Introduction
Today, nephrology stands at a critical crossroads. The coronavirus disease 2019 (COVID-19) pandemic and sweeping movements to advocate for racial equality have brought into focus the need for each of us to play a part and take the lead to shape our future. The American Association of Kidney Patients has proclaimed the years from 2020 to 2030 “The Decade of the Kidney.”
To create lasting change by 2030, each of us must focus on three key areas: building our workforce; advancing diversity, inclusion, and equity; and expanding innovation and collaboration.
Building Our Workforce
For too long, nephrology has been undervalued compared with other specialties, despite the lifesaving contributions of those in our field. This misperception has dampened interest among students and even residents, reducing the recruitment of talented professionals needed to build on today’s achievements. The COVID-19 pandemic has dispelled this misperception, demonstrating the indispensable value of our specialty. Nephrologists have been visible leaders providing life-sustaining care amid this crisis, but we must also lead in building our workforce.
We must recruit—and value—professionals of divergent races, ethnicities, experiences, and perspectives. Otherwise, we will not build the full range and depth of talent needed to deliver exceptional care, transform our patients’ lives through research and innovation, and educate the next generation.
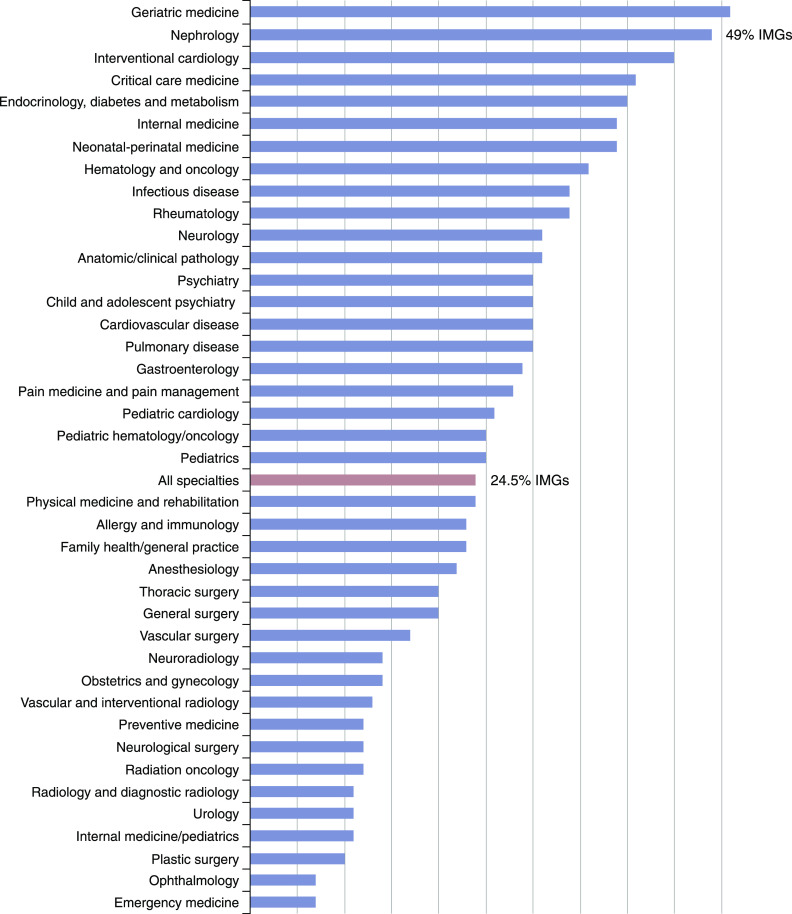
Also, we must focus on a key component of the nephrology workforce in the United States: international medical graduates. Today, 49% of the US nephrology workforce is made up of international medical graduates (Figure 1). Most face unnecessary restrictions on where and how they can practice. We must create avenues for these graduates to achieve permanent residency and citizenship and roll back restrictions that disproportionately affect immigrants from countries with higher rates of immigration to the United States.
Figure 1.
Percentage of physicians who are international medical graduates (IMGs) by specialty (data are from Association of American Medical Colleges 2017 American Medical Association Masterfile).
In addition, we must build a fair compensation structure. Nephrologists provide complex care and 24-hour coverage to a vulnerable patient population, but the remuneration for nephrologists does not reflect this complex care. This reality discourages interest in our specialty, compromises care, and leads many talented physicians to pursue better compensated careers that help pay down staggering medical student debt.
The American Society of Nephrology (ASN) has launched a task force, led by former ASN President Sharon M. Moe, MD, FASN, to help facilitate some of this much-needed change. For example, after 50 years as a board-certified specialty, nephrology should consider developing structured subspecialties (such as transplant nephrology, interventional nephrology, onconephrology, and critical care nephrology) with individual relative value units and compensation benchmarks similar to cardiology to address the changes needed to enhance patient care and professional fulfillment (1,2).
Finally, each of us must commit to ensuring work-life balance for our peers, trainees, and ourselves. We know when we enter health care that we will be called upon in times of crisis. However, we must distinguish crises from routine life. The COVID-19 pandemic and the tensions we are facing with systemic racism have exacerbated the multiple stressors health professionals experience. We must support work-life balance, promote mental health, and reduce stress and burnout. Only then will we have the resilience to lead nephrology forward.
Advancing Diversity, Inclusion, and Equity
In its fullest expression, diversity celebrates differences in age, race/ethnicity, sex, gender, thought, socioeconomic background, geography, and education. Why is diversity important? A richness of experiences, skills, perspectives, and insights empowers us to effect meaningful change. As Google Chief Executive Officer Sunder Pichai observed, “A diverse mix of voices leads to better discussions, decisions, and outcomes for everyone” (3). However, without inclusion, diversity has no meaning. In her Technology, Entertainment, and Design Talk, Verna Myers, Vice President, Inclusion Strategy at Netflix, notes: “Diversity is being invited to the party; inclusion is being asked to dance” (4). I believe inclusion means being essential and welcomed members of the group planning the party, choosing the music, and enjoying the music on the dance floor.
We must create positive, measurable change. Nephrology must reflect the diversity of the patient population we serve. Kidney diseases disproportionately afflict racial and ethnic minorities. Health disparities and limited access to care mean many enter the health care system with advanced kidney diseases. We must begin by focusing on diversity and inclusion in our own backyard, within ASN. For the first time, our eight-member council includes four women, and all eight of us have diverse racial and ethnic backgrounds.
We must also acknowledge when we fall short. Last year, ASN was justly criticized about representation among Kidney Week speakers, moderators, and award recipients. That critique helped us refocus our efforts to ensure that diversity and inclusion are reflected in all facets of our meeting. More than 45% of the 2020 Kidney Week speakers and moderators were women.
We must address the failure of US medical schools to increase representation of racial and ethnic minorities, particularly Black men. In 2021, ASN is launching a loan mitigation program focusing on trainees under-represented in medicine; that program will include outreach to undergraduates and medical students.
Diversity and inclusion can only thrive within a framework of equity. The recent movement around the globe to advocate for racial equality and to end systemic racism has crystallized the urgent need for institutions to embrace and value all people. I promise you, ASN will take the lead in building a racially equitable culture in nephrology throughout the world and will continue to collaborate with other organizations to advance these efforts. I do not minimize these challenges. However, as kidney professionals, our life’s work embraces complexities and difficulties. Together, we will make 2030 look very different than today.
Expanding Innovation and Collaboration
The perception that nephrology lacks innovation compromises our ability to attract future researchers. To lead the way to 2030 and beyond, we must leverage our groundbreaking work. This is one of the most exciting times in kidney research and innovation, encompassing the recent discovery of sodium-glucose co-transporter 2 inhibitors (5) and endothelin antagonists (6) in slowing progression of kidney diseases, the potential use of novel agents to target the hypoxia-inducible factor pathway for anemia in kidney diseases (7), and transformational innovations in dialysis care.
Less than 10% of today’s nephrologists pursue a career in research. In the United States, we must take advantage of the current higher funding levels for the National Institutes of Health. We must support more clinical trials and attract more scientists and researchers into our specialty to drive discoveries of new lifesaving therapies and devices. Additionally, we must inspire the students who will build the next generation of change.
Nephrology needs experts from across the globe, and from a variety of disciplines, to transform the future of our specialty. The COVID-19 pandemic has facilitated new methods of collaboration worldwide. Early in this pandemic, reports from China posted that kidney involvement was not commonly seen in patients with COVID-19 (8). However, as the pandemic hit Europe and the United States, cases of AKI and even glomerular lesions in patients with COVID-19 were increasingly reported from Italy, New York, and other areas.
Continued innovation and discovery in our field depend on outside funding. Together, we must flood the gates of all funding agencies and journals with our ideas, support our undergraduate and graduate students to pursue kidney-related research, make sure lawmakers understand the need to fund kidney research, and collaborate with experts across the globe. These four steps will ensure a future for our profession that will most benefit our patients.
This year, of all years, we should recognize fully what we have accomplished as foundational to future change. We must celebrate our landmark achievements—providing innovative care during a pandemic, developing promising new therapies, and creating research partnerships that make a difference. Our focus has never wavered.
Our patients will continue to benefit from our skills, determination, and commitment, and nephrology will thrive if we
improve practice to identify, prevent, slow, and ideally stop kidney diseases;
advance science and medicine to treat—and ultimately, cure—kidney diseases; and
enrich society by addressing health disparities and social determinants of health.
Then, by 2030, we will
implement systems that value and advance our specialty and our contributions to patients and to public health;
confront and address systemic racism in nephrology;
build a diverse and overflowing pipeline of students and trainees eager to cure kidney diseases;
overcome the barriers social determinants of health impose on kidney care; and
secure the funding that will spur research, discovery, and innovation and improve global health.
Starting today, we, and therefore nephrology, must take the lead.
Disclosures
A. Agarwal reports employment with the University of Alabama at Birmingham; consultancy agreements with Akebia Therapeutics to serve on an expert panel to review new therapeutics on the basis of the hypoxia-inducible factor pathway for AKI, Dynamed to review content related to AKI, and Reata Pharmaceuticals; receiving research funding from the Genzyme/Sanofi Fabry Fellowship Award; receiving honoraria from Akebia Therapeutics, Emory, the University of Southern California, and Vanderbilt; serving on the editorial boards of American Journal of Physiology-Renal Physiology, Kidney International, and Lab Investigation; serving on the advisory board and has stock options for Goldilocks Therapeutics, a New York–based company investigating delivery of drugs in the kidney using nanotechnology for acute kidney disease and CKD; and serving on the advisory boards of Alpha Young LLC and Angion. A. Agarwal’s wife, Lisa M. Curtis, is President for Women in Nephrology (2021).
Funding
None.
Acknowledgments
I thank Drs. Linda F. Fried, FASN, and Jon B. Klein, FASN, cochairs for the Education Committee, as well as the ASN staff, specifically Ms. Jin Soo Kim and Ms. Alex Zapple, for their efficient teamwork. I thank the current and past ASN Council members, particularly the past president and outgoing councilor, Dr. Mark Rosenberg. I also express my sincere gratitude to ASN Executive Vice President Mr. Tod Ibrahim, Ms. Adrienne Lea, and Mr. Kurtis Pivert. I am grateful to the members of my Division of Nephrology at the University of Alabama at Birmingham, as well as members of my research group. A special thanks to my mentors, Drs. K.S. Chugh, Karl A. Nath, C. Craig Tisher, and Harry Nick, who played key roles in shaping my career in academic nephrology. Finally, I express my love and gratitude to my family: my wife and a kidney scientist, Dr. Lisa M. Curtis, for her unconditional support and counsel and our children Alex and Megan.
This article is drawn in part from comments delivered during the ASN President’s Address at ASN Kidney Week 2020 Reimagined on Thursday, October 22.
The content of this article reflects the personal experience and views of the author(s) and should not be considered medical advice or recommendations. The content does not reflect the views or opinions of the American Society of Nephrology (ASN) or CJASN. Responsibility for the information and views expressed herein lies entirely with the author(s).
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Agarwal A, Ibrahim T: Stepping into the void: Remunerating, valuing, and understanding nephrologists. Clin J Am Soc Nephrol 15: 1832–1834, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sachdeva M, Shah AD, Singh HK, Malieckal DA, Rangaswami J, Jhaveri KD: Opportunities for subspecialization in nephrology. Adv Chronic Kidney Dis 27: 320–327.e1, 2020 [DOI] [PubMed] [Google Scholar]
- 3.Pichai S: Let’s not let fear defeat our values. 2015. Available at: https://medium.com/@sundar_pichai/let-s-not-let-fear-defeat-our-values-af2e5ca92371. Accessed December 1, 2020
- 4.Myers V: How to overcome our biases? Walk boldly toward them. 2014. Available at: https://www.ted.com/talks/verna_myers_how_to_overcome_our_biases_walk_boldly_toward_them. Accessed December 1, 2020
- 5.Heerspink HJL, Stefánsson BV, Correa-Rotter R, Chertow GM, Greene T, Hou F-F, Mann JFE, McMurray JJV, Lindberg M, Rossing P, Sjöström CD, Toto RD, Langkilde A-M, Wheeler DC; DAPA-CKD Trial Committees and Investigators: Dapagliflozin in patients with chronic kidney disease. N Engl J Med 383: 1436–1446, 2020 [DOI] [PubMed] [Google Scholar]
- 6.Heerspink HJL, Parving HH, Andress DL, Bakris G, Correa-Rotter R, Hou FF, Kitzman DW, Kohan D, Makino H, McMurray JJV, Melnick JZ, Miller MG, Pergola PE, Perkovic V, Tobe S, Yi T, Wigderson M, de Zeeuw D; SONAR Committees and Investigators: Atrasentan and renal events in patients with type 2 diabetes and chronic kidney disease (SONAR): A double-blind, randomised, placebo-controlled trial [published correction appears in Lancet 393: 1936, 2019 10.1016/S0140-6736(19)30939-0]. Lancet 393: 1937–1947, 2019 [DOI] [PubMed] [Google Scholar]
- 7.Kurata Y, Tanaka T, Nangaku M: Hypoxia-inducible factor prolyl hydroxylase inhibitor in the treatment of anemia in chronic kidney disease. Curr Opin Nephrol Hypertens 29: 414–422, 2020 [DOI] [PubMed] [Google Scholar]
- 8.Wang L, Li X, Chen H, Yan S, Li D, Li Y, Gong Z: Coronavirus disease 19 infection does not result in acute kidney injury: An analysis of 116 hospitalized patients from Wuhan, China. Am J Nephrol 51: 343–348, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]