Abstract
Importance
The relationship between obesity and impairments in male sexual functioning is well documented. Relatively few studies have investigated changes in sexual functioning and sex hormones in men who achieve significant weight loss with bariatric surgery.
Objective
To assess changes in sexual functioning, sex hormones, and relevant psychosocial constructs in men who underwent bariatric surgery.
Design, Setting and Participants
A prospective cohort study of 32 men from the Longitudinal Assessment of Bariatric Surgery-2 (LABS) investigation who underwent a Roux-en-Y gastric bypass (median BMI [25th percentile, 75th percentile] 45.1 [42.0, 52.2]) and completed assessments between 2006 and 2012.
Intervention
Bariatric surgery was performed by a LABS-certified surgeon.
Main Outcomes and Measures
Sexual functioning was assessed by the International Index of Erectile Functioning (IIEF). Hormones were assessed by blood assay. Quality of life (QoL), body image, depressive symptoms and marital adjustment were assessed by questionnaire.
Results
Men lost, on average, (95% confidence interval) 33.3% (36.1%, 30.5%) of initial body weight at postoperative Year 1, 33.6% (36.8%, 30.5%) at Year 2, 31.0% (34.1%, 27.9%) at Year 3, and 29.4% (32.7%, 26.2%) at Year 4. Participants experienced significant increases in total testosterone (P<0.001) and sex hormone binding globulin (SHBG) (P<0.001) through postoperative Year 4. While men reported improvements in sexual functioning after surgery, these changes did not significantly differ from baseline, with the exception of overall satisfaction at postoperative Year 3 (P=0.008). Participants reported significant improvements in physical domains of health-related quality of life (HRQoL), all domains of weight-related QOL, and body image, but not in the mental health domains of HRQoL or relationship satisfaction.
Conclusions and Relevance
Men who lost approximately one-third of their body weight following Roux-en-Y gastric bypass experienced significant increases in total testosterone and SHBG. They did not, however, report significant improvements in sexual functioning, relationship satisfaction or mental health domains of HRQoL. This pattern of results differs from that of women who have undergone bariatric surgery, who reported almost uniform improvements in sexual functioning and psychosocial status.
Trial Registration
http://www.clinicaltrials.gov ID# NCT00670098 https://register.clinicaltrials.gov/prs/app/action/SelectProtocol?sid=S0001JXP&selectaction=View&uid=U0000XTL&ts=4&cx=-2bwzz2
Keywords: Sexual Functioning, Sex Hormones, Quality of Life, Obesity, Bariatric Surgery
Introduction
Obesity, and extreme obesity in particular, is associated with significant medical and psychosocial comorbidity.1–2 A large number of studies have found a relationship between extreme obesity and impairments in quality of life, as well as greater depressive symptoms and increased body image dissatisfaction.3–7 Individuals with obesity often report untoward changes in sexual functioning and decreased sexual satisfaction.6,8–13 In a recent study of individuals with extreme obesity who presented for bariatric surgery, 51% of women and 36% of men reported a sexual dysfunction.13 The presence of dysfunctional sexual behavior was associated with lower levels of quality of life and impairment in other areas of psychosocial functioning for women. In contrast, the impact of sexual dysfunction on the psychosocial functioning of men was less pronounced or uniform.13 Obesity has been associated with untoward changes in several sex hormones in women and men, which also may adversely impact sexual functioning.13–17
Weight loss following lifestyle modification or bariatric surgery has been associated with significant improvements in sexual functioning18–21 and sex hormones.16, 21–23 For example, we recently found that women who underwent bariatric surgery, and experienced a mean weight loss of 33.5% (95% CI, 31.5%–35.6%) at postoperative year 2, reported significant improvements in overall sexual functioning and specific domains of functioning, including desire, arousal, lubrication, and statisfaction.24 These women also reported significant improvements in body image, depressive symptoms, and most domains of quality of life, and they experienced improvements in total testosterone, estradiol, follicular stimulating hormone, sex hormone binding globulin and DHEA-S.
As women represent the vast majority of individuals who present for bariatric surgery, there has been less opportunity to study changes in sexual functioning and sex hormones in men who undergo bariartric surgery. For example, in a study of 10 men who underwent Roux-en-Y gastric bypass, Reis and colleagues found marginally significant improvements in self-reported sexual functioning two years after surgery, improvements in total testosterone, follicle stimulating hormone and prolactin were more robust.21 This study, however, was limited by its small sample size. Further, it did not include an assessment of psychosocial factors, such as quality of life, body image and romantic relationship satisfaction, that could influence sexual behavior. The present study was undertaken to address this gap in the literature. We hypothesized that men would experience improvements in sexual functioning, sex hormones and psychosocial variables of interest, with a pattern of results similar to that seen with women.25
Method
Study Design
This study used data collected from the Longitudinal Assessment of Bariatric Surgery (LABS) consortium. The LABS study design is detailed elsewhere.26–28 LABS-2 is investigating the long-term effects of bariatric surgery on patients’ weight, as well as physical and mental health status. The present study is considered an ancillary study of LABS-2 as it extends lines of investigation to other, more specific questions, including our previous reports on baseline sexual functioning13 and changes in female sexual functioning two years after surgery.25
Thirty-two men undergoing Roux-en-Y gastric bypass and participating in the LABS-2 study from two of the ten LABS sites (the Neuropsychiatric Research Institute [NRI] and the University of Pittsburgh Medical Center [UPMC]) were studied. Data were collected between 2006 and 2012. Participants were assessed prior to surgery and annually thereafter. Year 2 was the primary point of interest since most bariatric surgery patients reach maximum weight loss by this time.29 We also report three and four year outcomes. The trial was approved by the Institutional Review Boards at NRI, UPMC, and the University of Pennsylvania. Informed consent was received from all participants.
Participants
Men met the inclusion criteria of the LABS-2 study (at least 18 years old and seeking a first bariatric surgical procedure) and also met all medical and mental health criteria for bariatric surgery. Men who were non-ambulatory, those with significant or uncontrolled medical conditions (including recent history of stroke, untreated or uncontrolled hypertension, history of renal or hepatic disease), and those with untreated or uncontrolled psychiatric conditions were excluded. Men had to report involvement in a relationship that provided them with opportunity for sexual activity with a partner. Participants received a $40.00 gift card (to a local department or bookstore) following completion of each assessment and to enhance retention.
Interventions
Bariatric surgery. Surgery was performed by a LABS-certified surgeon. Thirty-two men underwent Roux-en-Y gastric bypass performed using standard techniques.
Measures
Participants completed the following assessments:
International Index of Erectile Function (IIEF). The IIEF is a widely-used, 15-item scale that assesses five domains of male sexual functioning: erectile function (range: 0–30); orgasmic function (0–10); sexual desire (2–10); intercourse satisfaction (0–15); and overall satisfaction (2–10). Lower scores indicate less satisfaction and greater dysfunction.30–31
The Short Form Health Survey-36 item version (SF-36). The SF-36 was used to assess health-related quality of life (HRQoL). Eight subscales assess separate domains of health and related functioning. Items on the physical functioning, physical role functioning, pain, and general health subscales were used to calculate the physical health summary score. Items on vitality, social functioning, emotional role functioning and mental health subscales were used to calculate the mental health summary score. Higher scores indicate more positive health-related quality of life.32
Impact of Weight on Quality of Life-Lite (IWQOL-Lite). The IWQOL-Lite assessed weight-related quality of life.33–34 The measure contains 31 items, with each item beginning with the phrase “Because of my weight,” which assess five domains: work; physical function; public distress; sex life; and self-esteem. Responses are combined to calculate a total score that ranges from 0 to 100; higher scores indicate a better quality of life.
Body Image Quality of Life Inventory (BIQLI). The BIQLI is a 19-item measure of the positive and negative impact of body image on various qualities of life.35 Respondents’ feelings are assessed in regard to beliefs about the self and life in general, emotional states, same and other-sex relationships, eating and exercise, grooming activities, and sexual experiences, as well as family and work/school contexts. Participants respond to items using a 7-point scale ranging from −3 (“Very Negative Effect”) to +3 (“Very Positive Effect”); 0 is labeled “No Effect.” Higher scores suggest more positive body image quality of life.
Body Shape Questionnaire (BSQ). The Body Shape Questionnaire assessed dissatisfaction with body shape.36 The 38 items on the measure are rated on a scale of 1 (“Never”) to 6 (“Always”) based on how the respondent has been feeling over the last 4 weeks. Higher scores indicate greater dissatisfaction.
Dyadic Adjustment Scale (DAS). Relationship satisfaction was assessed by Dyadic Adjustment Survey.37 The measure addresses four domains that measure the quality of marriage or similar dyads: dyadic consensus, dyadic satisfaction, dyadic cohesion, and affectional expression. Items can be summed to a total score; higher scores indicate higher levels of satisfaction.
Beck Depression Inventory-II (BDI-II). The BDI-II assessed depressive symptoms.38 Scores range from 0 to 63, with higher scores indicating greater symptoms.
Sex Hormones
A 20 ml blood sample was obtained from each participant. Samples were cooled on ice and centrifuged within 15 min of drawing. Plasma was removed from the vacutainer within 15 min after centrifugation, placed into polypropylene tubes, and bulk-shipped to the Clinical Translational Research Center at the University of Pennsylvania for analysis. We assessed total testosterone, free testosterone, luteinizing hormone (LH), and sex hormone binding globulin (SHBG). Total testosterone and SHGB were analyzed using standard enzyme-linked immuno assay (ELISA) (IBL Hamburg) assay kits. Luteinizing hormone was analyzed by means of Chemiluminescent (Roche Elecys) laboratory assays. Free testosterone was analyzed using RIA assay kits (Siemens Los Angeles).
Statistical Analysis
Descriptive statistics were used to summarize the baseline characteristics of participants. Frequencies and percentages were used for categorical data; median values and inter-quartile ranges were calculated for continuous data.
An intercept and time point-only normal mixed model with a heterogeneous compound symmetry covariance matrix was used to report changes in sexual functioning scores, sex hormone levels, psychosocial measures, and weight. For each assessment, pairwise comparisons were made between baseline and each follow-up time point; P values and confidence limits were adjusted for the multiple comparisons using simulation. The reported modeling values and changes were used to account for missing data at each time point. (The observed mean values and standard deviations of each assessment are reported in the eTables 1 and 2 in the Supplemental Tables. The observed values were similar to the modeled values.)
Analyses were conducted using SAS version 9.2 (SAS Institute Inc). All reported P values are 2 sides; P < .05 was considered to be statistically significant.
Results
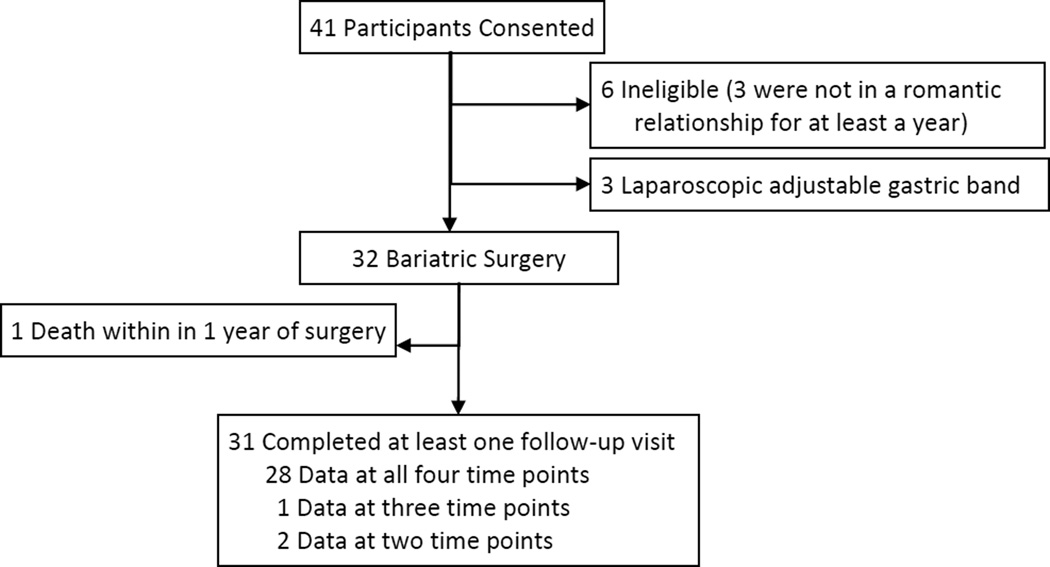
Forty one men provided informed consent. Six were found to be ineligible; 3 were not in a relationship that provided regular access to a sexual partner, two did not undergo surgery and one had a BMI that did not meet the inclusion criteria for the study. Three men underwent a laparoscopic adjustable gastric banding procedure and were excluded from these analyses. Of the thirty-two men who underwent a Roux-en-Y gastric bypass procedure, 1 died before the 1 year assessment. The other 31 participants completed at least 1 follow-up assessment. Follow-up data were collected at all 4 times points for 28 participants, at 3 time points for 1 participants, and at 2 time points for 2 participants. (Figure 1) Participants were considered as having provided data if any of the following were completed: physical measurements, blood samples or at least 1 self-assessment measure.
Figure 1.
Recruitment and retention of study participants
Demographic Characteristics
Baseline demographic and descriptive characteristics, reported previously,13 are presented in Table 1. Men had a median body mass index of 45.1 kg/m2. All were white and all but one reported at least a high school diploma or GED.
Table 1.
Baseline characteristics of participating men
| Number of men | 32 |
| Age (years) | |
| Median (Q1, Q3) | 48 (39, 55) |
| Range | 24 – 64 |
| Race -n (%) | |
| White | 32 (100) |
| Black | 0 (0.0) |
| Other | 0 (0.0) |
| Ethnicity -n (%) | |
| Hispanic | 1 (3) |
| Non-Hispanic | 31 (97) |
| Highest education levela -n (%) | |
| Some high school | 1 (3) |
| High school diploma or GED | 3 (10) |
| Some college | 9 (29) |
| Other post high school education | 11 (35) |
| College diploma | 4 (13) |
| Graduate or professional degree | 3 (10) |
| Body mass index (kg/m2) | |
| Median (Q1, Q3) | 45.1 (42.0, 52.2) |
| Range | 37.3 – 64.6 |
| Weight (kg) | |
| Median (Q1, Q3) | 149.3 (130.7, 170.0) |
| Range | 111.4 – 228.2 |
| Waist circumferencea (cm) | |
| Median (Q1, Q3) | 145.4 (136.5, 155.5) |
| Range | 122.4 – 183.0 |
Missing data: 1 education; 1 waist circumference
Q1 = 25th percentile; Q3=75th percentile
Weight Loss
The average (95% confidence interval) percent reduction in initial weight at postoperative Year 1 was 33.3% (36.1%, 30.5%), which increased at postoperative Year 2 to 33.6% (36.8%, 30.5%). At postoperative Years 3 and 4, total percent weight loss was 31.0% (34.1%, 27.9%) and 29.4% (32.7%, 26.2%), respectively.
Sexual Functioning and Sex Hormones
Men reported improvements on all subscales of the IIEF at postoperative Years 2, 3 and 4 as compared to baseline; however, with one exception, these changes did not reach statistical significance. At postoperative Year 3, overall satisfaction was significantly different from baseline. By Year 4, this change was no longer significant (Table 3).
Table 3.
Change in International Index of Erectile Function (IIEF) and Sex Hormone Levels
| Model Based Estimates, Mean (SD) | Model Based Mean Change (95% CI) | P-Value | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Year 1 | Year 2 | Year 3 | Year 4 | Year 1 from Baseline |
Year 2 from Baseline |
Year 3 from Baseline |
Year 4 from Baseline |
Year 1 vs Baseline |
Year 2 vs Baseline |
Year 3 vs Baseline |
Year 4 vs Baseline |
|
| IIEF Scores | |||||||||||||
| Erectile function | 19.9 (11.6) | 21.3 (10.4) | 24.4 (8.5) | 23.1 (10.2) | 23.1 (9.4) | 1.4 (−4.0, 6.8) | 4.5 (−0.6, 9.6) | 3.2 (−2.0, 8.4) | 3.1 (−2.3, 8.6) | 0.910 | 0.099 | 0.357 | 0.395 |
| Orgasmic function | 7.1 (3.9) | 7.2 (4.0) | 8.7 (2.7) | 8.1 (3.3) | 7.6 (3.8) | 0.1 (−2.1, 2.4) | 1.6 (−0.3, 3.5) | 1.0 (−0.9, 3.0) | 0.6 (−1.7, 2.8) | >0.99 | 0.113 | 0.490 | 0.926 |
| Sexual desire | 6.4 (2.5) | 7.6 (2.2) | 7.5 (1.9) | 7.1 (2.2) | 7.5 (2.3) | 1.2 (−0.0, 2.4) | 1.1 (−0.0, 2.2) | 0.7 (−0.5, 1.8) | 1.1 (−0.2, 2.3) | 0.058 | 0.057 | 0.423 | 0.118 |
| Intercourse satisfaction | 7.3 (5.6) | 8.5 (5.2) | 9.0 (4.9) | 9.0 (5.0) | 8.7 (5.0) | 1.2 (−1.6, 3.9) | 1.7 (−0.9, 4.4) | 1.7 (−0.9, 4.3) | 1.4 (−1.3, 4.1) | 0.672 | 0.308 | 0.281 | 0.531 |
| Overall satisfaction | 6.1 (2.8) | 7.0 (2.6) | 7.2 (2.8) | 7.6 (2.4) | 6.8 (2.5) | 0.9 (−0.4, 2.2) | 1.1 (−0.3, 2.4) | 1.5 (0.3, 2.7) | 0.7 (−0.6, 2.0) | 0.266 | 0.171 | 0.008 | 0.499 |
| Sex Hormone Levels | |||||||||||||
| Total testosterone, ng/dL | 317.1 (112.1) | 495.5 (185.8) | 508.7 (149.7) | 470.0 (137.7) | 432.8 (108.5) | 178.4 (99.1, 257.8) | 191.6 (121.0, 262.2) | 152.9 (84.3, 221.6) | 115.7 (52.9, 178.6) | <.001 | <.001 | <.001 | <.001 |
| Free testosterone, pg/mL | 7.7 (2.5) | 10.1 (5.4) | 8.5 (2.6) | 8.5 (3.1) | 8.0 (2.4) | 2.4 (0.0, 4.7) | 0.8 (−0.5, 2.1) | 0.7 (−0.8, 2.3) | 0.3 (−1.1, 1.7) | 0.045 | 0.361 | 0.582 | 0.963 |
| LH, miu/mL | 3.8 (3.2) | 6.3 (7.7) | 7.8 (10.4) | 6.8 (10.8) | 6.5 (8.3) | 2.5 (0.3, 4.8) | 4.0 (0.5, 7.5) | 3.0 (−0.7, 6.7) | 2.6 (−0.1, 5.4) | 0.024 | 0.024 | 0.136 | 0.063 |
| SHBG, nmol/L | 21.6 (8.1) | 60.3 (22.3) | 64.1 (19.4) | 66.6 (14.4) | 60.6 (16.0) | 38.7 (30.0, 47.4) | 42.5 (34.7, 50.3) | 45.0 (39.2, 50.9) | 39.0 (32.0, 46.1) | <.001 | <.001 | <.001 | <.001 |
Men experienced statistically significant increases in total testosterone (P < .001), free testosterone (P = 0.045), LH (P = .024) and SHBG (P < .001) at postoperative Year 1. The change in free testosterone did not remain significantly different from baseline after year 1; the change in LH remained significantly greaser at postoperative Year 2 (P = .024) but not at postoperative Year 3 or 4. The increases from baseline for total testosterone (P < .001) and SHBG (P < .001) were significant at all postoperative assessments (Table 2).
Table 2.
Percent weight loss at each time point
| n | Model-Based Estimates Mean (95% CI) |
||
|---|---|---|---|
| Year 1 | 30 | 33.3 | (36.1, 30.5) |
| Year 2 | 28 | 33.6 | (36.8, 30.5) |
| Year 3 | 30 | 31.0 | (34.1, 27.9) |
| Year 4 | 30 | 29.4 | (32.7, 26.2) |
We also were interested in the use of erectile dysfunction (ED) medications and their potential impact on changes in sexual functioning. The use of these medications was less common than anticipated. Four men reported taking (ED) medications during the course of the study. One participant reported taking ED medication at baseline, 2 participants reported taking ED medication at one follow-up visit; and 1 participant reported taking ED medication at baseline and multiple follow-up visits. The small numbers of individuals using these medications precluded formal analysis.
Psychosocial Variables
Results of the psychosocial variables of interest are found in Table 4. Participants reported statistically significant improvements in all of the physical domains of HRQoL (Physical Component Summary Score, Physical Functioning, Role Physical, Pain, and General Health) as well as the Vitality subscale from the mental health domain of the SF-36 at postoperative Years 1, 2, 3 and 4. They did not report significant changes in the Mental Component Summary Score or other mental domain subscales, except on the Social Functioning. At postoperative Years 2, 3 and 4, men reported significantly higher Social Functioning from baseline. Men also reported significant improvements in weight-related quality of life and body image. Relationship satisfaction did not change significantly from baseline at any postoperative assessment point. Depressive symptoms decreased after surgery, but the change from baseline did not reach statistical significance until Years 3 and 4.
Table 4.
Change in Psychosocial Measures
| Model Based Estimates, Mean (SD) | Model Based Mean Change (95% CI) | P-Value | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Year 1 | Year 2 | Year 3 | Year 4 | Year 1 from Baseline |
Year 2 from Baseline |
Year 3 from Baseline |
Year 4 from Baseline |
Year 1 vs Baseline |
Year 2 vs Baseline |
Year 3 vs Baseline |
Year 4 vs Baseline |
|
| SF-36 | |||||||||||||
| Physical component summary | 35.1 (9.9) | 51.9 (6.5) | 51.2 (6.8) | 50.9 (6.7) | 47.2 (7.7) | 16.9 (12.9, 20.9) | 16.1 (11.9, 20.3) | 15.8 (11.8, 19.8) | 12.1 (7.8, 16.5) | <.001 | <.001 | <.001 | <.001 |
| Mental component summary | 51.3 (9.4) | 48.0 (14.6) | 51.8 (10.2) | 51.5 (9.1) | 51.9 (7.4) | −3.3 (−9.7, 3.1) | 0.5 (−4.6, 5.6) | 0.1 (−4.4, 4.7) | 0.6 (−3.7, 4.9) | 0.511 | 0.998 | >0.99 | 0.992 |
| Physical functioning | 37.0 (10.9) | 52.2 (5.2) | 52.5 (5.3) | 51.5 (7.3) | 51.5 (5.6) | 15.2 (10.3, 20.0) | 15.5 (10.6, 20.4) | 14.5 (9.4, 19.6) | 14.4 (9.5, 19.4) | <.001 | <.001 | <.001 | <.001 |
| Role-physical | 39.5 (10.9) | 50.1 (10.0) | 52.8 (7.3) | 51.4 (8.2) | 47.3 (11.0) | 10.6 (5.1, 16.2) | 13.3 (8.2, 18.4) | 11.9 (6.8, 17.0) | 7.8 (1.7, 13.9) | <.001 | <.001 | <.001 | 0.008 |
| Pain | 39.0 (9.6) | 47.7 (12.9) | 48.4 (10.5) | 48.3 (8.9) | 44.2 (9.0) | 8.7 (3.4, 13.9) | 9.3 (4.7, 14.0) | 9.2 (5.2, 13.3) | 5.2 (0.9, 9.5) | <.001 | <.001 | <.001 | 0.011 |
| General health | 40.6 (10.4) | 54.0 (10.0) | 51.0 (9.1) | 52.0 (8.2) | 49.2 (8.2) | 13.4 (9.2, 17.6) | 10.4 (6.2, 14.5) | 11.4 (7.5, 15.2) | 8.6 (4.6, 12.6) | <.001 | <.001 | <.001 | <.001 |
| Vitality | 40.4 (9.4) | 52.3 (10.0) | 51.6 (8.8) | 52.8 (7.3) | 50.5 (7.2) | 12.0 (7.0, 17.0) | 11.3 (6.4, 16.2) | 12.4 (8.2, 16.7) | 10.1 (5.7, 14.6) | <.001 | <.001 | <.001 | <.001 |
| Social functioning | 45.3 (11.2) | 49.2 (13.0) | 52.2 (9.9) | 51.8 (9.5) | 51.1 (8.1) | 3.9 (−3.0, 10.9) | 6.9 (0.7, 13.1) | 6.5 (0.7, 12.3) | 5.8 (0.2, 11.5) | 0.416 | 0.025 | 0.024 | 0.042 |
| Role-emotional | 49.6 (9.5) | 48.2 (11.7) | 53.4 (6.8) | 50.2 (9.9) | 51.3 (9.8) | −1.4 (−7.3, 4.6) | 3.8 (−0.9, 8.5) | 0.7 (−4.7, 6.0) | 1.7 (−3.9, 7.3) | 0.942 | 0.141 | 0.995 | 0.871 |
| Mental health | 49.0 (8.1) | 48.3 (14.6) | 50.7 (9.9) | 51.2 (9.0) | 50.7 (6.5) | −0.8 (−6.6, 5.1) | 1.6 (−2.7, 6.0) | 2.1 (−1.7, 5.9) | 1.6 (−1.7, 5.0) | 0.993 | 0.778 | 0.456 | 0.587 |
| IWQOL - Lite | |||||||||||||
| Total IWQOL | 49.9 (20.0) | 91.7 (11.2) | 93.5 (11.2) | 91.7 (9.3) | 90.4 (11.2) | 41.8 (34.8, 48.9) | 43.6 (36.4, 50.8) | 41.8 (34.8, 48.9) | 40.5 (33.3, 47.7) | <.001 | <.001 | <.001 | <.001 |
| Work | 65.5 (18.5) | 94.4 (11.4) | 96.4 (14.8) | 94.0 (10.1) | 93.1 (12.9) | 28.9 (21.5, 36.3) | 30.9 (22.8, 38.9) | 28.5 (21.3, 35.8) | 27.6 (19.7, 35.6) | <.001 | <.001 | <.001 | <.001 |
| Physical function | 38.0 (21.1) | 92.0 (8.3) | 94.0 (8.0) | 90.1 (9.3) | 88.8 (11.2) | 54.0 (46.0, 62.0) | 56.0 (47.9, 64.1) | 52.0 (44.0, 60.0) | 50.7 (42.5, 59.0) | <.001 | <.001 | <.001 | <.001 |
| Public distress | 56.1 (28.9) | 94.0 (14.1) | 96.6 (10.5) | 96.6 (6.8) | 95.2 (9.7) | 37.9 (28.1, 47.7) | 40.5 (30.4, 50.7) | 40.5 (29.9, 51.0) | 39.1 (28.9, 49.3) | <.001 | <.001 | <.001 | <.001 |
| Sex life | 60.0 (37.1) | 93.7 (12.7) | 92.6 (17.6) | 92.7 (13.3) | 91.4 (15.0) | 33.7 (20.1, 47.2) | 32.5 (19.0, 46.1) | 32.7 (19.2, 46.2) | 31.4 (17.8, 45.0) | <.001 | <.001 | <.001 | <.001 |
| Self-esteem | 49.3 (30.1) | 86.7 (19.2) | 89.7 (21.0) | 88.9 (15.1) | 87.3 (17.5) | 37.4 (26.5, 48.3) | 40.4 (29.0, 51.7) | 39.6 (28.8, 50.4) | 38.0 (26.9, 49.1) | <.001 | <.001 | <.001 | <.001 |
| BIQOL | −0.3 (1.3) | 0.7 (1.4) | 0.8 (1.4) | 1.0 (1.3) | 0.7 (1.1) | 1.0 (0.3, 1.7) | 1.1 (0.4, 1.9) | 1.3 (0.6, 2.0) | 1.1 (0.4, 1.7) | 0.003 | <.001 | <.001 | <.001 |
| BSQ | 85.4 (33.3) | 55.8 (20.7) | 57.5 (23.2) | 54.2 (21.1) | 54.6 (21.1) | −29.6 (−42.3, −17.0) | −28.0 (−40.9, −15.0) | −31.2 (−43.8, −18.6) | −30.8 (−43.9, −17.7) | <.001 | <.001 | <.001 | <.001 |
| DAS | |||||||||||||
| Overall | 109.8 (17.3) | 106.6 (21.2) | 106.6 (23.3) | 111.5 (18.8) | 108.2 (18.0) | −3.2 (−10.8, 4.4) | −3.2 (−11.5, 5.2) | 1.7 (−4.9, 8.3) | −1.6 (−8.4, 5.1) | 0.706 | 0.773 | 0.926 | 0.945 |
| Consensus | 46.1 (6.4) | 45.0 (7.8) | 44.4 (10.5) | 47.5 (6.5) | 46.1 (6.4) | −1.1 (−4.5, 2.3) | −1.6 (−6.1, 2.8) | 1.4 (−1.5, 4.3) | 0.0 (−3.0, 3.1) | 0.853 | 0.795 | 0.598 | >0.99 |
| Satisfaction | 38.1 (6.3) | 37.5 (7.1) | 36.1 (10.0) | 38.3 (7.0) | 37.4 (8.2) | −0.6 (−3.0, 1.8) | −2.0 (−5.5, 1.5) | 0.2 (−2.1, 2.5) | −0.7 (−3.6, 2.1) | 0.944 | 0.434 | 0.998 | 0.923 |
| Cohesion | 15.5 (4.1) | 15.6 (4.5) | 15.5 (5.0) | 15.8 (5.4) | 14.1 (6.3) | 0.1 (−2.0, 2.1) | −0.1 (−2.4, 2.2) | 0.3 (−2.0, 2.6) | −1.5 (−4.3, 1.4) | >0.99 | >0.99 | 0.994 | 0.547 |
| Affectional expression | 8.3 (2.5) | 8.4 (2.3) | 8.3 (2.4) | 8.7 (2.4) | 8.6 (2.3) | 0.1 (−1.2, 1.3) | −0.1 (−1.4, 1.2) | 0.3 (−0.9, 1.6) | 0.2 (−1.0, 1.4) | >0.99 | >0.99 | 0.902 | 0.983 |
| BDI-I | 6.5 (5.9) | 4.1 (5.7) | 4.0 (7.1) | 2.1 (3.6) | 4.1 (5.1) | −2.4 (−5.1, 0.3) | −2.5 (−5.8, 0.9) | −4.4 (−6.9, −2.0) | −2.5 (−5.2, 0.3) | 0.103 | 0.203 | <.001 | 0.085 |
Discussion
The present study provides new information on changes in sexual functioning, sex hormones and associated domains of psychosocial functioning in men who underwent bariatric surgery. The sample of men lost approximately 30% of their weight two years after surgery, the primary endpoint, and experienced modest weight regain in years 3 and 4. These substantial weight losses were accompanied by significant increases in total as well as free testosterone, LH and SHBG at postoperative Year 1. However, only the increases in total testosterone and SHBG remained significantly improved from preoperative levels at postoperative Year 4. Contrary to expectations, men did not report significant improvements in sexual functioning on the primary measure, the IIEF. They did report significant improvements in the physical domains of HRQoL (as assessed by the SF-36), weight-related quality of life (including the Sex Life subscale), and body image. However, they did not report uniform changes in the mental health components of quality of life or satisfaction with their romantic relationships. Statistically significant changes in depressive symptoms were only seen at postoperative Year 3.
We recently found statistically significant improvements in self-reported sexual functioning in women who had lost a comparable amount of weight one and two years after bariatric surgery.25 Changes in self-reported sexual functioning for men one and two years after surgery, and as compared to baseline, were in the anticipated direction. Men reported increased sexual desire, improved erectile functioning and ejaculation, and greater satisfaction with intercourse and all sexual activity. However, the differences from baseline did not reach statistical significance.
Results of studies of changes in self-reported sexual behavior in men who have undergone bariatric surgery have been inconsistent. In a retrospective study of laparoscopic adjustable gastric banding patients, which also used the IIEF, Ranasinghe and colleagues similarly did not find statistically significant improvements in male sexual functioning.39 Our observations, as well as those by Ranasignhe and colleagues, are in contrast to studies by Reis et al21 and Mora et al40 which also used the IIEF and found statistically significant improvements in overall sexual functioning in the first two years after bariatric surgery. Review of the current results and those of Mora and colleagues suggests that we appeared to have larger variability in our self-reported sexual functioning, which may have prevented some of our changes from reaching statistical significance. The relatively small sample size also may have left us underpowered to detect statistically significance differences. Dallal and colleagues found statistically significant improvements in the sexual functioning, as assessed by the Brief Male Sexual Function Inventory, in 97 men who had undergone bariatric surgery.9 While the main LABS study has 156 men enrolled at NRI and UPMC, we were only able to recruit 32 into this study. This was an artifact of the nature of the recruitment for this ancillary study, which began after recruitment for the main study. Very few men who were ask to enroll in this study declined.
Men who underwent bariatric surgery had significant had increases in all sex hormones of interest at postoperative Year 1. These short-term results largely replicate those of Mora and colleagues.40 Changes in total testosterone and SHBG remained statistically significant from baseline through postoperative Year 4, suggesting that these improvements are durable over time. Free testosterone and LH also improved from baseline but did not remain statistically significant at postoperative Year 4. Mora and colleagues similarly found no changes in LH, but did observe statistically significant improvements in free testosterone one year after a comparable weight loss.40
Men also reported significant improvements in many, but not all, domains of psychosocial functioning following bariatric surgery. Improvements in HRQoL (predominantly the physical components assessed by the SF-36), weight-related quality of life, and body image were reported one year after surgery and remained significantly improved from baseline three years later. This is a novel contribution to the literature, as few studies have documented improvements in the psychosocial functioning of men who have undergone bariatric surgery. Men did not report statistically significant improvements on several of the “mental” domains of quality of life, assessed by the SF-36, nor did they report improvements in the domains of relationship satisfaction assessed by the DAS. This is in contrast to our study of women, which found statistically significant improvements in all domains of HRQoL and most domains of relationship satisfaction (with the exception of the Cohesion subscale of the DAS).
Despite the study’s novel contributions to the literature, the study has limitations. The small sample size is one. In addition, the sample was exclusively white and almost entirely non-Hispanic. The lack of minority representation limits our ability to comment on changes in sexual functioning, sex hormones, and psychosocial functioning in other individuals. This is an unfortunate circumstance for most of the bariatric surgical research conducted in the United States, where persons from racial and ethnic minorities present for surgery at lower rates compared to whites. We also were interested in exploring whether those individuals who had a sexual dysfunction diagnosis as baseline (primarily erectile dysfunction) reported resolution with weight loss. Unfortunately, the presence of missing data at selected assessment points, the use of ED medications in some men, and the changes sex hormones, made the results of this analysis largely impossible to interpret. Finally, it also is possible that the use of financial incentives to promote the completion of study visits could have biased the results in some manner. This is a well established practice in many areas of clinical research and without conclusive evidence that it promotes biased responding to paper and pencil assessments.
In conclusion, this study provides new information on changes in sexual functioning, sex hormones and psychosocial functioning in men who have undergone bariatric surgery. While men reported improvements in sexual functioning, these changes did not reach statistical significance. Relevant sex hormones increased significantly at postoperative Year 1 and changes in total testosterone and SHBG remained significant 4 years after surgery. Improvements in physical and weight-related quality of life, as well as body image, followed the same pattern. These results contrast with our recent investigation of women who had undergone bariatric surgery and reported consistent improvements in sexual functioning, quality of life, body image, depressive symptoms and relationship satisfaction. The psychosocial benefits that accompany the more substantial weight losses seen with bariatric surgery may be less broad and encompassing for men than for women.
Supplementary Material
Acknowledgements
Dr. Sarwer served as a paid consultant for Allergan, BariMD, BAROnova, EnteroMedics, and Ethicon Endo-Surgery, which are manufacturers of products for non-surgical weight loss treatment and bariatric surgery. At the time of the conduct of the study, he also was on the board of directors of the Surgical Review Corporation, which created the International Center of Excellence for Bariatric Surgery program to evaluate bariatric surgeons and hospitals around the world. Dr. Wadden serves on advisory boards for Novo Nordisk, Nutrisystem, and Orexigen Pharmaceuticals. Dr. Courcoulas has received research grants from Allergan, Pfizer, Covidien, EndoGastric Solutions, Nutrisystem and is on the Scientific Advisory Board of Ethicon J & J Healthcare System.
Funding/Support: This ancillary study to the Longitudinal Assessment of Bariatric Surgery-2 was funded by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) grant #R01DK072452.
Role of the Sponsor: The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) supported the study through funding and design of the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Contributions: Sarwer and Christian had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Sarwer, Wadden, Rosen, Mitchell, Courcoulas
Acquisition of data: Spitzer, Lancaster, Gourash
Analysis and interpretation of data: Sarwer, Christian
Drafting of the manuscript: Sarwer, Spitzer, Christian
Critical revision of the manuscript for important intellectual content: Sarwer, Spitzer, Wadden, Rosen, Mitchell, Lancaster, Courcoulas, Gourash, Christian
Statistical analysis: Christian
Final approval of manuscript: Sarwer, Spitzer, Wadden, Rosen, Mitchell, Lancaster, Courcoulas, Gourash, Christian
Conflict of Interest Disclosures: Dr. Mitchell, Ms. Spitzer, Ms. Lancaster, Mr. Gourash, and Dr. Christian have no relationships to disclose.
References
- 1.Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: A systematic review and meta-analysis. JAMA. 2004;292(14):1724–1737. doi: 10.1001/jama.292.14.1724. [DOI] [PubMed] [Google Scholar]
- 2.Sarwer DB, Wadden TA, Fabricatore AN. Psychosocial and behavioral aspects of bariatric surgery. Obes Res. 2005;13(4):639–648. doi: 10.1038/oby.2005.71. [DOI] [PubMed] [Google Scholar]
- 3.Moore RH, Sarwer DB, Lavenberg JA, et al. Relationship between sexual function and quality of life in obese persons seeking weight reduction. Obesity. 2013;21(10):1966–1974. doi: 10.1002/oby.20398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fabricatore AN, Wadden TA, Sarwer DB, Faith MS. Health-related quality of life and symptoms of depression in extremely obese persons seeking bariatric surgery. Obes Surg. 2005;15(3):304–309. doi: 10.1381/0960892053576578. [DOI] [PubMed] [Google Scholar]
- 5.Kolotkin RL, Crosby RD, Pendelton R, Strong M, Gress RE, Adams T. Health-related quality of life in patients seeking gastric bypass surgery vs non-treatment seeking controls. Obes Surg. 2003;13(3):371–377. doi: 10.1381/096089203765887688. [DOI] [PubMed] [Google Scholar]
- 6.Sarwer DB, Lavery M, Spitzer JC. A review of the relationship between extreme obesity, quality of life, and sexual function. Obes Surg. 2012;22(4):668–676. doi: 10.1007/s11695-012-0588-1. [DOI] [PubMed] [Google Scholar]
- 7.Wadden TA, Butryn ML, Sarwer DB, et al. Comparison of psychosocial status in treatment-seeking women with class III vs. class I–II obesity. Surg Obes Relat Dis. 2006;2(2):138–145. doi: 10.1016/j.soard.2006.03.016. [DOI] [PubMed] [Google Scholar]
- 8.Bond DS, Vithiananthan S, Leahey TM, et al. Prevalence and degree of sexual dysfunction in a sample of women seeking bariatric surgery. Surg Obes Relat Dis. 2009;5(6):698–704. doi: 10.1016/j.soard.2009.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dallal RM, Chernoff A, O'Leary MP, Smith JA, Braverman JD, Quebbemann BB. Sexual dysfunction is common in the morbidly obese male and improves after gastric bypass surgery. J Am Coll Surg. 2008;207(6):859–864. doi: 10.1016/j.jamcollsurg.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Han TS, Tajar A, O'Neill TW, et al. Impaired quality of life and sexual function in overweight and obese men: the European Male Ageing Study. Eur J Endocrinol. 2011;164(6):1003–1011. doi: 10.1530/EJE-10-1129. [DOI] [PubMed] [Google Scholar]
- 11.Kolotkin RL, Binks M, Crosby RD, Østbye T, Gress RE, Adams TD. Obesity and sexual quality of life. Obesity. 2006;14(3):472–479. doi: 10.1038/oby.2006.62. [DOI] [PubMed] [Google Scholar]
- 12.Moore RH, Sarwer DB, Lavenberg JA, et al. Relationship between sexual function and quality of life in obese persons seeking weight reduction. Obesity. 2013;21(10):1966–1974. doi: 10.1002/oby.20398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sarwer DB, Spitzer JC, Wadden TA, et al. Sexual functioning and sex hormones in persons with extreme obesity and seeking surgical and nonsurgical weight loss. Surg Obes Relat Dis. 2013;9(6):997–1007. doi: 10.1016/j.soard.2013.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hammoud AO, Walker JM, Gibson M, et al. Sleep apnea, reproductive hormones and quality of sexual life in severely obese men. Obesity. 2011;19(6):1118–1123. doi: 10.1038/oby.2010.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gosman GG, Katcher HI, Legro RS. Obesity and the role of gut and adipose hormones in female reproduction. Hum Reprod Update. 2006;12(5):585–601. doi: 10.1093/humupd/dml024. [DOI] [PubMed] [Google Scholar]
- 16.Corona G, Rastrelli G, Monani M, Saad R, Luconi M, Lucchese M, Facchiano E, Sforza A, Forti G, Mannucci E, Maggi M. Body weight loss reverts obesity-associated hypogonadotropic hypogonadism: a systematic review and meta-analsysis. Eur J Endocrinol. 2013;168(6):829–843. doi: 10.1530/EJE-12-0955. [DOI] [PubMed] [Google Scholar]
- 17.Strain GW, Zumoff B, Miller LK, Rosner W. Sex difference in the effect of obesity on 24-hour mean serum gonadotropin levels. Horm Metab Res. 2003;35(6):362–366. doi: 10.1055/s-2003-41358. [DOI] [PubMed] [Google Scholar]
- 18.Bond DS, Wing RR, Vithiananthan S, et al. Significant resolution of female sexual dysfunction after bariatric surgery. Surg Obes Relat Dis. 2011;7(1):1–7. doi: 10.1016/j.soard.2010.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aversa A, Bruzziches R, Francomano D, et al. Weight loss by multidisciplinary intervention improves endothelial and sexual function in obese fertile women. J Sex Med. 2013;10(4):1024–1033. doi: 10.1111/jsm.12069. [DOI] [PubMed] [Google Scholar]
- 20.Wing RR, Bond DS, Gendrano IN, et al. Effect of intensive lifestyle intervention on sexual dysfunction in women with type 2 diabetes: results from an ancillary Look AHEAD study. Diabetes Care. 2013;36(10):2937–2944. doi: 10.2337/dc13-0315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reis LO, Favaro WJ, Barreiro GC, de Oliveira LC, Chaim EA, Fregonesi A, Ferreira U. Erectile dysfunction and hormonal imbalance in morbidly obese male is reversed after gastric bypass surgery: A prospective randomized controlled trial. Int J Androl. 2010;33(5):736–744. doi: 10.1111/j.1365-2605.2009.01017.x. [DOI] [PubMed] [Google Scholar]
- 22.Hammoud A, Gibson M, Hunt SC, et al. Effect of Roux-en-Y gastric bypass surgery on the sex steroids and quality of life in obese men. J Clin Endocrinol Metab. 2009;94(4):1329–1332. doi: 10.1210/jc.2008-1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaukua J, Pekkarinen T, Sane T, Mustajoki P. Sex hormones and sexual function in obese men losing weight. Obes Res. 2003;11(6):689–694. doi: 10.1038/oby.2003.98. [DOI] [PubMed] [Google Scholar]
- 24.Turcato E, Zamboni M, De Pergola G, et al. Interrelationships between weight loss, body fat distribution and sex hormones in pre- and postmenopausal obese women. J Intern Med. 1997;241(5):363–372. doi: 10.1046/j.1365-2796.1997.120129000.x. [DOI] [PubMed] [Google Scholar]
- 25.Sarwer DB, Spitzer JC, Wadden TA, et al. Changes in sexual functioning and sex hormone levels in women following bariatric surgery. JAMA Surg. 2014;149(1):26–33. doi: 10.1001/jamasurg.2013.5022. [DOI] [PubMed] [Google Scholar]
- 26.Belle SH, Berk PD, Courcoulas AP, et al. Safety and efficacy of bariatric surgery: Longitudinal Assessment of Bariatric Surgery. Surg Obes Relat Dis. 2007;3(2):116–126. doi: 10.1016/j.soard.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Belle SH, Berk PD, Chapman WH, et al. Baseline characteristics of participants in the Longitudinal Assessment of Bariatric Surgery-2 (LABS-2) study [published online ahead of print March 7, 2013] Surg Obes Relat Dis. doi: 10.1016/j.soard.2013.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Longitudinal Assessment of Bariatric Surgery (LABS) Consortium. Flum DR, Belle SH, et al. Perioperative safety in the longitudinal assessment of bariatric surgery. NEJM. 2009;361(5):445–454. doi: 10.1056/NEJMoa0901836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Courcoulas AP, Christian NJ, Belle SH, et al. Three Year Weight and Health Outcomes in the Longitudinal Assessment of Bariatric Surgery (LABS) Consortium. JAMA. 2013;310(22):2416–2425. doi: 10.1001/jama.2013.280928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49(6):822–830. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 31.Cappelleri JC, Rosen RC, Smith MD, Mishra A, Osterloh IH. Diagnostic evaluation of the erectile function domain of the International Index of Erectile Function. Urology. 1999;54(2):346–351. doi: 10.1016/s0090-4295(99)00099-0. [DOI] [PubMed] [Google Scholar]
- 32.Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 health survey manual and interpretation guide. Boston: New England Medical Center, The Health Institute; 1993. [Google Scholar]
- 33.Kolotkin RL, Head S, Hamilton M, Tse CJ. Assessing the impact of weight on the quality of life. Obes Res. 1995;3(1):49–56. doi: 10.1002/j.1550-8528.1995.tb00120.x. [DOI] [PubMed] [Google Scholar]
- 34.Kolotkin RL, Crosby RD, Kosloski KD, Williams GR. Development of a brief measure to assess quality of life in obesity. Obes Res. 2001;9(2):102–111. doi: 10.1038/oby.2001.13. [DOI] [PubMed] [Google Scholar]
- 35.Cash TF, Fleming EC. The impact of body-image experiences: Development of the Body Image Quality of Life Inventory. Int J Eat Disord. 2002;31(4):455–460. doi: 10.1002/eat.10033. [DOI] [PubMed] [Google Scholar]
- 36.Cooper PJ, Taylor MJ, Cooper Z, Fairburn CG. The development and validation of the body shape questionnaire. Int J Eat Disord. 1987;6:485–494. [Google Scholar]
- 37.Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. J Marital Fam Ther. 1976;38(2):15–38. [Google Scholar]
- 38.Beck AT, Steer RA, Brown GK. Beck depression inventory II (BDI-II) manual. San Antonio: Harcourt Brace; 1993. [Google Scholar]
- 39.Ranasinghe WK, Wright T, Attia J, et al. Effects of bariatric surgery on urinary and sexual function. BJU Int. 2011;107(1):88–94. doi: 10.1111/j.1464-410X.2010.09509.x. [DOI] [PubMed] [Google Scholar]
- 40.Mora M, Aranda GB, de Hollanda A, Flores L, Puig-Domingo M, Vidal J. Weight loss is a major contributor to improved sexual function after bariatric surgery. Surg Endosc. 2013;27(9):3197–3204. doi: 10.1007/s00464-013-2890-y. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.