Abstract
Background
Excessive worry is a common phenomenon. Our research group has previously developed an online intervention for excessive worry based on operant principles of extinction (IbET; internet-based extinction therapy) and tested it against a waiting-list. The aim of this study was to evaluate IbET against an active control comparator (CTRL).
Methods
A 10-week parallel participant blind randomised controlled trial with health-economical evaluation and mediation analyses. Participants (N = 311) were randomised (ratio 4.5:4.5:1) to IbET, to CTRL (an internet-based stress-management training program) or to waiting-list. The nation-wide trial included self-referred adults with excessive worry. The primary outcome was change in worry assessed with the Penn State Worry Questionnaire from baseline to 10 weeks.
Results
IbET had greater reductions in worry compared to CTRL [−3.6 point difference, (95% CI −2.4 to −4.9)] and also a significantly larger degree of treatment responders [63% v. 51%; risk ratio = 1.24 (95% CI 1.01–1.53)]. Both IbET and CTRL made large reductions in worry compared to waiting-list and effects were sustained up to 1 year. Treatment credibility, therapist attention, compliance and working alliance were equal between IbET and CTRL. Data attrition was 4% at the primary endpoint. The effects of IbET were mediated by the hypothesized causal mechanism (reduced thought suppression) but not by competing mediators. Health-economical evaluation indicated that IbET had a 99% chance of being cost-effective compared to CTRL given societal willingness to pay of 1000€.
Conclusions
IbET is more effective than active comparator to treat excessive worry. Replication and extensions to real-world setting are warranted.
Key words: Cognitive behaviour therapy, cost-effectiveness, exposure, internet, mediation, worry
Introduction
Many clinicians meet patients with excessive worry in everyday practice. Worry is the core symptom of generalized anxiety disorder (GAD), which accounts for 50% of all primary care visits by patients with an anxiety disorder (Wittchen & Hoyer, 2001). Additionally, 4–6% of primary care patients present with subthreshold symptoms of GAD (Haller, Cramer, Lauche, Gass, & Dobos, 2014; Wittchen & Hoyer, 2001). This warrants attention as GAD and subthreshold GAD lead to equal levels of distress and psychosocial impairment (Haller et al., 2014). Other mental health conditions such as obsessive-compulsive disorder (OCD), social anxiety disorder (SAD), insomnia and panic disorder (PD) also include excessive worry in the symptom presentation (American Psychiatric Association, 2013) and, as in the case of GAD, there is a large additional subclinical population further contributing to the societal burden (Batelaan et al., 2007; Cuijpers & Smit, 2004; de Bruijn, Beun, de Graaf, ten Have, & Denys, 2010; Fehm, Beesdo, Jacobi, & Fiedler, 2008; Sarsour, Kalsekar, Swindle, Foley, & Walsh, 2011). Recent research has also shown that worry might be a causal mechanism of persecutory delusions (Freeman et al., 2015). Altogether, worry-related problems add up to a considerable challenge for healthcare.
Psychological treatments, and especially different forms of disorder-specific cognitive behaviour therapy (CBT), have been shown to be effective for a range of different mental health conditions (Hofmann & Smits, 2008); unfortunately, it is difficult to implement and scale these disorder-specific treatments to meet the increasing need in healthcare. One possible solution to this problem may be to develop scalable treatments that target specific psychopathological processes shared by a number of different mental health conditions (Craske, 2012). This strategy has been endorsed by the National Institute of Mental Health (NIMH) initiative Research Domain Criteria (RDoC) as a way to improve diagnostics and treatment of psychiatric disorders (Cuthbert & Insel, 2013; Insel & Gogtay, 2014). Our research group recently developed and evaluated a novel online intervention which uses principles of operant conditioning to target worry. More specifically, the treatment (IbET; internet-based extinction therapy) hypothesises that worry is maintained by excessive use of comforting thoughts, and the main intervention in this treatment is therefore exposure to the feared catastrophic thoughts using operant blocking techniques. IbET targets worry irrespective of principal diagnosis, and the online format, with limited therapist resource use, also removes many logistical barriers for both the patient and the healthcare provider (Andersson & Titov, 2014). Although IbET has been shown to be superior to a waiting-list with large controlled effect sizes in a randomised trial (Andersson et al., 2017), this treatment has not yet been tested against an active comparator controlling for non-specific treatment factors such as therapist attention, number of completed modules, treatment credibility or therapeutic alliance (Gold et al., 2017; Mulder, Murray, & Rucklidge, 2017). Consequently, the aim of the present trial was to test IbET against a credible comparator in a rigorously designed trial. We hypothesised that IbET would be more effective and cost-effective than both active comparator and a waiting-list in reducing worry. We also performed a mediation analysis to investigate whether IbET achieves its effects through the hypothesised pathway by decreasing thought suppression
Method
Trial design
This study was a superiority trial conducted at the Karolinska Institutet, Sweden, between December 2015 and May 2017. Ninety percent of the participants were randomly assigned to 10 weeks of IbET (n = 140) or to an active control comparator (CTRL, n = 140) which consisted of an internet-based stress-management program. Ten percent of the participants (n = 31) were randomised to a waiting-list condition in order to replicate previous findings (Andersson et al., 2017) and to control for spontaneous improvements. The primary endpoint was set to 10 weeks (i.e. directly post-treatment). Long-term follow-ups were also conducted at 4- and 12-months post-treatment. Participants randomised to the waiting-list were offered active treatment after the initial 10 weeks (IbET or CTRL; data is not reported here). The regional ethical review board in Stockholm approved the protocol (registration ID: 2015/1698-31/1) and the trial was registered at ClinicalTrials.gov registration ID: NCT02638792. The study is reported in accordance with the CONSORT statement for nonpharmacological treatments. Further details about the study methods below are shown in the online supplement.
Participants
Eligible participants were individuals with access to the internet, aged 18 or over, with excessive worry defined as a score >56 on the Penn State Worry Questionnaire (Meyer, Miller, Metzger, & Borkovec, 1990). Exclusion criteria were: (a) substance dependence in the last 6 months; (b) post-traumatic stress disorder, bipolar disorder or psychosis; (c) severe comorbid psychiatric disorder that could jeopardize treatment participation (e.g. axis II borderline personality disorder with self-harm); (d) moderate-to-severe depression (defined as a score >25 on the Montgomery Åsberg Depression Rating Scale – Self report; Svanborg and Asberg, 2001); (e) psychotropic medication changes within 2 months prior to enrolment and (f) completed CBT for worry within the last 2 years. Participants who were taking psychotropic medication with stable dose for at least 2 months prior to enrolment were asked to keep their dose stable during the 10-week trial period. Parallel psychological treatment was not allowed during the trial period. After description of the study to the subjects, written informed consent was obtained.
Recruitment and determination of eligibility
Residents in all of Sweden could register for the study. Flyers were distributed to psychiatrists and general practitioners throughout Sweden with information about the study and the trial was also advertised in national newspapers and social media. Applicants registered their interest on the study's secure website and completed an online screening consisting of the PSWQ, the MADRS-S, Alcohol Use Disorders Identification Test (Saunders, Aasland, Babor, de la Fuente, and Grant, 1993), Drug User Disorders Identification Test (Berman, Bergman, Palmstierna, and Schlyter, 2005) and general background information. Applicants who scored ⩽56 on the PSWQ or >25 on the MADRS-S were excluded from the study. Potentially eligible participants underwent a structured diagnostic interview (using the Mini-International Neuropsychiatric Interview; MINI; Sheehan et al., 1998) with a clinical psychologist or with a trained student in the final semester of a 5-year clinical psychology programme. The interviews were conducted over the telephone, which is a reliable administration format for structured psychiatric assessments (Rohde, Lewinsohn, & Seeley, 1997). All assessors had received extensive training in structured diagnostic interviews [in total 20 60-min examinations on real patients or actors using the MINI (all difficult cases with multiple diagnoses) and at least four months full-time internship]. To ensure the reliability of the diagnostic procedure and eligibility criteria, the principal investigator reviewed each case (and in some cases telephoned participants for additional assessment) and made the final decision on enrolment.
Interventions
General description of the two active treatments
The two active treatments (IbET and CTRL) were delivered via a secure online platform using a two-factor authentication to guarantee participant confidentiality. The treatment was divided in eight modules (book chapters) spanning over 10 weeks. In order to progress to the next module, the participant had to complete a number of homework assignments such as reading text material, answering a quiz at the end of each module, filling out worksheets and report treatment progression to the therapist. Each participant had contact with an identified therapist throughout the entire treatment using a built-in messaging system in the online platform.
Internet-based extinction therapy
The IbET treatment is based on a model where excessive worry is explained as an operant process consisting of the interplay between two types of cognitions: catastrophic thoughts and comforting thoughts (Andersson et al., 2017; Wadström, 2015). Catastrophic thoughts are defined as intrusive and anxiety provoking thoughts about uncertain future or past events e.g. ‘did I come across as a complete idiot during the meeting?’, or ‘what if my son is hit by a car?!’. Comforting thoughts are defined as thoughts with the primary function of relieving the discomfort evoked by the catastrophic thoughts e.g. ‘no, you looked great at the meeting!’, or ‘no, he will be fine!’. Comforting thoughts have a short-term rewarding function offering temporary relief and thereby reinforcing the catastrophic thoughts. Through this reinforcement, the worrier gets stuck moving back and forth between catastrophic- and comforting thoughts (catastrophic thought → comforting thought → temporary relief → new catastrophic thought and so on). In the IbET treatment, the patient is instructed to use competing responses incompatible with thinking comforting thoughts, thereby extinguishing the reinforcement of the catastrophic thought.
Active control comparator
The CTRL treatment was designed to (a) be perceived as equally credible as IbET, (b) promote structured behaviour change with the purpose of reducing worry and (c) to be equal to IbET in ability to establish therapeutic alliance and amount of therapist attention provided. The CTRL treatment consisted of an internet-based stress-management intervention where the main treatment component is applied relaxation which is a recommended treatment for worry/GAD according to NICE guidelines (National Institute for Health & Care Excellence, 2011). In the CTRL treatment, the patient was introduced to a coping model of worry where the main aim is to take control over the worry through relaxation techniques. Thus, a fundamental difference compared with the IbET treatment was that the CTRL treatment specifically instructed the patients to use relaxation exercises as a strict means of coping with worry and as a self-regulation strategy, which is theoretically the opposite to IbET. The CTRL treatment also incorporated regular relaxation practise on a daily basis. There were no content or instructions regarding extinction-based techniques in the CTRL treatment.
Waiting-list
Participants randomised to the waiting-list were informed that they would receive delayed treatment and were given an emergency number in case of acute worsening of symptoms. None of the data collected from the waiting-list participants were used after the primary endpoint (10 weeks).
Power calculation
The power calculation to test differences between IbET and CTRL was based on the previous trial by our research group (Andersson et al., 2017) and other trials testing stress management techniques (Hedman et al., 2014a; Ljotsson et al., 2011). Given 90% power (two-sided alpha test), the study was powered to detect a small between-group effect size (d = 0.4) rendering a sample size of 140 participants (accounting for ~5% data attrition) in each active treatment group. The power calculation between IbET and waiting-list was based on the lower bound of 95% confidence intervals obtained from our previous trial (d = 1.0) (Andersson et al., 2017) and in the present trial rendering a sample size of 31 participants. There were no interim analyses or rules for stopping in the current study.
Randomisation and masking
Participants were randomised, using simple randomisation with no constraints, by an independent party (using www.random.org) on a 4.5:4.5:1 ratio (140 participants to IbET, 140 participants to CTRL, 31 participants to waiting-list). Participants who received IbET/CTRL were also randomised to one of 10 therapists. To control for therapist effects, all therapists treated an equal number of participants in the two active treatment conditions (14 in each group; in total 28 participants per therapist). In order to control for performance bias, participants were blinded to the two active treatment conditions i.e. participants were informed that they would receive one of two internet-based treatments that had previously been shown to be effective. There was no detailed information about the IbET/CTRL treatment components nor the trial superiority hypothesis. All participants were randomised after formal inclusion in the study in order to ensure allocation concealment. Treatment started within 48 h after randomisation and participants received information how to log into the secure online platform immediately after randomisation. As in all studies of psychological therapies, the treating therapists were not blinded to treatment. Participants randomised to waiting-list were told that they would receive one of the two internet-based treatments after 10 weeks i.e., participants randomised to waiting-list were not blinded to allocation.
Assessment points and outcomes
Participants were assessed with the primary outcome measure at baseline, weekly during treatment and after 10 weeks (primary endpoint). Long-term follow-up was also conducted 4- and 12-months post-treatment (the waiting-list was excluded from long-term follow-up after crossover).
The primary outcome was the PSWQ, which is regarded as the gold standard in assessment of worry severity (Meyer et al., 1990). Responder status was defined as ⩾9 points reduction on the PSWQ from baseline to post-treatment (Stanley et al., 2009). Cognitive avoidance was measured using the Cognitive Avoidance Questionnaire (CAQ; Sexton and Dugas, 2008). Depressive symptoms were assessed using the MADRS-S (Svanborg & Asberg, 2001). Intolerance of uncertainty symptoms was assessed using the Intolerance of Uncertainty Scale (IUS; Buhr and Dugas, 2002). Quality of life was assessed using the Brunnsviken Brief Quality of life Questionnaire (BBQ; Lindner et al., 2016). The number of adverse events was assessed week 3, 8 and at post-treatment using a self-report questionnaire which has been used in a previous trial with similar results to face-to-face interviews (Andersson et al., 2015). Participants were encouraged to notify the study personnel if there were any deviations in the study protocol regarding the change (or start) of pharmacological or psychological treatments during treatment. If the clinician was notified of any deviations of medication changes during treatment, this was documented in the digital case report form. All participants were systematically asked at post-treatment if they had made any changes in medication or sought other psychological treatment during the 10-week period. All secondary outcomes (i.e. CAQ, MADRS-S, IUS and BBQ) were assessed at baseline, post-treatment and at 4- and 12-month follow-up. The non-specific factors treatment credibility and therapeutic alliance were measured using the Treatment Credibility scale (Borkovec & Nau, 1972; week 3) and the Working Alliance Inventory (Tracey & Kokotovic, 1989; week 5) respectively. Therapist time per patient and amount of messages were logged by the online platform.
In order to investigate mediators of treatment response, participants were assessed weekly using the thought suppression subscale of the CAQ, the self-regulation subscale of the Multidimensional Assessment of Interoceptive Awareness (MAIA; Mehling et al., 2012) and the Patient Health Questionnaire-2 (PHQ-2; Arroll et al., 2010) which measures depressive symptoms. Theoretically, a decrease in thought suppression should mediate the treatment effects between IbET and CTRL (the main focus in IbET is to reduce thought suppression through operant extinction techniques) but not self-regulation (which is rather the main treatment component in the CTRL group), nor depressive symptoms. Thus, the hypothesised mediator of effect was change in thought suppression and the competing control mediators were changes in self-regulation and depressive symptoms.
In addition to efficacy and mediation analyses, we conducted a cost-effectiveness analysis of the IbET intervention using the Trimbos/iMTA questionnaire for Costs associated with Psychiatric illness (TIC-P; Hakkaart-van Roijen and Donker, 2002) at baseline, post-treatment and at 4- and 12-month follow-up. This self-rated questionnaire assesses monthly healthcare visits, medication consumption, sick-leave, work- and household cutback. The primary health economical outcome used responder status measured using the PSWQ. The secondary outcome was based on quality of life using the EuroQol questionnaire (EQ-5D; Rabin and Charro, 2001).
Statistical analyses
Primary analyses were conducted according to the intention-to-treat principle. The effect of group (IbET v. waiting-list, CTRL v. waiting-list, IbET v. CTRL), time (baseline to week 10 using all weekly measures) and group × time interaction effects were analysed using linear mixed models with maximum likelihood estimations and random intercepts. Per protocol analyses were also conducted only including participants completing all treatment modules. Post-hoc tests on between-group differences were conducted on therapist time, treatment credibility, working alliance (controlling for symptom change) and on all outcome measures at post-treatment using linear regression analysis. Treatment sustainability was tested by repeating the mixed effects regression model testing the effect of time on outcome from post-treatment to 4- and 12-month follow-up for each treatment group. χ2 analyses with risk ratios (RR) were used to test between-group differences in responder rates at post-treatment.
The mediation analyses were conducted according to the Preacher and Hayes (2008) framework using a mixed-effects regression model. In the mediation analysis, we investigated if group (IbET v. CTRL) interacted with time (week 0–10) on the mediators (as the hypothesized mediator for the IbET was thought suppression whereas neither self-regulation nor depressive symptoms should theoretically mediate the treatment effects) and also if the mediators interacted with the weekly outcome on the PSWQ throughout the treatment period. The statistical significance of the mediated effect (the ab product or indirect effect) was investigated by constructing 95% confidence intervals around the mediated effect based on 5000 bootstrapped resamples. All competing mediators were analysed in the model simultaneously.
We also conducted a cost-effectiveness analysis based on both specific symptoms (treatment responder) and a generic outcome (quality adjusted life years; QALYs). Incremental cost-effectiveness ratios (ICERs) were estimated using linear regression with 5000 bootstrap replications and plotted in cost-effectiveness planes.
Results
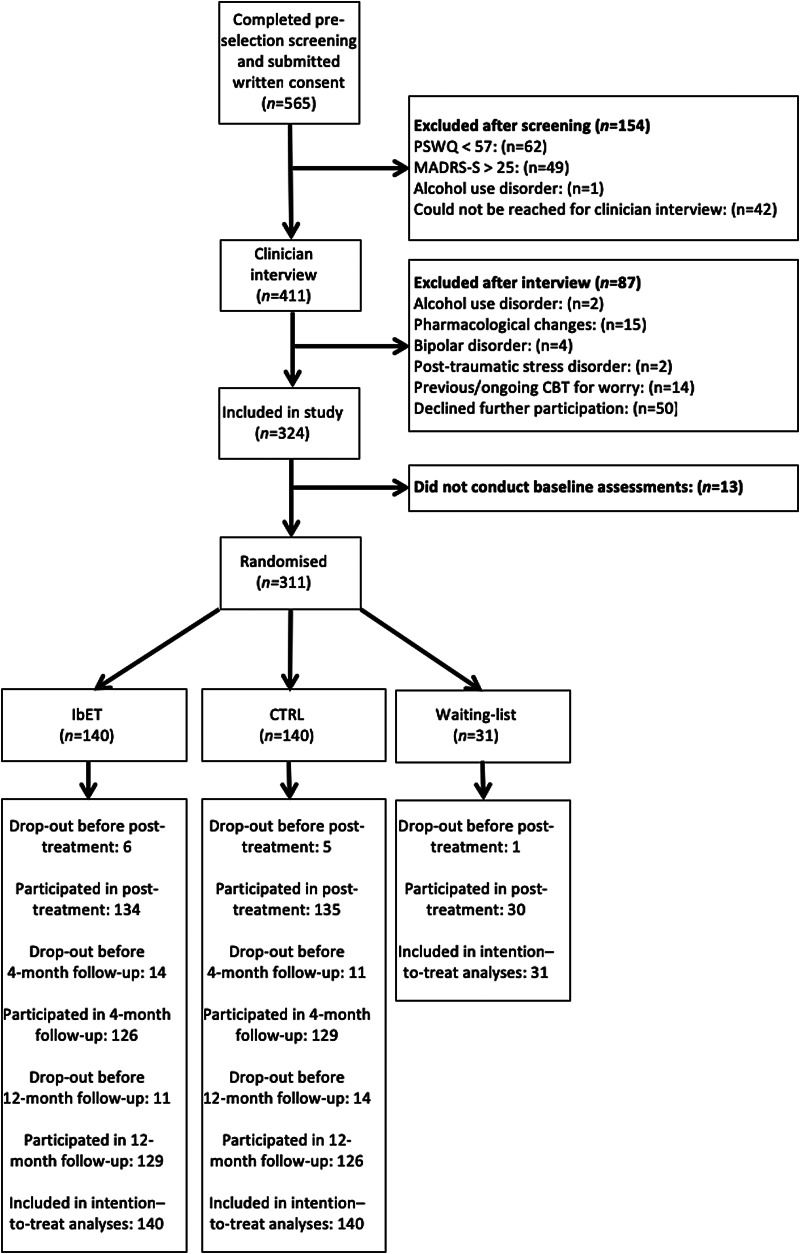
Figure 1 shows the participant flow through the trial and Table 1 presents baseline characteristics of the 311 included participants. Data attrition was low at post-treatment (primary endpoint; 4%) and at follow-up (9% at 4- and 12-months) and was equally distributed across the groups. As displayed in Table 1, three quarters of the participants represented a wide spectrum of psychiatric disorders marked by excessive worry while about a quarter did not fulfil the criteria for any of the psychiatric disorders.
Fig. 1.
Trial profile. IbET, internet-based extinction therapy; CTRL, control condition (active comparator); PSWQ, Penn State Worry Questionnaire; MADRS-S, Montgomery Asberg Depression Rating Scale – Self report; CBT, cognitive behaviour therapy.
Table 1.
Socio-demographic and clinical characteristics of the sample
| Variable | IbET (N = 140) | CTRL (N = 140) | WL (N = 31) |
|---|---|---|---|
| Gender | |||
| Women | 113 (81%) | 111 (79%) | 24 (77%) |
| Men | 27 (19%) | 29 (21%) | 7 (23%) |
| Age | |||
| Mean age (s.d.) | 44 (16) | 43 (14) | 46 (13) |
| Min-max | 19-87 | 21-79 | 26-70 |
| Highest education | |||
| Primary school | 2 (1%) | 5 (4%) | – |
| Secondary school | 43 (31%) | 43 (31%) | 7 (23%) |
| College/university | 77 (55%) | 76 (54%) | 18 (59%) |
| Other education | 10 (7%) | 10 (7%) | 4 (13%) |
| Doctorate | 8 (7%) | 10 (7%) | 2 (6%) |
| Occupational status | |||
| Working | 96 (69%) | 106 (76%) | 23 (74%) |
| Student | 20 (14%) | 12 (9%) | 1 (3%) |
| Retired | 17 (12%) | 13 (9%) | 4 (13%) |
| Parental leave | 2 (1%) | 2 (1%) | 1 (3%) |
| Unemployed | 5 (4%) | 7 (5%) | 2 (6%) |
| Excessive worry | |||
| Mean length in years (s.d.) | 22.29 (17.95) | 22.67 (17.30) | 21.71 (15.68) |
| Min-max | 0–75 | 1–64 | 2–60 |
| Psychiatric diagnoses according to the MINI | |||
| Current depressive episode | 11 (8%) | 18 (13%) | 4 (13%) |
| Previous depressive episodes | 79 (56%) | 86 (61%) | 18 (58%) |
| PD | 13 (9%) | 12 (9%) | 1 (3%) |
| Agoraphobia | 7 (5%) | 8 (6%) | 1 (3%) |
| SAD | 22 (16%) | 20 (14%) | 5 (16%) |
| OCD | 10 (7%) | 6 (4%) | 5 (16%) |
| Bulimia/binge eating disorder | 3 (2%) | 2 (1%) | 1 (3%) |
| GAD | 90 (64%) | 89 (64%) | 22 (71%) |
| Number of current diagnoses | |||
| No diagnosis | 34 (24%) | 35 (25%) | 6 (20%) |
| One diagnosis | 74 (53%) | 71 (51%) | 15 (48%) |
| Two diagnoses | 17 (12%) | 21 (15%) | 8 (26%) |
| Three or more diagnoses | 15 (11%) | 13 (9%) | 2 (7%) |
| Previous psychological treatments | |||
| CBT | 56 (40%) | 48 (34%) | 11 (36%) |
| Psychodynamic therapy | 16 (11%) | 18 (13%) | 3 (10%) |
| Other psychotherapy | 45 (32%) | 61 (44%) | 15 (48%) |
| Current medication | |||
| Antidepressants | 25 (18%) | 18 (13%) | 4 (13%) |
| Sedatives/hypnotics | 23 (16%) | 18 (13%) | 4 (13%) |
| Neuroleptics | 3 (2%) | 4 (3%) | – |
| Thyroxine | 6 (4%) | 7 (5%) | 1 (3%) |
IbET, internet-based extinction therapy; CTRL, control condition (active comparator); WL, waiting-list; PD, panic disorder; SAD, social anxiety disorder; OCD, obsessive-compulsive disorder; GAD, generalized anxiety disorder; CBT, cognitive behaviour therapy.
Primary outcome
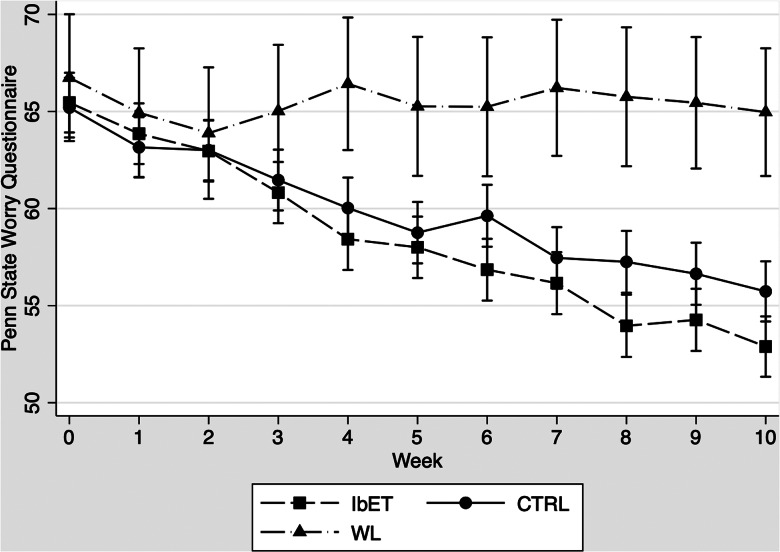
Results are displayed in Table 2, online Supplementary eTables 3 and 4 and Fig. 2. Both IbET and CTRL were significantly more effective in reducing worry compared with waiting-list (ps < 0.001) and between-group effect sizes were in the large and expected range at post-treatment (IbET v. waiting-list: d = 1.34, 95% CI 1.00–1.66 ‖ CTRL v. waiting-list: d = 0.98, 95% CI 0.68–1.28). Importantly, IbET was superior to CTRL (p < 0.001) with a significant between-group effect-size at post-treatment (d = 0.38, 95% CI 0.09–0.67). Per protocol analysis of participants who completed all modules (~30% in both groups) showed that IbET was superior to CTRL (p < 0.001) but with a considerably larger between-group effect size at post-treatment (d = 0.79, 95% CI 0.34–1.24). Both the IbET (p = 0.003) and the CTRL (p < 0.001) groups improved significantly from post-treatment to 4- and 12-month follow-up. Detailed subgroup analyses are shown in online Supplementary eFigs. 1–3.
Table 2.
Treatment outcome mean scores, by group
| IbET (n = 140) | CTRL (n = 140) | WL (n = 31) | ||||
|---|---|---|---|---|---|---|
| Variable | m | s.d. | m | s.d. | m | s.d. |
| PSWQ | ||||||
| Pre-treatment | 65.46 | 6.93 | 65.20 | 7.54 | 66.74 | 6.33 |
| Post-treatment | 52.99 | 11.49 | 55.93 | 10.71 | 65.00 | 8.45 |
| 4 FUP | 50.92 | 11.26 | 52.48 | 10.91 | ||
| 12 FUP | 50.55 | 10.96 | 52.61 | 11.48 | ||
| CAQ | ||||||
| Pre-treatment | 68.85 | 20.02 | 68.04 | 19.97 | 68.77 | 17.87 |
| Post-treatment | 59.19 | 18.88 | 64.41 | 20.50 | 70.90 | 21.12 |
| 4 FUP | 53.78 | 18.81 | 53.94 | 19.25 | ||
| 12 FUP | 54.16 | 17.11 | 57.91 | 21.70 | ||
| MADRS-S | ||||||
| Pre-treatment | 14.76 | 6.50 | 14.33 | 6.30 | 16.03 | 6.00 |
| Post-treatment | 10.30 | 6.37 | 10.89 | 7.22 | 16.23 | 6.86 |
| 4 FUP | 9.75 | 6.66 | 9.39 | 6.08 | ||
| 12 FUP | 9.68 | 6.13 | 10.29 | 7.13 | ||
| IUS | ||||||
| Pre-treatment | 77.38 | 21.75 | 75.48 | 19.93 | 77.55 | 20.03 |
| Post-treatment | 63.22 | 20.60 | 66.12 | 22.22 | 76.57 | 21.55 |
| 4 FUP | 61.16 | 19.88 | 61.16 | 21.61 | ||
| 12 FUP | 59.19 | 20.41 | 60.75 | 21.75 | ||
| BBQ | ||||||
| Pre-treatment | 45.92 | 20.57 | 43.81 | 21.71 | 42.42 | 18.59 |
| Post-treatment | 54.17 | 20.40 | 49.84 | 21.61 | 43.07 | 20.58 |
| 4 FUP | 54.14 | 22.71 | 53.47 | 23.02 | ||
| 12 FUP | 53.43 | 21.43 | 50.98 | 22.54 | ||
IbET, internet-based extinction therapy; CTRL, control condition (active comparator); WL, waiting-list; PSWQ, Penn State Worry Questionnaire; CAQ, Cognitive Avoidance Questionnaire; MADRS-S, Montgomery Asberg Depression Rating Scale – Self report; IUS, Intolerance of Uncertainty Scale; BBQ, Brunnsviken Brief Quality of life Questionnaire; 4 FUP, 4-month follow-up; 12 FUP, 12-month follow-up.
Fig. 2.
Change on primary outcome (Penn State Worry Questionnaire) during the treatment phase. IbET, internet-based extinction therapy; CTRL, control condition (active comparator); WL, waiting-list. The graph shows adjusted mean values and 95% confidence intervals for each group.
Responder rates
There were 85 (63%) responders in the IbET group, 69 (51%) in the CTRL group and 4 (13%) in the waiting-list condition respectively at post-treatment. Both IbET [risk ratio (RR) = 4.76, 95% CI 1.90–11.96] and the CTRL group (RR = 3.83, 95% CI 1.52–9.69) had significantly larger proportions of responders compared to waiting-list and the IbET group had significantly more responders than CTRL (RR = 1.24, 95% CI 1.01–1.53).
Secondary outcomes
IbET was superior to waiting-list in reducing cognitive avoidance (p = 0.001), intolerance of uncertainty (p < 0.001), depressive symptoms (p < 0.001) and also increased quality of life (p = 0.022). The CTRL group had similar improvements on cognitive avoidance (p = 0.026), depressive symptoms (p = 0.001) and intolerance of uncertainty (p = 0.012) but not on quality of life compared to the waiting-list (p = 0.112). IbET was superior to CTRL on cognitive avoidance (p = 0.006) and intolerance of uncertainty (p = 0.016) but not on depression nor quality of life (ps = 0.113–0.306). Improvements were sustained for both IbET and CTRL on depression and quality of life (ps = 0.180–0.512) at the 4- and 12-month follow-up. Both IbET and CTRL had further reductions on intolerance of uncertainty and cognitive avoidance (ps = 0.001–<0.001) from post-treatment to the 4- and 12-month follow-up.
Control for non-specific factors
There were no significant differences between IbET and CTRL in terms of completed modules, therapist time spent per participant, number of sent or received messages, treatment credibility, nor working alliance (p = 0.073–0.694) (online Supplementary eTable 5). Participants in the IbET group completed on average 5.89 (s.d. = 2.20) modules out of eight and the corresponding figure in the CTRL group was 6.03 (s.d. = 2.02). The treating therapists spent on average 130 (s.d. = 89) minutes per participant in the IbET group and 113 (s.d. = 72) minutes per participant in the CTRL condition. Thus, the superior improvements in IbET compared to the active comparator could not be attributed to systematic differences in non-specific factors.
Adverse events and protocol deviations
There were six protocol deviations associated with changes in antidepressants or antipsychotics during the acute treatment period (four deviations in the IbET group and two in the CTRL group). Results remained the same after repeating the main analyses excluding these participants in the outcome analyses. No serious adverse events were reported (online Supplementary eTable 7).
Mediation analysis
As hypothesized, the thought suppression subscale on the CAQ significantly mediated the effect in the IbET group compared with CTRL [43% proportion mediated effect controlling for the competing mediators, ab point estimate = −0.11, (95% CI −0.06 to −0.17), p < 0.001]. As expected, neither the self-regulation subscale on the MAIA [estimate = 0.01, (95% CI −0.03 to 0.05), p = 0.64], nor depressive symptoms, assessed using the PHQ-2 [estimate = −0.01, (95% CI −0.04 to 0.02), p = 0.50], mediated the treatment effects (online Supplementary eTable 6).
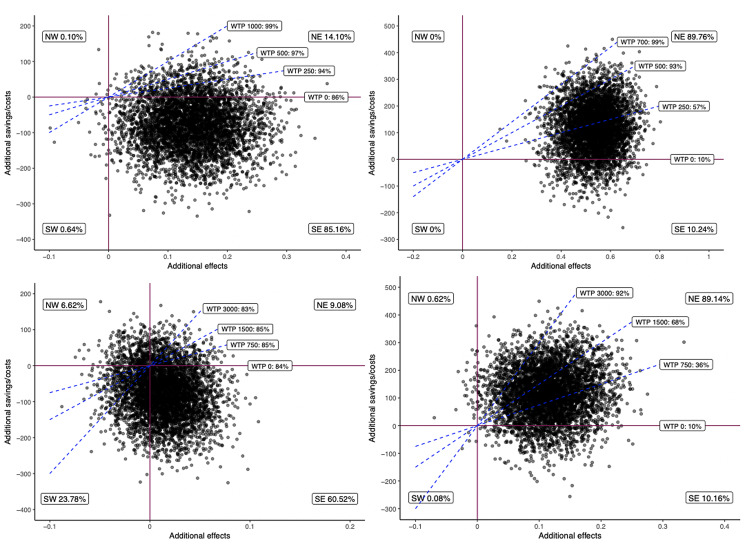
Cost-effectiveness analysis
Cost-effectiveness planes are shown in Fig. 3. The average ICER between IbET and CTRL was −550€ which means that each improved case of excessive worry was associated with a societal earning of 550€. The corresponding ICER estimating QALYs was 7300€ (online Supplementary eTable 8).
Fig. 3.
Cost-effectiveness planes IbET v. CTRL and waiting-list. IbET, internet-based extinction therapy; CTRL, control condition (active comparator); NE, northeast. NW, northwest; SE, southeast; SW, southwest; WTP, willingness to pay.
The upper left cost-effectiveness plane compares IbET with CTRL using responder status as outcome. Here, 85% of the dots are located in the south-east quadrant indicating a high probability that IbET incurs both better treatment effects (x-axis; higher degree of responders) at a lower cost than CTRL (y-axis). Given a societal willingness to pay (WTP) of 1000€ for one extra responder case, the probability of IbET being cost-effective compared to CTRL rises to 99%. The upper right cost-effectiveness plane compares IbET v. waiting list using responder status as outcome. Here, 90% of the dots are located in the northeast quadrant indicating that IbET achieves incremental effects (more responders) but to higher costs. Given a WTP of 700€, IbET stands a 99% chance of being cost-effective against waiting-list. The lower left cost-effectiveness plane shows IbET v. CTRL using QALY as outcome (measured using the EQ-5D). Here, IbET has a 61% chance of being cost-effective and this figure increases to 83% given a WTP of 3000€. The lower right plane in the same figure compares IbET with waiting-list using QALY as outcome. Here, only 10% of the dots are located in the superior quadrant but given a WTP of 3000€, the probability of IbET being cost-effective increases to 92%.
Discussion
The results of this trial showed that a novel scalable internet-based psychological intervention (IbET) can be effective and cost-effective in reducing excessive worry compared with an active control comparator (CTRL). Importantly, the IbET and CTRL groups did not differ on non-specific factors such as therapist attention, number of completed modules, treatment credibility or therapeutic alliance. From a clinical perspective, we believe that the findings of this study are important for several reasons. First, the trial suggests that clinicians may use IbET for a range of patients where excessive worry is the primary concern but who do not suffer from serious disorders such as moderate-to-severe depression and post-traumatic stress disorder. This may be of particular importance for clinicians in primary care where a substantial proportion of patients present with subthreshold anxiety- and depressive disorders, but still experience significant functional impairments (Batelaan et al., 2007; de Bruijn et al., 2010; Sarsour et al., 2011). Second, using the internet to deliver and scale up treatments means that a wider population can be reached. Third, as indicated in the health economical evaluation, IbET is a potentially cost-effective treatment. An important next step is to investigate whether the results from this trial are generalizable to the ‘real world’ setting. Although there is evidence that internet-delivered treatments are efficacious when implemented in regular care (Hedman et al., 2013, 2014b), there may be several therapist and patient characteristics that affect the outcomes when tested in real-world practice (Gibbons, Wiltsey Stirman, DeRubeis, Newman, & Beck, 2013; Holmqvist, Philips, & Barkham, 2015; Kazdin, 2008).
As a novel element, the treatment used in this study (IbET) targets a specific psychological process (excessive worry) common in several psychiatric disorders, instead of treating the disorder as a whole. The participants in this trial represented a range of different psychiatric disorders and one-quarter of the sample did not fulfil the criteria of any psychiatric condition but nonetheless experienced excessive worry only. This focus on precision-based interventions for specific processes has been highlighted by the NIMH (Cuthbert & Insel, 2013; Insel & Gogtay, 2014) and is part of a scientific shift towards process- rather than diagnosis-oriented interventions. Thus, the present trial represents a clear step forward in the understanding and treatment of psychiatric disorders (Holmes et al., 2018). With that being said, GAD was clearly the most common diagnosis in the present sample, which probably reflects that worry is a core symptom of this disorder. Our subgroup analyses (shown in the online supplement) however indicated that this treatment is effective also for a wider spectrum of symptom profiles and not just for the GAD population.
Another important feature in the current study and in line with recent recommendations from NIMH (Insel & Gogtay, 2014) was to include a mediation analysis. As hypothesized, a decrease in thought suppression (which is the main principle of the IbET treatment but not in the active comparator) mediated the treatment effects between IbET and CTRL while the competing non-relevant mediators (self-regulation and depressive symptoms) did not. Although these analyses were correlational (i.e. not causal) by nature, the results from the mediation analyses in the present study provide further support for the proposed mechanisms in the IbET treatment. In future studies we aim to link the completion of specific modules to subsequent changes in the mediators in a panel data analysis, in order to better understand the mechanisms of change in the IbET treatment. A next step could also be to make a qualitative in-depth analysis of treatment adherence as, judging from the large effect sizes observed in this trial, completing all modules does not seem to be necessary for substantial improvements to occur. Another important target for future research is to investigate whether intervening in worry processes can have a cascade effect and affect the expression of other psychiatric symptoms, as indicated by a previous trial (Freeman et al., 2015).
It is important to stress that the active comparator used in this trial was also highly efficacious in reducing worry symptoms compared to the waiting-list group. This is not surprising given that the interventions included in the CTRL treatment consisted mainly of relaxation exercises, which are recommended intervention strategies by the NICE guidelines (2011) to tackle worry and GAD. A recommendation for future studies is therefore to analyse moderators and/or moderated mediators of treatment response and investigate who would benefit most from which treatment.
The strengths of this study were the randomised design, weekly measurements, the control for non-specific treatment factors, the low attrition rates and the high statistical power. Additionally, the firm structure of the internet-format with standardised written texts significantly reduces the risk of therapy drift. Major limitations were that participants were self-referred and that we excluded participants with severe disorders such as moderate-to-severe depression, substance dependence, self-harm and post-traumatic stress disorder. This may affect the external validity of the results, which may not be generalizable to the whole population with excessive worry. On the other hand, the advantage of IbET is that it is an accessible and scalable intervention that may target populations who would not otherwise receive care. Moreover, only 9% of the applicants were excluded due to high depressive symptoms and only a fraction (1.6%) was excluded due to the other exclusion criteria. We therefore view the impact on the generalizability of the results as fairly limited, but future research should investigate whether the IbET treatment is also effective for patients with a broader range of disorders. Also, as in most trials of psychological disorders, we did not use a structured diagnostic assessment of personality disorders and it is therefore still unclear how well IbET works for this particular patient group. Additionally, the therapists were not blinded to the study hypothesis. A final limitation of the current study was the use of a self-administered outcome measurement. A meta-analysis has shown that effect sizes based on self-report measures for worry are lower than clinician-rated instruments (Cuijpers et al., 2014). Consequently, it is possible that the between-group effect sizes in this study were underestimated.
Despite these limitations, we regard the results in this trial as clinically and scientifically relevant. We conclude that IbET is an effective and cost-effective treatment for people with excessive worry but without severe psychiatric problems. Replication and further extension of study results to real-world settings is warranted.
Acknowledgement
This study was funded by the Fredrik and Ingrid Thuring foundation. The corresponding author confirms that he had full access to all the data in the study and had final responsibility for the decision to submit the paper for publication.
Author contributors
EA, BL and EHL designed the trial. EA took the main responsibility for drafting the study report. EA was the main lead for the trial. EA did the analyses of the trial outcome. EA and BL did the cost-effectiveness analyses. BL did the mediation analyses. EA was the trial coordinator. EA provided the training and supervision for the trial therapists and research workers. MHL, JB, LN, MP, AG, KR, LA and TS provided the therapy and collected all trial data. All authors contributed to, read, and approved the final report.
Financial support
The funding organization (Fredrik and Ingrid Thuring foundation) had no role in the conception of the study design, nor in the collection, analysis or interpretation of the data, in the writing of the report or in the decision to submit the paper.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional guides on the care and use of laboratory animals.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0033291720000781.
click here to view supplementary material
Conflict of interest
Drs Brjánn Ljótsson and Erik Hedman-Lagerlöf are shareholders of DahliaQomit Inc, a company specializing in online psychiatric symptom assessment. All remaining authors report that they have no competing interests.
References
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American Psychiatric Publishing. [Google Scholar]
- Andersson, E., Hedman, E., Enander, J., Djurfeldt, D. R., Ljotsson, B., Cervenka, S., … Ruck, C. (2015). D-Cycloserine vs placebo as adjunct to cognitive behavioral therapy for obsessive-compulsive disorder and interaction with antidepressants: A randomized clinical trial. JAMA Psychiatry, 72(7), 659–667. doi: 10.1001/jamapsychiatry.2015.0546. [DOI] [PubMed] [Google Scholar]
- Andersson, E., Hedman, E., Wadstrom, O., Boberg, J., Andersson, E. Y., Axelsson, E., … Ljotsson, B. (2017). Internet-based extinction therapy for worry: A randomized controlled trial. Behavior Therapy, 48(3), 391–402. doi: 10.1016/j.beth.2016.07.003. [DOI] [PubMed] [Google Scholar]
- Andersson, G., & Titov, N. (2014). Advantages and limitations of internet-based interventions for common mental disorders. World Psychiatry, 13(1), 4–11. doi: 10.1002/wps.20083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arroll, B., Goodyear-Smith, F., Crengle, S., Gunn, J., Kerse, N., Fishman, T., … Hatcher, S. (2010). Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Annals of Family Medicine, 8(4), 348–353. doi: 10.1370/afm.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batelaan, N., Smit, F., de Graaf, R., van Balkom, A., Vollebergh, W., & Beekman, A. (2007). Economic costs of full-blown and subthreshold panic disorder. Journal of Affective Disorders, 104(1–3), 127–136. doi: 10.1016/j.jad.2007.03.013. [DOI] [PubMed] [Google Scholar]
- Berman, A. H., Bergman, H., Palmstierna, T., & Schlyter, F. (2005). Evaluation of the Drug Use Disorders Identification Test (DUDIT) in criminal justice and detoxification settings and in a Swedish population sample. European Addiction Research, 11(1), 22–31. doi: 10.1159/000081413. [DOI] [PubMed] [Google Scholar]
- Borkovec, T. D., & Nau, S. D. (1972). Credibility of analogue therapy rationales. Journal of Behavior Therapy and Experimental Psychiatry, 3(4), 257–260. doi: 10.1016/0005-7916(72)90045-6. [DOI] [Google Scholar]
- Buhr, K., & Dugas, M. J. (2002). The intolerance of uncertainty scale: Psychometric properties of the English version. Behaviour Research and Therapy, 40(8), 931–945. doi: 10.1016/S0005-7967(01)00092-4. [DOI] [PubMed] [Google Scholar]
- Craske, M. G. (2012). Transdiagnostic treatment for anxiety and depression. Depression and Anxiety, 29(9), 749–753. doi: 10.1002/da.21992. [DOI] [PubMed] [Google Scholar]
- Cuijpers, P., Sijbrandij, M., Koole, S., Huibers, M., Berking, M., & Andersson, G. (2014). Psychological treatment of generalized anxiety disorder: A meta-analysis. Clinical Psychology Review, 34(2), 130–140. doi: 10.1016/j.cpr.2014.01.002. [DOI] [PubMed] [Google Scholar]
- Cuijpers, P., & Smit, F. (2004). Subthreshold depression as a risk indicator for major depressive disorder: A systematic review of prospective studies. Acta Psychiatrica Scandinavica, 109(5), 325–331. doi: 10.1111/j.1600-0447.2004.00301.x. [DOI] [PubMed] [Google Scholar]
- Cuthbert, B. N., & Insel, T. R. (2013). Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Medicine, 11, 126. doi: 10.1186/1741-7015-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bruijn, C., Beun, S., de Graaf, R., ten Have, M., & Denys, D. (2010). Subthreshold symptoms and obsessive-compulsive disorder: Evaluating the diagnostic threshold. Psychological Medicine, 40(6), 989–997. doi: 10.1017/s0033291709991012. [DOI] [PubMed] [Google Scholar]
- Fehm, L., Beesdo, K., Jacobi, F., & Fiedler, A. (2008). Social anxiety disorder above and below the diagnostic threshold: Prevalence, comorbidity and impairment in the general population. Social Psychiatry and Psychiatric Epidemiology, 43(4), 257–265. doi: 10.1007/s00127-007-0299-4. [DOI] [PubMed] [Google Scholar]
- Freeman, D., Dunn, G., Startup, H., Pugh, K., Cordwell, J., Mander, H., … Kingdon, D. (2015). Effects of cognitive behaviour therapy for worry on persecutory delusions in patients with psychosis (WIT): A parallel, single-blind, randomised controlled trial with a mediation analysis. The Lancet. Psychiatry, 2(4), 305–313. doi: 10.1016/S2215-0366(15)00039-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons, C. R., Wiltsey Stirman, S., DeRubeis, R. J., Newman, C. F., & Beck, A. T. (2013). Research setting versus clinic setting: Which produces better outcomes in cognitive therapy for depression? Cognitive Therapy Research, 37(3), 605–612. doi: 10.1007/s10608-012-9499-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold, S. M., Enck, P., Hasselmann, H., Friede, T., Hegerl, U., Mohr, D. C., & Otte, C. (2017). Control conditions for randomised trials of behavioural interventions in psychiatry: A decision framework. The Lancet. Psychiatry, 4(9), 725–732. doi: 10.1016/S2215-0366(17)30153-0. [DOI] [PubMed] [Google Scholar]
- Hakkaart-van Roijen, L., & Donker, M. C. H. (2002). Manual/iMTA questionnaire for costs associated with psychiatric illness (TIC-P). Retrieved from http://hdl.handle.net/1765/1337.
- Haller, H., Cramer, H., Lauche, R., Gass, F., & Dobos, G. J. (2014). The prevalence and burden of subthreshold generalized anxiety disorder: A systematic review. BMC Psychiatry, 14, 128. doi: 10.1186/1471-244x-14-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedman, E., Axelsson, E., Gorling, A., Ritzman, C., Ronnheden, M., El Alaoui, S., … Ljotsson, B. (2014a). Internet-delivered exposure-based cognitive-behavioural therapy and behavioural stress management for severe health anxiety: Randomised controlled trial. British Journal of Psychiatry, 205(4), 307–314. doi: 10.1192/bjp.bp.113.140913. [DOI] [PubMed] [Google Scholar]
- Hedman, E., Ljotsson, B., Kaldo, V., Hesser, H., El Alaoui, S., Kraepelien, M., … Lindefors, N. (2014b). Effectiveness of internet-based cognitive behaviour therapy for depression in routine psychiatric care. Journal of Affective Disorders, 155, 49–58. doi: 10.1016/j.jad.2013.10.023. [DOI] [PubMed] [Google Scholar]
- Hedman, E., Ljotsson, B., Ruck, C., Bergstrom, J., Andersson, G., Kaldo, V., … Lindefors, N. (2013). Effectiveness of internet-based cognitive behaviour therapy for panic disorder in routine psychiatric care. Acta Psychiatrica Scandinavica, 128(6), 457–467. doi: 10.1111/acps.12079. [DOI] [PubMed] [Google Scholar]
- Hofmann, S. G., & Smits, J. A. (2008). Cognitive-behavioral therapy for adult anxiety disorders: A meta-analysis of randomized placebo-controlled trials. Journal of clinical psychiatry, 69(4), 621–632. doi: 10.4088/jcp.v69n0415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes, E. A., Ghaderi, A., Harmer, C. J., Ramchandani, P. G., Cuijpers, P., Morrison, A. P., … Craske, M. G. (2018). The Lancet Psychiatry Commission on psychological treatments research in tomorrow's science. The Lancet. Psychiatry, 5(3), 237–286. doi: 10.1016/S2215-0366(17)30513-8. [DOI] [PubMed] [Google Scholar]
- Holmqvist, R., Philips, B., & Barkham, M. (2015). Developing practice-based evidence: Benefits, challenges, and tensions. Psychotherapy Research, 25(1), 20–31. doi: 10.1080/10503307.2013.861093. [DOI] [PubMed] [Google Scholar]
- Insel, T. R., & Gogtay, N. (2014). National institute of mental health clinical trials: New opportunities, new expectations. JAMA Psychiatry, 71(7), 745–746. doi: 10.1001/jamapsychiatry.2014.426. [DOI] [PubMed] [Google Scholar]
- Kazdin, A. E. (2008). Evidence-based treatment and practice: New opportunities to bridge clinical research and practice, enhance the knowledge base, and improve patient care. American Psychologist, 63(3), 146–159. doi: 10.1037/0003-066X.63.3.146. [DOI] [PubMed] [Google Scholar]
- Lindner, P., Frykheden, O., Forsstrom, D., Andersson, E., Ljotsson, B., Hedman, E., … Carlbring, P. (2016). The Brunnsviken Brief Quality of Life Scale (BBQ): Development and psychometric evaluation. Cognitive Behaviour Therapy, 45(3), 182–195. doi: 10.1080/16506073.2016.1143526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ljotsson, B., Hedman, E., Andersson, E., Hesser, H., Lindfors, P., Hursti, T., … Andersson, G. (2011). Internet-delivered exposure-based treatment vs. stress management for irritable bowel syndrome: A randomized trial. American Journal of Gastroenterology, 106(8), 1481–1491. doi: 10.1038/ajg.2011.139. [DOI] [PubMed] [Google Scholar]
- Mehling, W. E., Price, C., Daubenmier, J. J., Acree, M., Bartmess, E., & Stewart, A. (2012). The Multidimensional Assessment of Interoceptive Awareness (MAIA). PLoS One, 7(11), e48230. doi: 10.1371/journal.pone.0048230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer, T. J., Miller, M. L., Metzger, R. L., & Borkovec, T. D. (1990). Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy, 28(6), 487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Mulder, R., Murray, G., & Rucklidge, J. (2017). Common versus specific factors in psychotherapy: Opening the black box. The Lancet. Psychiatry, 4(12), 953–962. doi: 10.1016/S2215-0366(17)30100-1. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence. (2011). Generalised anxiety disorder and panic disorder (with or without agoraphobia) in adults. Retrieved from https://www.nice.org.uk/guidance/cg113. [PubMed]
- Preacher, K. J., & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. doi: 10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- Rabin, R., & Charro, F. d. (2001). EQ-SD: A measure of health status from the EuroQol Group. Annals of Medicine, 33(5), 337–343. doi: 10.3109/07853890109002087. [DOI] [PubMed] [Google Scholar]
- Rohde, P., Lewinsohn, P. M., & Seeley, J. R. (1997). Comparability of telephone and face-to-face interviews in assessing axis I and II disorders. The American journal of psychiatry, 154(11), 1593–1598. doi: 10.1176/ajp.154.11.1593. [DOI] [PubMed] [Google Scholar]
- Sarsour, K., Kalsekar, A., Swindle, R., Foley, K., & Walsh, J. K. (2011). The association between insomnia severity and healthcare and productivity costs in a health plan sample. Sleep, 34(4), 443–450. doi: 10.1093/sleep/34.4.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders, J. B., Aasland, O. G., Babor, T. F., de la Fuente, J. R., & Grant, M. (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption--II. Addiction, 88(6), 791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Sexton, K. A., & Dugas, M. J. (2008). The cognitive avoidance questionnaire: Validation of the English translation. Journal of Anxiety Disorders, 22(3), 355–370. doi: 10.1016/j.janxdis.2007.04.005. [DOI] [PubMed] [Google Scholar]
- Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., … Dunbar, G. C. (1998). The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of clinical psychiatry, 59 (Suppl 20), 22–33;quiz 34–57. [PubMed] [Google Scholar]
- Stanley, M. A., Wilson, N. L., Novy, D. M., Rhoades, H. M., Wagener, P. D., Greisinger, A. J., … Kunik, M. E. (2009). Cognitive behavior therapy for generalized anxiety disorder among older adults in primary care: A randomized clinical trial. JAMA, 301(14), 1460–1467. doi: 10.1001/jama.2009.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svanborg, P., & Asberg, M. (2001). A comparison between the Beck Depression Inventory (BDI) and the self-rating version of the Montgomery Asberg Depression Rating Scale (MADRS). Journal of Affective Disorders, 64(2–3), 203–216. doi: 10.1016/s0165-0327(00)00242-1. [DOI] [PubMed] [Google Scholar]
- Tracey, T. J., & Kokotovic, A. M. (1989). Factor structure of the working alliance inventory. Psychological Assessment, 1(3), 207–210. doi: 10.1037/1040-3590.1.3.207. [DOI] [Google Scholar]
- Wadström, O. (2015). Quit ruminating and brooding: It is easier to do with cognitive behavior therapy (CBT). Scotts Valley: Createspace. [Google Scholar]
- Wittchen, H. U., & Hoyer, J. (2001). Generalized anxiety disorder: Nature and course. Journal of Clinical Psychiatry, 62 (Suppl 11), 15–19; discussion 20-11. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/11414546. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0033291720000781.
click here to view supplementary material