The Extracellular Matrix in Development, Aging, and Disease
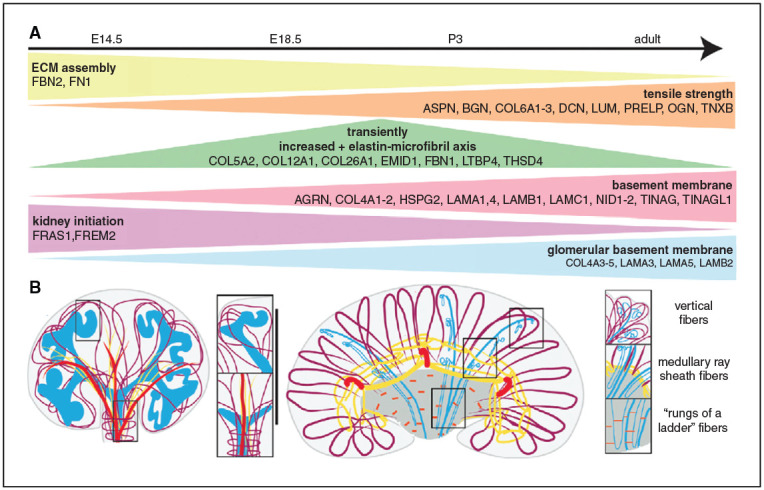
The extracellular matrix (ECM) biomechanically regulates nephrogenesis, and abnormal ECM is a histologic feature of kidney aging and disease. Two reports in this issue use state-of-the-art methods to characterize the ECM in development, aging and disease. Lipp et al. used proteomics and 3D imaging of the murine kidney to investigate dynamics of the interstitial matrix of the cortex and corticomedullary junction during development. Scaffolds modeled after the composition and organization of the developing ECM have the potential to improve engineeredmodels of the kidney. In the second report, Randles et al. describe ultrastructural and proteomic studies inmouse models of genetic kidney disease and human tissue to define amolecular basis for alteredmatrixwith aging and disease progression.Within both aging and disease, basement membrane components were reduced and interstitial matrix proteins were increased, suggesting that a signature of altered matrix proteins might have utility as a biomarker of kidney health. See Lipp et al., pages 1649–1665 and Randles et al., pages 1713–1732. Also see related editorial by Clotet-Freixas and Konvalinka, pages 1541–1543.
Plasma Proteomics of Kidney Function
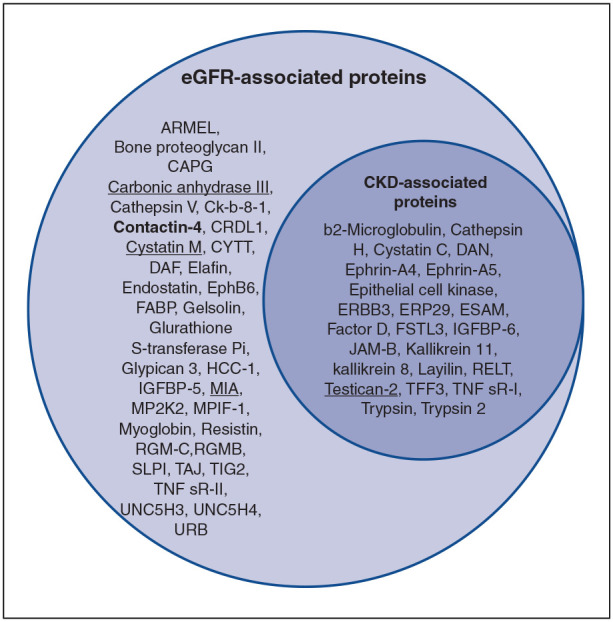
Studies examining the association of the plasma proteome with renal function have identified several biomarkers, but have limitations such as lacking replication, including only European populations, or not investigating correlation with the development of chronic kidney disease (CKD). The authors found that among four cohorts in a trans-ethnic cross-sectional study, 57 plasma proteins were associated with estimated glomerular filtration rate, 23 of which were also associated with CKD. Mendelian randomization and gene expression analyses in kidney tissue highlighted testican-2 as a physiological marker of kidney disease progression with potential clinical relevance, and identified a few additional proteins warranting further investigation. See Matías-García et al., pages 1747–1763.
Lost Opportunities for Kidney Transplant
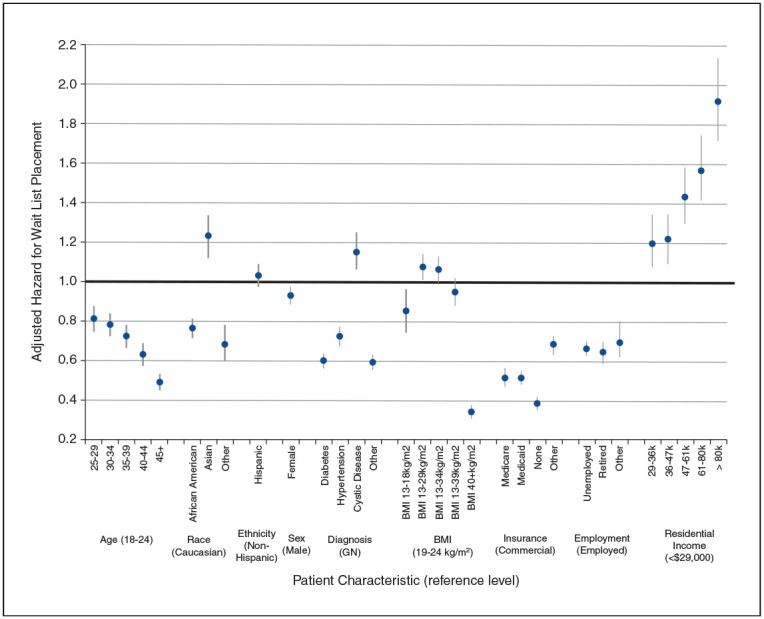
Transplant candidates with top 20% Estimated Post-Transplant Survival (EPTS) scores, which signify longest expected survival post-transplantation, are prioritized to receive optimal deceased-donor kidneys. An analysis of registry data found that fewer than half of eligible end-stage kidney disease patients with top 20% EPTS scores were placed on the transplant waiting list. Nonlisted patients were disproportionally Black/African American, lacked commercial insurance, and resided in lower-income communities. Many patients, particularly those initiating dialysis before waitlist placement, lose EPTS status over time, narrowing the window to receive an optimal deceased-donor kidney based on top EPTS status. These findings point to barriers to transplant among some patients with excellent prognoses and a need for efforts to expedite their access to transplantation. See Schold et al., pages 1733–1746. Also see related editorial by Gill, Butler, and Powe, pages 1544–1545.
Anemia Treatment for Nondialysis-Dependent CKD
Hypoxia-inducible factor prolyl hydroxylase inhibitors (HIF-PHIs) have been shown in clinical trials to increase hemoglobin levels via production of endogenous erythropoietin. Vadadustat, an oral HIF-PHI, is an alternative to erythropoiesis-stimulating agents for treating chronic kidney disease (CKD)–related anemia. This appears to be the first phase 3 randomized trial to demonstrate noninferiority of vadadustat to darbepoetin alfa for treatment of anemia in Japanese patients with nondialysis-dependent CKD. Mean hemoglobin increased to the target range (11.0–13.0 g/dl) in participants receiving vadadustat, and was within this range up to week 52. Vadadustat was generally well tolerated over 52 weeks of treatment and exhibited no major safety concerns. These findings suggest that vadadustat may be a potential treatment for anemia in patients with nondialysis-dependent CKD. See Nangaku et al., pages 1779–1790.



