Abstract
Introduction
Patients on dialysis (HDPs) are a category at high risk from COVID-19 and thus a high-priority group for vaccination. COVID-19 vaccine hesitancy has been a concern since the availability of the first vaccine. The objective of this study was to determine hesitancy rates and factors associated with hesitancy toward COVID-19 vaccination in HDP.
Methods
HDP were surveyed with an ad hoc questionnaire in 4 large dialysis facilities in Europe: Le Mans and Paris, in France, and Cagliari and Pavia, in Italy. The questionnaire explored different domains associated with vaccine hesitancy, such as perception of disease severity, sources of information about the vaccine and the disease, and confidence in the health care system.
Results
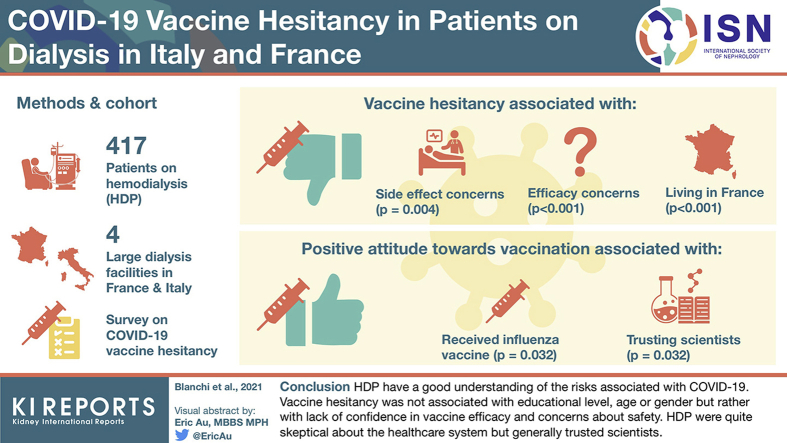
A total of 417 patients (average age 69 years, 60% men) agreed to answer the questionnaire. Hesitancy was associated with younger age (P = 0.003), lower perception of disease severity (P < 0.001) and vaccine efficacy (P < 0.001), and lower trust in vaccination (P < 0.001) and in the health care system and scientists (P < 0.001) in the univariate analysis. In the multivariate models, concerns about side effects (P = 0.004) and vaccine efficacy (P < 0.001) and living in France (P = 0.04) remained associated with higher vaccine hesitancy, whereas having received an influenza vaccine (P = 0.032) and trusting scientists (P = 0.032) were associated with a more positive attitude toward vaccination.
Conclusions
HDPs have a good understanding of the risks associated with COVID-19. Vaccine hesitancy was not associated with educational level, age, or gender but rather with lack of confidence in vaccine efficacy and concerns about safety. HDPs were quite skeptical about the health care system but generally trusted scientists.
Keywords: COVID-19, dialysis, hesitancy, SARS-CoV-2, vaccine
Graphical abstract
The COVID-19 epidemic had highlighted the fragility of some groups, in particular elderly and high-comorbidity individuals.1 The fragility of patients on dialysis, in combination with immunodepression, high morbidity, and older age, is well acknowledged. During the first year of the pandemic, their fragility, plus the need for regular visits to often crowded dialysis wards, resulted in a high rate of infection in patients on dialysis (a cumulative incidence of more than 14% in France and in Italy), with high mortality (between 15% and 20% of all cases).2, 3, 4
On April 8, 2021, the European Medicines Agency (EMA) granted conditional marketing authorization to 4 COVID-19 vaccines: 2 mRNA vaccines, Comirnaty (Pfizer/BioNTech) and COVID-19 Vaccine Moderna; and 2 nonreplicative viral vector vaccines, Vaxzevria (Astra Zeneca) and COVID-19 Vaccine Janssen. Starting in January 2021, patients on dialysis in France were identified by the Haute Autorité de Santé (HAS) as a priority population for vaccination against SARS-CoV-2. The HAS in France and Italy’s Ministero della Salute recommends prioritizing the vaccination for people at a very high risk of death, including dialysis and kidney transplant patients, regardless of their age.5,6 The use of mRNA vaccines is preferred for these patients. COVID-19 vaccines are free of charge in both countries.
However, the availability of vaccines and their acknowledged priority by the health authorities has not guaranteed vaccine acceptance.
In 2019, the WHO identified vaccine hesitancy as one of the 10 most serious threats to global health.7 Vaccine hesitancy is defined as “delay in acceptance or refusal of vaccines despite availability of vaccine services.” This phenomenon is of particular concern in Western Europe.
Several factors have been identified as being associated with COVID-19 vaccine acceptance in the general population: perception of the seriousness of the infection, perception of the risk of infection for oneself and one’s family, trust in the health care system, trust in the information given by doctors, trust in vaccine research, vaccine safety, vaccine effectiveness, having received a flu vaccine, male gender, white ethnicity, educational level, income level, urban versus rural living, and older age.8, 9, 10, 11, 12, 13, 14 People with comorbidities at risk of severe COVID-19 were found more likely to accept a COVID-19 vaccine.12,13 However, COVID-19 vaccine refusal remains high: in a recent US study, less than half the respondents between 18 and 64 years of age with underlying medical conditions replied that they would be likely to receive a COVID-19 vaccine.14
To date, only 1 study on COVID-19 vaccine hesitancy in patients on dialysis has been conducted. Done in the United States, its findings related hesitancy to younger age, female gender, and some ethnic groups.15 In-depth knowledge about the perceived barriers to vaccination is, however, crucial for acceptance, and because there is likely to be a significant degree of vaccine hesitancy in the dialysis population, everything possible should be done to obtain a high rate of vaccine coverage and protect this community.
Given that this is so, we designed this international multicenter study to assess COVID-19 vaccine hesitancy rates in patients on dialysis in 4 large dialysis facilities in Italy and France, with 1 center in each country in a rural area and 1 in a city, in order to identify factors associated with vaccine acceptance and hesitancy.
Methods
Settings and Patients
Le Mans
Centre Hospitalier du Mans (CHM), one of the 3 largest nonuniversity hospitals in France, has about 1700 beds, 500 of them in geriatric units and about 300 for different medical specialties (20 in nephrology). Le Mans has about 150,000 inhabitants, with approximately another 150,000 people living in its suburbs; CHM serves a population of about 800,000 inhabitants. Two dialysis facilities run by a nonprofit association (ECHO) are present in the area but nephrology beds are only available at CHM. Patients on peritoneal dialysis are managed conjunctly and were not included in the present survey. The dialysis ward has 25 beds. These are occupied by chronic patients on dialysis, patients with acute kidney injury (AKI), and patients from out-of-hospital centers who need to be hospitalized. The pool of patients on chronic hemodialysis ranges from 95 to 110, depending on the incidence of kidney transplantation, deaths, and transfers. In keeping with the indications of the French Society of Nephrology (Société Francophone de Néphrologie, Dialyse et Transplantation [SFNDT]), out-of-hospital dialysis is widely used and only cases posing particular clinical, attitudinal, or psychological problems are managed in the hospital. Hence, the population studied is a large sample of the most difficult patients treated in the area. The ratio between cases treated at CHM and those treated at the nonprofit association is around 1:6.
All physicians without contraindications and all the nurses working in dialysis (7 nephrologists and all the nurses) had received at least 1 dose of the vaccine at the time the survey began.
Cagliari
The study was conducted at Azienda Ospedaliera Brotzu, the largest hospital in Sardinia, Italy’s largest island. The hospital has about 677 beds (24 in the nephrology ward) and a transplant center, performing 35 to 40 kidney grafts per year. Cagliari has a population of about 150,000 inhabitants, which rises to 420,000 if those living in districts surrounding the city are counted, and the entire area Ospedale Brotzu serves has a population of about 800,000. Nephrology beds are available only in the hospital. A network of public out-of-hospital dialysis facilities provides treatment for patients with lower comorbidity, in keeping with Italian practice. The ratio between patients treated at Ospedale Brotzu and those receiving dialysis in out-of-hospital settings is around 1:6.
The dialysis unit has 26 beds dedicated to chronic patients and 8 for patients from other units with AKI or CKD, requiring hospitalization. The pool of patients on chronic treatment ranges from 90 to 100, depending on kidney transplantation, deaths, and transfers. Between 50 and 55 peritoneal patients on dialysis are also followed in the unit (monthly clinical visits in the center). All physicians and 87% of the nurses working in dialysis had received at least 1 dose of the vaccine when the survey began.
Pavia
The Maugeri Institute is the leading Italian group in rehabilitation medicine and in the treatment of chronic fragile patients, with 18 institutes located throughout the country. The Maugeri Institute in Pavia has about 306 beds, 100 of which are for acute clinical conditions in different medical specialties (at the time of the study, 12 in the nephrology unit). Pavia has about 73,000 inhabitants with approximately another 470,000 people living in outlying districts. The Institute serves a population of about 200,000. Three public hospitals with dialysis facilities are present in the area. The Maugeri Institute’s dialysis center is the largest in the district and nephrology beds are available there and at a nearby public hospital. Maugeri’s dialysis ward has 36 beds. They are occupied mainly by chronic patients on dialysis and patients from other centers who need rehabilitation treatment. The pool of patients on chronic treatment ranges from 120 to 140 depending on the incidence of kidney transplantation, deaths, and transfers. In keeping with the indications of the Italian Society of Nephrology, out-of-hospital dialysis is widely used, and only cases posing particular clinical, attitudinal, or psychological problems are managed in the hospital. Hence, the population studied is a large sample of the most difficult patients treated in the area. The ratio between cases treated at ICS Maugeri and those treated in the public dialysis unit is around 1:4.
All the physicians and 96% of the nurses working in dialysis (8 nephrologists, 34 nurses, and 4 helpers) had received 2 doses of Comirnaty vaccine, completing the vaccination program when the survey began.
Paris
Hôpital Tenon (Groupe Hospitalier Sorbonne Université), one of 9 nephrology university hospitals in Ile de France, has 525 beds, 60 in geriatric units, and about 300 for different medical specialties (at the time of the study, 33 in the nephrology unit, and 8 in the nephrology intensive care unit). Hôpital Tenon serves a population of about 400,000. The dialysis ward has 24 in-center beds and 5 training home-hemodialysis beds. These are occupied by chronic patients on dialysis, patients with AKI (not needing intensive care), as well as by patients from out-of-hospital centers who need to be hospitalized. The pool of patients on chronic in-center treatment ranges from 80 to 100, depending on the incidence of kidney transplantation, deaths, and transfers. The pool of patients on home hemodialysis ranges from 55 to 65. All physicians and 80% of the nurses working in dialysis (5 nephrologists and 45 nurses and helpers) had received at least 1 dose of the vaccine when the survey began.
Patient Participation
In the 4 centers in which the study was carried out, all patients on chronic dialysis without dementia and without language barriers that would impair basic comprehension of the questions were asked to participate. All patients were outpatients and none was hospitalized when the questionnaire was administered. Each center distributed the questionnaire according to their usual way of proposing questionnaires to patients. In detail, in Le Mans, the questionnaires were introduced by the caregivers and patients were free to complete them in the dialysis ward or at home, or, alternatively, to complete them with the help of a clinical research assistant, during, before or after their dialysis session. The last of these was the preferred modality: owing to advanced age and social isolation, many patients had become accustomed to completing questionnaires (mainly periodic assessments of their quality of life) in the unit with help from nurses or clinical research assistants. In Le Mans, the questionnaires—distributed about 3 weeks before the start of the vaccination campaign—were the first step in an educational program, whose target was to give patients information on COVID-19 vaccines.
In Cagliari and Pavia, the questionnaires were proposed by the senior physician and completed by patients, generally with some help from the residents. In both settings, the questionnaire was administered 4 to 6 weeks before vaccination had started. In Cagliari, patients had occasionally been asked in the past to participate in observational studies requiring the completion of a questionnaire, and in these cases the preferred way to answer was with assistance from caregivers. In Paris, the questionnaire was proposed just a few days before the start of the vaccination program in the dialysis ward. Patients there had never before been asked to participate in a survey. The questionnaires were introduced by residents or, in the case of home hemodialysis patients, by nurses. Although patients were given the choice of being given assistance to complete the questionnaire during their dialysis session, the majority preferred to answer at home, and return the completed survey afterward.
Clinical Data
In all 4 participating centers, patients’ general data are stored in dedicated databases. The following information was gathered for the current analysis: age, gender, country of birth, native language(s), educational level, working status, cause of end-stage kidney disease, Charlson comorbidity index (CCI), date of start of dialysis, dialysis vintage, previous transplantation, type of dialysis, and number of dialysis sessions per week (hemodialysis) or of daily exchanges in peritoneal dialysis.
Questionnaires
A team of infectiologists and nephrologists at CHM in Le Mans designed a questionnaire to collect information on whether patients on dialysis intended to be vaccinated and identify obstacles to vaccination (available in the Supplementary Material). The development of this questionnaire was based on a literature review of identified barriers to vaccination in general and to vaccination against SARS-CoV-2.8, 9, 10, 11, 12, 13, 14,16 Besides the respondent’s decision on whether or not he or she would receive the vaccine against COVID-19 (yes, no, or uncertain), the questions regarded the following topics: acknowledgement of the severity of COVID-19; amount of information received from the dialysis team and from the media; fear of side effects from the vaccine; confidence in the health care system; and confidence in the efficacy of the vaccine. Whether or not a respondent had previously received an anti-influenza vaccine was also recorded. Patients could add personal remarks at the end of the questionnaire (available as supplementary material). With the aim of avoiding intrusive questions, the questionnaire posed nonspecific questions regarding confidence in the system of care, dealing with the health care system and scientists in general terms, and avoided posing direct questions about confidence in the individual patient’s dialysis team.
The final version was agreed on by a focus group. A visual analog scale, which is a validated tool for medical questionnaires, was used for indicating answers to questions. The questionnaire was tested by the team of dialysis nurses at CHM, and the final version was submitted to the participating centers, to ensure that the questions were correctly phrased in both French and Italian. Because of the urgency of starting the vaccination campaign, formal validation from groups of nephrology patients was not sought. The survey was conducted between January (Le Mans and Paris) and March (Pavia and Cagliari) 2021, and the questionnaire was administered to patients in paper format to be filled during the dialysis session or at home, according to the patient’s convenience.
The visual analog questions were analyzed as actual number reported and summarized in 3 major scores: low, 0 to 3; medium, 4 to 6; and high, 7 to 10.17
The analysis of the actual prevalence of anti–COVID-19 vaccination (first dose considered) was performed considering only individuals who did not have contraindications and were alive, and were being treated in the same center as at the time of their first vaccine dose.
Statistical Analysis
Statistical analysis was performed with SPSS, version 14 (IBM Corp, Armonk, NY, USA), and JASP, version 0.11.1 (JASP Team, Amsterdam, the Netherlands). Descriptive analysis was conducted as appropriate; the Shapiro-Wilk test was used to verify the normality distribution of the data, and the Leven test was used to verify homoscedasticity. Depending on distribution of the data, the unpaired t test was used to compare 2 groups (eg, acceptance vs nonacceptance of vaccination), whereas the analysis of variance was used to compare ≥3 groups (eg, comparing the study centers). Otherwise, the Mann-Whitney test was applied to compare 2 groups, whereas the Kruskal-Wallis test was used for additional comparisons.
Categorial results were presented as size with a percentage and compared with the chi-squared test or the Fisher exact test for small subgroups.
Univariate logistic regressions were performed to test the outcome of refusal to be vaccinated against COVID-19 in comparison to baseline data and answers to questions on the questionnaire. receiver operating characteristic curves, together with the Youden index, were used to identify the best cutoff point for the continuous items associated with the outcome (age only).
The outcome “refusal to be vaccinated against COVID-19” was tested in a multivariate logistical regression analysis. The explanatory variables were chosen according to their clinical relevance or to the significance in the univariate analysis. At baseline, they were the following: age (dichotomized at Youden index, 64 years), gender (female or male), and country (Italy or France). As for the questionnaire entries, because of the high degree of correlation between questions inquiring about a specific aspect of vaccine hesitancy (fear of the disease or acknowledgement of its severity, confidence in the health care system and scientists, information received, concerns about safety, trust in the efficacy of the COVID-19 vaccine and vaccines in general, and previous vaccination against influenza), 1 sample question was chosen on the basis of its higher statistical hazard ratio or clinical relevance. The explanatory variables were dichotomized at both the lowest values (scores 0-3) and the highest ones (scores 7-10), thus building 2 separate models. A 2-tailed alpha risk at 5% was considered statistically significant.
Ethical Issues
The study was performed in compliance with the Declaration of Helsinki. Patient participation was voluntary. Permission for publication of the anonymous questionnaires and of anonymous general clinical data was obtained when a completed questionnaire was returned. The study was approved by the ethics committee at CHM in April 2021, and the ethics committees at the University of Cagliari and the Maugeri Institute were also notified that the study was being conducted in April 2021.
Results
Baseline Data
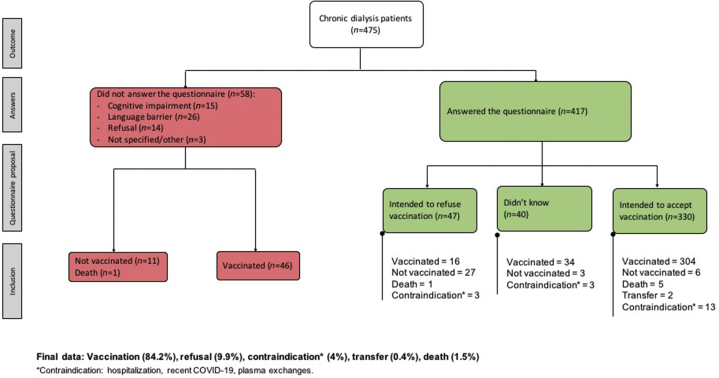
The baseline data of the patients who answered the questionnaires are reported in Table 1, and the flow chart of the study is presented in Figure 1, whereas data on the patients who did not answer the questionnaires and their reasons for not participating are reported in Supplementary Table S1. Supplementary Figure S1 shows the study flow chart of each participating center.
Table 1.
Baseline data of the study population: only patients who answered the questionnaire are included
| Centers |
P value | |||||
|---|---|---|---|---|---|---|
| All (N = 417) | Le Mans (n = 128) | Cagliari (n = 136) | Paris (n = 44) | Pavia (n = 109) | ||
| % of questionnaires retrieved | 87.8 | 93.4 | 96.4 | 54.3 | 94.0 | |
| Age, median (min-max) | 69 (16–94) | 70 (16–94) | 67 (22–93) | 52 (27–86) | 73 (31–93) | <0.001 |
| Gender (woman), % | 39.8 | 43.0 | 40.4 | 36.4 | 36.7 | 0.750 |
| Charlson Comorbidity Index, median (min-max) | 7 (2–16) | 8 (2–16) | 7 (2–16) | 6 (2–12) | 6 (2–13) | 0.007 |
| Patients born in a country other than the one of residence, n (%) | 51 (12.2) | 26 (20.3) | 2 (1.5) | 18 (40.9) | 5 (4.6) | <0.001 |
| Education level, n (%) | <0.001 | |||||
| Illiterate | 7 (1.7) | 3 (2.3) | 3 (2.2) | 1 (2.3) | 0 | |
| Primary to middle school | 238 (57.0) | 75 (58.6) | 67 (49.3) | 6 (13.6) | 90 (82.6) | |
| Secondary school | 104 (24.9) | 33 (25.8) | 49 (36.0) | 15 (34.1) | 7 (6.4) | |
| University | 68 (16.3) | 17 (13.3) | 17 (12.5) | 22 (50.0) | 2 (11.0) | |
| Local language understanding, n (%) | 0.666 | |||||
| 3: Some difficulty | 2 (0.5) | 1 (0.8) | 0 | 0 | 1 (0.9) | |
| 4: Almost complete understanding | 7 (1.7) | 3 (2.3) | 1 (0.7) | 0 | 3 (2.8) | |
| 5: Near–native speaker competence/bilingual | 408 (97.8) | 124 (96.9) | 135 (99.3) | 44 (100) | 105 (96.3) | |
| Activity, n (%) | <0.001 | |||||
| Student | 6 (1.5) | 2 (1.6) | 4 (2.9) | 0 | 0 | |
| Unemployed | 76 (18.2) | 30 (23.4) | 24 (17.7) | 12 (27.3) | 10 (9.2) | |
| Working full or part time | 66 (15.8) | 3 (2.3) | 29 (21.3) | 18 (40.9) | 16 (14.7) | |
| Retired | 269 (64.5) | 93 (72.7) | 79 (58.1) | 14 (31.8) | 83 (76.1) | |
| Primary kidney disease, n (%) | 0.025 | |||||
| Glomerulonephritis / systemic disease | 80 (19.2) | 22 (17.2) | 29 (21.3) | 11 (25.0) | 18 (16.5) | |
| Nephroangiosclerosis/diabetes | 91 (21.8) | 42 (32.8) | 22 (16.2) | 7 (15.9) | 20 (18.4) | |
| Polycystic kidney disease | 38 (9.1) | 9 (7.0) | 9 (6.6) | 4 (9.1) | 16 (14.7) | |
| Other | 208 (49.9) | 55 (43.0) | 76 (55.9) | 22 (50.0) | 55 (50.5) | |
| Renal replacement therapy vintage, yr, median (min-max) | 3 (0–47) | 2 (0–47) | 3 (0–41) | 5 (0–30) | 3 (0–33) | <0.001 |
| Type of dialysis, n (%) | <0.001 | |||||
| Peritoneal dialysis | 56 (13.4) | — | 56 (41.2) | — | — | |
| Hemodialysis | 337 (80.8) | 128 (100) | 80 (58.8) | 20 (45.5) | 109 (100) | |
| Home hemodialysis | 24 (5.8) | — | — | 24 (54.5) | 0 | |
| Previous kidney transplant, n (%) | 48 (11.5) | 9 (7.0) | 24 (17.7) | 5 (11.4) | 10 (9.2) | 0.043 |
| Vaccine hesitancy (refusal and undecided), n (%) | 79 (18.9) | 22 (17.2) | 26 (19.1) | 13 (29.6) | 18 (16.5) | 0.273 |
| Vaccine refusal (refusal only), n (%) | 47 (11.3) | 21 (16.4) | 10 (7.4) | 11 (25.0) | 5 (4.6) | <0.001 |
P values in bold indicate significance.
Figure 1.
Flow chart of the study population. Overall data.
In the context of a high response to the questionnaires (overall ≥85%), some baseline differences emerged: the highest retrieval of questionnaires was in Italy (Cagliari and Pavia), and the lowest in Paris, a center that differs in significant respects from the others in the study. The median age is lower, to some extent reflecting the high number of patients on home hemodialysis. Educational level is also higher, as is the prevalence of patients who were born in a country other than the one of residence (40%, double the percentage in Le Mans, while Pavia and Cagliari had significantly lower percentages of foreign-born patients). In keeping with differences in age, the prevalence of patients working was higher and the CCI was lower in Paris compared with the other settings of study.
Reasons for declining to answer the survey were also different: language barriers and dementia were the main ones in Italy, whereas in Paris refusal was more often due to lack of interest and/or lack of confidence in why the survey was being conducted (Supplementary Table 1). The situation in Le Mans was intermediate. Language barriers and mental problems accounted for some patients’ unwillingness to respond, but for most of those who refused, this was the result of personal or family convictions.
Quantitative Answers to the Questionnaires and Relationship With the Acceptance of Anti-influenza Vaccine
Table 2 summarizes the median scores recorded in each center. The distribution of the answers in the 3 main scores (low-medium-high) is reported in Supplementary Table 2. Supplementary Figure 2 shows the details of each answer to the questionnaire.
Table 2.
Main scores recorded in the answers to the questionnaire and differences across the participating centers
| Questions | All | Centers |
P value | |||
|---|---|---|---|---|---|---|
| Le Mans | Cagliari | Paris | Pavia | |||
| n | 417 | 128 | 136 | 44 | 109 | |
| Do you think you are a person at risk for COVID-19? (median, IQR) | 7 (4) | 7 (3) | 7 (5) | 6 (5.25) | 7 (6) | 0.856 |
| Do you think that COVID-19 is a serious disease? (median, IQR) | 9 (3) | 9 (3) | 9 (3) | 10 (2) | 9 (3) | 0.376 |
| Do you think you get enough information about COVID-19 from the media? (median, IQR) | 7 (4) | 8 (5) | 7 (4) | 9 (3) | 7 (4) | 0.001 |
| Do you feel you have enough information about COVID-19 from the dialysis team? (median, IQR) | 7 (4) | 5 (6) | 8 (4) | 8 (5) | 7 (4) | <0.001 |
| Do you think you have enough information about COVID-19 vaccines from the media? (median, IQR) | 6 (4) | 6 (5) | 6 (4) | 7 (4.5) | 6 (4) | 0.130 |
| Do you feel you have enough information about COVID-19 vaccines from the dialysis team? (median, IQR) | 6 (5) | 3 (4) | 7 (3) | 8 (5) | 7 (5) | <0.001 |
| Do you think it is complicated for you to get vaccinated against COVID-19? (median, IQR) | 2 (6) | 2 (5) | 2 (4) | 2 (6.75) | 2 (5) | 0.124 |
| Do you think that COVID-19 vaccine is effective? (median, IQR) | 7 (4) | 5 (3) | 8 (3) | 7 (4) | 8 (2) | <0.001 |
| Do you think that COVID-19 vaccines can cause serious side effects? (median, IQR) | 5 (5) | 5 (3.75) | 5 (4.5) | 5 (5.5) | 4 (4) | 0.102 |
| Do you have any concerns about the safety of COVID-19 vaccines? (median, IQR) | 3 (6) | 5 (7) | 2.5 (6) | 4.5 (7.75) | 3 (7) | 0.713 |
| In general, are you in favor of vaccination? (median, IQR) | 10 (2) | 10 (2.25) | 10 (2) | 9 (4.75) | 10 (2) | 0.294 |
| In general, do you trust the authorities to manage the health crisis? (median, IQR) | 5 (5) | 5 (5) | 5 (4) | 5 (5.5) | 5 (5) | 0.817 |
| In general, do you trust scientists to manage the health crisis? (median, IQR) | 7 (3.25) | 8 (4) | 7 (2) | 6 (4) | 7 (4) | 0.661 |
| Vaccine hesitancy (refusal & undecided), n (%) | 79 (18.9) | 22 (17.2) | 26 (19.1) | 13 (29.6) | 18 (16.5) | 0.273 |
| Vaccine hesitancy (refusal only), n (%) | 47 (11.3) | 21 (16.4) | 10 (7.4) | 11 (25.0) | 5 (4.6) | <0.001 |
| Did you get your seasonal flu shot this year?, n (%) | 0.083 | |||||
| Yes | 261 (62.9) | 90 (70.3) | 81 (59.6) | 25 (59.5) | 65 (59.6) | |
| No | 148 (35.7) | 34 (26.6) | 55 (40.4) | 17 (40.5) | 42 (38.5) | |
| I don’t know | 6 (1.5) | 4 (3.1) | 0 | 0 | 2 (1.8) | |
IQR, interquartile range.
In the context of a perception of a high risk of being infected by SARS-CoV-2, the appreciation of the severity of the disease was high (median score 9), without differences in the 4 settings. Patients reported they had been extensively informed by the media about the disease (median score 7) but had received less information about the vaccine (median score 6). Delivery of information from the dialysis team was reported differently, with the lowest score in Le Mans, where the administration of the questionnaire preceded the delivery of capillary oral and written information on vaccination (including timing and side effects). The highest scores were recorded in Paris, where the questionnaires were proposed almost at the same time as the vaccination campaign began. Overall, patients stated they were favorable to vaccination, as a general concept (median score 10), but their confidence in the efficacy of the COVID-19 vaccine was a good deal lower (median score 7).
Confidence in the way the health care system is managing the crisis was not high in all centers (median score 5), whereas patients had more trust in scientists (median score 7), with the highest score in Le Mans (8) and the lowest in Paris (6). Although the risk of side effects from the vaccine appears to be well acknowledged (median score 5), this did not seem to frighten patients on dialysis, who were not particularly worried about their personal well-being (median score 3).
In the 2 French centers, the answers to questions regarding the choice of COVID-19 vaccine were straightforward, and only a minority of the patients stated they were uncertain, whereas in Italy the number of uncertain individuals was higher than the number of refusals. Interestingly, the prevalence of vaccine hesitancy for COVID-19 was significantly lower than those who indicated they would refuse to have an influenza vaccine (18.9% vs. 35.7% P < 0.001).
Relationship Between Vaccine Hesitancy, Baseline Data, and Response to the Questionnaire: Univariate Analysis
Table 3 reports the results of the logistic regression correlating refusal to be vaccinated, as stated on the questionnaire, with clinical and demographic features and with answers to other questions, dichotomized as low versus all other scores.
Table 3.
Univariate logistic regression correlating COVID-19 vaccine hesitancy (refusal in the questionnaire) with demographic data and other answers
| Univariate analysis | Odds ratio | 95% CI |
P value | |
|---|---|---|---|---|
| Lower limit | Higher limit | |||
| Country (France vs. Italy) | 3.505 | 1.833 | 6.702 | <0.001 |
| Area (industrial vs. rural) | 0.878 | 0.463 | 1.663 | 0.689 |
| Age (yr) | 0.973 | 0.955 | 0.991 | 0.003 |
| Age (≥64 yr old)a | 0.248 | 0.129 | 0.475 | <0.001 |
| Charlson Comorbidity Index (a.u.) | 0.907 | 0.814 | 1.010 | 0.076 |
| Charlson Comorbidity Index (≥7) | 0.730 | 0.398 | 1.341 | 0.310 |
| Gender (female vs. male) | 1.676 | 0.911 | 3.081 | 0.097 |
| Dialysis vintage (yr) | 1.020 | 0.985 | 1.056 | 0.257 |
| No previous history of kidney transplantation | 0.591 | 0.258 | 1.353 | 0.213 |
| Glomerulonephritis / systemic disease | 1.333 | 0.646 | 2.750 | 0.437 |
| Being born in a country other than the one of residence | 1.561 | 0.684 | 3.558 | 0.291 |
| Educational level | ||||
| University vs. fewer years of schooling | 1.755 | 0.905 | 3.403 | 0.096 |
| University and college to high school vs. lower degrees | 1.724 | 0.937 | 3.171 | 0.080 |
| Covid-19 vaccine acceptance on questionnaire | ||||
| Do you think you are a person at risk for COVID-19? (low vs. medium and high) | 1.922 | 0.965 | 3.695 | 0.055 |
| Do you think that COVID-19 is a serious disease? (low vs. medium and high) | 5.008 | 2.010 | 11.822 | <0.001 |
| Do you think you get enough information about COVID-19 from the media? (low vs. medium and high) | 2.053 | 0.967 | 4.119 | 0.050 |
| Do you feel you have enough information about COVID-19 from the dialysis team? (low vs. medium and high) | 1.546 | 0.780 | 2.954 | 0.197 |
| Do you think you have enough information about COVID-19 vaccines from the media? (low vs. medium and high) | 2.954 | 1.547 | 5.590 | <0.001 |
| Do you feel you have enough information about COVID-19 vaccines from the dialysis team? (low vs. medium and high) | 1.793 | 0.948 | 3.356 | 0.069 |
| Do you think that COVID-19 vaccine is effective? (low vs. medium and high) | 25.650 | 11.980 | 57.050 | <0.001 |
| In general, are you in favor of vaccination? (low vs. medium and high) | 35.405 | 15.780 | 84.462 | <0.001 |
| In general, do you trust the authorities to manage the health crisis? (low vs. medium and high) | 4.667 | 2.486 | 8.968 | <0.001 |
| Do you think it is complicated for you to get vaccinated against COVID-19? (low vs. medium and high) | 0.185 | 0.086 | 0.370 | <0.001 |
| Do you think that COVID-19 vaccines can cause serious side effects? (low vs. medium and high) | 0.163 | 0.048 | 0.416 | <0.001 |
| Do you have any concerns about the safety of COVID-19 vaccines? (low vs. medium and high) | 0.098 | 0.033 | 0.231 | <0.001 |
| In general, do you trust scientists to manage the health crisis? (low vs. medium and high) | 7.118 | 3.507 | 14.345 | <0.001 |
| Did you get your seasonal flu shot this year? (refusal) | 4.451 | 2.351 | 8.776 | <0.001 |
CI, confidence interval.
Statistically significant data are in bold.
Defined using the Youden index calculated by means of the receiver operating characteristic curve.
The analysis confirms the importance of context: the odds ratio (OR) for respondents living in France refusing vaccination against SARS-COV-19 is 3.505; being aged ≥64 years is associated with lower vaccine hesitancy (OR: 0.248).
Conversely, it was found that gender, renal replacement therapy vintage, having been exposed to immunosuppressive treatments (because of glomerulonephritis or transplantation), educational level, or being born in a country other than the one currently residing in had no effect on answers to the questionnaire.
Considering that the information delivered from the media was not sufficient was associated with a higher probability of refusing vaccination, differently from the amount of information delivered by the dialysis team.
Confidence in getting the vaccine easily and not being worried about side effects were associated with a lower probability of vaccine refusal. On the contrary, low confidence in vaccination (OR: 35.405) and not having been vaccinated against influenza (OR: 25.650) had the highest impact on vaccine refusal. Lack of confidence in scientists and in the health care system was significantly associated with vaccine refusal.
The same items were confirmed as significantly associated with vaccine refusal considering the answers on the 1 to 10 scale and dichotomizing them as high scores (7–10) versus lower ones (0–6) (Supplementary Tables S3 and S4).
Narrative Insights From the Questionnaire
Supplementary Table S5 reports some of the additional comments patients wrote on the questionnaires.
Some points deserve to be underlined: the importance of the family in patients’ decisions, which holds true for both large extended families (gypsies) and smaller nuclear families (parents, children, and grandchildren); the idea that the attention the disease has received is “much ado about nothing”; the fear that the vaccine is not safe and that, therefore, for the moment it may be wise to wait. A lack of confidence emerges from some answers, whereas the importance of the dialysis team is also clearly shown.
Relationship Between Vaccine Hesitancy, Baseline Data, and Response to the Questionnaire: Multivariate Analyses
In the multivariate analysis (Tables 4 and 5), vaccine hesitancy was strongly correlated with country of study, whereas age had little statistical significance; confidence in the efficacy of the vaccine and having had an anti-influenza vaccine were strongly associated with vaccine hesitancy. Concerns about safety was an important modulator of choice. High confidence in scientists maintained its statistical significance in the analysis, whereas the acknowledgment of the potential severity of the disease was not associated with vaccine hesitancy in either models. The residual analysis demonstrated the goodness of fit of the statistical models used (Supplementary Figures S3 and S4).
Table 4.
Multivariate analysis with vaccine refusal as outcome and explanatory variables dichotomized (lower scores vs. others)
| Odds ratio | 95% CI |
P value | VIF | |||
|---|---|---|---|---|---|---|
| Lower limit | Upper limit | |||||
| Do you have any concerns about the safety of COVID-19 vaccines? (low vs. medium and high) | 0.211 | 0.065 | 0.571 |
 Lower vaccine hesitancy Higher vaccine hesitancy |
0.004 | 1.059 |
| Age (≥64 yr old) | 0.646 | 0.271 | 1.537 | 0.319 | 1.120 | |
| Do you think that COVID-19 is a serious disease? (low vs. medium and high) | 2.181 | 0.459 | 9.562 | 0.313 | 1.066 | |
| In general, do you trust scientists to manage the health crisis? (low vs. medium and high) | 2.419 | 0.827 | 6.669 | 0.095 | 1.177 | |
| Country (France vs. Italy) | 2.461 | 1.050 | 5.929 | 0.040 | 1.087 | |
| Did you get your seasonal flu shot this year? (refusal) | 2.624 | 1.095 | 6.475 | 0.032 | 1.162 | |
| Do you think that the COVID-19 vaccine is effective? (low vs. medium and high) | 10.253 | 3.850 | 28.293 | <0.001 | 1.236 | |
CI, confidence interval; VIF, variance inflation factor.
Akaike information criterion: 183.41
See Supplementary Figure S2 for residuals of the model.
Statistically significant data are in bold.
Table 5.
Multivariate analysis with vaccine refusal as outcome and explanatory variables dichotomized (high scores vs. others)
| Odds ratio | 95% CI |
P value | VIF | |||
|---|---|---|---|---|---|---|
| Lower limit | Upper limit | |||||
| Do you think that the COVID-19 vaccine is effective? (high vs. medium and low) | 0.315 | 0.104 | 0.861 |
 Lower vaccine hesitancy Higher vaccine hesitancy |
0.030 | 1.216 |
| In general, do you trust scientists to manage the health crisis? (high vs. medium and low) | 0.387 | 0.159 | 0.907 | 0.032 | 1.092 | |
| Age (≥64 yr old) | 0.529 | 0.227 | 1.218 | 0.134 | 1.128 | |
| Do you think that COVID-19 is a serious disease? (high vs. medium and low) | 0.579 | 0.242 | 1.409 | 0.221 | 1.038 | |
| Did you get your seasonal flu shot this year? (refusal) | 1.884 | 0.811 | 4.420 | 0.140 | 1.143 | |
| Country (France vs. Italy) | 2.290 | 1.014 | 5.309 | 0.048 | 1.090 | |
| Do you have any concerns about the safety of COVID-19 vaccines? (high vs. medium and high) | 8.192 | 3.402 | 22.053 | <0.001 | 1.064 | |
CI, confidence interval; VIF, variance inflation factor.
Akaike information criterion: 185.74.
See supplementary figure 3 for residuals of the model.
Statistically significant data are in bold.
Relationship Between Vaccine Hesitancy and Actual Administration of the Vaccine
The flowchart of the study population presented in Figure 1, and in Supplementary Figure S1 for the individual centers, shows the relationship between the choices indicated in the questionnaires and actual administration of the vaccine, both for patients who answered and those who did not answer the questionnaires. Out of 417 patients who answered the survey, 47 said they did not want to be vaccinated but, eventually, 16 of them got vaccinated (Figure 1).
Overall, the responses given in the questionnaire were strongly predictive of the patient’s choice. Lack of response to the questionnaire was not associated with vaccine hesitancy in the cases in which the decision rested with the family or tutors (cognitive impairment), or was the result of language barriers, whereas declining to fill in the questionnaire was associated with vaccine hesitancy.
Discussion
This study, analyzing the answers to a questionnaire designed to assess vaccine hesitancy in more than 400 patients on dialysis, found a relatively low overall prevalence of vaccine hesitancy in the dialysis population, defined as present refusal to undergo COVID-19 vaccination in individuals without contraindications. Only 11.3% of the patients who answered the dedicated questionnaire stated they did not intend to have the COVID-19 vaccine. There were, however, significant differences, as the percentage ranged from 4.6% (Pavia, industrial setting, northern Italy) to 25% in Paris, France (Table 1). The actual figures (vaccines administered) were similar (Figure 1, Supplementary Figure S1), thus also indirectly validating this type of questionnaire for assessing patients’ opinions. However, a questionnaire such as ours probably underestimates vaccine hesitancy, as those who refused to answer it were more likely not to have the COVID-19 vaccine (Figure 1). These differences are consistent with previous studies of the general population that found high vaccine hesitancy in France.8,9
These differences were at least partly expected on account of the different degree of penetrance of COVID-19 vaccine among health care workers, which was reported as significantly lower in France, in particular in Paris,18, 19, 20 than in Italy. In fact, in 2016, France and Italy were the 2 countries with the highest rates of vaccine safety skepticism.21 A European study conducted in April 2020 in 7 countries showed that France had the largest proportion of the population opposed to a COVID-19 vaccine (10%) and the largest group of people who had not decided whether or not they would be vaccinated (28%). Denmark and the United Kingdom were the countries with the largest proportion of respondents who stated they would be willing to be vaccinated (80%). In Italy, this rate was 74%.8 Similarly, in an international study conducted in June 2020 in 19 countries, when asked “If a COVID-19 vaccine is proven safe and effective and is available, I will take it,” only 58.89% of participants in France answered that they would, versus 70.79% in Italy.9 It is noteworthy, however, that the percentage of COVID-19 vaccination in the 4 study centers was higher than the national average for health care workers (100% of the doctors and 100%, 80%, 87%, and 96% of the nurses in Le Mans, Paris, Cagliari, and Pavia, respectively). Because of a high incidence of SARS CoV2 infection in patients on dialysis,2,4 dialysis teams often had to care for COVID-19 patients, which may explain this difference.22
Differently from what has been described in the overall population, gender and educational level did not correlate with vaccine refusal; older age was associated with lower vaccine refusal, but the difference emerged only in the univariate analysis (Table 3). Likewise, in the subset of the population that answered the questionnaires (overall more than 85%), being born in a country other than the one of residence (chosen as a marker of belonging to an ethnic minority) did not affect vaccine acceptance (Table 3), contrary to what has been reported for the general population.23, 24, 25, 26, 27, 28 Furthermore, in a context of low vaccine hesitancy, answers were not modulated by dialysis vintage, or by exposure to immunosuppressive drugs (because of previous transplantation or glomerular and systemic kidney disease).
Patients were well aware of the risks and severity of COVID-19. The question “Do you think that COVID-19 is a serious disease?” recoded a median score of 9, without differences between centers (Table 2). This perception of the seriousness of the infection was much higher than that of the general population and may explain the low rate of vaccine refusal, as it is a factor associated with better acceptability of vaccination.10,12,23 Furthermore, patients were not worried about vaccine availability (median score 2), probably because in all centers the questionnaire was linked to the vaccination campaign, and, in the context of generic confidence in vaccines (median score 10), the majority of the patients were not extremely concerned about safety (median score 3), although they were, in general, aware of the risks of side effects (median score 5) (Table 3).
Patients on dialysis are keen observers; their evaluation of the degree of information delivered by the health care team corresponded closely with what was actually delivered in the different settings (no systematic information in Le Mans, where the questionnaire was intended to be the first step in the vaccine campaign; in-depth information in Paris, where the vaccine had been available earlier; and an intermediate level in the 2 Italian centers). The level of information did not, however, uniformly correlate with vaccine hesitancy (Tables 4 and 5). A recent study in England showed that information about COVID-19 vaccines did not influence vaccination intentions.29
Concordance between the answers on the influenza vaccine and on the COVID-19 vaccine raises questions that merit further discussion: although, as expected, not having received the influenza vaccine was associated with a significantly higher probability of refusing the COVID-19 vaccine (OR of about 7 for refusing COVID-19 vaccine in the univariate analysis, and of 2–3 in the 2 multiple regression models; Table 3, Table 4, Table 5), the prevalence of influenza refusal was almost double compared with COVID-19 (Table 1). This can be explained by a lower perceived severity of seasonal influenza than COVID-19 by patients on dialysis.30
Confidence in the health care system was relatively low in all settings (median score 5; Table 2). However, confidence in scientists (a generic term chosen to avoid being intrusive and clearly alluding to the health care team) was higher (median score 7; Table 2) and both were correlated with vaccine hesitancy in the univariate analysis, whereas in the multivariate analysis only high confidence in the scientific community was associated with a low probability of refusing the COVID-19 vaccine.
We consider that this is one of the most interesting findings of our study, suggesting that confidence in the scientific community is more important than having been given information by the media or by a health care team. In this regard, although we agree that from an ethical point of view, information campaigns are important for supporting choices, we have come to think that they may be less relevant than confidence in the role of science, a term that was chosen to indirectly allude to the medical community. Lack of confidence in the health care system was in fact identified as a major determinant of vaccine hesitancy in the case of COVID-19 and of other vaccines,10,19,26, 27, 28 and the low vaccine acceptance of health care workers in some “difficult” settings may also be evidence of this attitude.
In fact, vaccine hesitancy was not associated with fear of COVID-19, nor with generic high hesitancy about vaccines; patients on dialysis, probably like most of our physicians, focused on the efficacy and security of this specific vaccine, suggesting that educational campaigns should be specifically addressed to these 2 points.
Interestingly, one-third of patients who expressed their refusal to vaccination eventually got vaccinated, suggesting that the personal belief expressed at the beginning was not always consistent with the final decision. However, the limited number of patients who changed their decision after completing the questionnaire is too small to draw any conclusion.
The findings of a similar study, recently conducted in 150 dialysis centers with 1515 patients in the United States, were significantly different from ours.15 Younger patients, blacks, Native Americans, Pacific Islanders, and women were more likely to state that they would not be vaccinated. However, the authors did not correlate vaccine hesitancy with the actual percentage of patients in their sample who were subsequently vaccinated. Moreover, only 14% of the eligible participants answered the survey in the United States, whereas our sample accounts for almost 88% of the entire dialysis population in the 4 participating centers.
Our study needs to be contextualized. It was performed before the controversy over the side effects of COVID-19 vaccines arose. Therefore, the responses might have been different had it been done later. Furthermore, it has several limitations: like all cross-sectional studies, it only makes it possible to establish associations, and cause-effect relationships are only hypothetical. Although it enrolled more than 400 patients on dialysis, the number may be too low to highlight other important differences relevant to the rollout of a vaccine campaign for patients on dialysis. Furthermore, many of the answers are mutually related, and therefore a mathematical model may fail to identify the leading ones and only suggest which associations may be of interest for understanding the phenomenon of vaccine hesitancy in dialysis and for suggesting targeted interventions. In addition, questionnaires were administered at different times in the 4 dialysis facilities, between January and March, and the perception of vaccine efficacy and safety may change over time as new information became available. Although questions referred to health care workers and the health care system in general, the help of caregivers could have had an impact on patients’ answers. Finally, no explanation on the reason for vaccine hesitancy was available in cases that did not fill the questionnaire. Within these limits, our study, the first one of its type performed in Europe, showed that our dialysis population is an interesting microcosm whose answers can help us improve care and mutual confidence in the long term, a major potential reinvestment of this difficult experience.
In conclusion, patients on dialysis have a keen understanding of COVID-19 risks. In the context of low, but variable, vaccine hesitancy, this attitude is not linked to educational level, age, or gender. Vaccine hesitancy is closely associated with lack of confidence in vaccine efficacy and concerns about safety. Patients on dialysis are quite skeptical about the health care system but generally trust scientists. The high acceptance of COVID-19 vaccination may be linked to this trust, and this pattern should prompt us to reflect on the fact that building a system of mutual trust is more important than giving detailed information when advising patients on important decisions, such as whether or not to be vaccinated against COVID-19.
Disclosure
All the authors declared no competing interests.
Footnotes
Study Questionnaire.
Table S1. General data on patients who did not answer the questionnaires and main reasons for declining/not being asked to participate in the study.
Table S2. Distribution of the quantitative answers categorized into the three main scores (low: 0–3; medium 4–6; high 7–10).
Table S3. Univariate logistic regression correlating COVID-19 vaccine hesitancy (refusal in the questionnaire).
Table S4. Univariate logistic regression correlating COVID-19 vaccine hesitancy (refusal in the questionnaire) dichotomized as high (7–10) versus low scores (0–6).
Table S5. Some thematic comments on the questionnaires.
Figure S1. Flow chart of the study population: single center data.
Figure S2. Detail of responses given in the questionnaire.
Figure S3. Residuals of the multivariate analysis with vaccine refusal as outcome. Explanatory variables dichotomized (low scores vs. others).
Figure S4. Residuals of the multivariate analysis with vaccine refusal as outcome. Explanatory variables dichotomized (higher scores vs. others).
Supplementary Material
Study Questionnaire.
Table S1. General data on patients who did not answer the questionnaires and main reasons for declining/not being asked to participate in the study.
Table S2. Distribution of the quantitative answers categorized into the three main scores (low: 0–3; medium 4–6; high 7–10).
Table S3. Univariate logistic regression correlating COVID-19 vaccine hesitancy (refusal in the questionnaire).
Table S4. Univariate logistic regression correlating COVID-19 vaccine hesitancy (refusal in the questionnaire) dichotomized as high (7–10) versus low scores (0–6).
Table S5. Some thematic comments on the questionnaires.
Figure S1. Flow chart of the study population: single center data.
Figure S2. Detail of responses given in the questionnaire.
Figure S3. Residuals of the multivariate analysis with vaccine refusal as outcome. Explanatory variables dichotomized (low scores vs. others).
Figure S4. Residuals of the multivariate analysis with vaccine refusal as outcome. Explanatory variables dichotomized (higher scores vs. others).
References
- 1.Grasselli G., Greco M., Zanella A., et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern Med. 2020;180:1345–1355. doi: 10.1001/jamainternmed.2020.3539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Situation de l’épidémie de Covid-19 chez les patients dialysés et greffés rénaux en France au 12 avril 2021. Bulletin numéro 45 du registre REIN [COVID-19 epidemic situation in dialysis and kidney transplant patients in France as of April 12, 2021] Agence de la biomédecine; 2021. [Google Scholar]
- 3.Rombola G., Heidempergher M., Pedrini L., et al. Practical indications for the prevention and management of SARS-CoV-2 in ambulatory dialysis patients: lessons from the first phase of the epidemics in Lombardy. J Nephrol. 2020;33:193–196. doi: 10.1007/s40620-020-00727-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nordio M., Reboldi G., Di Napoli A., et al. Risk factors and action thresholds for the novel coronavirus pandemic. Insights from the Italian Society of Nephrology COVID-19 Survey. J Nephrol. 2021;34:325–335. doi: 10.1007/s40620-020-00946-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Piccoli G.B., Leone F., Attini R., et al. Association of low-protein supplemented diets with fetal growth in pregnant women with CKD. Clin J Am Soc Nephrol. 2014;9:864–873. doi: 10.2215/CJN.06690613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garofalo C., Borrelli S., De Stefano T., et al. Incremental dialysis in ESRD: systematic review and meta-analysis. J Nephrol. 2019;32:823–836. doi: 10.1007/s40620-018-00577-9. [DOI] [PubMed] [Google Scholar]
- 7.Longhitano E., Trabace T., Fois A., et al. Ready to change: attitudes of an elderly CKD stage 3-5 population towards testing protein-free food. Nutrients. 2020;12:3519. doi: 10.3390/nu12113519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neumann-Bohme S., Varghese N.E., Sabat I., et al. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020;21:977–982. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lazarus J.V., Ratzan S.C., Palayew A., et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27:225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lin C., Tu P., Beitsch L.M. Confidence and receptivity for COVID-19 vaccines: a rapid systematic review. Vaccines (Basel) 2020;9:16. doi: 10.3390/vaccines9010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Detoc M., Bruel S., Frappe P., et al. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38:7002–7006. doi: 10.1016/j.vaccine.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwarzinger M., Watson V., Arwidson P., et al. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021;6:e210–e221. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams L., Flowers P., McLeod J., et al. Social patterning and stability of intention to accept a COVID-19 vaccine in Scotland: will those most at risk accept a vaccine? Vaccines (Basel) 2021;9:17. doi: 10.3390/vaccines9010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nguyen K.H., Srivastav A., Razzaghi H., et al. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination - United States, September and December 2020. Am J Transplant. 2021;21:1650–1656. doi: 10.1111/ajt.16560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garcia P., Montez-Rath M.E., Moore H., et al. SARS-CoV-2 vaccine acceptability in patients on hemodialysis: a nationwide survey. J Am Soc Nephrol. Published online April 29, 2021 doi: 10.1681/ASN.2021010104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oduwole E.O., Pienaar E.D., Mahomed H., et al. Current tools available for investigating vaccine hesitancy: a scoping review protocol. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2019-033245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Heller G.Z., Manuguerra M., Chow R. How to analyze the visual analogue scale: myths, truths and clinical relevance. Scand J Pain. 2016;13:67–75. doi: 10.1016/j.sjpain.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 18.Gagneux-Brunon A., Detoc M., Bruel S., et al. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. J Hosp Infect. 2021;108:168–173. doi: 10.1016/j.jhin.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilson R.J.I., Vergelys C., Ward J., et al. Vaccine hesitancy among general practitioners in Southern France and their reluctant trust in the health authorities. Int J Qual Stud Health Well-being. 2020;15:1757336. doi: 10.1080/17482631.2020.1757336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Di Gennaro F., Murri R., Segala F.V., et al. Attitudes towards anti-SARS-CoV2 vaccination among healthcare workers: results from a national survey in Italy. Viruses. 2021;13:371. doi: 10.3390/v13030371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Larson H.J., de Figueiredo A., Xiahong Z., et al. The State of Vaccine Confidence 2016: global insights through a 67-country survey. EBioMedicine. 2016;12:295–301. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dror A.A., Eisenbach N., Taiber S., et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35:775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fisher K.A., Bloomstone S.J., Walder J., et al. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of U.S. adults. Ann Intern Med. 2020;173:964–973. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Robertson E., Reeve K.S., Niedzwiedz C.L., et al. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav Immun. 2021;94:41–50. doi: 10.1016/j.bbi.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nguyen L.H., Joshi A.D., Drew D.A., et al. Racial and ethnic differences in COVID-19 vaccine hesitancy and uptake. Preprint. Posted online February 28, 2021 doi: 10.1101/2021.02.25.21252402. medRxiv. 2021.02.25.21252402. [DOI] [Google Scholar]
- 26.COCONEL Group A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. Lancet Infect Dis. 2020;20:769–770. doi: 10.1016/S1473-3099(20)30426-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Palamenghi L., Barello S., Boccia S., et al. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. Eur J Epidemiol. 2020;35:785–788. doi: 10.1007/s10654-020-00675-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barello S., Nania T., Dellafiore F., et al. 'Vaccine hesitancy' among university students in Italy during the COVID-19 pandemic. Eur J Epidemiol. 2020;35:781–783. doi: 10.1007/s10654-020-00670-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kerr J.R., Freeman A.L.J., Marteau T.M., et al. Effect of Information about COVID-19 vaccine effectiveness and side effects on behavioural intentions: two online experiments. Vaccines (Basel) 2021;9:379. doi: 10.3390/vaccines9040379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Battistella C., Quattrin R., Celotto D., et al. Factors predicting influenza vaccination adherence among patients in dialysis: an Italian survey. Hum Vaccin Immunother. 2019;15:2434–2439. doi: 10.1080/21645515.2019.1588005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.