Abstract
Objective
Development of novel informatics methods focused on improving pregnancy outcomes remains an active area of research. The purpose of this study is to systematically review the ways that artificial intelligence (AI) and machine learning (ML), including deep learning (DL), methodologies can inform patient care during pregnancy and improve outcomes.
Materials and methods
We searched English articles on EMBASE, PubMed and SCOPUS. Search terms included ML, AI, pregnancy and informatics. We included research articles and book chapters, excluding conference papers, editorials and notes.
Results
We identified 127 distinct studies from our queries that were relevant to our topic and included in the review. We found that supervised learning methods were more popular (n = 69) than unsupervised methods (n = 9). Popular methods included support vector machines (n = 30), artificial neural networks (n = 22), regression analysis (n = 17) and random forests (n = 16). Methods such as DL are beginning to gain traction (n = 13). Common areas within the pregnancy domain where AI and ML methods were used the most include prenatal care (e.g. fetal anomalies, placental functioning) (n = 73); perinatal care, birth and delivery (n = 20); and preterm birth (n = 13). Efforts to translate AI into clinical care include clinical decision support systems (n = 24) and mobile health applications (n = 9).
Conclusions
Overall, we found that ML and AI methods are being employed to optimize pregnancy outcomes, including modern DL methods (n = 13). Future research should focus on less-studied pregnancy domain areas, including postnatal and postpartum care (n = 2). Also, more work on clinical adoption of AI methods and the ethical implications of such adoption is needed.
Keywords: literature review, pregnancy, artificial intelligence, machine learning
Introduction
In the field of medicine, the theory of ‘joint decision-making’ between humans and artificial intelligence (AI) holds the promise of promoting high-performance medicine. AI is a broad science of simulating the natural intelligence demonstrated by humans and animals via artificial means. Machine learning (ML) is a subset of AI, in the field of computer science. ML refers to a number of methods and algorithms, and different learning types: supervised, unsupervised and reinforcement learning [1, 2]. In the early days of AI in medicine, AI systems were standalone systems without direct connection to electronic health records (EHRs). Today, medicine is progressing towards a learning health system in which knowledge derived from information EHR data can be directly applied to care. Digitized clinical data in the EHR, genomics and biology present a wealth of information, open new opportunities and come with new challenges. AI and informatics methodologies are critical to enabling the learning health system.
One of the ways that AI and ML can be used in healthcare is in enabling ‘deep phenotyping’. In medicine, a disease phenotype refers to a deviation from healthy morphology or physiology [3]. Study of phenotypes requires knowledge of the spectrum of phenotypes associated with a disease entity. Defining what constitutes a diseased phenotype versus a healthy phenotype is often challenging. Deep phenotyping disease is a step towards precision medicine in which a comprehensive and precise phenotyping of disease presentation takes place. The individual components of the phenotype are observed, described and analyzed in order to develop knowledge of human disease. AI and ML methodologies naturally apply to characterize phenotypes in a ‘deep’ manner including multiple methodologies (e.g. genetics, imaging, diagnostics and so forth). These methods can exhaustively examine data with high granularity and dimensionality and make use of the broad range of data types that may be processed in deep phenotyping. For instance, nuanced phenotypic traits may be more readily available in unstructured data (e.g. clinical notes), requiring natural language processing (NLP) to identify relative information [4]. Several diseases and adverse outcomes during pregnancy (e.g. preterm birth, preeclampsia and miscarriage) have complicated and difficult to understand etiology, leaving little to be done for prevention [5–7]. Deep phenotyping these patient states (i.e. pregnancy phenotypes) could help improve adverse outcomes and provide further insight into diseases during pregnancy.
AI and ML methods can be employed to enable deep phenotyping, especially with regards to the pregnancy state where many different data types are used (e.g. ultrasound imaging, diagnostic screening, fetal monitoring, genetics). AI and ML methods in medicine are an emerging field and have been described in detail of its theory and current applications across several medical disciplines [8, 9] and many disease areas and clinical states [8, 10]. However, the use of AI to improve women’s health, specifically during the pregnancy, has had limited clinical use. In the 2019 International Medical Informatics Association Yearbook of Medical Informatics, there are no research articles focused on pregnancy and maternal health, illustrating the lack of research focus on this important aspect of women’s health [11]. For researchers and clinicians alike, AI techniques have promise to derive sound results and improve care at each stage of pregnancy [12–14].
Overall, the purpose of this study is to systematically review the ways that AI and ML methodologies can inform patient care during pregnancy and improve outcomes. We seek to (a) describe which medical fields and informatics areas apply AI and ML, (b) find where in pregnancy are these methodologies used, (c) describe clinical decision support systems (CDSSs) that employ AI or ML and (d) identify literature gaps for future research.
Methods
We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines when conducting our literature review [15]. See Supplementary Table available online at https://academic.oup.com/bib for PRISMA 2009 Checklist.
Systematic review of literature
We searched three databases: EMBASE, PubMed and SCOPUS. PubMed is a freely available database housing publications maintained by the United States National Center for Biotechnology Information. PubMed facilitates searching across three National Library of Medicine resources; the largest component is MEDLINE, followed by content from PubMed Central (PMC) and Bookshelf [16]. EMBASE is a bibliographic database focused on pharmacovigilance. SCOPUS is Elsevier’s publication database containing articles from over 36 000 peer-reviewed journals. We used site licenses from the University of Pennsylvania libraries to search SCOPUS and EMBASE. The initial query was broad: in PubMed, we searched the keywords in all fields; in SCOPUS, we searched article title, abstract and keywords; and in EMBASE, we used quick search. On 5 December 2019, we used the following search query to cast a wide net of potentially relevant papers for inclusion of our review: AI AND pregnancy. On 18 February 2020, we completed a more focused query, in order to identify papers that focused on ML: informatics AND pregnancy AND AI AND ML.
The PubMed interface uses Automatic Term Mapping to automatically map search words to their respective Medical Subject Headings terms [17]. After retrieving results from each database, we removed duplicate studies using exact PubMed ID match. When PubMed IDs were absent, we reviewed articles, comparing title, author list and publication date to further identify duplicate publications. We filtered the results by excluding non-English studies, conference papers, editorials and notes.
The eligibility criteria include AI and maternal health; papers were categorized by pregnancy stage and health concern. No location or publication date restrictions were applied and no unpublished papers were retained. Retrieved articles were inspected by an independent review (L.D.), and in cases where the eligibility of the study was unclear, it was reviewed by a second reviewer (M.R.B.). We excluded studies for which we were not able to gain access to the manuscripts.
Results
Systematic literature review results
First, we searched EMBASE, PubMed and SCOPUS for articles on pregnancy and AI. We found 245 from SCOPUS, 181 from EMBASE and 128 from PubMed. We removed duplicate studies. In total, we found that 381 distinct research papers were retrieved on the first query. For the second query, we found additional papers, including 4 from SCOPUS, 4 from EMBASE and 46 from PubMed. After removing duplicates from the new query, we had a result set of 427 distinct papers. Of these 427 distinct research studies, we excluded the 9 non-English studies, 124 conference papers, 4 editorials and 5 notes, resulting in a set of 285 research papers (Figure 1).
Figure 1 .
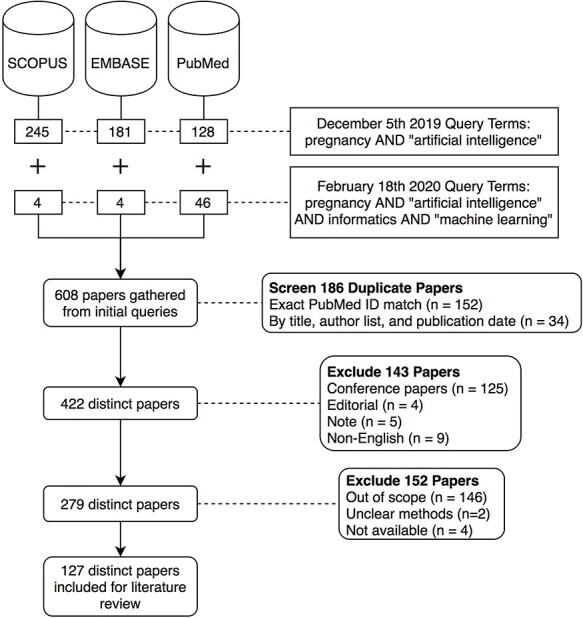
PRISMA diagram showing our literature search inclusion process.
The next step was to assess the 285 remaining research articles for relevance. We manually reviewed the 285 articles to determine if they met selection criteria: (1) focused on AI, (2) related to pregnancy and (3) related to healthcare and health information. These inclusion criteria resulted in 127 relevant papers. The final set contains almost four decades of research, issued from 1982 to 2020.
Identification of themes
We grouped the studies by the stage in pregnancy: preconception, assisted reproductive technology (ART), prenatal screening and monitoring, preterm labor, birth and delivery (full term) and postnatal to illustrate the different clinical areas where AI and ML methods were applied. These areas are shown in Figure 2; we distinguish between pregnant person and embryo, fetus or neonate as methods are designed explicitly for each respective concern. References to maternal and women’s health are reflecting the terms and concepts of research included in this paper. Pregnant people include transgender and gender non-conforming individuals; however, no papers (n = 0 studies) define this population explicitly.
Figure 2 .
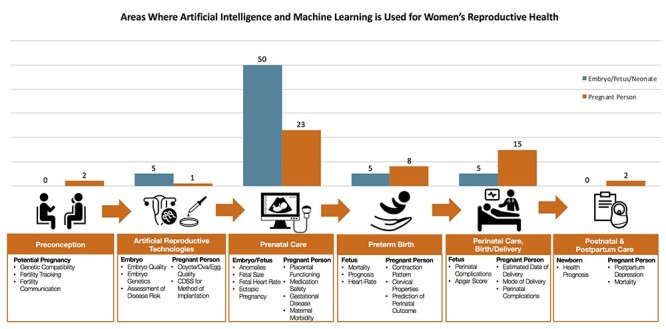
Different stages along the pregnancy timeline where AI and ML methods are used. This figure illustrates the points of care where AI and ML have been applied at each stage of pregnancy: preconception; artificial reproductive technologies; prenatal care; preterm birth; perinatal care, birth and delivery; and postnatal care. Healthcare concerning the pregnant person and fetus is distinguished for ease of reading. We also include the distribution of studies by pregnancy stage to illustrate the stages of the pregnancy with the most number of studies for easy identification of literature gaps.
CDSSs are explicitly described in each category where they are present. Table 1 presents studies by pregnancy stage, with an overview of the methodology and results. Not included in Table 1 is one evaluation of an application described in an included paper [18], and 8 review papers, reviewing applications in the following: general obstetrics [19], translational science [20], intrapartum surveillance [21, 22], fetal heart rate (FHR) [23], labor fetal assessment [24], ART [12] and mobile health (mHealth) for antepartum care [25]. AI may help address challenges in birth defects research. [20]. Reviews found great promise in AI applications, but not realized in clinical care [21, 22, 25], or missing external validation [12]. AI applications are warned as adjunct, not replacement, of healthcare professionals [19, 23]. One review found no evidence supporting improved pregnancy outcomes with AI applications [24]. AI methods applied are shown in Figure 3. Refer to Table 2 for further references into the methodologies observed in this review, along with pregnancy and informatics domains in which these methods were applied. Of the 127 studies, 16 applied AI and ML methods to retrospective EHR data. A total of 12 studies used expert systems as their AI methods (Figure 3), and these are often older, more historical AI methods applied to women’s health. Studies tended to focus on the prenatal care aspect of the pregnancy (Figure 2), with more studies focused on fetal aspects of the prenatal care (n = 50 studies) versus the maternal aspects of care (n = 23 studies). Another popular area where AI methods were used was perinatal/birth and delivery (15 studies focused on maternal outcomes and 5 focused on fetal outcomes). Other stages are represented to a lesser extent, especially preconception care and postpartum care with two studies each (Figure 2).
Table 1.
Articles published using AI to improve pregnancy outcomes: method details, pregnancy area, health issue, dataset details and model results
| Study | Methods | Objective | Health issue | Dataset | Result |
|---|---|---|---|---|---|
| Preconception | |||||
| Goodale et al. (2019) | Residual maximum likelihood, Satterthwaite degrees of freedom, Bonferroni correction, RF | To develop an algorithm that could identify the fertile window in real time | Fertility window | 237 conception-seeking Swiss women | Can detect significant, concurrent phase-based shifts in WST, heart rate and respiratory rate (all P < 0.001), while HRV and skin perfusion show less significance (P < 0.05) |
| Green et al. (2019a) | NB, NLP | Apply a text-mining approach to characterize the ways that Kenyan men and women communicated with the first iterations of askNivi, a free sexual and reproductive health information service | Reproductive health | 179 609 total messages (87 180 inbound and 92 429 outbound) from askNavi database | Users wrote most often about family planning methods, contraception, side effects, pregnancy, menstruation and sex. Most users sought factual information, but requests for advice and symptom reports were common |
| ART | |||||
| Morales et al. (2008) | Bayes’ classifiers: NB, selective NB, semi NB, tree-augmented NB, k-dependence Bayesian classifier | Proposes the application of Bayesian classifiers to the embryo selection problem | IVF outcome | 63 clinical files from IVF program in Clínica del Pilar in San Sebastián, (July 2003–December 2005, aged 27–46) and morphological characteristics of embryos | General accuracy of 68.25% with 95.55% of specificity and no-implantation predictive value of 70.49% |
| Nyalwidhe et al. (2013) | Genetic algorithm, SVM, k-NN | To identify differentially expressed peptides/proteins in the culture media of embryos grown during IVF treatment to establish their value as biomarkers predictive of implantation potential and live birth | Pregnancy success | Micro-droplets of embryo culture media from IVF patients (conditioned) and control media (January 2006–December 2010) | Found downregulation of apolipoprotein A-1 peptides and apolipoprotein A-1 protein in the pregnancy groups |
| Uyar et al. (2015) | NB, DT, k-NN, SVM, MLP, RBF | To predict implantation outcome of individual embryos in an IVF cycle with the aim of providing decision support on the number of embryos transferred | Pre-implantation | 2453 embryos transferred at day 2 or day 3 after intracytoplasmic sperm injection (ICSI) | NB, accuracy = 80.4%, sensitivity = 63.7%, false alarm rate = 17.6% |
| Milewski et al. (2017) | Principal component analysis, ANN | To answer the question of how much information about embryo implantation potential can be obtained from morphokinetic parameters | Pre-implantation | Time–lapse recordings of 610 embryos | Validation set, AUC = 0.71 |
| Khosravi et al. (2019) | DNN, Google’s Inception Model, chi-squared automatic interaction detection (CHAID) DT | Implemented an AI approach to select highest quality embryos using a large collection of human embryo time–lapse images | Pre-implantation | Time–lapse images from 10 148 embryos from the Center for Reproductive Medicine at Weill Cornell Medicine (2012/05–2017/12) | Chance of pregnancy based on individual embryos varies from 13.8% (age ≥ 41 and poor quality) to 66.3% (age < 37 and good quality) |
| Tran et al. (2019) | DL | To investigate if a DL model named IVY is a valid tool for the prediction of the implantation potential of human pre-implantation embryos | Pre-implantation | Time–lapse videos and clinical outcomes of 10 638 embryos from eight different IVF clinics, across four different countries (January 2014–December 2018) | 5-fold cross validation, AUC = 0.93 hold-out validation test, AUC ranges from 0.90 to 0.95 |
| Prenatal | |||||
| Bassil and Dripps (1989) | Interpolation at the comb filter output stage, peak selection algorithm | Facilitate safe long-term patient monitoring and reduce erroneous estimates during periods of now signal-to-noise ratio | Fetal heart rate | Phonocardiographic signals | N/A |
| Hernando et al. (1996) | Causal probabilistic network | Describes the integration of qualitative and quantitative reasoning modules within the DIABNET advisory system | CDSS | 9 GDM patients, blood glucose samples—52 cases for review | 82.8% of cases correctly identified |
| Nagy et al. (1997) | Rule-based (static and dynamic knowledge base) | To automatically interpret serological test results of toxoplasma infection | Fetal health | Retrospective study group of 1000 pregnant women | Latent infections correctly classified = 99.10% |
| Alonso-Betanzos et al. (1999) | Bayes’ model, discriminant analysis, ANNs and the Shortliffe and Buchanan uncertainty-based model | Compare developed NST-EXPERT system against other ML methods in prediction of fetal outcome | Fetal health | 3386 cases, including fetal–maternal risk features and early neonatal status parameters | Proposed model is less flexible than ANN method but does not depend on expert input |
| Meinecke et al. (2002) | ICA, BSS | Propose resampling methods to tackle this question and illustrate their usefulness for blind-source separation (BSS) | Fetal health | 2500 points sampled at 500 Hz with eight electrodes located on abdomen and thorax of a pregnant woman | JADE is able to separate the heartbeat of the fetus from the heartbeat of the mother |
| Polak et al. (2004) | ANN | To develop novel GDM diagnosis system based on ANN | Maternal diagnosis | Epidemiological database obtained from National Center for Health Statistics (NCHS), Center for Disease Control and Prevention (CDC) | 70% = true positive diagnoses |
| Kagan et al. (2008) | Likelihood ratio, multiples of the median, regression analysis | To examine the performance of first-trimester screening for trisomies 21, 18 and 13 | Chromosomal abnormality | Singleton pregnancies (at 11+0–13+6 weeks), including 56 376 normal cases, 395 with trisomy 21, 122 with trisomy 18 and 61 with trisomy 13 | Overall FPR was 3.1% and the DRs of trisomies 21, 18 and 13 were 91, 97 and 94%, respectively |
| Etikan and Çaglar (2005) | Stepwise linear regression model, neural network with MLPs | To determine more accurate prediction method between linear and non-linear methods for prediction of babies’ birth weight among maternal demographic characteristics | Birth weight | 300 pregnant women | LR R2 = 59.8% Non-LR R2 = 59.8% |
| Mantini et al. (2005) | ICA | To describe an automatic method that restores the fetal cardiac trace from fMCG recordings | Fetal heart function | Multichannel fMCG datasets of 66 healthy and 4 arrhythmic fetuses | Validation performed on healthy fetuses |
| Assaleh (2007) | Fuzzy logic, neural network, ANFIS | Investigate the use of ANFIS for fetal electrocardiogram extraction from two ECG signals recorded at the thoracic and abdominal areas of the mother’s skin | Fetal health | Synthetic ECG data and 1 case of real ECG data | Performed well to suppress maternal components from fetal signal |
| Comani et al. (2007) | ICA, approximate entropy (ApEn) and sample entropy (SampEn) | Discusses a novel automated system based on entropy estimators for the classification of independent components (ICs) | Fetal heart function | 40 fMCG datasets of normal fetuses with the gestational age ranging from 22 to 37 weeks | ApEn = detection rate of 98.75% SampEn = detection rate of 97.92% |
| Karvounis et al. (2007) | Time–frequency (T–F) analysis, complex wavelets and matching theory techniques, heuristic algorithm, histogram-based technique | Introduces an automated methodology for the extraction of fetal heart rate (FHR) from cutaneous potential abdominal electrocardiogram (abdECG) recordings | Fetal heart function | 8 short and 10 long-duration abdECG recordings, obtained between the 20th and the 41st week of gestation | Accuracy = 97.47% |
| Singh et al. (2007) | Data management resources, comparative bioinformatics | Conceptualize a system that can help address the new challenges posed by the translational science of birth defects research | Birth defects | Mouse model | N/A |
| Mosaliganti et al. (2007) | Surface pocket modeling | Propose a technique for detecting pockets on a surface-of-interest | Placenta functioning | Case study of genetically modified mouse placenta | Sensitivity = 0.84 Specificity = 0.90 |
| Yu et al. (2009) | Support vector regression (SVR), fuzzy logic, non-dominated sorting genetic algorithm (NSGA) | A novel method based on the SVR is proposed to improve the weight estimation accuracy for fetuses of less than 2500 g | Fetal weight and low birth weight | Records of 386 fetuses with ABW less than 2500 g (Shanghai First Maternity and Infant Health Hospital, China) | Proposed model produces significant improvement (1.9%–4.2%) on the accuracy of fetal weight estimation over several widely used formulas |
| Evans and Cuckle (2011) | Multiples of the gestation-specific median (MoMs) | Develop a method to allow for differences in quality among ultrasound nuchal translucency providers or laboratories, in order to improve performance | Chromosomal abnormality | 7237 women (median age of 36 at delivery), who had first trimester screening, including 32 cases of Down syndrome | Performance demonstrated in 5 theoretical examples |
| Marttala et al. (2011) | Multiples of medians | To examine the performance of first-trimester combined screening after adding the specific algorithms for trisomies 18 and 13 in the Down syndrome screening program for chromosomal abnormalities other than trisomy 21 and to determine the outcomes of such pregnancies | Chromosomal abnormality | Pregnant women (n = 56 076), first-trimester combined Down syndrome screening in Northern and Eastern Finland (1 June 2002–31 December 2008) | Adding a T13 algorithm DR improved from 36.4 to 54.5%, with an increase of FPR from 4.3 to 4.5%. T18 algorithm improved the DR from 55.6 to 74% with the same increase of FPR of 0.2% |
| Tejera et al. (2011) | ANN | A model construction for classification of women with normal, hypertensive and preeclamptic pregnancy in different gestational ages using maternal heart rate variability (HRV) indexes | Hypertensive disorders | 568 ECG records | Sensitivity for preeclampsia around 80%, specificity = 85–90% |
| Boisvert et al. (2012) | Bayesian classification | To identify, using capillary electrophoresis and chemometrics, early biomarkers in human amniotic fluid of large-for-gestational-age (LGA) infants | Birth weight | 109 mother–infant pairs, pregnant women undergoing routine age-related amniocentesis between 12 and 20 gestational weeks at St Mary’s Hospital Center in Montreal, QC, Canada | LGA (n = 23) was differentiated from appropriate for GA (n = 86) with a sensitivity of 100% and a specificity of 98% |
| Gebeh et al. (2012) | geNorm, Normfinder | To evaluate the stability of 12 reference genes and suggest those that are stable for use as internal control genes in fallopian tubes and endometrium from ectopic pregnancy and healthy non-pregnant controls | Ectopic pregnancy | Fallopian tubes and endometrial biopsies were obtained from a total of 12 volunteers | Ranked top 6 by geNorm and Normfinder: UBC, GAPDH, CYC1 and EIF4A2 (fallopian tubes) and UBC and ATP5B (endometrium) |
| Ocak (2013) | SVM, genetic algorithm | To evaluate fetal well-being from the CTG recordings using ML methods | Fetal health | 1831 CTG recordings from the UCI Machine Learning Repository (1655 normal fetal state, 176 pathological state) | Predict fetal state as normal, accuracy = 99.3%, or pathological, accuracy = 100% |
| Yeo and Romero (2013) | Spatiotemporal image correlation, ‘intelligent navigation’ technology | To explore visualization of standard fetal echocardiography views from volume datasets obtained with spatiotemporal image correlation (STIC) | Fetal health | Tested on 50 STIC volume datasets, echocardiography | A combination of diagnostic planes and/or VIS-Assistance® in 98–100% in normal cases |
| Haghpanahi and Borkholder (2014) | QRS annotation, Gaussian model selection, Kalman filtering | Describe an algorithm to automatically locate QRS complexes in non-invasive fetal ECG signals | Fetal health | Obtained from a set of four electrodes placed on the mother’s abdomen, ECG datasets provided by the PhysioNet/CinC challenge 2013 | SE = 98.22% and PPV = 97.75% |
| Varanini et al. (2014) | ICA, weighted singular value decomposition | Present an efficient unsupervised algorithm for fetal QRS complex detection from abdominal multichannel signal recordings combining ICA and maternal ECG cancelling | Fetal health | 447 records extracted from five abdominal signal collections acquired, fECG datasets provided by the PhysioNet/CinC challenge 2013 | Subset of 69 records, SE = 99.4% and PPV = 99.2% |
| Sanderson et al. (2014) | Virtual organ computer-aided analysis (VOCAL), sub-noise gain (SNG) | Asses the intra-observer and inter-observer repeatability of selecting the SNG level when acquiring placental volumes with 3D power Doppler for analysis using VOCAL | Tissue perfusion | 240 static 3D volumes from 60 women with uncomplicated singleton pregnancies (20–38 weeks of gestation) | SNG exhibited excellent intra-observer and inter-observer reliability |
| Chu et al. (2014) | Non-invasive prenatal tests, whole genome sequencing | To explore the lower limits of microdeletion size detection via non-invasive prenatal tests using minimally invasive karyotyping (MINK) and introduce/evaluate the GC Content Random Effect Model (GCREM) | Genetic diagnosis | Maternal plasma DNA, amniocentesis at 21 weeks of gestation | The combination of targeted capture and the GCREM algorithm makes it possible to detect relatively small fetal mutations with low sequencing cost |
| Kutarnia and Pederson (2015) | Markov random field (MRF) | Develop an algorithm to produce anatomically correct abdominal ultrasound volumes for use in obstetrics ultrasound simulators | Fetal health | FAST/ER FAN dataset Visible Human Female CT dataset |
A fusion approach to MRF registration can produce accurate displacement fields much faster than standard approaches |
| Re et al. (2015) | LR, VOCAL | To evaluate the potential of VOCAL to estimate fetal thymus volume in normal pregnancies | Fetal health | 3D volume data sets from the axial upper mediastinal section from 37 normal pregnancies (12–35 weeks’ gestation) | Identification of the borders of the thymus and calculation of its volume were successful in 28 patients (77.7%) |
| Lei et al. (2015) | Gaussian mixture model (GMM), Fisher vector (FV) | Propose a method to automatically stage placenta maturity from B-mode ultrasound images based on dense sampling and novel feature descriptors | Placental maturity | 443 placental images | AUC = 96.77%, sensitivity = 98.04%, specificity = 93.75% |
| Nambuerte et al. (2015) | Regression forest, surface parametrization | Propose an automated framework for predicting gestational age (GA) and neurodevelopmental maturation of a fetus based on 3D ultrasound brain image appearance | Gestational age | Two study databases: INTERGROWTH-21st and INTERBIO-21st | Age prediction results strongly correlate with true GA confirming the link between maturational progression and neurosonographic activity observable across gestation |
| Gentillon et al. (2016) | Wavelet-based parameter, histogram-based parameters, Fisher texture analysis in three-dimensional space | To objectively compare the quality of 1.5tesla (1.5T) versus 3T MRI of the developing human brain (Figure 1), in order to determine whether the extra administrative cost is worthy for the patient and the healthcare system | Fetal health | 288 MR images of normal fetal brain were used in the main assessment and 72 MR images of normal fetal brain (gestational age 20–40 weeks) | Both encoding modes are possible with both units, but higher 3T resolution is the main difference |
| Neocleous et al. (2016) | ANN, SVM, k-NN | To examine the potential value of using ML for the non-invasive estimation, at 11–13 weeks of gestation, the risk for euploidy, trisomy 21 (T21) and OCA, from suitable sonographic, biochemical markers and other relevant data | Chromosomal abnormalities | A database of 51 208 singleton pregnancy cases, while undergoing first trimester screening for aneuploidies | ANN system correctly identified all T21 cases 0% false-negative rate (FNR) and 96.1% of euploidies, i.e. 3.9% false-positive rate (FPR) |
| Boland et al. (2017) | ICD-9, ATC, LR, RF, multi-dimensional scaling | To classify these drugs into harmful and safe categories using knowledge gained from chemoinformatics and empirical data | Medication safety | Fetal loss cohort: 14 922 affected and 33 043 unaffected pregnancies Congenital anomalies cohort: 5658 affected and 31 240 unaffected infants |
Out-of-bag accuracy of 91% for fetal loss and 87% for congenital anomalies |
| Neocleous et al. (2017) | ANN | To introduce a non-invasive diagnosis procedure for aneuploidy and to minimize the social and financial cost of prenatal diagnosis tests that are performed for fetal aneuploidies in an early stage of pregnancy | Chromosomal abnormalities | Total of 122 362 euploid and 967 aneuploid cases | 100% detection rate for Trisomy 21 80% DR for Trisomies 13 and 18, Turner and Triploid syndromes |
| Pangalos et al. (2016) | Whole exome sequencing (WES) | Report the development and first applications of an expanded exome sequencing-based test, coupled to a bioinformatics-driven prioritization algorithm, targeting gene disorders presenting with abnormal prenatal ultrasound findings | Genetic abnormalities | 14 euploid fetuses, from 11 on-going pregnancies and 3 products of abortion | Definitive or highly likely diagnosis was made in 6 of 14 cases (43%) |
| Abassi et al. (2017) | ‘footprint of uncertainty’ (FOU), type-2 fuzzy logic system (FLS) classifier, wavelet transform (WT) | To detect sharp wave transients that exist in the latent phase after hypoxia–ischemia (HI) in the electroencephalogram (EEG) in order to determine if these microscale transients are potential biomarkers of HI | Fetal health | EEG recordings of preterm fetal sheep model cohort | Best performing Type-2 FLS classifier occurred when the FOUs were built from Gaussian 2, scale 32 wavelet transformations of the sharp waves for a 1024 Hz sampled EEG. |
| Luo et al. (2017) | Weight SVM, weighted RF, LR | To develop and validate ML models for predicting, before and during pregnancy, women’s risks of bearing children with CHD | Fetal hearth health | Dataset of 33 831 live births, which contained 78 cases of CHD | TPR and TNR of the three classifiers were above 0.65 and 0.93 |
| Fiorentino et al. (2017) | Genome-wide cfDNA analysis | Expanded conventional cfDNA-based non-invasive prenatal testing (NIPT) to cover the entire genome | Chromosomal abnormalities | 12 114 pregnant women (>10 weeks of gestation) undergoing NIPT for common fetal aneuploidy, whole-blood samples (10 ml) | Detection of 12 (7.4%) potentially viable clinically relevant chromosomal abnormalities, which would have remained overlooked if only conventional NIPT had been performed |
| Luo et al. (2017) | BOLD-MRI | Propose to use BOLD-MRI with maternal hyperoxia to quantitatively assess mismatch in placental function in seven monozygotic twin pairs naturally matched for genetic growth potential | Placental function | Twin birth weights were recorded at delivery, with time from the fetal MRI scan to birth ranging from 0.2 to 5.5 weeks | Mean placental TTP negatively correlated with fetal liver and brain volumes at the time of MRI as well as with birth weights. Mean placental TTP positively correlated with placental pathology |
| Abaci Turk et al. (2017) | BOLD-MRI | To present a method for spatiotemporal alignment of in utero MRI time series acquired during maternal hyperoxia for enabling improved quantitative tracking of BOLD signal changes that characterize oxygen transport through the placenta to fetal organs | Placental functioning | Four singletons and six twin pregnancies between 26 and 34 weeks of gestational age | Unexpected temporal signal fluctuations during the first normoxia period were significantly decreased (P < 0.01), volume overlap and distance between region boundaries measures were significantly improved (P < 0.01) |
| Ambroise Grandjean et al. (2018) | Smartplanes® software | To evaluate the feasibility and reproducibility of AI software To automatically identify the transthalamic plane from 3D ultrasound volumes and to measure the biparietal diameter and head circumference in fetus |
Fetal health | Thirty fetuses (evaluated at 17–30 weeks’ gestation), two 3D volumes of fetal head, one conventional 2D image of the transthalamic plane | High intra- and interobserver reproducibility, ICC values >0.98 |
| Caballero-Ruiz et al. (2017) | Expectation–maximization clustering algorithm, C4.5 DT | To improve access to specialized healthcare assistance, to prevent patients from unnecessary displacements, to reduce the evaluation time per patient and to avoid gestational diabetes adverse outcomes | CDSS | 90 patients with GDM at Parc Tauli University Hospital | Time devoted by clinicians to patients’ evaluation was reduced by 27% and face-to-face visits per patient were reduced by 89% |
| Moreira et al. (2018) | ANN, fuzzy logic, ANFIS | Propose the use of a neuro-fuzzy ML technique for predicting the most complex hypertensive disorder in pregnancy called HELLP syndrome | Hypertensive disorder | 205 parturient women diagnosed with a hypertensive disorder during pregnancy | AUC = 0.829 |
| Moreira et al. (2018) | Evolutionary radial basis function network | To identify possible cases of gestational diabetes that can lead to multiple risks for both the pregnant women and the fetus | Maternal diagnosis | National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) dataset (n = 394) | F-measure of 0.786 |
| Peleg et al. (2017) | Computer-interpretable guidelines | To establish a ubiquitous, user-friendly, patient-centered mobile decision support system for patients and for their care providers, based on the continuous application of clinical guidelines and on semantically integrated electronic health records | CDSS | 19 GDM patients used the GDM MobiGuide system in Spain | Achieved high compliance to self-measurement recommendations, while enhancing the satisfaction of patients and care providers |
| Rigla et al. (2018) | Computer-interpretable guidelines | To test the feasibility and acceptance of a mobile decision support system for GDM, developed in the seventh framework program MobiGuide Project | CDSS | 20 patients diagnosed with GDM | High degree of patient satisfaction. Research demonstrates feasibility of this telemedicine application |
| Yang et al. (2018) | cfDNA, NIPT, SVM, RBF | To develop an accurate SVM-based approach and showed its potential in trisomy prediction on chromosomes 13/18/21 | Chromosomal abnormalities | 5518 NIPT data, contains 47 triploid cases | T21: predicted 100%, T18: 99.61%, T13: 99.87% |
| Neocleous et al. (2018) | Feed-forward ANN, cfDNA | To estimate the risk of fetal trisomy 21 (T21) and OCA at 11–13 weeks’ gestation using computational intelligence classification methods | Chromosomal abnormalities | Training set = dataset consisting of 72 054 euploid pregnancies, 295 cases of T21 and 305 cases of OCA Validation = 36 058 euploid, 137 T21 and 133 OCA cases |
T21 SE = 97.1%, specificity = 99.5% |
| Zhang et al. (2018) | Genome-wide association, multi-kernel SVM | To address the gap in our knowledge of gene regulatory elements in the placenta | Placental functioning | Trained a placental enhancer classifier using the 748 known placental enhancers as positives and a random subset of 2000 robust non-placental enhancers as the negatives | Created a map of 33 010 predicted placental enhancers, including 4562 high-confidence enhancer predictions |
| Looney et al. (2018) | Fully CNN (OxNNet) | To fully automate the segmentation of an organ from 3D ultrasound (3D US) volumes, using the placenta as the target organ | Placental functioning | 2393 first trimester 3D-US volumes | AUC = 0.65 |
| Koivu et al. (2018) | SVM, DL, LR | Evaluate ML algorithms to improve performance of first trimester screening of Down syndrome | Chromosomal abnormalities | 3 datasets from three individual clinical studies from routine first trimester screening programs | DNN AUC = 0.96, detection rate = 78% and 1% FPR |
| Moreira et al. (2018a) | ANN, MLP, PSO | The use of a biologically inspired technique, known as PSO, is proposed for reducing the computational cost of the ANN-based method referred to as the MLP, without reducing its precision rate | High-risk pregnancy | 100 parturient women diagnosed with a hypertensive disorder during pregnancy | Proposed method outperformed, on average, other approaches by 26.4% in terms of precision and 14.9% in terms of the true-positive ratio (TPR), and showed a reduction of 35.4% in the FPR |
| Moreira et al. (2018b) | Semantic interoperability, ontologies, ICD-10 | To develop a knowledge-based decision support system that uses ontologies for integrating data related to hypertensive disorders in pregnancy | Pregnancy-induced hypertension | 133 participants diagnosed with a hypertensive disorder during pregnancy (May–September 2017) | Recent state-of-the-art approaches based on openEHR data representation are not sufficient for representing all pregnancy-related data |
| Naimi et al. (2018) | Linear and quantile regression, RF, Bayesian additive regression trees, generalized boosted models | Assess whether ML algorithms can accurately predict estimated fetal weight over the course of gestation using readily available ex utero information and assess the relationship between smoking and fetal/birthweight across gestation | Fetal weight | 18 517 pregnancies (31 948 ultrasound visits) from the Magee-Womens Obstetric Maternal and Infant data and 240 pregnancies in a separate dataset of high-risk pregnancies, Obstetrical Determinants of Neonatal Survival (ODNSR) | Generalized boosted models performed best overall risk of small-for-gestational-age 1.65 fold, using the correct fetal weight standard |
| Hou et al. (2018) | CNN | Present a learning-based image registration method capable of predicting 3D rigid transformations of arbitrarily oriented 2D image slices, with respect to a learned canonical atlas co-ordinate system | Fetal health | Simulated data | Achieves an average spatial prediction error of 7 mm on simulated data and produces qualitatively improved reconstructions for heavily moving fetuses with gestational ages of approximately 20 weeks |
| Ren et al. (2018) | RF, gradient boosting | Investigate the non-linear effects of PM10 exposure during the critical time window, weeks 3–8 in pregnancy, on risk of congenital heart defects (CHD) | Air pollution and fetal health | 39 053 live-born infants in Beijing, from 2009 to 2012 | Both ML models found an association between maternal exposure to ambient PM10 and CHDs in Beijing |
| Pisapia et al. (2018) | Image-based ML | To determine whether extraction of multiple imaging features from fetal MRI and integration using ML techniques can predict which patients require postnatal cerebrospinal fluid (CSF) diversion after birth | Fetal health | 253 patients with fetal ventriculomegaly (2008–2014) | Discovery cohort: correctly classified patients who required CSF diversion with 82% accuracy, 80% sensitivity and 84% specificity Replication cohort: 91% accuracy, 75% sensitivity and 95% specificity |
| Troisi et al. (2018) | Ensemble learning | To perform a characterization of maternal serum in order to build a metabolomic fingerprint resulting from congenital anomalies of the central nervous system | Fetal health | Metabolomic profiles were obtained from serum of 168 mothers (98 controls and 70 cases) | Maternal serum metabolomics is a promising tool for the accurate and sensitive screening of such congenital defects |
| Akbulut et al. (2018) | Averaged perceptron, boosted DT, Bayes point machine, DF, decision jungle, locally deep SVM, LR, neural network, SVM | To help clinicians and families to better predict fetal congenital anomalies besides the traditional pregnancy tests using ML techniques and e-Health applications | Fetal health | Obtained through maternal questionnaire and detailed evaluations from 3 clinicians | Tested on 16 users, accuracy = 87.5% |
| Miao and Miao (2018) | DNN, ensemble learning | Developed model is used to distinguish and classify the presence or absence of multiclass morphologic patterns for outcome predictions of complications during pregnancy | Fetal health | CTG dataset with 2126 clinical instances, from 1980, and 1995–1998 (UCI Machine Learning Repository dataset) | Accuracy = 88.02%, recall = 94.30%, precision = 85.01%, F-score = 0.8508 |
| Vasconcelos et al. (2018) | Deep learning, ResNet101 architecture, SVM | Propose a deep learning method for classification of different surgical actions performed during laser ablation therapy during twin-to-twin transfusion syndrome interventions | Twin-to-twin transfusion syndrome (TTTS) | Videos obtained from five different TTTS ablation procedures | Automatic detection of surgical action in fetoscopic video is feasible |
| De Rámon Fernández et al. (2019) | ANN, MLP, DL, SVM, NB | A CDSS has been developed to help clinicians to choose the initial treatment to be followed by the patient | Ectopic pregnancy | 406 cases of tubal ectopic pregnancies collected at the Department of Obstetrics and Gynecology of the University Hospital ‘Virgen de la Arrixaca’ in the Murcia Region (Spain) (November 2010–September 2015) | SVM and MLP show best performance SVM accuracy = 96.1%, sensitivity = 96%, specificity = 98% |
| Al-Shaer et al. (2019) | Principal component analysis, k-means clustering | To discover signaling pathways and miRNAs that inform mechanisms underlying fetal alcohol spectrum disorder (FASD) | Fetal alcohol spectrum disorder | RNA-seq dataset derived from neural fold-stage chicken embryos that were exposed to pharmacologically relevant alcohol concentration or isotonic saline, followed by a 4.5-hour recovery period. Cranial headfolds were isolated 6 hours following initial exposure | Identified 6857 differentially expressed exons representing 1251 geneIDs Identified exons encoding 23 microRNAs having significantly differential expression profiles in response to alcohol |
| Burton et al. (2019) | Random forest, neural network, Extreme Gradient Boosting | Explored the potential for a MLsolution to reduce the burden of culturing the large number of culture-negative samples without reducing detection of culture-positive samples | Maternal diagnosis | 212 554 urine reports | Workload reduction of 41% and a sensitivity of 95% |
| Corona-Figueroa (2019) | ANFIS. rule-based expert system | Develop a prototype meant to be an auxiliary for the detection of fetal arrhythmias by analyzing the FHR and its variability | Fetal heart health | Set of 5 artificial signals Set of real ECG signals from a group of 9 pregnant women from 8 electrodes at a sample rate of 500 Hz |
Synthetic signal tests, DR = 88.88% |
| Gao et al. (2019) | Observational Medical Outcomes Partnership (OMOP) common data model, ICD, CPT, regularized logistic regression models |
To identify severe maternal morbidity (SMM) during delivery hospitalizations, we introduce a ML framework that incorporates data in EHRs | Maternal morbidity | 45 858 deliveries for obstetric inpatients, from Vanderbilt University Medical Center EHR system (2005–2008) | AUC = 0.94, 85% patients diagnosed with fluid and/or electrolytes disorder experienced SMM during their delivery hospitalization, 82% patients diagnosed with systemic inflammatory response syndrome developed SMM |
| Gomes Filho et al. (2019) | Bayesian networks, rule-based | To present a hybrid model capable of performing the early diagnosis of GDM based on the disease code, analyzing the medical history of pregnant patients | Maternal diagnosis | The database of a health insurance company which covers eleven Brazilian states (January 2004–December 2009) | Prototype demonstrates feasibility |
| Mohseni Salehi et al. (2019) | CNN | To increase the capture range and accelerate the performance of state-of-the-art inter-subject and subject-to-template 3D rigid registration | Fetal brain | 93 reconstructed T2-weighted MRI scans of fetuses, as well as T1- and T2-weighted MRI scans of 40 newborns | Proposed methods provided very fast (real-time) registration with a wide capture range on the space of all plausible 3D rotations and provided good initialization |
| Moriera et al. (2019) | Averaged one-dependence estimators (AODE) algorithm, Bayes’ theorem, ANN, DT | The use of AODE is proposed for real-time pregnancy data analysis from Internet of Things (IoT) devices and gateways | Pregnancy complications | 205 parturient women diagnosed with a hypertensive disorder during pregnancy | AODE algorithm has inferior accuracy performance (versus DT and ANNs), but superior computational time performance |
| Signorini et al. (2020) | ApEn, Lempel Ziv complexity, phase-rectified signal average, robust linear regression, RF, SVM, classification trees, elastic NET, LASSO, NB | Tested the performance of 15 ML techniques in discriminating healthy versus IUGR fetuses | Intrauterine growth restriction (IUGR) | CTG traces and prenatal fetal condition from a database of 60 healthy and 60 IUGR fetuses | RFs achieved best performance Mean accuracy for all 10 tests = 0.911 |
| Lu et al. (2020) | Ensemble model, random forest, XGBoost, LightGBM, genetic algorithm | To predict fetal weight at varying gestational age in the absence of ultrasound examination within a certain accuracy | Fetal weight | 4212 intrapartum recordings | Ensemble model: accuracy = 64.3%, mean relative error = 7.0% |
| Preterm | |||||
| Grignolio (1982) | Multiple regression | Predict probability of being alive at 30 days of life for premature newborns weighing less than 2000 g | Neonate mortality | Weight of 92 preterm neonates | 80% accuracy on prediction |
| Woolery (1994) | Multiple regression analysis, rule-based (ID3 algorithm) | Develop clinical knowledge base for preterm birth risk assessment | Preterm risk | 2739/~16 000 cases from a database of high-risk pregnancy women referred for home uterine monitoring services | Overall, experts determined rules did not provide enough information, missing important data |
| Wu et al. (2004) | Adaptive speckle suppression using variable length sticks algorithm, region-based segmentation, curve-fitting function | Develop an algorithm that is able to identify the anatomic landmarks of the cervix on a transvaginal ultrasound image and determine the standard cervical length | Cervical length | 101 cervical ultrasound images were selected from a series of 37 examinations performed on 17 patients over an 8-month period | Pairwise comparison, the mean cervical length for the computer method matches with the mean manual cervical length |
| Alamedine et al. (2013) | Jeffrey divergence (JD) distance, a sequential forward selection (SFS) and a binary PSO (BPSO), quadratic discriminant analysis (QDA), k-NN, LDA | To reduce the number of features from EHG signals by selecting only the relevant ones which are useful for solving the classification problem | Fetal health | Signals recorded on 48 women: 32 during pregnancy (33–39 weeks of gestation) and 16 during labor (39–42 weeks of gestation) | Feature selected by BPSO with QDA corresponds to the highest percentage of correct classification (88.72%) |
| Fergus et al. (2013) | Synthetic minority oversampling technique (SMOTE), density-based classifiers, linear- and polynomial-based classifiers, non-linear-based classifiers | Presents a supervised ML approach that classifies term and preterm records | Fetal health | Open-source dataset containing 300 records (38 preterm and 262 term). | 96% sensitivity, 90% specificity and a 95% area under the curve value with 8% global error using the polynomial classifier |
| Góralska et al. (2013) | CHAID classification tree | To prove that precise information about the proper course of action that is included in the expanded Apgar score might have a prognostic value for the early death incidence in preterm newborns | Fetal health | 276 children (born from <32 weeks of gestational age pregnancies) at the 2nd Department of Obstetrics and Gynecology, who were hospitalized between the years 2009 and 2011at the Neonatology and Intensive Care Unit, Medical University of Warsaw |
Concentration of oxygen used during resuscitation at birth (a component of the expanded Apgar score) has significantly more prognostic value |
| Cerqueira et al. (2014) | ANN, SVM, cost-sensitive algorithm | Describes NICeSim, an open-source simulator that uses ML techniques to aid health professionals to better understand the treatment and prognosis of premature newborns | Fetal health | Data collected in the Neonatal Intensive Care Unit of São Sebastião Hospital, at Viçosa, Minas Gerais State, Brazil, (2008–2010), 293 instances | Accuracy = 86.7% |
| Sadi-Ahmed et al. (2017) | Huang-Hilbert transform, intrinsic mode function, SVM | To achieve a fully automated method for predicting preterm deliveries only basing on EHG signal analysis | Preterm birth prediction | 30 pregnant women (1997–2005), 15 of which delivered prematurely, EHG records (27–32 weeks of gestation), 1 record per patient | Two-channel combination achieved the best mean results with accuracy = 95.70%, sensitivity = 98.40%, specificity = 93.00%, AUC = 0.95. |
| Bahado-Singh et al. (2019) | DL, RF, SVM, LDA, GLM, prediction analysis for microarrays | To evaluate the application of AI to amniotic fluid metabolomics and proteomics, alone and in combination with sonographic, clinical and demographic factors, in the prediction of perinatal outcome in asymptomatic pregnant women with short cervical length | Preterm birth prediction | 32 cases, Early preterm (<34 weeks), control (≥34 weeks) | DL showed best performance, AUC = 0.890 for delivery <34 weeks’ gestation, 0.890 for delivery <28 days post-amniocentesis and 0.792 for NICU admission |
| Lee and Ahn (2019) | ANN, DT, NB, RF, SVM, multinomial LR | Analyze preterm birth and its determinants based on general hospital data and compare ANN to other ML methods | Preterm birth preventive measures | 596 obstetric patients during 27 March 2014–21August 2018 at Anam Hospital in Seoul, Korea | Accuracy of ANN comparable to LR and RF Determinants = BMI, hypertension, DM, prior cone biopsy, prior placenta previa, parity, cervical length, age, prior preterm birth, and myomas and adenomyosis |
| Torres Torres et al. (2019) | SVM, CNN | Present a novel method for postnatal gestational age estimation that eliminated the subjectivity issues present in the Ballard Score | Postnatal gestational age prediction | The GestATional Dataset (2015–2017), 130 babies’ images of foot, ear and face | Expected error of 6 days and a 30% improvement over prediction based on weight only |
| Gao et al. (2019) | DL, recurrent neural networks (RNN) | Investigated the extent to which DL models that consider temporal relations documented in EHRs can predict extreme preterm birth (EPB) | Preterm birth prediction | EHR data from 5689 deliveries at Vanderbilt University Medical Center (9 August 2005–31 July 2017) | RNN ensemble model: AUC = 0.82, sensitivity = 0.96 |
| Shi et al. (2019) | Genetic algorithm | To measure the anisotropic mechanical properties of human cervical tissue using indentation and video extensometry | Cervix tissue properties | Material properties of human cervical slices taken at different anatomical locations from 7 women of different obstetric backgrounds | The anatomic anterior and posterior quadrants of cervical tissue are more anisotropic than the left and right quadrants. There is no significant difference in material properties between samples of different parities |
| Perinatal, birth and delivery | |||||
| Hernández et al. (1986) | Syntactic pattern recognition combined with Hon’s Apgar prediction method | To overcome communication of automatic pattern recognition to obstetric professionals with a topogram | FHR and prognosis with Apgar prediction | Uterine pressure via intrauterine catheters FHR via subcutaneous electrodes Tested on 69 patients |
95 ± 1% success at predicting Apgar rating at birth |
| Anderson and Barclay (1988) | Date conversion and averages | Allow clinician to input up to 20 clinical data points and determine average estimated day of delivery | Estimated date of delivery | Not validated | N/A |
| Sokol and Chik (1998) | Text processing utilities from UNIX, coded into PROLOG compatible files | Expert system for perinatal knowledge | Clinical knowledge system | Prototype system | N/A |
| Alonso-Betanzos et al. (1991) | Mixed frame- and rule-based approach for clinical knowledge representation | Help clinical professionals interpret: biophysical profile, contraction stress test and non-stress test. It also interprets supervision of labor and newborn diagnosis | Fetal health | 87 cases randomly selected from Ob–Gyn Dept. of the Hospital General de Galicia, Spain | Retrospective and prospective validation—similar performance to expert systems of the time |
| Keith et al. (1994) | ANN | Evaluate an intelligent system to assist clinicians in their assessment of fetal condition and management of labor by expert and system agreement | Fetal health | Intrapartum CTG and patient information 100 training set, 30 test set | System achieved good agreement with 3 experts |
| Beksaç et al. (1995) | Supervised ANN (back propagation learning algorithm) | Development of an AI diagnostic system for the interpretation of umbilical artery blood flow velocity waveform measurements | Fetal health | Training set: 952 umbilical artery blood flow velocity waveform images of 174 normal pregnancies Testing set: 138 images derived from 20 normal pregnancies, 68 images of 16 high risk pregnancies |
Specificity = 98.6% Sensitivity = 51.5% |
| Beksaç et al. (1996) | Generalized learning vector quantization (GLVQ) algorithm | To develop an automated intelligent diagnostic system for the interpretation of umbilical artery velocity waveforms | Fetal health | Training set: 278 and 380 waveform images of 94 normal and 157 high risk pregnancies Testing set: 193 normal pregnancy and 61 high-risk pregnancy waveform images |
Specificity = 80.3% Sensitivity = 54.1% |
| Devoe et al. (1996) | Neural network (three-layered, feed-forward with a back propagation) | To create a neural network that predicts the length of the first stage of term labor | Labor management | 159 for training and 41 for testing | 36 of 41 first-stage durations were predicted within 2 hours of actual length |
| Ungureanu et al. (2007) | Maternal beat subtraction with linear modeling, noise cancelling methods, | Propose a new method to subtract mECG after detecting and removing abdominal signal segments with high-amplitude variations due to uterine contractions | Fetal health | Signals were recorded at a sampling rate of 400 Hz, using unipolar measurement and 12 electrodes were placed on the abdomen Fetal ECG was also acquired using fetal scalp electrodes at a sampling rate of 1024 Hz |
Comparable performance to methods of the time |
| La Rosa et al. (2008) | Schwarz information criterion (SIC), non-supervised k-means cluster algorithm | Propose a single-channel two-stage time-segment discriminator of uterine magnetomyogram (MMG) contractions during pregnancy | Fetal health | MMG records obtained from 10 patients admitted to the hospital for contractions (31–40 weeks of gestation) | Detection rate and false alarm rate are favorable |
| Terrien et al. (2008) | Time-frequency representation, gradient vector flow | Describe a new ridge extraction method based on the image processing technique of active contours or snakes | Fetal health | Testing: two pregnant monkeys by the implantation of a telemetric transducer | Application on real EHG: able to obtain 63 contractions per placental location for a total of 126 contractions and identified a total of 52 polyphasic contractions |
| Yilmaz and Kilikçier (2013) | Least-squares SVM, PSO, binary DT | To classify CTG data to determine the fetal state as normal, suspect or pathologic | Fetal health | CTG data set = 2126 data points, with 21 features, taken from the UCI Machine Learning Repository | Accuracy = 91.62% |
| Liu et al. (2013) | Genetic algorithm | To identify novel serological protein markers to diagnose preeclampsia (PE) with a multi ‘omics’-based discovery approach | Maternal diagnosis | n = 111 PE and n = 152 control placenta samples | Developed two optimal biomarker panels for early and late onset PE assessment |
| Ge et al. (2014) | Spatial-color pixel classification, maximizing cluster validity index, k-NN | Describes a system for automated counting and distinguishing fetal and maternal RBCs on clinical KB slides | Fetal–maternal hemorrhage (FMH) | 120 raw color images of KB slides | Capable of completing the counting of over 60 000 cells (versus ∼2000 by technologists) within 5 minutes (versus∼15 minutes by technologists) |
| Sahin and Subasi (2015) | SVM, ANN, radial basis functions, DTs, k-NN, RF | To evaluate the classification performances of eight different ML methods on the antepartum cardiotocogram (CTG) data | Fetal health | UCI CTG dataset with 1831 instances, each containing 21 features (8 continuous, 13 discrete) | RF can be accepted as a good classifier of normal and pathological classes of the CTG data accuracy = 99.18% |
| Czabanski et al. (2016) | Fuzzy inference-based learning, Lagrangian SVM | Present a method of retrospective fetal state assessment using the results of the fuzzy analysis of delivery outcome attributes | Fetal health | CTG recordings from 1-hour fetal monitoring sessions via an external pulsed Doppler ultrasound transducer | Fuzzy reasoning improved the efficiency of the LSVM classification when compared with the standard learning |
| Chen and Hao (2017) | Extreme learning machine, single-hidden layer feedforward neural network, Hilbert–Huang transform | Present a method for feature extraction and classification of EHG between pregnancy and labor group | Labor classification | 122 EHG recordings (112 pregnancy recordings and 10 labor recordings) made on 45 pregnant women | Accuracy = 88.00%, sensitivity = 91.30%, specificity = 85.19% |
| Alberola-Rubio et al. (2017) | SVM, majority voting | To help distinguish patients that will achieve labor spontaneously from those that will need late-term induction of labor | Route of delivery | EHG recordings from 62 singleton term pregnancies, 38 spontaneously entered labor and 24 induced | Aggregation of majority voting of SVM models using contextualized EHG parameters: AUC = 0.93 |
| Fergus et al. (2017) | DL, RF, recursive feature eliminator algorithm, SMOTE, Fishers LDA | Present a proof-of-concept using ML and FHR signals as an ambulatory decision support to antenatal care | Route of delivery | 506 normal vaginal deliveries and 46 cases of cesarean section, CTG recordings for singleton pregnancies, gestational age <36 weeks (CTU-UHB database) | DL classifier, sensitivity = 94%, specificity = 91%, AUC = 99%, F-score = 100%, and MSE = 1% |
| Beksac et al. (2018) | ANN | To develop a supportive computerized prediction system for the route of delivery | Route of delivery | 2127, 3548 and 1723 deliveries for the years 1976, 1986 and 1996 | Specificity = 97.5%, Sensitivity. = 60.9%, FPR = 2.5%, FNR – 39.1%, PPV = 81.8%, NPV = 93.1% |
| Fergus et al. (2018) | Synthetic minority oversampling, Fishers LDA (FDLA), RF, SVM | To determine whether ML could be used to optimize the decisions made by obstetricians and midwives, in the presence of FHR traces, linked to caesarean section and normal vaginal deliveries | Route of delivery | 552 records from the CTU-UHB database | Ensemble classifier: sensitivity = 87%, Specificity = 80%, AUC = 96%, MSE = 8% |
| Postnatal and postpartum | |||||
| Green et al. (2019b) | mHealth. NLP, Tess AI, DT | To test the Healthy Moms perinatal depression intervention using a single-case experimental design with pregnant women and new mothers recruited from public hospitals outside of Nairobi, Kenya | Perinatal depression | Initial prepilot round of formative testing with 10 women from a private maternity hospital in May and June | Prototype followed up with more research |
| Wang et al. (2019) | L2-regularized LR, SVM, DT, NB, XGBoost, RF | To demonstrate that ML models can be used to predict PPD and to carefully evaluate the risk factors identified from EHR data | Postpartum depression | 9980 episodes of pregnancy (EHRs from Weill Cornell Medicine and New York-Presbyterian Hospital between 2015 and 2017) | SVM: AUC = 0.79, Significant predictors = race, obesity, anxiety, depression, different types of pain, antidepressants and anti-inflammatory drugs during pregnancy |
| Any stage | |||||
| Prieto et al. (2014) | SVMs, NB, DT, k-NN | Exploit the wealth of user-generated data, available through the microblogging service Twitter, to estimate and track the incidence of health conditions in society | Social media | More than 10 million tweets, Spanish and Portuguese | Correlation-based feature selection proved to be the most effective |
| Yom-Tov et al. (2015) | ICD-10, linear SVM, the Self-Controlled Case Series method | Report that Web search engine queries coupled with information on Wikipedia access patterns can be used to infer health events associated with an individual user and automatically generate Web-based risk markers for some of the common medical conditions worldwide (including pregnancy) | Internet usage | English language queries submitted to the Bing search engine by users in the United States for the 6-month period starting May 2012, zip code of user and small proportion of users provided year of birth | Most common medical condition identified was pregnancy |
| Zhang and Demner-Fushman (2017) | SVM, NLP | To develop automated classification methods for eligibility criteria in ClinicalTrials.gov to facilitate patient-trial matching for specific populations such as persons living with HIV or pregnant women | Clinical trials | 891 interventional cancer trials and the eligibility criteria for 1570 of the most recent interventional trials from ClinicalTrials.gov for HIV-positive and pregnancy eligibility | Achieved macro-averaged F2 scores of 0.91 and 0.85 for HIV and pregnancy, relatively |
| Klein et al. (2018) | NLP, rule-based, boot-strapping | To assess whether rare health-related events (birth defects) are reported on social media, to design an NLP approach for collecting data from social media and to utilize the collected data to discover a cohort of women whose pregnancies with birth defect outcomes could be observed for epidemiological analysis | Social media | Mined 432 million tweets posted by 112 647 users who were automatically detected via their public announcements of pregnancies on Twitter | Discovery of 195 users that met the inclusion criteria Recall = 0.95 |
Figure 3 .
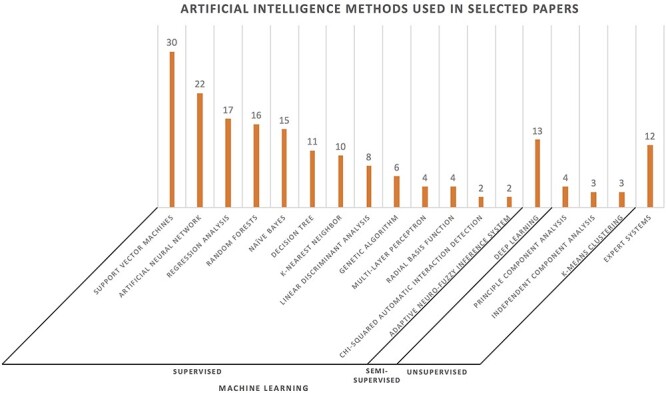
AI methods used in studies included in review. ML methods are ordered by frequency and further categorized by supervised and unsupervised learning methods. Totals here do not equal the number of included papers, as studies often demonstrate several methods.
Table 2.
ML methods and their applications to the pregnancy domain
| ML techniques | Application to pregnancy | |||
|---|---|---|---|---|
| Method | Description of method | Additional references for more details on method | Pregnancy area most used | Informatics domain |
| Supervised | ||||
| SVM | Constructs a hyperplane or set of hyperplanes; finds the decision boundary for classification. | [155] | • ART | • Prediction and assessment |
| • Preterm birth | • Chromosomal anomalies | |||
| • Prenatal | • CDSS | |||
| • Perinatal, labor and delivery | • Electronic monitoring | |||
| • Postpartum | • NLP and search analytics | |||
| ANN | Composed of nodes or states that are connected to a second set of nodes via functions; contains an input layer, at least one hidden layer and an output layer | [156] | • ART | • Prediction and assessment |
| • Prenatal | • Chromosomal anomalies | |||
| • Preterm birth | • CDSS | |||
| • Perinatal, labor and delivery | • mHealth | |||
| • Electronic monitoring | ||||
| MLP | A class of feedforward ANN. | [157] | • ART | • Prediction and assessment |
| • Prenatal | • CDSS | |||
| Radial basis function (RBF) network | A type of ANN that performs classification by measuring the input’s similarity to examples from the training set | [158] | • Perinatal, labor and delivery | • Prediction and assessment |
| • Chromosomal anomalies | ||||
| RF | A classification method that contains multiple decision trees | [159] | • Preconception | • Prediction and assessment |
| • Prenatal | • CDSS | |||
| • Preterm birth | • Radiology, Imaging | |||
| • Postpartum | • NLP and search analytics | |||
| NB | A family of algorithms based on Bayes’ theorem with an assumption of independence between predictors | [160] | • Preconception | • Prediction and assessment |
| • ART | • CDSS | |||
| • Prenatal | • mHealth | |||
| • Postpartum | • NLP and search analytics | |||
| k-NN | An algorithm that classifies new cases based on a similarity measure | [161] | • Art | • Chromosomal anomalies |
| • Perinatal, labor and delivery | • Electronic monitoring | |||
| Discriminant analysis | A method that finds a set of prediction equations based on independent variables that are used to classify individuals into groups | [162] | • Preterm birth | • Prediction and assessment |
| • Perinatal, labor and delivery | • Genetics and biomarkers | |||
| Genetic algorithm (GA) | An algorithm that imitates the process of natural selection | [163] | • Art | • Prediction and assessment |
| • Prenatal screening | • Genetics and biomarkers | |||
| • Preterm birth | ||||
| • Perinatal, labor and delivery | ||||
| Semi-supervised | ||||
| DL | Constructs of ANN using a large number hidden layers | [164] | • Art | • Prediction and assessment |
| • Prenatal | • Radiology, Imaging | |||
| • Preterm | ||||
| • Perinatal, labor and delivery | ||||
| Unsupervised | ||||
| Principle component analysis | A dimensionality reduction method for large datasets, often used before the ML algorithm. It attempts to find uncorrelated components | [165] | • Art | • Electronic monitoring |
| • Prenatal | • Genetics and biomarkers | |||
| • Perinatal care, labor and delivery | ||||
| Independent component analysis | A technique for decomposing a complex dataset into independent components | [166] | • Prenatal | • Electronic monitoring |
| • Perinatal care, labor and delivery | ||||
| k-means clustering | A clustering method that partitions data into a specified number of K clusters | [167] | • Prenatal | • Genetics and biomarkers |
| • Perinatal, labor and delivery | • Electronic monitoring | |||
Pregnancy care spans across several disciplines, some of which overlap: electronic monitoring, radiology and imaging, mHealth, CDSS, NLP and search analytics, genetic and chromosomal abnormalities, pregnancy complications, labor and delivery, and postpartum care. Electronic monitoring was the most common with 27 studies (Figure 4). Radiology and CDSS were also popular areas for using AI methods. Informatics areas that are only beginning to utilize AI methods for pregnancy-related care include mHealth (n = 9), chromosomal anomaly detection (n = 7) and NLP (n = 3).
Figure 4 .
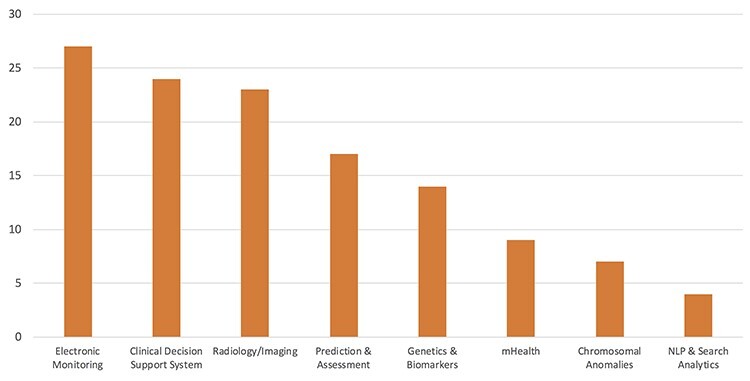
Informatics areas utilized by included studies. Because a study may utilize multiple domains (e.g. NLP + Radiology), there may be overlap across domains for a given study. For example, mHealth applications overlap multiple domains.
Discussion
Mobile health
Development of provider-facing and direct-to-consumer mHealth applications supports preconception [26], gestational disease management [27], remote health monitoring [28], low-resource prenatal care [29–31], text messaging [32–34], patient education [32, 35], fetal health status prediction [36], preeclampsia prediction [37] and perinatal depression [34]. A 2019 systematic review determined mHealth applications with promising potential for use by healthcare workers during antenatal care [25]: Babyscripts [32], OpenSRP [29], PANDA [28], PotM [37], mHealth Guatemala [30], Expect With Me [35], mPAMANECH [31] and COMMCARE [38]. A CDSS with mobile patient support predicts normal, pathological and potentially pathological fetal health status; significant features found include fetal age, maternal age, blood serotype, delivery number and illnesses regarding the current pregnancy [36]. Together, boosted decision tree (DT), decision forest (DF) and decision jungle were found to be the most efficient.
Direct-to-consumer mHealth applications have potential to increase engagement and empower pregnant people in their healthcare. Three studies arose, focusing on predicting the fertility window [26], text mining to understand communications with a sexual and reproductive health information service [33] and a mHealth text messaging system for perinatal depression [34]. It should be noted that in these studies the authors declare financial conflict of interest. A text mining approach was developed using naïve Bayes (NB) and basic NLP techniques, to understand how Kenyan men and women communicated with askNivi, a free sexual and reproductive health information service [33]. The users wrote most often about family planning methods, contraception, side effects, pregnancy, menstruation and sex. A majority of users sought factual information, followed by requests for advice and reporting symptoms. A prototype mHealth text messaging system for perinatal depression, Tess, was tested with mothers recruited from public hospitals outside of Nairobi, Kenya [34]. Prediction of a woman’s fertile window through data received by a wearable bracelet achieved 90% accuracy using a random forest (RF) classifier [26]. A prospective longitudinal study determined what phase-based differences a wearable bracelet could detect in users’ wrist skin temperature, heart rate, heart rate variability, respiratory rate and skin perfusion [26].
Applications address the needs of the pregnant person, support clinical care and often aim to limit in-person visits without compromising quality of care. Post the COVID-19 lockdown, development and application of mHealth and telehealth for pregnancy care, especially for pregnancy with comorbidities [39, 40], will be needed to provide adequate care while reducing exposure during prenatal care.
NLP and search analytics
A wealth of data is accessible through social media, including health behaviors and health outcomes. NLP techniques were applied to user-generated Twitter data to estimate and track the incidence of pregnancy [41] and collect data on birth defect outcomes [42]. Support vector machine (SVM) was used to infer health events associated with individual users and found pregnancy to be the most commonly identified medical condition [43]. NLP techniques and SVM were applied to automatically classify eligibility criteria in ClinicalTrials.gov to facilitate patient-trial matching [44]. A great tool for public health and pharmacovigilance, NLP can analyze unstructured health data, improve EHR usability, and facilitate interoperability.
Assisted reproductive technology
AI assessment of embryo images or videos has great potential to improve ART outcomes. Applications guide identification of embryos from the culture medium during early human in vitro development [45], raw time-lapse videos/images of embryos [46–48] and in vitro fertilization (IVF) EHR data [49, 50]. Evaluation of morphokinetic time-lapse microscopy data depends on the experience and knowledge of embryologists—this work is highly subjective with a lack of standardization. Applications may reveal details of embryo morphology imperceptible to the human eye or predict successful pregnancy by integrating other relevant health data points. DL can determine robust quantitative imaging biomarkers for embryo selection, improve therapy outcomes and reduce clinical burden.
Assisted Reproductive Technology CDSS
A convolutional neural network (CNN) was implemented to select highest quality embryos using a large collection of human embryo time-lapse images from a high-volume fertility center in the United States [48]. This 22-layer deep model resulted in the trained algorithm called STORK. STORK performed well on additional datasets of embryo images from two other IVF centers. Different grading systems (i.e. unstandardized) across clinics affect performance; STORK demonstrated lower performance for one clinic dataset and therefore lower generalizability. For embryo selection, STORK outperformed individual embryologists in assessing embryo image quality. However, STORK could not predict positive and negative live births using embryo morphology alone.
Medical imaging in pregnancy
Fetal development
Applications of AI have targeted fetal development: predicting fetal health status [36], improving fetal brain imaging [51–53] and other fetal anatomy [54, 55]. Semi-automated learning-based framework approach reported to improve gestational age prediction, with accuracy of ±6.1 days, using DF on structural brain image and clinical data [56]. AI has been applied to improve knowledge and treatment of ectopic pregnancy, using ML classifiers [57] and using gene stability algorithms [58]. Studies aim to improve imaging of fetal organ development with virtual organ computer-aided analysis (VOCAL) [55], texture analysis [52] and CNN [53, 59]. Three studies observe EHR data; higher performing classification ML approaches used in these studies include DF [36, 56] and SVM [57].
Placental functioning
Placental health is deeply connected with maternal–fetal health and plays an essential role in supporting fetal development [60]. Placental function and characteristics have been observed with VOCAL with 3D power Doppler, blood oxygen level-dependent magnetic resonance imaging (BOLD-MRI) [61, 62], ultrasound images [63] and CNN [64]. Research focuses on improving placental pathology and sufficiency knowledge [62], placental volume imaging methods [61, 65] and placental maturity identification [63]. BOLD-MRI has gained attention as a promising non-invasive technique to monitor placental function in vivo; however, the use in practice is limited.
Diagnostic imaging CDSS
The prenatal diagnosis rate of major congenital heart defects remains low most likely due to the downfalls of manual navigation during sonographic screening, as it is operator-dependent, challenging and time-consuming. The Fetal Intelligent Navigation Echocardiography (FINE) method provides visualization of standard fetal electrocardiogram (fECG) views from volume datasets obtained with spatiotemporal image correlation, aiming to consistently display diagnostic planes, regardless of fetal position or initial orientation [54]. The Virtual Intelligent Sonographer Assistant tool was developed to visualize specific structures in the complex anatomy of the fetal heart. When applied to four abnormal cases, the FINE method demonstrated evidence of abnormal fetal cardiac anatomy in multiple fECG views.
Genetic screening and chromosomal abnormalities
Definitive prenatal diagnosis of genetic disease is performed via invasive procedures, specifically amniocentesis or chorionic villus sampling. Risks include miscarriage, fetal morbidity, parental anxiety and Rh sensitization [66]. Non-invasive prenatal tests (NIPTs) hold no such risks and usually tests only for trisomy 21 (T21). Trisomies 18 (T18) and 13 (T13) are the second and third most common trisomies after T21. Expansion of NIPT could include screening for T18 and T13 [67, 68] and other chromosomal abnormalities (OCA) [69, 70]. A number of ML techniques were applied to improve chromosomal screening, including artificial neural network (ANN) [69, 70]; SVM [70, 71]; k-nearest neighbor [70, 71] and deep NN, RF, NB, DT and logistic regression (LR) [71]. Studies comparing methods found NN methods to perform best [70, 71]. AI methods were applied to optimize detection of relatively small mutations at a low sequencing cost [72]. In order to build a ‘metabolic fingerprint’ resulting from congenital anomalies of the central nervous system, ensemble learning was applied to characterize maternal serum [73].
During pregnancy, the pregnant person and the fetal–placental unit produce cell-free DNA (cfDNA). Using next generation sequencing, a SVM model demonstrated high accuracy for cfDNA testing [74]. Genome-wide cfDNA analysis detected OCA with high sensitivity, in comparison with standard cfDNA screening [75]. A proposed two-stage routine procedure, with combined tests, invasive tests and cfDNA tests, achieved high detection rate for T21 cases and proved to be minimally invasive and of relatively low cost [76].
Chromosomal screening CDSS
Nuchal translucency (NT) measurement, a well-established ultrasonographic marker for fetal aneuploidy screening, can vary greatly and as a result impair screening performance. The performance-adjusted risk (PAR) method allows for these differences in measurements and improves performance [77]. PAR analyzes individual provider and laboratory marker distribution parameters, compares with national expectations and then assigns a handicap. NT and serum markers are considered in the method, using commercially available software and knowledge from meta-analysis of published literature. The PAR method informs providers of their handicap and their performance in relationship to others.
Electronic monitoring
The FHR signal is more complicated to identify than the adult signal, and therefore, there has been an effort to improve methods to detect, sample and quantify the FHR signal accurately. Computer analysis of the FHR is categorized into three stages: (1) raw signal processing, (2) pattern analysis and (3) expert/intelligent systems [23]. Early computer programs only identified deceleration patterns and outcomes of normal, warning or ominous patterns. Studies apply AI methods to ECG [78–84], magnetocardiography (MCG) [85, 86] and cardiotocogram (CTG) [87–90]. In attempt to improve fetal signal extraction from ECG and MCG recordings, several supervised learning methodologies were proposed: adaptive neuro-fuzzy inference (ANFIS) [79, 84] and time–frequency analysis [81]. Unsupervised learning techniques were applied: independent component analysis [78, 83, 85, 86], principle component analysis [46, 91] and Kalman filtering [82]. Moreover, studies applied a variety of ML methods to classify CTG signals and determine fetal state, with best performances demonstrated using SVM [87, 89], DL [90] and RF [88].
Fetal monitoring and diagnostic CDSS
A portable prototype expert system detected modeled fetal arrhythmias with 88% accuracy and could be applied to scenarios where there is an insufficient number of experts and a large number of patients [84]. The prototype uses ANFIS to extract fECG from thoracic and abdominal signals, extracts the FHR and then detects fetal arrhythmia through an expert system based on production rules.
Pregnancy complications
Maternal diagnosis during pregnancy
Accurate prediction methods and diagnosis during prenatal care allow health professionals and prospective parents detect problems with the pregnancy as early as possible. Some studies investigate patient comorbidities including gestational diabetes mellitus [18, 27, 92–97], gestational hypertension disorders [98–100] and bacteriuria [101]. Studies aim to predict and classify disease in early pregnancy, improve screenings and provide clinical decision support for disease management. Methods proposed include rule-based [27, 97], Bayesian networks [18, 94, 95], ANN [92, 98, 101], evolutionary radial basis function network [93], genetic algorithm [99], expert systems [94, 96] and DT [96].
Preterm birth
Concerning preterm birth, studies focus on cervix-related risk [102, 103], classifying true preterm labor [104, 105], determining neonate mortality and prognosis [106, 107], predicting preterm birth risk [108–111], professional learning [112], estimating postnatal gestational age [113] and improving knowledge of gene regulatory elements in the placenta [114]. In 1982, Grignolio [106] presented a method to predict neonate mortality of premature newborns, using multiple regression. In 1990, Andersen et al. [115] found that shorter cervical length (CL) was associated with a high risk of preterm delivery. Woolery [108, 116] developed a clinical knowledge base for preterm birth risk assessment and developed an expert system for preterm birth risk assessment of pregnant women.
For pregnancy and labor contraction classification, studies found that AI methods improve diagnosis from EHG records, including polynomial classifiers [104], feature selection using binary particle swarm optimization with quadratic discriminant analysis [105] and a ridge extraction method [117]. Cervix properties were observed using AI methods to determine material properties [103] and CL [115]. Perinatal outcome was predicted with a DL model interpreting amniotic fluid metabolomics and proteomics in asymptomatic pregnant women with short CL [109]. SVM was applied to predict genome-wide placental enhancers, in order to further the understanding of placental dysfunction and implications of preterm birth and preeclampsia [114].
Two studies turn to EHR data to determine preterm birth risk, using ANN, LR, RF [110] and recurrent neural networks [111]. Both studies found associations with preterm birth risk and hypertensive disorders, as well as CL.
CDSS for pregnancy complications
Ectopic pregnancy can be potentially life-threatening, and therefore, early diagnosis and treatment of the condition are needed. A three-stage classifier (3SC) developed finds and limits diagnostic errors and then assists clinicians in choosing the initial treatment of ectopic pregnancy [57]. The model was evaluated across four algorithms: SVM, NB, DL and auto multilayer perceptron (MLP). 3SC achieved the best performance, in comparison with single-stage classifiers.
At the event of fetal–maternal hemorrhage, the standard clinical method to quantify fetal and maternal red blood cells (RBCs) is the Kleihauer–Betke test, which is performed by a certified technologist. The automated system can count over 60 000 RBCs within 5 minutes, versus a technologist counting ~2000 in about 15 minutes [118].
The Apgar score [119, 120] evaluates the condition of newborns in their first minutes of neonatal life. However, the score is not intended as a prognostic value; it has limitations and is often highly subjective, depending largely on the clinical experience of the evaluator. The prognostic value of the Expanded Apgar Score Form [121] was studied, observing the early death incidence in preterm newborns [107]. The chi-square automatic interaction detection classification tree generated decision rules based upon clinical data. The concentration of the oxygen applied during resuscitation was found to be an important criterion to neonatal outcome.
An open-source simulator, called NICeSim, was developed to aid health professionals to better understand the treatment and prognosis of premature newborns admitted to the neonatal intensive care unit [112]. The system allows for flexibility and provides alterations of the chosen variables. The attributes used to calculate death risk include Apgar scale, respiratory distress syndrome, gestational age and birth weight. Sufficient predictive power was demonstrated; ANN achieved better accuracy and specificity, whereas SVM performed better sensitivity. Important attributes are most likely absent as the ML model uses four attributes for a complex problem.
Perinatal care, birth and delivery
Fetal weight estimation
Clinicians and prospective parents want to be informed about the well-being of the unborn infant. AI applications observe infant growth and health status from imaging and maternal EHR data history. ML methods were applied to predict babies’ birth weight, using LR [122, 123], MLP [123] and fuzzy logic support vector regression [124], RF [122], Bayesian models [122, 125] and generalized boosted model [122]. The studies predict weight using EHR data [123, 124, 126], amniotic fluid [125], ultrasound images [122] and CTG traces [127].
Contraction classification
When extracting the FHR from an ECG recording, uterine contractions during labor can introduce significant noise. In order to improve perinatal knowledge and outcomes, AI has been applied to estimating date of delivery [115], route of delivery [128–131], fetal health prognosis [132] and length of labor [133]. Methods were been developed to provide perinatal knowledge [134], improve fetal monitoring and assessment [87–89, 117, 135–139] and classify true labor contractions [140]. A single paper employed unsupervised ML, using k-means clustering [139]. A 2015 systematic review found no strong evidence that the use of CTG with an expert system has an effect on the incidence of cesarean delivery nor a reduction in the incidence of forceps-assisted vaginal birth [24].
Route of delivery
Solely based upon FHR traces, models were developed to improve classifying route of delivery [129, 131] and classifying pregnancy and labor contractions [105]. Performance varied between ML techniques and number of features included in models; using 13 features, the DL classifier demonstrated the best performance, while selecting 8 features, the RF classifier performed best [129]. An ensemble classifier of three ML techniques, FLDA, RF and SVM classifiers, allows the strength of each model to be used to classify between cesarean section and vaginal delivery types [131].
Models take advantage of available EHR data in conjunction with labor monitoring data. Another study found that an aggregation double-layer SVM model using contextualized EHG parameters performed best to distinguish patients that will achieve spontaneous labor before the end of their full term from those that will require late-term induction of labor based upon EHG signals and obstetrical parameters [128]. Obstetrical parameters include maternal age, BMI, gestations, parity, Bishop score and days of gestation at recording moment.
CDSS for birth and delivery
The Adana System applied ANN to classify between cesarean section and vaginal delivery, including input variables of maternal characteristics and labor information [130]. Predicting route of delivery can inform care, allow appropriate allocation of resources and improve pregnancy outcomes.
Postpartum
During the postpartum period, many mothers try to cope with physical, social and psychological changes [141, 142]. Postpartum depression (PPD) affects an estimated 13–19% of women who have recently given birth [143]. Wang et al. [144] applied several ML models to predict PPD using EHRs and found several associated risk factors: race, obesity, anxiety, depression, antidepressants and anti-inflammatory drugs during pregnancy and different types of pain [144].
Unintended consequences and AI ethics
The potential of AI for pregnancy care exists but not without its barriers and potential pitfalls. Challenges include dataset shift, discriminatory bias, generalizability, poor clinical applicability, accidental fitting of cofounders and unintended negative consequences on health outcomes [145].
For instance, no papers were retrieved concerning transgender and gender non-conforming pregnancy. We also performed another literature search and found that there were no transgender-related AI studies on pregnancy. Many transgender men and gender non-conforming individuals (assigned female at birth) retain the capacity to become pregnant, use contraception, desire to become pregnant and give birth, and there are some case studies on this process [146, 147]. Little research focuses on the reproductive needs of this population [146, 148–150] and stigma can lead individuals to avoid seeking medical care or disclosing medically relevant health information [151]. Transgender individuals are likely to have unique needs surrounding pregnancy health and psychosocial health (e.g. gender dysphoria, lactation following chest surgery or binding, hormone replacement therapy) [151]. It would not be ethical to employ off-the-shelf AI methods designed for gender-conforming populations to those that were transgender or gender non-conforming populations.
It is unrealistic to assume that AI applications in health are ethically neutral. AI technology has the capacity to violate the basic rights of individuals, such as learning patterns from past clinical care that might increase discrimination (e.g. structural racism), violate privacy and inadvertently create inequalities in care. Unintentional discrimination (e.g. vulnerable populations, sexism and racism) need to be proactively accounted for in algorithms [152, 153], especially given that algorithms utilize data collected in the past that may be unintentionally biased in various ways. For patients and healthcare providers, individuals need a good understanding of the algorithm’s decision-making in order to have agency over the derived clinical decisions. In congruence with current best practices, AI needs to provide room for healthcare providers to influence the decision-making process. The patterns underlying AI decisions should also be made transparent to researchers for them to understand the potential biases underlying these algorithms.
Limitations and future work
We used ‘pregnancy’ as one of the search terms for identifying relevant papers. Therefore, preconception and postpartum studies were only included if they also discussed a pregnancy element. This may have lowered the overall number of studies focused on preconception and postpartum stages of pregnancy included in our literature review. Preconception care and postpartum care encompass healthcare beyond the scope of this particular review, and therefore, this study does not represent AI and ML applications in the entirety of these fields. Studies included in our review do not explicitly report the gender of their patients; therefore, it is unclear how many transgender patients may have been included in the research studies that we cite.
Conclusion
We found that AI and ML methodologies are used to help inform pregnancy outcomes. Of which 16 took advantage of EHR data to derive sound and reliable information about maternal and fetal health—illustrating the need to increase research using EHR data. Applications of mHealth were used in nine studies in the following areas: preconception [26, 33], during gestation [27, 36, 93, 96, 97, 154] and postpartum [34]. Unsupervised methods were limited to automated EHR and contraction monitoring [78, 82, 83, 85, 86, 139], imaging [46], genetics [91] and trisomy screening [69] applications. Research aimed to detect anomalies and diagnoses earlier, inform practice and support patients, improve fetal and maternal health knowledge, deep phenotype obstetric complications and automate aspects of current practice.
Past reviews of AI applications in pregnancy research and healthcare have described great potential but little realization in the clinical setting. While the papers in our review did not describe adoption explicitly in the clinical setting, the variety of CDSS (n = 24) and mHealth applications (n = 9) in our review illustrate the effort to translate AI into clinical care. Low adoption of AI in clinical care in the pregnancy domain may likely be due to liability questions in case of medical error that remain unresolved—especially for so-called black-box algorithms. More research on maternal healthcare is needed, with only 31% of prenatal stage papers focused on maternal needs. In addition, future research should proactively account for unintentional discrimination in algorithms. Potential pitfalls need to be accounted for in development of AI algorithms, in order to prevent adverse events and negative clinical impacts. Greater use of unsupervised methods may be appropriate with only nine studies using this approach but could be limited by the interpretability of their results. DL has begun to gain traction in recent years [10]—unsupervised ML and DL naturally apply well to imaging analysis and large datasets in biomedicine. The amalgamation of supervised and unsupervised learning (i.e. semi-supervised ML) could be valuable, as labeling data for supervised ML methods is time-consuming and expensive. AI and ML methods can be successfully employed to optimize pregnancy outcomes; with proper algorithmic improvement, refinement and ethics results, these methods could be incorporated into clinical care.
Key Points
Artificial intelligence and machine learning methods can be successfully employed to optimize pregnancy outcomes.
Supervised methods are the most common approach, and deep learning methods are gaining traction.
Future research should focus on less-studied areas: maternal healthcare needs, postpartum care, pregnancy care for transgender individuals and in algorithmic improvement, refinement and translation of results back into clinical care.
Supplementary Material
Lena Davidson received her MS degree at College of St. Scholastica, Duluth, MN, USA. Presently, she is a data analyst in the Department of Biostatistics, Epidemiology, and Informatics at the University of Pennsylvania.
Mary Regina Boland is an assistant professor of informatics in the Department of Biostatistics, Epidemiology, and Informatics at the University of Pennsylvania. He specializes in developing informatics methods that utilize data from Electronic Health Records to reveal novel clinical and scientific findings. Principally, these methods involve novel machine learning, artificial intelligence and language processing techniques.
Contributor Information
Lena Davidson, MS degree at College of St. Scholastica, Duluth, MN, USA.
Mary Regina Boland, Department of Biostatistics, Epidemiology, and Informatics at the University of Pennsylvania.
Data Availability Statement
This is a review paper and the primary data is the analysis of the papers themselves. This analysis and the main result of our work is included in Table 1 for all to access. We have also included a Prisma checklist as a supplementary document. Any additional data requests could be sent to the corresponding author: bolandm@upenn.edu
Funding
This work was supported by the Perelman School of Medicine at the University of Pennsylvania with generous funds to support this project.
Authors’ contribution
L.M.D. and M.R.B. conceived study design; wrote paper and reviewed, edited and approved final manuscript.
References
- 1.Shahid N, Rappon T, Berta W. Applications of artificial neural networks in health care organizational decision-making: a scoping review. PLoS One 2019;14:e0212356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fatima M, Pasha M. Survey of machine learning algorithms for disease diagnostic. J Intell Learn Syst Appl 2017;09:1–16. [Google Scholar]
- 3.Robinson PN. Deep phenotyping for precision medicine. Hum Mutat 2012;33:777–80. [DOI] [PubMed] [Google Scholar]
- 4.Weng C, Shah NH, Hripcsak G. Deep phenotyping: embracing complexity and temporality—towards scalability, portability, and interoperability. J Biomed Inform 2020;105:103433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sen C. Preterm labor and preterm birth. J Perinat Med 2017;45:911–3. [DOI] [PubMed] [Google Scholar]
- 6.Correa PJ, Palmeiro Y, Soto MJ, et al. . Etiopathogenesis, prediction, and prevention of preeclampsia. Hypertens Pregnancy 2016;35:280–94. [DOI] [PubMed] [Google Scholar]
- 7.Larsen EC, Christiansen OB, Kolte AM, et al. . New insights into mechanisms behind miscarriage. BMC Med 2013;11:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deo RC. Machine learning in medicine. Circulation 2015;132:1920–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Handelman GS, Kok HK, Chandra RV, et al. . eDoctor: machine learning and the future of medicine. J Intern Med 2018;284:603–19. [DOI] [PubMed] [Google Scholar]
- 10.Miotto R, Wang F, Wang S, et al. . Deep learning for healthcare: review, opportunities and challenges. Brief Bioinform 2018;19:1236–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.IMIA & Georg Thieme Verlag KG Stuttgart. Contents IMIA yearbook of medical informatics 2019. Yearb Med Inform 2019;28:I–VIII. [Google Scholar]
- 12.Raef B, Ferdousi R. A review of machine learning approaches in assisted reproductive technologies. Acta Inform Med 2019;27:205–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Balayla J, Shrem G. Use of artificial intelligence (AI) in the interpretation of intrapartum fetal heart rate (FHR) tracings: a systematic review and meta-analysis. Arch Gynecol Obstet 2019;300:7–14. [DOI] [PubMed] [Google Scholar]
- 14.Iftikhar PM, Kuijpers MV, Khayyat A, et al. . Artificial intelligence: a new paradigm in obstetrics and Gynecology research and clinical practice. Cureus 2020;12:e7124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liberati A, Altman DG, Tetzlaff J, et al. . The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Williamson PO, Minter CIJ. Exploring PubMed as a reliable resource for scholarly communications services. J Med Libr Assoc 2019;107:16–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adlassnig K-P. Medical Informatics in a United and Healthy Europe: Proceedings of MIE 2009, the XXII International Congress of the European Federation for Medical Informatics, 2009, 238. IOS Press, Amsterdam, Netherlands. [Google Scholar]
- 18.Hernando ME, Gómez EJ, Corcoy R, et al. . Evaluation of DIABNET, a decision support system for therapy planning in gestational diabetes. Comput Methods Prog Biomed 2000;62:235–48. [DOI] [PubMed] [Google Scholar]
- 19.Catanzarite VA, Jelovsek FR. Computer applications in obstetrics. Am J Obstet Gynecol 1987;156:1049–53. [DOI] [PubMed] [Google Scholar]
- 20.Singh AV, Rouchka EC, Rempala GA, et al. . Integrative database management for mouse development: systems and concepts. Birth Defects Res Part C Embryo Today Rev 2007;81:1–19. [DOI] [PubMed] [Google Scholar]
- 21.Greene KR. Intelligent fetal heart rate computer systems in intrapartum surveillance. Curr Opin Obstet Gynecol 1996;8:123–7. [PubMed] [Google Scholar]
- 22.Devoe LD. Future perspectives in intrapartum fetal surveillance. Best Pract Res Clin Obstet Gynaecol 2016;30:98–106. [DOI] [PubMed] [Google Scholar]
- 23.McCartney PR. Computer analysis of the fetal heart rate. J Obstet Gynecol Neonatal Nurs 2000;29:527–36. [DOI] [PubMed] [Google Scholar]
- 24.Lutomski JE, Meaney S, Greene RA, et al. . Expert systems for fetal assessment in labour. Cochrane Database Syst Rev 2015;4:1–2. [Google Scholar]
- 25.Haddad SM, Souza RT, Cecatti JG. Mobile technology in health (mHealth) and antenatal care–searching for apps and available solutions: a systematic review. Int J Med Inform 2019;127:1–8. [DOI] [PubMed] [Google Scholar]
- 26.Goodale BM, Shilaih M, Falco L, et al. . Wearable sensors reveal menses-driven changes in physiology and enable prediction of the fertile window: observational study. J Med Internet Res 2019;21:e13404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rigla M, Martínez-Sarriegui I, García-Sáez G, et al. . Gestational diabetes management using smart mobile telemedicine. J Diabetes Sci Technol 2018;12:260–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Benski AC, Stancanelli G, Scaringella S, et al. . Usability and feasibility of a mobile health system to provide comprehensive antenatal care in low-income countries: PANDA mHealth pilot study in Madagascar. J Telemed Telecare 2017;23:536–43. [DOI] [PubMed] [Google Scholar]
- 29.World Health Organization . OpenSRP|Open Smart Register Platform. 2020.
- 30.Stroux L, Martinez B, Coyote Ixen E, et al. . An mHealth monitoring system for traditional birth attendant-led antenatal risk assessment in rural Guatemala. J Med Eng Technol 2016;40:356–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bakibinga P, Kamande E, Omuya M, et al. . The role of a decision-support smartphone application in enhancing community health volunteers’ effectiveness to improve maternal and newborn outcomes in Nairobi, Kenya: quasi-experimental research protocol. BMJ Open 2017;7:e014896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marko KI, Krapf JM, Meltzer AC, et al. . Testing the feasibility of remote patient monitoring in prenatal care using a mobile app and connected devices: a prospective observational trial. JMIR Res Protoc 2016;5:e200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Green EP, Whitcomb A, Kahumbura C, et al. . ‘What is the best method of family planning for me?’: a text mining analysis of messages between users and agents of a digital health service in Kenya. Gates Open Res 2019;3:1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Green EP, Pearson N, Rajasekharan S, et al. . Expanding access to depression treatment in Kenya through automated psychological support: protocol for a single-case experimental design pilot study. JMIR Res Protoc 2019;8:e11800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cunningham SD, Lewis JB, Thomas JL, et al. . Expect with me: development and evaluation design for an innovative model of group prenatal care to improve perinatal outcomes. BMC Pregnancy Childbirth 2017;17:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Akbulut A, Ertugrul E, Topcu V. Fetal health status prediction based on maternal clinical history using machine learning techniques. Comput Methods Prog Biomed 2018;163:87–100. [DOI] [PubMed] [Google Scholar]
- 37.Lim J, Cloete G, Dunsmuir DT, et al. . Usability and feasibility of PIERS on the move: an mHealth app for pre-eclampsia triage. JMIR Mhealth Uhealth 2015;3:e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Balakrishnan R, Gopichandran V, Chaturvedi S, et al. . Continuum of care services for maternal and child health using mobile technology - a health system strengthening strategy in low and middle income countries. BMC Med Inform Decis Mak 2016;16:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Murphy HR. Managing diabetes in pregnancy before, during, and after COVID-19. Diabetes Technol Ther 2020;22:454–61. [DOI] [PubMed] [Google Scholar]
- 40.Aziz A, Zork N, Aubey JJ, et al. . Telehealth for high-risk pregnancies in the setting of the COVID-19 pandemic. Am J Perinatol 2020;37:800–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Prieto VM, Matos S, Álvarez M, et al. . Twitter: a good place to detect health conditions. PLoS One 2014;9:e86191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Klein AZ, Sarker A, Cai H, et al. . Social media mining for birth defects research: a rule-based, bootstrapping approach to collecting data for rare health-related events on Twitter. J Biomed Inform 2018;87:68–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yom-Tov E, Borsa D, Hayward AC, et al. . Automatic identification of web-based risk markers for health events. J Med Internet Res 2015;17:e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang K, Demner-Fushman D. Automated classification of eligibility criteria in clinical trials to facilitate patient-trial matching for specific patient populations. J Am Med Inform Assoc 2017;24:781–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nyalwidhe J, Burch T, Bocca S, et al. . The search for biomarkers of human embryo developmental potential in IVF: a comprehensive proteomic approach. Mol Hum Reprod 2013;19:250–63. [DOI] [PubMed] [Google Scholar]
- 46.Milewski R, Kuczyńska A, Stankiewicz B, et al. . How much information about embryo implantation potential is included in morphokinetic data? A prediction model based on artificial neural networks and principal component analysis. Adv Med Sci 2017;62:202–6. [DOI] [PubMed] [Google Scholar]
- 47.Tran D, Cooke S, Illingworth PJ, et al. . Deep learning as a predictive tool for fetal heart pregnancy following time-lapse incubation and blastocyst transfer. Hum Reprod 2019;34:1011–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Khosravi P, Kazemi E, Zhan Q, et al. . Deep learning enables robust assessment and selection of human blastocysts after in vitro fertilization. NPJ Digit Med 2019;21:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Morales DA, Bengoetxea E, Larrañaga P, et al. . Bayesian classification for the selection of in vitro human embryos using morphological and clinical data. Comput Methods Prog Biomed 2008;90:104–16. [DOI] [PubMed] [Google Scholar]
- 50.Uyar A, Bener A, Ciray HN. Predictive modeling of implantation outcome in an in vitro fertilization setting: an application of machine learning methods. Med Decis Mak 2015;35:714–25. [DOI] [PubMed] [Google Scholar]
- 51.Ambroise Grandjean G, Hossu G, Bertholdt C, et al. . Artificial intelligence assistance for fetal head biometry: assessment of automated measurement software. Diagn Interv Imaging 2018;99:709–16. [DOI] [PubMed] [Google Scholar]
- 52.Gentillon H, Stefańczyk L, Strzelecki M, et al. . Parameter set for computer-assisted texture analysis of fetal brain. BMC Res Notes 2016;9:496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mohseni Salehi SS, Khan S, Erdogmus D, et al. . Real-time deep pose estimation with geodesic loss for image-to-template rigid registration. IEEE Trans Med Imaging 2019;38:470–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yeo L, Romero R. Fetal intelligent navigation echocardiography (FINE): a novel method for rapid, simple, and automatic examination of the fetal heart. Ultrasound Obstet Gynecol 2013;42:268–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Re C, Bertucci E, Weissmann-Brenner A, et al. . Fetal thymus volume estimation by virtual organ computer-aided analysis in normal pregnancies. J Ultrasound Med 2015;34:847–52. [DOI] [PubMed] [Google Scholar]
- 56.Namburete AIL, Stebbing RV, Kemp B, et al. . Learning-based prediction of gestational age from ultrasound images of the fetal brain. Med. Image Anal 2015;21:72–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.De Ramón FA, Ruiz Fernández D, Prieto Sánchez MT. A decision support system for predicting the treatment of ectopic pregnancies. Int J Med Inform 2019;129:198–204. [DOI] [PubMed] [Google Scholar]
- 58.Gebeh AK, Marczylo EL, Amoako AA, et al. . Variation in stability of endogenous reference genes in fallopian tubes and endometrium from healthy and ectopic pregnant women. Int J Mol Sci 2012;13:2810–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hou B, Khanal B, Alansary A, et al. . 3-D reconstruction in canonical co-ordinate space from arbitrarily oriented 2-D images. IEEE Trans Med Imaging 2018;37:1737–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Burton GJ, Fowden AL. The placenta: a multifaceted, transient organ. Philos Trans R Soc B Biol Sci 2015;370:20140066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Turk EA, Luo J, Gagoski B, et al. . Spatiotemporal alignment of in utero BOLD-MRI series. J Magn Reson Imaging 2017;46:403–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Luo Y, Li Z, Guo H, et al. . Predicting congenital heart defects: a comparison of three data mining methods. PLoS One 2017;12:e0177811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lei B, Yao Y, Chen S, et al. . Discriminative learning for automatic staging of placental maturity via multi-layer fisher vector. Sci Rep 2015;5:12818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Looney P, Stevenson GN, Nicolaides KH, et al. . Fully automated, real-time 3D ultrasound segmentation to estimate first trimester placental volume using deep learning. JCI Insight 2018;3:e120178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sanderson J, Wu L, Mahajan A, et al. . Selection of the sub-noise gain level for acquisition of VOCAL data sets: a reliability study. Ultrasound Med Biol 2014;40:562–7. [DOI] [PubMed] [Google Scholar]
- 66.Centers for Disease Control and Prevention. Chorionic villus sampling and amniocentesis: recommendations for prenatal counseling. MMWR Recomm Rep 1995;44:1–12. [PubMed] [Google Scholar]
- 67.Kagan KO, Wright D, Valencia C, et al. . Screening for trisomies 21, 18 and 13 by maternal age, fetal nuchal translucency, fetal heart rate, free β-hCG and pregnancy-associated plasma protein-a. Hum Reprod 2008;23:1968–75. [DOI] [PubMed] [Google Scholar]
- 68.Marttala J, Peuhkurinen S, Ranta JK, et al. . Screening and outcome of chromosomal abnormalities other than trisomy 21 in northern Finland. Acta Obstet Gynecol Scand 2011;90:885–9. [DOI] [PubMed] [Google Scholar]
- 69.Neocleous AC, Nicolaides KH, Schizas CN. Intelligent noninvasive diagnosis of aneuploidy: raw values and highly imbalanced dataset. IEEE J Biomed Health Informatics 2017;21:1271–9. [DOI] [PubMed] [Google Scholar]
- 70.Neocleous AC, Nicolaides KH, Schizas CN. First trimester noninvasive prenatal diagnosis: a computational intelligence approach. IEEE J Biomed Health Informatics 2016;20:1427–38. [DOI] [PubMed] [Google Scholar]
- 71.Koivu A, Korpimäki T, Kivelä P, et al. . Evaluation of machine learning algorithms for improved risk assessment for Down’s syndrome. Comput Biol Med 2018;98:1–7. [DOI] [PubMed] [Google Scholar]
- 72.Chu T, Yeniterzi S, Rajkovic A, et al. . High resolution non-invasive detection of a fetal microdeletion using the GCREM algorithm. Prenat Diagn 2014;34:469–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Troisi J, Landolfi A, Sarno L, et al. . A metabolomics-based approach for non-invasive screening of fetal central nervous system anomalies. Metabolomics 2018;14:1–10. [DOI] [PubMed] [Google Scholar]
- 74.Yang J, Ding X, Zhu W. Improving the calling of non-invasive prenatal testing on 13−/18−/21-trisomy by support vector machine discrimination. PLoS One 2018;13:1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fiorentino F, Bono S, Pizzuti F, et al. . The clinical utility of genome-wide non-invasive prenatal screening. Prenat Diagn 2017;37:593–601. [DOI] [PubMed] [Google Scholar]
- 76.Neocleous AC, Syngelaki A, Nicolaides KH, et al. . Two-stage approach for risk estimation of fetal trisomy 21 and other aneuploidies using computational intelligence systems. Ultrasound Obstet Gynecol 2018;51:503–8. [DOI] [PubMed] [Google Scholar]
- 77.Evans MI, Cuckle HS. Performance adjusted risks: a method to improve the quality of algorithm performance while allowing all to play. Prenat Diagn 2011;31:797–801. [DOI] [PubMed] [Google Scholar]
- 78.Meinecke F, Ziehe A, Kawanabe M, et al. . A resampling approach to estimate the stability of one-dimensional or multidimensional independent components. IEEE Trans Biomed Eng 2002;49:1514–25. [DOI] [PubMed] [Google Scholar]
- 79.Assaleh K. Extraction of Fetal electrocardiogram using adaptive neuro-fuzzy inference systems. IEEE Trans Biomed Eng 2007;54:59–68. [DOI] [PubMed] [Google Scholar]
- 80. Kumar, Sharma SK, Prasad S. CAD for detection of fetal electrocardiogram by using wavelets and neuro-fuzzy systems. Int J Appl Eng Res 2016;11:2321–6. [Google Scholar]
- 81.Karvounis EC, Tsipouras MG, Fotiadis DI, et al. . An automated methodology for Fetal heart rate extraction from the abdominal electrocardiogram. IEEE Trans Inf Technol Biomed 2007;11:628–38. [DOI] [PubMed] [Google Scholar]
- 82.Haghpanahi M, Borkholder DA. Fetal QRS extraction from abdominal recordings via model-based signal processing and intelligent signal merging. Physiol Meas 2014;35:1591–605. [DOI] [PubMed] [Google Scholar]
- 83.Varanini M, Tartarisco G, Billeci L, et al. . An efficient unsupervised fetal QRS complex detection from abdominal maternal ECG. Physiol Meas 2014;35:1607–19. [DOI] [PubMed] [Google Scholar]
- 84.Corona-Figueroa A. A portable prototype for diagnosing fetal arrhythmia. Unlocked: Informatics Med, 2019. [Google Scholar]
- 85.Mantini D, Alleva G, Comani S. A method for the automatic reconstruction of fetal cardiac signals from magnetocardiographic recordings. Phys Med Biol 2005;50:4763–81. [DOI] [PubMed] [Google Scholar]
- 86.Comani S, Srinivasan V, Alleva G, et al. . Entropy-based automated classification of independent components separated from fMCG. Phys Med Biol 2007;52:N87–97. [DOI] [PubMed] [Google Scholar]
- 87.Yilmaz E, Kilikçier Ç. Determination of fetal state from cardiotocogram using LS-SVM with particle swarm optimization and binary decision tree. Comput Math Methods Med 2013;2013:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sahin H, Subasi A. Classification of the cardiotocogram data for anticipation of fetal risks using machine learning techniques. Appl Soft Comput J 2015;33:231–8. [Google Scholar]
- 89.Czabanski R, Jezewski M, Horoba K, et al. . Fuzzy analysis of delivery outcome attributes for improving the automated Fetal state assessment. Appl Artif Intell 2016;30:556–71. [Google Scholar]
- 90.Miao JH, Miao KH. Cardiotocographic diagnosis of fetal health based on multiclass morphologic pattern predictions using deep learning classification. Int J Adv Comput Sci Appl 2018;9:1–11. [Google Scholar]
- 91.Al-Shaer AE, Flentke GR, Berres ME, et al. . Exon level machine learning analyses elucidate novel candidate miRNA targets in an avian model of fetal alcohol spectrum disorder. PLoS Comput Biol 2019;15:1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Polak S, Mendyk A. Artificial intelligence technology as a tool for initial GDM screening. Expert Syst Appl 2004;26:455–60. [Google Scholar]
- 93.Moreira MWL, Rodrigues JJPC, Kumar N, et al. . Evolutionary radial basis function network for gestational diabetes data analytics. J Comput Sci 2018;27:410–7. [Google Scholar]
- 94.Gomes Filho E, Pinheiro PR, Pinheiro MCD, et al. . Heterogeneous methodology to support the early diagnosis of gestational diabetes. IEEE Access 2019;7:67190–9. [Google Scholar]
- 95.Hernando ME, Gómez EJ, Del Pozo F, et al. . DIABNET: a qualitative model-based advisory system for therapy planning in gestational diabetes. Med Inf 1996;21:359–74. [DOI] [PubMed] [Google Scholar]
- 96.Caballero-Ruiz E, García-Sáez G, Rigla M, et al. . A web-based clinical decision support system for gestational diabetes: automatic diet prescription and detection of insulin needs. Int J Med Inform 2017;102:35–49. [DOI] [PubMed] [Google Scholar]
- 97.Peleg M, Shahar Y, Quaglini S, et al. . Assessment of a personalized and distributed patient guidance system. Int J Med Inform 2017;101:108–30. [DOI] [PubMed] [Google Scholar]
- 98.Tejera E, Joseareias M, Rodrigues A, et al. . Artificial neural network for normal, hypertensive, and preeclamptic pregnancy classification using maternal heart rate variability indexes. J Matern Neonatal Med 2011;24:1147–51. [DOI] [PubMed] [Google Scholar]
- 99.Liu LY, Yang T, Ji J, et al. . Integrating multiple ‘omics’ analyses identifies serological protein biomarkers for preeclampsia. BMC Med 2013;11:236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Moreira MWL, Rodrigues JJPC, Al-Muhtadi J, et al. . Neuro-fuzzy model for HELLP syndrome prediction in mobile cloud computing environments. Concurrency Computat Pract Exper. 2018;e4651. [Google Scholar]
- 101.Burton RJ, Albur M, Eberl M, et al. . Using artificial intelligence to reduce diagnostic workload without compromising detection of urinary tract infections. BMC Med Inform Decis Mak 2019;19:171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wu M, Fraser RF, Chen CW. A novel algorithm for computer-assisted measurement of cervical length from transvaginal ultrasound images. IEEE Trans Inf Technol Biomed 2004;8:333–42. [DOI] [PubMed] [Google Scholar]
- 103.Shi L, Yao W, Gan Y, et al. . Anisotropic material characterization of human cervix tissue based on indentation and inverse finite element analysis. J Biomech Eng 2019;141:0910171–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Fergus P, Cheung P, Hussain A, et al. . Prediction of preterm deliveries from EHG signals using machine learning. PLoS One 2013;8:e77154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Alamedine D, Khalil M, Marque C. Comparison of different EHG feature selection methods for the detection of preterm labor. Comput Math Methods Med 2013;2013:585–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Grignolio G. Medical diagnoses by artificial intelligence process. Clin Exp Obstet Gynecol 1982;9:233–4. [PubMed] [Google Scholar]
- 107.Góralska A, Puskarz-Gąsowska J, Borszewska-Kornacka MK. Practical application and prognostic value of the expanded Apgar score. Arch Perinat Med 2013;19:88–93. [Google Scholar]
- 108.Woolery LK, Grzymala-Busse J. Machine learning for an expert system to predict preterm birth risk. J Am Med Inform Assoc 1994;1:439–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bahado-Singh RO, Sonek J, McKenna D, et al. . Artificial intelligence and amniotic fluid multiomics: prediction of perinatal outcome in asymptomatic women with short cervix. Ultrasound Obstet Gynecol 2019;54:110–8. [DOI] [PubMed] [Google Scholar]
- 110.Lee KS, Ahn KH. Artificial neural network analysis of spontaneous preterm labor and birth and its major determinants. J Korean Med Sci 2019;34:e128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gao C, Osmundson S, Velez Edwards DR, et al. . Deep learning predicts extreme preterm birth from electronic health records. Inform: J. Biomed, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Cerqueira FR, Ferreira TG, Paiva OA, et al. . NICeSim: an open-source simulator based on machine learning techniques to support medical research on prenatal and perinatal care decision making. Artif Intell Med 2014;62:193–201. [DOI] [PubMed] [Google Scholar]
- 113.Torres Torres M, Valstar M, Henry C, et al. . Postnatal gestational age estimation of newborns using small sample deep learning. Image Vis Comput 2019;83–84:87–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zhang J, Simonti CN, Capra JA. Genome-wide maps of distal gene regulatory enhancers active in the human placenta. PLoS One 2018;13:e0209611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Andersen HF, Nugent CE, Wanty SD, et al. . Prediction of risk for preterm delivery by ultrasonographic measurement of cervical length. Am J Obstet Gynecol 1990;163:859–67. [DOI] [PubMed] [Google Scholar]
- 116.Fitzgerald Woolery LK. Clinical knowledge base development for preterm-birth risk assessment. Appl Nurs Res 1994;7:141–4. [DOI] [PubMed] [Google Scholar]
- 117.Terrien J, Marque C, Germain G. Ridge extraction from the time–frequency representation (TFR) of signals based on an image processing approach: application to the analysis of uterine electromyogram AR TFR. IEEE Trans Biomed Eng 2008;55:1496–503. [DOI] [PubMed] [Google Scholar]
- 118.Ge J, Gong Z, Chen J, et al. . A system for counting fetal and maternal red blood cells. IEEE Trans Biomed Eng 2014;61:2823–9. [DOI] [PubMed] [Google Scholar]
- 119.Apgar V. A proposal for a new method of evaluation of the newborn. Class Pap Crit Care 1952;32:97. [Google Scholar]
- 120.Apgar V, Holaday DA, James LS, et al. . Evaluation of the newborn infant-second report. JAMA 1958;168:1985–8. [DOI] [PubMed] [Google Scholar]
- 121.Stark AR, Adamkin DH, Batton DG, et al. . The Apgar score. Pediatrics 2006;117:1444–7. [DOI] [PubMed] [Google Scholar]
- 122.Naimi AI, Platt RW, Larkin JC. Machine learning for fetal growth prediction. Epidemiology 2018;29:290–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Etikan I, Çaglar MK. Prediction methods for babies’ birth weight using linear and nonlinear regression analysis. Technol Health Care 2005;13:131–5. [PubMed] [Google Scholar]
- 124.Yu J, Wang Y, Chen P. Fetal weight estimation using the evolutionary fuzzy support vector regression for low-birth-weight fetuses. IEEE Trans Inf Technol Biomed 2009;13:57–66. [DOI] [PubMed] [Google Scholar]
- 125.Boisvert MR, Koski KG, Burns DH, et al. . Early prediction of macrosomia based on an analysis of second trimester amniotic fluid by capillary electrophoresis. Biomark Med 2012;6:655–62. [DOI] [PubMed] [Google Scholar]
- 126.Lu Y, Fu X, Chen F, et al. . Prediction of fetal weight at varying gestational age in the absence of ultrasound examination using ensemble learning. Artif Intell Med 2020;102:101748. [DOI] [PubMed] [Google Scholar]
- 127.Signorini MG, Pini N, Malovini A, et al. . Integrating machine learning techniques and physiology based heart rate features for antepartum fetal monitoring. Comput Methods Prog Biomed 2020;185:105015. [DOI] [PubMed] [Google Scholar]
- 128.Alberola-Rubio J, Garcia-Casado J, Prats-Boluda G, et al. . Prediction of labor onset type: spontaneous vs induced; role of electrohysterography? Comput Methods Prog Biomed 2017;144:127–33. [DOI] [PubMed] [Google Scholar]
- 129.Fergus P, Hussain A, Al-Jumeily D, et al. . Classification of caesarean section and normal vaginal deliveries using foetal heart rate signals and advanced machine learning algorithms. Biomed Eng Online 2017;16:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Beksac MS, Tanacan A, Bacak HO, et al. . Computerized prediction system for the route of delivery (vaginal birth versus cesarean section). J Perinat Med 2018;46:881–4. [DOI] [PubMed] [Google Scholar]
- 131.Fergus P, Selvaraj M, Chalmers C. Machine learning ensemble modelling to classify caesarean section and vaginal delivery types using cardiotocography traces. Comput Biol Med 2018;93:7–16. [DOI] [PubMed] [Google Scholar]
- 132.Hernández C, Arjas JE, Gómez L. A perinatal monitoring display based on the fetal topogram. IEEE Trans Biomed Eng 1986;BME-33:785–92. [DOI] [PubMed] [Google Scholar]
- 133.Devoe LD, Samuel S, Prescott P, et al. . Predicting the duration of the first stage of spontaneous labor using a neural network. J Matern Neonatal Med 1996;5:256–61. [DOI] [PubMed] [Google Scholar]
- 134.Sokol RJ, Chik L. A prototype system for perinatal knowledge engineering using an artificial intelligence tool. J Perinat Med 1988;16:273–81. [DOI] [PubMed] [Google Scholar]
- 135.Keith RDF, Westgate J, Hughes GW, et al. . Preliminary evaluation of an intelligent system for the management of labour. J Perinat Med 1994;22:345–50. [PubMed] [Google Scholar]
- 136.Beksaç MS, Egemen A, Izzetoǵlu K, et al. . An automated intelligent diagnostic system for the interpretation of umbilical artery Doppler velocimetry. Eur J Radiol 1996;23:162–7. [DOI] [PubMed] [Google Scholar]
- 137.Beksaç MS, Başaran F, Eskiizmirliler S, et al. . A computerized diagnostic system for the interpretation of umbilical artery blood flow velocity waveforms. Eur J Obstet Gynecol Reprod Biol 1996;64:37–42. [DOI] [PubMed] [Google Scholar]
- 138.Ungureanu M, Bergmans JWM, Oei SG, et al. . Fetal ECG extraction during labor using an adaptive maternal beat subtraction technique. Biomed Tech 2007;52:56–60. [DOI] [PubMed] [Google Scholar]
- 139.La Rosa PS, Nehorai A, Eswaran H, et al. . Detection of uterine MMG contractions using a multiple change point estimator and the K-means cluster algorithm. IEEE Trans Biomed Eng 2008;55:453–67. [DOI] [PubMed] [Google Scholar]
- 140.Chen L, Hao Y. Discriminating pregnancy and labour in electrohysterogram by sample entropy and support vector machine. J Med Imaging Health Informatics 2017;7:584–91. [Google Scholar]
- 141.Aber C, Weiss M, Fawcett J. Contemporary women’s adaptation to motherhood: the first 3 to 6 weeks postpartum. Nurs Sci Q 2013;26:344–51. [DOI] [PubMed] [Google Scholar]
- 142.Aydemir S, Onan N. The relationship between maternal self-confidence and postpartum depression in primipara mothers: a follow-up study. Community Ment Health J 2020;56:1–8. [DOI] [PubMed] [Google Scholar]
- 143.O’Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annu Rev Clin Psychol 2013;9:379–407. [DOI] [PubMed] [Google Scholar]
- 144.Wang S, Pathak J, Zhang Y. Using electronic health records and machine learning to predict postpartum depression. Stud Health Technol Inform 2019;264:888–92. [DOI] [PubMed] [Google Scholar]
- 145.Kelly CJ, Karthikesalingam A, Suleyman M, et al. . Key challenges for delivering clinical impact with artificial intelligence. BMC Med 2019;17:195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Light AD, Obedin-Maliver J, Sevelius JM, et al. . Transgender men who experienced pregnancy after female-to-male gender transitioning. Obstet Gynecol 2014;124:1120–7. [DOI] [PubMed] [Google Scholar]
- 147.Light A, Wang LF, Zeymo A, et al. . Family planning and contraception use in transgender men. Contraception 2018;98:266–9. [DOI] [PubMed] [Google Scholar]
- 148.MacDonald T, Noel-Weiss J, West D, et al. . Transmasculine individuals’ experiences with lactation, chestfeeding, and gender identity: a qualitative study. BMC Pregnancy Childbirth 2016;16:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Obedin-Maliver J, Makadon HJ. Transgender men and pregnancy. Obstet Med 2016;9:4–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Sterling J, Garcia MM. Fertility preservation options for transgender individuals. Transl Androl Urol 2020;9:S215–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Hoffkling A, Obedin-Maliver J, Sevelius J. From erasure to opportunity: a qualitative study of the experiences of transgender men around pregnancy and recommendations for providers. BMC Pregnancy Childbirth 2017;17:332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kearns M, Roth A. The ethical algorithm: the science of socially aware algorithm design. New York, NY: Oxford University Press, 2019. [Google Scholar]
- 153.The Lancet Digital Health . There is no such thing as race in health-care algorithms. Lancet Digit Health 2019;1:e375. [DOI] [PubMed] [Google Scholar]
- 154.Moreira MWL, Rodrigues JJPC, Furtado V, et al. . Averaged one-dependence estimators on edge devices for smart pregnancy data analysis. Comput Electr Eng 2019;77:435–44. [Google Scholar]
- 155.Schölkopf B. SVMs - a practical consequence of learning theory. IEEE Intell Syst Their Appl 1998;13:18–21. [Google Scholar]
- 156.Renganathan V. Overview of artificial neural network models in the biomedical domain. Bratislava Med J 2019;120:536–40. [DOI] [PubMed] [Google Scholar]
- 157.Pal SK, Mitra S. Multilayer perceptron, fuzzy sets, and classification. IEEE Trans Neural Netw 1992;3:683–97. [DOI] [PubMed] [Google Scholar]
- 158.Dash CSK, Behera AK, Dehuri S, et al. . Radial basis function neural networks: a topical state-of-the-art survey. Open Comput Sci 2016;6:33–63. [Google Scholar]
- 159.Dankowski T, Ziegler A. Calibrating random forests for probability estimation. Stat Med 2016;35:3949–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Puga JL, Krzywinski M, Altman N. Points of significance: Bayes’ theorem. Nat Methods 2015;12:277–8. [DOI] [PubMed] [Google Scholar]
- 161.Keller JM, Gray MR. A fuzzy k-nearest neighbor algorithm. IEEE Trans Syst Man Cybern 1985;SMC-15:580–5. [Google Scholar]
- 162.Friedman JH. Regularized discriminant analysis. J Am Stat Assoc 1989;84:165–75. [Google Scholar]
- 163.Mitchell M. An Introduction to Genetic Algorithms. Cambridge, MA: MIT Press, 2020. [Google Scholar]
- 164.Ching T, Himmelstein DS, Beaulieu-Jones BK, et al. . Opportunities and obstacles for deep learning in biology and medicine. J R Soc Interface 2018;15:20170387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Bro R, Smilde AK. Principal component analysis. Anal Methods 2014;6:2812–31. [Google Scholar]
- 166.Tharwat A. Independent component analysis: an introduction. Appl. Comput. Inform. 2018. [Google Scholar]
- 167.Jain AK. Data clustering: 50 years beyond k-means. Pattern Recogn Lett 2010;31:651–66. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
This is a review paper and the primary data is the analysis of the papers themselves. This analysis and the main result of our work is included in Table 1 for all to access. We have also included a Prisma checklist as a supplementary document. Any additional data requests could be sent to the corresponding author: bolandm@upenn.edu


