Abstract
As the COVID-19 pandemic continues causing problems around the world, Chile is facing a new episode of increasing cases and deaths. However, at the same time, the country has succeeded in providing vaccines for an important part of its population over a short period.
What are the factors behind this successful process? What are the challenges faced by the country today? This article explores potential explanations for the “Chilean paradigm”, regarding the COVID-19 vaccine rollout. Borrowing from implementation science frameworks, the analysis proposed an alternative explanation—based on multiple actors, approaches, and history—as opposed to one in which the outcome is due mainly to the government’s performance.
The rapid and extensive coverage of vaccination can be explained by the role played by the government and the academia in securing vaccines through a pragmatic approach; the capacity built at local level, as well as the coordination between the health system and local authorities; and favorable vaccine culture, developed through the implementation of the National Immunization Program. Short and long-term elements (such as investment in infrastructure and relationships between stakeholders, and actions carried out during the pandemic), as well as contextual factors (such as the political and socioeconomic context), provide a more complex story to explain the observed outcomes.
While other countries could try to follow the Chilean example, the article shows that short-term actions are necessary but might not be sufficient to achieve results. At a global level, the situation calls for rethinking how countries will face these global challenges, including issues such as international cooperation and global health governance.
Keywords: Vaccines, Chile, Implementation Science, COVID-19
Introduction
Chile has been hit by the COVID-19 disproportionately compared to other countries. In 2021, the country is still among the most affected countries in the world in terms of cases and deaths [1]. As the country was still struggling with the 2020 wave, cases started to increase in January 2021; while the country’s peak of daily cases reached almost 7,000 in June 2020, during 2021 these figures already surpassed the 9,000 cases per day in April 2021 [2].
It was in this scenario that the country faced the availability of COVID-19 vaccines. Like many other countries, the new vaccines became a symbol of hope but also a public policy challenge, since they represented an opportunity to meet their population’s needs after a year 2020 plagued by problems.
In December 2020, Chile announced the arrival of the first shipment of vaccines and a vaccination schedule that would eventually cover most of the country [3]. This process was centrally planned and comprised the definition of priority group and a detailed calendar in which people on each group should receive the first dose [4], [5]. The strategy was based on international recommendations, as well as the opinions from an external Expert Advisory Committee [6], [7].
Chile constitutes an interesting case study. First, it is a developing country, geographically isolated, and that relies on imports to satisfy the demand for vaccines. Today, the country represents a paradox. Chile is still one of the countries with more cases and deaths per capita [1]. However, and despite the adverse context—including geographical, economic, and political environment—, the country has achieved relatively high coverage of COVID-19 vaccination in a short period [8]. The mass COVID-19 vaccination campaign started in February 2021, and by July 26, more than 24 million doses have been administered, which represents 63.07% of the total population fully vaccinated [9]. Countries with similar populations in the region have lower coverage, such as Ecuador (11.43%) or Guatemala (1.68%). Countries with a human development index similar to Chile's (0.851) have lower coverage, such as Uruguay (61.2%), Portugal (49.9%), Panama (15.81%) and Argentina (12.98%). Other countries in the region have lower coverage, such as Mexico (18.31%), Brazil (17.42%) or Peru (13.18%). Chile's coverage is above that of developed countries, such as the United Kingdom (54.43%), Spain (54.32%) or the United States (48.57%). [10], [11].
The aim of this article is to identify the elements behind the country’s successful COVID-19 rollout as well as lessons and challenges derived from this process. The analysis is relevant to many countries today—as they keep searching for strategies to cope with the second year of the COVID-19 pandemic and the challenge of implementing a large-scale vaccine rollout—and in the coming years—as new variants develop and uncertainty about the vaccination strategy increases [12], [13].
Material and methods
The successful vaccine rollout in Chile has attracted international attention, mainly considering the difficulties that many countries still face in securing vaccines for their people [14]. What explains this apparently unexpected success?
One reason that has been used to explain the phenomenon lies in the government’s strategy and its proactive role in foreseeing the need to ensure enough doses to cover the whole country [11], [15]. However, limiting the observed outcome to this explanation is an unnecessary reduction of reality, and it is simply wrong. Although the government’s actions in this process need to be acknowledged, we present a broader explanation in which the government is not the sole responsible for the results, and where the actions carried out during the past months are not the only ones that explain the outcome.
Here, we expand the government’s management theory to one that includes more actors as well as a longer process behind the vaccine rollout success, instead of limiting it to the initiatives performed during 2020.
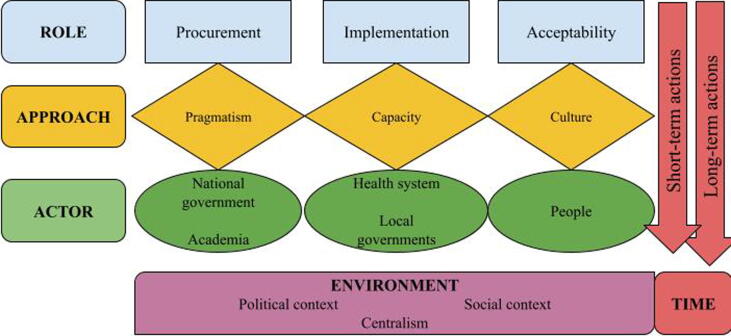
Borrowing from implementation science frameworks, we propose an explanation that includes the roles and interactions between different components of the intervention—provider, implementation, recipient, and environment—as an explanation for the observed outcome [16]. Fig. 1 represents this broader picture in which different actors—government, academia, the health system, local authorities, and the people—interact in contributing to the observed outcome. For each one of these actors, a role and a particular approach is identified to understand their contribution in the COVID1-9 vaccine rollout. In line with the proposed framework, we consider both implementation components and implementation time in the analysis.
Fig. 1.
Map of stakeholders, roles, and approaches in the vaccine rollout in Chile.
Regarding the implementation components—provider, intervention, recipient, and environment—, the intervention was defined as the vaccine rollout, while the main provider, i.e. the one who designed the implementation is the national government. As we explore in the analysis, the intervention also has providers at different levels. As for the environment, it is necessary to consider the socioeconomic and political context in which the intervention is carried out. In the case of Chile, the social context has been heavily shaped by the social outbreak that started in October 2019 [17]; on the other hand, the political environment, including the process to change the Constitution and the recent elections [18]. Finally, some institutional aspects of the country, notably centralized decision-making process, are also included as relevant to understand some of the results [19]. This is particularly useful to establish comparisons with other countries.
In terms of the time of implementation, the study consider actions carried out by different actors in the short and the long-term, i.e. initiatives developed to as part of the COVID-19 vaccination process—mostly carried out during 2020 and 2021—, as well as other relevant processes that have been occurring in the past decades.
The analysis is based on official documents issued by the government, as well as media sources published during 2020 and 2021.
Results
Following the scheme depicted in Fig. 1, the analysis is presented looking at the specific contributions of the three group of key actors identified. In each case, their role and approach is explained.
Pragmatism in procurement: Government and academia
Within this strategy, the key approach was pragmatism. This approach was manifested through the country’s goal of obtaining as many vaccine doses as possible, regardless of where they came from [20]. In this line, two main players were behind the successful procurement process: first, academic institutions that ensured doses by partnering with laboratories to perform vaccines’ clinical trials in the country and; second, the government that decided to diversify the pool of agreements with potential providers.
Regarding the first point, Chile was offered to host clinical trials to different laboratories; finally, four laboratories ended up carrying out trials in the country: Sinovac partnered with the Universidad Católica, Oxford-AstraZeneca and Janssen developed clinical studies in the country in agreement with the Universidad de Chile, and CanSino-Laval developed the clinical studies with the Universidad de la Frontera [21]. Here, it is important to highlight that each one of the partners all had a network of public health centers, which allowed them to recruit potential volunteers. In this case, this group of universities contributed to the availability of vaccines and their successful implementation by promoting collaboration with the pharma industry, essentially trading access to vaccines for research and facilitating the development of clinical trials [21].
On the other hand, the government also played a role in the procurement strategy. In this case, the country used a strategy of diversification of providers, purchasing as many vaccines from as many providers as possible [22]. Although there is no information on the contracts and prices paid for each vaccine, the Government of Chile has recognized agreements with Sinovac, Pfizer-Biontech, Oxford-AstraZeneca, and Janssen, as well as agreements on the provision of doses through COVAX, an initiative led by several international organizations aimed to provide a more equitable access to COVID-19 vaccines [22], [23]. It has been pointed out that there are pre-agreements with Sinopharm, CanSino, the Serum Institute, and the Gamaleya Institute for Sputnik V [22].
Data reported by international sources show that Chile would be the country with the highest number of doses assured per capita, with more than 200% of doses with respect to the population [24]. In both cases—universities’ partnership and government’s agreements with the industry—pragmatism was the guiding principle. In geopolitical terms, the country used the principle of active non-alignment, i.e. buying vaccines regardless of the laboratory’s features, including different management/ property nature (public or private) and country of origin. Hence, the country reached agreements with a state-owned Chinese laboratory (Sinovac), as well as private ones from different countries: United States-Germany in the case of the Pfizer-Biontech alliance; Oxford-AstraZeneca from England; Serum Institute from India; China-Canada in the case of CanSino, and Gamaleya Institute - Sputnik V from Russia [22]. The country’s political and social context—starting with the social outbreak in October 2019 and followed by the entry of the COVID-19 into the country—, and the fact that Chile has a centralized government, provided a strong motivation (improve the low population approval) and means (quick decision-making, national-level standards, and guidelines) for the government to perform well [11].
Fig. 1 also establishes the existence of short and long-term actions carried out for these players. The short-run activities have been highlighted as the “proximal cause” of the outcomes: the government made agreements with several laboratories, and universities secured doses through clinical trials. However, there are “distal causes” that made these short term actions possible: a long list of bilateral and multilateral agreements between Chile and several countries points out more of a success of the Chilean diplomacy (over decades) than the single efforts of the current authorities; similarly, the agreements in the academic realm can be explained by a longer process of building partnerships.
Capacity for implementation: Local stakeholders and health system
A second crucial factor in explaining the successful vaccination was the design of a strategy that considered the capacity already in place in the intervention’s design. In the case of Chile, the vaccination process was led at the central level but implementation was carried out at the local level, mostly using resources from the primary health—but also public hospitals and private providers— and local governments [4]. One of the main features of the Chilean health system is its segmentation—people covered either by public or private health insurers—and fragmentation—low level of integration between levels and between public and private providers [25], [26]. This scenario presents an important challenge in terms of coordination and implementation of interventions at the national level.
Here, the local authorities and the primary health care (PHC) played an important role. The Chilean health system is based on a Family Health Model, a person-centered model with emphasis on promotion and prevention, and that coordinates healthcare services between the health system and the community [27]. The model has a territorial approach, in which health centers are matched to specific geographical areas; this link encourages a permanent collaboration between actors at the local level—health, education, and social policy—, with better information on the territory’s features and needs. This environment facilitated implementing the campaign by using PHC as well as local resources.
The process that started at the national level with the procurement strategy to ensure availability of doses was complemented by an efficient implementation at the local level, supported by PHC—contributing with technical resources—and local authorities—facilitating local-level resources, such as spaces and staff, and promoting it. Primary care covers more than 70% of the population, has more than 2,500 establishments, almost 60,000 workers [26]. It is estimated that 6,000 health professionals are available daily for vaccination [28]; exceptionally dentists and midwives were also authorized to vaccinate during this campaign [4]. On the other hand, vaccination was carried out in health centers but also schools, recreational spaces such as parks and sports facilities, and streets and parking lots. Additionally, local authorities had strong incentives to perform this process successfully, considering that 87% of the PHC is municipal, and the vaccination process took place during the campaigns for the municipal elections [29].
The other factor helping the implementation of the vaccination campaign was the existence of installed capacity in the country. After the H1N1 flu pandemic, in 2009, Chile created a National Network of Vaccine and Immunoglobulin Deposits, with 26 centers in the country [30]. This infrastructure contributed to solving important logistic issues that appeared with the COVID-19 vaccines. For example, it had the equipment to meet the hyper-freezing requirement for the Pfizer-Biontech vaccine, which otherwise would have limited the alternatives for the country [31]. Also, all the PHC centers in the country, even the smallest, had already implemented a cold chain for vaccines, used to implement the National Immunization Plan [30]. In a similar vein, in 2011 the country created an Electronic Vaccine Registry [30]. This tool has been important in the COVID-19 vaccine rollout, particularly to monitor the coverage in different populations and to carry out the follow-up process. This has been key to support the strategy—increasing efficiency and minimizing mistakes—, considering the existence of different vaccination schedules for different groups, vaccines that require two doses, and the presence of several different vaccines at the same time in the same place.
In this case, the time dimension is also relevant. As the coordination between different institutions at the local level (and between local and national authorities) was fostered by the political environment (elections), the channels which permitted that coordination has been built through the years, mainly with the implementation of the Family Health Model and the presence of PHC. Similarly, as much as the implementation of vaccination centers implied investing new resources, the core infrastructure that enabled the implementation of the vaccination campaign—including physical capital, human capital, and information systems—is the result of several years of changes, mostly investments in the public health sector. Nothing but health system strengthening.
Acceptability and culture: The role of people
Finally, considering the scale of the intervention, people need to be considered in the analysis. Vaccines can be available, providers can deliver but, in the end, it is people who voluntarily decide whether to be vaccinated.
One factor that explains the high willingness of being vaccinated is pandemic fatigue. The country has been severely affected; besides the uncertainty in the current context of increasing cases and deaths, a large fraction of the population has been exposed to prolonged periods of restrictions, including lockdowns and a curfew that started in October 2019, after the social outbreak [32]. Fear and the promise of a quick “solution” could explain the Chilean phenomenon, as it has been communicated by the country’s authorities [33], [34], [35]. Other elements related to the large coverage could be related to the action of the government. In this case, the government’s media campaign, as well as other policies, such as the recently issued mobility pass that allow people to move in lockdown areas [36], can also be identified as incentives behind people’s decisions, aligning intervention’s and recipient's goals [37], [38].
However, there are long-term issues—particularly the country’s vaccine culture—that need to be considered. This underlying element can explain people's willingness to vaccinate directly but could also have an indirect effect, potentiating the impact of the short-term measures.
This vaccine culture is related to the existence of public trust and awareness of the benefits of vaccines. Of course, this culture was not developed overnight. A first factor is the existence of the National Immunization Program (PNI by its Spanish acronym), established in 1978 [30]. Among its achievements the PNI allowed Chile to become a leader in the region regarding the eradication of diseases such as smallpox in 1950 and polio in 1975 [39]. Today, vaccination processes have high adherence. For example, the influenza vaccine—with coverage between 80% and 90% in the previous five years and 99% during 2020 [40]—, can be seen as “training” since it also has defined priority groups that are vaccinated over a short period [41]. This is particularly important, considering the increasing influence of the anti-vaccines movements around the world [42].
Finally, the vaccination calendar also took into account the complex social and political environment since the outbreak in October 2019. Considering the great awareness of the existing inequalities in the country [43], [44], the strategy defined priority groups that started with people at higher risk—health personnel, older people—generating a sense of justice and a common goal, since people who were more in need were the first receiving the vaccine, while the rest waited for their turn [4]. The vaccine was also offered for free, which also could have enhanced these feelings, contrary to unpopular measures taken during 2020, such as charging for PCR tests or relying on private providers to host COVID-19 patients [44]. The fact that, contrary to other countries, authorities were vaccinated when scheduled according to the vaccine calendar also contributed to this feeling [45], [46], [47].
Discussion
The article shows some elements to understand the successful COVID-19 vaccination process in Chile and draw lessons for other countries. From an implementation science perspective, this success can be explained by the alignment between the designed intervention (the vaccination strategy) and the existing capacities in the country. In this line, the first element highlighted by the analysis is the need to abandon the search for “silver bullets” or attribute the success of the process to one specific actor or action. The Chilean case shows that the observed outcome is the product of the decisions of several stakeholders. Although not necessarily coordinated, they managed to achieve the desired results.
Similarly, the study shows that short-term actions are necessary but might not be sufficient. Again, this goes against the idea of implementing magic solutions in a short span. Even though the role of governments in reacting proactively is important, success—at least in the Chilean case—cannot be exclusively by actions developed during the past months. Previous experience in vaccine rollout, emergency preparedness, as well as the installed capacity within the health system is crucial for understanding the high rates of vaccination. These factors have also been identified as key in other high-performing countries, such as Israel, although others (like geography and small size) do not necessarily apply to Chile [11], [48]. This conclusion put back the relevance of investing in health systems strengthening as an effective way to improve preparedness.
This article presents some elements to understand the Chilean successful vaccine rollout. However, the fact that the country is, at the same time, experiencing the worst figures in terms of cases and deaths turns this “Chilean paradigm”—i.e. how to carry out the vaccination process—into a “Chilean paradox”. The high vaccination/ increasing contagion scheme becomes the main lesson/ challenge for Chile and other countries: how to balance coexistence between the preventive message (and the need to keep basic preventive measures) with the message of victory coming from the vaccine rollout. Although counterintuitive at first sight, the observed “paradox” can be also explained by other factors, such as the decline in temperatures due to change to cold seasons in the Southern hemisphere, and the irruption of new SARS-CoV-2 variants [13]. In the long run, the country also faces important challenges, related to the dynamics of the pandemic, including the rise of new variants and the consequent debate on the effectiveness of the vaccine and its future rollout [12].
Finally, the effect of vaccination on health outcomes needs to be evaluated. Although a recent study showed the effectiveness of the CoronaVac vaccine in reducing cases, hospitalizations, and deaths in the country, long run results—considering the rise of new variants and the development of new vaccines—are still uncertain [12], [49]. This information will be key for planning strategies and assessing the vaccination process [11].
Conclusions
The lessons from the Chilean experience are important to other countries looking for strategies to deal with the COVID-19 pandemic in a world with COVID-19 vaccines. At the country level, Chile, as well as the rest of the world will continue struggling to respond to the challenges posed by the pandemic, including the emergence of new variants, economic pressures, and new ways to establish links between countries. However, the situation also calls for rethinking how countries will face these global challenges in the future, including issues such as international cooperation and global health governance [50]. Hopefully, the new normal will be different.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Claudio Castillo, Email: claudio.castillo.c@usach.cl.
Pablo Villalobos Dintrans, Email: pvillalobos.d@gmail.com.
Matilde Maddaleno, Email: matilde.maddaleno@usach.cl.
References
- 1.Johns Hopkins University. Coronavirus Research Center. Baltimore: Johns Hopkins University; 2021. Available from: https://coronavirus.jhu.edu/; 2021 [accessed 2021 May 20].
- 2.Gobierno de Chile. Cifras Oficiales COVID-19. Santiago: Gobierno de Chile; 2021. Available from: https://www.gob.cl/coronavirus/cifrasoficiales/; 2021 [accessed 2021 Jun 3].
- 3.Ministerio de Salud de Chile. Presidente Piñera recibe primer cargamento de vacunas contra el COVID-19: “Son una luz de esperanza”. Santiago: Ministerio de Salud; 2020. Available from: https://www.minsal.cl/presidente-pinera-recibe-primer-cargamento-de-vacunas-contra-el-covid-19-son-una-luz-de-esperanza/; 2020 [accessed 2021 Jun 1].
- 4.Ministerio de Salud de Chile. Resolución Exenta N°1138 del 24.12.2020 que aprueba Lineamientos Técnico Operativos Vacunación SARS-CoV-2. Santiago: Ministerio de Salud; 2020. Available from: https://www.minsal.cl/wp-content/uploads/2020/12/RE-N%C2%BA-1138-Lineamientos-SARS-CoV-2.pdf; 2020 [accessed 2021 Jun 1].
- 5.Ministerio de Salud de Chile. Calendario de vacunación masiva contra COVID-19. Santiago: Ministerio de Salud; 2021. Available from: https://www.minsal.cl/calendario-de-vacunacion-masiva-contra-covid-19/; 2021[accessed 2021 Jun 3].
- 6.World Health Organization. WHO SAGE values framework for the allocation and prioritization of COVID-19 vaccination. Geneva: World Health Organization; 2020. Available from: https://apps.who.int/iris/bitstream/handle/10665/334299/WHO-2019-nCoV-SAGE_Framework-Allocation_and_prioritization-2020.1-eng.pdf?sequence=1&isAllowed=y; 2020 [accessed 2021 May 20].
- 7.Comité Asesor en Vacunas y Estrategias de Vacunación. Consideraciones del Comité Asesor en Vacunas y Estrategias de Vacunación (CAVEI) en relación con los servicios de vacunación durante la emergencia sanitaria COVID-19. Rev Chil Pediatr. 2020; 91(4). doi: 10.32641/rchped.vi91i4.2475. [DOI] [PubMed]
- 8.The Lancet. COVID-19 in Latin America-emergency and opportunity. Lancet. 2021;10;398(10295): 93. doi: 10.1016/S0140-6736(21)01551-8. [DOI] [PMC free article] [PubMed]
- 9.Ministerio de Salud de Chile. DEIS. Avance de vacunación SARS-Cov2 en Chile 2020-2021. Santiago: Ministerio de Salud; 2021. Available from: https://informesdeis.minsal.cl/SASVisualAnalytics/?reportUri=%2Freports%2Freports%2F9037e283-1278-422c-84c4-16e42a7026c8§ionIndex=1&sso_guest=true&sas-welcome=false; 2021 [accessed 2021 Jul 26].
- 10.Mathieu E., Ritchie H., Ortiz-Ospina E., Roser M., Hasell J., Appel C. A global database of COVID-19 vaccinations. Nat Hum Behav. 2021;5:947–953. doi: 10.1038/s41562-021-01122-8. [DOI] [PubMed] [Google Scholar]
- 11.Aguilera X., Mundt A.P., Araos R., Weitzel T. The story behind Chile's rapid rollout of COVID-19 vaccination. Travel Med Infect Dis. 2021;26(42) doi: 10.1016/j.tmaid.2021.102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.García L.Y., Cerda A.A. Authors’ Reply to Sprengholz and Betsch: “Willingness to Pay for a COVID-19 Vaccine”. Appl Health Econ Health Policy. 2021;19:623–624. doi: 10.1007/s40258-021-00657-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Taylor L. Covid-19: Spike in cases in Chile is blamed on people mixing after first vaccine shot. BMJ 2021; 373: n1023. doi: 10.1136/bmj.n1023. [DOI] [PubMed]
- 14.United Nations News. Without access to vaccines, COVID will continue widening inequality everywhere. New York: United Nations; 2021. Available from: https://news.un.org/en/story/2021/04/1089462; 2021 [accessed 2021 Jun 4].
- 15.Black M., Ford J., Lee A. Vaccination against COVID-19 and inequalities - Avoiding making a bad situation worse. Public Health Pract (Oxf) 2021;2 doi: 10.1016/j.puhip.2021.100101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Villalobos Dintrans P., Bossert T.J., Sherry J., Kruk M.E. A synthesis of implementation science frameworks and application to global health gaps. Glob Health Res Policy. 2019;4:25. doi: 10.1186/s41256-019-0115-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fraser B. Violent protests in Chile linked to health-care inequities. Lancet. 2019;394(10210):1697–1710. doi: 10.1016/S0140-6736(19)32720-5. [DOI] [PubMed] [Google Scholar]
- 18.BBC. Chile constitution: Sweeping changes possible as independents win. BBC; 2021. Available from: https://www.bbc.com/news/world-latin-america-57142087; 2021 [accessed 2021 Jun 4].
- 19.Biblioteca del Congreso Nacional de Chile. Chile, el país mas centralizado de Latinoamérica. Santiago: Biblioteca del Congreso Nacional de Chile. Available from: https://www.bcn.cl/seminarios_actividades/evento.html?h=10221.1/54934&hs=10221.1/54925; 2015 [accessed 2021 Jun 4].
- 20.Ministerio de Salud de Chile. Presidente Piñera anuncia avances para la obtención de potenciales vacunas contra el COVID-19. Santiago: Ministerio de Salud; 2020. Available from: https://www.minsal.cl/presidente-pinera-anuncia-avances-para-la-obtencion-de-potenciales-vacunas-contra-el-covid-19/; 2020 [accessed 2021 May 23].
- 21.Ministerio de Ciencia, Tecnología e Innovación de Chile. Santiago: Ministerio de Ciencia, Tecnología e Innovación; 2020. Available from: https://www.minciencia.gob.cl/noticias/como-participar-en-uno-de-los-cuatro-ensayos-clinicos-para-una-vacuna-covid-19/#:~:text=C%C3%B3mo%20participar%20en%20uno%20de,la%20vacuna%20contra%20el%20Coronavirus; 2020 [accessed 2021 Jun 3].
- 22.Subsecretaría de Relaciones Exteriores Económicas de Chile. Vacunas COVID-19. Santiago: Subsecretaría de Relaciones Exteriores Económicas de Chile; 2021. Available from: https://www.subrei.gob.cl/landings/vacunas; 2021 [accessed 2021 Jun 1].
- 23.World Health Organization. COVAX: Working for global equitable access to COVID-19 vaccines; 2021. Available from: https://www.who.int/initiatives/act-accelerator/covax.
- 24.Horwitz L, Zissis C. Cronología: Rastreando el camino hacia la vacunación en América Latina. New York: Americas Society Council of the Americas; 2021. Available from: https://www.as-coa.org/articles/cronologia-rastreando-el-camino-hacia-la-vacunacion-en-america-latina#inicios-de-campaa; 2021 [accessed 2021 Jun 3].
- 25.Villalobos D.P. Out-of-pocket health expenditure differences in Chile: Insurance performance or selection? Health Policy. 2018;122(2):184–191. doi: 10.1016/j.healthpol.2017.11.007. [DOI] [PubMed] [Google Scholar]
- 26.González C, Castillo-Laborde C, Matute I (editors). Serie de salud poblacional: Estructura y funcionamiento del sistema de salud chileno. Santiago, Chile: CEPS, Fac. de Medicina. CAS-UDD; 2019.
- 27.Ministerio de Salud de Chile. Orientaciones para la implementación del modelo de atención integral de salud familiar y comunitaria. Santiago: Ministerio de Salud de Chile; 2012. Available from: https://www.minsal.cl/portal/url/item/e7b24eef3e5cb5d1e0400101650128e9.pdf; 2012 [accessed 2021 Jun 1].
- 28.Del Castillo B, Aravena C, Latorre R. Cómo se fraguó el engranaje logístico que permitió vacunar a cinco millones de personas en 41 días. La Tercera, 2021 Mar 19. Available from: https://www.latercera.com/la-tercera-pm/noticia/como-se-fraguo-el-engranaje-logistico-que-permitio-vacunar-a-cinco-millones-de-personas-en-41-dias/SNQWQVSIPRCHPGENMI4MMI5RJA/; 2021 [accessed 2021 Jun 4].
- 29.Biblioteca del Congreso Nacional de Chile. Ley 21.324. Posterga las próximas elecciones municipales, de gobernadores regionales y de convencionales constituyentes por motivo del COVID-19. Santiago: Biblioteca del Congreso Nacional de Chile; 2021. Available from: https://www.bcn.cl/leychile/navegar?idNorma=1157863; 2021 [accessed 2021 May 15].
- 30.González C. Programa Nacional de inmunización en Chile, pasado, presente y futuro. Revista Médica Clínica Las Condes. 2020;31:225–232. doi: 10.1016/j.rmclc.2020.04.005. [DOI] [Google Scholar]
- 31.Ministerio de Salud de Chile. Departamento de Inmunizaciones. Instructivo de preparación y administración de vacuna BNT162b2 del laboratorio Pfizer-BioNTech. Santiago: Ministerio de Salud de Chile; 2020. Available from: https://www.minsal.cl/wp-content/uploads/2021/03/Instructivo-vacuna-Pfizer-23022021.pdf; 2020 [accessed 2021 Jun 3].
- 32.Gobierno de Chile. Paso a Paso Nos cuidamos. Santiago: Gobierno de Chile; 2021. Available from: https://www.gob.cl/coronavirus/pasoapaso/; 2021 [accessed 2021 Jun 1].
- 33.Ministerio de Salud de Chile. Reporte COVID-19: Vacuna CoronaVac tiene un 90,3% de efectividad para prevenir el ingreso a UCI. Santiago: Ministerio de Salud de Chile. Available from: https://www.minsal.cl/reporte-covid-19-vacuna-coronavac-tiene-un-903-de-efectividad-para-prevenir-el-ingreso-a-uci/; 2021 [accessed 2021 Jun 2].
- 34.Cerda AA, García LY. Factors explaining the fear of being infected with COVID-19. Health Expect 2021;11:10.1111/hex.13274. doi: 10.1111/hex.13274. [DOI] [PMC free article] [PubMed]
- 35.Cerda A.A., García L.Y. Hesitation and Refusal Factors in Individuals' Decision-Making Processes Regarding a Coronavirus Disease 2019 Vaccination. Front Public Health. 2021;21(9) doi: 10.3389/fpubh.2021.626852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gobierno de Chile. Gobierno explica alcance del Pase de Movilidad. Santiago: Gobierno de Chile; 2021. Available from: https://www.minsal.cl/gobierno-explica-alcance-del-pase-de-movilidad/; 2021 [accessed 2021 Jun 3].
- 37.Chambers D.A., Glasgow R.E., Stange K.C. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci. 2013;8:117. doi: 10.1186/1748-5908-8-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Villalobos Dintrans P, Bossert TJ. Institutionalization and sustainability of donor-funded quality assurance initiatives: The case of Honduras. Research and Evaluation Report. Published by the USAID ASSIST Project. Chevy Chase, MD: University Research Co., LLC (URC); 2017.
- 39.Laval E. Anotaciones para la historia de la poliomielitis en Chile. Rev Chil Infect. 2007;24(3):247–250. doi: 10.4067/S0716-10182007000300017. [DOI] [PubMed] [Google Scholar]
- 40.Bastías M, Avendaño M, Muñoz F, Brstilo I, Álvarez A, Burgos P, et al. Campaña influenza 2020 en contexto de pandemia por SARS-CoV-2: una experiencia inédita de salud pública en Chile. Rev Chilena Infectol 2021;38(2):178–84. Available from: https://mail.revinf.cl/index.php/revinf/article/view/1048 [accessed 2021 Jun 3] [DOI] [PubMed]
- 41.García L.Y., Cerda A.A. Contingent assessment of the COVID-19 vaccine. Vaccine. 2020;38(34):5424–5429. doi: 10.1016/j.vaccine.2020.06.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hotez P. COVID vaccines: time to confront anti-vax aggression. Nature. 2021;592:661. doi: 10.1038/d41586-021-01084-x. [DOI] [PubMed] [Google Scholar]
- 43.Castillo C, Molina Milman H. El Sistema de Salud chileno: Análisis y perspectivas en el marco del estallido social de octubre de 2019. Revista Estado y Políticas Públicas. 2020;VIII(14):53–67. Available from: https://revistaeypp.flacso.org.ar/files/revistas/1590800088_53-67.pdf [accessed 2021 Jun 4].
- 44.Bossert T.J., Villalobos D.P. Health Reform in the Midst of a Social and Political Crisis in Chile, 2019–2020. Health Syst Reform. 2020;6(1) doi: 10.1080/23288604.2020.1789031. [DOI] [PubMed] [Google Scholar]
- 45.Gobierno de Chile. Presidente Piñera recibe vacuna contra el Covid-19: “Me siento orgulloso de la forma en que los chilenos hemos enfrentado con coraje, con disciplina y con resiliencia esta pandemia”. Santiago: Gobierno de Chile; 2021. Available from: https://www.gob.cl/noticias/presidente-pinera-recibe-vacuna-contra-el-covid-19-me-siento-orgulloso-de-la-forma-en-que-los-chilenos-hemos-enfrentado-con-coraje-con-disciplina-y-con-resiliencia-esta-pandemia/; 2021 [accessed 2021 Jun 3].
- 46.United Nations Office on Drugs and Crime. COVID-19 vaccines and corruption risks: preventing corruption in the manufacture, allocation and distribution of vaccines. Vienna: United Nations Office on Drugs and Crime. Available from: https://www.unodc.org/documents/corruption/COVID-19/Policy_paper_on_COVID-19_vaccines_and_corruption_risks.pdf; 2021 [accessed 2021 Jun 4].
- 47.Berti L. Vaccine line-cutting scandals challenge Latin American authorities. The Brazilian Report; 2021. Available from: https://brazilian.report/liveblog/coronavirus/2021/01/28/vaccine-line-cutting-scandals-challenge-latin-american-authorities/; 2021 [accessed 2021 Jun 4].
- 48.Rosen B., Waitzberg R., Israeli A. Israel's rapid rollout of vaccinations for COVID-19. Israel J Health Policy Res. 2021;10(6) doi: 10.1186/s13584-021-00440-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jara A, Undurraga EA, González C, Paredes F, Fontecilla T, Jara G, et al. Effectiveness of an Inactivated SARS-CoV-2 Vaccine in Chile. N Engl J Med 2021;7:NEJMoa2107715. doi: 10.1056/NEJMoa2107715. [DOI] [PMC free article] [PubMed]
- 50.Bollyky T.J., Bown C.P. The tragedy of vaccine nationalism. Only cooperation can end the pandemic. Foreign Affairs. 2020;99(5):96–108. [Google Scholar]