Abstract
Background
Patients with mental disorders have an increased risk of developing somatic disorders, just as they have a higher risk of dying from them. These patients often report feeling devaluated and rejected by health professionals in the somatic health care system, and increasing evidence shows that disparities in health care provision contribute to poor health outcomes. The aim of this review was to map and synthesize literature on somatic health professionals’ stigmatization toward patients with mental disorders.
Methods
We conducted a scoping review using Arksey and O’Malley’s framework and carried out a systematic search in three databases: Cinahl, MEDLINE, and PsycINFO in May–June 2019. Peer-reviewed articles published in English or Scandinavian languages during 2008–2019 were reviewed according to title, abstract and full-text reading. We organized and analyzed data using NVivo.
Results
A total of 137 articles meeting the eligibility criteria were reviewed and categorized as observational studies (n = 73) and intervention studies (n = 64). A majority of studies (N = 85) focused on patients with an unspecified number of mental disorders, while 52 studies focused on specific diagnoses, primarily schizophrenia (n = 13), self-harm (n = 13), and eating disorders (n = 9). Half of the studies focused on health students (n = 64), primarily nursing students (n = 26) and medical students (n = 25), while (n = 66) focused on health care professionals, primarily emergency staff (n = 16) and general practitioners (n = 13). Additionally, seven studies focused on both health professionals and students. A detailed characterization of the identified intervention studies was conducted, resulting in eight main types of interventions.
Conclusions
The large number of studies identified in this review suggests that stigmatizing attitudes and behaviors toward patients with mental disorders is a worldwide challenge within a somatic health care setting. For more targeted interventions, there is a need for further research on underexposed mental diagnoses and knowledge on whether specific health professionals have a more stigmatizing attitude or behavior toward specific mental disorders.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12888-021-03415-8.
Keywords: Mental health, Mental disorders, Scoping review, Health care professional, Health care student, Stigma
Background
Mental disorders, such as anxiety, depression and substance use disorders, are among the most burdensome disorders in the world [1, 2], and the estimated life expectancy is generally 15–20 years lower for patients with mental disorders compared to the general population [3]. Research shows that somatic disorders are the main cause of this excess mortality [4] and respiratory, digestive and cardiovascular diseases account for the largest impact on mortality among patients with schizophrenia [5]. Not only do patients with mental disorders have a higher risk of developing somatic disorders, they also have a higher risk of dying from them [3, 6–8]. While numerous factors affect the morbidity and mortality of this patient group, increasing evidence shows that disparities in health care provision contribute to poor health outcomes [9–12]. ‘Diagnostic overshadowing’ – the misattribution of physical symptoms to mental illness – is a key concept used in many studies to describe these disparities, as it can contribute to treatment delay and the development of complications [13–15].
In this review, we argue that stigma is key to understanding these disparities. First, stigma can affect multiple life domains and probably has a dramatic bearing on the distribution of life chances in a variety of areas such as earnings, housing and criminal involvement [12]. Second, patients with mental disorders often report feeling devaluated and rejected by health professionals [13, 16], and third, previous research shows that stigma affects patients’ willingness to seek treatment and the quality of care [17–20].
Stigma is a complex phenomenon, and definitions vary across disciplines and research fields. According to Link et al. (2001) researchers criticize the term for being too vaguely defined and individually focused. In response to this criticism, Link et al. (2001) proposed a new definition highlighting that: “Stigma exists when elements of labeling, stereotyping, separation, status loss, and discrimination occur together in a power situation that allows them” [12]. This paper focuses specifically on stigma in the somatic health care system toward patients with mental disorders, because suboptimal treatment of serious and potentially life-threatening somatic conditions can have profound negative implications for the patients. Previous literature on mental disorder stigma within somatic health care typically focuses on specific mental disorders or specific health professions and settings [8, 21–24]. Thus, a general overview is lacking. This review aims to provide an overview of the literature on stigmatization among somatic health care professionals toward patients with mental disorders—across different health care professions and mental disorders. More specifically, we aim to: 1) provide an overall characterization of existing observational and intervention studies according to health care profession and diagnosis, 2) provide a detailed characterization of the identified intervention studies, and 3) identify knowledge gaps.
Method
Scoping reviews aim to create an overview of a research field and to give an indication of the volume of the literature. Furthermore, a scoping review can be helpful in identifying knowledge gaps [25]. The process of conducting a scoping review is systematic and structured [26] and to ensure transparency, we were informed by the PRISMA-ScR guidelines [27] and Arksey and O’Malley’s methodological framework [28], which outlines six stages of conducting scoping reviews.
Stage 1: identification of research question
In health research, it has become increasingly common to engage with stakeholders such as policy makers; clinicians; and patients, just as many research institutions offers research-based collaboration and advice to external parties. These collaborations can help improve study questions and provide more useful findings [29]. In the design of the literature study, we collaborated with The Danish Health Authority and the organization EN AF OS, who aims to destigmatize mental illness in Denmark. They were both involved in developing the research question, and the organization was additionally involved in qualifying keywords and search strings. As recommended by Arksey and O’Malley, we both considered relevant aspects of the research question (e.g. study population, phenomenon of interest and context) and were aware of developing a research question with a wide approach in order to generate breadth of coverage [28].
Stage 2: identifying relevant data
The first author developed the search strategy in collaboration with research librarians. The search strategy was based on the PICo model that specifies the population (P), phenomenon of interest (I), and context (Co). Following the PICo model the search consisted of two search strings. The first search string specified the population (P), which included patients with frequently occurring mental disorders. We used broad search terms such as ‘mental disorders’ and additionally performed searches on seven specific disorders, since a too broad search can result in missing relevant studies. The seven specific disorders included: anxiety, depression, bipolar disorder, borderline, schizophrenia, eating disorders, and self-harm. We chose these, because they are among the most common and disabling mental disorders [2]. The second search string specified the phenomenon of interest (I) and context (Co), which included stigmatizing behaviors, attitudes, and perceptions among health professionals, e.g. nurses and physicians, in the somatic health care system (see Additional file 1 for full search string). The search was based on keywords (subject headings/ MeSH terms) and free text searches (title, keywords, text). We tested the search string before we formed the final search string. To delimit the search, we applied proximity searching of two words. The search was carried out in May 2019 in three databases: Cinahl, MEDLINE and PsycINFO. Title, abstract and full paper screening were based on inclusion and exclusion criteria. To narrow down the search, we only included studies published 2008–2019 in peer-reviewed journals in English or Scandinavian languages. The temporal delineation was made as we wanted to find the most recent published literature in the field. Protocols, conference literature, book chapters, opinion papers and reviews were excluded. We excluded studies focusing on the mental health of health professionals as well as studies where somatic and psychiatric health professionals could not be separated. While we only included observational studies from the Western Hemisphere, we applied no geographical exclusion criteria for the intervention studies. This is because we wanted to gain insight into experiences from interventions conducted all over the world and because the wide range of interventions may contribute as inspiration for future prevention work. We made the choice of only including observational studies from the Western Hemisphere in collaboration with the organization EN AF OS, to narrow down the search.
Stage 3: data selection
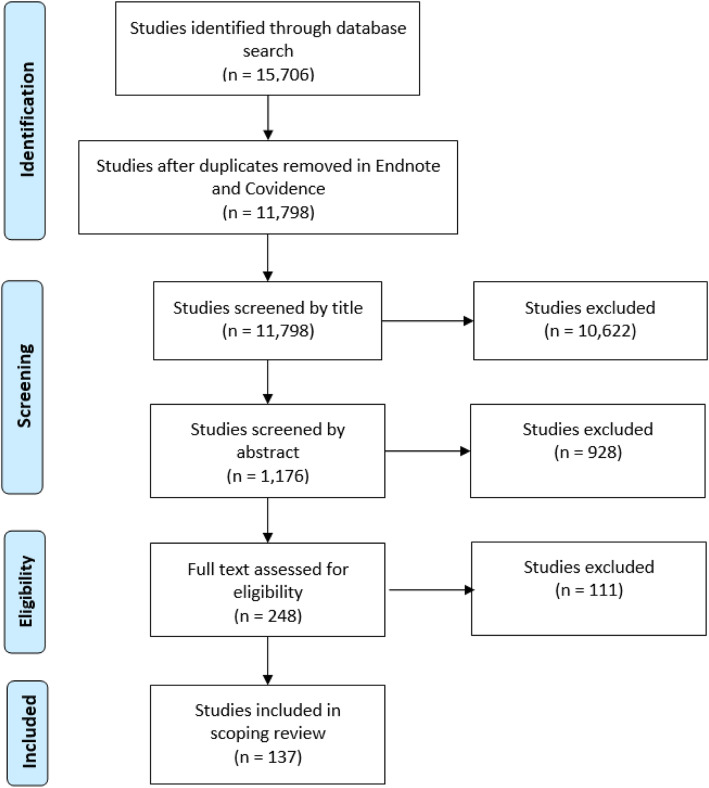
We stored the studies in Endnote and removed duplicates. Next, we moved the studies to the review manager Covidence and performed another duplicate check, after which we began the screening process of the 11,798 identified studies. During the initial title screening, we excluded 10,622 studies for being out of scope. Additionally, we excluded 928 studies during abstract screening for not meeting the inclusion criteria. Of the remaining 248 studies, 111 studies were excluded for not meeting the inclusion criteria. Finally, we included a total of 137 studies in the scoping review. Figure 1 summarizes the literature search and study selection.
Fig. 1.
Flow Diagram
Stage 4 and 5: charting and collating data
We used NVivo to organize and analyze the data. The data charting took the following information into consideration: author(s), year of publication, country of origin, study design, study population (health professionals in the somatic health system), sample size, and mental disorders. Additionally, we coded the scope, method, intervention type, instrument, and outcome in each study. Subsequently, we summarized the studies by study design: observational studies and intervention studies.
Stage 6: consultation exercise
As briefly described above, we collaborated with The Danish Health Authority and the organization EN AF OS, in the development of the design of the literature review and of the research question. The organization was additionally involved in the process of further qualifying keywords and search strings to ensure that relevant keywords, including mental disorders and specific health professionals were not omitted. Thus, the organization played an important role in quality assuring the first two stages of the scoping review. Further, we discussed the findings of the scoping review with the organization and learned that our findings corresponded well with the organization’s knowledge of the phenomenon.
Results
In total, we included 137 studies of which 73 were observational studies and 64 were intervention studies. In the following, we describe and categorize the identified studies according to diagnosis and health care profession. All included studies examined stigmatizing behaviors, attitudes, and/or perceptions among health professionals in the somatic health care system toward patients with mental disorders. For the sake of readability, we will primarily refer to this information as ‘attitudes and behaviors’.
Categorization of health professionals and patients
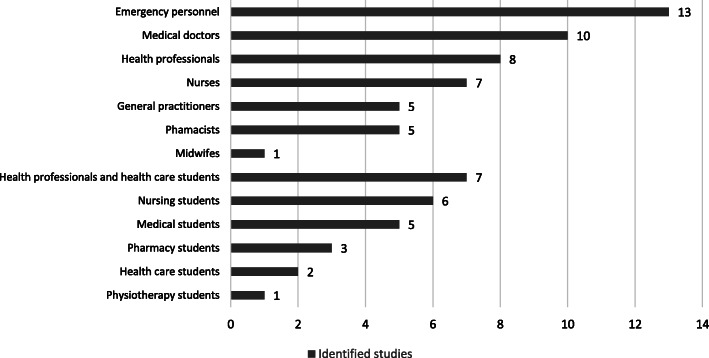
To create an overview of the wide range of different health professions included in the identified studies, we divided the health professionals into 13 categories (Fig. 2). Some studies focused on students rather than trained professionals, and we categorized these studies separately. Other studies included both students and professionals. Moreover, while some studies included well-defined groups of health professionals, such as nurses or general practitioners, others did not focus on specific health professionals. These studies were categorized under the heading ‘Health professionals’, e.g. various hospital employees. Similarly, the category ‘Health care students’ refers to various students within health education. However, we also identified studies examining both students and health professionals, which formed the broad category ‘Health professionals and health care students’. Finally, the category ‘Medical doctors’ covers all other types of medical doctors besides general practitioners, e.g. surgeons or different types of medical specialists.
Fig. 2.
Identified observational studies categorized according to health profession
We also categorized the identified studies according to the patients’ diagnoses and formed seven categories. Five of the categories cover specific diagnoses. In addition, we included a ‘Mixed mental disorders’ category. This category includes studies not confined to a specific mental disorder or studies that examined multiple diagnoses. Furthermore, the category ‘Dual diagnosis’ covers studies examining patients with a mental disorder and a substance use disorder.
Characteristics of the observational studies
The main purpose of the observational studies was to investigate the magnitude of stigmatizing attitudes and behaviors among health professionals in the somatic health care system toward patients with mental disorders. In total, we identified 73 observational studies, all from the Western Hemisphere. About half of the studies were from Europe (n = 41), including a large proportion of studies from England (n = 16), followed by North America (n = 15), Oceania (n = 11), and Asia (n = 3). Furthermore, we identified three studies comparing populations across countries. Most studies used quantitative methods (n = 58); however, we also identified qualitative studies (n = 13) and mixed methods studies (n = 2).
As illustrated in Fig. 2, we found that most studies (n = 13) focused on emergency personnel, followed by medical doctors (n = 10) and health professionals (n = 8). Most studies (n = 40) focused on several, different diagnoses (Table 1). In studies focusing on single, specific diagnoses, the most frequent mental disorders were self-harm (n = 10) and schizophrenia (n = 9).
Table 1.
Combination of diagnoses and health care profession (observational studies)
| Diagnosis | Health care profession | Number of studies |
|---|---|---|
| Depression (n = 3) | Health care students | 1 |
| Pharmacists | 1 | |
| Medical doctors | 1 | |
| Borderline (n = 2) | Nurses | 1 |
| Emergency personnel | 1 | |
| Schizophrenia (n = 9) | Health professionals and health care students | 2 |
| Nursing students | 1 | |
| Pharmacy students | 2 | |
| Pharmacists | 1 | |
| Medical students | 1 | |
| Medical doctors | 1 | |
| General practitioners | 1 | |
| Eating disorder (n = 5) | Health care students | 1 |
| Health professionals | 1 | |
| Medical doctors | 2 | |
| General practitioners | 1 | |
| Self-harm (n = 10) | Health professionals | 2 |
| Medical doctors | 2 | |
| Emergency personnel | 6 | |
| Mixed mental disorders (n = 40) | Physiotherapy students | 1 |
| Midwifes | 1 | |
| Health professionals and health care students | 5 | |
| Nursing students | 6 | |
| Nurses | 5 | |
| Health professionals | 3 | |
| Pharmacy students | 1 | |
| Pharmacists | 4 | |
| Medical students | 4 | |
| Medical doctors | 3 | |
| General practitioners | 3 | |
| Emergency personnel | 5 | |
| Dual diagnosis (n = 4) | Health professionals | 2 |
| Medical doctors | 1 | |
| Emergency personnel | 1 | |
| Total | 73 | |
We combined type of health profession with diagnosis as shown in Table 1. The table shows that a relatively large proportion of studies examined attitudes and behaviors among emergency staff toward patients who self-harm (n = 6). In contrast, studies examining attitudes and behaviors among medical doctors (n = 10) were divided into a wide range of diagnoses, such as depression (n = 1), schizophrenia (n = 1), eating disorders (n = 2), self-harm (n = 2), mixed mental disorders (n = 3), and dual diagnosis (n = 1).
For a detailed description of study design, target group, sample size and diagnosis on observational studies, see Table 2.
Table 2.
Observational studies
| First author, year, reference | Country | Population | Sample size | Diagnosis | Design |
|---|---|---|---|---|---|
| Abood, 2009 [30] | UK | Medical doctors | N = 47 | Self-harm | Quantitative |
| Anderson, 2017 [31] | USA | Medical doctors | N = 80 | Eating disorder | Quantitative |
| Arbanas, 2019 [32] | Croatia | Health professionals | N = 387 | Mixed | Quantitative |
| Artis, 2013 [33] | UK | Emergency personnel | N = 10 | Self-harm | Qualitative |
| Arvaniti, 2009 [34] | Greece | Health professionals and health care students | N = 592 | Mixed | Quantitative |
| Avery, 2019 [35] | USA | Medical doctors | N = 411 | Dual diagnosis | Quantitative |
| Bannatyne, 2017 [36] | Australia | Health care students | N = 126 | Eating disorder | Quantitative |
| Bell, 2010 [37] | Australia, Belgium, India, Finland, Estonia, Latvia | Pharmacy students | N = 649 | Schizophrenia | Quantitative |
| Bell, 2008 [38] | Australia, Belgium, India, Finland, Estonia, Latvia | Pharmacy students | N = 642 | Mixed | Quantitative |
| Bjorkman, 2008 [39] | Sweden | Nurses | N = 120 | Mixed | Quantitative |
| Brunero, 2017 [40] | Australia | Nurses | N = 16 | Mixed | Qualitative |
| Castillejos, 2019 [41] | Spain | General practitioners | N = 145 | Mixed | Quantitative |
| Ceylan, 2019 [42] | Turkey | Nurses | N = 186 | Schizophrenia | Quantitative |
| Chapman, 2014 [43] | Australia | Emergency Personnel | N = 186 | Self-harm | Quantitative |
| Clifton, 2016 [44] | UK | Health professionals | N = 85 | Mixed | Qualitative |
| Conlon, 2012 [45] | Ireland | Emergency personnel | N = 87 | Self-harm | Quantitative |
| Crapanzano, 2018 [46] | USA | Medical doctors | N = 96 | Depression | Quantitative |
| Currin, 2009 [47] | UK | General practitioners | N = 154 | Eating disorders | Quantitative |
| Cutler, 2009 [48] | USA | Medical students | N = 47 | Mixed | Qualitative |
| Dixon, 2008 [49] | UK | Medical students | N = 1081 | Mixed | Quantitative |
| Ewalds-Kvist, 2013 [50] | Sweden | Nursing students | N = 246 | Mixed | Quantitative |
| Gawley, 2011 [51] | Canada | Health care students | N = 309 | Depression | Quantitative |
| Giannetti, 2018 [52] | USA | Pharmacists | N = 239 | Mixed | Quantitative |
| Gordon, 2012 [53] | UK | Emergency personnel | N = 32 | Mixed | Quantitative |
| Granados-Gamez, 2017 [54] | Spain | Nursing students | N = 194 | Mixed | Quantitative |
| Happell, 2008 [55] | Australia | Nursing students | N = 148 | Mixed | Quantitative |
| Happell, 2018 [56] | Australia, Ireland, Finland, Norway, Netherland | Nursing students | N = 423 | Mixed | Quantitative |
| Heyward-Chaplin, 2018 [57] | UK | Health professionals | N = 59 | Self-harm | Quantitative |
| Ihalainen-Tamlander, 2016 [58] | Finland | Nurses | N = 218 | Mixed | Quantitative |
| Janouskova, 2017 [59] | The Czech Republic | Health professionals and health care students | N = 308 | Mixed | Quantitative |
| Jones, 2009 [60] | USA | Medical doctors | N = 51 | Mixed | Quantitative |
| Koning, 2018 [61] | Australia | Emergency personnel | N = 15 | Self-harm | Qualitative |
| Thongpriwan, 2015 [62] | USA | Nursing students | N = 229 | Mixed | Quantitative |
| Kopera, 2015 [63] | Polonia | Health professionals and health care students | N = 57 | Mixed | Quantitative |
| Korszun, 2012 [64] | UK | Medical students | N = 760 | Mixed | Quantitative |
| Kuzman, 2014 [65] | The Czech Republic | Medical students | N = 199 | Mixed | Quantitative |
| Leddy, 2009 [66] | USA | Medical doctors | N = 504 | Eating disorder | Quantitative |
| Liekens, 2012 [67] | Belgium | Pharmacists | N = 149 | Depression | Quantitative |
| Magliano, 2011 [68] | Italy | Medical students | N = 194 | Schizophrenia | Quantitative |
| Magliano, 2017 [69] | Italy | General practitioners | N = 387 | Schizophrenia | Quantitative |
| McCann, 2018 [70] | Australia | Emergency personnel | N = 1230 | Dual diagnosis | Quantitative |
| McCarthy, 2010 [71] | Ireland | Emergency Personnel | N = 68 | Self-harm | Quantitative |
| Morral, 2016 [72] | UK | Pharmacists | N = 351 | Mixed | Quantitative |
| Muehlenkamp, 2013 [73] | Belgium | Health professionals | N = 342 | Self-harm | Quantitative |
| Nash, 2013 [13] | UK | Emergency personnel | N = 39 | Mixed | Qualitative |
| Nauta, 2019 [74] | Netherlands | Medical doctors | N = 187 | Mixed | Quantitative |
| Neauport, 2012 [75] | France | Medical doctors | N = 322 | Mixed | Quantitative |
| Noonan, 2018 [76] | Ireland | Midwifes | N = 157 | Mixed | Quantitative |
| Nutt, 2017 [77] | Scotland | Health professionals | N = 113 | Dual diagnosis | Quantitative |
| O’Reilly, 2012 [78] | Australia | Health professionals and health care students | N = 23 | Mixed | Qualitative |
| O’Reilly, 2015 [79] | Australia | Pharmacists | N = 188 | Schizophrenia | Quantitative |
| Peitl, 2011 [80] | Croatia | Health professionals and health care students | N = 151 | Mixed | Quantitative |
| Perboell, 2015 [81] | Denmark | Emergency personnel | N = 122 | Self-harm | Quantitative |
| Prener, 2015 [82] | USA | Emergency personnel | N = 20 | Mixed | Qualitative |
| Rai, 2019 [83] | UK | Medical doctors | N = 37 | Self-harm | Mixed methods |
| Rao, 2009 [84] | UK | Health professionals | N = 108 | Dual diagnosis | Quantitative |
| Raveneau, 2014 [85] | USA | Health professionals | N = 82 | Eating disorder | Quantitative |
| Reavley, 2014 [86] | Australia | Health professionals | N = 1536 | Mixed | Quantitative |
| Rickles, 2010 [87] | USA | Pharmacists | N = 292 | Mixed | Quantitative |
| Sandhu, 2019 [88] | Canada | Health professionals and health care students | N = 538 | Schizophrenia | Quantitative |
| Schafer, 2011 [89] | UK | Nursing students | N = 288 | Mixed | Quantitative |
| Schmidt, 2017 [90] | Netherlands | General practitioners | N = 63 | Mixed | Quantitative |
| Serafini, 2011 [91] | Italy | Health professionals and health care students | N = 202 | Schizophrenia | Quantitative |
| Shefer, 2014 [15] | UK | Emergency personnel | N = 39 | Mixed | Qualitative |
| Stumbo, 2018 [92] | USA | General practitioners | N = 597 | Mixed | Mixed methods |
| Treloar, 2009 [93] | Australia | Emergency personnel | N = 140 | Borderline personality disorder | Qualitative |
| Van Nieuwenhui, 2013 [94] | UK | Emergency personnel | N = 25 | Mixed | Qualitative |
| Volmer, 2008 [95] | Estonia | Pharmacy students | N = 157 | Schizophrenia | Quantitative |
| Weare, 2019 [96] | Australia | Nurses | N = 40 | Mixed | Quantitative |
| Winkler, 2016 [97] | The Czech Republic | Medical doctors | N = 3010 | Mixed | Quantitative |
| Woollaston, 2008 [98] | UK | Nurses | N = 6 | Borderline personality disorder | Qualitative |
| Yildirim, 2015 [99] | Turkey | Physiotherapy students | N = 524 | Mixed | Quantitative |
| Zolnierek, 2012 [100] | USA | Nurses | N = 1 | Mixed | Qualitative |
Characteristics of the intervention studies
The main purpose of the intervention studies was to evaluate interventions to reduce health professionals’ stigmatizing attitudes and behaviors toward people with mental disorders. We identified 64 intervention studies, most of which were from North America (n = 19), followed by studies from Europe (n = 16), Oceania (n = 13), Asia (n = 13), and Africa (n = 1). In addition, two interventions studies were comparative studies. Most studies were based on quantitative methods (n = 51); seven were mixed methods studies, and six were qualitative studies.
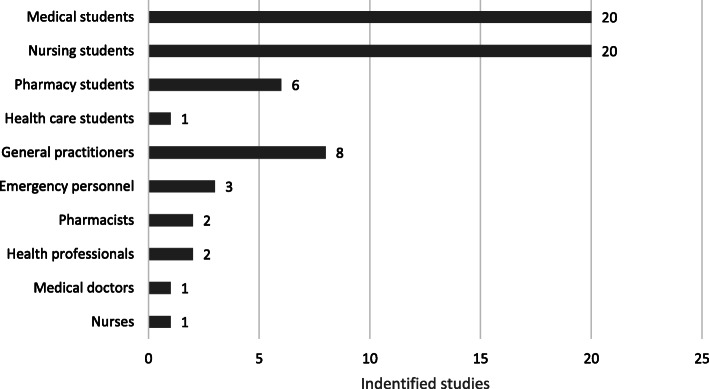
Most intervention studies focused on changing students’ attitudes and behaviors toward patients with mental disorders; 20 of these studies focused on medical students, 20 focused on nursing students and six focused on pharmacy students, as illustrated in Fig. 3. Furthermore, eight studies focused on general practitioners, constituting the third-largest category when distributing the studies by health profession.
Fig. 3.
Identified intervention studies categorized according to health profession
Most intervention studies (n = 45) did not focus on patients with a specific mental disorder, but typically on attitudes and behaviors toward multiple mental disorders or mental disorder in general as shown in Table 2. Depression (n = 5), eating disorder (n = 4), and schizophrenia (n = 4) were among the most common diagnoses.
By combining health profession with diagnosis (Table 3), we found that most of the studies focusing on attitudes and behaviors among nursing students did not focus on a specific mental disorder, as 17 of the 20 identified studies looked at multiple diagnoses or mental disorder in general. Similarly, 16 of 20 identified studies examining attitudes and behaviors among medical students focused on multiple diagnoses or mental disorder in general. We found a similar pattern for studies examining attitudes and behaviors among pharmacy students (n = 6) and health care students (n = 1).
Table 3.
Combination of diagnoses and health care profession (intervention studies)
| Diagnosis | Health care profession | Number of studies |
|---|---|---|
| Depression (n = 5) | General practitioners | 3 |
| Pharmacists | 2 | |
| Borderline (n = 2) | Emergency personnel | 1 |
| Health professionals | 1 | |
| Schizophrenia (n = 4) | Medical doctors | 1 |
| Medical students | 3 | |
| Eating disorder (n = 4) | General practitioners | 1 |
| Medical students | 1 | |
| Nursing students | 2 | |
| Self-harm (n = 3) | Emergency personnel | 2 |
| Nursing students | 1 | |
| Bipolar disorder (n = 1) | Health professionals | 1 |
| Mixed mental disorders (n = 45) | General practitioners | 4 |
| Medical students | 16 | |
| Pharmacy students | 6 | |
| Health care students | 1 | |
| Nurses | 1 | |
| Nursing students | 17 | |
| Total | 64 | |
For a detailed description of study design, target group, sample size, and diagnosis in the intervention studies, see Table 4.
Table 4.
Intervention studies
| First author, year | Country | Population | Sample size | Diagnosis | Design | Intervention |
|---|---|---|---|---|---|---|
| Airagnes, 2014 [101] | France | Medical students | N = 163 | Mixed | Quasi-experimental with control group | Lectures |
| Arbanas, 2018 [102] | Croatia | Nursing students | N = 51 | Mixed | Quasi-experimental without control group | Expeditionary interventions |
| Bannatyne, 2015 [103] | Australia | Medical students | N = 41 | Eating disorder | Quasi-experimental with control group | Lectures |
| Beaulieu, 2017 [104] | Canada | General practitioners | N = 73 | Mixed | RCT | Interventions targeting general practitioners and medical doctors |
| Bilge, 2017 [105] | Turkey | Nursing students | N = 322 | Mixed | Other | Lectures |
| Bingham, 2018 [106] | New Zealand | Nursing students | N = 45 | Mixed | Quasi-experimental without control group | Expeditionary interventions |
| Brenner, 2011 [107] | USA | Medical students | N = 100 | Mixed | Qualitative | Expeditionary interventions |
| Calloway, 2017 [108] | USA | Nurses | N = 82 | Mixed | Qualitative | Interventions targeting health professionals |
| Chiles, 2017 [109] | USA | Medical students | N = 289 | Mixed | Quasi-experimental without control group | Observational studies |
| Clement, 2012 [110] | UK | Nursing students | N = 216 | Mixed | RCT | Contact-based interventions |
| Coppens, 2018 [111] | Portugal, Germany, Ireland, Hungary | General practitioners | N = 208 | Depression | Quasi-experimental without control group | Interventions targeting general practitioners and medical doctors |
| Crisafulli, 2008 [112] | USA | Nursing students | N = 115 | Eating disorder | Quasi-experimental with control group | Lectures |
| Crockett, 2009 [113] | Australia | Pharmacists | N = 32 | Depression | RCT | Interventions targeting pharmacists |
| Demiroren, 2016 [114] | Turkey | Medical students | N = 190 | Mixed | Quasi-experimental with control group | Expeditionary interventions |
| Dipaula, 2011 [115] | USA | Pharmacy students | N = 278 | Mixed | Quasi-experimental with control group | Lectures |
| Duffy, 2016 [116] | USA | Nursing students | N = 131 | Eating disorder | Quasi-experimental without control group | Lectures |
| Duman, 2017 [117] | Turkey | Nursing students | N = 202 | Mixed | Quasi-experimental with control group | Lectures |
| Economou, 2017 [118] | Greece | Medical students | N = 678 | Mixed | Quasi-experimental without control group | Expeditionary interventions |
| Economou, 2012 [119] | Greece | Medical students | N = 158 | Schizophrenia | Quasi-experimental without control group | Expeditionary interventions |
| Eksteen, 2017 [120] | The South African Republic | Medical students | N = 616 | Mixed | Quasi-experimental without control group | Expeditionary interventions |
| Esen Danaci, 2016 [121] | Turkey | Medical students | N = 106 | Schizophrenia | Quasi-experimental without control group | Observational studies |
| Failde, 2014 [122] | Spain | Medical students | N = 171 | Mixed | Quasi-experimental without control group | Observational studies |
| Fernandez, 2016 [123] | Malaysia | Medical students | N = 102 | Mixed | RCT | Contact-based interventions |
| Flanagan, 2016 [124] | USA | General practitioners | N = 27 | Mixed | Quasi-experimental with control group | Interventions targeting general practitioners and medical doctors |
| Fokuo, 2017 [125] | USA | Nursing students | N = 70 | Mixed | Qualitative | Contact-based interventions |
| Gable, 2011 [126] | USA | Pharmacy students | N = 39 | Mixed | Quasi-experimental with control group | Lectures |
| Galletly, 2011 [127] | Australia | Medical students | N = 87 | Schizophrenia | Quasi-experimental without control group | Contact-based interventions |
| Gibson, 2019 [128] | UK | Nursing students | N = 55 | Self-harm | Quasi-experimental without control group | Lectures |
| Happell, 2008 [129] | Australia | Nursing students | N = 687 | Mixed | Quasi-experimental without control group | Expeditionary interventions |
| Happell, 2019 [130] | Australia, Ireland, Finland | Nursing students | N = 194 | Mixed | Quasi-experimental without control group | Contact-based interventions |
| Hastings, 2017 [131] | USA | Nursing students | N = 310 | Mixed | Quasi-experimental without control group | Expeditionary interventions |
| Itzhaki, 2017 [132] | Israel | Nursing students | N = 101 | Mixed | Quasi-experimental without control group | Contact-based interventions |
| Kassam, 2011 [133] | UK | Medical students | N = 110 | Mixed | Quasi-experimental with control group | Contact-based interventions |
| Knaak, 2015 [134] | Canada | Health professionals | N = 191 | Borderline personality disorder | Quasi-experimental without control group | Interventions targeting health professionals |
| Lam, 2011 [135] | Hong Kong | General practitioner | N = 69 | Mixed | Quasi-experimental without control group | Interventions targeting general practitioners and medical doctors |
| Lam, 2015 [136] | Hong Kong | General practitioners | N = 566 | Mixed | Quasi-experimental with control group | Interventions targeting general practitioners and medical doctors |
| Liekens, 2013 [137] | Belgium | Pharmacists | N = 141 | Depression | RCT | Interventions targeting pharmacists |
| Linville, 2013 [138] | USA | General practitioners | N = 45 | Eating disorder | Quasi-experimental without control group | Interventions targeting general practitioners and medical doctors |
| Lyons, 2015 [139] | Australia | Medical students | N = 151 | Mixed | Quasi-experimental without control group | Expeditionary interventions |
| Manzanera, 2018 [140] | Spain | General practitioners | N = 1322 | Depression | Quasi-experimental without control group | Interventions targeting general practitioners and medical doctors |
| Markstrom, 2009 [141] | Sweden | Health care students | N = 167 | Mixed | Quasi-experimental without control group | Expeditionary interventions |
| Martinez-Martinez, 2019 [142] | Spain | Nursing students | N = 185 | Mixed | Quasi-experimental without control group | Contact-based interventions |
| McAllister, 2009a [143] | Australia | Emergency personnel | N = 28 | Self-harm | Quasi-experimental without control group | Interventions targeting emergency personnel |
| McAllister, 2009b [144] | Australia | Emergency personnel | N = 36 | Self-harm | Quasi-experimental without control group | Interventions targeting emergency personnel |
| Michalak, 2014 [145] | Canada | Health professionals | N = 164 | Bipolar disorder | Quasi-experimental without control group | Interventions targeting health professionals |
| Morrison, 2009 [146] | Australia | Nursing students | N/A | Mixed | Qualitative | Contact-based interventions |
| Moxham, 2016 [147] | Australia | Nursing students | N = 9 | Mixed | Quasi-experimental with control group | Expeditionary interventions |
| Muzyk, 2017 [148] | USA | Pharmacy students | N = 74 | Mixed | Quasi-experimental without control group | Lectures |
| O′ Connor, 2013 [149] | Ireland | Medical students | N = 285 | Mixed | Quasi-experimental without control group | Expeditionary interventions |
| Omori, 2012 [150] | Japan | Medical doctors | N = 51 | Schizophrenia | Quasi-experimental without control group | Interventions targeting general practitioners and medical doctors |
| O’Reilly, 2010 [151] | Australia | Pharmacy students | N = 178 | Mixed | Quasi-experimental without control group | Contact-based interventions |
| O’Reilly, 2011 [152] | Australia | Pharmacy students | N = 60 | Mixed | Quasi-experimental with control group | Lectures |
| Papish, 2013 [153] | Canada | Medical students | N = 111 | Mixed | RCT | Expeditionary interventions |
| Patten, 2012 [154] | Canada | Pharmacy students | N = 131 | Mixed | RCT | Contact-based interventions |
| Poreddi, 2015 [155] | India | Medical students | N = 176 | Mixed | Quasi-experimental with control group | Lectures |
| Romem, 2008 [156] | Israel | Nursing students | N = 126 | Mixed | Quasi-experimental without control group | Expeditionary interventions |
| Shen, 2014 [157] | China | Medical students | N = 325 | Mixed | Quasi-experimental without control group | Expeditionary interventions |
| Stacey, 2018 [158] | UK | Nursing students | N/A | Mixed | Qualitative | Lectures |
| Stuhlmiller, 2019 [159] | USA | Nursing students | N = 85 | Mixed | Quasi-experimental without control group | Expeditionary interventions |
| Telles-Correia, 2015 [160] | Portugal | Medical students | N = 398 | Mixed | Quasi-experimental without control group | Observational studies |
| Treloar, 2009 [161] | Australia | Emergency personnel | N = 65 | Borderline personality disorder | Quasi-experimental with control group | Interventions targeting emergency personnel |
| Upshur, 2008 [162] | USA | General practitioners | N = 9 | Depression | Quasi-experimental without control group | Interventions targeting general practitioners and medical doctors |
| Wang, 2016 [163] | Taiwan | Medical students | N = 72 | Mixed | Quasi-experimental with control group | Observational studies |
| Winkler, 2017 [164] | The Czech Republic | Nursing students | N = 499 | Mixed | RCT | Contact-based interventions |
Note: RCT = Randomized controlled trial, Observational studies = Observational studies of the effect of attending medical school
Intervention types and content
Of the 64 included intervention studies, 47 targeted health care students while 17 targeted health professionals. To provide a more detailed characterization of the type and content of the identified intervention studies, we categorized the interventions into eight main types: four targeting students and four targeting health professionals. We categorized the interventions targeting students based on the content of the intervention, whereas we categorized interventions targeting health professionals according to the content and specific health profession (e.g. nurses or medical doctors) because these were often closely related. We present one example of each intervention type, focusing on examples that are illustrative of the intervention types, well-described in the articles, and show a geographical breadth and variation between health care students and professionals. For a detailed description of the intervention studies, see Table 4.
Interventions targeting students
We identified 47 intervention studies targeting health care students. We categorized these into four different types of interventions: a) Lectures b) Expeditionary interventions c) Contact-based interventions, and d) Observational studies of the effect of attending medical school. Many interventions included a mix of different activities. We divided the interventions according to the most prominent ones. The interventions most often targeted nursing students (n = 20) or medical students (n = 20), while six interventions targeted pharmacy students and one targeted a mixed group of students.
Lectures
Interventions based on lectures (n = 13) were characterized by a teacher-centered approach, and typically took place in a classroom where the teacher provided different educational programs [101, 103, 105, 112, 115–117, 126, 128, 148, 152, 155, 158]. The topics of the lectures varied, including e.g. doctor-patient relationships [101], empathy [103], mental health literacy [152], social distancing [155], fear [148], and knowledge about how patients with mental disorders experience encounters with the somatic health care system [158]. In an example of a classical teaching intervention from Australia, pharmacy students participated in two 12-h Mental Health First Aid courses. The classes addressed themes such as symptoms, evidence-based treatment of several mental disorders, early warning signs of mental disorder, and how to provide initial help to people in a mental health crisis. The courses involved, e.g., case studies and group activities [152].
Expeditionary interventions
These interventions (n = 17) had in common that they primarily took place outside of the classroom and included clerkships and field trips, e.g. to psychiatric wards [102, 106, 107, 118–120, 129, 131, 139, 141, 147, 149, 153, 156, 157, 159]. The interventions lasted from four hours a week for three weeks [106] to full time for eight weeks [139], and some also included lectures on mental health and psychiatry [106, 118, 119, 139, 157]. While all 17 interventions aimed to reduce stigma, some also investigated the impact on a) students’ interest in psychiatry, b) psychiatry as a career choice, and c) attitudes toward psychiatry.
In some interventions, students visited psychiatric facilities [131] or pharmacies [115], since a visit at local pharmacies allowed pharmacy students to meet patients with mental disorders. Other interventions were mental health camps consisting of a 2–5-day immersive learning program outside of the ‘typical’ clinical setting, where students could meet and interact with people with a mental disorder at camp sites [147, 159]. One of these interventions included students in the United States, who participated in a mental health camp after receiving didactic teaching. The camp consisted of two days working with a group of patients from the local mental health service. The program included trust and confidence-building exercises and socialization through joint preparation of meals and leisure activities. Following the camp, students attended a 15-week mental health placement at either a community facility or a hospital [159].
Contact-based interventions
Contact-based interventions (n = 12) had in common that they focused on facilitated encounters with patients with mental disorders [110, 123, 125, 127, 130, 132, 133, 142, 146, 151, 154, 164]. These types of interventions were mainly characterized by patients with mental disorders being involved in the lectures, either as educators [130, 151] or as visitors giving testimonies [133, 142, 154]. In some cases, the testimonies were introduced to students via video display [110, 123, 132, 164]. In contrast to interventions based on expeditionary learning, contact-based interventions typically took place in classrooms or other educational settings.
To exemplify, in Spain nursing students participated in a 90-min intervention including testimonies from a mental health professional, a person with a mental disorder and a family member of another person with a mental disorder. They described their experiences with mental disorder, e.g., how the disorder emerged, symptoms and side effects of medication, problems related to family coexistence, and problems in the workplace. Following this, a 30-min discussion among students and the presenters was held [142].
Observational studies of the effect of attending medical school
We identified five studies investigating the effect of attending medical school on stigmatizing attitudes and behaviors toward patients with mental disorders [109, 121, 122, 160, 163]. These studies were observational or based on natural experiments in contrast to the other studies. For instance, in Turkey researchers followed freshman medical students from 2008 to 2013. A questionnaire was administered to the participants on their first study year, before receiving any theoretical or practical training on psychiatry. Participants who completed their psychiatry internship were reassessed with a questionnaire five years later [121].
Interventions targeting health professionals
We identified 17 intervention studies targeting health professionals, including general practitioners and other medical doctors (n = 9), emergency personnel (n = 3), nurses (n = 1), pharmacists (n = 2), and non-specific groups of health professionals (n = 2). We categorized these interventions into four intervention types: (1) Interventions targeting general practitioners and medical doctors, (2) Interventions targeting pharmacists, (3) Interventions targeting emergency personnel, and (4) Interventions targeting non-specific groups of health professionals.
Interventions targeting general practitioners and medical doctors
Nine studies focused on interventions targeting general practitioners and medical doctors [104, 111, 124, 135, 136, 138, 140, 150, 162]. They focused on attitudes and behaviors toward patients with specific mental disorders such as depression [111, 140, 162] or eating disorders [138]. The interventions differed considerably in content and scope. For example, in Hong Kong general practitioners participated in a 1-year part-time course. The course included 20 interactive seminars on mental disorders and 20 sessions visiting general practitioner consultations, including a written assignment. The seminars were developed and conducted by a family physician and a psychiatrist. After completing the seminars, the participants began clinical attachment in groups [135].
Interventions targeting pharmacists
We found two interventions targeting pharmacists (n = 2), both of which addressed attitudes and behaviors toward patients with depression [113, 137]. The interventions aimed to empower pharmacists when encountering patients with depression through courses in communication skills, awareness of depression, and use of anti-depressants. For example, Australian pharmacists were taught, by a psychiatrist, a psychologist, and a general practitioner, to give advice and support when dispensing medication. To upgrade their knowledge, the pharmacists received pamphlets on depression [113].
Interventions targeting emergency personnel
Few studies (n = 3) investigated the impact of educational programs on emergency personnel [143, 144, 161]. These interventions primarily focused on the reception of patients with mental disorders at emergency rooms through courses in evidence-based treatment and communication. For example, in Australia, researchers tested a 2-h lecture focusing on participants’ attitudes and current practice in relation to self-harm. Lectures included theories for understanding self-harm and evidence-based treatment. Teaching material consisted of PowerPoint presentations and short video narratives from clinical practice and consumer reports [143].
Interventions targeting non-specific groups of health professionals
Three interventions did not target a specific group of health professionals, but included different professions [108, 134, 145]. These interventions differed considerably in content given that one was a lecture [108], one a workshop [134], and one a stage play [145]. In the latter, researchers from Canada worked closely with an actress and playwright who had bipolar disorder. They developed a one-woman stage play specifically targeting stigma toward that specific disorder. A director was hired for the rehearsal period. The audiences comprised people with bipolar disorder and health care providers working with this target group [145].
Discussion
The aim of this scoping review was to provide a comprehensive overview of the vast amount of literature within the research field of stigma toward people with a mental disorder in the somatic health care system. In total, we identified 137 studies, which include 73 observational studies and 64 intervention studies. We included qualitative and quantitative studies and a wide range of health care professionals and students. In the analysis, we described the characteristics of the studies and categorized them according to health profession and diagnosis. This contrasts with previous literature reviews that have typically focused more narrowly on, for instance, specific diagnoses or health care professionals ([23, 24, 165–167], e.g.), and only a few previous reviews have had health care students as a target population [168, 169].
This scoping review created a comprehensive overview of the existing literature, employing a broad focus on both health care students and health professionals as well as inclusion of several mental disorders. This broad approach is helpful for identifying important knowledge gaps. All observational studies examined stigmatizing behaviors, attitudes, and/or perceptions among health professionals in the somatic health care system toward patients with mental disorders. We found that most observational studies (n = 13) focused on emergency personnel, followed by medical doctors (n = 10) and health professionals (n = 8), and that most studies (n = 40) focused on several diagnoses. In studies focusing on single, specific diagnoses, the most frequent mental disorders were self-harm (n = 10) and schizophrenia (n = 9). Finally, we found that most of the observational studies used quantitative methods (n = 58), while 13 studies used qualitive methods and only two studies used mixed methods. Considering the complexity of the phenomena, more qualitative- and mixed method studies could deepen our understanding of stigma in somatic health care further.
With this review, we have provided insight into the distribution of studies in relation to the specific health profession and diagnosis that have dominated the literature, and which have been overlooked. We found that only a small number of all the included studies explicitly address stigma toward people with anxiety, bipolar disorder, and borderline personality disorder. This points to a need for future research to explore further the extent and characteristics of somatic health care professionals’ stigmatizing attitudes and behaviors toward patients diagnosed with these disorders.
In general, the content of the included studies spans many different combinations of health professionals and diagnoses, confer Tables 1 and 2. Because of this diversity, it is not possible to conclude whether stigmatizing attitudes and behaviors may be more prevalent among some health care professions compared to others, and whether patients with a specific mental disorder are more exposed to stigmatization than others. However, this could be an interesting theme to investigate further in future research, as this knowledge can develop and strengthen anti-stigma campaigns targeting specific professions within the health sector.
We found that interventions to prevent or reduce stigma toward patients with mental disorders focused either on health care students or health care professionals. We categorized student interventions according to their content and the interventions targeting health professional according to the target group. In total, we identified four types of intervention studies targeting students (including lectures, expeditionary interventions, contact-based interventions, and observational studies of the effect of attending medical school) and four targeting health professionals (including general practitioners/medical doctors, pharmacists, emergency personnel and non-specific health professionals). The interventions varied in content and design, both within and across different target groups. Student interventions generally did not examine a specific mental disorder but rather multiple mental disorders or mental disorders in general, as opposed to interventions for health professionals, which often focused on both a specific target group and a specific diagnosis. This extended focus on intervention studies is, to our knowledge, not seen in previous reviews. Several previous reviews, however, call for more educational interventions to reduce negative attitudes and stigma among health professionals [167, 170], since more education and competency development can be associated with more positive attitudes [23, 171].
Following the scoping review methodology, we did not assess the quality of the studies included in the review, given that we focused on the overview of the literature. Thus, we cannot draw inferences about the effectiveness of interventions toward somatic health care professionals to reduce or prevent stigma. However, we did find that the quality of the effectiveness evaluations varied and that the majority used a quasi-experimental design (with or without a control group), while only eight studies employed an RCT. Therefore, this review points to a need for intervention studies with stronger evaluation designs.
Overall, our scoping review underlines the presence of stigmatizing attitudes and behaviors toward people with a mental disorder in the somatic health care system. The included studies show that stigma may be caused by several factors, e.g. lack of knowledge about mental disorders among health professionals, lack of time to care for more demanding or difficult patients and by health professionals’ experiences of feeling insecure and unsafe in the presence of patients with mental disorders [111, 132, 152]. Following Link and Phelan’s conceptualization of stigma, health professionals’ experiences of lacking knowledge and competencies regarding mental disorders may initiate a stigmatization process in which they—due to dominant cultural beliefs—link undesirable characteristics and negative stereotypes to patients with mental disorders and engage in a separation of “us” from “them”, leading the patients to experience status loss, discrimination and unequal outcomes and opportunities [12]. However, the identified intervention studies reveal that attitudes toward people with mental disorders among somatic health care professionals to a great extent reflect the attitudes of the general population [16, 108, 133]. This way, somatic health care professionals seem to exercise neither more nor less stigmatizing behavior than people in the general population. Importantly, and in contrast to the general population, health professionals possess power to determine the course, type and circumstances of treatment offered to patients with mental disorders. According to Link and Phelan (2001), power is precisely key to understanding stigma, because stigmatization is entirely contingent on access to social, economic and/or political power that allows the different elements of stigma to unfold [12]. Therefore, stigmatizing attitudes and behaviors toward mental disorders among health professionals constitute a critical problem that needs to be addressed both during their education and continuously throughout their professional career as part of their continuing professional development.
Strengths and weaknesses
This review has several limitations. First, as the search was limited to studies published after 2008, as well as studies in English or Nordic languages, we may have overlooked relevant studies and anti-stigmatizing interventions. Second, as mentioned above and as applies to scoping reviews in general, we did not assess the quality of the included studies.
Despite these limitations, we note several strengths of this study. First, a methodological strength is the fundamental systematic approach to charting the studies. We have systematically selected keywords and searched in selected databases based on several inclusion and exclusion criteria. Additionally, the screening process was undertaken on different levels: by title screening, abstract screening, and full-text screening in the review manager Covidence, after which all included studies were systematically organized and analyzed in NVivo. The use of NVivo contributed to a systematic organization of the included studies, which provided a useful tool for creating overview and high-level systematization of all included studies. Additionally, we consider it a strength that we have included intervention studies from the entire world. Although organization and practice within the somatic health care system are diverse worldwide, which reduces the transmissibility of the interventions, this knowledge contributes to the research field and can further inspire and mobilize new interventions. Finally, we consider it a strength that we have included a consultation element (e.g. stage 6) in our review process, as recommended by Arksey and O’Malley [28].
Conclusion
This scoping review has contributed to our knowledge about stigmatization of people with mental disorders in the somatic health care system. The large number of studies identified in this review suggests that stigmatizing attitudes and behaviors toward patients with mental disorders, within a somatic health care setting, is a worldwide challenge. By including studies focusing on different health professions and mental disorders, instead of focusing solely on a single profession or diagnosis as seen in many reviews, this review contributes with a more comprehensive overview.
The findings point to a need for further research on stigma toward patients with anxiety, bipolar disorder and borderline personality disorder. Furthermore, it would be beneficial to further knowledge on whether stigmatizing attitudes or behaviors toward mental disorders are more prevalent in some health care professions than others. Such knowledge could contribute to more targeted interventions.
Supplementary Information
Acknowledgements
Not applicable.
Authors’ contributions
INS designed the research protocol and screened all articles. INS and AOK worked together to review the articles until agreement was reached. AOK and INS designed the tables. INS and AOK led the writing with contributions from MBDN. MBDN and PVP checked and revised the text. INS led the final editing stages of the manuscript. All authors read and approved the final manuscript.
Funding
We received funding from the organization EN AF OS. The organization took part in developing the research question and wasadditionally involved in qualifying keywords and search strings. The funding body had no role in the analysis, and interpretationof data and in writing the manuscript. The views expressed in this article are those of the authors and do not necessarily represent or reflect the views of the organization EN AF OS.
Availability of data and materials
All data generated or analyzed during this study are included in this published article. The search strategy is available as an additional file.
Declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, Charlson FJ, Norman RE, Flaxman AD, Johns N, et al. Global burden of disease attributable to mental and substance use disorders: findings from the global burden of disease study 2010. Lancet. 2013;382(9904):1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 2.Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, Olesen J, Allgulander C, Alonso J, Faravelli C, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21(9):655–679. doi: 10.1016/j.euroneuro.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 3.Nordentoft M, Wahlbeck K, Hällgren J, Westman J, Ösby U, Alinaghizadeh H, Gissler M, Laursen TM. Excess mortality, causes of death and life expectancy in 270,770 patients with recent onset of mental disorders in Denmark, Finland and Sweden. PLoS One. 2013;8(1):e55176. doi: 10.1371/journal.pone.0055176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and Meta-analysis. JAMA Psychiatry. 2015;72(4):334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kugathasan P, Stubbs B, Aagaard J, Jensen SE, Munk Laursen T, Nielsen RE. Increased mortality from somatic multimorbidity in patients with schizophrenia: a Danish nationwide cohort study. Acta Psychiatr Scand. 2019;140(4):340–348. doi: 10.1111/acps.13076. [DOI] [PubMed] [Google Scholar]
- 6.Laursen TM, Munk-Olsen T, Gasse C. Chronic somatic comorbidity and excess mortality due to natural causes in persons with schizophrenia or bipolar affective disorder. PLoS One. 2011;6(9):e24597. doi: 10.1371/journal.pone.0024597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stubbs B, Vancampfort D, Veronese N, Kahl KG, Mitchell AJ, Lin PY, Tseng PT, Mugisha J, Solmi M, Carvalho AF, et al. Depression and physical health multimorbidity: primary data and country-wide meta-analysis of population data from 190 593 people across 43 low- and middle-income countries. Psychol Med. 2017;47(12):2107–2117. doi: 10.1017/S0033291717000551. [DOI] [PubMed] [Google Scholar]
- 8.Stone EM, Chen LN, Daumit GL, Linden S, McGinty EE. General medical Clinicians' attitudes toward people with serious mental illness: a scoping review. J Behav Health Serv Res. 2019;46(4):656–679. doi: 10.1007/s11414-019-09652-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitchell AJ, Santo Pereira IE, Yadegarfar M, Pepereke S, Mugadza V, Stubbs B. Breast cancer screening in women with mental illness: comparative meta-analysis of mammography uptake. Br J Psychiatry. 2014;205(6):428–435. doi: 10.1192/bjp.bp.114.147629. [DOI] [PubMed] [Google Scholar]
- 10.Lord O, Malone D, Mitchell AJ. Receipt of preventive medical care and medical screening for patients with mental illness: a comparative analysis. Gen Hosp Psychiatry. 2010;32(5):519–543. doi: 10.1016/j.genhosppsych.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 11.Havercamp SM, Scott HM. National health surveillance of adults with disabilities, adults with intellectual and developmental disabilities, and adults with no disabilities. Disabil Health J. 2015;8(2):165–172. doi: 10.1016/j.dhjo.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 12.Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27(1):363–385. doi: 10.1146/annurev.soc.27.1.363. [DOI] [Google Scholar]
- 13.Nash M. Diagnostic overshadowing: a potential barrier to physical health care for mental health service users. Ment Health Pract. 2013;17(4):22–26. doi: 10.7748/mhp2013.12.17.4.22.e862. [DOI] [Google Scholar]
- 14.Thornicroft G. Physical health disparities and mental illness: the scandal of premature mortality. Br J Psychiatry. 2011;199(6):441–442. doi: 10.1192/bjp.bp.111.092718. [DOI] [PubMed] [Google Scholar]
- 15.Shefer G, Henderson C, Howard LM, Murray J, Thornicroft G. Diagnostic overshadowing and other challenges involved in the diagnostic process of patients with mental illness who present in emergency departments with physical symptoms--a qualitative study. PLoS One. 2014;9(11):e111682. doi: 10.1371/journal.pone.0111682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Knaak S, Mantler E, Szeto A. Mental illness-related stigma in healthcare: barriers to access and care and evidence-based solutions. Healthcare Manage Forum. 2017;30(2):111–116. doi: 10.1177/0840470416679413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, Morgan C, Rüsch N, Brown J, Thornicroft G. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2015;45(1):11–27. doi: 10.1017/S0033291714000129. [DOI] [PubMed] [Google Scholar]
- 18.Mitchell AJ, Malone D, Doebbeling CC. Quality of medical care for people with and without comorbid mental illness and substance misuse: systematic review of comparative studies. Br J Psychiatry. 2009;194(6):491–499. doi: 10.1192/bjp.bp.107.045732. [DOI] [PubMed] [Google Scholar]
- 19.Kilbourne AM, Welsh D, McCarthy JF, Post EP, Blow FC. Quality of care for cardiovascular disease-related conditions in patients with and without mental disorders. J Gen Intern Med. 2008;23(10):1628–1633. doi: 10.1007/s11606-008-0720-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lawrence D, Kisely S. Inequalities in healthcare provision for people with severe mental illness. J Psychopharmacol (Oxford, England) 2010;24(4 Suppl):61–68. doi: 10.1177/1359786810382058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rayner G, Blackburn J, Edward KL, Stephenson J, Ousey K. Emergency department nurse's attitudes towards patients who self-harm: a meta-analysis. Int J Ment Health Nurs. 2019;28(1):40–53. doi: 10.1111/inm.12550. [DOI] [PubMed] [Google Scholar]
- 22.Giandinoto JA, Stephenson J, Edward KL. General hospital health professionals’ attitudes and perceived dangerousness towards patients with comorbid mental and physical health conditions: systematic review and meta-analysis. Int J Ment Health Nurs. 2018;27(3):942–955. doi: 10.1111/inm.12433. [DOI] [PubMed] [Google Scholar]
- 23.Karman P, Kool N, Poslawsky IE, van Meijel B. Nurses' attitudes towards self-harm: a literature review. J Psychiatr Ment Health Nurs. 2015;22(1):65–75. doi: 10.1111/jpm.12171. [DOI] [PubMed] [Google Scholar]
- 24.Alexander V, Ellis H, Barrett B. Medical-surgical Nurses' perceptions of psychiatric patients: a review of the literature with clinical and practice applications. Arch Psychiatr Nurs. 2016;30(2):262–270. doi: 10.1016/j.apnu.2015.06.018. [DOI] [PubMed] [Google Scholar]
- 25.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthcare. 2015;13(3):141–146. doi: 10.1097/XEB.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 27.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 28.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 29.Concannon TW, Grant S, Welch V, Petkovic J, Selby J, Crowe S, Synnot A, Greer-Smith R, Mayo-Wilson E, Tambor E, et al. Practical guidance for involving stakeholders in Health Research. J Gen Intern Med. 2019;34(3):458–463. doi: 10.1007/s11606-018-4738-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abood A, Jain S, Zhong J. Self-harm and the surgeon. J Plastic Reconstruct Aesthetic Surg. 2009;62(5):e106–e107. doi: 10.1016/j.bjps.2008.07.019. [DOI] [PubMed] [Google Scholar]
- 31.Anderson K, Accurso E, Kinasz K, Grange D, Accurso EC, Kinasz KR, Le Grange D. Residents' and Fellows' knowledge and attitudes about eating disorders at an Academic Medical Center. Acad Psychiatry. 2017;41(3):381–384. doi: 10.1007/s40596-016-0578-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arbanas G, Rožman J, Bagarić Š. The attitudes of medical doctors, nurses and lay people towards schizophrenia, depression and PTSD. Psychiatr Danub. 2019;31(Suppl 1):84–91. [PubMed] [Google Scholar]
- 33.Artis L, Smith JR. Emergency department staff attitudes toward people who self-harm: exploring the influences of norms and identity. Adv Emerg Nurs J. 2013;35(3):259–269. doi: 10.1097/TME.0b013e31829d202b. [DOI] [PubMed] [Google Scholar]
- 34.Arvaniti A, Samakouri M, Kalamara E, Bochtsou V, Bikos C, Livaditis M. Health service staff's attitudes towards patients with mental illness. Soc Psychiatry Psychiatr Epidemiol. 2009;44(8):658–665. doi: 10.1007/s00127-008-0481-3. [DOI] [PubMed] [Google Scholar]
- 35.Avery JD, Taylor KE, Kast KA, Kattan J, Gordon-Elliot J, Mauer E, et al. Attitudes Toward Individuals With Mental Illness and Substance Use Disorders Among Resident Physicians. Primary Care Companion CNS Disord. 2019;21(1). [DOI] [PubMed]
- 36.Bannatyne AJ, Stapleton PB. Attitudes towards anorexia nervosa: volitional stigma differences in a sample of pre-clinical medicine and psychology students. J Mental Health (Abingdon, England) 2017;26(5):442–448. doi: 10.3109/09638237.2016.1149801. [DOI] [PubMed] [Google Scholar]
- 37.Bell JS, Aaltonen SE, Airaksinen MS, Volmer D, Gharat MS, Muceniece R, Vitola A, Foulon V, Desplenter FA, Chen TF. Determinants of mental health stigma among pharmacy students in Australia, Belgium, Estonia, Finland, India and Latvia. Int J Soc Psychiatry. 2010;56(1):3–14. doi: 10.1177/0020764008097621. [DOI] [PubMed] [Google Scholar]
- 38.Bell JS, Aaltonen SE, Bronstein E, Desplenter FA, Foulon V, Vitola A, Muceniece R, Gharat MS, Volmer D, Airaksinen MS, et al. Attitudes of pharmacy students toward people with mental disorders, a six country study. Pharm World Sci. 2008;30(5):595–599. doi: 10.1007/s11096-008-9211-x. [DOI] [PubMed] [Google Scholar]
- 39.Bjorkman T, Angelman T, Jonsson M. Attitudes towards people with mental illness: a cross-sectional study among nursing staff in psychiatric and somatic care. Scand J Caring Sci. 2008;22(2):170–177. doi: 10.1111/j.1471-6712.2007.00509.x. [DOI] [PubMed] [Google Scholar]
- 40.Brunero S, Buus N, West S. Categorising patients mental illness by medical surgical nurses in the general hospital Ward: a focus group study. Arch Psychiatr Nurs. 2017;31(6):614–623. doi: 10.1016/j.apnu.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 41.Castillejos Anguiano MC, Bordallo Aragon A, Aguilera Fernandez D, Moreno Kustner B. Perceptions about mental illness among general practitioners. Int J Ment Heal Syst. 2019;13:27. doi: 10.1186/s13033-019-0284-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ceylan B, Kocoglu-Tanyer D. An examination of Turkish Nurses' attitudes, awareness and practices regarding reproductive health needs of individuals with schizophrenia. Mental Health Nursing. 2019;40(5). [DOI] [PubMed]
- 43.Chapman R, Martin C. Perceptions of Australian emergency staff towards patients presenting with deliberate self-poisoning: a qualitative perspective. Int Emerg Nurs. 2014;22(3):140–145. doi: 10.1016/j.ienj.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 44.Clifton A, Burgess C, Clement S, Ohlsen R, Ramluggun P, Sturt J, Walters P, Barley EA. Influences on uptake of cancer screening in mental health service users: a qualitative study. BMC Health Serv Res. 2016;16:257. doi: 10.1186/s12913-016-1505-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Conlon M, O'Tuathail C. Measuring emergency department nurses' attitudes towards deliberate self-harm using the self-harm antipathy scale. Int Emerg Nurs. 2012;20(1):3–13. doi: 10.1016/j.ienj.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 46.Crapanzano K, Fisher D, Hammarlund R, Hsieh EP, May W. An exploration of Residents' implicit biases towards depression-a pilot study. J Gen Intern Med. 2018;33(12):2065–2069. doi: 10.1007/s11606-018-4593-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Currin L, Waller G, Schmidt U. Primary care physicians' knowledge of and attitudes toward the eating disorders: do they affect clinical actions? Int J Eat Disord. 2009;42(5):453–458. doi: 10.1002/eat.20636. [DOI] [PubMed] [Google Scholar]
- 48.Cutler JL, Harding KJ, Mozian SA, Wright LL, Pica AG, Masters SR, Graham MJ. Discrediting the notion "working with 'crazies' will make you 'crazy'": addressing stigma and enhancing empathy in medical student education. Adv Health Sci Educ Theory Pract. 2009;14(4):487–502. doi: 10.1007/s10459-008-9132-4. [DOI] [PubMed] [Google Scholar]
- 49.Dixon RP, Roberts LM, Lawrie S, Jones LA, Humphreys MS. Medical students' attitudes to psychiatric illness in primary care. Med Educ. 2008;42(11):1080–1087. doi: 10.1111/j.1365-2923.2008.03183.x. [DOI] [PubMed] [Google Scholar]
- 50.Ewalds-Kvist B, Hogberg T, Lutzen K. Student nurses and the general population in Sweden: trends in attitudes towards mental illness. Nordic J Psychiatry. 2013;67(3):164–170. doi: 10.3109/08039488.2012.694145. [DOI] [PubMed] [Google Scholar]
- 51.Gawley L, Einarson A, Bowen A. Stigma and attitudes towards antenatal depression and antidepressant use during pregnancy in healthcare students. Adv Health Sci Educ Theory Pract. 2011;16(5):669–679. doi: 10.1007/s10459-011-9289-0. [DOI] [PubMed] [Google Scholar]
- 52.Giannetti V, Caley CF, Kamal KM, Covvey JR, McKee J, Wells BG, Najarian DM, Dunn TJ, Vadagam P. Community pharmacists and mental illness: a survey of service provision, stigma, attitudes and beliefs. Int J Clin Pharm. 2018;40(5):1096–1105. doi: 10.1007/s11096-018-0619-7. [DOI] [PubMed] [Google Scholar]
- 53.Gordon JT. Emergency department junior medical staff's knowledge, skills and confidence with psychiatric patients: a survey. Psychiatrist. 2012;36(5):186–188. doi: 10.1192/pb.bp.111.035188. [DOI] [Google Scholar]
- 54.Granados-Gamez G, Lopez Rodriguez MDM, Corral Granados A, Marquez-Hernandez VV. Attitudes and beliefs of nursing students toward mental disorder: the significance of direct experience with patients. Perspect Psychiatric Care. 2017;53(2):135–143. doi: 10.1111/ppc.12147. [DOI] [PubMed] [Google Scholar]
- 55.Happell B, Robins A, Gough K. Developing more positive attitudes towards mental health nursing in undergraduate students: part 2--the impact of theory and clinical experience. J Psychiatr Ment Health Nurs. 2008;15(7):527–536. doi: 10.1111/j.1365-2850.2007.01233.x. [DOI] [PubMed] [Google Scholar]
- 56.Happell B, Platania-Phung C, Bocking J, Scholz B, Horgan A, Manning F, Doody R, Hals E, Granerud A, Lahti M, et al. Nursing Students' attitudes towards people diagnosed with mental illness and mental health nursing: an international project from Europe and Australia. Issues Mental Health Nurs. 2018;39(10):829–839. doi: 10.1080/01612840.2018.1489921. [DOI] [PubMed] [Google Scholar]
- 57.Heyward-Chaplin J, Shepherd L, Arya R, O'Boyle CP. Audit of healthcare professionals' attitudes towards patients who self-harm and adherence to national guidance in a UK burns and plastic surgery department. Scars Burn Heal. 2018;4:2059513118764100. doi: 10.1177/2059513118764100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ihalainen-Tamlander N, Vahaniemi A, Loyttyniemi E, Suominen T, Valimaki M. Stigmatizing attitudes in nurses towards people with mental illness: a cross-sectional study in primary settings in Finland. J Psychiatr Ment Health Nurs. 2016;23(6–7):427–437. doi: 10.1111/jpm.12319. [DOI] [PubMed] [Google Scholar]
- 59.Janouskova M, Weissova A, Formanek T, Pasz J, Bankovska Motlova L. Mental illness stigma among medical students and teachers. Int J Soc Psychiatry. 2017;63(8):744–751. doi: 10.1177/0020764017735347. [DOI] [PubMed] [Google Scholar]
- 60.Jones SM, Vahia IV, Cohen CI, Hindi A, Nurhussein M. A pilot study to assess attitudes, behaviors, and inter-office communication by psychiatrists and primary care providers in the care of older adults with schizophrenia. Int J Geriatric Psychiatry. 2009;24(3):254–260. doi: 10.1002/gps.2098. [DOI] [PubMed] [Google Scholar]
- 61.Koning KL, McNaught A, Tuffin K. Emergency department staff beliefs about self-harm: a thematic framework analysis. Community Ment Health J. 2018;54(6):814–822. doi: 10.1007/s10597-017-0178-8. [DOI] [PubMed] [Google Scholar]
- 62.Thongpriwan V, Leuck SE, Powell RL, Young S, Schuler SG, Hughes RG. Undergraduate nursing students' attitudes toward mental health nursing. Nurse education today. 2015;35(8):948-53. [DOI] [PubMed]
- 63.Kopera M, Suszek H, Bonar E, Myszka M, Gmaj B, Ilgen M, Wojnar M. Evaluating explicit and implicit stigma of mental illness in mental health professionals and medical students. Community Ment Health J. 2015;51(5):628–634. doi: 10.1007/s10597-014-9796-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Korszun A, Dinos S, Ahmed K, Bhui K. Medical student attitudes about mental illness: does medical-school education reduce stigma? Acad Psychiatry. 2012;36(3):197–204. doi: 10.1176/appi.ap.10110159. [DOI] [PubMed] [Google Scholar]
- 65.Kuzman MR, Bosnjak D, Vokal P, Kuharic J, Brkic I, Kuzman T, Dujmovic J. Can medical students recognize depression? A survey at the Zagreb School of Medicine. Acad Psychiatry. 2014;38(3):312–315. doi: 10.1007/s40596-014-0109-8. [DOI] [PubMed] [Google Scholar]
- 66.Leddy MA, Jones C, Morgan MA, Schulkin J. Eating disorders and obstetric-gynecologic care. J Women's Health (Larchmt) 2009;18(9):1395–1401. doi: 10.1089/jwh.2008.1183. [DOI] [PubMed] [Google Scholar]
- 67.Liekens S, Smits T, Laekeman G, Foulon V. Factors determining social distance toward people with depression among community pharmacists. Eur Psychiatry. 2012;27(7):528–535. doi: 10.1016/j.eurpsy.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 68.Magliano L, Read J, Rega S, Oliviero N, Sagliocchi A, Patalano M, D'Ambrosio A. The influence of causal explanations and diagnostic labeling on medical students' views of schizophrenia. Acad Med. 2011;86(9):1155–1162. doi: 10.1097/ACM.0b013e318226708e. [DOI] [PubMed] [Google Scholar]
- 69.Magliano L, Strino A, Punzo R, Acone R, Affuso G, Read J. Effects of the diagnostic label 'schizophrenia', actively used or passively accepted, on general practitioners' views of this disorder. Int J Soc Psychiatry. 2017;63(3):224–234. doi: 10.1177/0020764017695353. [DOI] [PubMed] [Google Scholar]
- 70.McCann TV, Savic M, Ferguson N, Cheetham A, Witt K, Emond K, Bosley E, Smith K, Roberts L, Lubman DI. Recognition of, and attitudes towards, people with depression and psychosis with/without alcohol and other drug problems: results from a national survey of Australian paramedics. BMJ Open. 2018;8(12):e023860. doi: 10.1136/bmjopen-2018-023860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.McCarthy L, Gijbels H. An examination of emergency department nurses' attitudes towards deliberate self-harm in an Irish teaching hospital. Int Emerg Nurs. 2010;18(1):29–35. doi: 10.1016/j.ienj.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 72.Morral K, Morral J. A survey of community pharmacists' attitudes towards mental illness. J Public Ment Health. 2016;15(2):93–102. doi: 10.1108/JPMH-12-2015-0052. [DOI] [Google Scholar]
- 73.Muehlenkamp JJ, Claes L, Quigley K, Prosser E, Claes S, Jans D. Association of training on attitudes towards self-injuring clients across health professionals. Arch Suicide Res. 2013;17(4):462–468. doi: 10.1080/13811118.2013.801815. [DOI] [PubMed] [Google Scholar]
- 74.Nauta K, Boenink AD, Wimalaratne IK, Menkes DB, Mellsop G, Broekman B. Attitudes of general hospital consultants towards psychosocial and psychiatric problems in Netherlands. Psychol Health Med. 2019;24(4):402–413. doi: 10.1080/13548506.2018.1546020. [DOI] [PubMed] [Google Scholar]
- 75.Neauport A, Rodgers RF, Simon NM, Birmes PJ, Schmitt L, Bui E. Effects of a psychiatric label on medical residents' attitudes. Int J Soc Psychiatry. 2012;58(5):485–487. doi: 10.1177/0020764011408652. [DOI] [PubMed] [Google Scholar]
- 76.Noonan M, Jomeen J, Galvin R, Doody O. Survey of midwives' perinatal mental health knowledge, confidence, attitudes and learning needs. Women Birth. 2018;31(6):e358–e366. doi: 10.1016/j.wombi.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 77.Nutt R, Gilchrist G, Marsa-Sambola F, Baldacchino A. Staff regard towards working with patients with co-morbid depression and substance misuse: an exploratory study. Heroin Addiction Relat Clin Problems. 2017;19(2):5–16. [Google Scholar]
- 78.O'Reilly CL, Bell JS, Chen TF. Mental health consumers and caregivers as instructors for health professional students: a qualitative study. Soc Psychiatry Psychiatric Epidemiol. 2012;47(4):607–613. doi: 10.1007/s00127-011-0364-x. [DOI] [PubMed] [Google Scholar]
- 79.O'Reilly CL, Bell JS, Kelly PJ, Chen TF. Exploring the relationship between mental health stigma, knowledge and provision of pharmacy services for consumers with schizophrenia. Res Soc Adm Pharm. 2015;11(3):e101–e109. doi: 10.1016/j.sapharm.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 80.Peitl MV, Peitl V, Pavlović E, Proloscić J, Petrić D. Stigmatization of patients suffering from schizophrenia. Coll Antropol. 2011;35(Suppl 2):141–145. [PubMed] [Google Scholar]
- 81.Perboell PW, Hammer NM, Oestergaard B, Konradsen H. Danish emergency nurses' attitudes towards self-harm - a cross-sectional study. Int Emerg Nurs. 2015;23(2):144–149. doi: 10.1016/j.ienj.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 82.Prener C, Lincoln AK. Emergency medical services and "psych calls": examining the work of urban EMS providers. Am J Orthopsychiatry. 2015;85(6):612–619. doi: 10.1037/ort0000077. [DOI] [PubMed] [Google Scholar]
- 83.Rai L, Shepherd L, O'Boyle CP. Quantitative and thematic analysis of burns surgeons' attitudes, beliefs and surgical decision-making in self-harm burn injuries: the use of a questionnaire and hypothetical cases. Burns. 2019;45(1):180–189. doi: 10.1016/j.burns.2018.08.003. [DOI] [PubMed] [Google Scholar]
- 84.Rao H, Mahadevappa H, Pillay P, Sessay M, Abraham A, Luty J. A study of stigmatized attitudes towards people with mental health problems among health professionals. J Psychiatr Ment Health Nurs. 2009;16(3):279–284. doi: 10.1111/j.1365-2850.2008.01369.x. [DOI] [PubMed] [Google Scholar]
- 85.Raveneau G, Feinstein R, Rosen LM, Fisher M. Attitudes and knowledge levels of nurses and residents caring for adolescents with an eating disorder. Int J Adolescent Med Health. 2014;26(1):131–136. doi: 10.1515/ijamh-2013-0015. [DOI] [PubMed] [Google Scholar]
- 86.Reavley NJ, Mackinnon AJ, Morgan AJ, Jorm AF. Stigmatising attitudes towards people with mental disorders: a comparison of Australian health professionals with the general community. Aust New Zealand J Psychiatry. 2014;48(5):433–441. doi: 10.1177/0004867413500351. [DOI] [PubMed] [Google Scholar]
- 87.Rickles NM, Dube GL, McCarter A, Olshan JS. Relationship between attitudes toward mental illness and provision of pharmacy services. J Am Pharmacists Assoc. 2010;50(6):704–713. doi: 10.1331/JAPhA.2010.09042. [DOI] [PubMed] [Google Scholar]
- 88.Sandhu HS, Arora A, Brasch J, Streiner DL. Mental health stigma: explicit and implicit attitudes of Canadian undergraduate students, medical school students, and psychiatrists. Can J Psychiatr. 2019;64(3):209–217. doi: 10.1177/0706743718792193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Schafer T, Wood S, Williams R. A survey into student nurses' attitudes towards mental illness: implications for nurse training. Nurse Educ Today. 2011;31(4):328–332. doi: 10.1016/j.nedt.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 90.Schmidt HG, Van Gog T, Schuit SC, Van den Berge K, Van Daele PL, Bueving H, Van der Zee T, Van den Broek WW, Van Saase JL, Mamede S. Do patients' disruptive behaviours influence the accuracy of a doctor's diagnosis? A randomised experiment. BMJ Qual Saf. 2017;26(1):19–23. doi: 10.1136/bmjqs-2015-004109. [DOI] [PubMed] [Google Scholar]
- 91.Serafini G, Pompili M, Haghighat R, Pucci D, Pastina M, Lester D, Angeletti G, Tatarelli R, Girardi P. Stigmatization of schizophrenia as perceived by nurses, medical doctors, medical students and patients. J Psychiatr Ment Health Nurs. 2011;18(7):576–585. doi: 10.1111/j.1365-2850.2011.01706.x. [DOI] [PubMed] [Google Scholar]
- 92.Stumbo SP, Yarborough BJH, Yarborough MT, Green CA. Perspectives on providing and receiving preventive health care from primary care providers and their patients with mental illnesses. Am J Health Promot. 2018;32(8):1730–1739. doi: 10.1177/0890117118763233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Treloar AJ. A qualitative investigation of the clinician experience of working with borderline personality disorder. N Z J Psychol. 2009;38(2):30–34. [Google Scholar]
- 94.van Nieuwenhuizen A, Henderson C, Kassam A, Graham T, Murray J, Howard LM, Thornicroft G. Emergency department staff views and experiences on diagnostic overshadowing related to people with mental illness. Epidemiol Psychiatric Sci. 2013;22(3):255–262. doi: 10.1017/S2045796012000571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Volmer D, Maesalu M, Bell JS. Pharmacy students' attitudes toward and professional interactions with people with mental disorders. Int J Soc Psychiatry. 2008;54(5):402–413. doi: 10.1177/0020764008090427. [DOI] [PubMed] [Google Scholar]
- 96.Weare R, Green C, Olasoji M, Plummer V. ICU nurses feel unprepared to care for patients with mental illness: a survey of nurses' attitudes, knowledge, and skills. Intensive Crit Care Nurs. 2019;53:37-42. [DOI] [PubMed]
- 97.Winkler P, Mlada K, Janouskova M, Weissova A, Tuskova E, Csemy L, Evans-Lacko S. Attitudes towards the people with mental illness: comparison between Czech medical doctors and general population. Soc Psychiatry Psychiatr Epidemiol. 2016;51(9):1265–1273. doi: 10.1007/s00127-016-1263-y. [DOI] [PubMed] [Google Scholar]
- 98.Woollaston K, Hixenbaugh P. Destructive whirlwind: nurses' perceptions of patients diagnosed with borderline personality disorder. J Psychiatr Ment Health Nurs. 2008;15(9):703–709. doi: 10.1111/j.1365-2850.2008.01275.x. [DOI] [PubMed] [Google Scholar]
- 99.Yildirim M, Demirbuken I, Balci B, Yurdalan U. Beliefs towards mental illness in Turkish physiotherapy students. Physiother Theory Pract. 2015;31(7):461–465. doi: 10.3109/09593985.2015.1025321. [DOI] [PubMed] [Google Scholar]
- 100.Zolnierek CD, Clingerman EM. A medical-surgical nurse's perceptions of caring for a person with severe mental illness. J Am Psychiatric Nurses Assoc. 2012;18(4):226–235. doi: 10.1177/1078390312446223. [DOI] [PubMed] [Google Scholar]
- 101.Airagnes G, Consoli SM, De Morlhon O, Galliot A-M, Lemogne C, Jaury P. Appropriate training based on Balint groups can improve the empathic abilities of medical students: a preliminary study. J Psychosom Res. 2014;76(5):426–429. doi: 10.1016/j.jpsychores.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 102.Arbanas G, Bosnjak D, Sabo T. Impact of a nursing in psychiatry course on Students' attitudes toward mental health disorders. J Psychosoc Nurs Ment Health Serv. 2018;56(3):45–51. doi: 10.3928/02793695-20171024-01. [DOI] [PubMed] [Google Scholar]
- 103.Bannatyne A, Stapleton P. Educating medical students about anorexia nervosa: a potential method for reducing the volitional stigma associated with the disorder. Eat Disord. 2015;23(2):115–133. doi: 10.1080/10640266.2014.976102. [DOI] [PubMed] [Google Scholar]
- 104.Beaulieu T, Lauria-Horner B, Patten S, Knaak S, Weinerman R, Campbell H. Impact of skill-based approaches in reducing stigma in primary care physicians: results from a double-blind, parallel-cluster, randomized controlled trial. Can J Psychiatr. 2017;62(5):327–335. doi: 10.1177/0706743716686919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Bilge A, Palabiyik O. The effect of short films about mental health and disorders on preventing stigmatization in nursing education. Arch Psychiatr Nurs. 2017;31(1):88–92. doi: 10.1016/j.apnu.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 106.Bingham H, O'Brien AJ. Educational intervention to decrease stigmatizing attitudes of undergraduate nurses towards people with mental illness. Int J Ment Health Nurs. 2018;27(1):311–319. doi: 10.1111/inm.12322. [DOI] [PubMed] [Google Scholar]
- 107.Brenner AM. What medical students say about psychiatry: results of a reflection exercise. Acad Psychiatry. 2011;35(3):196–198. doi: 10.1176/appi.ap.35.3.196. [DOI] [PubMed] [Google Scholar]
- 108.Calloway SJ, Young CS, Ward-Smith P, Paulsen L. Management of mental disorders in primary care: the impact of case based learning on nurse practitioner student role perception and stigmatizing attitudes. Nurse Educ Pract. 2017;25:43–49. doi: 10.1016/j.nepr.2017.04.009. [DOI] [PubMed] [Google Scholar]
- 109.Chiles C, Stefanovics E, Rosenheck R. Attitudes of students at a US medical school toward mental illness and its causes. Acad Psychiatry. 2017;41(3):320–325. doi: 10.1007/s40596-016-0508-0. [DOI] [PubMed] [Google Scholar]
- 110.Clement S, van Nieuwenhuizen A, Kassam A, Flach C, Lazarus A, de Castro M, McCrone P, Norman I, Thornicroft G. Filmed v. live social contact interventions to reduce stigma: randomised controlled trial. Br J Psychiatry. 2012;201(1):57–64. doi: 10.1192/bjp.bp.111.093120. [DOI] [PubMed] [Google Scholar]
- 111.Coppens E, Van Audenhove C, Gusmao R, Purebl G, Szekely A, Maxwell M, Koburger N, Arensman E, Hegerl U. Effectiveness of general practitioner training to improve suicide awareness and knowledge and skills towards depression. J Affect Disord. 2018;227:17–23. doi: 10.1016/j.jad.2017.09.039. [DOI] [PubMed] [Google Scholar]
- 112.Crisafulli MA, Von Holle A, Bulik CM. Attitudes towards anorexia nervosa: the impact of framing on blame and stigma. Int J Eat Disord. 2008;41(4):333–339. doi: 10.1002/eat.20507. [DOI] [PubMed] [Google Scholar]
- 113.Crockett J, Taylor S. Rural pharmacist perceptions of a project assessing their role in the management of depression. Aust J Rural Health. 2009;17(5):236–243. doi: 10.1111/j.1440-1584.2009.01084.x. [DOI] [PubMed] [Google Scholar]
- 114.Demiroren M, Saka MC, Senol Y, Senturk V, Baysal O, Oztuna D. The impact of reflective practices on medical students' attitudes towards mental illness. Anadolu Psikiyatri Dergisi. 2016;17(6):466–475. doi: 10.5455/apd.214188. [DOI] [Google Scholar]
- 115.Dipaula BA, Qian J, Mehdizadegan N, Simoni-Wastila L. An elective psychiatric course to reduce pharmacy students' social distance toward people with severe mental illness. Am J Pharm Educ. 2011;75(4):72. doi: 10.5688/ajpe75472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Duffy ME, Henkel KE. Words on walls: passive eating disorder education. Eat Disord. 2016;24(2):148–160. doi: 10.1080/10640266.2015.1034054. [DOI] [PubMed] [Google Scholar]
- 117.Duman Z, Günüşen NP, İnan F, Ince S, Sari A. Effects of two different psychiatric nursing courses on nursing students' attitudes towards mental illness, perceptions of psychiatric nursing, and career choices. J Prof Nurs. 2017;33(6):452–459. doi: 10.1016/j.profnurs.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 118.Economou M, Kontoangelos K, Peppou LE, Arvaniti A, Samakouri M, Douzenis A, Papadimitriou GN. Medical students' attitudes to mental illnesses and to psychiatry before and after the psychiatric clerkship: training in a specialty and a general hospital. Psychiatry Res. 2017;258:108–115. doi: 10.1016/j.psychres.2017.10.009. [DOI] [PubMed] [Google Scholar]
- 119.Economou M, Peppou LE, Louki E, Stefanis CN. Medical students' beliefs and attitudes towards schizophrenia before and after undergraduate psychiatric training in Greece. Psychiatry Clin Neurosci. 2012;66(1):17–25. doi: 10.1111/j.1440-1819.2011.02282.x. [DOI] [PubMed] [Google Scholar]
- 120.Eksteen H-C, Becker PJ, Lippi G. Stigmatization towards the mentally ill: perceptions of psychiatrists, pre-clinical and post-clinical rotation medical students. Int J Soc Psychiatry. 2017;63(8):782–791. doi: 10.1177/0020764017735865. [DOI] [PubMed] [Google Scholar]
- 121.Esen Danacı A, Balıkçı K, Aydın O, Cengisiz C, Uykur AB. The effect of medical education on attitudes towards schizophrenia: a five-year follow-up study. Turk Psikiyatri Derg. 2016;27(3):176–184. [PubMed] [Google Scholar]
- 122.Failde I, Salazar A, Elorza J, Casais L, Pérez V, Martínez LC, Gilaberte I. Spanish medical students' attitudes and views towards mental health and psychiatry: a multicentric cross-sectional study. Acad Psychiatry. 2014;38(3):332–338. doi: 10.1007/s40596-014-0101-3. [DOI] [PubMed] [Google Scholar]
- 123.Fernandez A, Tan KA, Knaak S, Chew BH, Ghazali SS. Effects of brief psychoeducational program on stigma in Malaysian pre-clinical medical students: a randomized controlled trial. Acad Psychiatry. 2016;40(6):905–911. doi: 10.1007/s40596-016-0592-1. [DOI] [PubMed] [Google Scholar]
- 124.Flanagan EH, Buck T, Gamble A, Hunter C, Sewell I, Davidson L. "Recovery Speaks": A Photovoice Intervention to Reduce Stigma Among Primary Care Providers. Psychiatric Serv (Washington, DC) 2016;67(5):566–569. doi: 10.1176/appi.ps.201500049. [DOI] [PubMed] [Google Scholar]
- 125.Fokuo JK, Goldrick V, Rossetti J, Wahlstrom C, Kundert C, Larson J, Corrigan P. Decreasing the stigma of mental illness through a student-nurse mentoring program: a qualitative study. Community Ment Health J. 2017;53(3):257–265. doi: 10.1007/s10597-016-0016-4. [DOI] [PubMed] [Google Scholar]
- 126.Gable KN, Muhlstadt KL, Celio MA. A mental health elective to improve pharmacy students' perspectives on mental illness. Am J Pharm Educ. 2011;75(2):34. doi: 10.5688/ajpe75234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Galletly C, Burton C. Improving medical student attitudes towards people with schizophrenia. Aust New Zealand J Psychiatry. 2011;45(6):473–476. doi: 10.3109/00048674.2011.541419. [DOI] [PubMed] [Google Scholar]
- 128.Gibson R, Carson J, Houghton T. Stigma towards non-suicidal self-harm: evaluating a brief educational intervention. Br J Nurs (Mark Allen Publishing) 2019;28(5):307–312. doi: 10.12968/bjon.2019.28.5.307. [DOI] [PubMed] [Google Scholar]
- 129.Happell B. The importance of clinical experience for mental health nursing - part 1: undergraduate nursing students' attitudes, preparedness and satisfaction. Int J Ment Health Nurs. 2008;17(5):326–332. doi: 10.1111/j.1447-0349.2008.00555.x. [DOI] [PubMed] [Google Scholar]
- 130.Happell B, Platania-Phung C, Scholz B, Bocking J, Horgan A, Manning F, Doody R, Hals E, Granerud A, Lahti M, et al. Changing attitudes: the impact of expert by experience involvement in mental health nursing education: an international survey study. Int J Ment Health Nurs. 2019;28(2):480–491. doi: 10.1111/inm.12551. [DOI] [PubMed] [Google Scholar]
- 131.Hastings T, Kroposki M, Williams G. Can completing a mental health nursing course change Students' attitudes? Issues Mental Health Nurs. 2017;38(5):449–454. doi: 10.1080/01612840.2017.1278810. [DOI] [PubMed] [Google Scholar]
- 132.Itzhaki M, Meridan O, Sagiv-Schifter T, Barnoy S. Nursing Students' attitudes and intention to work with mentally ill patients before and after a planned intervention. Acad Psychiatry. 2017;41(3):337–344. doi: 10.1007/s40596-016-0521-3. [DOI] [PubMed] [Google Scholar]
- 133.Kassam A, Glozier N, Leese M, Loughran J, Thornicroft G. A controlled trial of mental illness related stigma training for medical students. BMC Med Educ. 2011;11:51. doi: 10.1186/1472-6920-11-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Knaak S, Szeto AC, Fitch K, Modgill G, Patten S. Stigma towards borderline personality disorder: effectiveness and generalizability of an anti-stigma program for healthcare providers using a pre-post randomized design. Borderline personality disorder and emotion dysregulation. 2015;2(1):9. doi: 10.1186/s40479-015-0030-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Lam TP, Goldberg D, Tse EYY, Lam KF, Mak KY, Lam EWW. What do primary care doctors get out of a year-long postgraduate course in community psychological medicine? Int J Psychiatry Med. 2011;42(2):133–149. doi: 10.2190/PM.42.2.c. [DOI] [PubMed] [Google Scholar]
- 136.Lam TP, Lam KF, Lam EWW, Sun KS. Does postgraduate training in community mental health make a difference to primary care Physicians' attitudes to depression and schizophrenia? Community Ment Health J. 2015;51(6):641–646. doi: 10.1007/s10597-015-9829-9. [DOI] [PubMed] [Google Scholar]
- 137.Liekens S, Smits T, Laekeman G, Foulon V. A depression training session with consumer educators to reduce stigmatizing views and improve pharmacists' depression care attitudes and practices. Am J Pharm Educ. 2013;77(6):120. doi: 10.5688/ajpe776120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Linville D, Aoyama T, Knoble NB, Gau J. The effectiveness of a brief eating disorder training programme in medical settings. J Res Nurs. 2013;18(6):544–558. doi: 10.1177/1744987112452182. [DOI] [Google Scholar]
- 139.Lyons Z, Janca A. Impact of a psychiatry clerkship on stigma, attitudes towards psychiatry, and psychiatry as a career choice. BMC Med Educ. 2015;15:34. doi: 10.1186/s12909-015-0307-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Manzanera R, Lahera G, Alvarez-Mon MA, Alvarez-Mon M. Maintained effect of a training program on attitudes towards depression in family physicians. Fam Pract. 2018;35(1):61–66. doi: 10.1093/fampra/cmx071. [DOI] [PubMed] [Google Scholar]
- 141.Markstrom U, Gyllensten AL, Bejerholm U, Bjorkman T, Brunt D, Hansson L, Leufstadius C, Sandlund M, Svensson B, Ostman M, et al. Attitudes towards mental illness among health care students at Swedish universities--a follow-up study after completed clinical placement. Nurse Educ Today. 2009;29(6):660–665. doi: 10.1016/j.nedt.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 142.Martinez-Martinez C, Sanchez-Martinez V, Sales-Orts R, Dinca A, Richart-Martinez M, Ramos-Pichardo JD. Effectiveness of direct contact intervention with people with mental illness to reduce stigma in nursing students. Int J Ment Health Nurs. 2019;28(3):735–743. doi: 10.1111/inm.12578. [DOI] [PubMed] [Google Scholar]
- 143.McAllister M, Billett S, Moyle W, Zimmer-Gembeck M. Use of a think-aloud procedure to explore the relationship between clinical reasoning and solution-focused training in self-harm for emergency nurses. J Psychiatr Ment Health Nurs. 2009;16(2):121–128. doi: 10.1111/j.1365-2850.2008.01339.x. [DOI] [PubMed] [Google Scholar]
- 144.McAllister M, Moyle W, Billett S, Zimmer-Gembeck M. 'I can actually talk to them now': qualitative results of an educational intervention for emergency nurses caring for clients who self-injure. J Clin Nurs. 2009;18(20):2838–2845. doi: 10.1111/j.1365-2702.2008.02540.x. [DOI] [PubMed] [Google Scholar]
- 145.Michalak EE, Livingston JD, Maxwell V, Hole R, Hawke LD, Parikh SV. Using theatre to address mental illness stigma: a knowledge translation study in bipolar disorder. Int J Bipolar Disord. 2014;2:1. doi: 10.1186/2194-7511-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Morrison PA. Using an adapted reflecting team approach to learn about mental health and illness with general nursing students: an Australian example. Int J Ment Health Nurs. 2009;18(1):18–25. doi: 10.1111/j.1447-0349.2008.00566.x. [DOI] [PubMed] [Google Scholar]
- 147.Moxham L, Taylor E, Patterson C, Perlman D, Brighton R, Sumskis S, Keough E, Heffernan T. Can a clinical placement influence stigma? An analysis of measures of social distance. Nurse Educ Today. 2016;44:170–174. doi: 10.1016/j.nedt.2016.06.003. [DOI] [PubMed] [Google Scholar]
- 148.Muzyk AJ, Lentz K, Green C, Fuller S, May DB, Roukema L. Emphasizing Bloom's affective domain to reduce pharmacy Students' stigmatizing attitudes. Am J Pharm Educ. 2017;81(2):35. doi: 10.5688/ajpe81235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.O'Connor K, Brennan D, O'Loughlin K, Wilson L, Pillay D, Clarke M, Casey P, Malone K, Lane A. Attitudes towards patients with mental illness in Irish medical students. Ir J Med Sci. 2013;182(4):679–685. doi: 10.1007/s11845-013-0955-5. [DOI] [PubMed] [Google Scholar]
- 150.Omori A, Tateno A, Ideno T, Takahashi H, Kawashima Y, Takemura K, Okubo Y. Influence of contact with schizophrenia on implicit attitudes towards schizophrenia patients held by clinical residents. BMC Psychiatry. 2012;12:205. doi: 10.1186/1471-244X-12-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.O'Reilly CL, Bell JS, Chen TF. Consumer-led mental health education for pharmacy students. Am J Pharm Educ. 2010;74(9):167. doi: 10.5688/aj7409167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.O'Reilly CL, Bell JS, Kelly PJ, Chen TF. Impact of mental health first aid training on pharmacy students' knowledge, attitudes and self-reported behaviour: a controlled trial. Aust New Zealand J Psychiatry. 2011;45(7):549–557. doi: 10.3109/00048674.2011.585454. [DOI] [PubMed] [Google Scholar]
- 153.Papish A, Kassam A, Modgill G, Vaz G, Zanussi L, Patten S. Reducing the stigma of mental illness in undergraduate medical education: a randomized controlled trial. BMC Med Educ. 2013;13:141. doi: 10.1186/1472-6920-13-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Patten SB, Remillard A, Phillips L, Modgill G, Szeto AC, Kassam A, Gardner DM. Effectiveness of contact-based education for reducing mental illness-related stigma in pharmacy students. BMC Med Educ. 2012;12(1):120. doi: 10.1186/1472-6920-12-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Poreddi V, Thimmaiah R, Math SB. Attitudes toward people with mental illness among medical students. J Neurosci Rural Pract. 2015;6(3):349–354. doi: 10.4103/0976-3147.154564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Romem P, Anson O, Kanat-Maymon Y, Moisa R. Reshaping students' attitudes toward individuals with mental illness through a clinical nursing clerkship. J Nurs Educ. 2008;47(9):396–402. doi: 10.3928/01484834-20080901-01. [DOI] [PubMed] [Google Scholar]
- 157.Shen Y, Dong H, Fan X, Zhang Z, Li L, Lv H, Xue Z, Guo X. What can the medical education do for eliminating stigma and discrimination associated with mental illness among future doctors? Effect of clerkship training on chinese students' attitudes. Int J Psychiatry Med. 2014;47(3):241–254. doi: 10.2190/PM.47.3.e. [DOI] [PubMed] [Google Scholar]
- 158.Stacey G, Baldwin V, Thompson BJ, Aubeeluck A. A focus group study exploring student nurse's experiences of an educational intervention focused on working with people with a diagnosis of personality disorder. J Psychiatr Ment Health Nurs. 2018;25(7):390–399. doi: 10.1111/jpm.12473. [DOI] [PubMed] [Google Scholar]
- 159.Stuhlmiller C, Tolchard B. Understanding the impact of mental health placements on student nurses' attitudes towards mental illness. Nurse Educ Pract. 2019;34:25–30. doi: 10.1016/j.nepr.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 160.Telles-Correia D, Gama Marques J, Gramaca J, Sampaio D. Stigma and attitudes towards psychiatric patients in Portuguese medical students. Acta Medica Port. 2015;28(6):715–719. doi: 10.20344/amp.6231. [DOI] [PubMed] [Google Scholar]
- 161.Treloar AJ. Effectiveness of education programs in changing clinicians' attitudes toward treating borderline personality disorder. Psychiatr Serv. 2009;60(8):1128–1131. doi: 10.1176/ps.2009.60.8.1128. [DOI] [PubMed] [Google Scholar]
- 162.Upshur C, Weinreb L. A survey of primary care provider attitudes and behaviors regarding treatment of adult depression: what changes after a collaborative care intervention? Primary Care Companion J Clin Psychiatry. 2008;10(3):182–186. doi: 10.4088/PCC.v10n0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Wang P-W, Ko C-H, Chen C-S, Yang Y-H, Lin H-C, Cheng C-C, Tsang H-Y, Wu C-K, Yen C-F, Yang Y-HC. Changes of explicit and implicit stigma in medical students during psychiatric clerkship. Acad Psychiatry. 2016;40(2):224–228. doi: 10.1007/s40596-015-0432-8. [DOI] [PubMed] [Google Scholar]
- 164.Winkler P, Janouskova M, Kozeny J, Pasz J, Mlada K, Weissova A, Tuskova E, Evans-Lacko S. Short video interventions to reduce mental health stigma: a multi-Centre randomised controlled trial in nursing high schools. Soc Psychiatry Psychiatr Epidemiol. 2017;52(12):1549–1557. doi: 10.1007/s00127-017-1449-y. [DOI] [PubMed] [Google Scholar]
- 165.Clarke D, Usick R, Sanderson A, Giles-Smith L, Baker J. Emergency department staff attitudes towards mental health consumers: a literature review and thematic content analysis. Int J Ment Health Nurs. 2014;23(3):273–284. doi: 10.1111/inm.12040. [DOI] [PubMed] [Google Scholar]
- 166.Rees N, Rapport F, Thomas G, John A, Snooks H. Perceptions of paramedic and emergency care workers of those who self harm: a systematic review of the quantitative literature. J Psychosom Res. 2014;77(6):449–456. doi: 10.1016/j.jpsychores.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 167.Vistorte AOR, Ribeiro WS, Jaen D, Jorge MR, Evans-Lacko S, Mari JJ. Stigmatizing attitudes of primary care professionals towards people with mental disorders: a systematic review. Int J Psychiatry Med. 2018;53(4):317–338. doi: 10.1177/0091217418778620. [DOI] [PubMed] [Google Scholar]
- 168.Petkari E, Masedo Gutierrez AI, Xavier M, Moreno Kustner B. The influence of clerkship on students' stigma towards mental illness: a meta-analysis. Med Educ. 2018;52(7):694–704. doi: 10.1111/medu.13548. [DOI] [PubMed] [Google Scholar]
- 169.Stubbs A. Reducing mental illness stigma in health care students and professionals: a review of the literature. Australas Psychiatry. 2014;22(6):579–584. doi: 10.1177/1039856214556324. [DOI] [PubMed] [Google Scholar]
- 170.McHale J, Felton A. Self-harm: what's the problem? A literature review of the factors affecting attitudes towards self-harm. J Psychiatr Ment Health Nurs. 2010;17(8):732–740. doi: 10.1111/j.1365-2850.2010.01600.x. [DOI] [PubMed] [Google Scholar]
- 171.Saunders KEA, Hawton K, Fortune S, Farrell S. Attitudes and knowledge of clinical staff regarding people who self-harm: a systematic review. J Affect Disord. 2012;139(3):205–216. doi: 10.1016/j.jad.2011.08.024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article. The search strategy is available as an additional file.