Abstract
Direct oral anticoagulants (DOACs) are not recommended in COVID-19 patients receiving dexamethasone because of potential drug-drug and drug-disease interactions affecting anticoagulant concentration and activity. To evaluate short- and long-term pharmacokinetic interactions, serial through and peak DOAC plasma levels were prospectively measured during and after dexamethasone therapy, as well as during the acute phase and after recovery from COVID-19 in hospitalized, non-critically ill patients undergoing treatment with DOACs. Thirty-three (18 males, mean age 79 years) consecutive patients received DOACs (17 apixaban, 12 rivaroxaban, 4 edoxaban) for atrial fibrillation (n = 22), venous thromboembolism (n = 10), and acute myocardial infarction (n = 1). Twenty-six patients also received dexamethasone at a dose of 6 mg once daily for a median of 14 days. Trough DOAC levels on dexamethasone were within and below expected reference ranges respectively in 87.5 and 8.3% of patients, with no statistically significant differences at 48–72 h and 14–21 days after dexamethasone discontinuation. Peak DOAC levels on dexamethasone were within expected reference ranges in 58.3% of patients, and below ranges in 33.3%, of whom over two thirds had low values also off dexamethasone. No significant differences in DOAC levels were found during hospitalization and after resolution of COVID-19. Overall, 28 patients were discharged alive, and none experienced thrombotic or bleeding events. In this study, dexamethasone administration or acute COVID-19 seemed not to affect DOAC levels in hospitalized, non-critically ill COVID-19 patients.
Keywords: COVID-19, Dexamethasone, Anticoagulants, Apixaban, Rivaroxaban, Embolism, Thrombosis
Highlights
The effects of dexamethasone and COVID-19 on DOAC plasma levels are uncertain.
We serially measured through and peak DOAC levels in COVID-19 inpatients receiving intravenous dexamethasone.
Dexamethasone use or acute COVID-19 did not to systematically affect DOAC concentrations.
DOAC anticoagulant activity may be preserved in this patient population.
Introduction
Venous and arterial thromboembolism represent frequent complications of COVID-19, affecting around 15 and 5% of hospitalized patients, respectively [1, 2]. Due to the relatively elderly age as well as the direct and indirect effects of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), atrial fibrillation is also highly prevalent in this patient population, with estimates ranging from 10 to 13% [3]. Adequate anticoagulation is therefore crucial in COVID-19 [2, 3]. Current guidelines suggest low-molecular-weight heparins as the preferred anticoagulants in hospitalized COVID-19 patients [1, 4]. Direct oral anticoagulants (DOACs) generally represent the first-line anticoagulants for patients with venous thromboembolism or atrial fibrillation, however, their safety and efficacy remain uncertain in COVID-19 [5]. One of the potential reasons for concern is the pharmacological interaction between DOACs and COVID-19 medications [6], which may interfere with cytochrome CP450, mainly CYP3A4, or transporter permeability glycoprotein (P-gp), and affect DOAC clearance and half-life [6–8]. Of note, dexamethasone, administered intravenously at a dose of 6 mg, has become standard-of-care for the treatment of hypoxemic COVID-19 patients [4]. Whether concomitant administration of DOACs and dexamethasone, a well-known inducer of both CYP3A4 and P-gp [9, 10], results in lower DOAC concentrations that may be clinically relevant is currently uncertain [6, 7, 11].
In addition, the coagulation abnormalities associated with COVID-19, including increased concentrations of coagulation factors such as activated factor X, may potentially reduce DOAC efficacy [1, 12]. Pharmacokinetic data on DOACs in COVID-19 are therefore urgently needed.
The aim of this study was to evaluate the impact of concomitant dexamethasone administration and moderate-to-severe COVID-19 on DOAC plasma levels.
Methods
Prospective study of patients admitted to the Divisions of Internal Medicine and Pulmonary Medicine of “SS. Annunziata” Hospital, Chieti, Italy for COVID-19 not requiring invasive mechanical ventilation and receiving DOACs. To assess the short- and long-term impact of dexamethasone, DOAC levels were measured at 48–72 h from the first dose of dexamethasone, and at 48–72 h and 14–21 days from the last dose of dexamethasone. To evaluate the influence of COVID-19, DOAC levels were measured during the acute hospital phase and after recovery from COVID-19. Trough samples were collected about 30 min before DOAC administration, whereas peak samples were collected on the same day, at 2–4 h from DOAC administration. DOAC levels, expressed as drug concentration-equivalent (ng/mL), were measured using chromogenic assays calibrated for apixaban, edoxaban, rivaroxaban (Biophen Dixal Coachrom, Hyphen Biomed, France), and dabigatran (Innovance DTI Assay, Siemens Healthineers AG, Germany). DOAC plasma levels at steady state were compared with the expected reference ranges derived from international consensus guidelines [7]. Clinical outcomes including symptomatic venous and arterial thromboembolism, bleeding, and death were recorded throughout the study period. The study was approved by the local Ethics Committee, and all patients gave their written informed consent before enrollment.
Continuous variables were presented as median and interquartile range, categorical variables as number and percentage. Mean differences in basal characteristics were tested using Fisher exact test and Kruskal-Wallis test, as appropriate. Between- and within-group differences in mean DOAC levels were tested using T-student test for independent samples. We used a two-sided alpha level of 0.05 for all statistical tests. All analyses were performed using R software, version 4.0.4 and Rstudio version 1.1.423—© 2009–2018 RStudio, Inc.
Results
Out of 265 COVID-19 patients admitted at our center between December 11, 2020 and May 18, 2021, 33 (12.4%, 18 males, median age 82 years) received DOAC and were consecutively enrolled (Table 1). Seventeen (51.5%) patients received apixaban, 12 (36.4%) rivaroxaban, and four (12.1%) edoxaban at the recommended doses. The indication for DOACs was atrial fibrillation in 22 (66.7%) cases, venous thromboembolism in 10 (30.3%), and acute myocardial infarction in one (3.0%). Twenty-six patients requiring supplemental oxygen also received intravenous dexamethasone at a dose of 6 mg once daily for a median of 14 days (range 3 to 23 days). No other drug potentially interfering with CYP3A4 or P-gp activity was administered, except for remdesivir, which was used in one patient.
Table 1.
Baseline characteristics of study population
| Overall N = 33 |
Dexamethasone group N = 26 |
No-dexamethasone group N = 7 |
P-values | |
|---|---|---|---|---|
| Sex, female, n (%) | 15 (45.5) | 10 (38.5) | 5 (71.4) | 0.203 |
| Age, years, median (IQR) | 82.0 (76.0, 86.0) | 83.0 (78.0, 86.0) | 79.0 (71.0, 84.5) | 0.427 |
| BMI, median (IQR) | 26.8 (25.0, 30.1) | 26.9 (25.0, 28.8) | 26.30 (24.6, 32.6) | 0.692 |
| Oral anticoagulant, n (%) | 0.54 | |||
| Apixaban 2.5 mg | 10 (30.3) | 7 (26.9) | 3 (42.9) | |
| Apixaban 5 mg BID | 5 (15.2) | 4 (15.4) | 1 (14.3) | |
| Apixaban 10 mg BID | 2 (6.1) | 2 (7.7) | 0 (0.0) | |
| Edoxaban 30 mg | 2 (6.1) | 1 (3.8) | 1 (14.3) | |
| Edoxaban 60 mg | 2 (6.1) | 1 (3.8) | 1 (14.3) | |
| Rivaroxaban 10 mg | 1 (3.0) | 1 (3.8) | 0 (0.0) | |
| Rivaroxaban 15 mg | 4 (12.1) | 3 (11.5) | 1 (14.3) | |
| Rivaroxaban 20 mg | 7 (21.2) | 7 (26.9) | 0 (0.0) | |
| New users, n (%) | 20 (60.6) | 15 (57.7) | 5 (71.4) | 0.676 |
| Anticoagulation indication, n (%) | 1 | |||
| Atrial fibrillation | 22 (66.7) | 17 (65.4) | 5 (71.4) | |
| Myocardial infarction | 1 (3.0) | 1 (3.8) | 0 (0.0) | |
| Venous thromboembolism | 10 (30.3) | 8 (30.8) | 2 (28.6) | |
| COVID-19 severity, n (%) | 0.001 | |||
| Moderate | 9 (27.3) | 3 (11.5) | 6 (85.7) | |
| Severe | 24 (72.7) | 23 (88.5) | 1 (14.3) | |
| Prior venous thromboembolism, n (%) | 3 (9.1) | 2 (7.7) | 1 (14.3) | 0.523 |
| Prior myocardial infarction, n (%) | 7 (21.2) | 5 (19.2) | 2 (28.6) | 0.623 |
| Prior stroke/TIA, n (%) | 2 (6.1) | 1 (3.8) | 1 (14.3) | 0.384 |
| Prior bleeding, n (%) | 3 (9.1) | 1 (3.8) | 2 (28.6) | 0.106 |
| Hypertension, n (%) | 23 (69.7) | 18 (69.2) | 5 (71.4) | 1 |
| Diabetes, n (%) | 13 (39.4) | 9 (34.6) | 4 (57.1) | 0.393 |
| Active cancer, n (%) | 2 (6.1) | 2 (7.7) | 0 (0.0) | 1 |
| Ventilation type, n (%) | 0.001 | |||
| Nasal cannula/venturi mask | 18 (54.5) | 17 (65.4) | 1 (14.3) | |
| CPAP | 5 (15.2) | 5 (19.2) | 0 (0.0) | |
| NIV | 7 (6.1) | 7 (7.7) | 0 (0.0) | |
| d-dimer, mcg/mL, median (IQR) | 1.09 (0.59, 2.28) | 1.14 (0.54, 2.26) | 1.09 (0.76, 2.37) | 0.843 |
| CRP, mg/L, median (IQR) | 64.20 (41.35, 124.50) | 85.16 (47.61, 129.50) | 24.06 (10.14, 54.48) | 0.014 |
IQR interquartile range, BID bis in die, the anticoagulant was administered once daily where not specified, BMI body mass index, TIA transient ischemic attack, CPAP continuous positive airway pressure, NIV non-invasive ventilation, CRP C-reactive protein. P-values were calculated with Fisher exact test and Kruskal–Wallis test as appropriate
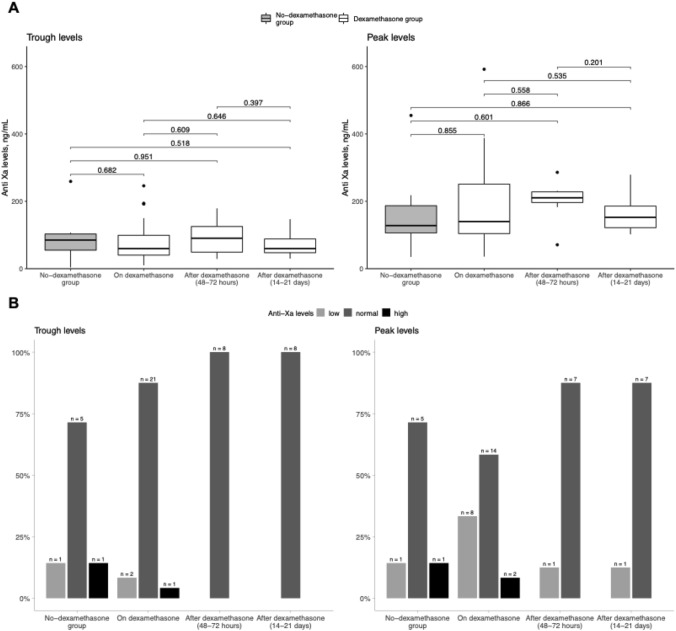
There were no differences in mean trough and peak DOAC plasma levels as measured at 48–72 h from dexamethasone initiation, and at 48–72 h and 14–21 days after dexamethasone discontinuation. Likewise, dexamethasone-treated patients showed similar mean DOAC levels to those of patients not receiving dexamethasone (Fig. 1A). During concomitant dexamethasone administration, trough DOAC levels were within the expected reference ranges in 21 (87.5%) patients, below ranges in two (8.3%) and above ranges in one (4.2%) (Fig. 1B). The corresponding values for peak levels were 14 (58.3%), eight (33.3%), and two (8.3%). Of note, six out of eight patients, all receiving rivaroxaban, with low peak DOAC levels on dexamethasone, displayed similarly low values off dexamethasone.
Fig. 1.
Panel A shows DOAC plasma levels according to dexamethasone use; Panel B shows the distribution of patients with DOAC levels within, below and above the expected reference ranges in relation to dexamethasone use
When patients were stratified according to DOAC type, none of the 11 (45.8%) patients treated with a twice daily dose of apixaban had both trough and peak levels outside the expected reference ranges during concomitant dexamethasone use, one patient had low trough and one high peak values. Among 13 (54.2%) patients receiving a once daily dose of DOAC (11 rivaroxaban, 2 edoxaban), only one who was treated with rivaroxaban had both trough and peak levels below the expected reference ranges. Two patients, one on edoxaban and one on rivaroxaban, had high peak drug levels during dexamethasone and normal levels when off dexamethasone.
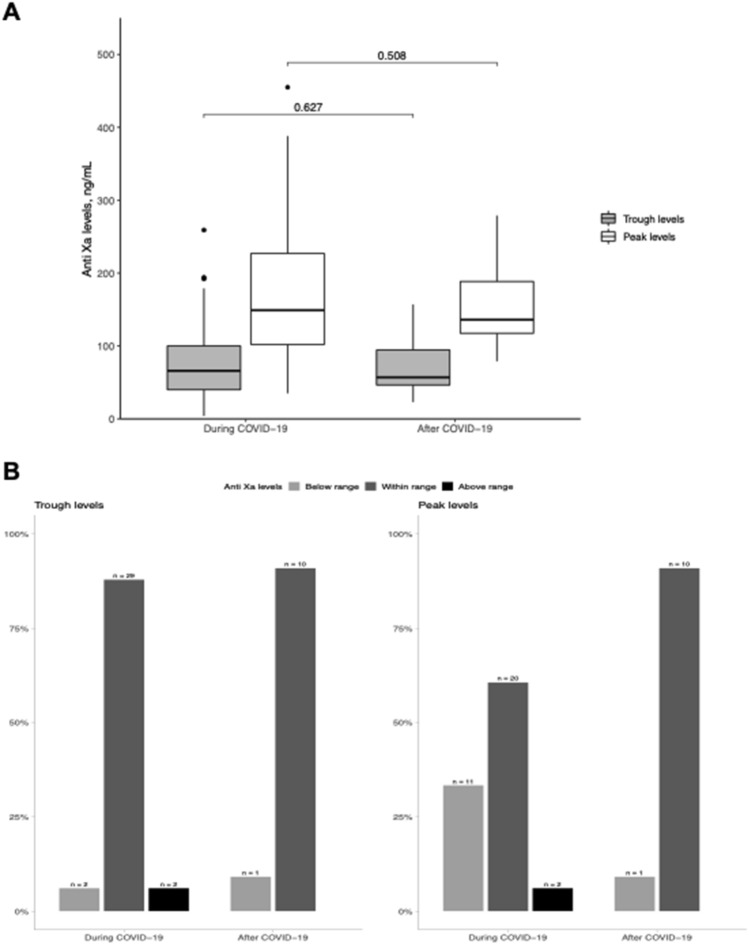
Both mean through and peak DOAC levels as well as the proportion of patients with values within ranges were similar during hospitalization and after recovery from COVID-19 (Fig. 2).
Fig. 2.
Panel A shows DOAC plasma levels as measured during and after recovery from COVID-19 in the overall study population; Panel B shows the distribution of DOAC levels within, below and above the expected reference ranges in relation to COVID-19
Overall, 28 patients were discharged alive after a median of 14 days (interquartile range 9.0, 22.0). During a median of 36 days (interquartile range 28.0, 73.5) after hospital discharge, seven patients died, and none developed symptomatic thromboembolic or bleeding events.
Discussion
In this study, intravenous dexamethasone at a dose of 6 mg once daily for a median of 14 days, and up to 23 days, was not associated with short- and long-term reductions in DOAC plasma levels among hospitalized, non-critically ill COVID-19 patients. Low-molecular-weight heparins are the suggested anticoagulants in hospitalized COVID-19 patients according to expert consensus guidelines [4]. Drugs employed for COVID-19, particularly those interacting with CYP3A4 and P-gp metabolic pathways, may affect the pharmacokinetic and pharmacodynamic profiles of DOACs, thereby altering their anticoagulant activity [6–8]. Dexamethasone, an inducer of both CYP3A4 and P-gp, may reduce bioavailability and increase clearance of DOACs, potentially leading to reduced plasma concentrations [9–11]. Although it remains possible that a longer exposure or higher doses of dexamethasone would result in clinically relevant effects, our data, which confirm and expand previous preliminary findings, seem to be reassuring as they suggest that relevant systematic interactions, if any, are unlikely [13]. However, the current findings are limited by the small number of patients included, both overall and by DOAC type, which hampers firm conclusions on DOAC safety and efficacy in COVID-19. Since all patients received activated factor X inhibitors, results may not apply to patients receiving dabigatran.
Increased levels of pro-inflammatory cytokines, as observed in COVID-19, have been linked to downregulation of hepatic drug-metabolizing enzymes including CYP3A4, which could counteract the enzyme-inducing effects of dexamethasone [14, 15]. Furthermore, the coagulopathy associated with SARS-CoV-2 may result in altered concentrations of coagulation factors, including higher levels of activated factor X, and influence DOAC anticoagulant activity [1, 12]. We found that DOAC levels following resolution of COVID-19 were similar to those observed during the acute phase of disease, suggesting that both SARS-CoV-2 and the associated inflammatory response may not have a relevant impact on DOAC anticoagulant activity. It is worth pointing out that reference ranges adopted for DOAC plasma levels are subject to high inter-individual variability and do not represent the optimal therapeutic window [16]. Therefore, despite there were no thrombotic or bleeding complications during DOAC treatment, it cannot be excluded that patients with DOAC concentrations within the expected reference ranges may still experience such events. Adequately powered randomized trials evaluating the pharmacological and clinical profiles of DOACs in COVID-19 are urgently needed to inform on the optimal anticoagulation strategy in these patients.
Conclusions
In hospitalized, non-critically ill COVID-19 patients, concomitant dexamethasone administration and the acute phase of disease did not systematically alter DOAC plasma levels, suggesting that anticoagulant activity of DOACs may be preserved in this patient population.
Author contributions
Concept and design: NP, MC, MDN. Acquisition, analysis, or interpretation of data: NP, MC, EP, CF, MDN. Drafting of the manuscript: NP, MC, MDN. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: MC. Administrative, technical, or material support: CF, RA. Dr. MDN had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Funding
There was no funding source for this study.
Data availability
The data supporting the findings of this study are available from the corresponding author, upon reasonable request.
Declarations
Conflict of interest
Dr. Di Nisio reports personal fees from Bayer, Daiichi Sankyo, Sanofi, Pfizer, Leo Pharma, and Aspen outside of the submitted work. All other authors have nothing to disclose.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Piazza G, Morrow DA. Diagnosis, management, and pathophysiology of arterial and venous thrombosis in covid-19. J Am Med Assoc. 2020;324(24):2548–2549. doi: 10.1001/jama.2020.23422. [DOI] [PubMed] [Google Scholar]
- 2.Tan BK, Mainbourg S, Friggeri A, et al. Arterial and venous thromboembolism in COVID-19: a study-level meta-analysis. Thorax. 2021;10:20. doi: 10.1136/thoraxjnl-2020-215383. [DOI] [PubMed] [Google Scholar]
- 3.Musikantow DR, Turagam MK, Sartori S, et al. Atrial fibrillation in patients hospitalized with COVID-19. JACC Clin Electrophysiol. 2021;10:20. doi: 10.1016/j.jacep.2021.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.COVID-19 Treatment Guidelines. Accessed June 14 (2021) https://www.covid19treatmentguidelines.nih.gov/
- 5.Talasaz AH, Sadeghipour P, Kakavand H, et al. Recent Randomized Trials of Antithrombotic Therapy for Patients With COVID-19: JACC State-of-the-Art Review. J Am Coll Cardiol. 2021;77(15):1903–1921. doi: 10.1016/j.jacc.2021.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liverpool COVID-19 Interactions. Accessed June 15 (2021) https://www.covid19-druginteractions.org/prescribing-resources
- 7.Steffel J, Collins R, Antz M, et al. European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. EP Eur. 2021;20:19. doi: 10.1093/europace/euab065. [DOI] [PubMed] [Google Scholar]
- 8.Testa S, Prandoni P, Paoletti O, et al. Direct oral anticoagulant plasma levels’ striking increase in severe COVID-19 respiratory syndrome patients treated with antiviral agents: the Cremona experience. J Thromb Haemost. 2020;18(6):1320–1323. doi: 10.1111/JTH.14871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teo YL, Saetaew M, Chanthawong S, et al. Effect of CYP3A4 inducer dexamethasone on hepatotoxicity of lapatinib: Clinical and in vitro evidence. Breast Cancer Res Treat. 2012;133(2):703–711. doi: 10.1007/s10549-012-1995-7. [DOI] [PubMed] [Google Scholar]
- 10.Narang VS, Fraga C, Kumar N, et al. Dexamethasone increases expression and activity of multidrug resistance transporters at the rat blood–brain barrier. Am J Physiol - Cell Physiol. 2008;295(2):C440. doi: 10.1152/ajpcell.00491.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smythe M, Burns C, Liu Q, Garwood C. Potential dexamethasone-direct oral anticoagulant drug interaction: is this a concern in COVID? Ann Pharmacother. 2021;17:106002802110250. doi: 10.1177/10600280211025042. [DOI] [PubMed] [Google Scholar]
- 12.Frydman GH, Streiff MB, Connors JM, Piazza G. The potential role of coagulation factor Xa in the pathophysiology of COVID-19: a role for anticoagulants as multimodal therapeutic agents. TH Open. 2020;04(04):e288–e299. doi: 10.1055/s-0040-1718415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bosch FTM, Candeloro M, Potere N, et al. Effect of dexamethasone on direct Xa-inhibitor oral anticoagulant plasma levels in patients with COVID-19. Thromb Res. 2021;205:106–109. doi: 10.1016/J.THROMRES.2021.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aitken AE, Morgan ET. Gene-specific effects of inflammatory cytokines on cytochrome P450 2C, 2B6 and 3A4 mRNA levels in human hepatocytes. Drug Metab Dispos. 2007;35(9):1687–1693. doi: 10.1124/dmd.107.015511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dickmann J, Patel LK, Wienkers SC, Greg Slatter L. Effects of interleukin 1β (IL-1β) and IL-1β/interleukin 6 (IL-6) combinations on drug metabolizing enzymes in human hepatocyte culture. Curr Drug Metab. 2012;13(7):930–937. doi: 10.2174/138920012802138642. [DOI] [PubMed] [Google Scholar]
- 16.Testa S, Tripodi A, Legnani C, et al. Plasma levels of direct oral anticoagulants in real life patients with atrial fibrillation: Results observed in four anticoagulation clinics. Thromb Res. 2016;137:178–183. doi: 10.1016/j.thromres.2015.12.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the findings of this study are available from the corresponding author, upon reasonable request.