Abstract
This series reports the safety and feasibility of MitraClip (Abbott Vascular) in 7 high surgical risk Indian patients with symptomatic mitral regurgitation (MR). The clip was deployed successfully in all patients, and more than one clip was required in 5. All had reduction in MR to ≤2+. Mean mitral valve gradient was 3.0 ± 0.8 mmHg. At 12 months follow up, all were alive, and the MR grade was 1+ in 6 patients and 2+ in one. Mean MV gradient was 3.4 ± 1.0 mmHg. The modified Kansas City Quality of life (KCQ) analysis revealed significant improvement in their quality of life (p < 0.0001).
Keywords: Edge-to-edge MV repair, MitraClip, Mitral regurgitation, High surgical risk
1. Introduction
Mitral regurgitation (MR) is the most common valvular heart disease among the adults aged more than 55 years.1 It results either from the abnormality of the valve apparatus (primary MR, P-MR) or from left ventricular (LV) dysfunction and alterations in LV geometry (secondary MR, S-MR).2 Severe MR causes progressive LV dilatation, dysfunction, heart failure and increased mortality.3 Surgical repair or replacement is the gold standard for treatment, however, it is not always feasible in a significant proportion of patients.4 Trans-catheter edge to edge repair with MitraClip system (Abbott Vascular, Menlo Park, California, US) is less invasive therapy that approximates the mitral leaflets and decreases MR similar to the surgical Alfieri stich.5 The present case series evaluated the feasibility and safety of percutaneous edge to edge repair with MitraClip in high surgical risk symptomatic Indian patients with significant MR.
2. Methods
The study comprised of 7 high surgical risk symptomatic patients with severe P or S-MR. The following echocardiographic criteria were used for patient selection: In P-MR, the eligibility criteria were flail gap <10 mm and width <15 mm and in S-MR, the coaptation depth of <10 mm and coaptation length of >2 mm.6The demographic, clinical, and echocardiographic data were captured retrospectively from the case records, while procedural and TEE data were collected prospectively. They were followed with echocardiography at 1 month, and 6 months. 12 month evaluation was done by their local physician due to travel restriction from lockdown from COVID-19 pandemic. However, their clinical status was assessed via phone conversation using modified Kansas City questionnaire (KCQ) on Quality of Live (QoL).7
3. Results
The mean age of the population was 76.7 ± 7.1 years and 4 were males. The mean EuroScore II and STS score predicted mortality were 7.4 ± 4.3 % and 7.2 ± 5.2 % respectively. The MR was P-MR in 5 and S-MR in 2 patients. Of the 5 patients with P-MR, the pathology involved P2 segment in 3, A2 in one and A3 in the other patient. The MR was grade 4+ in 6 and grade 3+ in 1 patient. The mean effective regurgitation orifice area and regurgitation volume were 0.5 ± 0.3 cm2 and 78.9 ± 56.0 ml respectively. The mean left ventricular end diastolic diameter (LVEDD), left ventricular end systolic diameter (LVESD), left ventricular end diastolic volume (LVEDV), left ventricular end systolic volume (LVESV), and left ventricular ejection fraction (LVEF) were 54.5 ± 5.1 mm, 33.3 ± 5.3 mm, 158 ± 45.6 ml, 73.3 ± 2 ml, and 53.9 ± 12.5% respectively. The mean right ventricular systolic pressure (RVSP) was 70.7 ± 23.2 mmHg (Supplementary table 1).The clip was deployed successfully in all patients and more than one clip was required in 5 patients (Supplementary figure 1 and 2). The mean left atrial pressure decreased from 27.7 ± 11.1 mmHg to 18.0 ± 6.5 mmHg and mean ‘V’ wave from 57.4 ± 23.5 mmHg to 24.5 ± 13.1 mmHg. The mean mitral valve gradient was 3.4 ± 1.0 mmHg. All had reduction in MR to ≤2+. The mean duration of the hospital stay was 4.0 ± 2.1 days. One patient had small pericardial effusion at the time of discharge which required pericardiocentesis after 3 weeks (Supplementary table 2).
The mean duration of follow up was 476 ± 122 days. All were in NYHA class I/II functional status. The QoL analysis performed using Radar plot test demonstrated significant improvement in QoL (p < 0.0001), in both individual and aggregate analyses (Supplementary figure 3).
On 6 months follow up echocardiography, MR grade was 1+ in 6 patients and 2+ in one. The mean MV gradient was 3.4 ± 1.0 mmHg. The mean LVEDD, LVESD, LVEDV, LVESV, LVEF and RVSP were 52.8 ± 3.6 mm, 34.3 ± 4.1 mm, 109.7 ± 28.4 ml, 52.8 ± 19.7 ml, and 53 ± 12.2% respectively (Supplementary table 3).
4. Discussion
Successful procedure with a reduction in the severity of MR to <2+, is an important determinant of post-procedure clinical improvement. Studies reported that persistent MR of >2+ severity as an independent predictor of heart failure re-hospitalization, all-cause mortality and worsening severity of MR following MitraClip therapy.8, 9, 10, 11 All patients in the current study had excellent reduction in MR severity and none had >2+ residual MR. MitraClip treatment results in decrease in MR severity leading to reduction in LA pressure (LAP) and V wave. Each 5 mmHg decrease in V wave was associated with a 49% improvement in 6 min walk test (MWT).12MitraClip reduces the effective mitral valve area and increases the trans-mitral gradients.13 All patients in this study attained good reduction in mean LAP and V wave post procedure and none had mean trans-valvular gradient > 4 mmHg. Although we did not get 6 MWT, the KCQ analysis demonstrated significant improvement in their QoL.7
Optimal MR reduction results in favorable LV remodeling, in the EVEREST II study, there was a significant reduction in the LVEDV, LVEDD, LVESV, and EF at 12 months follow up.6 All patients in the current study also demonstrated significant reduction in LVEDD, LVEDV, and LVESV at 6 month follow up and all were in NYHA class I/II during follow up. This demonstrates favorable translation of acute procedural outcomes and subsequent LV remodeling to good clinical outcomes. Furthermore, there was no mortality in this series till to date.
MitraClip percutaneous therapy to treat P-MR and S-MR was introduced in India very recently, and the experience is limited to a very small number of procedures thus far. This is the first series with short term and 12 months follow up data in India. Our results show that current MitraClip system can be safely used in Indian patients with smaller body surface area to treat symptomatic MR in whom surgical risk is prohibitive.
5. Conclusion
In selected symptomatic, high surgical risk Indian patients with significant MR, percutaneous edge-to-edge MV repair with MitraClip is feasible and safe. It is associated with improvement in functional status and favorable LV remodeling.
Financial disclosure
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ihj.2021.05.003.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
FigS1.
Primary mitral regurgitation (MR) from flail A3 segment. (A&B) Transesophageal echocardiography mid esophageal LV long axis (A) and commissural views (B) with color Doppler showing flail A3 segment and severe mitral regurgitation. (C) Fluoroscopy showing two clips in position. (D) Mid esophageal LV long axis view with color Doppler showing two small jets of MR after implantation of two clips. (E) 3D enface view of mitral valve showing flail A3 segment (arrow). (F) 3D en face view after deployment of 2 clips showing a large lateral orifice (star).
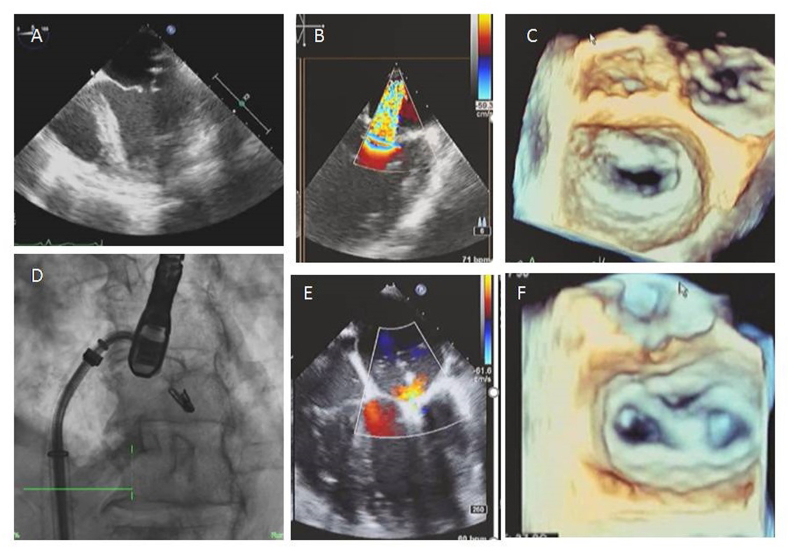
FigS2.
Secondary MR with posterior mitral leaflet (PML) restriction. (A) Transesophageal echocardiography mid esophageal 4 chamber view showing PML restriction. (B) Color Doppler imaging showing severe MR. (C) 3D enface view of mitral valve showing restricted PML and regurgitant orifice. (D) Fluoroscopy showing clip in position. (E) Mid esophageal 4 chamber view with color Doppler showing a small residual jet of MR after implantation of the clip. (F) 3D en- face view after deployment of Mitraclip showing double orifice.
FigS3.
Radar AxisPlot analysis of QoL Pre and post Mitral valve clipping. This figure demonstrates two concentric irregular polygons, the smaller polygon within the gray border (Pre QoL) and the larger polygon within the amber border (post QoL). The area in each polygon is the response to 21 of 25 QoL questinnaire. The response to each question is scored from -2 to 5. The larger the area the higher the score. Note that in each individual patient as well as the mean of the collective data, the area of the polygon bordered by amber colour is siignificantly larger than the area of the polygon bordered by gray, indicating significant improvement in the quality of life in each and every patient in the study after mitral valve clipping, p < 0.0001.
References
- 1.Nkomo V.T., Gardin J.M., Skelton T.N. Burden of valvular heart diseases: a population-based study. Lancet. 2006;368:1005–1011. doi: 10.1016/S0140-6736(06)69208-8. [DOI] [PubMed] [Google Scholar]
- 2.Bonow R.O., O'Gara P.T., Adams D.H. Focused update of the 2017 ACC expert consensus Decision pathway on the management of mitral regurgitation: a report of the American college of cardiology solution set oversight committee [published correction appears in J Am CollCardiol. 2020;75:3000] J Am Coll Cardiol. 2020;75:2236–2270. doi: 10.1016/j.jacc.2020.02.005. 2020. [DOI] [PubMed] [Google Scholar]
- 3.Trichon B.H., Felker G.M., Shaw L.K., Cabell C.H., O'Connor C.M. Relation of frequency and severity of mitral regurgitation to survival among patients with left ventricular systolic dysfunction and heart failure. Am J Cardiol. 2003;91:538–543. doi: 10.1016/s0002-9149(02)03301-5. [DOI] [PubMed] [Google Scholar]
- 4.Nishimura R.A., O'Gara P.T., Bavaria J.E. AATS/ACC/ASE/SCAI/STS expert consensus systems of care document: a proposal to optimize care for patients with valvular heart disease: a joint report of the American Association for Thoracic Surgery, American College of Cardiology, American Society of Echocardiography, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2019;73:2609–2635. doi: 10.1016/j.jacc.2018.10.007. 2019. [DOI] [PubMed] [Google Scholar]
- 5.Feldman T., Kar S., Rinaldi M. Percutaneous mitral repair with the MitraClip system: safety and midterm durability in the initial EVEREST (Endovascular Valve Edge-to-Edge REpair Study) cohort. J Am Coll Cardiol. 2009;54:686–694. doi: 10.1016/j.jacc.2009.03.077. [DOI] [PubMed] [Google Scholar]
- 6.Feldman T., Foster E., Glower D.D. Percutaneous repair or surgery for mitral regurgitation [published correction appears in N Engl J Med. 2011;365:189. Glower, Donald G [corrected to Glower, Donald D] N Engl J Med. 2011;364 1395-406. [Google Scholar]
- 7.Green C.P., Porter C.B., Bresnahan D.R., Spertus J.A. Development and evaluation of the Kansas city cardiomyopathy questionnaire: a New health status measure for heart failure. J Am Coll Cardiol. 2000;35:1245–1255. doi: 10.1016/s0735-1097(00)00531-3. [DOI] [PubMed] [Google Scholar]
- 8.Puls M., Tichelbacker T., Bleckmann A. Failure of acute procedural success predicts adverse outcome after percutaneous edge-to-edge mitral valve repair with MitraClip. EuroIntervention. 2014;9:1407–1417. doi: 10.4244/EIJV9I12A238. [DOI] [PubMed] [Google Scholar]
- 9.Suri R.M., Clavel M.-A., Schaff H.V. Effect of recurrent mitral regurgitation following degenerative mitral valve repair: long-term analysis of competing outcomes. J Am Coll Cardiol. 2016;67:488–498. doi: 10.1016/j.jacc.2015.10.098. [DOI] [PubMed] [Google Scholar]
- 10.Sakaguchi T., Kagiyama N., Toki M. Residual mitral regurgitation after repair for posterior leaflet prolapse—importance of preoperative anterior leaflet tethering. J Am Heart Assoc. 2018;7 doi: 10.1161/JAHA.117.008495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buzzatti N., De Bonis M., Denti P. What is a “good” result after transcatheter mitral repair? Impact of residual mitral regurgitation. J Thoracic CardiovasSurg. 2016;151:88–96. doi: 10.1016/j.jtcvs.2015.09.099. [DOI] [PubMed] [Google Scholar]
- 12.Maor E., Raphael C.E., Panaich S.S. Acute changes in left atrial pressure after MitraClip are associated with improvement in 6- minute walk distance. Circ Cardiovasc Interv. 2017;10 doi: 10.1161/CIRCINTERVENTIONS.116.004856. [DOI] [PubMed] [Google Scholar]
- 13.Itabashi Y., Utsunomiya H., Kubo S. Different indicators for postprocedural mitral stenosis caused by single- or multiple-clip implantation after percutaneous mitral valve repair. J Cardiol. 2018;71:336–345. doi: 10.1016/j.jjcc.2017.10.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.