Abstract
Background The telemedicine industry has been experiencing fast growth in recent years. The outbreak of coronavirus disease 2019 (COVID-19) further accelerated the deployment and utilization of telemedicine services. An analysis of the socioeconomic characteristics of telemedicine users to understand potential socioeconomic gaps and disparities is critical for improving the adoption of telemedicine services among patients.
Objectives This study aims to measure the correlation of socioeconomic determinants with the use of telemedicine services in Milwaukee metropolitan area.
Methods Electronic health record review of patients using telemedicine services compared with those not using telemedicine services within an academic-community health system: patient demographics (e.g., age, gender, race, and ethnicity), insurance status, and socioeconomic determinants obtained through block-level census data in Milwaukee area. The telemedicine users were compared with all other patients using regression analysis. The telemedicine adoption rates were calculated across regional ZIP codes to analyze the geographic patterns of telemedicine adoption.
Results A total of 104,139 patients used telemedicine services during the study period. Patients who used video visits were younger (median age 48.12), more likely to be White (odds ratio [OR] 1.34; 95% confidence interval [CI], 1.31–1.37), and have private insurance (OR 1.43; CI, 1.41–1.46); patients who used telephone visits were older (median age 57.58), more likely to be Black (OR 1.31; CI 1.28–1.35), and have public insurance (OR 1.30; CI 1.27–1.32). In general, Latino and Asian populations were less likely to use telemedicine; women used more telemedicine services in general than men. In the multiple regression analysis of social determinant factors across 126 ZIP codes, college education (coefficient 1.41, p = 0.01) had a strong correlation to video telemedicine adoption rate.
Conclusion Adoption of telemedicine services was significantly impacted by the social determinant factors of health, such as income, education level, race, and insurance type. The study reveals the potential inequities and disparities in telemedicine adoption.
Keywords: telemedicine, telehealth, health services, COVID-19, health inequality, health system
Background and Significance
Telemedicine leverages telecommunication technologies to enable the delivery of health care services remotely to patients. 1 2 With telemedicine, patients could gain access to needed care without in-person visits to health providers. Telemedicine is believed to have many benefits, 3 4 5 such as addressing health care access problems, 6 7 8 providing health services in a more timely and cost-effective manner, 9 10 11 and improving patient satisfaction. 12 13 These benefits have been demonstrated by various telemedicine applications. For example, convenient access makes telemedicine an amiable tool for patients who have challenges in accessing in-person health care, such as patients with movement disorders, 14 15 and pediatric patients in underserved areas. 16 17 Telemedicine systems provide user-friendly functionalities that could empower patients' self-care capabilities, such as improving treatment adherence for sleep apnea, 18 diabetes monitoring, 19 and chronic disease management. 20
The recent outbreak of coronavirus significantly increased the relevance of telemedicine. 21 22 23 The pandemic imposed a significant burden on many hospital systems around the world. Many hospital systems were overwhelmed by in-person patient visits and the extra care needed by the infected patients in the setting of a highly contagious pathogen. To reduce the spread of infection, health policymakers and administrators, such as the U.S. Centers for Disease Control (CDC) 24 and the Health Resources and Services Administration (HRSA), 25 encouraged hospitals and patients to use telemedicine to access health services remotely. Telemedicine became a critical tool for many health systems to ensure timely patient access to health care needs. Due to the quick escalation of the pandemic, many providers and patients had to adopt the use of telemedicine in a relatively short time. While telemedicine has been rolled out at scale quickly across health care systems, little has been done to understand the socioeconomic implication of this transition.
We hypothesized that socioeconomic differences could create gaps in telemedicine adoption among different patient groups during this period. Scant literature is available investigating the impact of socioeconomic factors on the adoption of telemedicine services by patients. Understanding the possible gaps and impacts of socioeconomic challenges is a crucial step toward addressing health care inequities which is one of the leading health indicators for the Healthy 2030 framework. 26 The objective of this study was to assess the impact of socioeconomic factors on the adoption of telemedicine services in a health system during the coronavirus disease 2019 (COVID-19) pandemic in Milwaukee metropolitan area.
We sought to understand how socioeconomic factors impacted the utilization of telemedicine services, further subdivided into video visit and audio-only (telephone) visit adoption. While telemedicine has been rolled out at scale quickly across health care systems, little has been done to understand the socioeconomic implication of this transition.
Methods
Telemedicine Implementation
Prior to the COVID-19 public health emergency, (PHE), telemedicine at the Froedtert Health System was available for primary care patients under select, commercial insurance plans. In response to the PHE, the shortages of personal protective equipment, and insurance coverage by both government and commercial payors, telemedicine was rapidly deployed across all specialties. During the stay-at-home order, clinic staff reviewed each reason for visit with the patient and the provider; much of routine follow-up care was either deferred or changed to virtual. Patients without video capabilities (e.g., smartphone, internet connection, or familiarity with computer/phone software interface) were scheduled as telephone visits. At the end of the stay-at-home order, the mode of care was guided by a scheduling grid of visit types that were eligible for virtual care and then by the patient preference.
Retrospective Analysis of Patient Populations
A deidentified patient dataset was acquired from the Medical College Wisconsin & the Froedtert Health System consisting of 1,365,021 patients with ambulatory visits (inclusive of telemedicine). The medical system is one of two academic medical centers in Wisconsin. The medical system has more than 45 health centers and clinics with over 1.2 million patient visits in 2019.
We defined patients who accessed telemedicine services one or more times as the telemedicine group. Patients who did not accessed telemedicine but had one or more in-person visits were categorized into the in-person group. We identified 20,189 telemedicine patient users during the study period between March 1st, 2020, and August 31st, 2020. During this period, telemedicine services were encouraged to be utilized for nonemergent visits, though the in-person nonemergent services were still open for access with the note that routine care was systematically changed to telemedicine or deferred during the State of Wisconsin's Stay-At-Home order running from March 23, 2020 to May 13, 2020. The criterion for determining telemedicine users was by the patients' encounter information that was recorded in the EHR system. The telemedicine system had not been systematically deployed in the hospital until the COVID-19 pandemic. The data elements extracted from the EHR system included age, gender, race, ethnicity, ZIP code, and insurance status. The ZIP code was used to correlate patient information with socioeconomics information collected from census data.
Extracting Social Economics Data from Census Community Survey
The study area was in the Milwaukee, including the following counties: Jefferson, Kenosha, Milwaukee, Ozaukee, Racine, Walworth, Washington, and Waukesha. The study area is the primary service area of the hospital system, including eight counties. The study area includes a metropolitan area that has a diverse racial population (2.08 million residents), including 77.9% White, 13.8% Black, 2.4% Asian, and 5.9% other racial groups. About 9.2% of the population were Hispanic or Latino. Patients who did not reside in this area were excluded. The 126 ZIP codes of the counties were collected. The ZIP code was used to link the patient information to the Census American Community Survey (ACS) Community Survey 5-year estimate data. The census data elements used in this study included the median age, median income, White ratio, poverty rate, and college education ratio in the ZIP code areas.
Utilization Outcome and Variables
We used electronic health record data for analysis. Telehealth visits were either interactive video/audio (video, Group A ) or telephone-based (audio only, Group B ) depending on how patients access the telemedicine. If patients had both a video and an audio-only visit, they were included in both populations. If patients had an in-person visit but neither a video nor an audio-only visit, they were included in the in-person-only category. For each patient, we collected data including age, gender, race, ethnicity, insurance type, and ZIP code.
The telemedicine adoption rate (TAR) in each ZIP code of the SE Wisconsin region was assessed to determine the impacts of median income, poverty rate, White ratio, and college education ratio. The adoption rate was defined as the unique patients that used the telemedicine system from one of the eight counties during the study period. The TAR was calculated using the formula:
Eq. 1: Telemedicine adoption rate (TAR)
TAR = Total patients who used telemedicine in the ZIP area ÷ Total population in the ZIP area
Two types of TAR were calculated, including TAR(A) for the video users and TAR(B) for the telephone users.
Statistical Analysis
The telemedicine adoption patterns were analyzed across the social determinant factors for patients at the SE Wisconsin region. The telemedicine patient groups were compared with hospital patients who had in-person office visits. The telemedicine visit system was deployed in March 2020, at the beginning of the COVID-19 pandemic; telemedicine visits between March 1st, 2020 and August 31st, 2020 were analyzed. Patients who used telemedicine services were further divided by their telemedicine service types, video visit ( Group A ) and telephone visit ( Group B ). The time span for the comparison group (in-person visits: Group C ) was from January 1st, 2019, to August 31st, 2020. Group D was the population background of the study region collected from the ACS census data. In the comparison group, we included patients in 2019 to form a representative in-person cohort not affected by the challenges of the COVID-19 pandemic. Group A and Group B were compared with Group C in five aspects, including age, gender, race, insurance type, and ethnicity. Odds ratios (ORs) were used to compare the effect sizes between groups.
The impacts of social economic factors on TAR were analyzed on the ZIP code level within the eight counties of SE Wisconsin. This area is selected because the hospital system primarily serves these counties. Linear regression was first used to assess the individual correlation between the social determinants and TAR rates. Multiple regression analysis was then used to analyze the collective impact of the social determinant factors on the TAR rates.
The statistical tests and analyses were performed using statistical tool R (version 3.6.1), and p < 0.05 was used as a threshold to determine statistical significance. See Supplementary Appendix A (available in the online version) for details for statistical analysis. To visualize the geographic distribution of adoption, the adoption rates of the ZIP areas were represented on a map.
Results
Gaps in Adoption across the Patient Population
A total of 104,139 unique patients accessed telemedicine services between March 1st, 2020, and August 31st, 2020. In the baseline comparison group, 453,848 patients used in-person office visits from January 1st, 2019, to August 31st, 2020 ( Table 1 ). Patients who used the telemedicine platform were generally older compared with the health system patients (median age, Group A: 48.12 vs. Group B: 57.58 vs. Group C: 46.71, p < 0.001). The telephone user group was significantly older (median difference 11 years) than the in-person visit group (median 57.6 vs. 46.7 years old, p < 0.001), while the video visit group was slightly older than the in-person visit group.
Table 1. Comparison between telemedicine user groups with in-person visits.
| Group A: Telemedicine (Video) n = 57915 |
Group B: Virtual check-in (Telephone) n = 46,224 |
Group C: In-person visit n = 453,848 |
Group D: SE Wisconsin region ( n = 2,083,474) | Effect size Odds ratio: A vs. C (95% CI) |
Effect size Odds ratio: B vs. C (95% CI) |
|
|---|---|---|---|---|---|---|
| Age group | ||||||
| Median age | 48.12 | 57.58 | 46.71 | 47.1 | 0.06 (0.05,0.07) | 0.48 (0.40,0.49) |
| Gender | ||||||
| Female | 62.00% | 58.20% | 55.90% | 51.1% | 1.29 (1.27, 1.31) | 1.10 (1.08, 1.12) |
| Male | 38.00% | 41.80% | 44.10% | 48.9% | 0.78 (0.76, 0.79) | 0.91 (0.9, 0.93) |
| Race | ||||||
| White | 79.00% | 76.20% | 73.80% | 77.9% | 1.34 (1.31, 1.37) | 1.14 (1.11, 1.16) |
| Black | 12.90% | 18.40% | 14.70% | 13.8% | 0.86 (0.84, 0.88) | 1.31 (1.28, 1.35) |
| Asian | 2.00% | 1.40% | 2.50% | 2.4% | 0.79 (0.75, 0.84) | 0.55 (0.51, 0.60) |
| Other | 3.80% | 3.70% | 4.40% | 5.9% | 0.85 (0.81, 0.89) | 0.82 (0.78, 0.87) |
| Unknown | 2.40% | 0.30% | 4.70% | 0% | 0.5 (0.47, 0.53) | 0.07 (0.06, 0.08) |
| Insurance | ||||||
| Private | 65.00% | 56.60% | 56.50% | 57.2% | 1.43 (1.41, 1.46) | 1.00 (0.99, 1.02) |
| Public | 32.30% | 42.70% | 36.50% | 31.4% | 0.83 (0.82, 0.85) | 1.30 (1.27, 1.32) |
| Other | 1.20% | 0.30% | 0.60% | 3.6% | 1.90 (1.75, 2.06) | 0.47 (0.39, 0.55) |
| Self-funded | 0.10% | 0.10% | 0.60% | 7.7% | 0.08 (0.06, 0.12) | 0.16 (0.12, 0.21) |
| Ethnicity | ||||||
| Latino | 3.90% | 3.90% | 4.80% | 9.2% | 0.81 (0.77, 0.84) | 0.79 (0.75, 0.83) |
| Non-Latino | 93.60% | 95.80% | 91.00% | 90.8% | 1.46 (1.41, 1.51) | 2.28 (2.17, 2.39) |
| unknown | 2.40% | 0.30% | 4.20% | 0% | 0.57 (0.54, 0.60) | 0.07 (0.06, 0.09) |
The telemedicine users (both video and telephone groups) were significantly more likely to be female than male (Video OR: 1.29 Telephone: 1.10, p < 0.001). White patients were significantly more likely to use telemedicine services—both video (OR 1.34) and telephone (OR 1.14) groups compared with non-White groups. Black patients were less likely to use video visits (OR 0.86) and significantly more likely to use telephone visits (OR 1.31) compared with non-Blacks. Asian patients' usage rates were lower in both telemedicine modalities (Video OR 0.79, Telephone OR 0.55). Similarly, the Latino population TARs were also low (Video OR 0.75, Telephone OR 0.85) compared with non-Latinos.
The telemedicine patients who utilized video visits were significantly more likely to have private insurance (OR 1.43; 95% confidence interval or CI 1.41–1.46) than public insurance (OR 0.83; 95% CI 0.82–0.85), while the telephone users were more likely to use public insurance (OR 1.30; 95% CI 1.27–1.32) and less likely to be privately insured (OR 1.00; 95% CI 0.99–1.02).
Linear Regression Analysis
Among the analyzed ZIP code areas ( Table 2 , Fig. 1 ), the linear regression results showed that median income (coefficient 1.65, p < 0.001) and college education (coefficient 1.58, p < 0.001) had a significant positive correlation with video visits. Income and college education also had a positive correlation with telephone visits; however, the correlation was not statistically significant. The ZIP code areas' White population ratio had a positive correlation with video visits and a negative correlation with telephone visits.
Table 2. Linear regression modeling of the impact of social determinant factors for telemedicine usage across SE Wisconsin ZIP code areas.
| Coefficients | Median income | White ratio | College education | Median age |
|---|---|---|---|---|
| Video (Group A) | 1.65 ( p <0.001) | 0.16 ( p = 0.624) | 1.58 ( p <0.001) | 1.84 ( p = 0.11) |
| Telephone (Group B) | 0.50 ( p = 0.27) | −0.33 ( p = 0.245) | 0.57 ( p = 0.11) | 0.74 ( p = 0.45) |
Fig. 1.
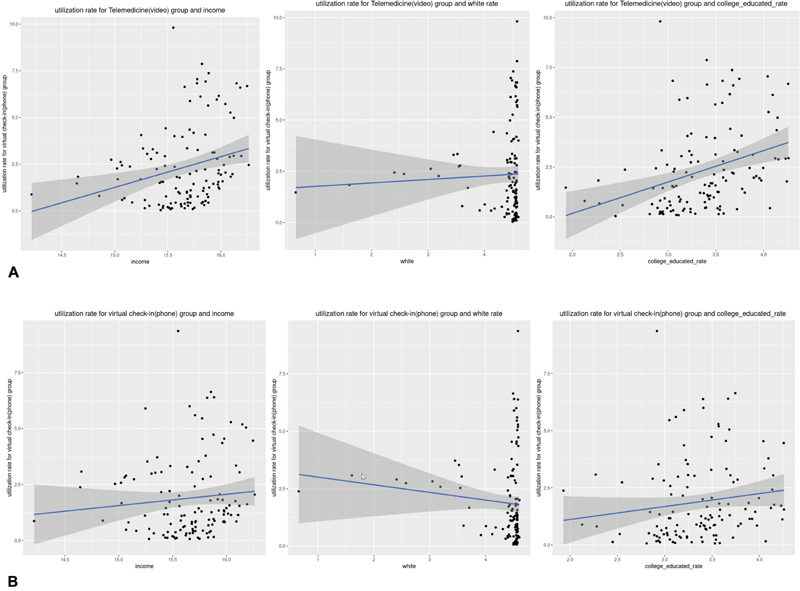
( A ) Video group, linear regression. ( B ) Telephone group, linear regression.
Multiple Regression Analysis
To analyze the correlated impact of the social determinant factors, a multiple regression analysis was conducted on the social determinant factors for the 126 ZIP code areas in the SE Wisconsin region. Table 3 shows the results—median age, median income (logarithmic transformed), White resident ratio, and college education were independent predictors for telemedicine use across the ZIP code areas. The college education rate had a strong correlation with video visits (coefficient 1.41, p = 0.01) in the multiple regression. The White ratio in the areas had a small negative correlation for both video and telephone visits (video coefficient −0.953, p < 0.05; phone coefficient −0.99, p < 0.01).
Table 3. Multiple regression modeling of the impact of social determinant factors for telemedicine usage across SE Wisconsin areas.
| Social determinant(log value) | Telemedicine groups | Coefficients | Std error | p -Value (Significance: “**” 0.01; “*” 0.05) |
|---|---|---|---|---|
| Median income | Video | 1.376 | 0.999 | 0.1711 |
| Phone | 0.601 | 0.8861 | 0.49895 | |
| White ratio | Video | −0.953 | 0.4204 | 0.0253* |
| Phone | −0.9955 | 0.3729 | 0.00867** | |
| College education rate | Video | 1.4196 | 0.5524 | 0.0114* |
| Phone | 0.7369 | 0.49 | 0.13529 | |
| Median age | Video | 0.096 | 1.6173 | 0.9529 |
| Phone | 0.8949 | 1.4345 | 0.05339 |
Geographic Distribution of TAR
To understand the preference of video and phone telemedicine access, the ratio of video and phone TAR was calculated for each ZIP code. The video utilization and phone utilization were documented in the patient encounters as a part of the electronic patient records. The video utilization versus phone utilization ratio is calculated by TAR (Video)/TAR(Phone) ( Fig. 2 left). Orange colors indicate higher level of video utilization and blue colors indicate higher level of phone utilization. The video and phone TAR ratio correlated with college education ( Fig. 3 right) ( p < 0.01). In this geographic area, higher college-education population was also positively associated with a higher median income with private insurance.
Fig. 2.
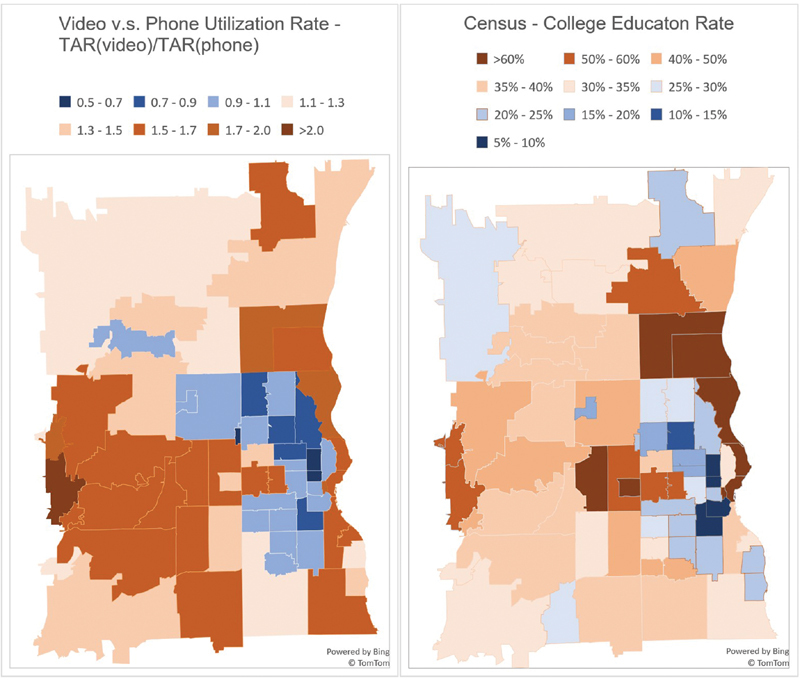
( Left ) The TAR ratio of video utilization versus phone utilization. ( Right ) Regional college education rate across ZIP. TAR, telemedicine adoption rate.
Fig. 3.
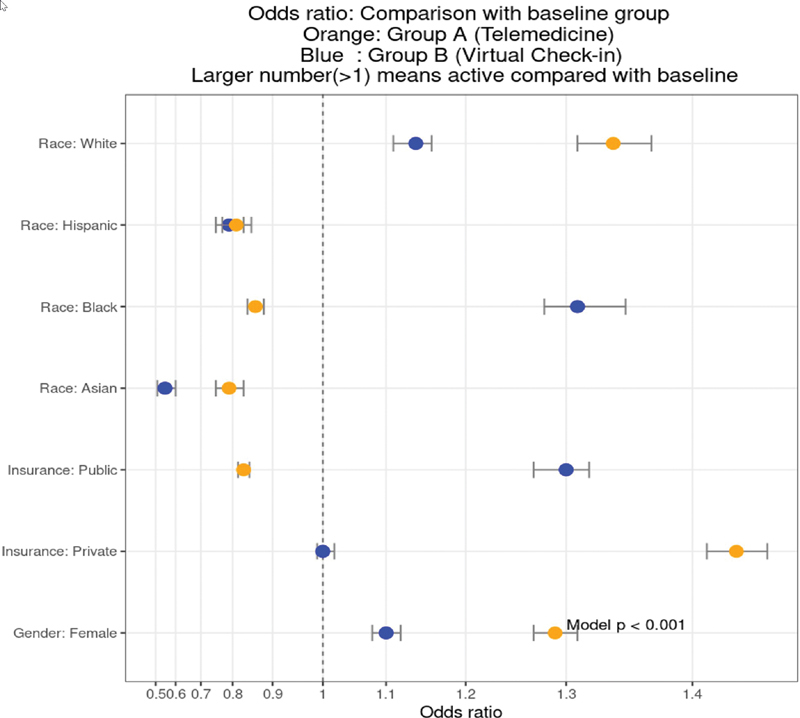
Comparing the odd ratios of telemedicine users. Baseline group: all in-person visits during January 01, 2019 to August 31, 2020. Video visit group: Patients accessed telemedicine services using multimedia video chat during March 01, 2020 to August 31, 2020. Telephone visit group: patients accessed telemedicine services using the telephone during March 01, 2020 to August 31, 2020.
Discussion
At the onset of COVID-19 pandemics, many health care systems quickly deployed telemedicine technologies to address the need for remote visits of health services. For example, Washington State was the first state in the United States that encountered with COVID patients. UW Medicine system shared their experience of the rapid rollout of a telehealth system to support their clinical response of the pandemic. 27 Knighton et al 28 reported the implementation of a telehealth system in an integrated community-based health care setting. The system leveraged the Center for Disease Control and Prevention Pandemic Interval Framework to create a multimodal technology platform. To monitor patients diagnosed with COVID remotely, many systems including this one 29 and the Mass General Brigham health system used remote patient monitoring. 30 in the MGB study; RPM reduced readmission for patients with COVID and provide scalable services upon discharge. While this study focused on ambulatory care, notably this system and many others also used inpatient telemedicine services to reduce PPE needs and support infection control. For example, Ong et al 31 studied the use of optional devices to support inpatient telehealth services across seven hospitals. The investigators discovered that large-scale distribution of consumer-grade devices was feasible and useful for inpatient telehealth services.
Despite the fast growth of telemedicine applications, socioeconomic factors that affect the access and adoption of telemedicine have not been well-studied. The recent impact of COVID-19 spurred a wave of deployment and adoption of telemedicine systems in hospital systems. It is critical to understand how social determinants of health could affect access to health care through telemedicine. Rodriguez et al have also identified demographic differences alongside age, race, language, and broadband access as drivers for using video visits. Further, they identified that practice and clinician variability accounted for more variation in choice of modality than patient. 32 Ortega et al 33 reviewed policy changes and outlined important recommendations that health system can adopt to improve telemedicine for the underserved patients. Our study specifically investigated the social economics disparities of telemedicine usages among patients in the SE Wisconsin areas.
In the studied health system, we saw that older patients were more likely to use telemedicine services, possibly reflecting the concerns they had around COVID-19 risk. At the same time, research has demonstrated that older patients are less likely to be prepared for telemedicine care, 34 whether by video or by telephone, and thus further attention should be paid to understanding access and difficulty accessing virtual services. We also saw a significantly higher proportion of female telemedicine users in both video and telephone groups. The gap of adoption between male patients and female patients was noticeably large (Video: 38.0 vs. 62.0%; Telephone: 41.8 vs. 58.2%) compared with normal hospital visits (44.1% male vs. 55.9% female). One possible explanation for the gap is that men are less concerned about COVID-19. 35 A recent Reuter-Ipsos survey showed 54% of women were “very concerned” about the coronavirus while only 45% of men were concerned. 36 Women are also much more likely to take action to modify their daily routines to reduce chances of infections, such as using disinfectants and practicing social distancing. In general, women also more commonly take the “care manager” role in a family. 37 The impact of COVID-19 on the elderly and children could be more alarming to women. Therefore, women are more supportive than men in some strict measures, 38 such as closing schools, banning public gatherings, and stopping transportation. This could explain the use of greater use of telemedicine instead of in-person visits during COVID-19 by women. Some studies have also suggested that men have a higher mortality rate compared with women if infected by coronavirus. 39 40 However, our study shows that the higher risk did not lead to higher telemedicine utilization. A recent study performed an analysis of 7,742 family medicine encounters and compared telehealth users with in-person visits. 41 This study also discovered a higher usage rate among women. The gender gap in telemedicine adoption indicates the need to understand the hesitancy among men to utilize virtual visits and develop strategies to mitigate potential barriers.
Analysis of data showed that White patients had a higher odd ratio of using telemedicine for both video visits (OR: 1.34; 95% CI 1.31–1.37) and telephone visits (OR: 1.14; CI 1.11–1.16) when compared with minorities; while Black patients had a lower OR for video visits (OR:0.86; CI 0.84–0.88) and higher ratio for telephone visits (OR: 1.31; CI 1.28–1.35) when compared with non-Black. The racial gap for video visit-based telemedicine adoption was significant ( p < 0.001) for Black patients. Hispanic telemedicine users only consisted of 3.9% of the patients for both video visits (OR: 0.81; CI 0.77–0.84) and telephone visits (OR: 0.79; CI 0.75–0.83), which is lower than the representations of the health system (3.9 vs. 4.8%). Similarly, Asian patients also have a lower adoption rate in video visits (OR: 0.79; CI 0.75–0.84) and phone visits (OR: 0.55; CI 0.51–0.60). These results indicated that minority patients could have challenges in adopting telemedicine services. However, the barriers that led to such disparities in telemedicine adoption were not clearly studied. One potential explanation is the effect of the “digital divide.” Lorence et al examined how racial and ethnic factors could associate with online health information search. 42 They discovered a wide gap between White and Black and between White and Hispanic patients for online health information searches. More recently, other studies also showed that the digital divide in health-related technology usage also occurred in older adults of Black and Hispanic origin compared with White, including online access of the health record. 43 44 45 Most of the video-based telemedicine platforms require the patients to access the services through computers or smartphones. The digital divide could lead to the lagging adoption of telemedicine in Black and Hispanic patients. As policymakers consider future coverage of telemedicine services, ongoing coverage for telephone-based visits will help reduce the access disparities. Additionally, infrastructure in communities to support high-speed internet access and connection reliability, including broadband and/or municipal wi-fi networks and stations, may also improve access for disadvantaged populations.
Private insurance significantly correlated with video TAR (Video OR: 1.43; Telephone OR: 1.00); public insurance negatively correlated with the video TAR (OR: 0.83; CI 0.82–0.85) but positively correlated with telephone TAR (OR: 1.30; CI 1.27–1.32). Patients with private insurance generally are younger and have a better income than patients with public insurance. This can be confirmed by the median age of the telemedicine users (Video: 48.1 vs. Telephone: 57.5). The telephone telemedicine users were much older than the video users. It is possible that younger patients adopt technology better than older patients. Unlike younger patients, who are more familiar with using computers, smartphones, and video chat, older patients could potentially need more assistance in video telemedicine visits. However, providing such technical assistance remotely in a patient-friendly manner is a challenge during the COVID-19 pandemic. This could create a significant barrier for older patients to access advanced telehealth services.
We also attempted to analyze the impacts of social determinant factors in telemedicine adoption in the SE Wisconsin region. In the linear regression analysis ( Table 2 , Fig. 1 A–F ), we identified that the median income and college education rate had a positive correlation with the TAR in the ZIP areas. The impact of social determinant factors was more significant for the video visits group. For every 1% increase in median income, the video TAR rate increased 1.65% ( p < 0.001). Similarly, there was a 1.58% increase in video visits TAR for every 1% increase in the college education rate ( p < 0.001). Median income and college education also could have a positive impact on telephone TAR; however, the statistical test was not significant. Multiple regression analysis was used to determine the predictors' collective effects on telemedicine use. In the multiple regression analyses, the college education rate still had a significant positive correlation with video visits. White ratio became negatively correlated with telemedicine adoption in the multiple regression analyses in video and phone visit, although the coefficients were not very high. This result confirms that college education rate within the ZIP code areas is a key predictor for increased adoption of telemedicine in the SE Wisconsin area. There are many possible explanations for lower TARs among disadvantaged populations such as lack of insurance coverage, limited access to high-speed internet or smartphone, lower health technology literacy, poorer health communication skills, and less control of work/home life. This study could not uncover the underlying driving factors; rather, our analyses showed the inequality in telemedicine adaptation, which is closely linked to social determinant factors.
There are a few potential limitations to this study. Like other social determinant studies, we did not collect individual patient's income information, and the median income in a ZIP code was used as an estimate of patient income. Second, the patient cohort in this study represents a regional hospital system. Milwaukee is one of the cities with the highest racial segregation score in the United States (U.S.) according to the racial segregation in U.S. study 46 ; therefore, the patient characteristics may not be representative of other health care systems and areas. Third, this study focused on a few key social determinant factors. There are several potential factors that could be considered for future studies, including environmental and cultural factors. This study was intended to uncover potential gaps in the adoption of telemedicine and serve as a template to encourage more research in this area. Fourth, the pandemic could impact different health service types (e.g., cancer treatment, chronic condition management, laboratory services, pharmacy services) in very different ways. Lastly, we did not include clinical conditions or problems in this dataset; it is possible, for example, that older patients used more telemedicine services simply because they had a higher level of illness and needed more services. Studying how telemedicine could be deployed to address the needs of different health services will be our future study.
Conclusion
We observed significant disparities among patients in telemedicine adoption during the COVID-19 pandemic associated with gender, race, income, education, and insurance type. More studies are needed to investigate causal relationships between the underlying factors and telemedicine utilization. This study adds to literature that shows that telemedicine may not expand access to care services for underserved populations without special attention. With the growing deployment of telemedicine services, specific strategies are needed to uncover and address barriers to telemedicine adoption in underserved patient populations.
Clinical Relevance Statement
Telemedicine has been widely deployed in health systems during the COVID-19 pandemic. This study quantified the impact of socioeconomic determinants factors to telehealth adoption. This study reveals gaps and challenges in adopting telemedicine in disadvantage groups, which is crucial to develop strategies to improve telehealth adoption.
Multiple Choice Questions
-
Why patients choose telemedicine for health care?
Remote access to health services.
Test internet quality and connection.
Reduce workload of doctors.
Connect with families.
Correct Answer: The correct answer is option a. Patients use telemedicine services to access health service remotely.
-
Which is a barrier for telemedicine adoption?
Improved user interface.
Increased internet speed.
Reduced digital divide.
Increased service waiting time.
Correct Answer: The correct answer is option d. Increased service waiting time will be a barrier for telemedicine adoption because patients expect to access health services through telemedicine in a more efficient way than traditional in-person visits.
Conflict of Interest None declared.
Protection of Human and Animal Subjects
No human subjects were involved in the project. De-identified patient data was used.
Supplementary Material
References
- 1.Perednia D A, Allen A. Telemedicine technology and clinical applications. JAMA. 1995;273(06):483–488. [PubMed] [Google Scholar]
- 2.Wootton R, Craig J, Patterson V. London: CRC Press; 2017. Introduction to Telemedicine. [Google Scholar]
- 3.Hjelm N M. Benefits and drawbacks of telemedicine. J Telemed Telecare. 2005;11(02):60–70. doi: 10.1258/1357633053499886. [DOI] [PubMed] [Google Scholar]
- 4.Hailey D, Roine R, Ohinmaa A. Systematic review of evidence for the benefits of telemedicine. J Telemed Telecare. 2002;8 01:1–30. doi: 10.1258/1357633021937604. [DOI] [PubMed] [Google Scholar]
- 5.Moffatt J J, Eley D S. The reported benefits of telehealth for rural Australians. Aust Health Rev. 2010;34(03):276–281. doi: 10.1071/AH09794. [DOI] [PubMed] [Google Scholar]
- 6.Smith A C, Bensink M, Armfield N, Stillman J, Caffery L. Telemedicine and rural health care applications. J Postgrad Med. 2005;51(04):286–293. [PubMed] [Google Scholar]
- 7.Bagchi S. Telemedicine in rural India. PLoS Med. 2006;3(03):e82. doi: 10.1371/journal.pmed.0030082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heath B, Salerno R, Hopkins A, Hertzig J, Caputo M. Pediatric critical care telemedicine in rural underserved emergency departments. Pediatr Crit Care Med. 2009;10(05):588–591. doi: 10.1097/PCC.0b013e3181a63eac. [DOI] [PubMed] [Google Scholar]
- 9.Whole System Demonstrator evaluation team . Henderson C, Knapp M, Fernández J-L. Cost effectiveness of telehealth for patients with long term conditions (Whole Systems Demonstrator telehealth questionnaire study): nested economic evaluation in a pragmatic, cluster randomised controlled trial. BMJ. 2013;346:f1035. doi: 10.1136/bmj.f1035. [DOI] [PubMed] [Google Scholar]
- 10.Lindgren S, Wacker D, Suess A. Telehealth and autism: treating challenging behavior at lower cost. Pediatrics. 2016;137 02:S167–S175. doi: 10.1542/peds.2015-2851O. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hofstetter P J, Kokesh J, Ferguson A S, Hood L J. The impact of telehealth on wait time for ENT specialty care. Telemed J E Health. 2010;16(05):551–556. doi: 10.1089/tmj.2009.0142. [DOI] [PubMed] [Google Scholar]
- 12.Mair F, Whitten P.Systematic review of studies of patient satisfaction with telemedicine BMJ 2000320(7248):1517–1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kruse C S, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(08):e016242. doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Srinivasan R, Ben-Pazi H, Dekker M. Telemedicine for hyperkinetic movement disorders. Tremor Other Hyperkinet Mov (N Y) 2020;10:10. doi: 10.7916/tohm.v0.698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koceska N, Koceski S, Beomonte Zobel P, Trajkovik V, Garcia N. A telemedicine robot system for assisted and independent living. Sensors (Basel) 2019;19(04):834. doi: 10.3390/s19040834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marcin J P, Ellis J, Mawis R, Nagrampa E, Nesbitt T S, Dimand R J.Using telemedicine to provide pediatric subspecialty care to children with special health care needs in an underserved rural community Pediatrics 2004113(1 Pt 1):1–6. [DOI] [PubMed] [Google Scholar]
- 17.James H E. Pediatric neurosurgery telemedicine clinics: a model to provide care to geographically underserved areas of the United States and its territories. J Neurosurg Pediatr. 2016;25(06):753–757. doi: 10.3171/2016.6.PEDS16202. [DOI] [PubMed] [Google Scholar]
- 18.Fox N, Hirsch-Allen A J, Goodfellow E. The impact of a telemedicine monitoring system on positive airway pressure adherence in patients with obstructive sleep apnea: a randomized controlled trial. Sleep (Basel) 2012;35(04):477–481. doi: 10.5665/sleep.1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Whitehouse C R, Long J A, Maloney L M, Daniels K, Horowitz D A, Bowles K H. Feasibility of diabetes self-management telehealth education for older adults during transitions in care. Res Gerontol Nurs. 2020;13(03):138–145. doi: 10.3928/19404921-20191210-03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edwards L, Thomas C, Gregory A. Are people with chronic diseases interested in using telehealth? A cross-sectional postal survey. J Med Internet Res. 2014;16(05):e123. doi: 10.2196/jmir.3257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hollander J E, Carr B G. Virtually perfect? Telemedicine for COVID-19. N Engl J Med. 2020;382(18):1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 22.Ohannessian R, Duong T A, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill. 2020;6(02):e18810. doi: 10.2196/18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Portnoy J, Waller M, Elliott T. Telemedicine in the Era of COVID-19. J Allergy Clin Immunol Pract. 2020;8(05):1489–1491. doi: 10.1016/j.jaip.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.CDC Center for Disease Control and Prevention: Prepare your practice for COVID-19 2020. Accessed June 1st, 2020 at:https://www.cdc.gov/coronavirus/2019-ncov/hcp/preparedness-resources.html
- 25.HRSA Coronavirus Disease (COVID-19) Frequently Asked Questions 2020. Accessed June 1st, 2020 at:https://www.hrsa.gov/rural-health/coronavirus/frequently-asked-questions#telehealth
- 26.Prevention OoD. Promotion H. Healthy people 2030 framework; 2019. Accessed June 3, 2019 at:https://www.healthypeople.gov/2020/About-Healthy-People/Development-Healthy-People-2030/Framework
- 27.Grange E S, Neil E J, Stoffel M. Responding to COVID-19: the UW medicine information technology services experience. Appl Clin Inform. 2020;11(02):265–275. doi: 10.1055/s-0040-1709715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Knighton A J, Ranade-Kharkar P, Brunisholz K D. Rapid implementation of a complex, multimodal technology response to COVID-19 at an integrated community-based health care system. Appl Clin Inform. 2020;11(05):825–838. doi: 10.1055/s-0040-1719179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Crotty B.Caring for Covid: Our Strategy For Home-Based Connected Care. Accessed July 2020 athttps://medium.com/inception-health/caring-for-covid-how-digital-makes-it-possible-to-take-care-of-more-people-at-home-481771230509
- 30.Gordon W J, Henderson D, DeSharone A. Remote patient monitoring program for hospital discharged COVID-19 patients. Appl Clin Inform. 2020;11(05):792–801. doi: 10.1055/s-0040-1721039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ong S Y, Stump L, Zawalich M. Inpatient telehealth tools to enhance communication and decrease personal protective equipment consumption during disaster situations: a case study during the COVID-19 pandemic. Appl Clin Inform. 2020;11(05):733–741. doi: 10.1055/s-0040-1719180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rodriguez J A, Betancourt J R, Sequist T D, Ganguli I. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am J Manag Care. 2021;27(01):21–26. doi: 10.37765/ajmc.2021.88573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ortega G, Rodriguez J A, Maurer L R. Telemedicine, COVID-19, and disparities: policy implications. Health Policy Technol. 2020;9(03):368–371. doi: 10.1016/j.hlpt.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lam K, Lu A D, Shi Y, Covinsky K E. Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Intern Med. 2020;180(10):1389–1391. doi: 10.1001/jamainternmed.2020.2671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Thelwall M, Thelwall S.COVID-19 tweeting in English: gender differencesarXiv preprint arXiv:2003.11090.2020
- 36.Reuters U.S. men less likely to heed health warnings as coronavirus death toll mounts: Reuters PollAccessed June 1st, 2020 at:https://www.reuters.com/article/us-health-coronavirus-gender-poll/u-s-men-less-likely-to-heed-health-warnings-as-coronavirus-death-toll-mounts-reuters-poll-idUSKBN21E1C9
- 37.Guberman N, Maheu P, Maillé C. Women as family caregivers: why do they care? Gerontologist. 1992;32(05):607–617. doi: 10.1093/geront/32.5.607. [DOI] [PubMed] [Google Scholar]
- 38.Galasso V, Pons V, Profeta P, Becher M, Brouard S, Foucault M. Gender differences in COVID-19 attitudes and behavior: panel evidence from eight countries. Proc Natl Acad Sci U S A. 2020;117(44):27285–27291. doi: 10.1073/pnas.2012520117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jin J-M, Bai P, He W. Gender differences in patients with COVID-19: focus on severity and mortality. Front Public Health. 2020;8:152. doi: 10.3389/fpubh.2020.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gender and COVID-19 Working Group Wenham C, Smith J, Morgan R.COVID-19: the gendered impacts of the outbreak Lancet 2020395(10227):846–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pierce R P, Stevermer J J. Disparities in use of telehealth at the onset of the COVID-19 public health emergency. J Telemed Telecare. 2020:X20963893. doi: 10.1177/1357633X20963893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lorence D P, Park H, Fox S. Racial disparities in health information access: resilience of the Digital Divide. J Med Syst. 2006;30(04):241–249. doi: 10.1007/s10916-005-9003-y. [DOI] [PubMed] [Google Scholar]
- 43.Mitchell U A, Chebli P G, Ruggiero L, Muramatsu N. The digital divide in health-related technology use: the significance of race/ethnicity. Gerontologist. 2019;59(01):6–14. doi: 10.1093/geront/gny138. [DOI] [PubMed] [Google Scholar]
- 44.Ghaddar S, Vatcheva K P, Alvarado S G, Mykyta L. Understanding the intention to use telehealth services in underserved Hispanic border communities: cross-sectional study. J Med Internet Res. 2020;22(09):e21012. doi: 10.2196/21012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Crotty B H, Winn A N, Asan O, Nagavally S, Walker R J, Egede L E. Clinician encouragement and online health record usage. J Gen Intern Med. 2019;34(11):2345–2347. doi: 10.1007/s11606-019-05162-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Frey W H, Myers D. Racial segregation in US metropolitan areas and cities, 1990–2000: patterns, trends, and explanations. Population Stud Center Res Rep. 2005;5:573. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


