Abstract
Objectives:
This report provides analyses and perspective of a survey of critical care workforce, workload, and burnout among the intensivists and advanced practice providers (APPs) of established United States and Canadian critical care organizations (CCOs) and provides a research agenda.
Design:
A 97-item electronic survey questionnaire was distributed to the leaders of 27 qualifying organizations.
Participants:
Leaders of CCOs in the United States and Canada.
Data Synthesis and Main Results:
We received 23 responses (85%). The CCO survey recorded substantial variability of most organizational aspects that were not restricted by the CCO definition or regulatory mandates. The most common physician staffing model was a combination of full time and part time intensivists. Approximately 80% of CCOs had dedicated APPs that staffed some or all their ICUs. Full-time intensivists worked a median of 168 (range 42–192) days in the ICU (168 shifts = 24 7-day weeks). The median shift duration was 12 hours (range 7 −14) and the median number of consecutive shifts allowed was 7 (range 7–14). More than half of CCOs reported having burnout prevention programs targeted to ICU physicians, APPs, and nurses.
Conclusions:
The variability of current approaches suggests that systematic comparative analyses could identify best organizational practices. The research agenda for the study of CCOs should include studies that provide insights regarding the effects of the integrative structure of CCOs on outcomes at the levels of our patients, our workforce, our work practices, and sustainability.
Keywords: Critical Care Organization, Burnout Syndrome, Critical Care, ICU Management, Workforce, Work Environment
Introduction
The Society of Critical Care Medicine (SCCM) convened a taskforce of Academic Leaders in Critical Care Medicine (ALCCM) to develop a series of consensus articles with toolkits for advancing critical care organizations (CCOs). (1–3) We defined CCOs as organizations that have an advanced governance structure headed by an intensivist physician that has primary governance over the majority, if not all, of the ICUs and critical care operations of the healthcare organization or medical center. (4) CCOs serve health care organizations by providing physician-led primary governance for most of the organization’s intensive care units (ICU). The articles of this series have defined the vertical (relation to institutional leaders) and horizontal (interdepartmental) integration of critical care delivery for health care organizations and the methods by which CCOs promote patient safety, high quality care, research, education, and professional development. A third article presented a narrative review of the issues related to the critical care workforce, workload, and burnout syndrome (BOS) among intensivists and APPs and identified that the lack of published data about CCOs limits our ability to design a CCO research agenda. (3) The ALCCM group designed and SCCM supported the development of a 97-item survey to gather foundational facts about CCOs from the leaders of 27 functioning CCOs. The items of the survey provide information about CCO structure, workforce, work environment, and records the diversity of their intensivists. The main aim of the presentation of its analyses and results is to encourage research that fills emerging gaps on our knowledge of critical care organizational structure by defining a research agenda.
Methods
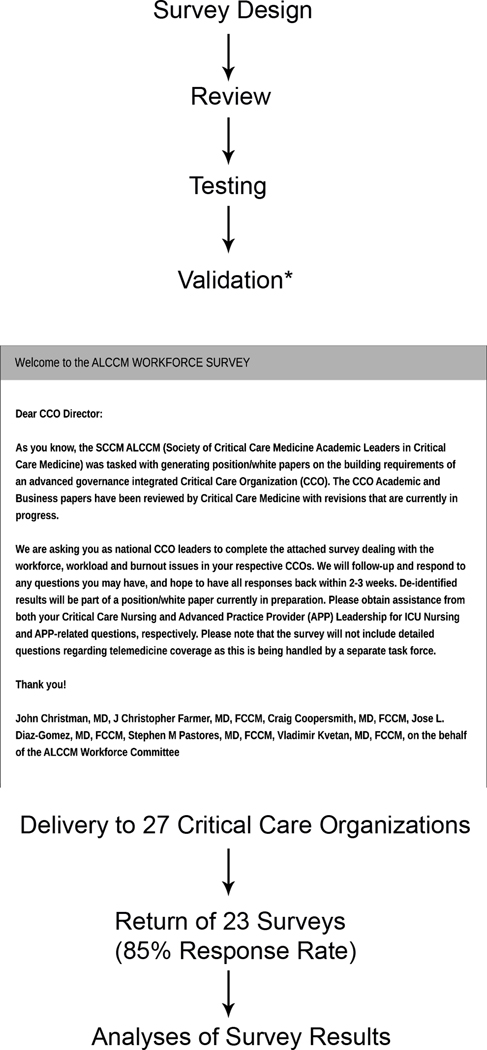
The leaders of CCOs were contacted after identification from web searches for content containing the terms “Critical Care or Intensive Care Department, Center, System, Institute, Operations Committee, Service or Product Line or Hospital” performed in April 2014. These CCO leaders provided contact information for other centers that might have also met the prespecified CCO definition; in all 37 potential CCOs provided descriptions of their structure. Twenty-seven health care organizations; 23 in the United States and 4 Canadian, met the prespecified CCO definition above. A 97-item survey instrument was developed for delivery on the Survey Monkey platform that captured structural, workforce, and burnout domain information using the processes presented in Figure 1. After validation by previously described methods including comparison to objectively measured workplace metrics and pilot testing, (5) the survey was deployed. The leaders of the institutions with CCOs presented in italic font in Table 1 were invited on behalf of the ALCCM by John W. Christman, MD, J Christopher Farmer, MD, FCCM, Craig Coopersmith, MD, FCCM, Jose L. Diaz-Gomez, MD, FCCM, Stephen M Pastores, MD, FCCM, and Vladimir Kvetan, MD, FCCM, to participate in the survey without compensation. Strength of association was measured by cubic regression.
Figure 1.
Process diagram of the development, validation, and deployment of the CCO survey. Development, validation, and analytical details are presented in the methods section.
Table 1.
North American Critical Care Organizations*
| Brooklyn Hospital Center | Cleveland Clinic** | Cooper Health System | Emory University |
|---|---|---|---|
| Geisinger Medical Center | Mayo Clinic Jacksonville | Mayo Clinic Phoenix | Mayo Clinic Rochester |
| MD Anderson Cancer Center | Medstar Washington Hospital | Memorial Sloan Kettering Cancer Center | Mercy Hospital |
| Montefiore Medical Center | Mount Sinai Medical Center | National Institutes of Health Clinical Center | Ohio State University |
| St. Michaels Hospital Toronto, Canada | Sunnybrook Health Sciences Center Toronto, Canada | The Hospital for Sick Children Toronto, Canada | UH Cleveland Medical Center |
| UMass Memorial Medical Center | University of Alberta Edmonton, Canada | University of Calgary Canada | University of Maryland |
| University of Minnesota | University of Mississippi | University of New Mexico Health Sciences Center | University of Pittsburgh |
| University of Southern California | Virginia Commonwealth University |
All of the CCOs that were invited to participate in the survey are presented in italic font.
The Cleveland Clinic has 2 CCOs.
Monthly email reminders were sent to non-responders who were also contacted by phone to confirm that they had received the invitation. The structure of the survey platform allowed only one consensus response from each CCO and reported only site-deidentified data. In all, 23 of the 27 (85%) institutions initially invited on July 12, 2017 completed the survey by May 30, 2019. The 97-item survey is provided as an electronic supplement. The survey was conceived, created, and refined by the SCCM ALCCM Task Force in the context of its charge to provide current and actionable information on the state of the critical care workforce to the SCCM. Survey data informed SCCM leaders and task force members with research expertise in support of an iterative process to develop an expert opinion-based research agenda.
Survey Results
The overall response rate was 85% (23/27). Results stratified by survey domain are presented for 80 of the 97 survey items. Items were not included when the information was nearly identical to that presented for a similar item. For example, the exclusion of the response pattern for part-time physicians was not included because it was nearly identical to that of full-time physicians. Items with non-meaningful numbers of responses, e.g., starting salaries, and free text only items were excluded.
CCO Characteristics
The adoption of the CCO model does not appear to be restricted to institutions of large size as some institutions with as few as two ICUs at their main institution have implemented a CCO. CCO leaders reported that the number of ICU, stepdown or progressive care beds at the main institution covered by their CCOs ranged from 18 to 400 (mean 123.5, median 95, interquartile range [IQR] 60 to 139). The number of CCO covered beds at affiliated hospitals ranged from 0 to 235 (mean 57, median 95, IQR 0 to 100). CCOs reported that 68% of the beds that they administered were located at their main institution.
Most leaders reported that their CCOs support a variety of specialty dedicated ICUs with only a single CCO using a uniform ICU type model (mixed ICU e.g., medical-surgical). The median number of different specialty unit types (not counting mixed ICUs) that CCOs governed was 4 (mean 4.5, range 0 to 9, IQR 3 to 6). The rank order frequency of reported ICU bed types were medical, other (unspecified), surgical, cardiothoracic, neurosciences, cardiac, pediatric, transplant, trauma, and burn beds.
The majority of senior leadership positions for the institutions that have adopted CCOs are held by physicians. The CEO is a physician for 11 and a non-physician for 8 CCOs of the 19 CCOs that responded to this item. The College of Medicine Dean is a physician for all 17 reporting institutions, the President is a physician for 12 and is a non-physician for 7 of 19 responding institutions, and the Chief Medical Officer is a physician for 21 and a non-physician for a single institution. In addition to a CCO leader, 17 of 22 reporting CCOs had directors for department-based critical care service lines. All 23 CCOs reported that they have a dedicated Medical Director for each of their medical center ICUs, 11 CCOs report also supporting Associate ICU Directors, and one CCO reported that some of their rural hospital ICUs did not have a dedicated medical director. All 23 CCOs reported participating in regularly scheduled intra-organizational and interdepartmental meetings.
Regularly scheduled staff surveys were used to solicit provider input by 22 of 23 CCOs. Periodic retreats that provided a forum for interactive discussion and teambuilding were used by 11 of 23 CCOs. The atmosphere or culture of critical care was rated by CCO leaders as an 82 ± 12 mean and standard deviation (SD) with a range of 59 to 100 on a 0 to 100 (more positive) scale.
Critical Care Organization Physicians and Clinical Staff
Workforce characteristics of the physicians and clinical staff of the CCOs is presented in Table 2.
Table 2.
CCO Workforce Characteristics.
| All Physicians | |||
|---|---|---|---|
| Number of Members | 41, [22–60] median, [IQR] | Range (9–118) | |
| Years of Service1 | 8, [5–10] median, [IQR] | Range (0–36) | |
| Age (years) | 34% were < 40 | 73% were <50 | 91% were <60 |
| Full Time Critical Care Physicians by Specialty | |||
| Internal Medicine | 57% | ||
| Anesthesiology | 15% | ||
| Neurosciences | 10% | ||
| Surgery | 8% | ||
| Emergency Medicine | 5% | ||
| Pediatrics | 3% | ||
| Cardiology | 2% | ||
| Advanced Practice Providers2 | |||
| Number of Members | 23, [10–40] median, [IQR] | Range (0–108) | |
| Years of Service | [IQR] 5, [4.7–7] median, | Range (0–35) | |
| Unfilled Positions | 1, [0–3] median, [IQR] | Range (0–11) | |
| Clinical Staff | |||
| All ICUs | Some ICUs | Not used | |
| Nurse Specialists | 12 | 9 | 2 |
| Nurse Administrator | 18 | 4 | 1 |
| Pharmacist3 | 12 | 10 | 1 |
| Respiratory Therapist3 | 17 | 6 | 0 |
| Nutritional Specialist3 | 14 | 7 | 2 |
| Rehabilitation Therapist3 | 9 | 10 | 4 |
| ECMO Perfusionist3 | 5 | 15 | 4 |
| Care Cordinator3 | 8 | 12 | 3 |
| Social Worker3 | 14 | 7 | 2 |
| Chaplain3,4 | 11 | 3 | 9 |
The years of service was not meaningfully different for programs that offered service duration-based accommodations and those that did not.
1 CCO reported that it did not use ICU Advanced Practice Providers.
The survey item used the term dedicated. IQR is interquartile range.
Religion based support staff. IQR: interquartile range.
Physicians
The survey asked the leaders of CCOs to share their institutions definition of a of a full-time critical care physician. Forty four percent of the respondents indicated that full time at their institution was defined as more than 50%, 30% defined it as more than 80%, and 26% defined it as 100% effort spent in CCO related clinical, education, research, or administrative activities. There is also substantial variation of the number of physicians that CCOs employ. Group size ranged from 9 to 118 physicians that their institution classified as full or part time with a median of 41 and an IQR of 22 to 60. The majority of physicians were classified as full time with part-time physicians ranging from 0 to 38 individuals and per diem physicians ranging from 0 to 7 individuals.
Advanced Practice Providers
The APPs of 21 programs reported working on weekends and 18 indicated that their APPs worked overnight. Graduated experience-based and revenue-based compensation models for APPs were reported by 3 each of the 21 CCOs. The APPs of 4 CCOs could be awarded an academic rank. The reported range of annual vacation time was 4 −6 weeks. Professional training was offered by 17 of 18 responding CCOs and 18 provided funding for medical education. An APP Training program was supported by 10 of the 21 CCOs.
Critical Care Workload
The majority of CCOs assign their intensivists responsibilities that are not related to direct care of their ICU patients at the same time that they are signed in as responsible for the patients of their ICUs. These additional activities include performing consultations, leading cardiac arrest or rapid response teams, performing operative procedures, performing bedside procedures, providing ICU telemedicine evaluation and management services, providing outpatient services, or managing stepdown unit patients. The physicians of 14 CCOs have responsibilities outside of their ICUs and the intensivists of 9 CCOs provide services only in their ICUs during weekdays. Many CCOs expand coverage responsibility off-hours with only 5 CCO’s intensivists providing only ICU services during weeknights, 3 during weekend days, and 2 during weekend nights. A shortage of ICU physicians was reported by 6 of 23 responding CCOs. The range of unfilled intensivist positions was 2 to 3 with no CCOs reporting single vacancies. The average 5-year attending intensivist attrition rate was 9.5 ± 6 (SD) %.
The number of ICU beds covered by the CCO to the number of attending physician FTE ratios ranged from 0.7 to 10 with a median of 2.5 (IQR 1.7 to 4) and a mean of 3.1 ± 2 (SD). The number of patients a CCO attending physician covers during a weekday ranged from 8 to 30 with a median of 13.5 (IQR 11.5 to 16.5) and a mean of 15 ± 5 (SD) patients. Patient to physician ratios are higher after hours and on weekends. Attending physicians of all CCOs were supported by residents, fellows, and APPs; however, 2 CCOs reported that attending physicians worked alone in some of their ICUs. The attending physicians of all CCOs were available at night either using an in-house call system for some (10 CCOs) or all (7 CCOs) ICUs, or a model in which off-duty staff are called in to the hospital on demand (6 CCOs all ICUs; 10 CCOs some ICUs).
The number of annual shifts worked by a full-time clinical faculty member ranged from 42 to 192 with a mean of 156 ± 43 (SD) and a median of 168 with an IQR of 143 to 186 (168 shifts corresponds to 24 7-day weeks). Shift duration was reported to range from 9 to 14 hours, with a median of 12 with an IQR of 10 to 12 and a mean of 11 ± 1.5 (SD) hours. All CCOs limited the number of consecutive shifts that could be worked without a 24 hour no service interval. The range of consecutive shifts allowed was 1 to 14, with a median of 7 with an IQR of 5 to 7 and a mean of 6 ± 1.2 (SD) days. The number of consecutive night shifts allowed was lower with only 2 CCOs allowing more than 6 consecutive night shifts. The annual number of weekends worked by attending physicians ranged from 6 to 20 with a median of 12 with an IQR of 10 to 15 and a mean of 13 ± 3.3 (SD) days. The range of protected time offered by 13 responding CCOs was 0 to 50% with a mean and median of 20%. Vacation time per years of service (queried in 5 year increments from 0 to 29 and > 30) ranged from 3 to 7 weeks with a median of 4.5 and an IQR of 4 to 5 for faculty with less than 15 years of service and ranged from 3.5 to 7.5 weeks with a median of 5.5 and an IQR of 4 to 6 weeks for those with more than 15 years of service.
CCO leaders rated the work life balance of their critical care physicians at a 64 ± 24 (SD) on a scale of 0 to 100 (higher indicates better balance) with a range of 15 to 99.
The leaders of all CCOs reported high default nurse to patient ratios with 14 CCOs reporting 1:2 ratios, 2 reporting 1:1 ratios and 2 reporting 1:1 or 1:2 ratios for their ICUs. CCOs that were able to provide 1:1 ratios listed complex device management (CVVH, ECMO, IABP, LVAD), post cardiac surgery ICU arrival, severe burn care, and physiological instability as the indications. The range of the number of available ICU nurse positions was 1 to 70 among the 6 CCOs that reported unfilled job postings.(6)
Burnout and Well-being
Programs to address burnout and promote well-being are available at 19 of the 23 reporting CCOs. The hospital is the sole program sponsor for 14 programs, CCOs and hospitals both provide programs at 4 sites, the medical school and practice plan provide the program at one site and support is not provided at 4 sites. The burnout prevention programs of 14 of 18 responding institutions were targeted to ICU physicians, APPs, and nurses, the programs of 2 institutions focused on physicians and nurses, and 2 programs were physician supporting. Respondents identified 15 of the 19 programs as being resilience based.(7)
The difference between the average Do Not Resuscitate (DNR) rate at ICU admission of 10% and the DNR rate of 75% at time of death in the ICU, suggests that a substantial portion of the end-of-life care and support is provided by CCO providers. All CCOs reported that palliative care consultation services were available.
Discussion
The survey results provide an objective cross-sectional view of the CCO workforce, its members, their workplaces, and workload. One theme of the survey results is the diversity and variability of most parameters that are not restricted by the CCO inclusion criteria or regulatory mandates.(1) The extent of the variation of operational methods suggests that few aspects of organizational approach (e.g., granular aspects of business, clinical, education, and research structures), are so effective that they have been universally adopted. We believe that the lack of established methods and resources to collect, protect, and share reliable information about CCOs has impeded our ability to provide evidence-based guidance regarding optimal CCO organizational characteristics. The development of the CCO survey instrument and information from its initial deployment form the foundational element of a CCO knowledge base, that with development, can be used to inform operational decisions and identify research opportunities.
Another prominent theme of the survey findings is that the workload of the intensivists of most CCOs is near the sustainable capacity of many of their attending physicians.(3, 8–13) The survey reported that most attending physicians managed workload with the help of other providers rather than by working as a lone physician. (14) The finding that nearly all CCOs placed limits on the number consecutive shifts that physicians could work, without a 24-hour break, appeared to acknowledge that their workloads are not sustainable. Non-sustainable workload is also suggested by the substantial gap between the number of shifts worked and available non-vacation shifts and the number of CCOs that provided protected, educational, or administrative time. Survey items that document that the ages of practicing intensivists are skewed to younger physicians and to shorter durations of service suggest that they may be leaving the ICU workforce due to burnout syndrome (BOS). Recent reports suggest that healthcare systems are modifying workload to improve retention.(15) Concern that excessive workload increased risk for BOS (10) is implied by the number of institutions that offered programs to improve well-being including resilience (7, 16, 17) and teamwork and team dynamics based (18) counter measures and the fact that some CCOs provided their own BOS programs.
The survey methodology used in this report has important limitations. Key limitations include not including leaders of institutions that do not use the CCO governance as a comparator group and not capturing outcome or patient level data. The instrument was not designed to provide insights into the reasons that institutions elected to form CCOs or about their value proposition relative to alternative organizational schemas.
The size, extent, and effort required to establish the United States and Canadian CCOs of this report suggest that their importance is sufficient to merit a research agenda.(1) The institutional leaders that created these structures that cross traditional organizational boundaries did so with the belief that the financial, service delivery, workforce retention, or patient safety benefits would justify the resources they invested. The research questions, presented in Table 3, allowed current SCCM leaders and experts from the ALCCM Taskforce to define patient, workforce, workflow, and outcome agenda topics that were suggested after analysis of the survey responses from concurrent CCO leaders. The aim of the task force was to provide a non-exhaustive list of consensus topical areas of current interest for active study. The consensus topical areas presented by survey domain in Table 3 should not discourage research into new, evolving, or other important issues that face our growing numbers of critical care organizations.
Table 3.
CCO Research Questions by Survey Domain
| Workforce |
| Are CCOs able to meet the workforce needs of the organizations that they serve better than alternative governance models? |
| Can organizations that have adopted a CCO governance structure more rapidly adapt care delivery processes to changing external demands than those using other models? |
| Are the number or focus of institution-wide processes of care delivery changes of CCO led institution different than institutions with other governance models? |
| Do disease stratified patients of institutions that use the CCO model to standardize care for their specific diseases have better outcomes than organizations that do not use the CCO model to standardize care? |
| Are the institutional total costs of ownership for CCO led institutions higher or lower than those of institutions without CCO governance? |
| Workload |
| Is the mission of academic physicians better supported by the CCO model than by alternative organizational structures? |
| Are organizations with CCOs better able to standardize the delivery of critical care services than those using other models? |
| Do institutions that use the CCO model have less variability of the devices that are required to deliver critical care than institutions that do not use CCO governance? |
| Burnout Well Being |
| Does the CCO governance structure attract providers that as a group achieve better patient level outcomes than other models? |
| Does the CCO governance structure provide better work life balance than alternative models? |
Advancing this research agenda will require the collection, protection, and sharing of information across CCOs (19) and with institutions that use other critical care governance models. The creation of the ALCCM group by the SCCM, its generous support of the development of a validated survey instrument and its deployment represent important advances toward an evidence-based understanding of critical care governance.
Acknowledgments
Financial Support: None
Copyright form disclosure: Dr. Lilly received support for article research from the National Institutes of Health. Dr. Pastores received funding from McGraw Hill Publishers (royalties) and Cleveland Clinic (Grand Rounds speaker). The remaining authors have disclosed that they do not have any potential conflicts of interest.
Acronym list:
- ALCCM
Academic Leaders in Critical Care Medicine
- BOS
burnout syndrome
- CEO
Chief Executive Officer
- CCOs
critical care organization
- CVVH
continuos veno-venous hemodialysis
- ECMO
extracorporeal membrane oxygenation
- IABP
intra-aortic balloon pump
- IQR
inter quartile range
- LVAD
left ventricular assist device
- SCCM
Society of Critical Care Medicine
Footnotes
Academic Leaders in Critical Care Medicine Task Force (Workforce Subgroup): John W. Christman, MD, The Ohio State University Wexner Medical Center, Columbus, OH; Craig M. Coopersmith, MD, FACS, FCCM, Emory Critical Care, Atlanta, GA; J. Christopher Farmer, MD, FCCM, Mayo Clinic, Scottsdale, AZ; Curtis Sessler, MD, FCCP, FCCM, Virginia Commonwealth University, Richmond, VA; Rhonda D’Agostino, ACNP, FCCP, FCCM, Memorial Sloan Kettering Cancer Center, New York, NY; Jose Diaz-Gomez, MD, FCCM, Miami, FL; Sara R. Gregg, MHA, Emory Critical Care, Atlanta, GA; Roozehra A Khan, DO, University of Southern California, Los Angeles, CA; April N Kapu, ACNP-BC, Vanderbilt University Medical Center, Nashville, TN; Sharon Leung, MD, Montefiore Medical Center, Bronx, NY; Craig M. Lilly, MD, FCCM, University of Massachusetts Medical School, Worcester, MA; Henry Masur, MD, MCCM, National Institutes of Health Clinical Center, Bethesda, MD; Gargi Mehta, PA-C, MSHS, Montefiore Medical Center, Bronx, NY; Jason Moore, MD, University of Pittsburgh Medical Center, Pittsburgh, PA; John M. Oropello, MD, FACP, FCCP, FCCM, Mount Sinai Medical Center, New York, NY; and Kristen Price, MD, MD Anderson Cancer Center, Houston, TX.
Disclosures: The authors report that they are leaders of Critical Care Organizations and have no financial conflict of interest related to the content of this manuscript.
References
- 1.Leung S, Gregg SR, Coopersmith CM, et al. Critical Care Organizations: Business of Critical Care and Value/Performance Building. Crit Care Med 2018;46(1):1–11. [DOI] [PubMed] [Google Scholar]
- 2.Moore JE, Oropello JM, Stoltzfus D, et al. Critical Care Organizations: Building and Integrating Academic Programs. Crit Care Med 2018;46(4):e334–e341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pastores SM, Kvetan V, Coopersmith CM, et al. Workforce, Workload, and Burnout Among Intensivists and Advanced Practice Providers: A Narrative Review. Crit Care Med 2019;47(4):550–557. [DOI] [PubMed] [Google Scholar]
- 4.Pastores SM, Halpern NA, Oropello JM, et al. Critical Care Organizations in Academic Medical Centers in North America: A Descriptive Report. Crit Care Med 2015;43(10):2239–2244. [DOI] [PubMed] [Google Scholar]
- 5.Lilly CM, Fisher KA, Ries M, et al. A national ICU telemedicine survey: validation and results. Chest 2012;142(1):40–47. [DOI] [PubMed] [Google Scholar]
- 6.Chan ZC, Tam WS, Lung MK, et al. A systematic literature review of nurse shortage and the intention to leave. J Nurs Manag 2013;21(4):605–613. [DOI] [PubMed] [Google Scholar]
- 7.Shanafelt T, Trockel M, Ripp J, et al. Building a Program on Well-Being: Key Design Considerations to Meet the Unique Needs of Each Organization. Acad Med 2019;94(2):156–161. [DOI] [PubMed] [Google Scholar]
- 8.Shanafelt TD, Sinsky C, Dyrbye LN, et al. Burnout Among Physicians Compared With Individuals With a Professional or Doctoral Degree in a Field Outside of Medicine. Mayo Clin Proc 2019;94(3):549–551. [DOI] [PubMed] [Google Scholar]
- 9.Moss M, Good VS, Gozal D, et al. An Official Critical Care Societies Collaborative Statement-Burnout Syndrome in Critical Care Health-care Professionals: A Call for Action. Chest 2016;150(1):17–26. [DOI] [PubMed] [Google Scholar]
- 10.Mealer M, Moss M, Good V, et al. What is Burnout Syndrome (BOS)? Am J Respir Crit Care Med 2016;194(1):P1–2. [DOI] [PubMed] [Google Scholar]
- 11.Ward NS, Afessa B, Kleinpell R, et al. Intensivist/patient ratios in closed ICUs: a statement from the Society of Critical Care Medicine Taskforce on ICU Staffing. Crit Care Med 2013;41(2):638–645. [DOI] [PubMed] [Google Scholar]
- 12.Peckham C. Medscape National Physician Burnout & Depression Report 2018. Medscape 2018. Available from: https://www.medscape.com/slideshow/2018-lifestyle-burnout-depression-6009235#3 [Google Scholar]
- 13.Vandevala T, Pavey L, Chelidoni O, et al. Psychological rumination and recovery from work in intensive care professionals: associations with stress, burnout, depression and health. Journal of intensive care 2017;5:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lilly CM, Cucchi E, Marshall N, et al. Battling Intensivist Burnout: a role for Workload Management. Chest 2019. [DOI] [PubMed] [Google Scholar]
- 15.Mikkelsen ME, Anderson BJ, Bellini L, et al. Burnout, and Fulfillment, in the Profession of Critical Care Medicine. Am J Respir Crit Care Med 2019;200(7):931–933. [DOI] [PubMed] [Google Scholar]
- 16.Tawfik DS, Sexton JB, Adair KC, et al. Context in Quality of Care: Improving Teamwork and Resilience. Clinics in perinatology 2017;44(3):541–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee KJ, Forbes ML, Lukasiewicz GJ, et al. Promoting Staff Resilience in the Pediatric Intensive Care Unit. Am J Crit Care 2015;24(5):422–430. [DOI] [PubMed] [Google Scholar]
- 18.Maslach C, Leiter MP. New insights into burnout and health care: Strategies for improving civility and alleviating burnout. Medical teacher 2017;39(2):160–163. [DOI] [PubMed] [Google Scholar]
- 19.Phan-Vogtmann LA, Helhorn A, Kruse HM, et al. Approaching Clinical Data Transformation from Disparate Healthcare IT Systems Through a Modular Framework. Stud Health Technol Inform 2019;258:85–89. [PubMed] [Google Scholar]