Abstract
Background:
Screening and timely follow-up have lowered cervical cancer incidence in the US; however, screening coverage, incidence, and death rates have remained fairly stable in recent years. Studies suggest that half of women diagnosed with cervical cancer don’t receive appropriate screening prior to diagnosis; cervical cancer survivors can provide crucial insight into barriers and facilitators to screening.
Methods:
Participants were cervical cancer survivors ≥21 years, identified through population-based central cancer registries (CR) in 3 US states or a social network (SN), Cervivor. CR participants completed a mailed survey on screening history, barriers, and facilitators to screening and sociodemographic data. SN participants completed the same survey online.
Results:
CR participants (N = 480) were older, with a lower proportion of non-Hispanic white, married, and insured women compared to SN participants (N = 148). Fifty percent of CR and 79% of SN participants were screened 5 years prior to their diagnoses. Of those screened, 28% in both groups reported not following-up on abnormal results. For both groups, the most frequently identified screening barrier was that participants never imagined they would develop cervical cancer (percent agree CR = 76%; SN = 86%), and the facilitator was wanting to take care of their bodies (CR = 95%; SN = 94%).
Conclusion:
Addressing key barriers to obtaining screening and timely follow-up related to lack of knowledge of cervical cancer risk and screening tests and addressing insurance coverage in the design or modification of interventions may increase cervical cancer screening and lower cervical cancer incidence in the US.
Keywords: cervical cancer screening, barriers, facilitators, cervical cancer survivors, cancer registries
Introduction
Cervical cancer screening and timely follow-up of cervical precancers have been effective in drastically reducing the cervical cancer incidence in the United States (US) for over 50 years.1 However, national estimates of cervical cancer screening coverage have remained fairly stable in recent years, at 84.5% in 2008 and 81.2% in 2015.2,3 National cervical cancer incidence rates have shown modest reductions but death rates have remained stable.4 Previous studies among women diagnosed with cervical cancer have shown that approximately half of them did not get the appropriate screening prior to their diagnoses.5,6 Cervical cancer survivors can provide insight into the barriers and facilitators to screening prior to their diagnoses to inform interventions aimed at increasing screening coverage and reducing cervical cancer incidence.
Several studies have been conducted to examine the barriers and facilitators to cervical cancer screening, particularly in populations of women with lower cervical cancer screening coverage such as Asian, Hispanic, immigrant, low-income, and uninsured women.7-10 These studies describe several barriers to cervical cancer screening including: the lack of cervical cancer knowledge, lack of insurance, recent or undocumented immigration status, lack of interpreter services, and sociocultural beliefs. Facilitators to screening identified from previous studies include knowledge of cervical cancer and the importance of screening, physician recommendation, access to culturally relevant education, and having access to regular care. Examining screening barriers and facilitators among cervical cancer survivors provides an additional lens through which to understand these previously identified barriers and facilitators to cervical cancer screening.
The Case Investigation of Cervical Cancer (CICC) study is a population-based study of cervical cancer survivors that examined screening coverage as well as barriers and facilitators to cervical cancer screening in these women.11 The findings from the CICC study on barriers and facilitators to cervical cancer screening are described in this manuscript. This information can be used to design or modify interventions to increase screening and reduce cervical cancer incidence and deaths in US women.
Materials and Methods
Participants were cervical cancer survivors identified in 2 ways: (1) through central cancer registries (CR) in 3 US states, Louisiana, Michigan, and New Jersey; and, (2) through a social network (SN) for cervical cancer survivors. Details of the study methods and enrollment of women identified through cancer registries have been previously described elsewhere.11 Briefly, cervical cancer survivors ≥21 years old who were diagnosed with invasive cervical cancer between 2014 and 2016 in Michigan and New Jersey, and between 2013 and 2016 in Louisiana were selected to participate in the study. A questionnaire was mailed to women who were not known to be deceased and for whom an address could be identified. Outreach was conducted between June 2017 and May 2018. Surveys were available in English and Spanish.
To supplement the participants identified through the cancer registries, outreach was conducted between September 2018 and January 2019 to identify a convenience sample of women through a social network of cervical cancer survivors (Cervivor; https://cervivor.org/). An invitation to participate in an online survey was shared by leadership at Cervivor via (1) email to their survivor database (n = 216), (2) monthly newsletter, (3) monthly Ambassador call, (4) the Cervivor.org website (blog), (5) posts on 4 private Facebook support group pages, (6) and announcements to 2 advocacy groups. Screener questions to determine eligibility asked women whether they had ever been diagnosed with invasive cervical cancer and if they were ≥21 years old. Online surveys were available in English and Spanish.
Measures
The same survey instrument was administered to both participant groups. The following measures were collected: sociodemographic and insurance characteristics; cervical screening cancer screening history and follow-up of abnormal test results; barriers and facilitators to cervical cancer screening and timely follow-up; knowledge of HPV and use of other preventive care.
Cervical cancer screening was assessed with the following question: “In the 5 years prior to your cancer diagnosis, did you get any cervical cancer screening tests (excluding the test that led to your cervical cancer diagnosis)?” Women who reported they were not screened were asked to review a list of 30 questions about potential barriers to screening. Women who reported screening were asked to review a list of 9 questions about potential facilitators of screening. Follow-up of abnormal test results was identified from the following question: “If you had an abnormal Pap or HPV test result in the 5 years prior to or leading to your diagnosis, did you follow up with your doctor as recommended about this result?” Women who reported that they “waited longer than recommended” or “did not follow up” were asked a series of 18 questions about potential barriers to follow-up.
Response options for the barrier and facilitator statements were “Agree,” “Disagree,” and “I don’t remember/I don’t know.” The responses provided for these questions in this survey were drawn from pilot-tested questionnaires in other cervical cancer studies.12-16 The survey also asked women to specify other barriers or facilitators that they experienced if they were not among those provided.
Statistical Analysis
The proportions of women who reported to “Agree” with each of the statements on barriers and facilitators to obtaining cervical cancer screening or appropriate follow-up were calculated. These proportions are reported for women identified through CR and the SN. Associations were tested with Pearson chi-square or Fisher’s exact as appropriate. All computations were performed using Stata statistical software (version 15.1).17 A P value <.05 was considered statistically significant.
Results
The 3 central cancer registries (CR) identified a total of 2748 women ≥21 years old diagnosed with invasive cervical cancer in the eligible years, 1780 women were reachable and eligible to participate, and of these 480 (28%) completed the questionnaire. The distribution of stage and histology of cervical cancers, race, ethnicity, insurance coverage and rural/urban residence of women who enrolled in this study were similar to those of the overall sample of women diagnosed with cervical cancer in these 3 states during the same time period.11 The social network (SN) sample included a total of 148 women who completed the online survey.
Study participants from the CR and SN had several differences; women identified from the CR were older, more of them were Hispanics and Non-Hispanic Blacks, and separated, widowed or divorced compared to women identified from the SN (Table 1). The average age of participants identified through the CR was 48 years (range 23-90 years) and that of women identified through the SN was 39 years (range 21-72 years). Approximately 65% of women identified through CR were non-Hispanic white compared to 85% among those identified through the SN. Women identified from the CR were also more likely to report lower annual household income and to report having had Medicare, public insurance, or no insurance at the time of their cancer diagnosis. Most women from CR and SN reported having a usual source of care (CR = 71%; SN = 85%, P < .001) and having health insurance to cover all or part of their medical care 5 years prior to diagnosis (CR = 74%; SN = 82%; P = .04). There was no difference in the country of birth; most of the women in both groups were born in the US (86% in CR and 91% in SN).
Table 1.
Sociodemographic Characteristics of Study Participants.
| Characteristics | Participants from cancer registries N = 480 | Participants from survivor social network N = 148 | P-value* |
|---|---|---|---|
| n (%) | n (%) | ||
| Age at diagnosis | |||
| 21-34 years | 89 (19%) | 58 (39%) | <.001 |
| 35-49 years | 178 (37%) | 71 (48%) | |
| 50-64 years | 161 (34%) | 15 (10%) | |
| 65-79 years | 40 (8%) | 4 (3%) | |
| 80 or more years | 12 (3%) | 0 (0%) | |
| Race/ethnicity | |||
| Hispanic | 60 (13%) | 8 (6%) | <.001 |
| Non-Hispanic Black | 87 (18%) | 7 (5%) | |
| Non-Hispanic White | 311 (65%) | 109 (85%) | |
| Non-Hispanic Other | 18 (4%) | 5 (4%) | |
| Marital status at diagnosis | |||
| Single (never married) | 90 (19%) | 23 (18%) | .017 |
| Married | 217 (45%) | 77 (60%) | |
| Living with partner | 41 (9%) | 9 (7%) | |
| Separated, divorced, widowed | 129 (27%) | 20 (16%) | |
| Annual Income | |||
| Less than $10 000 | 90 (19%) | 3 (2%) | <.001 |
| $10 000 to $29 999 | 107 (23%) | 15 (12%) | |
| $30 000 to $49 999 | 62 (13%) | 30 (23%) | |
| $50 000 to $89 999 | 87 (18%) | 35 (27%) | |
| $90 000 or more | 88 (19%) | 40 (31%) | |
| I don’t know | 39 (8%) | 5 (4%) | |
| Country of birth | |||
| United States | 406 (86%) | 117 (91%) | .174 |
| Other | 65 (14%) | 12 (9%) | |
| Health insurance at time of diagnosis (check all that apply) | |||
| Private insurance | 248 (52%) | 103 (78%) | <.001 |
| Medicare (including Medicare managed care) | 77 (16%) | 5 (4%) | <.001 |
| Military or veterans administration | 7 (1%) | 6 (5%) | .030 |
| Public insurance (Medicaid, other county or state public ins.) | 93 (19%) | 14 (11%) | .018 |
| No insurance | 66 (14%) | 7 (5%) | .008 |
| Other | 31 (6%) | 3 (2%) | .084 |
| Partial or full health insurance coverage during the 5 years prior to cervical cancer diagnosis | |||
| Yes | 349 (74%) | 108 (82%) | .040 |
| No | 123 (26%) | 23 (18%) | |
| Usual source of care, during the 5 years prior to diagnosis | |||
| No | 70 (15%) | 8 (6%) | <.001 |
| Yes, a doctor’s office, clinic, or health center | 333 (71%) | 110 (85%) | |
| Yes, an urgent care clinic or ER | 63 (14%) | 12 (9%) | |
Significance was tested with chi-square; Pearson when there are 5 or more cases per cell; Fisher’s exact test when any cell has <5 cases.
Self-Reported Cervical Cancer Screening History
Fifty percent (n = 219) of CR and 21% (N = 31) of SN participants reported not receiving any cervical cancer screening in the 5 years prior to their cervical cancer diagnosis (Table 2). About half of participants from CR (53%) and SN (48%) were first diagnosed with invasive cervical cancer when they were seeking medical care to check on problems or symptoms. About one third of women reported following up on abnormal results as recommended (CR = 37%; SN = 33%). Of the women who were supposed to follow-up on abnormal results (28% of women in both CR and SN groups reported not following-up on abnormal results as recommended.
Table 2.
Self-Reported Cervical Cancer Screening History of Study Participants.
| Cervical cancer screening history | Participants from cancer registries N = 480 | Participants from survivor social network N = 148 | P-value* |
|---|---|---|---|
| n (%) | n (%) | ||
| Received any cervical cancer screening 5 years prior to cervical cancer diagnosisa | |||
| Yes | 223 (50%) | 115 (79%) | <.001 |
| No | 219 (50%) | 31 (21%) | |
| When first diagnosed with invasive cervical cancer | |||
| Part of routine exams/screening (not because of symptoms) | 177 (37%) | 60 (41%) | .550 |
| Seeking medical care for problems/symptoms | 251 (53%) | 71 (48%) | |
| Other | 46 (10%) | 17 (11%) | |
| Follow-up of abnormal Pap or HPV test in 5 years prior to diagnosis | |||
| Follow-up of results as recommended by doctor | 168 (37%) | 43 (33%) | .506 |
| Follow-up of results, but waited longer than recommended | 34 (8%) | 11 (8%) | |
| No, did not follow-up | 32 (7%) | 6 (5%) | |
| Didn’t have an abnormal Pap or HPV test or never had Pap/HPV test | 218 (48%) | 71 (54%) | |
Participants were asked to exclude the screening test that led to cervical cancer diagnosis.
Significance was tested with Pearson chi-square when there were 5 or more cases in each cell; Fisher’s exact test when any cell had <5 cases.
Among participants identified through the CR, a greater proportion of those who reported being screened for cervical cancer also reported being aware of HPV (72%) and having had the flu shot (60%) compared to those who reported not being screened (42% and 43%, respectively) (Table 3). Additionally, among participants aged 55 to 74 years, a greater proportion of those who reported being screened for cervical cancer also reported having had a colorectal cancer screening test (78%) and a mammogram (95%) compared to those who reported not being screened (26% and 50%, respectively). Likewise, participants from the SN who reported being screened appeared to have greater awareness of HPV compared to those who were not screened, but differences in this group by screening status were not statistically detected.
Table 3.
HPV Knowledge and Use of Other Preventive Care of Respondents by Cervical Cancer Screening History.
| HPV knowledge and use of other preventive care | Participants from cancer registries N = 480 | Participants from survivor social network N = 148 | ||||
|---|---|---|---|---|---|---|
| Screened N = 223 | Not screened N = 219 | P-value* | Screened N = 115 | Not screened N = 31 | P-value* | |
| n (%) | n (%) | n (%) | n (%) | |||
| Aware of HPV prior to cervical cancer diagnosis | ||||||
| Yes | 154 (72%) | 91 (42%) | <.001 | 69 (69%) | 16 (55%) | .226 |
| No | 52 (24%) | 104 (48%) | 28 (28%) | 13 (45%) | ||
| I’m not sure | 9 (4%) | 23 (11%) | 3 (3%) | 0 (0%) | ||
| Receipt of cervical cancer vaccine (HPV vaccine) | ||||||
| Yes | 12 (5%) | 4 (2%) | .149 | 10 (10%) | 1 (3%) | .038 |
| No | 176 (80%) | 173 (83%) | 90 (90%) | 26 (90%) | ||
| Not sure | 31 (14%) | 32 (15%) | 0 (0%) | 2 (7%) | ||
| Tubal ligation or sterilization prior to cervical cancer diagnosis | ||||||
| Yes | 59 (27%) | 70 (33%) | .159 | 16 (16%) | 7 (24%) | .281 |
| No | 161 (73%) | 142 (67%) | 87 (84%) | 22 (76%) | ||
| Other preventive care in 5 years prior to cervical cancer diagnosis | ||||||
| Flu shot (all participants eligible) | ||||||
| Yes | 131 (60%) | 90 (43%) | <.001 | 56 (54%) | 12 (41%) | .335 |
| No | 71 (33%) | 106 (50%) | 43 (43%) | 15 (52%) | ||
| Not needed/required | 16 (7%) | 14 (7%) | 4 (4%) | 2 (7%) | ||
| Colorectal cancer screening test (participants aged 55-74 years)a | ||||||
| Yes | 31 (78%) | 18 (26%) | <.001 | 1 (33%) | 2 (67%) | 1.000 |
| No | 8 (20%) | 49 (70%) | 1 (33%) | 1 (33%) | ||
| Not needed/Required | 1 (3%) | 3 (4%) | 1 (33%) | 0 (0%) | ||
| Mammogram (participants aged 55-74 years)a | ||||||
| Yes | 38 (95%) | 36 (50%) | <.001 | 4 (100%) | 3 (100%) | N/A |
| No | 2 (5%) | 35 (49%) | 0 (0%) | 0 (0%) | ||
| Not needed/required | 0 (0%) | 1 (1%) | 0 (0%) | 0 (0%) | ||
There were 128 participants age 55 to 74 in cancer registry sample and 8 participants age 55-74 years in the social network sample.
Significance was tested with Pearson chi-square when there were 5 or more cases in each cell; Fisher’s exact test when any cell had <5 cases.
Barriers to Cervical Cancer Screening
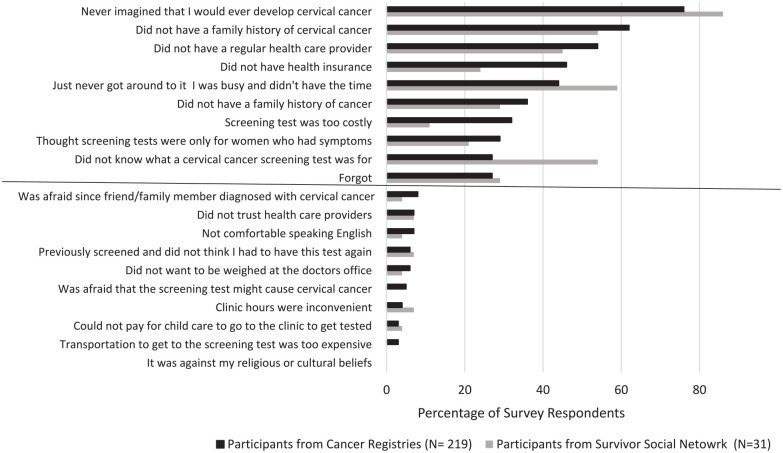
The most frequently identified reason for not being screened was the same for participants in both groups: they never imagined that they would develop cervical cancer (percent agree CR = 76%; SN = 86%) (Figure 1). Women in both groups also identified not having a family history of cervical cancer as one of the top 3 reasons they did not get screened (CR = 62% and SN = 54%). Seven of the ten reasons participants reported most frequently for not getting screened were the same, even though their order differed in participants identified from the CR and SN. Women recruited through the CR identified not having a health care provider and not having insurance as barriers to screening more frequently compared to women from the SN (percent agree was 54% vs 45% and 46% vs 24%, respectively). Women identified through the SN reported being busy or not having the time for screening and not knowing what a cervical cancer screening tests as barriers to screening more frequently compared to women identified through the CR (59% vs 44% and 54% vs 27%). Both groups of participants reported forgetting as one of the most frequently reported reasons they didn’t get screened (CR = 27%; SN = 29%).
Figure 1.
Self-reported barriers to obtaining screening in 5 years prior to diagnosis in women diagnosed with cervical cancer between 2013 and 2016 in the U.S.*
*Graph displays 10 of the most-frequently identified barriers to screening (above the line) and 10 of the least-frequently identified barriers to screening (below the line).
Seven of the ten least-frequently reported reasons for why women did not get screened were also the same in both participant groups. These included: transportation costs to get to screening (CR = 3%; SN = 0%), being afraid that the screening test might cause cervical cancer (CR = 5%; SN = 0%), not being able to pay for childcare to go to the clinic to get tested (CR = 3%; SN = 4%), being previously screened and not thinking that they had to have the test again (CR = 6%; SN = 7%), and not wanting to be weighed at the doctor’s office (CR = 6%; SN = 4%). For these participants, not being comfortable speaking English or the screening being against cultural or religious beliefs were also among the least-reported reasons for why they did not get screened.
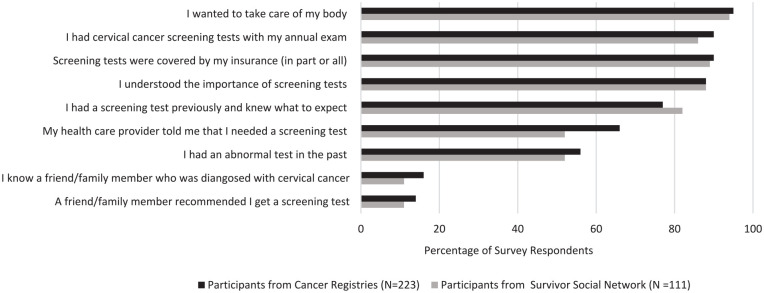
Facilitators of Cervical Cancer Screening
Participants in both groups reported very similar reasons for why they got screened (Figure 2). The most frequently reported facilitators of screening were wanting to take care of their bodies (CR = 95%; SN = 94%), understanding the importance of screening tests (88% in both groups), having screening tests with their annual exams (CR = 86%; SN = 89%), and having screening tests covered by insurance fully or partly (CR = 90%; SN = 89%). Having a friend or family member recommend screening or knowing a friend/family member diagnosed with cervical cancer were reported less frequently as facilitators of screening (CR = 16%; SN = 11% and CR = 14%; SN = 11%, respectively).
Figure 2.
Self-reported facilitators to obtaining screening in 5 years prior to diagnosis in women diagnosed with cervical cancer between 2013 and 2016 in the U.S.
Barriers to Obtaining Follow-Up for Abnormal Results as Recommended
Women who reported having abnormal screening test results in both groups reported the same key reasons for why they did not follow-up on results as recommended (Supplemental Figure 1. Self-reported barriers to following up on abnormal screening results as recommend among women diagnosed with cervical cancer between 2013 and 2016 in the U.S.). These were: not realizing an abnormal test could indicate cervical cancer (percent agree CR = 61%; SN = 63%), being scared to hear what an abnormal result meant (CR = 47%; SN = 29%), not having health insurance (CR = 43%; SN = 29%;), not having health insurance that covered additional procedures (CR = 42%; SN = 24%), and being busy or not having time (CR = 36% SN = 71%). The 2 participant groups also identified the same reasons that least explained why they did not follow-up on abnormal test results as recommended. These included: not having transportation to get to clinic (CR = 9%; SN = 0%), wanting someone else to go with them (CR = 5%; SN = 12%), not being able to pay for childcare to go to the clinic (CR = 5%; SN = 6%) and not being comfortable speaking English (CR = 3%; SN = 0%).
Discussion
In this study of cervical cancer survivors including those identified through population-based cancer registries, we found that about half of the women (50%) reported that they did not get screened in the 5 years prior to their cervical cancer diagnoses. This proportion of unscreened women was found to be higher, approximately 60%, when self-reported results from this analysis were validated against participant’s medical chart data in a complementary analysis.18 Of the women who were screened and needed to follow up on abnormal test results, 28% reported not following up on abnormal Pap or HPV test results as recommended in the 5 years prior to their cervical cancer diagnoses. The key self-reported barriers to obtaining screening and timely follow-up of abnormal test results were related to lack of knowledge of cervical cancer risk, risk factors for cervical cancer, and the meaning of screening test results. The main reasons why women did not get screened were that they never imagined that they could develop cervical cancer and that they did not have a family history of cervical cancer. The main reason women did not follow-up on abnormal results was that they didn’t realize that the results might indicate cervical cancer. Participants identified from the cancer SN were younger, had higher household income, better access to healthcare, and were more likely to be Non-Hispanic white compared to women identified from the CR. In spite of these sociodemographic and healthcare access differences, these women reported the same reasons related to cervical cancer knowledge as the main barrier to obtaining cervical cancer screening.
Our findings on the importance of knowledge of cervical cancer and screening tests in obtaining screening and timely follow-up of abnormal results are similar to what has been found in several other studies.7,8,19 A systematic review of screening studies conducted in immigrant women found that they reported very limited knowledge of screening procedures and of the signs and symptoms of cervical cancer.7 Similarly, studies conducted in low-income, uninsured women identified the lack of knowledge on cervical cancer screening, and signs and symptoms of cervical cancer as key barriers to obtaining screening and seeking follow-up for abnormal results.8 The lack of cervical cancer and screening knowledge has also been reported in studies conducted in both urban areas or major US cities.19 Women’s knowledge of cervical cancer, its risk factors, and screening tests affects their beliefs and self-efficacy, and subsequently influence whether they get screened for cervical cancer.9 This study further emphasizes the importance for continued public health efforts to educate women and increase their awareness of cervical cancer and its risk factors and the available prevention and control strategies.
Additionally, women who reported being screened identified reasons related to their knowledge of cervical cancer risk and screening tests as the key facilitators to screening; they reported that they wanted to take care of their bodies and that they understood the importance of screening tests. The importance of educating women on cervical cancer and screening tests is well-established, however, questions still remain on how best to effectively educate women to increase screening coverage. The national Inside Knowledge: Get the Facts About Gynecologic Cancer campaign led by the CDC has been developing and promoting educational material to increase awareness of gynecologic cancers, including cervical cancer since 2007. The Inside Knowledge (IK) campaign has been successful in developing and pilot-testing educational content,20 as well as disseminating the content nationally through various venues including websites, social media, magazines, newspapers, airport diorama, posters in shopping malls, and bus/bus shelter displays.21 Several other educational interventions such as AMIGAS (Ayudando a las Mujeres con Información,Guía, y Amor para su Salud)22and MARHABA (Muslim Americans Reaching for Health and Building Alliances)23 have focused on tailoring educational content to specific cultural or religious groups to increase screening coverage in these groups. Trials of these interventions show that they are effective in increasing screening coverage in an implementation research setting, but their effectiveness when adopted to real-life settings is yet to be established. Success stories from National Breast and Cervical Cancer Early Detection Program (NBCCEDP) education efforts from various states may provide promise for interventions that are effective in real public health settings; media campaigns with tailored material to eliminate the misconceptions about eligibility for screening services in several NBCCEDP awardees (Utah, Ohio, and New York) have proven successful in increasing cervical cancer screening coverage.24 Findings from this study could be used to inform future educational messages for the IK campaign and NBCCEDP awardees.
Lack of insurance was another key reason that women reported for not getting screened or receiving timely follow-up of abnormal results and, conversely, having screening tests covered by insurance (in-part or fully) was identified as a key facilitator of screening. National data show that cervical cancer screening coverage in women who are uninsured (approximately 60%) is significantly lower than screening coverage in women with public or private insurance (approximately 76% and 86%, respectively).2 The CDC through the NBCCEDP funds all 50 states, the District of Columbia, 6 US territories, and 13 American Indian/Alaska Native tribal organizations to help low-income, uninsured, and underinsured women gain access to timely cervical cancer screening, diagnostic, and treatment services. Since its establishment in 1991, the NBCCEDP has served more than 5.4 million women and in 2017, the program provided cervical cancer screening and diagnostic services to 138 590 women and diagnosed 168 invasive cervical cancers and 5990 premalignant cervical lesions.25 Nonetheless, the NBCCEDP is only able to reach a fraction of uninsured and underinsured women to provide cervical cancer screening.26Other national programs such as Title X and Community Health Centers (CHCs) provide cervical cancer screening to uninsured and underinsured women27,28; however insurance-related disparities in cervical cancer screening have been observed in CHCs even though screening is provided regardless of insurance status.28
Interestingly, we found that the women did not identify structural barriers such as childcare and transportation costs to go to clinics as important barriers to getting screened and receiving timely follow-up of abnormal results. These challenges have been described by women in previous studies,10 but our results suggest that they may be secondary to lack of cervical cancer screening knowledge or lack of insurance as barriers to obtaining screening. The Community Services Preventive Services Task Force (CPSTF) has found strong evidence that multicomponent interventions are effective in increasing community demand for and providing access to screening.29 These combine 2 or more intervention approaches such as interventions that increase demand for screening (like education and media) with those that increase community access (like reducing structural barriers by offering assistance with transportation barriers or childcare). When designed for underserved groups, such as rarely or never screened women, multicomponent interventions may increase screening coverage in these populations.
The strengths of this study are that it utilized population-based registries to recruit a nationally representative sample of cervical cancer survivors. Although the response rate for the sample recruited from the registries was low, the demographic characteristics (age, race, ethnicity) as well as the distribution of the stage and histology of cervical cancers of women who enrolled in the study are similar to those of cervical cancer survivors nationally.11 The low-participation rate observed in this study is similar to what has been observed in similar studies of cervical cancer survivors.30 The addition of participants identified from the cancer survivor network enabled this study to examine the robustness of the key findings; the 2 groups of women differed in the distribution of sociodemographic characteristics (age, race, annual household income, and access to healthcare) but identified the same key barriers and facilitators to cervical cancer screening. A limitation of this study is that it may be subject to bias from the healthy volunteer effect, particularly for the SN sample. However, the women enrolled through the central cancer registries had only slight differences from those who refused to enroll in the study.11 Additionally, the number of women in the study from documented under-screened populations such as foreign-born women or Asian women may have been too small to depict barriers and facilitators to screening in these populations; however, our findings regarding barriers and facilitators are similar to those reported in studies that focused on these under-screened women.7,8
This case investigation study found that at least half of the enrolled cervical cancer survivors did not receive the appropriate screening within the 5 years prior to their cervical cancer diagnoses. It also showed that the key barriers and facilitators to screening are related to knowledge of cervical cancer risk and screening tests as well as the availability of insurance to cover screening costs. These findings including data from population-based registries can guide the design or modification of interventions to increase cervical cancer screening in national or state programs. Although there are national programs dedicated to increasing women’s knowledge about cervical cancer screening (IK campaign) and to cover screening costs for low-income, uninsured or underinsured women (NBCCEDP), these findings suggest that increasing the number of women served by the program may help reach more unscreened women. Increasing screening coverage and timely follow-up by addressing the identified barriers and promoting the facilitators is may reach more unscreened or under-screened women and to continue lowering cervical incidence and deaths in the US.
Supplemental Material
Supplemental material, sj-docx-1-jpc-10.1177_21501327211041862 for Learning From Cervical Cancer Survivors: An Examination of Barriers and Facilitators to Cervical Cancer Screening Among Women in the United States by Virginia Senkomago, April Greek, J. Elizabeth Jackson, Cheryll C. Thomas, Lisa C. Richardson and Vicki B. Benard in Journal of Primary Care & Community Health
Acknowledgments
The authors thank cancer registry staff and physician offices who contributed to the project in NJ, LA, and MI as well as the CICC Study Working Group members: Xiao-Cheng Wu, MD, MPH, CTR; Mary O’Flarity, MN, RN; Christina Lefante, MPH; Molly Ariail, MPH; Lauren Maniscalco, MPH; Glenn Copeland, MS (retired); Amy Marquardt, BA; Adrian Botchway, CTR; Cynthia Nunez, BS; Natalia Herman, MPH; Lisa Paddock, PhD; and Karen Pawlish, ScD and Warner Huh, MD.
Footnotes
Authors’ Note: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Author Contributions: VS led the writing of manuscript. AG and JEJ conducted data analysis and contributed to writing of the manuscript; CT, LCR, and VBB contributed to the writing of manuscript draft. All co-authors reviewed and edited the manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study is supported by Centers for Disease Control and Prevention, Task Orders 200-2015-F-88212 and 200-2016-F-90920. The registries also receive support from the Centers for Disease Control and Prevention’s National Program of Cancer Registries: New Jersey State Cancer Registry (NJSCR) under cooperative agreement 5U58DP006279-02 awarded to the New Jersey Department of Health & Senior Services; Louisiana Tumor Registry (LTR) under cooperative agreement 5U58DP003915 awarded to the Louisiana State University Health Sciences Center; and Michigan Cancer Surveillance Program (MCSP) under cooperative agreement NU58DP003921 awarded to the Michigan Department of Health and Human Services. New Jersey cancer incidence data used in this study were collected with support from the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program under contract HHSN 261201300021I NCI Control No. N01PC-2013-00021. The collection of State of Louisiana cancer incidence data is also supported by SEER under contract HHSN 261201300016I.
Summary: Screening and timely follow-up have lowered cervical cancer incidence in the US; however, screening coverage has remained fairly stable in recent years. This study of cervical cancer survivors examined barriers and facilitators to screening in the 5 years prior to their diagnoses. Fifty percent of survivors reported that they did not get screened; key barriers to screening and timely follow-up were related to lack of knowledge of cervical cancer risk and risk factors, and the meaning of screening test results. This information can be used to design or modify interventions to increase screening and reduce cervical cancer incidence and deaths.
Ethical Considerations: This study was reviewed and approved by the Institutional Review Boards at CDC, Battelle, and all participating central cancer registries (OMB #0920-1162).
ORCID iD: Virginia Senkomago  https://orcid.org/0000-0002-9291-8016
https://orcid.org/0000-0002-9291-8016
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Singh GK. Rural-urban trends and patterns in cervical cancer mortality, incidence, stage, and survival in the United States, 1950-2008. J Community Health. 2012;37(1):217-223. [DOI] [PubMed] [Google Scholar]
- 2.White A, Thompson TD, White MC, et al. Cancer screening test use - United States, 2015. MMWR Morb Mortal Wkly Rep. 2017;66(8):201-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown ML, Klabunde CN, Cronin KA, White MC, Richardson LC, McNeel TS. Challenges in meeting healthy people 2020 objectives for cancer-related preventive services, National Health Interview Survey, 2008 and 2010. Prev Chronic Dis. 2014;11:E29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, Based on November 2020 Submission. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute. www.cdc.gov/cancer/dataviz (1999-2018, accessed June 2021). [Google Scholar]
- 5.Leyden WA, Manos MM, Geiger AM, et al. Cervical cancer in women with comprehensive health care access: attributable factors in the screening process. J Natl Cancer Inst. 2005;97(9):675-683. [DOI] [PubMed] [Google Scholar]
- 6.Sung HY, Kearney KA, Miller M, Kinney W, Sawaya GF, Hiatt RA. Papanicolaou smear history and diagnosis of invasive cervical carcinoma among members of a large prepaid health plan. Cancer. 2000;88(10):2283-2289. [PubMed] [Google Scholar]
- 7.Adunlin G, Cyrus JW, Asare M, Sabik LM. Barriers and facilitators to breast and cervical cancer screening among immigrants in the United States. J Immigr Minor Health. 2019;21(3):606-658. [DOI] [PubMed] [Google Scholar]
- 8.Ogedegbe G, Cassells AN, Robinson CM, et al. Perceptions of barriers and facilitators of cancer early detection among low-income minority women in community health centers. J Natl Med Assoc. 2005;97(2):162-170. [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson CE, Mues KE, Mayne SL, Kiblawi AN. Cervical cancer screening among immigrants and ethnic minorities: a systematic review using the health belief model. J Low Genit Tract Dis. 2008;12(3):232-241. [DOI] [PubMed] [Google Scholar]
- 10.Akinlotan M, Bolin JN, Helduser J, Ojinnaka C, Lichorad A, McClellan D. Cervical cancer screening barriers and risk factor knowledge among uninsured women. J Community Health. 2017;42(4):770-778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Benard VB, Greek A, Jackson JE, et al. Overview of centers for disease control and prevention’s case investigation of cervical cancer study. J Womens Health. 2019;28(7):890-896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spence AR, Alobaid A, Drouin P, et al. Screening histories and contact with physicians as determinants of cervical cancer risk in Montreal, Quebec. Curr Oncol. 2014;21(6):294-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.James AS, Campbell MK, Hudson MA. Perceived barriers and benefits to colon cancer screening among African Americans in North Carolina: how does perception relate to screening behavior? Cancer Epidemiol Prev. 2002;11(6):529-534. [PubMed] [Google Scholar]
- 14.Berkowitz Z, Hawkins NA, Peipins LA, White MC, Nadel MR. Beliefs, risk perceptions, and gaps in knowledge as barriers to colorectal cancer screening in older adults. J Am Geriatr Soc. 2008;56(2):307-314. [DOI] [PubMed] [Google Scholar]
- 15.Benard VB, Saraiya M, Greek A, et al. Overview of the CDC cervical cancer (Cx3) study: an educational intervention of HPV testing for cervical cancer screening. J Womens Health. 2014;23(3):197-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agency, For, Healthcare, Reserach, and, Quality. Medical Expenditure Panel Survey; Access to Healthcare. https://meps.ahrq.gov/survey_comp/hc_survey/2012/AC111912.pdf (accessed June 2021). [Google Scholar]
- 17.StataCorp LLC. Stata Statistical Software: Release 15. College Station TX. 2017. [Google Scholar]
- 18.Benard VB, Jackson JE, Greek A, et al. A population study of screening history and diagnostic outcomes of women with invasive cervical cancer. Cancer Med. 2021;10(12):4127-4137. doi: 10.1002/cam4.3951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cooper CP, Polonec L, Gelb CA. Women’s knowledge and awareness of gynecologic cancer: a multisite qualitative study in the United States. J Womens Health. 2011;20(4):517-524. [DOI] [PubMed] [Google Scholar]
- 20.Cooper CP, Gelb CA, Chu J. What’s the appeal? Testing public service advertisements to raise awareness about gynecologic cancer. J Womens Health. 2014;23(6):488-492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rim SH, Polonec L, Stewart SL, Gelb CA. A national initiative for women and healthcare providers: CDC’s inside knowledge: get the facts about gynecologic cancer campaign. J Womens Health. 2011;20(11):1579-1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith JL, Wilson KM, Orians CE, Byrd TL. AMIGAS: building a cervical cancer screening intervention for public health practice. J Womens Health. 2013;22(9):718-723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patel S. Muslim Americans Reaching for Health and Building Alliances (MARHABA): A Study of Breast and Cervical Cancer Screening Barriers and Facilitators among Muslim Women in New York city. Washington, DC: APHA abstract; 2014. https://apha.confex.com/apha/143am/webprogram/Paper333524.html [Google Scholar]
- 24.Levano W, Miller JW, Leonard B, et al. Public education and targeted outreach to underserved women through the National breast and cervical cancer early detection program. Cancer. 2014;120(S16):2591-2596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease Prevention and Control. National Breast and Cervical Cancer Early Detection Program (NBCCEDP). About the Progam. 2019. https://www.cdc.gov/cancer/nbccedp/about.htm (accessed June 2021).
- 26.Tangka FK, Howard DH, Royalty J, et al. Erratum to: Cervical cancer screening of underserved women in the United States: results from the National Breast and Cervical cancer early detection program, 1997-2012. Cancer Causes Control. 2015;26(5):687-686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fowler CI, Saraiya M, Moskosky SB, Miller JW, Gable J, Mautone-Smith N. Trends in cervical cancer screening in title X-Funded health centers - United States, 2005-2015. MMWR Morb Mortal Wkly Rep. 2017;66(37):981-985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cowburn S, Carlson MJ, Lapidus JA, DeVoe JE. The Association between insurance status and cervical cancer screening in community health centers: exploring the potential of electronic health records for population-level surveillance, 2008–2010. Prev Chronic Dis. Epub ahead of print 24 October 2013. DOI: 10.5888/pcd10.130034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Community Preventive Services Task Force (CPSTF). Cancer screening: multicomponent interventions - cervical cancer. https://www.thecommunityguide.org/findings/cancer-screening-multicomponent-interventions-cervical-cancer (2019, accessed June 2021).
- 30.Le Borgne G, Mercier M, Woronoff A-S, et al. Quality of life in long-term cervical cancer survivors: a population-based study. Gynecol Oncol. 2013;129(1):222-228. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jpc-10.1177_21501327211041862 for Learning From Cervical Cancer Survivors: An Examination of Barriers and Facilitators to Cervical Cancer Screening Among Women in the United States by Virginia Senkomago, April Greek, J. Elizabeth Jackson, Cheryll C. Thomas, Lisa C. Richardson and Vicki B. Benard in Journal of Primary Care & Community Health