlarb A., Frase L., Jernelöv S., Riemann D. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: Practical recommendations from a task force of the European CBT-I Academy. J Sleep Res. 2020;29(4):e13052. doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]
- Bahkir F.A., Grandee S.S. Impact of the COVID-19 lockdown on digital device-related ocular health. Indian J Ophthalmol. 2020;68(11):2378–2383. doi: 10.4103/ijo.IJO_2306_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bedford J., Enria D., Giesecke J., Heymann D.L., Ihekweazu C., Kobinger G., Lane H.C., Memish Z., Oh M.D., Sall A.A., Schuchat A., Ungchusak K., Wieler L.H. COVID-19: towards controlling of a pandemic. Lancet. 2020;395(10229):1015–1018. doi: 10.1016/s0140-6736(20)30673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benham G. 2020. Stress and sleep in college students prior to and during the COVID-19 pandemic. Stress Health. [DOI] [PubMed] [Google Scholar]
- Boehm M.A., Lei Q.M., Lloyd R.M., Prichard J.R. Depression, anxiety, and tobacco use: Overlapping impediments to sleep in a national sample of college students. J Am Coll Health. 2016;64(7):565–574. doi: 10.1080/07448481.2016.1205073. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/s0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cellini N., Canale N., Mioni G., Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020;29(4):e13074. doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan C.S., Poon C.Y.S., Leung J.C.Y., Lau K.N.T., Lau E.Y.Y. Delayed school start time is associated with better sleep, daytime functioning, and life satisfaction in residential high-school students. J Adolesc. 2018;66:49–54. doi: 10.1016/j.adolescence.2018.05.002. [DOI] [PubMed] [Google Scholar]
- Chen D., Jiang M., Shi X., Geng F., Qi H., Zhang Y., Lai Y., Fan F. Predictors of the initiation of shift work disorder among Chinese intern nurses: a prospective study. Sleep Med. 2020;68:199–206. doi: 10.1016/j.sleep.2019.11.1263. [DOI] [PubMed] [Google Scholar]
- Cheng S.K., Wong C.W., Tsang J., Wong K.C. Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS) Psychol Med. 2004;34(7):1187–1195. doi: 10.1017/s0033291704002272. [DOI] [PubMed] [Google Scholar]
- Cvejic E., Huang S., Vollmer-Conna U. Exploring the complex relationship between sleep, autonomic activity, wellbeing and performance in medical students. Aust N Z J Psychiatry. 2018;52(1):39–46. doi: 10.1177/0004867417716543. [DOI] [PubMed] [Google Scholar]
- de Zambotti M., Goldstone A., Colrain I.M., Baker F.C. Insomnia disorder in adolescence: Diagnosis, impact, and treatment. Sleep Med Rev. 2018;39:12–24. doi: 10.1016/j.smrv.2017.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du J., Mayer G., Hummel S., Oetjen N., Gronewold N., Zafar A., Schultz J.H. Mental Health Burden in Different Professions During the Final Stage of the COVID-19 Lockdown in China: Cross-sectional Survey Study. J Med Internet Res. 2020;22(12):e24240. doi: 10.2196/24240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan F., Long K., Zhou Y., Zheng Y., Liu X. Longitudinal trajectories of post-traumatic stress disorder symptoms among adolescents after the Wenchuan earthquake in China. Psychol Med. 2015;45(13):2885–2896. doi: 10.1017/s0033291715000884. [DOI] [PubMed] [Google Scholar]
- Ge F., Zhang D., Wu L., Mu H. Predicting Psychological State Among Chinese Undergraduate Students in the COVID-19 Epidemic: A Longitudinal Study Using a Machine Learning. Neuropsychiatr Dis Treat. 2020;16:2111–2118. doi: 10.2147/ndt.S262004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey A.G. A cognitive model of insomnia. Behav Res Ther. 2002;40(8):869–893. doi: 10.1016/s0005-7967(01)00061-4. [DOI] [PubMed] [Google Scholar]
- Hood H.K., Rogojanski J., Moss T.G. Cognitive-behavioral therapy for chronic insomnia. Curr Treat Options Neurol. 2014;16(12):321. doi: 10.1007/s11940-014-0321-6. [DOI] [PubMed] [Google Scholar]
- Corp. IBM. Armonk; 2015. IBM SPSS Statistics for Windows. Version 23.0. IBM Corp. [Google Scholar]
- Kang L., Li Y., Hu S., Chen M., Yang C., Yang B.X., Wang Y., Hu J., Lai J., Ma X., Chen J., Guan L., Wang G., Ma H., Liu Z. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7(3):e14. doi: 10.1016/s2215-0366(20)30047-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahiri A., Jha S.S., Acharya R., Dey A., Chakraborty A. Correlates of insomnia among the adults during COVID19 pandemic: evidence from an online survey in India. Sleep Med. 2020;77:66–73. doi: 10.1016/j.sleep.2020.11.020. [DOI] [PubMed] [Google Scholar]
- Lewis K. COVID-19: Preliminary Data on the Impact of Social Distancing on Loneliness and Mental Health. J Psychiatr Pract. 2020;26(5):400–404. doi: 10.1097/pra.0000000000000488. [DOI] [PubMed] [Google Scholar]
- Li X., Lv S., Liu L., Chen R., Chen J., Liang S., Tang S., Zhao J. COVID-19 in Guangdong: Immediate Perceptions and Psychological Impact on 304,167 College Students. Front Psychol. 2020;11:2024. doi: 10.3389/fpsyg.2020.02024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Qin Q., Sun Q., Sanford L.D., Vgontzas A.N., Tang X. Insomnia and psychological reactions during the COVID-19 outbreak in China. J Clin Sleep Med. 2020;16(8):1417–1418. doi: 10.5664/jcsm.8524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Zhao J., Ma Z., McReynolds L.S., Lin D., Chen Z., Wang T., Wang D., Zhang Y., Zhang J., Fan F., Liu X. Mental Health Among College Students During the COVID-19 Pandemic in China: A 2-Wave Longitudinal Survey. J Affect Disord. 2021;281:597–604. doi: 10.1016/j.jad.2020.11.109. [DOI] [PubMed] [Google Scholar]
- Lin L.Y., Wang J., Ou-Yang X.Y., Miao Q., Chen R., Liang F.X., Zhang Y.P., Tang Q., Wang T. The immediate impact of the 2019 novel coronavirus (COVID-19) outbreak on subjective sleep status. Sleep Med. 2020 doi: 10.1016/j.sleep.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y.H., Chiang T.W., Lin Y.L. Increased Internet Searches for Insomnia as an Indicator of Global Mental Health During the COVID-19 Pandemic: Multinational Longitudinal Study. J Med Internet Res. 2020;22(9):e22181. doi: 10.2196/22181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, D., Liu, S., Zhu, L., Li, D., Huang, D., Deng, H., Guo, H., Huang, D., Liao, Y., Mao, Z., Miao, Q., Liu, W., Xiu, M., Zhang, X., (2020). Prevalence and Related Factors of Insomnia Among Chinese Medical Staff in the Middle and Late Stage of COVID-19. Front Psychiatry, 11, 602315. doi:10.3389/fpsyt.2020.602315. [DOI] [PMC free article] [PubMed]
- Liu X., Chen H., Liu Z.Z., Fan F., Jia C.X. Early Menarche and Menstrual Problems Are Associated with Sleep Disturbance in a Large Sample of Chinese Adolescent Girls. Sleep. 2017;(9):40. doi: 10.1093/sleep/zsx107. [DOI] [PubMed] [Google Scholar]
- Liu X.C., Yang Y.Y., Liu Z.Z., Luo Y.C., Fan F., Jia C.X. Psychometric properties of Youth Self-Rating Insomnia Scale (YSIS) in Chinese adolescents. Sleep and Biological Rhythms. 2019;17(3):339–348. doi: 10.1007/s41105-019-00222-3. [DOI] [Google Scholar]
- Marelli S., Castelnuovo A., Somma A., Castronovo V., Mombelli S., Bottoni D., Leitner C., Fossati A., Ferini-Strambi L. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J Neurol. 2021;268(1):8–15. doi: 10.1007/s00415-020-10056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin C.M., Drake C.L., Harvey A.G., Krystal A.D., Manber R., Riemann D., Spiegelhalder K. Insomnia disorder. Nat Rev Dis Primers. 2015;1:15026. doi: 10.1038/nrdp.2015.26. [DOI] [PubMed] [Google Scholar]
- Ohayon M.M., Roth T. What are the contributing factors for insomnia in the general population? J Psychosom Res. 2001;51(6):745–755. doi: 10.1016/s0022-3999(01)00285-9. [DOI] [PubMed] [Google Scholar]
- Pesonen A.K., Lipsanen J., Halonen R., Elovainio M., Sandman N., Mäkelä J.M., Antila M., Béchard D., Ollila H.M., Kuula L. Pandemic Dreams: Network Analysis of Dream Content During the COVID-19 Lockdown. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.573961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts R.E., Roberts C.R., Duong H.T. Chronic insomnia and its negative consequences for health and functioning of adolescents: a 12-month prospective study. J Adolesc Health. 2008;42(3):294–302. doi: 10.1016/j.jadohealth.2007.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothe C., Schunk M., Sothmann P., Bretzel G., Froeschl G., Wallrauch C., Zimmer T., Thiel V., Janke C., Guggemos W., Seilmaier M., Drosten C., Vollmar P., Zwirglmaier K., Zange S., Wölfel R., Hoelscher M. Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. N Engl J Med. 2020;382(10):970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salehinejad, M.A., Majidinezhad, M., Ghanavati, E., Kouestanian, S., Vicario, C.M., Nitsche, M.A., Nejati, V., (2020). Negative impact of COVID-19 pandemic on sleep quantitative parameters, quality, and circadian alignment: Implications for health and psychological well-being. Excli j, 19, 1297-1308. doi:10.17179/excli2020-2831. [DOI] [PMC free article] [PubMed]
- Sateia M.J., Nowell P.D. Insomnia. Lancet. 2004;364(9449):1959–1973. doi: 10.1016/s0140-6736(04)17480-1. [DOI] [PubMed] [Google Scholar]
- Sidani S., Guruge S., Fox M., Collins L. Gender Differences in Perpetuating Factors, Experience and Management of Chronic Insomnia. J Gend Stud. 2019;28(4):402–413. doi: 10.1080/09589236.2018.1491394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Son C., Hegde S., Smith A., Wang X., Sasangohar F. Effects of COVID-19 on College Students' Mental Health in the United States: Interview Survey Study. J Med Internet Res. 2020;22(9):e21279. doi: 10.2196/21279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Taquet M., Luciano S., Geddes J.R., Harrison P.J. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62,354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8(2):130–140. doi: 10.1016/s2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The State Council Information Office of the People's Republic of China. 2020 Fighting Covid-19: China in Action. [Google Scholar]
- Taylor D.J., Lichstein K.L., Durrence H.H. Insomnia as a Health Risk Factor. Behavioral Sleep Medicine. 2003;1(4):227–247. doi: 10.1207/S15402010BSM0104_5. [DOI] [PubMed] [Google Scholar]
- Tong X., An D., McGonigal A., Park S.P., Zhou D. Validation of the Generalized Anxiety Disorder-7 (GAD-7) among Chinese people with epilepsy. Epilepsy Res. 2016;120:31–36. doi: 10.1016/j.eplepsyres.2015.11.019. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health. 2020;(5):17. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W., Bian Q., Zhao Y., Li X., Wang W., Du J., Zhang G., Zhou Q., Zhao M. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. 2014;36(5):539–544. doi: 10.1016/j.genhosppsych.2014.05.021. [DOI] [PubMed] [Google Scholar]
- Wang, X., Chen, H., Liu, L., Liu, Y., Zhang, N., Sun, Z., Lou, Q., Ge, W., Hu, B., Li, M., (2020). Anxiety and Sleep Problems of College Students During the Outbreak of COVID-19. Front Psychiatry, 11, 588693. doi:10.3389/fpsyt.2020.588693. [DOI] [PMC free article] [PubMed]
- Wilkinson K., Shapiro C. Nonrestorative sleep: symptom or unique diagnostic entity? Sleep Med. 2012;13(6):561–569. doi: 10.1016/j.sleep.2012.02.002. [DOI] [PubMed] [Google Scholar]
- Wright K.P., Linton S.K., Withrow D., Casiraghi L., Lanza S.M., Iglesia H., Vetter C., Depner C.M. Sleep in university students prior to and during COVID-19 Stay-at-Home orders. Curr Biol. 2020;30(14):R797–r798. doi: 10.1016/j.cub.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Li X., Luo H., He L., Bai Y., Zheng F., Zhang L., Ma J., Niu Z., Qin Y., Wang L., Ma W., Yu H., Zhang R., Guo Y. Depressive Symptoms, Sleep Quality and Diet During the 2019 Novel Coronavirus Epidemic in China: A Survey of Medical Students. Front Public Health. 2020;8 doi: 10.3389/fpubh.2020.588578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai K., Gao X., Wang G. The Role of Sleep Quality in the Psychological Well-Being of Final Year UndergraduateStudents in China. Int J Environ Res Public Health. 2018;(12):15. doi: 10.3390/ijerph15122881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Zhang H., Ma X., Di Q. Mental Health Problems during the COVID-19 Pandemics and the Mitigation Effects of Exercise: A Longitudinal Study of College Students in China. Int J Environ Res Public Health. 2020;(10):17. doi: 10.3390/ijerph17103722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou S.J., Wang L.L., Yang R., Yang X.J., Zhang L.G., Guo Z.C., Chen J.C., Wang J.Q., Chen J.X. Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Med. 2020;74:39–47. doi: 10.1016/j.sleep.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]