Abstract
Background
Atrial fibrillation (AF) is an important risk factor for acute ischemic stroke.
Methods
A nested case–control study was conducted among patients diagnosed with AF, whose information was acquired from the prospective China Atrial Fibrillation Registry (China-AF), from August 2011 to December 2018.
Results
This study compared patients with stroke group (n = 145) with a matched control group (n = 577). Demographic data were similar except for body mass index (BMI), diastolic blood pressure (DBP) which were higher, and new oral anticoagulant (NOAC) treatment rate which was lower in the stroke group (all P < 0.05). Baseline median [IQR] levels of including triglyceride (TG) were higher in the stroke group (21.96 [16.74, 21.52], mg/dL) than the control group (19.62 [14.76, 27.36], mg/dL) (P = 0.012), while the total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C) and high-density lipoprotein cholesterol (HDL-C) were similar between the two groups. Elevated TG and HDL-C were positively associated with ischemic stroke (OR 1.01, 95% CI 1.00–1.02, P = 0.032; OR 1.03, 95% CI 1.00–1.05, P = 0.025), after adjustment for BMI, systolic blood pressure, DBP, CHA2DS2-VASc score, HAS-BLED score, NOAC, LDL-C and HDL-C. However, NOAC (OR 0.20, 95% CI 0.05–0.84, P = 0.029) could decrease the likelihood of ischemic stroke in patients with AF. In subgroup analysis, higher TG level remained significantly associated with ischemic stroke for AF patients without a history of smoking (OR 1.26, 95% CI 1.02–1.55, P = 0.028).
Conclusion
Higher level of TG and HDL-C were positively associated with ischemic stroke in patients with AF.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12872-021-02237-6.
Keywords: Stroke, Risk, Hyperlipidemia, Triglycerides, Atrial fibrillation
Background
Around 16.9 million people suffer a stroke each year and the global burden of stroke is increasing dramatically [1]. China has the biggest stroke burden in the world and about 70% of cases are due to ischemic stroke, when a blood vessel supplying the brain becomes obstructed [2]. Therefore, ischemic stroke is a major cause of morbidity and mortality for Chinese adults. Atrial fibrillation (AF) is an important risk factor for an acute ischemic stroke [3]. Strokes related to AF are also associated with higher mortality and more severe neurologic disability [4]. So, patients with AF are encouraged to consider prevention measures such as oral anticoagulation therapy and modifying their diet and behavior [5].
Dyslipidemia is another well-established risk factor for stroke [6]. Dyslipidemia is implicated in the development of atherosclerosis and coronary heart disease, which are both closely related to AF development [7]. However, while high levels of low-density lipoprotein cholesterol (LDL-C) and low levels of high-density lipoprotein cholesterol (HDL-C) are closely associated with developing coronary artery disease, [7] the relationship with AF is less obvious. Meta-analysis suggests an inverse relationship between serum total cholesterol (TC), LDL-C, and HDL-C levels and AF risk, although there was no significant association between triglyceride (TG) levels and incident AF [8]. However, because both AF and dyslipidemia are independent risk factors for stroke there is a theoretical possibility that patients who experience both may be at greater risk of ischemic stroke.
One study, identified a high level of LDL-C as an independent risk factor for stroke in patients with AF [9]. Another study found that statin use by patients with AF prior to stroke reduced oxidized low-density lipoprotein levels and improved outcomes after stroke [10]. However, large-scale studies are lacking, so it is not clear whether blood lipid levels should be lowered in all patients with AF and if so, the appropriate level of blood lipids needs to be established with quantitative evidence.
Ischemic stroke is a major adverse event in patients with AF, which affects the prognosis of patients [11]. If AF is combined with dyslipidemia, there is a theoretical superposition effect, which further aggravates the occurrence of ischemic stroke [12]. In addition to directly causing ischemic stroke, blood lipid levels also reflect the level of inflammation in patients [13, 14], and studies have shown that blood lipid levels are related to the occurrence of atrial fibrillation [15]. Therefore, in addition to the superposition effect of AF with dyslipidemia, there may also be a synergistic effect, by which this combination further increases the incidence of ischemic stroke. Blood lipid is a risk factor for stroke, but medical personnel primarily focus on controlling the ventricular rate and anticoagulation in patients with AF. Elevated blood lipid levels can cause endothelial inflammation, theoretically increasing the likelihood of forming thrombosis. Thus far, it is unknown whether or not patients with AF need blood lipid management.
Therefore, our study aimed to explore the correlation between baseline blood lipid level and the occurrence of ischemic stroke in patients with AF. The China Atrial Fibrillation Registry (China-AF) is a prospective, multicenter, hospital-based registry of participants diagnosed with AF. This registry, therefore, provides a large amount of real data that can be analyzed and explored, to provide reference levels and evidence for the control of blood lipids in patients with AF.
Methods
Patients
Patients diagnosed with AF from August 2011 to December 2018 were investigated from data from the China-AF study. Details of the China-AF study design have been published previously [16, 17]. Briefly, the China-AF study is a prospective, multicenter, hospital-based registry of patients with AF from 31 hospitals providing AF treatment in Beijing. Beijing Anzhen Hospital, China provided study coordination and site management.
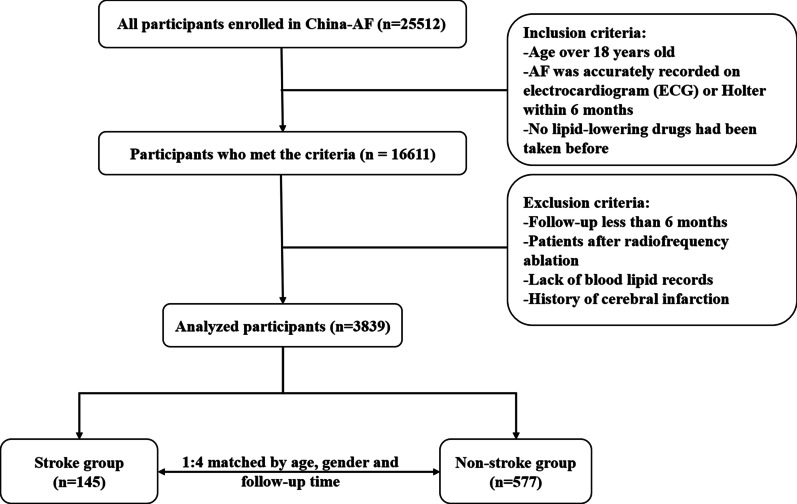
The inclusion criteria were as follows: (1) age over 18 years old; (2) AF was accurately recorded on electrocardiogram (ECG) or Holter within 6 months; (3) no lipid-lowering drugs had been taken before. The exclusion criteria were as follows: (1) follow-up less than 6 months; (2) patients after radiofrequency ablation; (3) lack of blood lipid records; (4) history of cerebral infarction.
This study complied with the standards required for an observational study. The procedures followed were in accordance with the Declaration of Helsinki (2008). Ethical approval was obtained from the Human Research Ethics Committees at Beijing Anzhen Hospital. Reference number: 20110610. The ethics review boards in Beijing Anzhen Hospital, Capital Medical University approved their participation. Each patient provided written informed consent for long-term follow-up. This study was registered (ChiCTR-OCH-13003729.).
Study design
This was a nested case–control study. Patients who were eligible for inclusion in the study and experienced ischemic stroke during the follow-up period were allocated to the stroke group. The remaining population was then matched according to age (difference of < 2 years), gender, and the same follow-up time (in months) with a 1:4 ratio of patients in the stroke group to patients in the non-stroke group.
Clinical data collection and examination method
The baseline data of the patients included age, gender, body mass index (BMI), education background, history of smoking, history of drinking, medical insurance, past history, and medication records, as well as blood pressure, heart rate, and biochemical indicators of the patients recorded at the time of visiting the hospital. Among the biochemical indexes, blood lipid related indexes included TG, TC, HDL-C, and LDL-C. The blood tests were taken at the baseline of the China-AF registry with the requirement of fasting. The information about blood lipids was collected before the onset of stroke without traditional lipid-lowering medication, which could avoid reverse causality inference.
At the same hospital visit, the patients completed a transthoracic echocardiography (TTE) examination, and left atrial inner diameter (LA), left ventricular end-diastolic dimension (LVEDD), left ventricular function (LVEF) were recorded. The type of AF was distinguished between paroxysmal AF and non-paroxysmal AF. The patients’ CHA2DS2-VASc and HAS-BLED scores [18] were evaluated.
Definitions and follow-up
Patients were followed up at 3 months, 6 months, and every 6 months thereafter by trained staff at the outpatient clinics or through telephone interview.
Statistical analysis
During the follow-up period each case that experienced an ischemic stroke was matched with four controls with similar follow-up time. The matching ensured that they had the same gender and were within 2 years of age. The continuous data in normal distribution were presented as mean ± standard deviation, and skewed data were presented as median (interquartile range, IQR). The categorical data were presented as frequency (percentage). Student’s t test or Mann–Whitney U test, and chi-square test was used in comparison between two groups.
Conditional logistic regression models were conducted, taking the occurrence of an ischemic stroke event as the dependent variable, and taking each serum lipid level as an independent variable, adjusted for confounders with important clinical concern. Subgroup analysis was also performed using conditional logistic regression models to explore the associations of serum lipid level and ischemic stroke by different BMI groups, smoking status, alcohol assumption status, different type of AF, history of cardiovascular disease and metabolic disease, different levels of CHA2DS2-VASc scores and HAS-BLED scores; heterogeneity across subgroups was tested by introducing an interaction term of serum lipid level and the grouping variable into models. Two-sided P < 0.05 was considered statistically significant. All statistical analysis was performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Baseline characteristics of the study population
Between August 2011 to December 2018, 16,611 patients were enrolled in the study according to the inclusion criteria. Of these, 2234 patients were excluded due to having less than 6 months of follow-up; 6326, due to previously having undergone radiofrequency ablation; 3675, due to the lack of blood lipid data; and 537, due to the history of cerebral infarction. Finally, 3839 patients were considered for inclusion in this study. Of this population, 145 were eligible for allocation in the stroke group, and the remaining 577 were identified eligible for allocation to the non-stroke control group after matching. Figure 1 presents the patient selection flowchart of this study.
Fig. 1.
Patient selection flowchart
Table 1 presents the baseline data of the study population. Apart from the differences in the BMI, diastolic blood pressure (DBP), and new oral anticoagulant (NOAC) utilization rate between the two groups, the other demographic baseline data were similar between the two groups.
Table 1.
Baseline data of patients
| Characteristics | Stroke (n = 145) | Non-stroke (n = 577) | P value |
|---|---|---|---|
| Demographics | |||
| Age (years), mean ± SD | 70.5 ± 10.7 | 70.5 ± 10.7 | 0.983 |
| Gender (male), n (%) | 78 (53.8) | 309 (53.5) | 0.959 |
| BMI, mean ± SD | 25.5 ± 3.8 | 24.8 ± 3.4 | 0.033 |
| Normal (< 24 kg/m2), n (%) | 40 (31.0) | 211 (40.8) | 0.014 |
| Overweight (24–28 kg/m2), n (%) | 56 (43.4) | 226 (43.7) | – |
| Obese (BMI ≥ 28 kg/m2), n (%) | 33 (25.6) | 80 (15.5) | – |
| Current Smoking, n (%) | 25 (17.2) | 77 (13.3) | 0.229 |
| Current Drinking, n (%) | 25 (17.2) | 99 (17.2) | 0.981 |
| High school completion, n (%) | 39 (26.9) | 134 (23.2) | 0.354 |
| Partial or full health insurance, n (%) | 134 (92.4) | 529 (91.7) | 0.773 |
| Medical history, n (%) | |||
| Cardiovascular System | 50 (34.5) | 191 (33.1) | 0.768 |
| Cerebrovascular system | 6 (4.1) | 18 (3.1) | 0.603 |
| Respiratory system | 1 (0.7) | 9 (1.6) | 0.696 |
| Metabolic disease | 50 (34.5) | 185 (32.1) | 0.620 |
| Vital signs | |||
| SBP (mmHg), mean ± SD | 132.0 ± 17.2 | 129.0 ± 17.0 | 0.058 |
| DBP (mmHg), mean ± SD | 79.0 ± 12.9 | 76.5 ± 11.0 | 0.029 |
| Heart rate (bpm), median (IQR) | 80 (65,94) | 78 (68,92) | 0.969 |
| Laboratory tests | |||
| FBG (mmol/L), median (IQR) | 5.5 (4.9,6.7) | 5.4 (4.9,6.2) | 0.252 |
| eGFR (mL/min/1.73 m2), median (IQR) | 96.0 (80.8,113.9) | 100.8 (81.3,121.22) | 0.284 |
| BNP (pg/mL), median (IQR) | 401.5 (139.0,860.3) | 221.0 (94.0,709.3) | 0.265 |
| NT-pro-BNP (pg/mL), median (IQR) | 1423.0 (682.0,3885.0) | 1129.0 (521.2,2295.0) | 0.233 |
| TTE | |||
| LA (mm), median (IQR) | 41.0 (37.0,46.3) | 42.0 (37.0,46.0) | 0.996 |
| LVEDD (mm), median (IQR) | 47.0 (45.0,52.0) | 48.0 (44.5,52.0) | 0.545 |
| LVEF (%), median (IQR) | 62.0 (55.0,67.0) | 63.0 (58.0,68.0) | 0.069 |
| Atrial fibrillation duration (year), median (IQR) | 2.5 (0.6,5.9) | 2.9 (0.8,8.3) | 0.168 |
| CAD | 18 (12.4) | 47 (8.2) | 0.108 |
| CKD | 11 (7.6) | 35 (6.1) | 0.503 |
| Atrial fibrillation type, n (%) | 0.364 | ||
| Paroxysmal | 62 (42.8) | 271 (47.0) | |
| Non-paroxysmal | 83 (57.2) | 306 (53.0) | |
| Atrial fibrillation type, n (%) | 0.212 | ||
| Valvular | 1 (0.7) | 15 (2.6) | |
| Non-valvular | 144 (99.3) | 562 (97.4) | |
| CHA2DS2-VASc score, n (%) | 3.0 (2.0–4.0) | 3.0 (2.0–4.0) | 0.628 |
| Low/medium risk (≤ 1) | 24 (16.6) | 114 (19.8) | 0.380 |
| High risk (≥ 2) | 121 (83.4) | 463 (80.2) | |
| HAS-BLED score, median (IQR)n (%) | 2.0 (2.0–3.0) | 2.0 (2.0–3.0) | 0.438628 |
| Low risk (< 3) | 84 (57.9) | 347 (60.1) | 0.628 |
| High risk (≥ 3) | 61 (42.1) | 230 (39.9) | |
| Contaminant medications, n (%) | |||
| Antiarrhythmic drugs | 16 (11.0) | 94 (16.3) | 0.123 |
| Ventricular rate control | 91 (62.8) | 341 (59.1) | 0.422 |
| Antithrombotic drugs | |||
| Aspirin | 66 (45.5) | 241 (41.8) | 0.453 |
| Warfarin | 47 (32.4) | 186 (32.2) | 0.967 |
| NOAC | 2 (1.4) | 39 (6.8) | 0.012 |
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; FBG, fasting blood glucose; eGFR, estimated glomerular filtration rate; BNP, B-type natriuretic peptide; NT-pro-BNP, N terminal pro-BNP; TTE, transthoracic echocardiography; LA, left atrial inner diameter; LVEDD, left ventricular end-diastolic dimension; LVEF, left ventricular ejection fraction; CAD, coronary artery disease; CKD, chronic kidney disease; NOAC, new oral anticoagulants
Comparison of blood lipid levels
Table 2 presents the difference in the blood lipid levels between the two groups. The TG level of patients was significantly higher in the stroke group (21.96 [16.74, 21.52]) than in the non-stroke group (19.62 [14.76, 27.36]; P = 0.012). There was no significant difference in the TC, LDL-C, and HDL-C between the groups.
Table 2.
Comparison of blood lipid levels between the stroke and non-stroke groups
| Lipid-related parameters | Stroke (n = 145) | Non-stroke (n = 577) | P value |
|---|---|---|---|
| TG (mg/dLmmol/L), median (IQR) | 21.961.22 (16.740.93, 21.521.64) | 19.621.09 (14.760.82, 27.361.52) | 0.012 |
| TC (mg/dLmmol/L), median (IQR) | 79.924.44 (70.743.93, 94.505.25) | 79.024.39 (66.783.71, 89.104.95) | 0.137 |
| LDL-C (mg/dLmmol/L), median (IQR) | 49.322.74 (36.182.01, 56.343.13) | 46.982.61 (37.082.06, 54.363.02) | 0.3243 |
| HDL-C (mg/dLmmol/L), median (IQR) | 21.061.17 (17.640.98, 25.021.39) | 21.241.18 (17.280.96, 25.021.39) | 0.701 |
TG, triglyceride; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol
Multivariable analysis of factors related to ischemic stroke
Multivariable analysis of the factors associated with the occurrence of ischemic stroke in patients with AF is shown in Table 3 for TG, and Additional file 1: Tables S1, S2 and S3 for TC/LDL-C/HDL-C. The results suggested that the elevation of TG and HDL-C increased the possibility of the occurrence of ischemic stroke in patients with AF (OR 1.05, 95% CI 1.00–1.02, P = 0.032; OR 1.03, 95% CI 1.00–1.05, P = 0.025), indicating that it was an independent risk factor. However, NOAC (OR 0.20, 95% CI 0.05–0.84, P = 0.029) decreased the likelihood of ischemic stroke in patients with AF. The TC and LDL-C showed no independent association with the occurrence of ischemic stroke in AF patients.
Table 3.
Conditional logistic regression analysis of TG level and ischemic stroke
| Univariable analysis | Multivariable analysis | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |
| TG (mg/dLmmol/L) | 1.0122 | 1.003–1.0244 | 0.024 | 1.0120 | 1.001–1.0242 | 0.0325 |
| BMI | 1.06 | 1.01–1.12 | 0.032 | 1.05 | 0.99–1.11 | 0.089132 |
| SBP | 1.01 | 0.99–1.02 | 0.066 | 1.00 | 0.99–1.02 | 0.56216 |
| DBP | 1.02 | 1.00–1.04 | 0.020 | 1.01 | 0.99–1.03 | 0.14780 |
| CHA2DS2-VASc score | ||||||
| Low/medium risk (≤ 1) | Reference | – | – | Reference | – | – |
| High risk (≥ 2) | 1.66 | 0.78–3.51 | 0.187 | 1.327 | 0.602–2.938 | 0.49036 |
| HAS-BLED score | ||||||
| Low risk (< 3) | Reference | – | – | Reference | – | – |
| High risk (≥ 3) | 1.11 | 0.73–1.69 | 0.637 | 0.991.01 | 0.635–1.56 | 0.9750 |
| NOAC | 0.19 | 0.04–0.79 | 0.022 | 0.20 | 0.05–0.84 | 0.029 |
| LDL-C (mg/dL) | 1.01 | 0.99–1.02 | 0.318 | 1.01 | 0.99–1.02 | 0.426 |
| HDL-C (mg/dL) | 1.02 | 0.99–1.04 | 0.163 | 1.03 | 1.00–1.05 | 0.025 |
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; TG, triglyceride; TC, total cholesterol; NOAC, new oral anticoagulant; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol
Subgroup analysis
The results of the subgroup analysis (Table 4) showed, after adjusting for confounders, that TG was associated with the occurrence of ischemic stroke in AF patients without a history of smoking (OR 1.01, 95% CI 15.12–28.08, P = 0.034), patients ≥ 70 years of age (OR 1.02, 95% CI 1.00–1.03; P = 0.036); and AF patients with CHA2DS2-VASc score ≥ 2 (OR 1.01, 95% CI 1.00–1.03, P = 0.047). However, no heterogeneity across subgroups were detected, so it cannot be concluded that the association between blood lipids and stroke in different subgroups was different.
Table 4.
Subgroup analysis of the associations of TG level and ischemic stroke
| Subgroups | TG (mgmol/dL), median (IQR) | OR | 95% CI | P value | P for interaction |
|---|---|---|---|---|---|
| BMI | 0.223263 | ||||
| Normal (< 24 kg/m2) | 18.181.01 (14.220.79, 1.3624.48) | 1.0128 | 0.9769–1.052.38 | 0.556434a | |
| Overweight (24–28 kg/m2) | 20.521.14 (15.300.85, 1.6229.16) | 1.2101 | 0.994–1.0357 | 0.13443a | |
| Obese (BMI ≥ 28 kg/m2) | 24.121.34 (18.181.01, 1.7932.22) | 0.981.07 | 0.9130–3.821.06 | 0.919a629a | |
| Age | 0.306 | ||||
| < 70 | 22.68 (16.20, 31.50) | 1.01 | 0.99–1.02 | 0.547a | |
| ≧70 | 18.90 (14.49, 25.65) | 1.02 | 1.00–1,03 | 0.036a | |
| Smoking | 0.21670 | ||||
| Yes | 18.361.02 (0.14.9483, 28.801.60) | 0.991.02 | 0.9341–1.062.53 | 0.822965a | |
| No | 20.521.14 (15.120.84, 1.5628.08) | 1.0126 | 1.003–1.0355 | 0.03428a | |
| Drinking | 0.73148 | ||||
| Yes | 19.891.11 (14.850.83,1.6128.89) | 1.0239 | 0.9763–1.083.07 | 0.366421a | |
| No | 20.251.13 (15.120.84, 1.5627.90) | 1.2101 | 0.991.00–1.0247 | 0.04961a | |
| Atrial fibrillation type | 0.76370 | ||||
| Paroxysmal | 21.421.19 (15.840.88,1.6229.16) | 1.0232 | 0.995–1.0482 | 0.130094a | |
| Non-paroxysmal | 18.901.05 (14.760.82, 1.4726.46) | 1.0119 | 0.992–1.0354 | 0.216181a | |
| Cardiovascular disease | 0.071062 | ||||
| Yes | 18.001.00 (13.860.77,1.3724.66) | 1.0255 | 0.9988–1.062.75 | 0.265132a | |
| No | 21.421.19 (16.020.89, 1.6229.16) | 1.0111 | 0.9987–1.4202 | 0.339403a | |
| Metabolic disease | 0.462380 | ||||
| Yes | 21.601.20 (16.020.89, 1.7631.68) | 1.0376 | 1.007–1.062.91 | 0.106027a | |
| No | 19.441.08 (0.8214.76, 1.4926.82) | 1.018 | 0.9975–1.0354 | 0.62990a | |
| CHA2DS2-VASc score | 0.29655 | ||||
| Low/medium risk (≤ 1) | 21.601.20 (15.30.85, 1.6830.24) | 1.014 | 0.9644–1.062.47 | 0.804922b | |
| High risk (≥ 2) | 1.0919.62 (15.120.84, 1.5227.27) | 1.0125 | 1.002–1.0352 | 0.04731b | |
| HAS-BLED score | 0.477544 | ||||
| Low risk (< 3) | 21.421.19 (15.300.85, 1.6128.98) | 1.0112 | 0.990–1.0241 | 0.265311c | |
| High risk (≥ 3) | 18.901.05 (14.580.81, 1.4726.46) | 1.3101 | 0.9881–1.042.13 | 0.503279c |
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; TG, triglyceride
aAdjusted by BMI, SBP, DBP, CHA2DS2-VASc score, and HAS-BLED score, NOAC, LDL and HDL
bAdjusted by BMI, SBP, DBP, and HAS-BLED score, NOAC, LDL and HDL
cAdjusted by BMI, SBP, DBP, and CHA2DS2-VASc score, NOAC, LDL and HDL
Discussion
In order to discover whether blood lipid levels are associated with ischemic stroke in patients with AF, this study investigated baseline blood lipid levels and other clinical factors in patients with AF who experienced ischemic stroke and compared them with the values in matched patients with AF who did not experience a stroke. The results show that TG levels were higher in the stroke group than the non-stroke group, but TC, LDL-C and HDL-C were similar. Elevated TG and HDL-C was also associated with ischemic stroke. Subgroup analysis suggested TG remained associated with ischemic stroke in patients with AF over 70 years old, in patients with AF without a history of smoking, and in patients with AF with CHA2DS2-VASc score ≥ 2. Therefore, patients with AF and high TG should consider methods to lower their TG levels, especially if they are over 70 years old, have not smoked, or have CHA2DS2-VASc score ≥ 2.
The relationship between blood lipid levels and the risk of ischemic stroke in patients with AF may be complex. It is generally established that the risk of atherosclerosis increases with higher LDL-C [19]. In general populations at risk of ischemic stroke, statin therapy trials have shown that lowering LDL-C by 1 mmol/L reduces the risk of both ischemic stroke and coronary heart disease by about 20% [20]. On the other hand, observational studies have found stronger effects of LDL-C on coronary heart disease than ischemic stroke [21]. These differences highlight the heterogeneity in the effects of cholesterol on different subtypes of ischemic stroke [22]. In Chinese populations, the LDL-C level tends to be lower than in Western populations. Nevertheless, lowering LDL-C in Chinese populations also showed a benefit in preventing ischemic stroke, even below levels considered a risk in Western populations [23]. In China, a previous study suggested a high level of LDL-C was an independent risk factor for stroke in patients with AF [9]. While another study found that reducing oxidized low-density lipoprotein levels with statins prior to stroke reduced and improved outcomes after stroke in patients with AF [10]. However, this study did not find an independent relationship between high LDL-C level and ischemic stroke risk. This result may be influenced by the results of a study that showed patients with AF have reduced LDL-C levels compared to healthy controls [7].
Low HDL-C was reportedly associated with increased possibility the ischemic stroke [24, 25]. However, most recent meta-analysis of the modifiable and non-modifiable risk factors in the Asian population showed that HDL-C was not significantly associated with ischemic stroke [26], while in the review by Kloska et al. decreased HDL-C have been identified as risk factor and predictor of cardiovascular disease, including stroke, in Caucasian population [27]. Conversely, study by Yang found that higher level of HDL was independent indicators of newly-detected AF [28], while Lee et al., also in the Asian population, reported that high TG and low HDL levels were associated with CHD risk (including risk of ischemic stroke) only in participants with an LDL-C level of ≥ 130 mg/dL, but this was not observed in those participants with lower LDL-C levels [29]. The results of our study suggest that the elevation of HDL-C might increase the possibility of the ischemic stroke in patients with AF. This result needs further confirmation, as it may be influenced by non-categorized HDL-C and a lower portion of NOAC users in the stroke group. This difference might lead to some bias. On the one hand, this may be because NOAC is expensive and patients with stroke already incur healthcare costs. On the other hand, perhaps fewer patients use NOAC due to non-compliance, resulting in an uneven distribution. Since the different distribution of NOAC users could introduce bias, NOAC was included as a covariate in the conditional logistic regression models. Still, regarding NOAC therapy, our findings are in line with previous study, reporting decreased ischemic stroke, remarkably low rate of systemic embolism and bleeding in AF patients [30], which suggests that patients receiving NOAC might have lower rate of ischemic stroke. The results of this study did suggest that TG levels were an important factor in ischemic stroke in patients with AF. High TG levels increase the chance of cardiovascular events due to increased atherosclerosis [31]. TG may also stimulate atherogenesis through availability of excessive free fatty acids, production of proinflammatory cytokines, fibrinogen, coagulation factors and impairment of fibrinolysis [32]. Some studies suggest a direct relationship between TG and stroke [33]. Elevated TG caused in relation to genetic factors may not affect stroke risk [34]. Paradoxically, even low TG levels have been shown to play a role in ischemic stroke. Jain et al. studied patients with acute ischemic stroke and found that low TG level was associated with a worse prognosis [35]. Ryu et al. reported that low serum TG is an independent predictor of mortality after ischemic stroke by non-cardioembolic causes [36]. To date, however, the relationship between TG and ischemic stroke in patients with AF has not been fully established. Thus, the results of this study suggest the need to further investigate the relationship between TG and ischemic stroke in patients with AF. TG-lowering methods including diet and lifestyle changes might be considered. When subgroup analysis was applied, the effect of high TG on ischemic stroke risk was maintained in patients over 70 years old but not in the younger group, those without a history of smoking, and those with CHA2DS2-VASc score ≥ 2. Therefore, patients in these particular subgroups may find that efforts to reduce TG levels yield the most benefit in terms of reduced incidence of stroke.
This study has some limitations. As this study was performed in a Chinese population, its results cannot entirely be generalized outside of this context. Further studies should be performed with patients of a different ethnicity. Of the total of 25,512 patients with AF enrolled in the China-AF study, only 3839 patients were analyzed and only 722 patients were analyzed in both the groups. Therefore, the potential for selection bias must be considered as a limitation. Although the groups were matched, there were some differences between them in terms of the BMI, DBP, and NOAC use, which may have introduced some bias into the results. While TG was identified as being associated with ischemic stroke, we did not identify a clinically meaningful cutoff value and the effect of decreasing TG levels was not investigated. Further prospective, large-scale randomized clinical trials are needed to further provide high-level evidence.
Conclusion
This study showed that patients with AF who experienced ischemic stroke had higher TG levels compared to matched patients with AF without stroke; however, the TC, LDL-C, and HDL-C levels were similar between both patient groups. Multivariate analysis showed that TG, HDL-C and NOAC were associated with ischemic stroke in patients with AF. TG was also found in subgroup analysis of patients with AF for those aged over 70 years, without a history of smoking, and with CHA2DS2-VASc score ≥ 2. These results suggest that studies to investigate the benefit to patients with AF in decreasing TG should be undertaken.
Supplementary Information
Additional file 1. Supplementary Table 1. Multivariable conditional logistic regression analysis for TC related to ischemic stroke. Supplementary Table 2. Multivariable conditional logistic regression analysis for LDL-C related to ischemic stroke. Supplementary Table 3. Multivariable conditional logistic regression analysis for HDL-C related to ischemic stroke.
Acknowledgements
This study was based in part on data from the Chinese Atrial Fibrillation Registry (China-AF). We would like to thank the China-AF investigators for assistance in the data collection.
Abbreviations
- AF
Atrial fibrillation
- China-AF
China Atrial Fibrillation Registry
- BMI
Body mass index
- DBP
Diastolic blood pressure
- LDL-C
Low-density lipoprotein cholesterol
- HDL-C
High-density lipoprotein cholesterol
- TC
Total cholesterol
- TG
Triglyceride
- ECG
Electrocardiogram
- TTE
Transthoracic echocardiography
- LA
Left atrial inner diameter
- LVEDD
Left ventricular end-diastolic dimension
- LVEF
Left ventricular function
Authors' contributions
FL, XD, JD and CM contributed to conception and design of the study. FL drafted the manuscript. LH performed the statistical analysis. CJ and SX organized the database, implemented the study and interpreted the data. XD, JD and CM critically revised the article. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This work was supported by the National Key Research and Development Program of China (grant number: 2016YFC1301002, 2020YFC2004803, and 2016YFC0900901) and Biosense Webster, Inc. The sponsor of the study had no role in study design, data collection, data analyses, data interpretation, nor writing of the report.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The procedures followed were in accordance with the Declaration of Helsinki (2008). Ethical approval was obtained from the Human Research Ethics Committees at Beijing Anzhen Hospital. Reference number: 20110610. The ethics review boards in Beijing Anzhen Hospital, Capital Medical University approved their participation. Each patient provided written informed consent for long-term follow-up. This study was registered (ChiCTR-OCH-13003729.).
Consent for publication
Written informed consent to publish this information was obtained from study participants.
Competing interests
J.-Z.D. has also received honoraria from Johnson & Johnson for giving lectures. C.-S.M. has received honoraria from Bristol-Myers Squibb (BMS), Pfzer, Johnson & Johnson, Boehringer-Ingelheim (BI) and Bayer for giving lectures. Dr X. Du received honoraria from Bayer for giving lectures. All the remaining authors have no disclosures.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bejot Y, Daubail B, Giroud M. Epidemiology of stroke and transient ischemic attacks: current knowledge and perspectives. Rev Neurol (Paris) 2016;172(1):59–68. doi: 10.1016/j.neurol.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 2.Zang S, Shao G, Cui C, Li TN, Huang Y, Yao X, Fan Q, Chen Z, Du J, Jia R, et al. 68Ga-PSMA-11 PET/CT for prostate cancer staging and risk stratification in Chinese patients. Oncotarget. 2017;8(7):12247–12258. doi: 10.18632/oncotarget.14691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Friberg L, Rosenqvist M, Lindgren A, Terent A, Norrving B, Asplund K. High prevalence of atrial fibrillation among patients with ischemic stroke. Stroke. 2014;45(9):2599–2605. doi: 10.1161/STROKEAHA.114.006070. [DOI] [PubMed] [Google Scholar]
- 4.Pistoia F, Sacco S, Tiseo C, Degan D, Ornello R, Carolei A. The epidemiology of atrial fibrillation and stroke. Cardiol Clin. 2016;34(2):255–268. doi: 10.1016/j.ccl.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, Fang MC, Fisher M, Furie KL, Heck DV, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160–2236. doi: 10.1161/STR.0000000000000024. [DOI] [PubMed] [Google Scholar]
- 6.Kopin L, Lowenstein C. Dyslipidemia. Ann Intern Med. 2017;167(11):ITC81–ITC96. doi: 10.7326/AITC201712050. [DOI] [PubMed] [Google Scholar]
- 7.Li ZZ, Du X, Guo XY, Tang RB, Jiang C, Liu N, Chang SS, Yu RH, Long DY, Bai R, et al. Association between blood lipid profiles and atrial fibrillation: a case-control study. Med Sci Monit. 2018;24:3903–3908. doi: 10.12659/MSM.907580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guan B, Li X, Xue W, Tse G, Waleed KB, Liu Y, Zheng M, Wu S, Xia Y, Ding Y. Blood lipid profiles and risk of atrial fibrillation: a systematic review and meta-analysis of cohort studies. J Clin Lipidol. 2020;14(1):133–142. doi: 10.1016/j.jacl.2019.12.002. [DOI] [PubMed] [Google Scholar]
- 9.Qi Z, Chen H, Wen Z, Yuan F, Ni H, Gao W, Shen J, Li J, Lin Y, Shan Y, et al. Relation of low-density lipoprotein cholesterol to ischemic stroke in patients with nonvalvular atrial fibrillation. Am J Cardiol. 2017;119(8):1224–1228. doi: 10.1016/j.amjcard.2016.12.031. [DOI] [PubMed] [Google Scholar]
- 10.Gillessen S, Omlin A, Attard G, de Bono JS, Efstathiou E, Fizazi K, Halabi S, Nelson PS, Sartor O, Smith MR, et al. Management of patients with advanced prostate cancer: recommendations of the St Gallen Advanced Prostate Cancer Consensus Conference (APCCC) 2015. Ann Oncol. 2019;30(12):e3. doi: 10.1093/annonc/mdw180. [DOI] [PubMed] [Google Scholar]
- 11.Seiffge DJ, De Marchis GM, Koga M, Paciaroni M, Wilson D, Cappellari M, Macha MK, Tsivgoulis G, Ambler G, Arihiro S, et al. Ischemic stroke despite oral anticoagulant therapy in patients with atrial fibrillation. Ann Neurol. 2020. [DOI] [PMC free article] [PubMed]
- 12.Zheng S, Yao B. Impact of risk factors for recurrence after the first ischemic stroke in adults: a systematic review and meta-analysis. J Clin Neurosci. 2019;60:24–30. doi: 10.1016/j.jocn.2018.10.026. [DOI] [PubMed] [Google Scholar]
- 13.Feingold KR, Grunfeld C. The effect of inflammation and infection on lipids and lipoproteins. In: Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dhatariya K, Dungan K, Grossman A, Hershman JM, Hofland J, editors. South Dartmouth (MA), Endotext. edn; 2019.
- 14.Zhang Y, Li S, Xu RX, Zhu CG, Guo YL, Wu NQ, Sun J, Li JJ. Systemic inflammatory markers are closely associated with atherogenic lipoprotein subfractions in patients. Mediators Inflamm. 2015;2015:235742. doi: 10.1155/2015/235742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alonso A, Yin X, Roetker NS, Magnani JW, Kronmal RA, Ellinor PT, Chen LY, Lubitz SA, McClelland RL, McManus DD, et al. Blood lipids and the incidence of atrial fibrillation: the multi-ethnic study of Atherosclerosis and the Framingham Heart Study. J Am Heart Assoc. 2014;3(5):e001211. doi: 10.1161/JAHA.114.001211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Du X, Ma C, Wu J, Li S, Ning M, Tang R, Guo X, Long D, Yu R, Sang C, et al. Rationale and design of the Chinese Atrial Fibrillation Registry Study. BMC Cardiovasc Disord. 2016;16:130. doi: 10.1186/s12872-016-0308-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chang SS, Dong JZ, Ma CS, Du X, Wu JH, Tang RB, Xia SJ, Guo XY, Yu RH, Long DY, et al. Current status and time trends of oral anticoagulation use among Chinese patients with nonvalvular atrial fibrillation: the Chinese atrial Fibrillation Registry Study. Stroke. 2016;47(7):1803–1810. doi: 10.1161/STROKEAHA.116.012988. [DOI] [PubMed] [Google Scholar]
- 18.Lane DA, Lip GY. Use of the CHA(2)DS(2)-VASc and HAS-BLED scores to aid decision making for thromboprophylaxis in nonvalvular atrial fibrillation. Circulation. 2012;126(7):860–865. doi: 10.1161/CIRCULATIONAHA.111.060061. [DOI] [PubMed] [Google Scholar]
- 19.Fernandez-Friera L, Fuster V, Lopez-Melgar B, Oliva B, Garcia-Ruiz JM, Mendiguren J, Bueno H, Pocock S, Ibanez B, Fernandez-Ortiz A, et al. Normal LDL-cholesterol levels are associated with subclinical atherosclerosis in the absence of risk factors. J Am Coll Cardiol. 2017;70(24):2979–2991. doi: 10.1016/j.jacc.2017.10.024. [DOI] [PubMed] [Google Scholar]
- 20.Cholesterol Treatment Trialists C, Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, Peto R, Barnes EH, Keech A, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376(9753):1670–1681. [DOI] [PMC free article] [PubMed]
- 21.Emerging Risk Factors C, Di Angelantonio E, Sarwar N, Perry P, Kaptoge S, Ray KK, Thompson A, Wood AM, Lewington S, Sattar N, et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009;302(18):1993–2000. [DOI] [PMC free article] [PubMed]
- 22.Valdes-Marquez E, Parish S, Clarke R, Stari T, Worrall BB, ISGC MCot, Hopewell JC. Relative effects of LDL-C on ischemic stroke and coronary disease: a Mendelian randomization study. Neurology. 2019;92(11):e1176–e1187. [DOI] [PMC free article] [PubMed]
- 23.Sun L, Clarke R, Bennett D, Guo Y, Walters RG, Hill M, Parish S, Millwood IY, Bian Z, Chen Y, et al. Causal associations of blood lipids with risk of ischemic stroke and intracerebral hemorrhage in Chinese adults. Nat Med. 2019;25(4):569–574. doi: 10.1038/s41591-019-0366-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tziomalos K, Giampatzis V, Bouziana SD, Spanou M, Kostaki S, Papadopoulou M, Angelopoulou SM, Tsopozidi M, Savopoulos C, Hatzitolios AI. Prognostic significance of major lipids in patients with acute ischemic stroke. Metab Brain Dis. 2017;32(2):395–400. doi: 10.1007/s11011-016-9924-9. [DOI] [PubMed] [Google Scholar]
- 25.Gu X, Li Y, Chen S, Yang X, Liu F, Li Y, Li J, Cao J, Liu X, Chen J, et al. Association of lipids with ischemic and hemorrhagic stroke: a prospective cohort study among 267 500 Chinese. Stroke. 2019;50(12):3376–3384. doi: 10.1161/STROKEAHA.119.026402. [DOI] [PubMed] [Google Scholar]
- 26.Cui Q, Naikoo NA. Modifiable and non-modifiable risk factors in ischemic stroke: a meta-analysis. Afr Health Sci. 2019;19(2):2121–2129. doi: 10.4314/ahs.v19i2.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kloska A, Malinowska M, Gabig-Ciminska M, Jakobkiewicz-Banecka J. Lipids and lipid mediators associated with the risk and pathology of ischemic stroke. Int J Mol Sci. 2020;21(10):3618. doi: 10.3390/ijms21103618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang X, Li S, Zhao X, Liu L, Jiang Y, Li Z, Wang Y, Wang Y. Atrial fibrillation is not uncommon among patients with ischemic stroke and transient ischemic stroke in China. BMC Neurol. 2017;17(1):207. doi: 10.1186/s12883-017-0987-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee JS, Chang PY, Zhang Y, Kizer JR, Best LG, Howard BV. Triglyceride and HDL-C dyslipidemia and risks of coronary heart disease and ischemic stroke by glycemic dysregulation status: the strong heart study. Diabetes Care. 2017;40(4):529–537. doi: 10.2337/dc16-1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gui YY, Zou S, Yang WL, Gong SZ, Cen ZF, Xie ZH, Cui KJ. The impact of renal function on efficacy and safety of new oral anticoagulant in atrial fibrillation patients: a systemic review and meta-analysis. Medicine (Baltimore) 2019;98(48):e18205. doi: 10.1097/MD.0000000000018205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Budoff M. Triglycerides and triglyceride-rich lipoproteins in the causal pathway of cardiovascular disease. Am J Cardiol. 2016;118(1):138–145. doi: 10.1016/j.amjcard.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 32.Tenenbaum A, Klempfner R, Fisman EZ. Hypertriglyceridemia: a too long unfairly neglected major cardiovascular risk factor. Cardiovasc Diabetol. 2014;13:159. doi: 10.1186/s12933-014-0159-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Labreuche J, Touboul PJ, Amarenco P. Plasma triglyceride levels and risk of stroke and carotid atherosclerosis: a systematic review of the epidemiological studies. Atherosclerosis. 2009;203(2):331–345. doi: 10.1016/j.atherosclerosis.2008.08.040. [DOI] [PubMed] [Google Scholar]
- 34.Hindy G, Engstrom G, Larsson SC, Traylor M, Markus HS, Melander O, Orho-Melander M, Stroke Genetics N. Role of blood lipids in the development of ischemic stroke and its subtypes: a mendelian randomization study. Stroke. 2018;49(4):820–827. doi: 10.1161/STROKEAHA.117.019653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jain M, Jain A, Yerragondu N, Brown RD, Rabinstein A, Jahromi BS, Vaidyanathan L, Blyth B, Stead LG. The triglyceride paradox in stroke survivors: a prospective study. Neurosci J. 2013;2013:870608. doi: 10.1155/2013/870608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ryu WS, Lee SH, Kim CK, Kim BJ, Yoon BW. Effects of low serum triglyceride on stroke mortality: a prospective follow-up study. Atherosclerosis. 2010;212(1):299–304. doi: 10.1016/j.atherosclerosis.2010.05.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Supplementary Table 1. Multivariable conditional logistic regression analysis for TC related to ischemic stroke. Supplementary Table 2. Multivariable conditional logistic regression analysis for LDL-C related to ischemic stroke. Supplementary Table 3. Multivariable conditional logistic regression analysis for HDL-C related to ischemic stroke.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.