Abstract
Importance and study objective
The COVID-19 pandemic has produced unprecedented changes in social, work, and leisure activities, which all have had major impact on sleep and psychological well-being. This study documented the prevalence of clinical cases of insomnia, anxiety, and depression and selected risk factors (COVID-19, confinement, financial burden, social isolation) during the first wave of the pandemic in 13 countries throughout the world.
Design and participants
International, multi-center, harmonized survey of 22 330 adults (mean age = 41.9 years old, range 18–95; 65.6% women) from the general population in 13 countries and four continents. Participants were invited to complete a standardized web-based survey about sleep and psychological symptoms during the first wave of the COVID-19 pandemic from May to August 2020.
Results
Clinical insomnia symptoms were reported by 36.7% (95% CI, 36.0–37.4) of respondents and 17.4% (95% CI, 16.9–17.9) met criteria for a probable insomnia disorder. There were 25.6% (95% CI, 25.0–26.2) with probable anxiety and 23.1% (95% CI, 22.5–23.6) with probable depression. Rates of insomnia symptoms (>40%) and insomnia disorder (>25%) were significantly higher in women, younger age groups, and in residents of Brazil, Canada, Norway, Poland, USA, and United Kingdom compared to residents from Asian countries (China and Japan, 8% for disorder and 22%–25% for symptoms) (all Ps < 0.01). Proportions of insomnia cases were significantly higher among participants who completed the survey earlier in the first wave of the pandemic relative to those who completed it later. Risks of insomnia were higher among participants who reported having had COVID-19, who reported greater financial burden, were in confinement for a period of four to five weeks, and living alone or with more than five people in same household. These associations remained significant after controlling for age, sex, and psychological symptoms.
Conclusion and relevance
Insomnia, anxiety, and depression were very prevalent during the first wave of the COVID-19 pandemic. Public health prevention programs are needed to prevent chronicity and reduce long-term adverse outcomes associated with chronic insomnia and mental health problems.
Keywords: Insomnia, Sleep problems, Anxiety, Depression, COVID-19, Pandemic
1. Introduction
The COVID-19 pandemic is one of the most significant health challenges of our time. In addition to the estimated 4.1 million deaths caused by this virus thus far (July 20, 2021), the pandemic has caused unprecedented changes in social, work, travel, and leisure activities. Stress has been ubiquitous due to health concerns, social isolation, financial hardship, home-schooling, and uncertainty about the future. Combined with mandatory confinement in many countries around the world, these multiple stressors have had major impacts on sleep and mental health [1,2].
Surveys conducted in several countries since the beginning of the pandemic, as well as meta-analyses [[3], [4], [5], [6]], have reported very high and variable rates of insomnia (20–35%), anxiety (20–45%), and depression (25–50%) in the general population [7,8], with rates even higher among health-care workers [[9], [10], [11], [12]] and patients with COVID-19 [6]. Such estimates clearly exceed base rates reported in most epidemiological studies conducted under normal circumstances (ie, pre-pandemic) and using similar criteria [13,14]. Although those studies are informative in documenting the unequivocal impact of the pandemic on sleep and mental health, there is much variability in the estimates provided due to different sampling methods, case definitions, and survey methodology across studies. This precludes valid comparisons across studies and an accurate portrayal of the extent of sleep and mental health problems in association with the pandemic around the world. Furthermore, very few studies have examined the specific role of confinement, social isolation, number of people living in same dwelling, and financial hardship in producing insomnia and psychological symptoms.
The present study used a harmonized questionnaire and case definitions, as well as a standard methodology to survey adults from the general population in 13 countries located on four continents around the world. The objective was to document the impact of the COVID-19 pandemic on insomnia and psychological symptoms. In addition to estimating the prevalence of insomnia, anxiety, and depression, the study aimed to examine their associations with COVID-19, confinement, social isolation, and financial burden. Specific research questions were: a) what is the prevalence of probable cases of clinical insomnia, anxiety, and depression? b) what is the trajectory of insomnia in relation to the time since the beginning of the pandemic? c) is there an association, above and beyond that explained by demographic and psychological factors, between insomnia and pre-pandemic history of sleep problems, and with COVID-19, duration of confinement, number of people living in the same home, and financial burden?
2. Methods
This study was part of an international collaboration involving investigators from several countries to examine sleep and circadian problems during the COVID-19 pandemic. The research protocol and survey questionnaire were published previously [15]. Several papers derived from this international collaboration are currently in progress and this paper focuses on insomnia and psychological symptoms (anxiety and depression). There were 13 participating countries (14 regions) including: Austria, Brazil, Canada, China/Jinlin, China/Hong Kong, Finland, France, Italy, Japan, Norway, Poland, Sweden, United Kingdom, and the United States. All investigators obtained ethical approval or exemptions from their local ethics committee. Participants provided consent in those countries where it was required by the local ethics committee.
The survey was anonymous, and participants did not have to provide identification information except for general sociodemographic variables. The platforms most used for administration of the survey were Redcap and Qualtrics. Dates of completion were recorded which allowed exploration of the relationship between responses and the temporal pattern of pandemic exposure and confinement in each country in accordance with WHO records of infections and deaths. Completion of the survey varied by country across May to August 2020.
2.1. Participants
Participants aged 18 years or older were invited via various means such as local media (eg, newspapers, television), social media (eg, Facebook and Instagram), and university mass mail lists to complete an online survey. A total of 25 484 adults entered the websites to complete the survey. People who failed to provide consent (N = 977), did not indicate gender and age (mandatory for weighting, N = 431), or did not complete the Insomnia Severity Index (N = 1746) were excluded, leaving a final sample of 22 330 participants in the study.
2.2. Measures
The survey included questions (100 items) from validated questionnaires, as well as questions that were developed for this study. It was translated in national languages and its completion was taking between 20 and 30 min. This paper focuses on data about insomnia and psychological symptoms (anxiety and depression) derived from the following measures.
Insomnia Severity Index (ISI). This 7-item instrument assesses perceived severity of nocturnal and daytime symptoms of insomnia. Each item is rated on a scale of 0–4 for a total score ranging from 0 to 28. A score of 0–7 indicates no insomnia, 8–14 subthreshold clinical insomnia, 15–21 insomnia of moderate severity, and 22 and above indicates severe insomnia. Cut-off scores of 10 and 15 have been used to identify probable cases of insomnia and cases with insomnia disorders in community samples [16].
Patient Health Questionnaire-2 (PHQ-2). A 2-item abbreviated version of the PHQ-9 measuring mood and interest in doing things over the preceding two weeks. The two items are rated on scales of 0–3 and a total score of three or more is the recommended optimal cut-off to screen for depression [17]. A PHQ-2 score equal or greater than three had a sensitivity of 83% and a specificity of 92% for major depression.
Generalized Anxiety Disorder-2 (GAD-2). Two screening items rated on scales of 0–3 and derived from the GAD-7 measure [17]. A score of three or greater is the preferred cut-off for identifying possible cases of anxiety disorder, with sensitivity of 86% and specificity of 83%, for diagnosing generalized anxiety disorder.
Potential moderators of insomnia. We examined four potential moderators of insomnia derived from specific questions on the sleep survey. These were: a) SARS-CoV-2 infection (yes or no), b) perceived financial burden due to pandemic (0 = none to 5 = very much), c) duration of confinements (number of weeks), and d) number of people living in same household.
2.3. Data analysis
As recruitment was based on voluntary participation, the sample was not random; consequently, we expected either under or oversampling according to countries, age groups, or sex. Thus, an approach to mitigate sampling bias, based on “crowdsourcing” strategy [18,19] was implemented. First, as the countries/regions included in the study were not selected to create a representative sample of the “world population”, country/region weight was not set according to relative adult population size of each participating country (where China and USA samples would have dominated the results). Rather, they were given an “equal” share basis (each country contributed a weighted share of 1/14th of the total sample, with China/Jinlin and China/Hong Kong receiving one share each). Second, to reduce potential bias resulting from the oversampling of young and female participants, post-stratification weights for the complete dataset were computed according to the joint distribution of age and sex for a population structure comparable to most countries included in the survey, that is the Canadian adult (18–75 years) population in 2020 (updated population estimates for 2016 Census, Statistics Canada). All descriptive and inferential analyses, except for sample description, were completed using weights on the SAS 9.4 statistical software, with standard two-tailed alpha of 5%.
Case definitions. Two insomnia subgroups were identified based on previously validated ISI cut off scores. Individuals with ISI scores ≥10 were identified as presenting clinically significant insomnia symptoms and those with ISI scores ≥15 were identified as probable cases of insomnia disorder according to DSM-5 or ICSD-3 diagnostic classifications [16]. Likewise, probable cases of anxiety and depressive disorders were based on previously validated cut-offs, with scores of three points or greater on the GAD-2 and PHQ-2 scales, respectively, indicating probable cases [17].
3. Results
The total sample of 22 330 adults comprised 14 642 women and 7688 men, aged from 18 to 95 years (M = 41.9, SD = 16.0). Non-weighted distribution of participants by country, sex and age groups are shown in Table 1 . A total of 12 513 (56.2%) were married/cohabitating, 8018 (36.0%) were single, and 22.3% lived alone. Regarding ethnicity, 9434 (43%) participants self-identified as white/Caucasian, 8980 (40.9%) as Asian, 776 (3.5%) as Hispanic, 446 (2.0%) as black, and 2329 (10.6%) as other/not specified.
Table 1.
Non-weighted distribution (%) of women and age groups by country.
| Country | Sample N |
18-34y % |
35-54y % |
55 + y % |
Women % |
|---|---|---|---|---|---|
| Austria | 834 | 20.9 | 54.6 | 24.6 | 77.9 |
| Brazil | 1821 | 65.8 | 25.6 | 8.5 | 75.1 |
| Canada | 2934 | 29.9 | 36.2 | 33.9 | 72.8 |
| China, Hong Kong | 1241 | 60.4 | 27.1 | 12.6 | 60.1 |
| China, Jinlin | 1071 | 47.1 | 47.9 | 5.0 | 74.2 |
| Finland | 787 | 24.8 | 49.4 | 25.8 | 79.2 |
| France | 880 | 28.9 | 42.3 | 28.9 | 70.8 |
| Italy | 1587 | 72.0 | 20.0 | 7.9 | 80.8 |
| Japan | 7000 | 35.4 | 29.8 | 34.9 | 50.0 |
| Norway | 1065 | 24.6 | 50.0 | 25.4 | 74.5 |
| Poland | 379 | 22.4 | 62.3 | 15.3 | 90.8 |
| Sweden | 566 | 42.2 | 47.2 | 10.6 | 76.3 |
| UK | 1140 | 23.7 | 40.6 | 35.7 | 86.2 |
| USA | 1025 | 51.1 | 38.5 | 10.3 | 35.9 |
| Total Sample | 22 330 | 40.1 | 35.3 | 24.6 | 65.6 |
3.1. Insomnia
Table 2 shows average total ISI scores, and proportions of participants with insomnia symptoms (ISI ≥ 10) and probable insomnia disorder (ISI ≥ 15), for the overall sample and for each country. There were 17.4% (95% CI, 16.9–17.9) of respondents who were identified with probable insomnia disorder while 36.7% (95% CI, 36.0–37.4) had insomnia symptoms. There was considerable variability across countries for both rates of insomnia symptoms, χ2 (13) = 1132.75, P < 0.001, and insomnia disorder, χ2 (13) = 939.19, P < 0.001, with significantly lower rates in Asian countries (China and Japan, 7.5–8.5% for probable insomnia disorder and 22.3–25.2% for symptoms) compared with Brazil, UK, Canada, USA, Poland, and Norway, which all presented the highest rates of insomnia symptoms (all above 40%) and disorder (all above 22%).
Table 2.
Mean (SD) Insomnia Severity Index (ISI) score, clinical level of insomnia symptoms (ISI ≥ 10) and probable insomnia cases (ISI ≥ 15) by country, weighted.
| Country | ISI |
Insomnia Symptoms |
Probable Insomnia Disorder |
||
|---|---|---|---|---|---|
| Mean (SE) | % | 95% CI | % | 95% CI | |
| Austria | 6.9 (0.15) | 30.3 | 28.1–32.6 | 12.5 | 11.0–14.2 |
| Brazil | 10.0 (0.15) | 48.8 | 46.4–51.3 | 25.4 | 23.3–27.6 |
| Canada | 9.6 (0.18) | 47.1 | 44.2–50.1 | 26.3 | 23.8–29.0 |
| China, Hong Kong | 6.6 (0.16) | 24.0 | 21.9–26.3 | 8.5 | 7.2–10.0 |
| China, Jinlin | 5.4 (0.15) | 22.3 | 20.4–24.4 | 7.5 | 6.3–8.9 |
| Finland | 7.3 (0.16) | 28.9 | 26.7–31.3 | 13.6 | 11.9–15.4 |
| France | 8.1 (0.17) | 38.0 | 35.3–40.8 | 19.0 | 16.9–21.4 |
| Italy | 6.5 (0.15) | 27.5 | 25.4–29.8 | 8.2 | 6.9–9.7 |
| Japan | 6.9 (0.15) | 25.2 | 23.2–27.4 | 7.9 | 6.7–9.3 |
| Norway | 8.9 (0.18) | 40.8 | 38.0–43.7 | 22.2 | 19.9–24.7 |
| Poland | 9.4 (0.16) | 45.2 | 42.6–47.8 | 24.4 | 22.3–26.7 |
| Sweden | 7.5 (0.16) | 32.2 | 29.9–34.7 | 16.0 | 14.2–18.0 |
| UK | 10.2 (0.16) | 48.6 | 46.0–51.2 | 25.6 | 23.4–27.9 |
| USA | 10.6 (0.15) | 59.8 | 57.4–62.2 | 31.4 | 29.2–33.8 |
| Total Sample | 8.1 (0.04) | 36.7 | 36.0–37.4 | 17.4 | 16.9–17.9 |
The rate of insomnia symptoms was significantly higher in women (39.5%) than in men (33.9%), χ2 (1) = 74.22, P < 0.001. A similar difference was observed for insomnia disorder, with 19.1% of women and 15.7% of men with ISI score of 15 or higher, χ2 (1) = 41.86, P < 0.001. Regarding age groups, insomnia symptoms were more frequently reported by participants aged 18–34 years old (38.5%) and 35–54 years old (38.6%), compared to participants aged 55 years old or older (33.0%) (both Ps < 0.001). Probable cases of insomnia disorder showed a similar pattern of results, with rates of 17.9% (18–34 years old), 18.6% (35–54 years old), and 15.7% (55 years old or older), respectively for the three subgroups (both Ps < 0.001).
Insomnia subtypes (initial, middle, early morning awakenings) were estimated based on the first three ISI items with a score ≥ 2 (indicating at least moderate severity). Overall, 46.8% participants reported at least one type of insomnia. Specifically, 28.9% reported sleep onset difficulties, 32.1% sleep maintenance difficulties, and 31.7% reported early morning awakenings. Mixed sleep onset and sleep maintenance (middle or early morning awakenings) difficulties were reported by 22.6% of the sample.
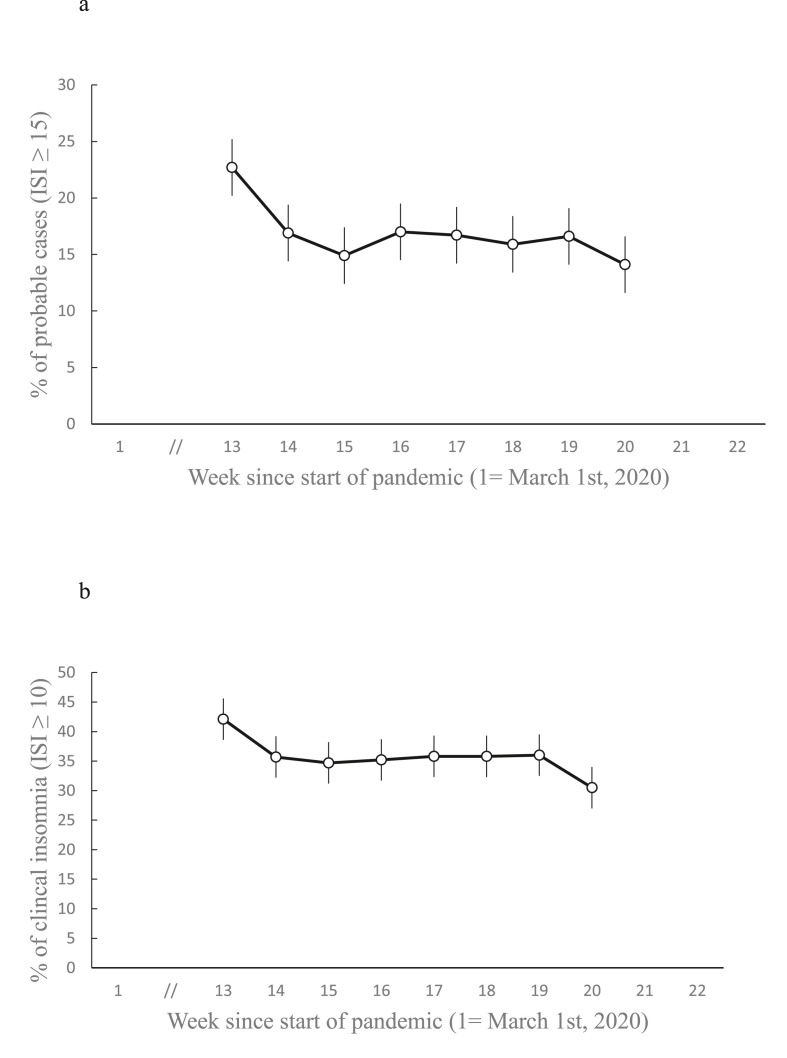
The proportion of cases with insomnia was examined as a function of the number of weeks since the start of the pandemic (Fig. 1 a and b). Weighted estimates were obtained according to a multi-level logistic model, using country as a random intercept (ie, to take into account that different countries have different base rates of insomnia, as seen in Table 2). Percentages of respondents with insomnia symptoms were significantly different according to the number of weeks since the beginning of the pandemic, F (7, 20117) = 3.83, P < 0.001, with significant reductions observed between weeks 13th and 14th (first two weeks of data collection for the current study) and weeks 19th and 20th (last two weeks of data collection). Percentages of cases of insomnia disorder were also significantly different according to week, F (7, 20117) = 4.32, P < 0.001, with an identical pattern of reductions to those of symptoms over time.
Fig. 1.
a. Weighted % (with standard errors) of probable cases of insomnia, according to the number of weeks since start of pandemic. b. Weighted % (with standard errors) of clinical level of insomnia symptoms, according to the number of weeks since start of pandemic.
3.2. Anxiety and depression
Table 3 displays the weighted percentages of probable cases of anxiety and depression for the total sample and by country. There were 25.6% (95% CI, 25.0–26.2) with probable anxiety and 23.1% (95% CI, 22.5–23.6) with probable depressive disorders. As for insomnia, there was significant variability across countries with the lowest rates obtained among respondents from Japan (12.5% anxiety, 11.7% depression), China (12.3% anxiety, 14.1% depression), Finland (13.9% anxiety, 12.8% depression), and the highest rates were in the USA (48.8% for anxiety and 48.3% for depression) and Brazil (47.2% anxiety, 38.0% depression), followed by Canada, Poland, and the UK.
Table 3.
Proportion of respondents with probable anxiety (GAD2 ≥ 3) and depressive disorder (PHQ2 ≥ 3), by country, weighted.
| Country | Probable Anxiety Cases |
Probable Depression Cases |
||
|---|---|---|---|---|
| % | 95% CI | % | 95% CI | |
| Austria | 21.2 | 19.3–23.3 | 18.2 | 16.4–20.2 |
| Brazil | 47.2 | 44.8–49.7 | 38.0 | 35.6–40.4 |
| Canada | 35.3 | 32.6–38.2 | 28.1 | 25.6–30.8 |
| China, Hong Kong | 14.6 | 13.0–16.5 | 15.5 | 13.7–17.4 |
| China, Jinlin | 10.1 | 8.7–11.7 | 12.6 | 11.1–14.3 |
| Finland | 13.9 | 12.2–15.7 | 12.8 | 11.2–14.6 |
| France | 29.2 | 26.7–31.8 | 19.1 | 17.0–21.4 |
| Italy | 22.0 | 20.0–24.1 | 17.1 | 15.3–19.0 |
| Japan | 12.5 | 10.9–14.2 | 11.7 | 10.2–13.3 |
| Norway | 19.9 | 17.6–22.3 | 23.4 | 21.0–25.9 |
| Poland | 32.5 | 30.0–35.1 | 25.6 | 23.3–28.0 |
| Sweden | 19.9 | 17.9–22.0 | 22.5 | 20.4–24.7 |
| UK | 31.3 | 28.9–33.8 | 28.3 | 26.0–30.8 |
| USA | 51.3 | 48.8–53.7 | 50.7 | 48.3–53.2 |
| Total Sample | 25.6 | 25.0–26.2 | 23.1 | 22.5–23.6 |
Note. GAD = Generalized Anxiety Disorder; PHQ = Patient Health Questionnaire.
The rates of probable cases of anxiety and depression were significantly higher among women (29.0% and 24.6%) than in men (22.2% and 21.6%) (both ps < 0.001). Comparison of age subgroups showed a decreasing trend for participants aged 18–34 years old to present the highest proportion of probable cases of anxiety (31.5%) and depression (29.6%), compared to participants aged 35–54 years old (26.9% and 22.5%), and participants aged 55 years of age or older (18.8% and 17.6%) (all ps < 0.001).
3.3. Sleep medication use
There were 84% of the sample who did not use sleep medication or reported using it less than once per month, 8% used it between less than once per week to two days per week, and 8% who reported regular use (3–7 nights per week) (see Supplement, Table 5). There was significant variability in reported usage across countries; regarding regular use, the lowest rates were among respondents from China-Jinlin (1.7%), France (3.4%), Italy (4.0%), Austria (4.1%) and UK (4.7%), and the highest rates were in the USA (21.3%), Poland (13.3%), Norway (12.8%), Brazil (10.9%), and Finland (10.2%).
3.4. Associations of insomnia with COVID-19, financial burden, confinement, and number of persons living in same household
Three weighted logistic GEE models, controlling for country clustering, were completed to estimate the association between four predictors (COVID-19; n = 669, financial burden, confinement duration, number of people living in household) and risk of insomnia symptoms and disorders. Three models were tested: (a) an unadjusted model to get the raw association between each predictor and insomnia symptoms/disorder, (b) model 1, adjusting for age and sex, and (c) model 2, additionally adjusting for anxiety and depressive symptoms (see Table 4 ). Since exploratory analyses suggested that confinement duration and number of persons in household exhibited a non-linear relationship with insomnia risk, these variables were examined as categorical predictors.
Table 4.
Prediction of insomnia symptoms (ISI ≥ 10) and insomnia disorder (ISI ≥ 15), based on GEE logistic models including four predictors: COVID-19, financial burden, duration of confinement, and number of persons in the same household (N = 15 094).
| Predictors | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Clinical cases of insomnia symptoms (chi-square and p-value) | |||
| Infection (Y/N) | 5.12, P = 0.02 | 5.49, P = 0.02 | 1.78, P = 0.18 |
| Financial burden (0–4) | 272.84, P < 0.001 | 244.83, P < 0.001 | 29.26, P < 0.001 |
| Duration of confinement (0–10 weeks) | 22.37, P < 0.001 | 23.21, P < 0.001 | 8.95, P = 0.11 |
| Number of persons living in same household (0–7) | 48.47, P < 0.001 | 47.26, P < 0.001 | 146.88, P < 0.001 |
| Age | – | 12.21, P = 0.03 | 12.74, P = 0.03 |
| Sex | – | 20.70, P < 0.001 | 1.69, P = 0.19 |
| Anxiety symptoms (GAD2) | – | – | 112.85, P < 0.001 |
| Depression symptoms (PHQ2) | – | – | 281.85, P < 0.001 |
| Correct classification (%) | 63.0% | 63.6% | 75.4% |
| Probable cases of insomnia disorder (chi-square and p-value) | |||
| Infection (Y/N) | 7.96, P = 0.005 | 8.49, P = 0.004 | 4.20, P = 0.04 |
| Financial burden (0–4) | 335.25, P < 0.001 | 273.35, P < 0.001 | 25.96, P < 0.001 |
| Duration of confinement (in weeks) (0–10) | 35.61, P < 0.001 | 53.37, P < 0.001 | 16.28, P = 0.006 |
| Number of persons living in same household) (0–7) | 35.75, P < 0.001 | 35.31, P < 0.001 | 131.23, P < 0.001 |
| Age | – | 4.83, P = 0.44 | 58.54, P < 0.001 |
| Sex | – | 5.48, P = 0.02 | 0.20, P = 0.66 |
| Anxiety symptoms (GAD2) | – | – | 44.14, P < 0.001 |
| Depression symptoms (PHQ2) | – | – | 109.84, P < 0.001 |
| Correct classification (%) | 81.7% | 81.7% | 85.2% |
∗P < 0.05, ∗∗P < 0.01, ∗∗∗P < 0.001.
Note. Model 1 included only predictor, model 2 included model 1 + age + sex, model 3 included model 2 + anxiety (GAD2) + depression (PHQ2).
All four predictors were significantly associated with both insomnia symptoms and insomnia disorders in Model 1 (no adjustment) and Model 2 (adjusted for sex and age). The associations remained significant with Model 3 (adjusted for sex, age, anxiety, and depression), with the exception of two predictors (infection and confinement) that were no longer significant for insomnia symptoms. Model 3 correctly classified 75.5% of cases with insomnia symptoms and 85.2% of cases with insomnia disorders.
Examination of non-linearity revealed that duration of confinement had an inverse, U-shape, relationship with risk of insomnia symptoms/disorder: people reporting no confinement or the longest confinement (7 weeks or more) had the lowest risk (37% for insomnia symptoms and 15% for insomnia disorder) while those confined for 3–6 weeks had the highest risk (44% for insomnia symptoms and 20% for insomnia disorder). A lesser “U-shape” relationship was also found for number of people living in same household: people living with 2–4 other persons in same household showed a lower risk of insomnia (symptoms = 36%, disorder = 14%) compared to those living alone (symptoms = 40%, disorder = 17%) or those with 5 or more persons (symptoms = 42%, disorder = 18%). An additional analysis revealed that respondents living alone (22.3%) had a higher risk (38.0% vs. 32.6%) to report insomnia symptoms, OR = 1.27 (95% CI1.19–1.35) and insomnia disorder (19.0% vs. 13.6%), OR = 1.49 (95% CI, 1.31–1.69) compared with those living with at least one other person, even after controlling for age and sex.
Similar analyses were conducted to estimate the association between the same four predictors with anxiety and depression and the results are shown in Table 6 (Supplement).
3.5. Association of insomnia with number of COVID-19 cases and deaths at survey time
To study the association between the perceived risk of contracting COVID-19 and insomnia, two predictors were derived at the country level (number of COVID cases and deaths per 100 000 population at the time of survey). Controlling for age, sex and country clustering effect, a first GEE weighted model showed that number of COVID-19 cases (p = 0.19) and number of deaths (p = 0.11) failed to predict cases with insomnia symptoms. A second GEE model found that number of deaths per 100 000 significantly predicted probable cases of insomnia disorder, OR = 0.969 (95% CI = 0.939–0.999), but the association with number of COVID-19 cases failed to reach significance, p = 0.09.
4. Discussion
This international study revealed that rates of insomnia symptoms (36.7%) and insomnia disorder (17.4%) were about twice as high during the first wave of the pandemic as prevalence rates typically reported in non-pandemic times [14,20], and those differences were even higher in some countries, particularly in Brazil, Canada, United Kingdom and in the United States. Similar findings were observed for prevalence rates of probable anxiety (25.6%) and depression (23.1%), which were significantly higher than the typical population-based prevalence rates [21]. Although comparisons with epidemiological surveys conducted before the pandemic are tentative given the obvious differences in methodology and sample representativeness, the present findings indicate very high rates of clinical insomnia, anxiety, and depression during the first wave of the COVID-19 pandemic.
Prevalence rates obtained for all three conditions - insomnia, anxiety, and depression, are comparable or higher to those reported in previous surveys conducted during the COVID-19 pandemic within the general population [3,7] and with health-care workers [4,5,9,10]. For example, a meta-analysis of 44 studies conducted in 13 countries revealed a 35.7% prevalence rate of sleep problems across studies conducted in the general population, although no standard criteria or measures were used across studies to define sleep problems. In another meta-analysis of 22 studies, rates of depression and anxiety (38% for each) and of insomnia (48%) were even higher than the current one, although the definitions of each conditions were not the same as in the present study [6]. Another meta-analysis of studies conducted with health-care workers [9] found pooled prevalence of 38.9% for insomnia, 23.2% for anxiety, and 22.8% for depression. Other studies that focused on health-care workers in China reported prevalence rates of 34% [10] and 36.1% [11], despite using quite different cut-off scores on the ISI (15 and 8, respectively). In addition to targeting different samples, those studies used different sampling methods, measures, and definitions of sleep problems, hence making comparisons across studies very tentative.
Rates of insomnia were higher among those who completed the survey during the early phase of the pandemic, which could suggest that the novelty of the stressor (pandemic) had a greater impact on sleep of those who completed the survey early on (May–June) compared to those who completed it later (July–August). These changing rates of insomnia over time could also be explained by a reduction in perceived stress among individuals who completed the survey later in the summer when there were fewer measures of restrictions and confinements.
With regard to potential contributors to insomnia, the occurrence of stressful life events is among the most prominent precipitating factors associated with new onset of sleep disturbances [22]. In the context of the COVID-19 pandemic, stress about health and the fear of contracting COVID-19, concerns about finances and employment, confinement, and social isolation were all involved in contributing to insomnia. In the present study, higher risks of insomnia were associated, as expected, with more financial burden and reports of COVID-19. However, the associations with duration of confinement and social isolation were not as clear. The association with confinement suggests that participants in confinement for a moderate duration (3–6 weeks) were at greater risk of insomnia, whereas risks were lower among those reporting no confinement or confinement for longer periods (7 weeks and more). It is plausible that the immediate stress response associated with the announcement of mandatory confinement increased the risk of sleep disturbances, which was eventually followed by people adjusting their routines to the confinement. This may have been followed once again after two months by re-emergence of distress or anger which may have increased vulnerability to disturbances. This interpretation remains tentative as we do not have repeated assessment and longitudinal data to validate this trajectory.
Although it was expected that people living alone would show increased vulnerability to insomnia, possibly due to social isolation, we found a more complex relationship in that not only people living alone but also those with five or more individuals in the same household were at greater risks for insomnia. This might suggest that people in confinement, working from home, and living either alone or with several other people in the same household may have experienced increased stress, burden, and sleep disturbances. There could be several possible explanations for this association such as the need to care for children and the frustration of not being able to accomplish one's work due to an overcrowded dwelling. Environmental factors such as noise and light, as well as electronic media use may also have played a role in poor sleepers living with their family in restricted spaces. Another international study found that difficulties accomplishing work because of having to care for other people and increased verbal arguments with other adults in the same household were associated with poorer sleep health [23].
Although the current study did not specifically address the impact of the pandemic on sleep schedule changes, some studies have reported a significant shift in sleep schedules with important delay in both bedtimes and rise times occurring during the pandemic, particularly among younger adults, those working from home, and among people reporting higher psychological distress [24,25]. Although some people used that opportunity to catch up on chronic sleep loss accumulated in the pre-pandemic period, for others, the actual increased in time spent in bed was not paralleled by an equivalent increase in sleep time, with a net result of poorer sleep efficiency and sleep quality [24,26]. Thus, it is possible that sleep schedule shifting may have contributed to increased insomnia in the current study.
A critical issue that cannot be resolved with the current cross-sectional study design is the extent to which individuals who developed clinically significant insomnia and psychological symptoms during the pandemic will remit and, for those who don't, what will be the long-term consequences. There is solid evidence, however, that insomnia often follows a persistent course [27] and, when it reaches a chronic status, it produces adverse health outcomes, such as enhanced risk of depression [28], prolonged leave of absences from work [29], and increased risk for hypertension [30]. It is also possible that milder form of sleep disturbances remit with the end of confinement as was observed with the end of the confinement following the first wave in France [31].
The present findings must be interpreted in light of several caveats, most of which are inherent to survey methodology. For instance, the high rates of insomnia, depression and anxiety may be tinted by a sampling bias in that individuals with more sleep and psychological symptoms may have been more inclined to participate in such a survey; thus, these prevalence rates are relative and cannot be compared directly to those derived from epidemiological survey using a random sample of the population. In addition, any comparison of those rates with pre-pandemic data are likely to be counfounded by recall bias and must be interpreted cautiously in the absence of repeated data from the same individuals. Finally, the dynamic of the virus spreading, death rates, and confinement were all very different in different countries and any attempts at predicting insomnia, anxiety, and depression with these predictors remain tentative.
In conclusion, the rates of insomnia symptoms (36.7%), insomnia disorder (17.4%), probable anxiety (25.6%), and depression (23.1%) were very high during the first wave of the pandemic. The main implication of the current findings is that health authorities must deploy large and efficient, population-based sleep and mental health prevention programs, as well as clinical interventions/resources [32,33], to assist at-risk individuals and reduce long-term adverse health outcomes and morbidity.
Credit author statement
Not applicable.
Footnotes
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleep.2021.07.035.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sleep.2021.07.035.
Conflict of interest
The following is the supplementary data to this article:
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Cox R.C., Olatunji B.O. Sleep in a pandemic: implications of COVID-19 for sleep through the lens of the 3P model of insomnia. Am Psychol. 2021 Jun 17 doi: 10.1037/amp0000850. Online ahead of print. PMID: 34138586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zitting K.M., Lammers-van der Holst H.M., Yuan R.K., et al. Google Trends reveals increases in internet searches for insomnia during the 2019 coronavirus disease (COVID-19) global pandemic. J Clin Sleep Med. 2021;17(2):177–184. doi: 10.5664/jcsm.8810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jahrami H., BaHammam A.S., Bragazzi N.L., et al. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. 2021;17(2):299–313. doi: 10.5664/jcsm.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alimoradi Z., Brostrom A., Tsang H.W.H., et al. Sleep problems during COVID-19 pandemic and its' association to psychological distress: a systematic review and meta-analysis. EClinical Med. 2021;36:100916. doi: 10.1016/j.eclinm.2021.100916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hao Q., Wang D., Xie M., et al. Prevalence and risk factors of mental health problems among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Front Psychiatr. 2021;12:567381. doi: 10.3389/fpsyt.2021.567381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu C., Pan W., Li L., et al. Prevalence of depression, anxiety, and insomnia symptoms among patients with COVID-19: a meta-analysis of quality effects model. J Psychosom Res. 2021;147:110516. doi: 10.1016/j.jpsychores.2021.110516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meaklim H., Junge M.F., Varma P., et al. Pre-existing and post-pandemic insomnia symptoms are associated with high levels of stress, anxiety and depression globally during the COVID-19 pandemic. J Clin Sleep Med. 2021 May 14 doi: 10.5664/jcsm.9354. Online ahead of print. PMID: 33985647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Petrov M.E., Pituch K.A., Kasraeian K., et al. Impact of the COVID-19 pandemic on change in sleep patterns in an exploratory, cross-sectional online sample of 79 countries. Sleep Health. 2021 Jun 27 doi: 10.1016/j.sleh.2021.05.007. S2352-7218(21)00114-5. Online ahead of print. PMID: 34193394. [DOI] [PubMed] [Google Scholar]
- 9.Pappa S., Ntella V., Giannakas T., et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lai J., Ma S., Wang Y., et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang C., Yang L., Liu S., et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psychiatr. 2020;11:306. doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beck F., Leger D., Fressard L., et al. Covid-19 health crisis and lockdown associated with high level of sleep complaints and hypnotic uptake at the population level. J Sleep Res. 2021;30(1):e13119. doi: 10.1111/jsr.13119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kessler R.C., Berglund P., Demler O., et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatr. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 14.Ohayon M.M. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6(2):97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 15.Partinen M., Bjorvatn B., Holzinger B., et al. Sleep and circadian problems during the coronavirus disease 2019 (COVID-19) pandemic: the International COVID-19 Sleep Study (ICOSS) J Sleep Res. 2020 doi: 10.1111/jsr.13206. Nov 12. [DOI] [PubMed] [Google Scholar]
- 16.Morin C.M., Belleville G., Belanger L., et al. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kroenke K., Spitzer R.L., Williams J.B.W., et al. An ultra-brief screening scale for anxiety and depression : the PHQ-4. Psychosomatics. 2009;50(6):613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 18.Statistics Canada Impacts of COVID-19 on Canadians: data collection series. 2020. https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&Id=1280907 Online document.
- 19.Renaud M. Use of crowdsourcing at Statistics Canada during the COVID-19 pandemic – methodological considerations. Talk Support Doc. 2021 https://www.ciqss.org/presentation/use-of-crowdsourcing-at-statistics-canada-during-covid-19-pandemic [Google Scholar]
- 20.Morin C.M., LeBlanc M., Belanger L., et al. Prevalence of insomnia and its treatment in Canada. Can J Psychiatr Revue Canadienne de Psychiatrie. 2011;56(9):540–548. doi: 10.1177/070674371105600905. [DOI] [PubMed] [Google Scholar]
- 21.Kessler R.C., Chiu W.T., Demler O., et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatr. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bastien C.H., Vallières A., Morin C.M. Precipitating factors of insomnia. Behav Sleep Med. 2004;2(1):50–62. doi: 10.1207/s15402010bsm0201_5. [DOI] [PubMed] [Google Scholar]
- 23.Yuksel D., McKee G.B., Perrin P.B., et al. Sleeping when the world locks down: correlates of sleep health during the COVID-19 pandemic across 59 countries. Sleep Health. 2021 Apr;7(2):134–142. doi: 10.1016/j.sleh.2020.12.008. Epub 2021 Jan 26. PMID: 33509687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cellini N., Conte F., DeRosa O., et al. Changes in sleep timing and subjective sleep quality during the COVID-19 lockdown in Italy and Belgium: age, gender and working status as modulating factors. Sleep Med. 2021;77:112–119. doi: 10.1016/j.sleep.2020.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Korman M., Tkachev V., Reis C., et al. COVID-19-mandated social restrictions unveil the impact of social time pressure on sleep and body clock. Sci Rep. 2020;10(1):22225. doi: 10.1038/s41598-020-79299-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robillard R., Dion K., Pennestri M.H., et al. Profiles of sleep changes during the COVID-19 pandemic: demographic, behavioural and psychological factors. J Sleep Res. 2021;30(1) doi: 10.1111/jsr.13231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morin C.M., Jarrin D.C., Ivers H., et al. Incidence, persistence, and remission rates of insomnia over 5 Years. JAMA Netw Open. 2020;3(11) doi: 10.1001/jamanetworkopen.2020.18782. Nov 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baglioni C., Battagliese G., Feige B., et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135(1–3):10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 29.Sivertsen B., Overland S., Neckelmann D., et al. The long-term effect of insomnia on work disability: the HUNT-2 historical cohort study. Am J Epidemiol. 2006;163(11):1018–1024. doi: 10.1093/aje/kwj145. [DOI] [PubMed] [Google Scholar]
- 30.Suka M., Yoshida K., Sugimori H. Persistent insomnia is a predictor of hypertension in Japanese male workers. J Occup Health. 2003;45(6):344–350. doi: 10.1539/joh.45.344. [DOI] [PubMed] [Google Scholar]
- 31.Beck F., Leger D., Cortaredona S., et al. Would we recover better sleep at the end of Covid-19? A relative improvement observed at the population level with the end of the lockdown in France. Sleep Med. 2021;78:115–119. doi: 10.1016/j.sleep.2020.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Espie C.A., Emsley R., Kyle S.D., et al. Effect of digital cognitive behavioral therapy for insomnia on health, psychological well-being, and sleep-related quality of life: a randomized clinical trial. JAMA Psychiatr. 2019;76(1):21–30. doi: 10.1001/jamapsychiatry.2018.2745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Altena E., Baglioni C., Espie C.A., et al. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J Sleep Res. 2020;29(4) doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.