Abstract
We study the impact of new information on people’s perceptions of the risks of e-cigarettes. In September 2019 the U.S. experienced an outbreak of e-cigarette, or vaping, associated lung injuries (EVALI). The EVALI outbreak created an information shock, which was followed by additional new information in a later CDC recommendation. We use data on consumer risk perceptions from two sets of surveys conducted before (HINTS survey data) and during the EVALI outbreak (Google Survey data). The empirical model examines changes in risk perceptions during the early crisis period when the CDC was warning consumers that they should avoid all vaping products and during a later period when the message was refined and focused on a narrower set of illegal vaping products that contain THC (the main psychoactive compound in marijuana). Econometric results suggest that the immediate impact of the first information shock was to significantly increase the fraction of respondents who perceived e-cigarettes as more harmful than smoking. As the outbreak subsided and the CDC recommendation changed to emphasize the role of THC e-cigarette products, e-cigarette risk perceptions were only partially revised downwards. Individuals who had higher risk perceptions showed a weaker response to the first information shock but were more likely to later revise their risk perceptions downwards. We conclude the paper by discussing the public policy issues that stem from having risk perceptions of e-cigarette relative to combustible cigarettes remain at these elevated levels where a substantial portion of consumers believe that e-cigarettes are more harmful than cigarettes.
JEL Codes: D8, D18, D83, H12, I12, I18, K0
Keywords: information, smoking, e-cigarette, vaping, health, risk-perception, EVALI, lung injury
I. Introduction
The dissemination of evolving science about health risks related to food and drug products has enormous potential to influence consumer welfare. In typical markets consumers obtain information about product risk from a variety of sources that include the product’s manufacturer through advertising and any associated required warning statements, dissemination in the news media of the results of scientific studies regarding product risk, government pronouncements from agencies such as the Centers for Disease Control and Prevention (CDC), the Surgeon General, the Consumer Product Safety Commission, and the Food and Drug Administration (FDA), and finally through broad social and conventional media coverage of such risks. All of these sources of information have the potential to influence risk perceptions of the product, and in turn affect consumers’ utilization behaviors.
This study focuses on the evolution of risk perceptions of e-cigarettes relative to combustible cigarettes. The formation of health risk beliefs in this market is especially interesting because of the active role that the government has played in messaging about e-cigarettes, the restrictions that the FDA has placed on any reduced-harm statements in advertising and promotion from the industry, and the recent health concerns about vaping products in general and vaping products that contain Tetrahydrocannabinol (THC) in particular. The investigation of the national outbreak of e-cigarette or vaping product use lung injury (EVALI) has been intense, with story after story focusing on the lung complications that e-cigarette users were experiencing. In some cases these complications led to death. Statements issued by the CDC during the early ‘crisis’ period were direct and clear suggesting that individuals should stop using all vaping products in the late summer of 2019 (Perrine et al. 2019).1 Coverage of the epidemic in the mainstream press generally echoed the CDC’s messaging, conflating all vaping products during the initial phase of the crisis when the direct causes were still unknown.2
This messaging changed over time as investigation of the cause of the lung injury pointed toward only a subset of the vaping market. By December and January, the CDC had significantly changed its messaging, remarking that the CDC, FDA, and state health authorities have made progress in identifying the cause of the harm.3 It noted that emergency visits continue to decline and that THC products obtained from informal sources are the ones most closely linked to the health crisis (CDC, 2020). The warnings to avoid all vaping products have since been refined. Currently the CDC and the FDA recommend, among other things, that ‘people not use THC-containing e-cigarette or vaping products, particularly from informal sources like friends, family, or in-person or online dealers,’ that ‘vitamin E acetate should not be added to any e-cigarette, or vaping products,’ that ‘adults using nicotine-containing e-cigarettes or vaping products as an alternative to cigarettes should not go back to smoking,’ and that ‘e-cigarette or vaping products should never be used by youths, young adults, or women who are pregnant”.4
The EVALI outbreak, and the evolution of the CDC statements from the initial conflation of all e-cigarette and vaping products to a subsequently more refined message about a subset of vaping products, present a unique natural experiment to study how risk perceptions regarding e-cigarettes respond to information shocks. Government and media messaging about risk may be especially impactful on the formation of risk perceptions for e-cigarettes compared with government messaging impacts in other markets. As noted by Koslowski and Sweanor (2016), relative risk claims for a reduced-harm product are strictly regulated by the FDA and require that the manufacturer ex ante prove that such a claim will not have an adverse effect on population health. They note that this is unique to tobacco regulation and essentially eliminates all industry-provided reduced risk claims. Consequently, risk information provided by government, and by traditional and social media, may have an enhanced role in shaping risk perceptions for e-cigarettes relative to combustible cigarettes. The perceived risk profile for new products such as e-cigarettes – even if on average lower than that for cigarettes – is also likely to exhibit greater variability and uncertainty. Moreover, for a new tobacco product entry like e-cigarettes, individuals are likely to draw on existing tobacco products such as cigarettes as a frame of reference for initial risk beliefs (Viscusi 2016). In light of both of these considerations, risk perceptions for e-cigarettes may be particularly elastic with respect to any new information shocks as individuals update their beliefs regarding potential health outcomes and the weights associated with alternate outcomes in the presence of uncertainty. Another factor that makes this market important to study is the complicated nature of how different populations might respond to health risk beliefs of e-cigarettes relative to traditional cigarettes. As noted above, the CDC and the FDA have shaped meaningfully different messages to adult smokers versus youth. While adults are discouraged from moving back from e-cigarettes to traditional cigarettes, youth are advised to never use e-cigarettes. One can infer from the advice for adults not to switch from e-cigarettes back to smoking traditional cigarettes that the FDA and CDC implicitly believe that cigarettes are more harmful that e-cigarettes. The health risks of smoking traditional cigarettes are well-known and less uncertain. According to the CDC (Control, 2020) approximately 16 million people are living with a disease attributed to smoking and more than 480,000 deaths are attributed to smoking each year. If e-cigarettes are perceived as less harmful than cigarettes, then this presents a potentially attractive alternative to smoking, either as a mechanism for smokers to attempt to quit, to switch to e-cigarettes, or to even use a combination of both products while cutting down on the consumption of cigarettes.
Current recommendations from the CDC and FDA urge all youth not to use e-cigarette and vaping products because of the harm associated with these products. Most recently, the FDA has taken additional action in its focus on youth and e-cigarettes by banning certain flavors that may be appealing to youth. In the statement accompanying this ban, Secretary of Health and Human Services Alex Azar noted that “(b)y prioritizing enforcement against the products that are most widely used by children, our action today seeks to strike the right public health balance by maintaining e-cigarettes as a potential off-ramp for adults using combustible tobacco while ensuring these products don’t provide an on-ramp to nicotine addiction for our youth”.5 It is notable that the FDA chose not to include a more refined message that youth should not use e-cigarettes or vaping products, but if they were going to start smoking it is preferable that they use e-cigarettes rather than smoking combustible cigarettes. One can infer that the CDC and FDA calculated that such a message might implicitly endorse the use of e-cigarettes by youth. However, the absence of a more nuanced risk statement regarding e-cigarettes and smoking may also generate equalized health risk beliefs among youth for both products, which in turn could lead to more youth choosing traditional cigarettes than otherwise.
Perceived harm of e-cigarettes has been found to be a significant predictor of behavior of smokers, as they consider quitting or switching some of their smoking activity to e-cigarettes, and of the behavior of youth, as they consider whether to smoke cigarettes, use e-cigarettes, abstain from both, or sequence from one product to the other (Pericot-Valverde et al. 2017; Amrock et al. 2015; Brose et al. 2015). Understanding the formation of risk perceptions and how they are impacted by external health and information shocks is therefore integral towards understanding different use patterns and towards the development of policies to rectify misperceptions and minimize negative public health outcomes. Our study contributes to the very limited evidence base on this issue, and provides some of the first analyses on how risk perceptions respond to an adverse information shock and during a period of significant messaging by the government and media about the risks of vaping. Of critical importance is assessing whether risk perceptions are altered permanently, whether they undergo further updating, or revert towards the pre-crisis baseline once the uncertainty regarding the EVALI outbreak subsided and the public health messaging backed away from all vaping products and focused on those containing THC and derived from non-official sources. We provide the first evidence on the trajectory of risk perceptions before, during, and after the EVALI outbreak and periods enveloping the shift in messaging. We further assess whether these responses differed across younger and older adults – groups that were subject to potentially differential public health messaging regarding the use of e-cigarettes.
The remainder of the paper proceeds as follows. Section II provides some background on the relative trends of e-cigarette and cigarette use over time for youth and adults. Section III summarizes the literature on the perceptions of the health risks of e-cigarettes compared with combustible cigarettes and how such perceptions might influence use of e-cigarettes. Section IV discusses the timeline of the EVALI outbreak, introduces a model of risk formation and develops hypotheses about how the flow of information from government and media can influence perceptions of the relative risk of e-cigarettes compared with combustible cigarettes. Section V presents an overview of the data and methods used to measure health risk perceptions over time, with the results reported in Section VI. Section VII outlines the policy implications of the work and suggested directions for future research that can inform policy.
II. Background on Use of E-cigarettes
The use of e-cigarettes has risen dramatically in the past decade and the public health implications of this trend continue to be debated by researchers and policy makers. One key question that arises in this debate is how consumer risk perceptions of the relative harm of e-cigarettes compared with combustible cigarettes influence decisions about use of both of these products. Broad trends in cigarette use over time are consistent with the view that the introduction of e-cigarettes, and the perception that they may be less harmful than cigarettes, helped accelerate the pre-existing downward trend in cigarette smoking among youth. Data from the Monitoring the Future (MTF) Surveys, for instance, show a dramatic decline in youth smoking rates coincidental with the rise of youth e-cigarette use (see Figure 1). Between 2007 and 2013, the 30-day prevalence rate for cigarette use dropped from 21.6% to 16.3%. Over the subsequent six-year period, from 2013–2019, which witnessed a rapid increase in e-cigarette use, the 30-day prevalence rate for cigarette use plummeted from the 16.3% to 5.7%. What was unexpected was the even larger and more rapid increase in e-cigarette use, which skyrocketed over this same period from 4.5% to 27.5% (National Youth Tobacco Surveys). Similar to youth, adult smoking rates have also continued their long-run decline (see Figure 2). Data from the National Health and Interview Surveys indicate that the adult cigarette smoking prevalence accelerated its decline since 2013, and is currently stands at the lowest level (13.7%) in the past five decades (Creamer et al. 2019).6 This decrease in smoking prevalence was driven by significant increases in quit attempts and successful quits, and more recently accompanied by an increase in e-cigarette use primarily among younger adults ages 18–24. These contrasting trends between declines in smoking rates and increases in vaping raises, for both youth and adults, underscore the importance of analyzing the evolution of risk perceptions for these products over the past decade and how they differ across different populations. Use of cigarettes and e-cigarettes is mediated by risk perceptions (Popova et al. 2018), and trends in risk perceptions may be an important driver of trends in e-cigarette use and smoking (Pepper et al. 2014).
Figure 1:
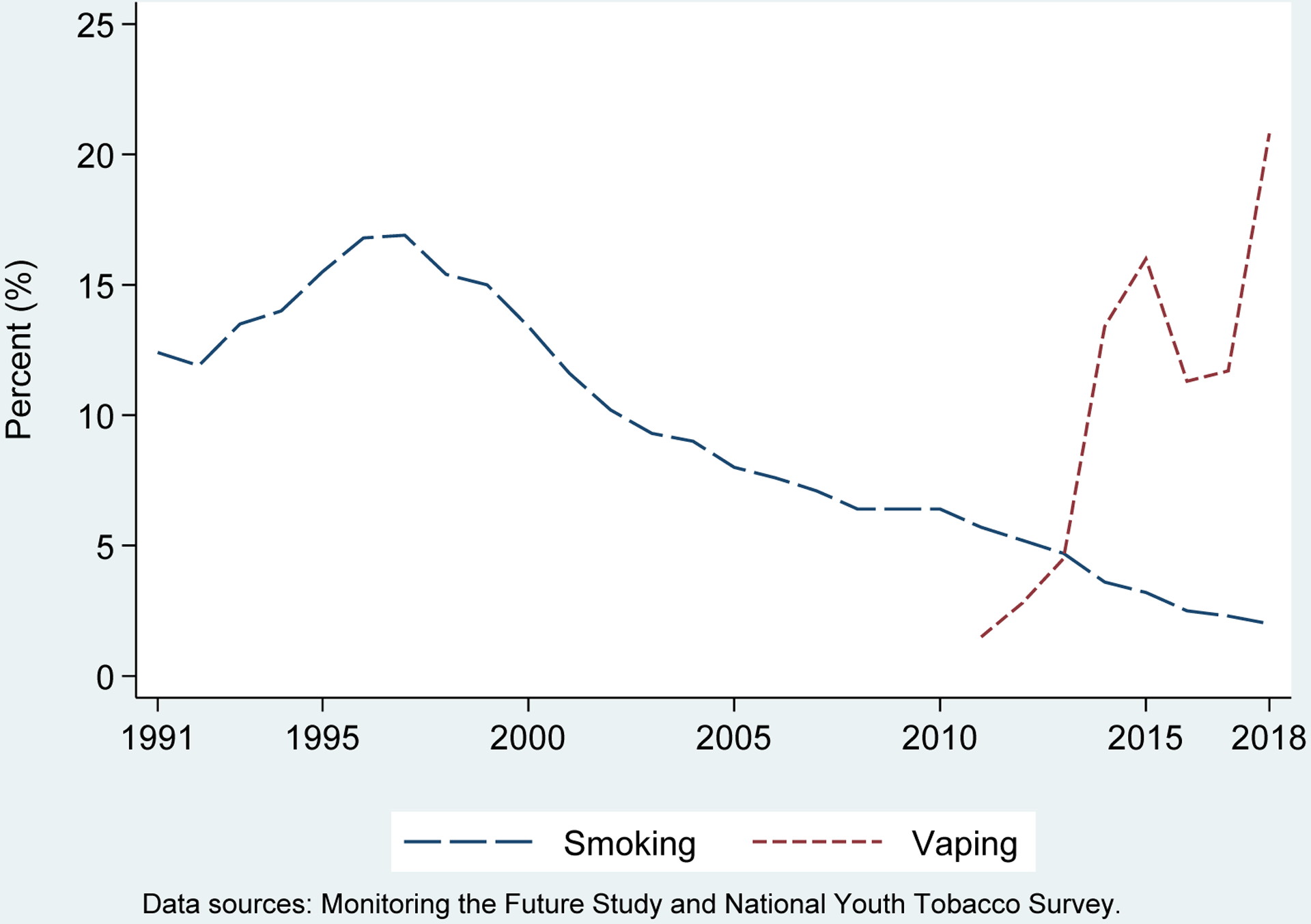
Trends in Smoking and E-cigarette Use among Youth
Figure 2:
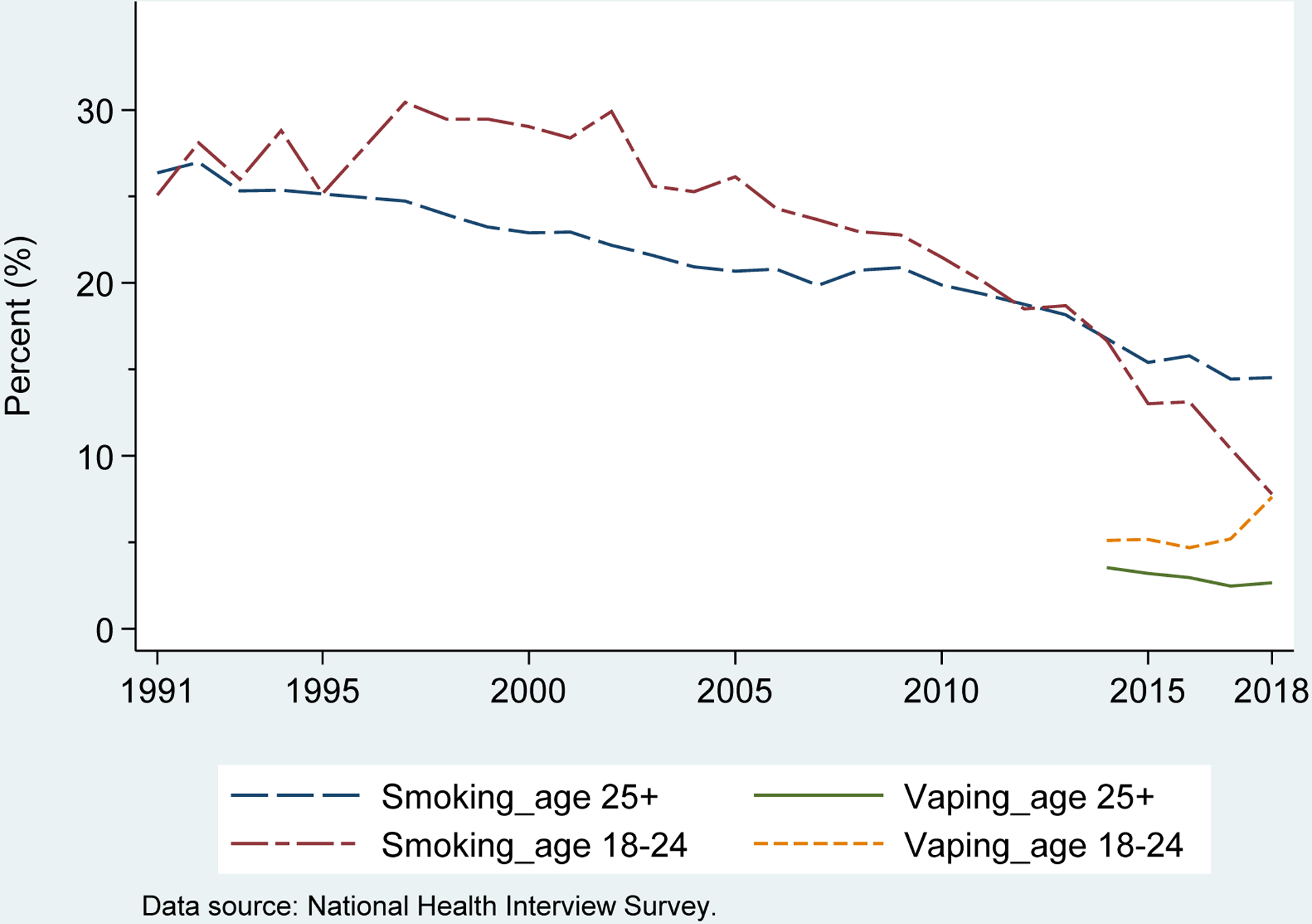
Trends in Smoking and E-cigarette Use among Adults
III. Perceptions of E-cigarettes
Perceptions that e-cigarettes are a safer way to ingest nicotine can lead adult smokers to switch from combustible cigarettes to e-cigarettes, continue to use a mix of both while cutting down on the consumption of cigarettes, or use e-cigarettes as a means to quit all tobacco consumption (Kenkel et al. 2017; Pericot-Valverde et al. 2017). It is possible also that these perceptions can lead non-smoking adults who otherwise would not smoke combustible cigarettes into the e-cigarette market. Some of these might be former smokers whose perceptions of a safer alternative to cigarettes lead them to use e-cigarettes.
Studies have focused on these various populations and their reasons for using e-cigarettes. Many of these studies typically combine information on perceived risk of e-cigarettes and reported e-cigarette and cigarette use from surveys to identify the inter-relationships between vaping and smoking and between perceptions and use. Drawing on a web-enabled panel survey of 2,254 adults, Rutten et al. (2015) examine the use of e-cigarettes among current adult smokers and the correlation between stated reasons for use and quit intentions. Among smokers, 20.4% self-reported using e-cigarettes with 3.7% being daily users. The majority of respondents indicated that quitting smoking, reducing cigarette consumption, and reducing health risks were their main reason for use of e-cigarettes. Perception that e-cigarettes are less harmful than conventional cigarettes is also a significant predictor of e-cigarette use among adolescents, including those who have no history of using cigarettes, based on analyses of the 2012 National Youth Tobacco Survey (Amrock et al. 2015).
Using the 2012/2013 data from the Health Information National Trends Surveys (HINTS), Tan and Bingham (2014) find that 77% of respondents were aware of e-cigarettes, and that among those who were aware the prevalent view was that e-cigarettes were less harmful than cigarettes, particularly among more educated respondents and current smokers. Pepper et al. (2015) drew on data from an online survey administered to a national sample in order to measure the perceived harm of e-cigarettes vs. cigarettes. Participants viewed e-cigarettes as less likely to cause lung cancer, heart disease, and oral cancer compared with conventional cigarettes. The belief that e-cigarettes were less harmful than regular cigarettes was robust and extended to virtually all demographic groups examined. Results also suggest that young adults who had viewed e-cigarettes as less harmful or in aiding smoking cessation at baseline were more likely to experiment with e-cigarettes in the future (Choi and Forster 2014).
Perceptions of harm of e-cigarettes have expectedly not remained static over the past decade. Majeed et al (2017) analyzed data from the Tobacco Products and Risk Perceptions surveys spanning 2012–2015. Whereas 12.8% of adults had perceived e-cigarettes to at least as harmful as cigarettes in 2012, this perception more than tripled to 39.8% by 2015. In a comprehensive survey of the literature on risk perceptions across nicotine products, Czoli et al. (2016) conclude that perceived relative risk on non-combustible nicotine products is highly variable by product-type and across sub-populations. For e-cigarettes, which represent the newest entry into the market for non-combustible nicotine products during many of the time periods examined in the various studies, relative risk perceptions appear to better match epidemiological data than for other tobacco products.
Viscusi (2016) analyzes data for 2014 drawn from the GfK Knowledge Panel, a nationally-representative web-based panel, and finds that respondents generally view e-cigarettes as posing lower mortality risk from lung cancer and overall, when compared with combustible cigarettes. However, they vastly overestimate these risks associated with e-cigarette use. Viscusi also finds that intended use is more strongly correlated with health risk perceptions than other attributes such as perceived nicotine content. Specifically, the study finds that lower perceived risk of e-cigarettes relative to cigarettes is significantly associated with trying e-cigarettes. Interestingly, with respect to absolute risk beliefs, e-cigarette risk beliefs – but not conventional cigarette beliefs – are significant determinants of trying e-cigarettes.7 This implies that e-cigarette risk beliefs may disproportionately affect comparative risk beliefs, and thus exert a stronger influence on intended and actual use.
Given this link from perceived risk to actual decisions on the use of various tobacco products, disparities between actual risk and perceived risk can lead to sub-optimal consumption decisions, and pose a particular challenge for policy makers with respect to correcting for the internal and external costs of misaligned consumption decisions. Risk-based misperceptions may also lead to a public health loss if current or potential smokers are discouraged from switching to other less-risky products because of an over-estimation of the relative risk of these products.
IV. Analytical Framework
EVALI Timeline
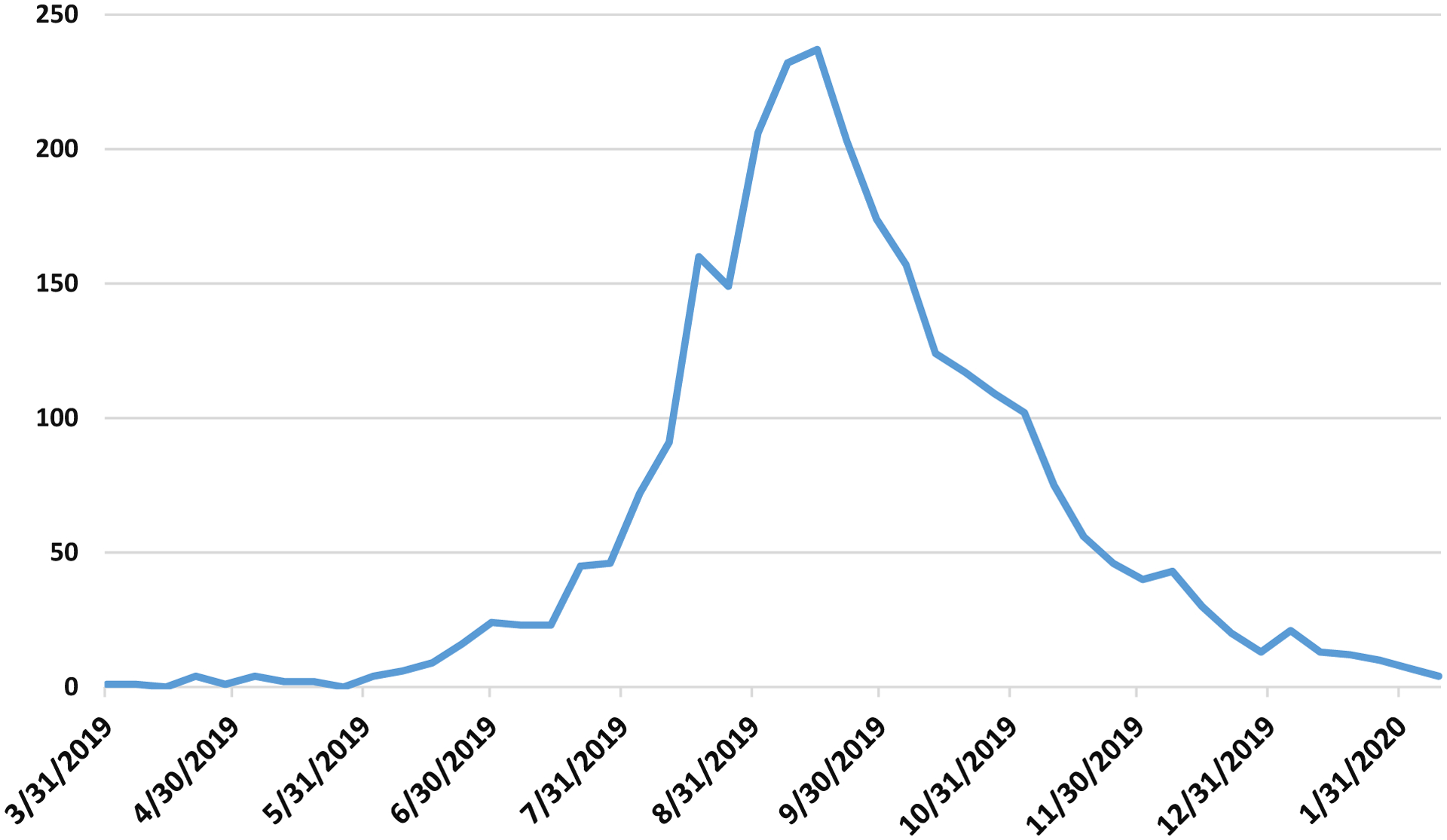
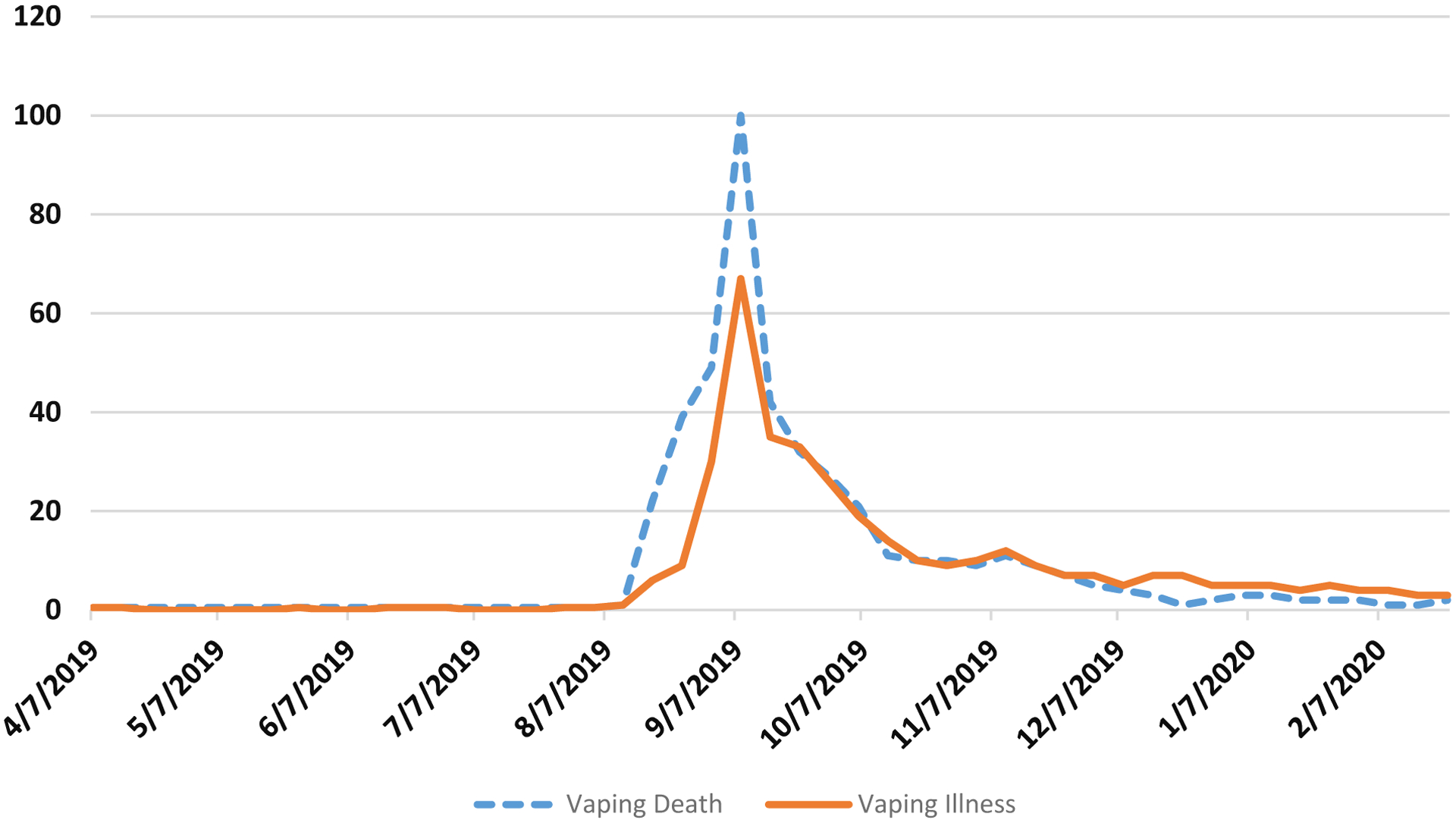
The outbreak of e-cigarette, or vaping, product use associated lung injury (EVALI) began in 2019, with the first cases identified in Illinois and Wisconsin around April. The illness was first recognized by the CDC in August, with cases peaking around mid-September followed by a gradual but persistent decline (see Figure 4). Reporting of the outbreak and consumer interest tracked almost one-to-one with the caseload, as evidenced by trends in Google Searches (Figure 3). The acronym EVALI – to describe this newly identified lung disease linked to vaping – was initially used by the CDC in its interim guidance issued to health care providers on October 11th (Siegel et al., MMWR October 11, 2019). As of February 18, 2020 (date of the final CDC update), there have been a total of 2,807 hospitalized EVALI cases or deaths reported nationwide, across all 50 states, D.C., and Puerto Rico and the U.S. Virgin Islands, and 68 deaths confirmed in 29 states and D.C.
Figure 4:
Hospital Admissions for Patients with EVALI (Source: https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html#map-cases)
Figure 3:
Indexed Trends in Google Search Terms (Source: Google Trends)
On September 27, 2019, the CDC issued a statement through Twitter and recommended “refraining from using e-cigarette/vaping products, especially those with THC”.8 The interim guidance for health care providers, issued on October 11, continued to stress that the “FDA and the CDC have not identified the cause or causes of the lung injuries among the EVALI cases, and the only commonality among all cases is that patients report the use of e-cigarette, or vaping, products” (Siegel et al. 2019, p. 924). Drawing on this uncertainty, the guidance underscored that the “CDC recommends that persons should not use e-cigarette, or vaping, products that contain THC” but then also issued the broader statement that the “CDC continues to recommend that persons consider refraining from using e-cigarette, or vaping, products that contain nicotine”. In all of these initial messages, the CDC did qualify that if adults are using e-cigarette or vaping products to quit smoking, then they should not return to smoking – implying that nicotine-based e-cigarettes may be safer than smoking; however, the CDC also qualified that these individuals should use evidence-based treatments – implying that they should switch out of e-cigarettes to sanctioned nicotine replacement therapy. With respect to youth, young adults, and pregnant women, the recommendation was that “irrespective of the ongoing investigation, e-cigarette, or vaping, products, should never be used” (Siegel et al. 2019, p. 924).
As the cumulative caseload increased, and investigation centered on a subset of the vaping market as the likely cause, the CDC changed its recommendations. Specifically, on December 10, 2019, the CDC issued a recommendation through Twitter urging individuals to “not use e-cigarette, or vaping, products that contain THC, as data suggest these products play a major role in the current lung injury outbreak”.9 This recommendation currently stands, and further specifies that people not use THC-containing e-cigarette or vaping products, particularly from informal sources (i.e. friends, family, online dealers).10
Model of Risk Perception
The question of how the perceived relative risk of vaping responds to information shocks can be framed within a Bayesian learning context. The discussion in this section follows Viscusi (2016). While smoking and vaping can carry a multitude of health risks, it is convenient to collapse all of the various risks in terms of a single parameter capturing the probability of dying.11 In this respect, v represents the perceived e-cigarette related risk of mortality, and s is an analogous measure of the mortality risk associated with smoking. Since e-cigarettes are a relatively new product entry in the tobacco market with considerable uncertainty regarding their health profile, it is reasonable to assume that individuals form their beliefs regarding v based on an initial frame of reference – another similar product whose risk profile is less uncertain and well-publicized – and then update those beliefs based on other information and sources. Hence, the perceived risk of using e-cigarettes, v, is a function of the perceived risk of cigarettes, s, and any additional or reduced risk, q, implied by product-specific external information that is not captured in s.
Assuming that individuals’ prior probability beliefs follow a beta distribution, the posterior perceived risk of e-cigarettes becomes a weighted-average linear function of the prior perceived risk, s, and additional implied risk, q.12
| (1) |
| (2) |
The informational weights, φ and γ, represent the proportion of total information (φ0 + γ0) available to the individual that is represented by risk-related information regarding conventional cigarettes (φ0), which is the reference point, and other available information that may be specific to e-cigarettes and vaping (γ0).13
Dividing both sides of equation (1) by s yields the following posterior relative risk of vaping vs. smoking.
| (3) |
It can be shown that individuals will perceive e-cigarettes to be less risky relative to cigarettes , that is if the additional implied risk associated with vaping is lower than the reference risk level.
The EVALI outbreak, and ensuing news reports regarding lung morbidity and deaths associated with vaping, represented a negative health informational shock (an increase in q). Furthermore, this was occurring during a time when there was no new information or adverse health reports regarding smoking. Thus, in terms of information draws, more information content specific to vaping (an increase in γ0) was entering the market and informing individuals’ beliefs. In terms of equation (3), this implies an increase in γ, a decrease in φ, and an increase in , all of which would lead to a shift in the relative risk perception of vaping towards greater harm compared to smoking – that is, an increase in . Note that the negative informational shock regarding vaping leads to a shift in the perceived relative risk due to both an updating process, through q, as well as due to a reweighting from the greater emphasis placed on the new product-specific information (change in the informational weights, φ and γ).
As noted above, initial recommendations and media reports conflated all vaping products and e-cigarettes, though THC-containing products were referenced in the CDC and FDA messaging as well as in some of the earlier media reports. Only later (December 10, 2019) did the government messaging clarify the recommendations as applying explicitly to the subset of e-cigarette or vaping products containing THC, and reports began to stress that it is these specific products that are strongly implicated in the current lung injury outbreak. These clarifications provide an additional informational shock regarding e-cigarettes, in the reverse direction to the earlier shock that fused all vaping products into a single category. For individuals, potentially learning that nicotine e-cigarettes derived from official sources were not the cause of the lung injuries and related mortality, this is akin to a decrease in q, and thus a downward revision of . The downward revision is reinforced further by an increase in γ, the weight placed on the new informational content.
This scenario implicitly assumes symmetry in the updates, that is once an individual has revised their relative risk upwards, any further new information to the contrary leads to a similar effect in reverse. However, it does not need to be the case that risk beliefs revert to the baseline, even if risk perceptions decrease. For instance, if individuals are sticky in their beliefs, or weight new information that contradicts their priors differently, then the clarifications in the messaging by the CDC and the media may not lead risk perceptions for nicotine e-cigarettes to return to baseline. The clarification represents a new shock with its own informational content and a lower risk level, which is predicted to pull assessed risk probability downwards but may not fully wipe out the effects of the initial warning. Furthermore, the media coverage and interest in the first shock was greater than that for the clarification (see Figure 3), which would imply a larger information weight (γ0) for the first alarmist report relative to the clarification. In this case, the later clarifications, while leading to some decrease in the perceived relative risk of e-cigarettes, would not be predicted to fully revert perceptions to baseline.
In the empirical analyses that follow, we also specifically probe respondents’ risk beliefs regarding nicotine e-cigarettes and those containing THC in order to analyze the evolution of these beliefs as the information content shifted. Given the ambiguity in how respondents may update their risk beliefs once the reporting coalesced around the main cause and no longer implicated nicotine e-cigarettes, it remains an empirical question how these risk beliefs shifted during the early and latter parts of the EVALI outbreak. It is possible that the risk beliefs will stabilize at a permanently new steady-state level. It is also possible that they will revert, either fully or partially, towards the risk beliefs held prior to the crisis. Each of these scenarios has important implications for optimal consumption decisions, public health, and rationales for informational regulations.
V. Empirical Analyses
Data
We use data on consumer risk perceptions from two sets of surveys conducted before and during the EVALI outbreak. The first set of surveys are cycles of the National Cancer Institute’s (NCI) Health Information National Trends Survey (HINTS). The HINTS data are a set of repeated cross-sections that provide nationally representative estimates of consumer information about a range of health topics. HINTS cycles conducted in 2012, 2014, 2015, 2017, 2018, and 2019 measure consumer perceptions of the risk of e-cigarettes relative to combustible cigarettes. The sample sizes of these cycles range from 3,630 to 5,438 per year, and sampling weights are provided to generalize results to the national population.14 In these cycles the surveys asked: “Compared to smoking cigarettes, would you say that electronic cigarettes are much less harmful, less harmful, just as harmful, more harmful, or much more harmful?” The most recent HINTS cycle that asked about e-cigarettes was conducted in February through April of 2019, before the EVALI outbreak was recognized.
Second, to collect information during the EVALI outbreak, we commissioned a series of online Google Surveys (GS) that included versions of the HINTS question on the harmfulness of e-cigarettes compared to smoking cigarettes. GS is a commercial organization that recruits respondents from internet users who visit websites that use a “surveywall” where the site’s content is blocked until the user completes the survey. GS reports that they can reach tens of millions of unique daily internet and smartphone users (Sostek and Slatkin 2017) and describes how it works to eliminate biases (Sostek, 2019). Academic researchers in marketing and social sciences increasingly rely on online opt-in surveys as a valuable source of data on a range of topics (Hulland and Miller 2018). Several studies have been conducted of the accuracy and biases of online opt-in survey data (Mercer, Lau, and Kennedy 2018, Sostek 2019). Santoso, Stein and Stevenson (2016) discuss GS methods in more detail and report the results of several methodological studies. They conclude that there is no evidence that GS is either more or less representative than other online opt-in survey datasets. Unlike other online surveys, GS uses inferred demographics derived from the user’s browsing history or IP address. Santoso et al. (2016) find that the inferred demographics are comparable to self-reported demographics but introduce some apparently random noise.
The sample sizes of our GS repeated cross-sections range from 2,656 to 3,679. GS provides sampling weights to approximate the target population, which is the national population of internet users, derived from estimates from the Current Population Survey Computer and Internet Use Supplement.15 Close to 90% of the adult population has internet access (based on the 2018 American Community Survey), and polls from the Pew Research Center (conducted in January-February 2019) also indicate that 90% of all adults are internet users.16 Thus, the population represented by HINTS (adults) and the GS (adult internet users) for 2019–2020 almost fully overlap. We adjust for the sampling weights provided in the HINTS and the GS to produce summary statistics, and to show the comparability of the samples. We also provide differential estimates by age groups, since for non-elderly adults the GS and the HINTS are essentially representing the same population.17
We fielded ten waves of online Google Surveys, bimonthly from September 2019 through the end of January 2020. For six of these surveys, we used the HINTS version of the question, asking respondents, “Compared to smoking cigarettes, would you say that electronic cigarettes, which deliver nicotine through vapor, are much less harmful, less harmful, just as harmful, more harmful, or much more harmful?”. For the other four surveys, we modified this question to probe respondents’ perceived risk of all e-cigarettes and vaping products, including those that may deliver THC, by asking “Compared to smoking cigarettes, would you say that electronic cigarettes, which deliver nicotine or other substances such as THC oil through a vapor, are much less harmful, less harmful, just as harmful, more harmful, or much more harmful?”.18 After accounting for missing information on age, gender, and geographic region, the combined sample size across all of the GS waves is 21,184 observations. The sample of analysis for our econometric model consists of the pooled HINTS and GS data, which provides a sample size of 37,015 observations.
In order to disentangle shifts in risk perception due to the EVALI outbreak from other policy shifts, we match information on cigarette excise taxes, e-cigarette taxes, e-cigarette work restrictions, and the minimum legal sales age for e-cigarettes, to the HINTS and the GS data based on the survey month/year and the respondent’s residential census division.19 We also similarly match and control for an index of anti-smoking sentiment. This measure, first introduced by DeCicca et al (2008), used the Tobacco Use Supplements from the CPS to measure respondent attitudes toward smoking based on their opinions on topics such as policies that restrict tobacco use in public places, policies that relate to the promotion and advertising of tobacco products, and whether they allow smoking in their homes. These measures are then aggregated at the state level to obtain a state specific measure of anti-smoking attitudes. Studies have used this measure as a control variable when examining tobacco use (DeCicca, et al. 2008).
To provide an overview of the data, Tables 1–3 present summary statistics from the pooled sample of data from the HINTS and the GS, separately for both surveys, and for various subgroups. Overall, for the period spanning 2012–2020 as captured by the pooled HINTS and GS data, about 22% of adults perceived e-cigarettes to be more harmful than cigarettes. This mean masks a substantial increase in this perceived harm pre- and post-EVALI outbreak, from 9% in the HINTS (October 2012 – April 2019) to 31% in the GS (September 2019 – February 2020). Comparing the socio-demographics between the HINTS and the GS, the samples are highly similar across gender, age groups, and representation of the geographic regions, providing some validation on their comparability. Table 2 provides a breakdown of these statistics across age groups and across gender, which suggest that perceived relative risk of e-cigarettes is generally similar for adults between the ages of 18–44 (around 20%) but then significantly increases for older adults (around 24% for adults ages 45+). Males are also more likely to perceive e-cigarette use to be more harmful compared to smoking (24%), relative to females (20%). Interestingly, we do not find any substantial or significant difference in perceived risk across respondents from GS that asked about nicotine-based e-cigarettes vs. all e-cigarettes including those containing THC (Table 3). This may reflect the conflation of all e-cigarette products during the early phase of the crisis.
Table 1.
Summary Statistics for Pooled Sample, HINTS and GS
| Full Sample | HINTS Sample | GS Sample | |
|---|---|---|---|
| E-cigs more harmful | 0.22 [0.41] | 0.09 [0.29] | 0.31 [0.46] |
| Predicted risk perception | 0.15 [0.14] | 0.09 [0.06] | 0.18 [0.16] |
| EVALI outbreak began | 0.57 [0.49] | 0.00 [0.00] | 1.00 [0.00] |
| CDC suspected THC | 0.23 [0.42] | 0.00 [0.00] | 0.40 [0.49] |
| Question mentions THC | 0.23 [0.42] | 0.00 [0.00] | 0.40 [0.49] |
| Female | 0.54 [0.50] | 0.50 [0.50] | 0.46 [0.50] |
| Age (Ref=18–24) | |||
| 25–34 | 0.15 [0.35] | 0.18 [0.38] | 0.18 [0.38] |
| 35–44 | 0.16 [0.37] | 0.18 [0.39] | 0.17 [0.37] |
| 45–54 | 0.19 [0.39] | 0.22 [0.41] | 0.18 [0.38] |
| 55–64 | 0.22 [0.41] | 0.16 [0.36] | 0.18 [0.38] |
| 65+ | 0.22 [0.42] | 0.15 [0.36] | 0.18 [0.38] |
| Census Div. (Ref=New England) | |||
| Middle Atlantic | 0.10 [0.31] | 0.13 [0.33] | 0.11 [0.31] |
| East North Central | 0.16 [0.36] | 0.15 [0.36] | 0.12 [0.32] |
| West North Central | 0.10 [0.30] | 0.07 [0.25] | 0.09 [0.29] |
| South Atlantic | 0.20 [0.40] | 0.20 [0.40] | 0.20 [0.40] |
| East South Central | 0.07 [0.25] | 0.06 [0.23] | 0.08 [0.27] |
| West South Central | 0.10 [0.30] | 0.11 [0.31] | 0.09 [0.29] |
| Mountain | 0.10 [0.30] | 0.08 [0.26] | 0.13 [0.34] |
| Pacific | 0.12 [0.33] | 0.16 [0.37] | 0.11 [0.31] |
| 2008 Anti-smoking Sentiment | 0.23 [0.15] | 0.24 [0.13] | 0.24 [0.17] |
| Cigarette Tax | 1.73 [0.99] | 1.81 [0.78] | 1.75 [1.16] |
| E-cig Tax (Yes) | 0.28 [0.41] | 0.11 [0.16] | 0.39 [0.49] |
| E-cig Work Restrictions | |||
| Restricted area | 0.01 [0.10] | 0.00 [0.03] | 0.02 [0.14] |
| Banned | 0.23 [0.37] | 0.17 [0.21] | 0.31 [0.46] |
| E-cig minimum age law | |||
| 18 | 0.63 [0.42] | 0.62 [0.30] | 0.60 [0.49] |
| 19 | 0.08 [0.22] | 0.09 [0.12] | 0.09 [0.28] |
| 21 | 0.18 [0.36] | 0.07 [0.15] | 0.28 [0.45] |
| Year | 2017.8 [2.29] | 2015.8 [2.26] | 2019.2 [0.40] |
| Observations | 37,015 | 15,831 | 21,184 |
Notes: Summary statistics are presented from the seven HINTS waves for 2012–2019 and the ten GS waves from 9/2019–1/2020. Means are reported, with standard deviations in brackets. Sampling weights are utilized when presenting the statistics separately for the HINTS and the GS, but not for the pooled model due to non-comparability of the scale of the sampling weights between the HINTS and the GS. Weighted and unweighted statistics are highly similar.
Table 3.
Summary Statistics for GS with and without THC question
| GS with THC | GS w/o THC | |
|---|---|---|
| E-cigs more harmful | 0.31 [0.46] | 0.31 [0.46] |
| Predicted risk perception | 0.19 [0.16] | 0.18 [0.16] |
| EVALI outbreak began | 1.00 [0.00] | 1.00 [0.00] |
| CDC suspected THC | 0.48 [0.50] | 0.34 [0.47] |
| Female | 0.46 [0.50] | 0.45 [0.50] |
| Age (Ref=18–24) | ||
| 25–34 | 0.18 [0.38] | 0.18 [0.38] |
| 35–44 | 0.17 [0.37] | 0.17 [0.37] |
| 45–54 | 0.18 [0.39] | 0.18 [0.38] |
| 55–64 | 0.18 [0.39] | 0.18 [0.38] |
| 65+ | 0.18 [0.38] | 0.18 [0.38] |
| Census Div. (Ref=New England) | ||
| Middle Atlantic | 0.11 [0.31] | 0.11 [0.31] |
| East North Central | 0.11 [0.32] | 0.12 [0.33] |
| West North Central | 0.09 [0.30] | 0.09 [0.29] |
| South Atlantic | 0.20 [0.40] | 0.21 [0.40] |
| East South Central | 0.08 [0.28] | 0.08 [0.27] |
| West South Central | 0.09 [0.28] | 0.09 [0.29] |
| Mountain | 0.14 [0.35] | 0.13 [0.33] |
| Pacific | 0.10 [0.30] | 0.11 [0.32] |
| Year | 2,019.2 [0.43] | 2,019.2 [0.38] |
| Obs | 8,518 | 12,666 |
Notes: Summary statistics (means) are presented from the four GS waves with the THC reference in the risk perception question and the six GS waves without the THC reference.
Table 2.
Summary Statistics for Full Sample by age and gender
| Age | Gender | |||||||
|---|---|---|---|---|---|---|---|---|
| 18–24 | 25–34 | 35–44 | 45–54 | 55–64 | 65+ | Male | Female | |
| E-cigs more harmful | 0.20 | 0.19 | 0.21 | 0.24 | 0.24 | 0.23 | 0.24 | 0.20 |
| Predicted risk perception | 0.13 | 0.14 | 0.15 | 0.15 | 0.15 | 0.15 | 0.14 | 0.15 |
| EVALI outbreak began | 0.78 | 0.64 | 0.61 | 0.58 | 0.54 | 0.46 | 0.61 | 0.54 |
| CDC suspected THC | 0.33 | 0.25 | 0.24 | 0.21 | 0.21 | 0.20 | 0.25 | 0.21 |
| Question mentions THC | 0.31 | 0.27 | 0.24 | 0.23 | 0.22 | 0.18 | 0.24 | 0.22 |
| Female | 0.53 | 0.56 | 0.54 | 0.54 | 0.53 | 0.53 | 0 | 1 |
| Age (Ref=18–24) | ||||||||
| 25–34 | 0 | 1 | 0 | 0 | 0 | 0 | 0.14 | 0.15 |
| 35–44 | 0 | 0 | 1 | 0 | 0 | 0 | 0.16 | 0.16 |
| 45–54 | 0 | 0 | 0 | 1 | 0 | 0 | 0.19 | 0.19 |
| 55–64 | 0 | 0 | 0 | 0 | 1 | 0 | 0.22 | 0.21 |
| 65+ | 0 | 0 | 0 | 0 | 0 | 1 | 0.23 | 0.22 |
| Census Div. (Ref=New England] | ||||||||
| Middle Atlantic | 0.100 | 0.10 | 0.093 | 0.11 | 0.10 | 0.11 | 0.10 | 0.11 |
| East North Central | 0.19 | 0.16 | 0.15 | 0.16 | 0.16 | 0.14 | 0.16 | 0.15 |
| West North Central | 0.13 | 0.11 | 0.10 | 0.092 | 0.096 | 0.083 | 0.10 | 0.095 |
| South Atlantic | 0.19 | 0.21 | 0.20 | 0.21 | 0.20 | 0.21 | 0.21 | 0.20 |
| East South Central | 0.059 | 0.057 | 0.071 | 0.081 | 0.072 | 0.065 | 0.071 | 0.067 |
| West South Central | 0.092 | 0.099 | 0.10 | 0.099 | 0.11 | 0.11 | 0.098 | 0.11 |
| Mountain | 0.10 | 0.098 | 0.10 | 0.091 | 0.094 | 0.10 | 0.10 | 0.095 |
| Pacific | 0.098 | 0.12 | 0.13 | 0.11 | 0.11 | 0.14 | 0.12 | 0.12 |
| 2008 Anti-smoking Sentiment | 0.22 | 0.23 | 0.23 | 0.22 | 0.22 | 0.24 | 0.23 | 0.23 |
| Cigarette Tax | 1.73 | 1.72 | 1.72 | 1.71 | 1.73 | 1.76 | 1.71 | 1.75 |
| E-cig Tax (Yes/No) | 0.34 | 0.31 | 0.29 | 0.28 | 0.27 | 0.25 | 0.29 | 0.27 |
| E-cig Work Restrictions | ||||||||
| Restricted area | 0.0076 | 0.012 | 0.012 | 0.011 | 0.009 | 0.012 | 0.011 | 0.010 |
| Banned | 0.23 | 0.23 | 0.22 | 0.22 | 0.22 | 0.24 | 0.22 | 0.23 |
| E-cig minimum age law | ||||||||
| 18 | 0.64 | 0.62 | 0.62 | 0.62 | 0.63 | 0.63 | 0.63 | 0.62 |
| 19 | 0.072 | 0.073 | 0.082 | 0.081 | 0.080 | 0.078 | 0.079 | 0.078 |
| 21 | 0.21 | 0.20 | 0.19 | 0.18 | 0.17 | 0.17 | 0.18 | 0.18 |
| Year | 2018.5 | 2018.0 | 2017.9 | 2017.7 | 2017.7 | 2017.5 | 2017.9 | 2017.7 |
| Observations | 2,408 | 5,368 | 6,012 | 6,946 | 8,084 | 8,197 | 17,142 | 19,873 |
Notes: Summary statistics (means) are presented from the pooled seven HINTS waves for 2012–2019 and the ten GS waves from 9/2019–1/2020.
Figure 5 shows the fraction of HINTS and GS respondents over time who reported that e-cigarettes were more harmful or much more harmful than smoking cigarettes. The fraction is sharply higher in the GS data collected after the EVALI outbreak. The HINTS data from October 2012 through April 2019 show an upward trend in the fraction perceiving e-cigarettes to be more or much more harmful. Based on a linear trend fitted to the HINTS data points, the fraction reporting more or much more harmful is predicted to be 18% in September 2019. In the actual GS data after the EVALI outbreak in September 2019, over 30% of the respondents report that e-cigarettes are more or much more harmful than smoking cigarettes.20 The 2018 HINTS included questions about internet use. Compared to HINTS respondents who do not use the internet, HINTS respondents who use the internet tend to perceive e-cigarettes as less harmful, although the differences are small and statistically insignificant. Because all respondents in the GS samples are internet users, by this factor alone we would predict that compared to the HINTS samples, the fractions reporting the e-cigarettes are more or much more harmful in the GS should be slightly lower, not sharply higher.
Figure 5:
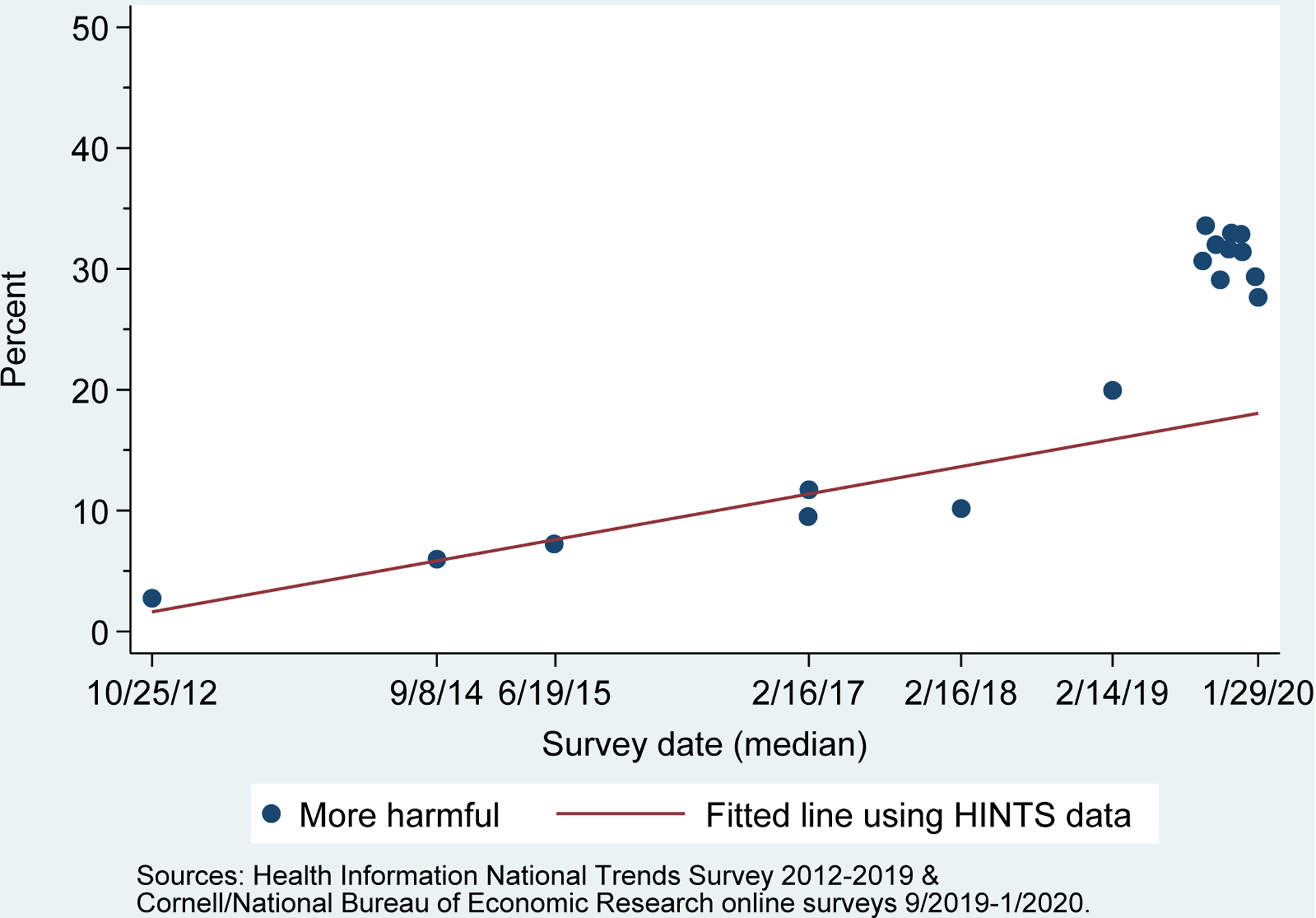
Respondents who think e-cigarettes are more harmful compared to smoking cigarettes HINTS and GS data
In contrast to the GS results, data from online surveys conducted in 2014 and 2019 show only a modest increase in the fraction of respondents reporting that e-cigarettes are somewhat more or much more risky than conventional cigarettes (Viscusi 2020). The 2019 survey was conducted in late November and early December, a few months after the peak of the EVALI outbreak. In the 2014 survey, four percent of respondents reported that e-cigarettes were either somewhat more or much more risky. In the 2019 survey, the fraction increases to 15 percent. The observed increase between the two surveys Viscusi analyzes is roughly consistent with the trend over time in the HINTS data before the EVALI outbreak (Figure 5). However, compared to either the HINTS data or the GS data, Viscusi finds higher fractions of respondents reporting that e-cigarettes are much less risky or somewhat less risky than conventional cigarettes. We speculate that the differences might be due to the differences in survey design. In Viscusi’s survey, respondents were first asked about the absolute levels of risk of conventional cigarette and e-cigarettes. Their responses to the relative risk question might reflect the effort their prior thinking about risks when answering the absolute risk questions. The surveys also used slightly different wording; Viscusi’s survey asked about relative risk while the HINTS and GS surveys asked about relative harm.
Figure 6 provides a closer look at the GS data collected during the EVALI outbreak. From September 2019 through January 2020, the fraction of respondents reporting that e-cigarettes are more or much more harmful has stayed fairly stable at around 30%, with a slight decline in the most recent samples. There is no apparent systematic difference between the responses to surveys that mention THC and those that did not mention THC.
Figure 6:
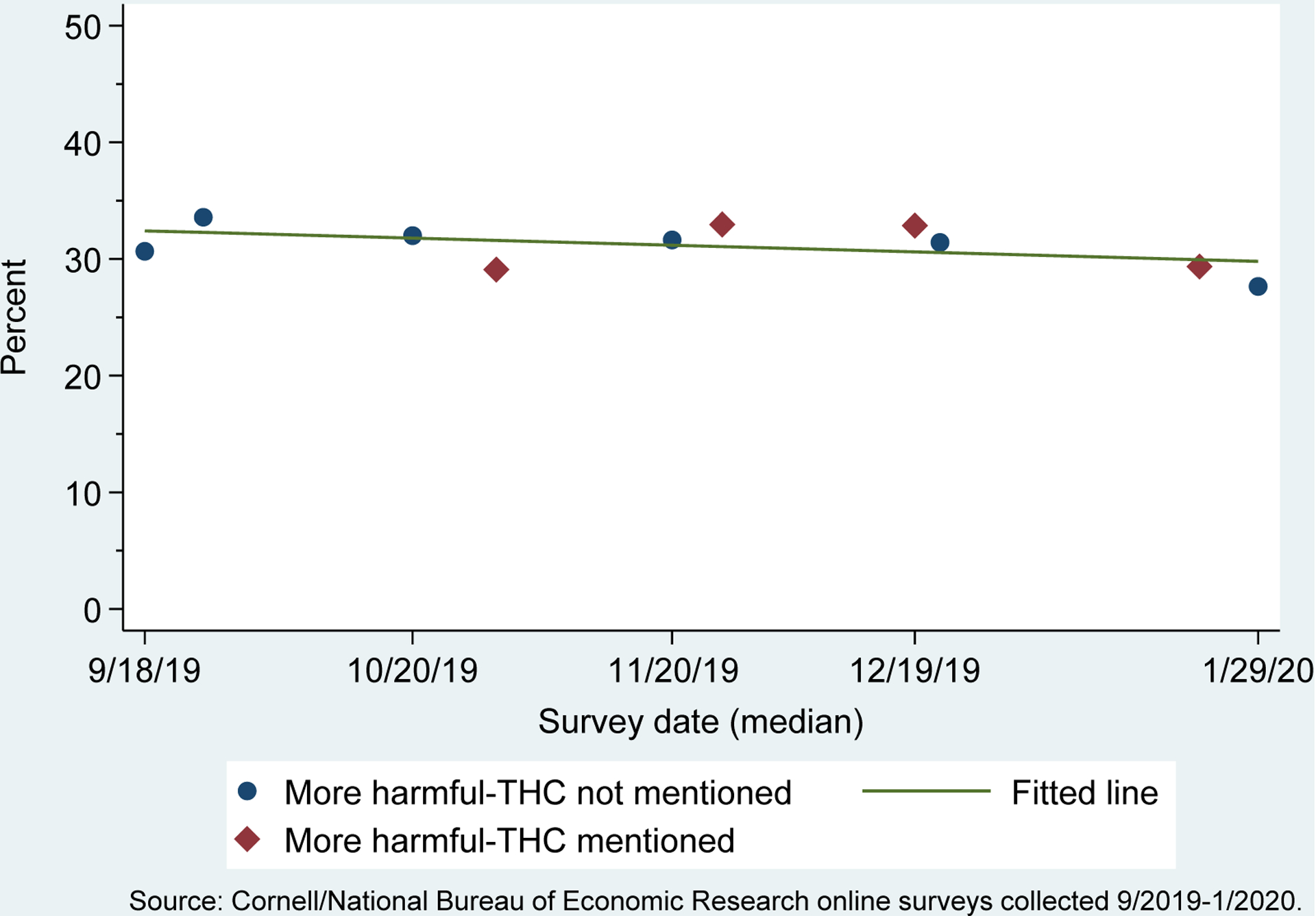
Respondents who think e-cigarettes are more harmful compared to smoking cigarettes GS data
The descriptive statistics and patterns shown in Figures 5 and 6 suggest that there was a sharp upward revision in the relative harm perception of e-cigarettes during the EVALI outbreak, and little downward correction even after the CDC had clarified its message to specifically apply only to THC-containing e-cigarettes. Below, we test for these shifts more formally, while accounting for trends and other potential confounding shifts over this period.
Methods
We begin with a baseline specification to test whether or not there were significant breaks from trend in risk perception after the EVALI crisis. Specifically, drawing on the EVALI timeline, we evaluate two salient periods as the crisis unfolded, and estimate the following specification:
| (4) |
The subscripts denote the ith respondent residing in census division c and interviewed in year t. Equation (4) represents a reduced-form of equation (3), wherein the right-side of equation (3) capturing the informational weights and the information shock is proxied by the crisis indicators. Above, R is a measure of the relative risk perception of e-cigarettes compared with cigarettes ( in equation 3), and is an indicator for whether the respondent perceives e-cigarettes to be more or much more harmful compared with cigarettes.21
We capture two relevant aspects of the crisis period. The first indicator, Outbreak, captures the periods of the EVALI outbreak and equals one for all surveys fielded after August 2019. This is when the CDC identified the outbreak of illnesses associated with vaping. As noted above, during the initial phase of the crisis, there was uncertainty regarding the cause(s) and the CDC recommendations (along with the media reporting) conflated all e-cigarette products including those that delivered only nicotine. These recommendations were subsequently revised and clarified on December 10, 2019, as vaping products containing THC emerged to be the likely cause; the CDC backed away from its earlier blanket recommendation regarding all e-cigarette products, now urging individuals to not use any vaping products containing THC. The second indicator, Clarification THC, therefore turns on for all surveys fielded after this revision and reflects responses to this new information shock. The parameters of interest are the vector π, which captures how these phases of the EVALI outbreak impacted respondents’ relative perceived harm.
The above model controls for whether the GS wave reflected risk perception for nicotine-based e-cigarettes or included a specific reference to THC (THC Mention). Finally, in order to assess that the effects picked up by the crisis indicators are not due to secular trends, we also parametrically control for a linear time trend in year.22
We extend the above baseline specification in several ways to address additional issues. First, we expand the model to account for observed demographics (indicators for gender and age groups) and geographic region (indicators for census division) (denoted X in equation 4). Given that the GS sample is drawn from a slightly different population (adult internet users) than the HINTS (all adults), and given that internet use is a strong function of age and other observed demographics, these controls may address any differences due to the sampling scheme. If the estimates are robust to controlling for the socio-demographics, this provides further validation for the comparability of the HINTS and the GS. Second, we further include a vector of policy controls (denoted Z in equation 4) to assess whether the observed breaks in risk perception during the EVALI outbreak are driven by other confounding factors.
Next, we assess heterogeneity in the response of risk perception during the EVALI outbreak, across socio-demographic factors. Table 2 indicated that certain groups (younger adults, females) were less likely to view e-cigarettes as being harmful compared with conventional cigarettes. We modify equation (4) to including interactions between the crisis indictors and socio-demographics (age groups, gender) in order inform which groups were most elastic in updating their belief, and whether these groups were more likely to further revise their perceived risk following the CDC’s revised recommendations.
Finally, to better understand how prior belief affects risk perception updating, we consider whether the groups that experience the biggest changes in risk perceptions are those groups that started with low levels of e-cigarette harm expectations, or if groups with higher pre-EVALI risk perceptions experience the greater informational shock. One should expect that if groups are more susceptible to information that supports higher e-cigarette harm relative to cigarettes, than these groups will have larger jumps in risk perception around the information shock. Alternatively, groups with low levels of risk perception could be more influenced by the shock simply because they have more room to adjust.
In order to evaluate these hypotheses, we first estimate a model relating risk perception to observed demographics and policy factors prior to the crisis, based on the HINTS data.
| (5) |
The vector X is now fully-interacted, and includes interactions between age groups, gender, and census divisions. This model is used to estimate predicted risk perception for each respondent, for the full dataset, based on their observed age, gender, geographic region, and the policies in effect at the time. We define an indicator (High Risk) for whether the predicted risk perception is higher or lower than the median. Using this predicted risk perception indicator we re-estimate equation (4) but interacting predicted risk with all variables in the model.23
| (6) |
The coefficients of interests are π, with π3 and π4 specifically indicating whether groups who held a relatively higher perceived risk of using e-cigarettes, prior to the EVALI outbreak, adjusted their beliefs more (π3 > 0) or less (π3 < 0) due to the information shock, and whether they updated these beliefs more (π4 < 0) or less (π4 > 0) following the revised information from the CDC regarding the role of THC.
VI. Results
Table 4 presents our baseline estimates for equation (4), for how respondents’ changed their perceived harm of e-cigarettes vs. smoking during the EVALI outbreak. Model 1 presents results from a parsimonious specification, suggesting that there was a significant increase in perceived risk following the outbreak. Specifically, the probability of regarding e-cigarettes as more harmful compared with cigarettes increased by 15.9 percentage points following the outbreak. This represents a substantial updating of perceived harm, 175% relative to the mean across all periods prior to the outbreak, and about 80% relative to the perceived harm in the HINTS wave directly preceding the outbreak. This increase is conditional on, and beyond what would be predicted by, the trend in perceived harm, which is significantly positive at a rate of about two percentage points each year.
Table 4.
Effects of the EVALI Outbreak on Perceived Relative Risk of E-cigarettes as More Harmful
| Model | 1 | 2 | 3 |
|---|---|---|---|
| EVALI Outbreak | 0.15887*** | 0.16797*** | 0.16428*** |
| (0.00659) | (0.00666) | (0.00686) | |
| CDC THC Clarification | −0.02162*** | −0.02319*** | −0.02454*** |
| (0.00570) | (0.00568) | (0.00573) | |
| Question mentions THC | −0.00273 | −0.00180 | −0.00226 |
| (0.00565) | (0.00563) | (0.00564) | |
| Trend | 0.02006*** | 0.01974*** | 0.02268*** |
| (0.00131) | (0.00131) | (0.00179) | |
| Controls for Demographics | No | Yes | Yes |
| Controls for Census Division | No | Yes | Yes |
| Controls for Tobacco Control Policies | No | No | Yes |
| Observations | 37,015 | 37,015 | 37,015 |
| Mean of Dependent Variable | 0.22 | 0.22 | 0.22 |
Notes: Coefficient estimates from linear probability models estimated for the pooled HINTS and GS sample are presented. Standard errors are reported in parentheses. See Table 1 for the list of included control variables. Asterisks represent statistical significance as follows:
p<0.05,
p<0.01,
p<0.001
We also find that there was a slight downward revision of perceived risk, following the CDC’s shift in recommendations highlighting THC-containing e-cigarettes and media reports centering on this subset of vaping products as the common cause of the EVALI outbreak. Model 1 suggests that respondents significantly readjusted their harm perception downward by about two percentage points; however, this downward revision was partial and substantially smaller than the upward revision during the early phase of the outbreak suggesting some stickiness in harm perceptions once they have been adjusted upwards. Hence, overall, belief that nicotine e-cigarettes are more harmful than cigarettes remained significantly higher (by 13.7 percentage points) even after messaging had zeroed in on THC as the cause of the lung injuries. Consistent with the means reported in Table 3 and shown in Figure 5, there is no significant difference in perceived risk across nicotine-based e-cigarettes and all e-cigarette products, including specific reference to THC, over the EVALI outbreak. This is consistent with respondents conflating all e-cigarette products, and thus exhibiting stickiness in their downward revisions once relative positive information on nicotine-based e-cigarettes was implied after narrowing down the cause to only THC-containing vaping products.
Model 2 adds in controls for demographics and geographic region, and model 3 further includes policy controls. The estimates are robust to these controls, continuing to suggest about a 16–17 percentage points upward revision in perceived harm following the outbreak, and a slight two percentage point downward revision following news and recommendations regarding THC. This instills a degree of confidence that the observed break in trend is not driven by differences in the populations surveyed across the HINTS and the GS or by concurrent policy shifts.
Next, we consider heterogeneity in this updating process across demographic groups. Models 1 and 2 in Table 5 assess differential effects by interacting the outbreak indicators with age groups and gender. Estimates are not sensitive across the basic (model 1) and the extended specification (model 2), and we discuss here estimates conditional on the full set of controls. We find that both males and females revised their perceived harm of e-cigarettes upwards following the crisis; however, the upward revision was significantly lower for females (9.6 percentage points) than for males (16.8 percentage points). This difference may be driven by variation in tobacco use across gender.24 In 2018, 21% (13%) of males (females) were smokers, and use of e-cigarettes among males (4.3%) was almost double that among females (2.3%) (2018 National Health Interview Surveys - NHIS). If women have less experience with tobacco products in general, and e-cigarettes in particular, they may find information shocks less salient and thus may be less responsive. There is no significant difference in the downward revision of perceive risk following the THC clarification (both genders exhibiting about a 2.2 percentage points decrease). This, however, does imply heterogeneity in how males and female update their harm perceptions. Males responded more strongly to the adverse informational shock, and “corrected” their beliefs by only about 14% (2.3 / 16.8) in response to more precise information on the cause of the EVALI outbreak. Females, on the other hand, responded less strongly in their upward revision, and when the new information on THC products was disseminated they were relatively quicker in their downward revision (about 2.3/9.6 = 24%). Neither gender, however, completely reverted their risk perceptions to pre-EVALI levels.
Table 5.
Effects of the EVALI Outbreak on Perceived Relative Risk of E-cigarettes as More Harmful Heterogeneous Effects by Demographics and Baseline Risk Perception
| Model | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| EVALI Outbreak | 0.15887*** | 0.16797*** | 0.20347*** | 0.21044*** |
| (0.00659) | (0.00666) | (0.01025) | (0.01124) | |
| CDC THC Clarification | −0.02162*** | −0.02319*** | 0.01592 | 0.01374 |
| (0.00570) | (0.00568) | (0.00982) | (0.00986) | |
| Question mentions THC | −0.00273 | −0.00180 | −0.00298 | −0.00214 |
| (0.00565) | (0.00563) | (0.00565) | (0.00564) | |
| Trend | 0.02006*** | 0.01974*** | 0.00947*** | 0.01112*** |
| (0.00131) | (0.00131) | (0.00175) | (0.00230) | |
| Predicted Risk Perception > Median | - | - | 0.08622*** | 0.08099*** |
| (0.00939) | (0.00981) | |||
| EVALI Outbreak * Pred. Risk Perception>Median | - | - | −0.06584*** | −0.06617*** |
| (0.01194) | (0.01385) | |||
| CDC THC Clarification * Pred. Risk Perception>Median | - | - | −0.04816*** | −0.04767*** |
| (0.01192) | (0.01192) | |||
| EVALI Outbreak * Female | −0.07292*** | −0.07204*** | - | - |
| (0.00953) | (0.00953) | |||
| EVALI Outbreak * Ages 25–34 | −0.00485 | −0.00613 | - | - |
| (0.02444) | (0.02443) | |||
| EVALI Outbreak * Ages 35–44 | 0.02896 | 0.02715 | - | - |
| (0.02404) | (0.02403) | |||
| EVALI Outbreak * Ages 45–54 | 0.08403*** | 0.08252*** | - | - |
| (0.02357) | (0.02356) | |||
| EVALI Outbreak * Ages 55–64 | 0.10089*** | 0.09958*** | - | - |
| (0.02328) | (0.02327) | |||
| EVALI Outbreak * Ages 65+ | 0.12947*** | 0.12723*** | - | - |
| (0.02347) | (0.02347) | |||
| CDC THC Clarification * Female | −0.00774 | −0.00804 | - | - |
| (0.01115) | (0.01115) | |||
| CDC THC Clarification * Ages 25–34 | 0.02845 | 0.02923 | - | - |
| (0.02319) | (0.02318) | |||
| CDC THC Clarification * Ages 35–44 | −0.00277 | −0.00205 | - | - |
| (0.02293) | (0.02292) | |||
| CDC THC Clarification * Ages 45–54 | 0.00540 | 0.00519 | ||
| (0.02269) | (0.02268) | |||
| CDC THC Clarification * Ages 55–64 | −0.02907 | −0.02914 | ||
| (0.02227) | (0.02227) | |||
| CDC THC Clarification * Ages 65+ | −0.03131 | −0.02996 | ||
| (0.02272) | (0.02271) | |||
| Controls for Demographics | No | Yes | No | Yes |
| Controls for Census Division | No | Yes | No | Yes |
| Controls for Tobacco Control Policies | No | Yes | No | Yes |
| Observations | 37,015 | 37,015 | 37,015 | 37,015 |
| Mean of Dependent Variable | 0.22 | 0.22 | 0.22 | 0.22 |
Notes: Coefficient estimates from linear probability models estimated for the pooled HINTS and GS sample are presented. Standard errors are reported in parentheses. See Table 1 for the list of included control variables. Predicted risk perception is based on Equation (5); see text. Asterisks represent statistical significance as follows:
p<0.05,
p<0.01,
p<0.001
We also find a significantly stronger response to the outbreak among older adults. Specifically, adults ages 44 and younger revised their perceived harm upwards by about 16.8 percentage points; in comparison, older adults updated their beliefs by an additional statistically significant 8–13 percentage points, with this increase being monotonic with age. There are no significant differences across age groups in further updating these harm perceptions following reports pointing to THC; however, the point estimates for older adults (ages 55+) are negative (−2.9 percentage points) which suggests that these groups are also quicker to revised their revisions downwards. In order words, older adults experienced a larger swing in their risk perceptions, both on the upside (from the negative information shock) and on the downside (from the relative positive information shock relating to nicotine e-cigarettes as THC was identified as the cause).
While the demographic differences may be related to variation in use and experience with tobacco products, they may also reflect baseline differences in risk perceptions. To further assess whether groups with a higher perceived harm at baseline were more or less likely to update their beliefs, we present estimates for equation (6) in models 3 and 4 (Table 5). These results indicate that those groups who had a higher perceived harm of e-cigarettes relative to cigarettes exhibited a significantly weaker revision of their beliefs on the upside, but were also quicker to revise their beliefs downward following the THC clarification. Specifically, the estimates indicate that groups who had a higher (lower) perceived risk (predicted risk score above median vs. below median) witnessed an increase in their perceived harm by 14.4 percentage points (21 percentage points). This suggests that groups with low levels of risk perception are more influenced by the initial information shock; interestingly these groups do not revise their beliefs downward in any significant manner after the waning of the uncertainty regarding the cause of the EVALI outbreak. Groups who started out with a higher level of risk perception were less responsive to the adverse informational shock; however, after the revisions in the CDC recommendations and reports on the involvement of THC, these groups were also more likely to re-update their beliefs and revise their harm perceptions downwards. Estimates in model 4 indicate that these groups reduced their perceived harm by about 4.8 percentage points following the THC clarification, correcting their initial upward adjustment still only partially by about one-third (4.8 / 14.4).
VII. Discussion
In this paper we study the impact of new information on people’s perceptions of the risks of e-cigarettes. The EVALI outbreak in September 2019 created an information shock, which was followed by additional new information in a later CDC recommendation. Our econometric results suggest that the immediate impact of the first information shock was to increase the fraction of respondents who perceived e-cigarettes as more harmful than smoking by about 16 percentage points. As the outbreak subsided and the CDC recommendation changed to emphasize the role of THC e-cigarette products, e-cigarette risk perceptions were partially revised downwards. Additional econometric results show that different demographic groups reacted somewhat differently to the information shock. In particular, we find that groups who had higher risk perceptions showed a weaker response to the first information shock but were more likely to later revise their risk perceptions downwards.
One approach to public policy towards e-cigarettes follows the precautionary principle that emphasizes the scientific uncertainty about the long-run health consequences of vaping. The EVALI outbreak is an example of the unforeseen risks that the precautionary principle protects against. The early versions of the CDC EVALI recommendations were also consistent with the precautionary principle; the early recommendations broadly advised against the use of e-cigarettes without making distinctions between nicotine and THC products or distinctions between youth and adult use. Our econometric results suggest that an unintended consequence of this approach was that most people did not perceive the extra risks of THC products.
Ironically, the precautionary principle to protect against unforeseen consequences can itself have unintended consequences. More targeted advice about the risks of THC e-cigarettes might have more effectively reduced the use of those products, potentially preventing EVALI cases. Moreover, the increase in e-cigarette risk perceptions might discourage adult smokers from using e-cigarettes as a way to quit smoking, despite evidence from a clinical trial that e-cigarettes are a more effective cessation method than FDA-approved products such as the nicotine patch (Hajek et. al. 2019). More controversially, the increase in e-cigarette risk perceptions might slow the downward trend in youth smoking (Pesko and Warman, 2017). Future work should develop evidence on the links between risk perceptions and vaping and smoking behaviors. Evidence on these links would help complete quantified cost-benefit analysis to inform public policy towards e-cigarettes.
Acknowledgments
Dhaval Dave acknowledges support through grant R01DA039968 from the National Institute on Drug Abuse. The authors are grateful to Cornell University and the Health Thought Leadership Network at Bentley University for funding the data collection. The authors thank Michael Pesko and W. Kip Viscusi for valuable suggestions and feedback. Donald Kenkel is on leave from his academic positions and is currently Chief Economist, Council of Economic Advisers. The article reflects his academic research and is not related to his current position at the Council of Economic Advisers. Any views or opinions expressed in the paper reflect his personal views and are not the views or opinions of the Council of Economic Advisers or the United States government.
Footnotes
On September 27, 2019, the CDC issued the following statement through Twitter: “Lung injury assoc. w/ e-cigarette product use/vaping was recently reported in most states. CDC & others continuing to investigate. CDC recommends considering refraining from using e-cigarette/vaping products, especially those with THC” (see https://twitter.com/CDCgov/status/1177673832909430787). While THC was specifically referenced, the statement conflated all e-cigarette and vaping products and recommended that “while this investigation is ongoing…persons consider refraining from using e-cigarette, or vaping, products, particularly those containing THC” (Perrine et al., Morbidity and Mortality Weekly, October 4 2019). Messages from state health departments generally followed suit. For instance, the state health department in Wisconsin – which was among the first few states to experience EVALI cases – “strongly urge(d) people to avoid vaping products and e-cigarettes” (https://www.dhs.wisconsin.gov/news/releases/080219.htm).
See for instance: “The Mysterious Vaping Illness that’s ‘Becoming an Epidemic’ (New York Times, August 31, 2019, https://www.nytimes.com/2019/08/31/health/vaping-marijuana-ecigarettes-sickness.html); “Vaping Illness Epidemic Shows No Sign of Slowing” (NBC News, October 10, 2019, https://www.nbcnews.com/health/vaping/vaping-illness-epidemic-shows-no-sign-slowing-n1064546); “Vaping is Suspected in Severe Lung Illnesses” (Wall Street Journal, August 22, 2019, https://www.wsj.com/articles/vaping-is-suspected-in-severe-lung-illnesses-11566508797); “Death toll rises from mysterious lung illnesses linked to vaping, prompting CDC to sound alarm on e-cigarettes” (CNBC, September 6, 2019, https://www.cnbc.com/2019/09/06/cdc-reports-at-least-three-deaths-in-vaping-related-lung-disease-outbreak.html).
On December 10, 2019, the CDC noted through its official Twitter account that the “CDC recommends that you do not use e-cigarette, or vaping, products that contain THC, as data suggest these products play a major role in the current lung injury outbreak” (see https://twitter.com/CDCgov/status/1204526209310306304).
See https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html and https://twitter.com/CDCgov/status/1217197454636044289.
Viscusi (2016) measures absolute risk beliefs by asking respondents “Out of every 100 cigarette smokers, how many of them do you think will die from lung cancer?”. Similar questions are asked with respect to e-cigarette use, and with respect to total mortality.
Interestingly, the term EVALI, which conflates all e-cigarettes and vaping products, continues to be used on the CDC website. See https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html#map-cases
Media coverage of the EVALI outbreak highlighted deaths associated with the lung injury, and Google searches for “vaping deaths” and “vaping illness” tracked lock-step from July 2019 through February 2020 (see Figure 3). Hence, focusing on the relative mortality risk is particularly salient for the study of the EVALI outbreak.
The beta distribution is a family of continuous probability distributions, applied to random variables that are constrained along a finite range. Hence, it is particularly well-suited to studying the behavior of perceived probabilities, which by definition are confined to the 0–1 interval. For Bayesian inference, the beta distribution also represents the conjugate prior probability distribution for the Bernoulli and binomial distributions among others.
Given that s and q follow a beta distribution, ϕ0 and γ0 can be interpreted as draws of information, that follow a Bernoulli process, from the set of total information.
The HINTS is a mail-based survey of the U.S. adult, civilian, non-institutionalized population. We use data from the following HINTS cycles: 2012 Cycle 2, 2014 Cycle 4, 2015 FDA, 2017 Cycle 1, 2017 FDA Cycle 2, 2018 Cycle 2, and 2019 Cycle 3.
Since the weights are meant to approximate the national population of internet users, based on their inferred demographics and geographic region, observations that are missing information on any of this are assigned a zero weight by GS. We also exclude these observations with non-valid (zero) weights from all analyses.
About 94% of adults ages 64 and below are internet users, and among adults ages 50 and below, the prevalence ranges from 97–100% (Pew Research Center; https://www.pewresearch.org/internet/fact-sheet/internet-broadband/).
The surveys, on the harm perception of nicotine-based e-cigarettes, were fielded as follows. Wave 1: 9/17/2019 – 9/19/2019; Wave 2: 9/23/2019 – 9/25/2019; Wave 3: 10/18/2019 – 10/20/2019; Wave 5: 11/19/2019 – 11/21/2019; Wave 8: 12/20/2019 – 12/23/2020; Wave 10: 1/27/2020 – 1/29/2020. Surveys, on the harm perception of all e-cigarette products including those that deliver THC, were fielded on: Wave 4: 10/28/2019 – 10/31/2019; Wave 6: 11/25/2019 – 11/27/2019; Wave 7: 12/17/2019 – 12/19/2019; and Wave 9: 1/20/2020 – 1/22/2020. All surveys also included an option for respondents to choose “I don’t know”. The percent of individuals choosing this option fairly substantial but stable over time, across both the HINTS and the GS.
Policy variables were collected using the CDC STATE system. While we are able to observe inferred state of residence in the GS (based on the internet protocol address at the time of responding to the survey), the smallest level of geography in the HINTS is census division. Hence, for consistency, we match the policy data to all records bases on census division. Our main results are virtually unchanged if we match the GS records based on the residential state.
We use the HINTS and the GS sampling weights in generating the data points in Figures 5 and 6. The results are similar if for weighted data points.
We estimate all models using OLS. Results (marginal effects) are robust to using logit or probit estimates.
We present models with linear trends for ease of exposition. Estimates are not sensitive to controls for a quadratic trend.
For convenience, we subsume the other interactions in the reported Equation (6). However, these interactions are included in the estimation. Results are robust to excluding interactions between predicted risk perception and the other variables in the model.
The fielded Google Surveys do not contain information on tobacco use. Hence, we draw on the NHIS for gender differences in smoking and vaping, in relation to the estimated gender effects in risk perceptions.
Contributor Information
Dhaval Dave, Bentley University, National Bureau of Economic Research (NBER) & Institute of Labor Economics (IZA).
Daniel Dench, The Graduate Center, CUNY.
Donald Kenkel, Cornell University.
Alan Mathios, Cornell University.
Hua Wang, Cornell University.
References
- Amrock SM, Zakhar J, Zhou S, & Weitzman M (2015), Perception of E-Cigarette Harm and Its Correlation With Use Among U.S. Adolescents, Nicotine & Tobacco Research, 17 (3), 330–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brose LS. Brown J, Hitchman SC, & McNeill A (2015), Perceived Relative Harm of Electronic Cigarettes Over Time and Impact on Subsequent Use: A Survey With 1- Year and 2-Year Follow-Ups, Drug and Alcohol Dependence, 157 (1), 106–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control (2020), Fast Facts. Diseases and Death. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/fast_facts/index.htm
- Choi K, & Forster JL, (2014), Beliefs and Experimentation With Electronic Cigarettes: A Prospective Analysis Among Young Adults, American Journal of Preventive Medicine, 46, (2), 175–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creamer MR, Wang TW, Babb S, Cullen KA, Day H, Willis G, Jamal A, & Neff L (2019), Tobacco Product Use and Cessation Indicators Among Adults - United States, 2018. MMWR. Morbidity and Mortality Weekly Report, 68(45), 1013–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czoli CD, Fong GT, Mays D & Hammond D (2017), How Do Consumers Perceive Differences in Risk Across Nicotine Products? A Review of Relative Risk Perceptions Across Smokeless Tobacco, E-Cigarettes, Nicotine Replacement Therapy and Combustible Cigarettes, Tobacco Control, 26, (E1). [DOI] [PubMed] [Google Scholar]
- Dave D, Dench D, Grossman M, Kenkel DS & Saffer H (2019). Does e-cigarette advertising encourage adult smokers to quit? Journal of Health Economics, 68, 102227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeCicca P, Kenkel D, & Mathios A, (2008) Cigarette Taxes and the Transition From Youth to Adult Smoking: Smoking Initiation, Cessation, and Participation, Journal of Health Economics, (27), 4, 904–917. [DOI] [PubMed] [Google Scholar]
- DeCicca P, Kenkel D, Mathios A, Shin YJ, & Lin JY, (2008). Youth Smoking, Cigarette Prices, and Anti-Smoking Sentiment, Health Economics, 17, (6), 733–749. [DOI] [PubMed] [Google Scholar]
- Hajek P, Phillips-Waller A, Przuli D, Pesola F, Smith KM, Bisal N, Li J, Parrott S, Sasieni P, Dawkins L, Ross L, Goniewicz M, Wu Q, & McRobbie HJ (2019), A Randomized Trial of E-Cigarettes Versus Nicotine-Replacement Therapy, New England Journal of Medicine, 380 (7), 629–637. [DOI] [PubMed] [Google Scholar]
- Hulland J, & Miller J Keep on Turkin’?. (2018) J. of the Acad. Mark. Sci 46, 789–794 [Google Scholar]
- Kenkel DS, Peng S, Pesko MF, & Wang H (2017). Mostly Harmless Regulation? Electronic Cigarettes, Public Policy and Consumer Welfare, NBER Working Paper No. 23710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koslowski LT & Sweanor D (2016). Withholding Differential Risk Information on Legal Consumer Nicotine/Tobacco Products: The Public Health Ethics of Health Information Quarantines, International Journal of Drug Policy, 32, 17–23. [DOI] [PubMed] [Google Scholar]
- Majeed BA, Weaver SR, Gregory KR, Whitney CF, Slovic P, Pechacek TF & Eriksen MP (2017). Changing Perceptions of Harm of E-Cigarettes Among U.S. Adults, 2012–2015, American Journal of Preventive Medicine, 52, (3), 331–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercer A, Lau A, & Kennedy C (2018), For Weighting Online Opt-In Samples, What Matters Most, Pew Research Center. [Google Scholar]
- Pepper JK & Brewer NT (2014). Electronic nicotine delivery system (electronic cigarette) awareness, use, reactions and beliefs: a systematic review, Tobacco Control, 23 375–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepper JK, Emery SL, Ribisl KM, Rini CM & Brewer NT (2015). How risky is it to use e-cigarettes? Smokers’ beliefs about their health risks from using novel and traditional tobacco products. J Behavioral Medicine, 38, 318–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pericot-Valverde I, Gaalema DE, Priest JS, & Higgins ST (2017). E-Cigarette Awareness, Perceived Harmfulness and Ever Use Among U.S. Adults, Preventive Medicine, 104, 92–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrine CG, Pickens CM, Boehmer TK, King BA, Jones CM, DeSisto CL, Duca LM, Lekiachvili A, Kenemer B, Shamout M, Landen MG, Lynfield R, Ghinai I, Heinzerling A, Lewis N, Pray IW, Tanz LJ, Patel A, Briss PA, & Lung Injury Response Epidemiology/Surveillance Group (2019). Characteristics of a Multistate Outbreak of Lung Injury Associated with E-cigarette Use, or Vaping - United States, 2019. MMWR. Morbidity and Mortality Weekly Report, 68 (39), 860–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pesko M, & Warman C (2017). The Effect of Prices and Taxes on Youth Cigarette and E-cigarette Use: Economic Substitutes or Complements?. Available at SSRN 3077468. [Google Scholar]
- Popova L, Owusu D, Weaver SR, Kemp CB, Mertz CK, Pechacek TF, & Slovic P (2018), Affect, Risk Perception, and the Use of Cigarettes and E-Cigarettes: A Population Study of U.S. Adults, BMC Public Health, 18 (385). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutten LJF, Blake KD, Agunwamba AA, Grana RA, Wilson PM, Ebbert JO, Okamoto J, & Leischow SJ (2015). Use of E-Cigarettes Among Current Smokers: Associations Among Reasons for Use, Quit Intentions, and Current Tobacco Use, Nicotine & Tobacco Research 17, (10), 1228–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santoso LP, Stein R, Stevenson R (2016). Survey Experiments with Google Consumer Surveys: Promise and Pitfalls for Academic Research in Social Science. Political Analysis 24 (3): 356–373. [Google Scholar]
- Siegel DA, Jatlaoui TC, Koumans EH, Kiernan EA, Layer M, Cates JE, Kimball A, Weissman DN, Petersen EE, Reagan-Steiner S, Godfred-Cato S, Moulia D, Moritz E, Lehnert JD, Mitchko J, London J, Zaki SR, King BA, Jones CM, Patel A, Delman DM, Koppaka R, Lung Injury Response Clinical Working Group, and Lung Injury Response Epidemiology/Surveillance Group. (2019). Update: Interim Guidance for Health Care Providers Evaluating and Caring for Patients with Suspected E-Cigarette or Vaping, Product Use Associated Lung Injury – United States, October 2019, MMWR: Morbidity and Mortality Weekly Report, 68 (41), 919–927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sostek K, (2019). Evaluating the Accuracy of Google Surveys, Google Inc. [Google Scholar]
- Sostek K, & Slatkin (2017). How Google Surveys Work, Google Inc. [Google Scholar]
- Tan ASL, & Bigman CA (2014). E-Cigarette Awareness and Perceived Harmfulness: Prevalence and Associations with Smoking-Cessation Outcomes, American Journal of Preventive Medicine, (47), 2, 141–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viscusi WK (2016), Risk Beliefs and Preferences for E-Cigarettes, American Journal of Health Economics, 2 (2), 213–240. [Google Scholar]
- Viscusi WK (2020). Electronic Cigarette Risk Beliefs after the Vaping Illness Outbreak, Journal of Risk and Uncertainty, this issue. [Google Scholar]


