Abstract
Aim
Studies on the changes in the presentation and management of acute myocardial infarction (AMI) during the COVID-19 pandemic from low- and middle-income countries are limited. We sought to determine the changes in the number of admissions, management practices, and outcomes of AMI during the pandemic period in India.
Methods & Results
In this two-timepoint cross-sectional study involving 187 hospitals across India, patients admitted with AMI between 15th March to 15th June in 2020 were compared with those admitted during the corresponding period of 2019.
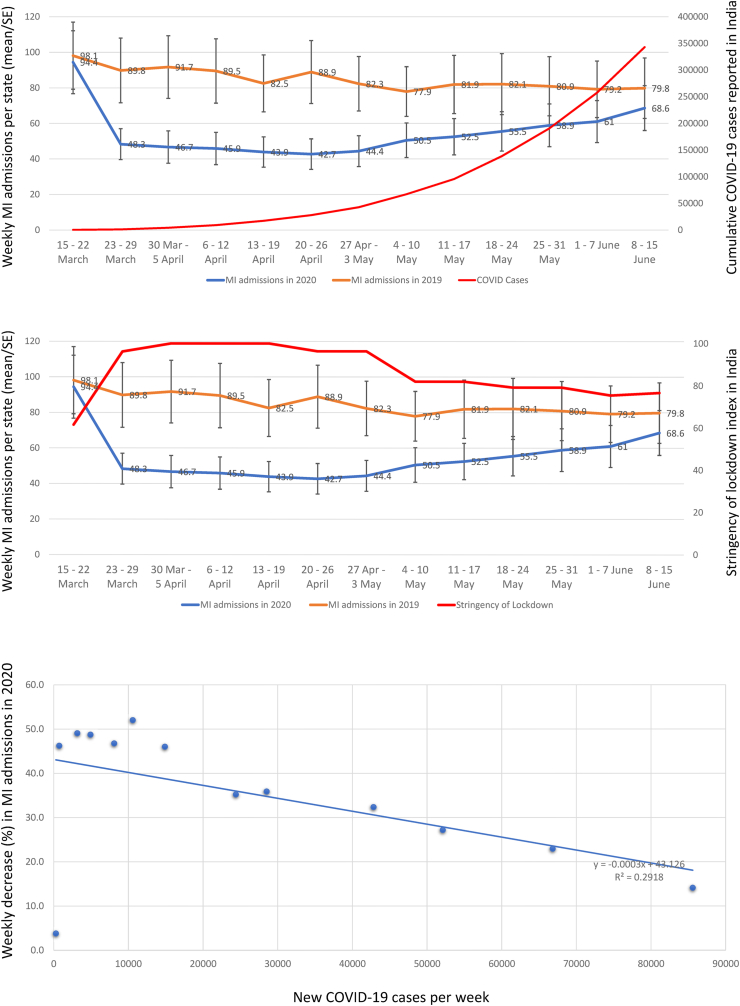
We included 41,832 consecutive adults with AMI. Admissions during the pandemic period (n = 16414) decreased by 35·4% as compared to the corresponding period in 2019 (n = 25418). We observed significant heterogeneity in this decline across India. The weekly average decrease in AMI admissions in 2020 correlated negatively with the number of COVID cases (r = −0·48; r2 = 0·2), but strongly correlated with the stringency of lockdown index (r = 0·95; r2 = 0·90). On a multi-level logistic regression, admissions were lower in 2020 with older age categories, tier 1 cities, and centers with high patient volume. Adjusted utilization rate of coronary angiography, and percutaneous coronary intervention decreased by 11·3%, and 5·9% respectively.
Conclusions
The magnitude of reduction in AMI admissions across India was not uniform. The nature, time course, and the patient demographics were different compared to reports from other countries, suggesting a significant impact due to the lockdown. These findings have important implications in managing AMI during the pandemic.
Keywords: Acute myocardial infarction (AMI), LMIC, Low-and middle-income country, COVID-19 pandemic, Acute coronary syndrome, ST elevation Myocardial infarction (STEMI), Non ST elevation Myocardial infarction (NSTEMI) and outcome
1. Introduction
Many countries have reported a significant decline in the hospitalization rates for acute myocardial infarction (AMI) during the time of COVID-19 pandemic with average rate of decline ranging from 13 to 48%.1, 2, 3, 4, 5, 6 India is the second most affected country in the world by COVID-19 pandemic with more than 10·4 million cases.7 The Government of India implemented strict nationwide lockdown in phases starting from 25th March 2020 to limit the spread of the pandemic. The central and various state governments directed the major hospitals to focus on COVID-19 crisis. This approach may have resulted in unintended compromises in acute cardiac care across the country. Recent studies from Europe,1, 2, 3, 4, 5,8, 9, 10 the USA,6,11,12 Asia,13,14 and New Zealand15 have not only shown a decrease in hospital admissions for AMI, but also an increase in time to medical contact, decrease in interventions, and increase in out of hospital cardiac arrests10 during the pandemic period. The impact of COVID-19 on AMI admissions in low- and middle-income countries including India is largely unknown.
Previous studies of acute coronary syndrome from India have shown several deficiencies in the care of AMI in the country.16, 17, 18 Even in the non-COVID times, the symptom-to door times were longer, interventions rates for AMI lower, and the reported in-hospital mortality higher in India as compared to developed countries.18 We hypothesized that these measures of access, and quality may have worsened during the COVID-19 pandemic, leading to an increase in morbidity, and mortality. Given the poor availability of ambulance services in various states,16 and the prolonged periods of lock down would potentially make it difficult for the patients to access cardiac care across India. A detailed study of the pattern of weekly admission rates is important to understand the determinants of changes in rates of AMI admissions in India, since the nationwide lockdown preceded the increase in COVID cases by a few months in India. Some reports have suggested that reduction in air pollution levels due to lockdown may have been at least partly responsible for the reduction in AMI admissions.19 We intended to study the effect of these factors on the weekly changes in the rate of AMI admissions across India, and the contribution of heterogeneity in AMI care facilities to the quality of care. Thus, this nationwide study initiated by the Cardiological Society of India (CSI) aims to assess the pattern of AMI admissions in India and evaluate the changes in the in-hospital management of these patients.
2. Methods
We conducted a multicenter, nation-wide, cross-sectional study among selected cardiac care hospitals in India, mimicking a natural interrupted time series with the data of 2019 serving as baseline, and the selected 2020 COVID-19 pandemic period as the change, in the factors that determine AMI patterns, demography, and outcomes. The detailed methodology of this CSI-AMI (Cardiological Society of India – AMI) study is described elsewhere.20 All consecutive cases of AMI admitted in the participating hospitals between 15th of March to 15th of June in 2020 were analyzed and compared with AMI cases admitted during the corresponding period in 2019. Upon initial screening, 257 public and private hospitals in urban and rural settings across India consented to participate. However, 70 hospitals could not participate due to various reasons including inability to provide ethical approval in time (n = 21), site investigator (s) or hospital record system being overwhelmed with COVID-19 (n = 43), and inability to provide 2019 data (n = 6). The study thus involved 187 hospitals with 275 site investigators, and 30 state/regional coordinators from 24 states, and 2 union territories covering all the regions, and major states and cities of India. Of the 26 chapters of CSI (chapters are branches of CSI located in various states/cities), 22 chapters participated in the study. Individual participating centers either obtained an ethical approval from respective Institutional ethics committees or a no objection certificate from the administration.21 Since this was a retrospective study without disclosing any confidential patient related data, informed consent was waived off by the Ethics committee of the CSI Kerala Chapter and all ethics committees of the participating centers. The study was prospectively registered with the Clinical Trial Registry of India CTRI (No CTRI/2020/09/027613). The study was conducted as per Indian Council of Medical Research (ICMR) collaborative study- and Good Clinical Practice (GCP)- guidelines (21). All the state coordinators were encouraged to complete the GCP certification process.
We included all consecutive adult (age >18 years) patients presenting to the participating hospitals with a diagnosis of AMI within 14-days of symptom onset. We used the standard definitions of ST elevation myocardial infarction (STEMI), and non-ST elevation myocardial infarction (NSTEMI).22,23 We excluded NSTEMI patients who were troponin negative at the time of hospitalization, already enrolled earlier in the study by another center, and where the required medical records could not be retrieved. The site investigators collected all consecutive case records. The patient data was anonymized in the electronic case report forms (e-CRF) and uploaded to a dedicated website. The state/regional coordinators supervised the e-CRF entries periodically for errors and missing information, and finally verified and submitted the data for analysis. We also randomly verified 3% of the e-CRFs with source documents. We received 42525 entries from participating centers. Cases with admission outside the study period (n = 394), duplicate entries (n = 273), incomplete data (n = 17), and significant variations found on source document verification (n = 9) were excluded.
We obtained data from all participating centers regarding the number of consultants in cardiology, their location (Metro/urban/rural), whether running an academic program [Doctorate in medicine (DM)/Diplomate of national board (DNB),] usual initial strategy of revascularization in STEMI (thrombolysis/primary percutaneous coronary intervention (PCI)/pharmaco-invasive), availability of onsite coronary artery bypass grafting (CABG) and facility for 24∗7 PCI for STEMI. We classified the location of the hospital into tier 1, 2 and 3 cities based on a classification system used by the Government of India centered on 2011 census population.24
We compared the demographics, procedures, and outcomes among patients admitted with AMI in 2019 and 2020 with 99% confidence intervals (CI). Average state-wise and zone-wise reduction in AMI admissions was estimated. We also calculated weekly decrease in admission rates for AMI and STEMI, and mortality rates in 2020 as compared with 2019 with 99% CI. To assess the determinants of weekly decrease in AMI in 2020, weekly state-wise number of confirmed COVID-19 cases was obtained.25 We also used the indices measuring strictness of lockdown and others during the study period reported by Oxford University for India including government response index, containment health index, stringency of lockdown and economic support.26 An effort was made to estimate these indices for different States of India. However, they were identical across the states for most of the study period. We calculated weekly average air quality index (AQI) and PM-2·5 for 2019 and 2020 from monitoring stations in 25 major cities.
2.1. Statistical methods
All data cleaning and statistical analyses were performed using Stata 15·0 (Stata Corp LP, TX, USA). Quantitative variables are expressed as mean and standard deviation and qualitative variables expressed as frequencies, and percentages. The characteristics of hospitalized patients with AMI and with respect to prespecified groups such as STEMI and NSTEMI were compared between the years 2019 and 2020 using the z-test for comparison of proportions/means and the results are reported as percent change and 99% confidence interval (CI). The weekly admission rates and in-hospital mortality in 2019 and 2020 were plotted against weekly increase in COVID-19 cases and strictness of lockdown index across the country with the estimation of correlation coefficient.
Multilevel logit model accounting for clustering effect (hospital) to identify independent characteristics that were different among AMI admissions in 2020 as compared to 2019 was fitted using ‘xtmelogit’ command. The results are reported as odds ratio along with 95% CI. The adjusted differences in the utilization rates for angiography, PCI, primary PCI and CABG, and in-hospital mortality were estimated using multilevel linear regression model and these were adjusted for clustering effect and various factors including age, gender, STEMI, complication, tier of city, and nature of hospital. The results are reported as regression coefficient along with 95% CI. We used generalized estimating equation (GEE) population averaged model with Poisson distribution to identify predictors of state-wise weekly decrease in AMI admissions and the results are reported as incidence rate ratio (IRR) along with 95% CI (supplement).
All the p-values were two-tailed and less than 0·05 was considered statistically significant.
3. Results
We included 41,832 (78·4% male) patients of AMI in our study with a mean (±SD) age of 58·2 ± 11·7 years. Admissions for MI during the three months of the pandemic period in 2020 decreased by 35·4% compared to corresponding three months period in 2019 with numbers dropping from 25418 to 16414. Admissions in 2020 included a higher proportion of males and STEMI (Table 1). The utilization rates of angiography, any PCI and CABG in 2020 decreased by 10·4%, 4% and 2% respectively. Adjusted utilization rate of CAG decreased by 11·3% (95% CI: −15·9, −6·7; P = <0.001), PCI decreased by 5·9% (95% CI: −10·3, −1·4; P = 0.02) and CABG decreased by 2·1% (95% CI: −3·6, −0·6; P = 0.006). The mean days of hospitalization did differ significantly between the two periods, but the difference was not clinically relevant. Comparing the two periods, the mean age at admission differed only by 0.3 years. However, the proportion of patients aged 60–80 years (39.6% in 2019 Vs. 38.8 in 2020) and 80-plus years (2.5% in 2019 Vs. 2.3% in 2020) reaching the hospital was significantly lesser in 2020 as compared to 2019. Moreover, the percentage reduction in AMI admissions during the pandemic was greater in the age groups 60–80 years (36.8%) and 80-plus (40.6%) than among < 40-year-olds (32.4%). Greater proportion of patients admitted in 2020 had complications associated with AMI and lesser proportion had LVEF >50%. However, the in-hospital mortality rate did not differ significantly (Table 1). The adjusted in-hospital mortality in 2020 was 0·2% higher, which was not significantly different from 2019 (95% CI: −0·6, 1·0; p = 0·6].
Table 1.
Characteristics of hospitalized patients with myocardial infarction.
| Characteristic | Total (n = 41832) | 2019 (n = 25418) | 2020 (n = 16414) | Change (99% CI) | P Value |
|---|---|---|---|---|---|
| Age (years) | 58·2 ± 11·7 | 58·3 ± 11·8 | 58·0 ± 11·7 | −0·23 (−0·5, 0·07) | 0·05 |
| Male gender | 32,814 (78·4%) | 19,847 (78·1%) | 12,967 (79·0%) | +0·9% (- 0·1, 1·9) | 0·03 |
| STEMI | 27,184 (65·0%) | 16,055 (63·2%) | 11,129 (67·8%) | +4·6% (3·4, 5·9) | <0·001 |
| Coronary angiography | 33,149 (79·2) | 21,176 (83·3%) | 11,973 (72·9%) | - 10·4% (- 11·4, - 9·3) | <0·001 |
| Any PCI | 23,593 (56·4%) | 14,738 (58·0%) | 8855 (54·0%) | - 4·0% (- 5·3, - 2·8) | <0·001 |
| CABG | 1796 (4·3%) | 1293 (5·1%) | 503 (3·1%) | - 2·0% (- 2·5, - 1·5) | <0·001 |
| Complications of MI∗ | 4665 (11·2%) | 2729 (10·7%) | 1936 (11·8%) | +1·1% (0·2, 1·9) | <0·001 |
| LVEF Categories | |||||
| <30% | 2950 (7·1%) | 1780 (7·0%) | 1170 (7·1%) | +0·1% (−0·5, 0·8) | 0·61 |
| 30–50% | 25,107 (62·4%) | 15,734 (61·9%) | 10,373 (63·2%) | +1·3% (0·05, 2·5) | 0·007 |
| >50% | 10,515 (25·1%) | 6690 (26·3%) | 3825 (23·3%) | - 3·0% (−4·1, −1·9) | <0·001 |
| Unknown | 2260 (5·4%) | 1214 (4·8%) | 1046 (6·4%) | +1·6% (1·0, 2·2) | <0·001 |
| Days admitted | 3·8 ± 2·9 | 3·9 ± 3·0 | 3·8 ± 2·8 | −0·1 (−0·2, – 0·05) | 0·004 |
| In- Hospital mortality | 1975 (4·7%) | 1172 (4·6%) | 803 (4·9%) | +0·3% (−0·3, 0·8) | 0·19 |
CI – Confidence interval, STEMI – ST elevation myocardial infarction, PCI – percutaneous coronary intervention, CABG – coronary artery bypass grafting, MI – myocardial infarction, and LVEF – left ventricular ejection fraction.
∗Complications of MI include cardiogenic shock, mechanical complications, and malignant arrhythmia.
Admissions for STEMI decreased by 30·7%; from 16055 in 2019–11129 in 2020 (Table 2). Patients admitted with STEMI in 2020 were less likely to undergo coronary angiography, PCI, and CABG. The adjusted difference in the primary PCI rates was 2·6% (95% CI: −5·2, −0·07; p = 0·04) lower in 2020. However, the complication rate, duration of hospitalization and in-hospital mortality did not differ between the two time periods. The proportion of patients with STEMI receiving thrombolysis increased by 4·7% during the COVID period. Patients of STEMI admitted in 2020 were less likely to undergo pharmaco-invasive therapy (- 3·3%) or rescue PCI (−3·0%. Information on symptom to lysis time and door to needle time did not differ between 2019 and 2020. However, the symptom to balloon time among patients undergoing primary PCI decreased significantly in 2020 (Table 2).
Table 2.
Baseline characteristics of ST elevation myocardial infarction (STEMI) patients.
| Characteristic | Total (n = 27,184) | 2019 (n = 16,055) | 2020 (n = 11,129) | Change with 99% CI | P Value |
|---|---|---|---|---|---|
| Age | 57·3 ± 11·8 | 57·4 ± 11·8 | 57·1 ± 11·8 | - 0·3% (−0·7, 0·1) | 0·05 |
| Male gender | 21,914 (80·6%) | 12,893 (80·3%) | 9021 (81·1) | +0·8% (−0·5, 2·0) | 0·12 |
| Coronary angiography | 21,286 (78·3%) | 13,313 (82·9%) | 7973 (71·6%) | - 11·3% (−12·6, −9·9) | <0·001 |
| Any PCI | 16,799 (61·8%) | 10,327 (64·3%) | 6472 (58·2%) | - 6·2% (−5·7, −5·9) | <0·001 |
| CABG | 985 (3·6%) | 708 (4·4%) | 277 (2·5%) | - 1·9% (−2·5, −1·4) | <0·001 |
| Complications of MI∗ | 3790 (13·9%) | 2211 (13·8%) | 1579 (14·2%) | +0·4% (−1·5, 0·7) | 0·33 |
| Type of MI | <0·001 | ||||
| Anterior wall | 15,786 (58·1%) | 9234 (57·5%) | 6552 (58·9%) | +1·4% (0·2, 2·9) | 0·03 |
| Inferior wall | 10,052 (36·98%) | 5911 (36·8%) | 4141 (37·2%) | +0·4% (−1·1, 1·4) | 0·51 |
| Others | 1346 (4·9%) | 910 (5·7%) | 436 (3·9%) | −1·8% (−1·1, −2·4) | <0·001 |
| Type of revascularization | <0·001 | ||||
| Primary PCI | 8397 (30·9%) | 5015 (31·2%) | 3382 (30·4%) | - 0·9% (- 0·6, 2·3) | 0·14 |
| Thrombolysis | 9349 (34·4%) | 5216 (32·5%) | 4133 (37·1%) | +4·7% (3·1, 6·2) | <0·001 |
| No initial revascularization | 9438 (34·7%) | 5824 (36·3%) | 3614 (32·5%) | - 3·8% (−5·3, −2·3) | <0·001 |
| In- Hospital mortality | 1640 (6·0%) | 983 (6·1%) | 657 (5·9%) | - 0·2% (−0·5–0·9) | 0·46 |
| Thrombolysis | |||||
| Agent used | |||||
| Streptokinase | 5685 (60·8%) | 3163 (60·6%) | 2522 (61·0%) | +0·4% (−2·2, 2·99) | 0·71 |
| Tenecteplase | 2892 (30·9%) | 1580 (30·3%) | 1312 (31·7%) | +1·5% (−1·0, 3·9) | 0·13 |
| Others∗∗ | 772 (8·3%) | 473 (9·1%) | 299 (7·2%) | 0·004 | |
| Post-thrombolysis | |||||
| Pharmaco-invasive strategy | 1676 (20·3%) | 1015 (21·8%) | 661 (18·4%) | - 3·3% (−1·0, −5·6) | <0·001 |
| Rescue PCI | 1940 (23·5%) | 1158 (24·8%) | 782 (21·8%) | - 3·0% (−5·4, −0·6) | 0·001 |
| Primary PCI | |||||
| Median Symptom to balloon time (min) (n = 5961) | 240 (IQR 140–360) | 240 (IQR 150–360) | 240 (IQR 130–360) | - 21·8 (−36·3, −6·9) | <0·001 |
|
Median Door to balloon time (min) (n = 6031) |
45 (IQR 30–74) | 45 (IQR 30–70) | 45 (IQR 30–75) | +0·8 (- 2·5, 4·0) | 0·54 |
| No revascularization (9438) | |||||
| Contraindication to lysis | 152 (1·8%) | 92 (1·7%) | 60 (1·8%) | ||
| Other Causes | 1416 (16·4%) | 876 (16·5%) | 540 (16·3%) | ||
| Late presentation | 7063 (81·8%) | 4348 (81·8%) | 2715 (81·9%) | ||
| 12–24 h | 1895 (26·8%) | 1176 (27·1%) | 719 (26·5%) | ||
| 24–48 h | 1895 (26·8%) | 1150 (26·5%) | 745 (27·4%) | ||
| >48 h | 3273 (46·3%) | 2022 (46·5%) | 1251 (46·1%) | 0·65 |
CI – Confidence interval, PCI – percutaneous coronary intervention, CABG – coronary artery bypass grafting, MI – myocardial infarction, and LVEF – left ventricular ejection fraction.
∗Complications of MI include cardiogenic shock, mechanical complications, and malignant arrhythmia.
∗∗Alteplase, reteplase and urokinase.
Hospitalization for NSTEMI decreased by 43·6% in 2020, significantly more than the reduction in STEMI admissions. Patients of NSTEMI admitted in 2020 were less likely to have LVEF >50%, less likely to undergo angiography, PCI, or CABG and more likely to have complications of MI (Table 3). The in-hospital mortality was higher for NSTEMI in 2020 by 0·7% (99% CI: 0·1, 1·4; P = 0.004).
Table 3.
Characteristics of NSTEMI patients.
| Characteristic | Total (n = 14,648) | 2019 (n = 9363) | 2020 (n = 5285) | Absolute Change with 99% CI | P Value |
|---|---|---|---|---|---|
| Age | 59·8 ± 11·5 | 59·7 ± 11·6 | 59·9 ± 11·4 | +0·2 (−0·3, 0·7) | 0·30 |
| Male gender | 10,900 (74·4%) | 6954 (74·3%) | 3946 (74·7%) | +0·4% (−1·5, 2·3) | 0·60 |
| Coronary angiography | 11,863 (80·99%) | 7863 (83·98%) | 4000 (75·7%) | −8·3% (−10·1, −6·5) | <0·001 |
| Any PCI | 6794 (46·4%) | 4411 (47·1%) | 2383 (45·1%) | −2·0% (−4·2, −0·2) | 0·02 |
| CABG | 811 (5·5%) | 585 (6·3%) | 226 (4·3%) | −2·0% (−2·9, −1·0) | <0·001 |
| Complications of MI∗ | 875 (6·0%) | 518 (5·5%) | 357 (6·8%) | +1·2% (0·1, 2·3) | 0·003 |
| LVEF Categories | |||||
| <30% | 766 (5·2%) | 471 (5·0%) | 295 (5·6%) | +0·6% (−0·4, 1·5) | 0·15 |
| 30–50% | 6844 (46·7%) | 4304 (46·0%) | 2540 (48·1%) | +2·1% (0·1, 4·3) | 0·02 |
| >50% | 6334 (43·2%) | 4184 (44·7%) | 2150 (40·7%) | −4·0% (−1·8, −6·2) | <0·001 |
| Unknown | 704 (4·8%) | 404 (4·3%) | 300 (5·7%) | +1·4% (0·4, 2·4) | <0·001 |
| In- Hospital mortality | 335 (2·3%) | 189 (2·0%) | 146 (2·8%) | +0·7% (0·1, 1·4) | 0·004 |
CI – Confidence interval, PCI – percutaneous coronary intervention, CABG – coronary artery bypass grafting, MI – myocardial infarction, and LVEF – left ventricular ejection fraction.
∗Complications of MI include cardiogenic shock, mechanical complications, and malignant arrhythmia.
Patterns of AMI admissions varied significantly among various zones of India with the North zone reporting a 44·8% decrease as compared to South zone which reported a 27·7% decrease in AMI hospitalization in 2020 (Fig. 1). Also, there was significant inter-state variation with Kerala, a southern state reporting only 8·4% decrease as compared to Delhi reporting 53·6% decrease in AMI admissions in 2020. The weekly average decrease in AMI admissions across all the states in 2020 peaked around the middle of the study period. The difference significantly lessened after the end of second phase of lockdown and the trend continued till the end of the study period (Fig. 2A). The percentage decrease in weekly AMI was negatively correlated to the number of COVID cases (r = −0·48; r2 = 0·2). However, the weekly decrease in AMI admissions correlated linearly with the stringency of lockdown index (r = 0·95; r2 = 0·90) (Fig. 2A–D). The weekly decrease in STEMI admissions also followed a similar trend, but there was no change in weekly mortality rates (Fig. 2E–F).
Fig. 1.
Decrease in MI admissions across various zones of India in 2020 as compared to 2019 with 99% CI.
Fig. 2.
A. Weekly trends in MI admissions per state as compared to cumulative COVID-19 cases in India.B. Weekly trends in MI admissions per state as compared to stringency of lockdown index.C. Correlation between weekly decrease in MI admissions in 2020 and new COVID-19 cases in India. D. Correlation between weekly decrease in MI admissions in 2020 and stringency of lockdown index. E. Weekly STEMI admissions as compared to new COVID-19 cases. F. Weekly trends in MI mortality as compared to Government response index.
On univariate analysis, age, gender, complications, nature of hospital (public or private), teaching category (DM/DNB/None), volume of AMI admissions in 2019, tier of city, and number of cardiologists were significantly different. On a multi-level logistic regression, admissions were lower in 2020 with increasing age categories and increasing patient volume of admitting centers in a graded manner. Tier 1 cities and hospitals with a teaching DM program also reported significant decrease in AMI admissions in 2020. Proportion of STEMI and complications of AMI were more represented in 2020.
3.1. Predictors of weekly decrease in AMI admissions
Predictors of state-wise weekly AMI admissions were analyzed using Poisson GEE population averaged model. The IRR for AMI admissions in 2020 was 0.68 (95% CI: 0.6, 0.8; P < 0.001) as compared to 2019. Weekly reduction was significant for all the subsequent 12-weeks as compared to the first week of the study (15–23 March 2020), when there was no lock down. The reduction peaked around the 7th week of the study period (IRR 0.68; 95% CI: - 0.6, 0.8). The number of state-wise COVID cases and PM-2.5 levels were not significantly predictive of the weekly state-wise AMI admissions (IRR 1.0; p = 0.9). However, higher AQI predicted increased weekly AMI admissions with an IRR of 1.002 (95% CI: 1.0003, 1.004; P = 0.02).
4. Discussion
The present study reports the number, nature, time course, patient characteristics, and outcomes of AMI admissions during COVID-19 pandemic from India. We observed a 35% reduction in AMI admissions across India during the COVID-19 pandemic as compared to a corresponding period in 2019, which was similar to the scale of reduction reported from other countries.1, 2, 3, 4 However, the nature, time course, and duration of changes were different in our study as compared to the other recent series from Western countries.1, 2, 3, 4 Changes in patient characteristics between the time periods, and significant heterogeneity across various regions of India are the major highlights of the study, which are substantially different from the data published from other countries.
Most of the earlier reports from other countries have either not reported differences in demographics or reported negligible differences.1, 2, 3, 4, 5, 6,8, 9, 10 However, we noted minor differences in the age distribution of patients during the pandemic period. The chance for sixty-year, and eighty-year-old getting admitted with AMI in 2020 was reduced by 10% and 18% respectively as compared to a forty-year-old patient. Even though female gender was less represented during the pandemic period, the gender difference was not statistically significant on multivariate analysis. These differences from the previous studies could be because of wider age distribution of Indian AMI patients, varied education and awareness levels of the patients, differences in healthcare systems, withdrawal of elderly healthcare due to economic and social reasons,8, and access to insurance for the elderly. Similar to the other reports, reduction in NSTEMI was higher than STEMI.1,27 Patients with STEMI usually develop significant and severe new onset symptoms especially among younger patients; therefore, these symptoms are unlikely to be ignored and patients would make attempts to reach the hospital despite the pandemic. In contrast, NSTEMI often occurs in older patients with previously established coronary artery disease and can have a myriad of symptoms, which may result in delay in patients reporting to a hospital. However, some studies identified similar2,6 or more reduction in STEMI than NSTEMI. Proportion of patients with complications of AMI was significantly more during the pandemic period, which was comparable to some of the reports from other countries.1
Our study identified significant changes in the management strategies of AMI patients. In England, 60% decrease in PCI and 80% decrease in CABG has been reported during the pandemic period.1 The corresponding figures were 40% for PCI and 60% for CABG in India. Much of the difference was accounted for by the decrease in number of admissions. Length of hospital stay did not change in India but was reduced in England.1 We observed interesting differences in the care of STEMI during the pandemic period. Primary PCI for STEMI was reduced by 32·6% and in comparison, PCI for NSTEMI was reduced by 46%. This was mostly driven by a decrease in STEMI admissions rather than a decrease in the proportion of STEMI patients undergoing primary PCI. Similarly, data from other countries also suggested that though overall primary PCI numbers were reduced, the relative proportion of patients receiving primary PCI actually increased during the pandemic period.27, 28, 29 The proportion of STEMI patients receiving thrombolysis also increased across India. Consequently, overall reperfusion rates increased during the pandemic period, which could in part explain the lack of mortality difference among STEMI patients treated in 2020 in our study. In addition, the various presentation times did not differ or in fact improved during the pandemic in contrast to those reported from China, which could be due to the lessened travel times during the lock down in the mostly congested Indian roads and patient preference for nearby hospitals rather than tertiary centers. However, the mortality significantly increased for NSTEMI during the pandemic, mostly related to sicker patients and lesser utilization of invasive procedures.
The decline in AMI admissions reported from various countries was uniform across geographies studied in the respective studies.1 However, we observed significant zone-wise and state-wide variations across India. While the states that were affected early by COVID-19 in India including Maharashtra, Delhi, Gujarat, and Tamil Nadu reported a significant decline in AMI admissions (ranging 40–53%), the less affected States by June 2020 showed wide variation in decline ranging from 8·4% in Kerala to 40% in Uttar Pradesh (UP) (Fig. 1). These observations may be explained by the differences in health systems and access to health care. For example, in Kerala the number of hospitals that could provide primary PCI per million population was 3.5 as compared to 0.5 in UP. Given that there are 127 PCI facilities available in all districts of Kerala as compared to only 120 facilities covering only 35% of districts in UP, the distance a patient needed to travel to avail PCI facilities was likely higher in UP (data not shown). India followed a nearly uniform nation-level of lockdown and most of the cities reported a decline in air pollution levels. Hence, the variation in decline cannot solely be explained by the rise in COVID cases, and levels of lockdown. The state-wise weekly increase in COVID-19 cases was not a determinant of weekly change in AMI admissions. Also, the reduction in AQI, a measure of air quality, and not PM-2.5 observed in 2020, was an independent determinant of state-wise decline in AMI admissions. However, air quality data was not available for all the participating cities. Differences in the response to COVID-19 by diverse healthcare systems, varying fear response among patients due to education and socioeconomic backgrounds, varied distribution of cardiac care centers across the states, private versus public health care systems, accessibility to cardiac care throughout the pandemic, and availability of ambulance services are some of the factors likely to be responsible for the heterogeneity. The quantum of reduction was lower in non-teaching hospitals and lower volume centers as seen in England also (28). Overall, tier 3 cities reported a lesser decline as compared to large tier 1 cities (Fig. 3). One reason for this could be that patients who generally preferred to go to better equipped hospitals in tier 1 cities during non-COVID times might have decided to seek care in nearby tier 2 and 3 cities to avoid long travel time during lock down and fear of cross infection with COVID. The Southern states (excluding Tamil Nadu, which was engulfed with COVID pandemic early) have reported only 18.2% decline and all of them have better healthcare infrastructure, ambulance services, widely available standalone cardiac care centers and private hospital/insurance based cardiac care as compared to North zone, which reported a 44.8% decline.
Fig. 3.
Multi-level logit model with patient and hospital level variables characterizing MI admissions in 2020 in comparison to 2019.
Very few studies have estimated the time course of changes in AMI admission rates. Recent studies from England,1,27 and USA6 suggested that the admission rates for AMI paralleled the COVID-19 pandemic with low rates of admissions in the peak phases of pandemic and an increase in admission rates with the decline of the pandemic. The decline in AMI admissions preceded lockdown by 2-weeks in England and US, whereas there was precipitous decline in India just at the onset of lockdown. This could be related to the fact that when the lockdown was first imposed in India on March 25, 2020, there were very few COVID-19 confirmed cases across the country. However, the trend followed what has been reported in the earlier studies, with the peak reduction happening after 4–6 weeks and then the trend partly reversed over time such that by 3-months, there was only marginal reduction of AMI admissions. Unlike in England, where the local cardiology societies made concerted efforts to bring back patients with AMI to hospitals with campaigns, in India there were no such concerted action, yet the decline in AMI admissions reduced over time. In contrast to the data from USA, where the decline coincided with increase in COVID-19 cases, we observed poor correlation with the number of cases whereas the strictness of lockdown correlated better with the quantum of decline.
Whether some of the decline represents a true decline in incident AMI resulting from improving air quality, less stress and so on, is difficult to prove or disprove. Considering all the available evidence, the initial fear of COVID-19, changing priorities of healthcare systems, strictness of lockdown and lack of dedicated cardiac care/ambulances (esp. in India) are the major factors responsible for decline in AMI admissions. These findings provide important lessons to plan for a second/third wave or to prepare for future pandemics or recurrences. A concerted effort to address most of these factors is needed to prevent the collateral damage. The cardiology societies and the governments should make sure patients are adequately educated about the need for emergency cardiac care, make hospitals and ambulances available for cardiac care. With some exceptions, the data and strategies may be applicable across several low- and middle-income countries. Considering an estimated 3 million STEMI per year in India, a 35% reduction in India during the pandemic, would translate to a staggering 1 million less STEMI admissions alone in a year. This would result in increased cardiac arrests in the community,30 more patients with LV dysfunction and heart failure presenting later, and lack of secondary prevention measures for a vast majority with AMI. With an average age of AMI of 58-years, the health and economic consequences would be staggering for an emerging economy.
4.1. Strengths and limitations
This is one of the largest data on AMI from India. The major strength of our study is that this is one of the most comprehensive study that evaluated various aspects of AMI care including patient characteristics, time trend of reduction and relevant outcomes. However, the major limitation is that it is retrospective in nature as we did not have readily accessible rapid data to analyses unlike in other developed countries. Like all retrospective studies of this nature, the mortality may be underrepresented, and data estimates inaccurate. The problem is compounded by the fact that systems of care for STEMI are not uniform and well established across the country as can be seen from the fact that the basic time intervals are not available in a significant proportion of patients. However, the study coordinators made every effort to ensure all consecutive AMI admissions were included and data quality verified at multiple levels. Another limitation is that even though we have collected data of large number of AMI patients, all regions of the country were not uniformly represented. Finally, the study was conducted during the initial phases of COVID-19 pandemic in India, and it is possible that if done during the later months when COVID peaked in India, results would have been different.
5. Conclusions
The admissions for AMI decreased by a third during the pandemic period with the decrease more for older age categories, NSTEMI, and in certain geographical parts of India. The overall angiography, PCI and CABG related to AMI decreased, however the in-hospital mortality did not differ. Lock down had more pronounced effect on decreased AMI admissions than the number of COVID cases. These findings may help in managing AMI patients during further recurrences of the pandemic in low-and middle-income countries.
Disclosure
The authors are solely responsible for the design of the study, the conduct of the study, drafting and editing of the paper, and its final contents.
Declaration of Helsinki: The authors declare that the study complies with the Declaration of Helsinki, and the locally appointed ethics committee has approved the research protocol and informed consent has been waived off since it was a retrospective study.
The authors do hereby declare that all illustrations and figures in the manuscript are entirely original and do not require reprint permission.
Contributions of authors
GZ-conceptualization, data curation, funding acquisition, methodology, project administration, resources, software, supervision, validation, and writing - review & editing. SR - data curation, formal analysis, methodology, validation, figures, writing - original draft, and writing - review & editing. MKD, AJ, JPB, VKN, DP, PKD, and MPP - methodology, project administration, resources, software, supervision, and writing - review & editing. KM - data curation and analysis, figures. GZ, SR, KM, and SK accessed and verified the underlying data. All authors contributed to data collection, study design, supervision, reviewing and editing the manuscript and approved the manuscript in the final form.
Source of funding
The work was supported by funds from Cardiological Society of India (CSI) and the participating chapters of CSI.
Declaration of competing interest
Nothing to declare for all the authors.
Acknowledgments
Our sincere thanks to the Cardiological Society of India (CSI) and its participating chapters.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ihj.2021.06.003.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Mafham M.M., Spata E., Goldacre R. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396:381–389. doi: 10.1016/S0140-6736(20)31356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Metzler B., Siostrzonek P., Binder R.K. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41:1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Filippo O., D'Ascenzo F., Angelini F. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Rosa S., Spaccarotella C., Basso C. Società Italiana di Cardiologia and the CCU Academy investigators group. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41:2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scholz K.H., Lengenfelder B., Thilo C. Impact of COVID-19 outbreak on regional STEMI care in Germany. Clin Res Cardiol. 2020;109:1511–1521. doi: 10.1007/s00392-020-01703-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Solomon M.D., McNulty E.J., Rana J.S. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383:691–693. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 7.COVID-19 pandemic in India. https://en.wikipedia.org/wiki/COVID-19_pandemic_in_India
- 8.Mesnier J., Cottin Y., Coste P. Hospital admissions for acute myocardial infarction before and after lockdown according to regional prevalence of COVID-19 and patient profile in France: a registry study. Lancet Public Health. 2020;5:e536–e542. doi: 10.1016/S2468-2667(20)30188-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rodríguez-Leor O., Cid-Álvarez B., Pérez de Prado A. Working group on the infarct code of the interventional cardiology association of the Spanish society of cardiology investigators. Impact of COVID-19 on ST-segment elevation myocardial infarction care. The Spanish experience. Rev Esp Cardiol. 2020;73:994–1002. doi: 10.1016/j.rec.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rashid Hons M., Gale Hons C.P., Curzen Hons N. Impact of coronavirus disease 2019 pandemic on the incidence and management of out-of-hospital cardiac arrest in patients presenting with acute myocardial infarction in England. J Am Heart Assoc. 2020;9 doi: 10.1161/JAHA.120.018379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gluckman T.J., Wilson M.A., Chiu S.T. Case rates, treatment approaches, and outcomes in acute myocardial infarction during the coronavirus disease 2019 pandemic. JAMA Cardiol. 2020;5:1419–1424. doi: 10.1001/jamacardio.2020.3629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xiang D., Xiang X., Zhang W. Management and outcomes of patients with STEMI during the COVID-19 pandemic in China. J Am Coll Cardiol. 2020;76:1318–1324. doi: 10.1016/j.jacc.2020.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tam C.F., Cheung K.S., Lam S. Impact of coronavirus disease 2019 (COVID-19) outbreak on outcome of myocardial infarction in Hong Kong, China. Cathet Cardiovasc Interv. 2021;97:E194–E197. doi: 10.1002/ccd.28943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chan Daniel Z.L., Stewart Ralph A.H., Kerr A.J. The impact of a national COVID-19 lockdown on acute coronary syndrome hospitalisations in New Zealand (ANZACS-QI 55) The Lancet Regional Health - Western Pacific. 2020;5 doi: 10.1016/j.lanwpc.2020.100056. 10 0 056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xavier D., Pais P., Devereaux P.J. CREATE registry investigators. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371:1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 17.Mohanan P.P., Mathew R., Harikrishnan S. Kerala ACS Registry Investigators. Presentation, management, and outcomes of 25 748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS Registry. Eur Heart J. 2013;34:121–129. doi: 10.1093/eurheartj/ehs219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guha S., Sethi R., Ray S. Cardiological Society of India: position statement for the management of ST elevation myocardial infarction in India. Indian Heart J. 2017;69:S63–S97. doi: 10.1016/j.ihj.2017.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Picano E. Where have all the myocardial infarctions gone during lockdown? The answer is blowing in the less-polluted wind. Eur Heart J. 2020;41:2146–2147. doi: 10.1093/eurheartj/ehaa411. [DOI] [PubMed] [Google Scholar]
- 20.Ramakrishnan S., Jabir A., Jayagopal P.B. Pattern of acute MI admissions in India during COVID-19 era: a Cardiological Society of India study - rationale and design. Indian Heart J. 2020;72:541–546. doi: 10.1016/j.ihj.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guidelines | Indian Council of medical research | government of India. https://main.icmr.nic.in/content/guidelines
- 22.O'Gara P.T., Kushner F.G., Ascheim D.D. American College of cardiology foundation/American heart association task force on practice guidelines. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of cardiology foundation/American heart association task force on practice guidelines. Circulation. 2013;127:e362–e425. doi: 10.1161/CIR.0b013e3182742cf6. [DOI] [PubMed] [Google Scholar]
- 23.Roffi M., Patrono C., Collet J.P., ESC Scientific Document Group ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European society of cardiology (ESC) Eur Heart J. 2015;37:267–315. doi: 10.1093/eurheartj/ehv320. 2016. [DOI] [PubMed] [Google Scholar]
- 24.Classification of Indian cities. https://en.wikipedia.org/wiki/Classification_of_Indian_cities assessed
- 25.https://api.covid19india.org/documentation/csv/on11th
- 26.Hale Thomas, Angrist Noam. Blavatnik School of Government; 2020. Oxford COVID-19 Government Response Tracker. [DOI] [PubMed] [Google Scholar]
- 27.Wu J., Mamas M., Rashid M. Patient response, treatments and mortality for acute myocardial infarction during the COVID-19 pandemic. Eur Heart J Qual Care Clin Outcomes. 2021;7:238–246. doi: 10.1093/ehjqcco/qcaa062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kwok C.S., Gale C.P., Kinnaird T. Impact of COVID-19 on percutaneous coronary intervention for ST-elevation myocardial infarction. Heart. 2020;106:1805–1811. doi: 10.1136/heartjnl-2020-317650. [DOI] [PubMed] [Google Scholar]
- 29.De Luca G., Verdoia M., Cercek M. Impact of COVID-19 pandemic on mechanical reperfusion for patients with STEMI. J Am Coll Cardiol. 2020;76:2321–2330. doi: 10.1016/j.jacc.2020.09.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shekhar A.C., Effiong A., Ruskin K.J. COVID-19 and the prehospital incidence of acute cardiovascular events (from the nationwide US EMS) Am J Cardiol. 2020;134:152–153. doi: 10.1016/j.amjcard.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.