Since the COVID-19 pandemic, several ophthalmological damages have been reported in relation with this infection. Acute macular neuroretinopathy (AMN) is a retinal pathology rarely described in the literature and even less in SARS-CoV-2 infection. We report the case of a young woman with AMN while being infected with the english variant of Covid-19. The patient gave us her oral agreement to publish her case.
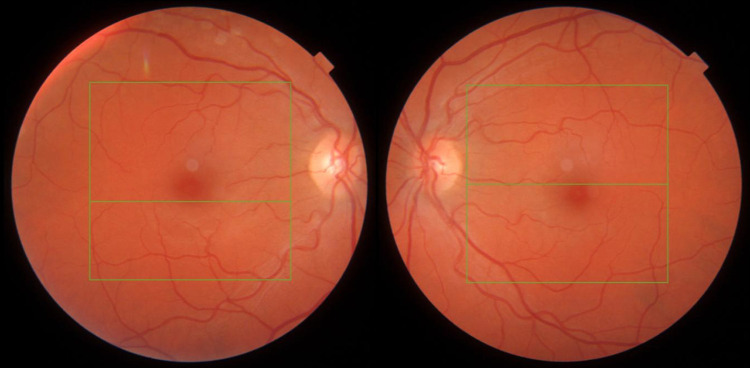
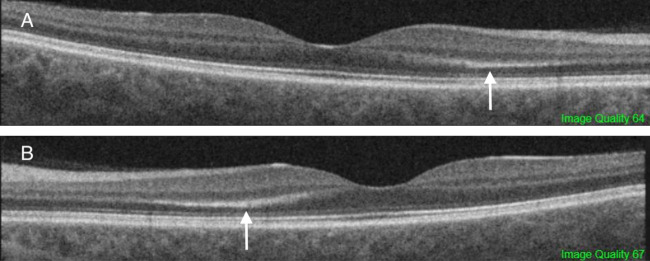
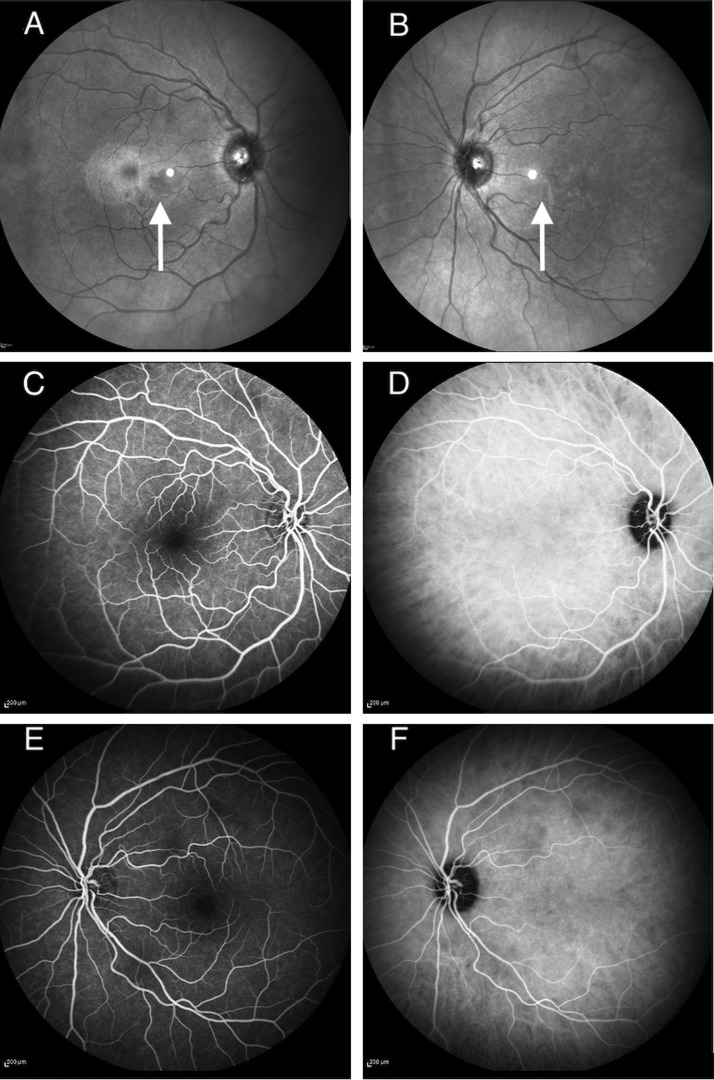
We describe a 39-years-old woman without medical antecedent, who presented to the ophthalmologic emergency for the onset of photopsia and bilateral para-central scotoma upon awakening. In addition, the patient had also been suffering from a symptomatic form of Covid-19 certified by polymerase chain reaction (PCR), the english variant, for 2 days. The patient had a cough and fever during the consultation. On examination, visual acuity corrected to -0.50 diopters was 10/10 in both eyes. The slit lamp examination was strictly normal, photomotor reflexes were present and symmetrical. The fundus examination was without pathological findings (Fig. 1 ). Macular optical coherence tomography (OCT) showed bilateral outer plexiform layer hyper-reflectivity in inter papillo-macular (Fig. 2 ). The visual field 10.2 was normal on the right and was observed an inferior para-central scotoma on the left. Infrared (IR) showed a bilateral greyish perifoveolar petaloids lesions. Fluorescein and indocyanine green angiographies were normal (Fig. 3 ) as autofluorescence (AF) images. In view of the background of the infection with the english variant Covid-19 with a flu-like syndrome, the age of the patient, and multimodal imaging, we concluded to an AMN.
Figure 1.
Non-mydriatic retinography right and left of the patient.
Figure 2.
Macular optical coherence tomography right (A) and left (B) with outer plexiform layer hyper-reflectivity (white arrows).
Figure 3.
IR right eye (A) and IR left eye (B) with greyish perifoveolar petaloids lesions (white arrows). Fluorescein (C) and indocyanine green (D) angiographies of the right eye. Fluorescein (E) and indocyanine green (F) angiographies of the left eye.
After 1 month, the patient's ophthalmologic symptoms persisted. A hyper-reflectivity of the external plexiform gave way to an iso-reflective thickening of this layer and to a disruption of the interdigitation zone on OCT.
AMN is a rare retinal disease. A few cases are reported in the literature. In Bhavsar KV's literature review, only 101 cases were described between 1975 and 2004 [1]. The physiopathology remains poorly explained but the vascular theory remains the most present in the literature [1], [2]. AMN is more often seen in young women with myopia, during or after a flu-like syndrome. Patients describe a para-central scotoma and photopsia. On OCT, hyper-reflectivity of the plexiform and the external nuclear are present. A disruption of the interdigitation zone can also be found. Symptoms and damages to OCT resolve gradually and spontaneously over a few months. Since the SARS-Cov2 pandemic, several ophthalmological damages have been described such as conjunctivitis, cotton wool spots, Roth spots, paracentral acute middle maculopathy [3], [4], [5], [6], [7]. Only 2 cases of AMN in the context of Covid-19 infection are reported in the literature [3], [4]. We must differentiate AMN and PAMM. The latter appear as placoid, hyperreflective bands at the level of the inner nuclear layer, sparing the outer retina while lesions affect the outer retina in the AMN. The vasculitis caused by this infection could explain the appearance of AMN and so reinforfces the vascular pathophysiology of this damage.
Disclosure of interest
The authors declare that they have no competing interest.
References
- 1.Bhavsar K.V., Lin S., Rahimy E., et al. Acute macular neuroretinopathy: A comprehensive review of the literature. Surv Ophthalmol. 2016;61:538–565. doi: 10.1016/j.survophthal.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Zamani G., Ataei Azimi S., Aminizadeh A., et al. Acute macular neuroretinopathy in a patient with acute myeloid leukemia and deceased by COVID-19: a case report. J Ophthalmic Inflamm Infect. 2021;10:39. doi: 10.1186/s12348-020-00231-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gascon P., Briantais A., Bertrand E., et al. Covid-19-Associated Retinopathy: A Case Report. Ocul Immunol Inflamm. 2020;28:1293–1297. doi: 10.1080/09273948.2020.1825751. [DOI] [PubMed] [Google Scholar]
- 4.Virgo J., Mohamed M. Paracentral acute middle maculopathy and acute macular neuroretinopathy following SARS-CoV-2 infection. Eye (Lond) 2020;34:2352–2353. doi: 10.1038/s41433-020-1069-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu P., Duan F., Luo C., et al. Characteristics of Ocular Findings of Patients With Coronavirus Disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020;138:575–578. doi: 10.1001/jamaophthalmol.2020.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amesty M.A., Alió Del Barrio J.L., Alió J.L. COVID-19 Disease and Ophthalmology: An Update. Ophthalmol Ther. 2020;9:1–12. doi: 10.1007/s40123-020-00260-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marinho P.M., Marcos A.A.A., Romano A.C., Nascimento H., Belfort R. Retinal findings in patients with COVID-19. Lancet. 2020;395:1610. doi: 10.1016/S0140-6736(20)31014-X. [DOI] [PMC free article] [PubMed] [Google Scholar]