1. Introduction
Subacute thyroiditis (SAT) represents an important diagnostic entity for otolaryngologists to be aware of due to the prolonged symptomatic clinical course if left untreated. Viral infections are the most common precipitating factor for SAT [1] with many reports of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection triggering SAT in patients hospitalized with coronavirus disease 2019 (Covid-19) [2]. Herein, we report a case of SAT induced by SARS-CoV-2 vaccination.
2. Report of a case
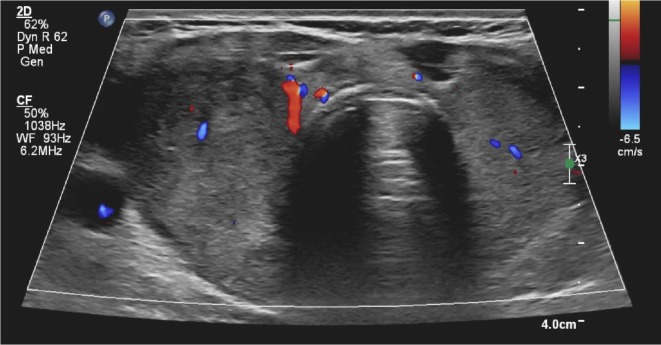
A healthy 48-year-old male was referred to our head and neck surgical oncology clinic for a three-week history of right neck swelling, throat discomfort, palpitations, fevers, and weight loss of 10 pounds. His symptoms started one week after administration of the second dose of the SARS-CoV-2 vaccine. His exam was notable for subtle tender fullness of the anterior right lower neck at the level of the thyroid. Thyroid ultrasonography (US) demonstrated diffuse enlargement of the thyroid gland with a hypoechoic and heterogeneous echotexture (Fig. 1 ). Laboratory testing was notable for an elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) and TFTs were consistent with hyperthyroidism (free T4 level of 3.6 ng/dL, thyroid-stimulating hormone (TSH) level of 0.01 uIU/mL). The clinical presentation and laboratory and imaging data were consistent with a diagnosis of SAT.
Fig. 1.
Thyroid US for subacute thyroiditis.
Legend: Transverse ultrasonographic image of the thyroid, taken at the level of the isthmus, demonstrates mild enlargement of the gland with heterogeneous, hypoechoic echotexture and no evidence of increased vascularity, consistent with subacute thyroiditis.
The patient was started on nonsteroidal anti-inflammatory drugs (NSAIDs) and prednisone 40 mg daily for one week. Within 24 h of initiating glucocorticoid therapy, he reported resolution of neck pain and fevers. He was referred to the endocrinology clinic for follow-up after completion of glucocorticoid therapy and repeat laboratory testing demonstrated decreased ESR, CRP and free T4 level and persistently suppressed TSH. He will undergo repeat TFTs and thyroid US at time of his two-month follow-up visit.
3. Discussion
Subacute thyroiditis is an inflammatory condition of the thyroid gland often precipitated by a viral illness with diagnosis based upon characteristic symptomatology (fevers, fatigue, enlarged and tender thyroid gland), laboratory data (elevated ESR, CRP and free T4 and suppressed TSH) and imaging findings. Thyroid US demonstrates diffuse heterogeneous echotexture with focal hypoechoic areas and decreased or normal color Doppler blood flow signals, contrary to Graves' thyroiditis, which has markedly increased vascularity [1], [3]. Subacute thyroiditis has been reported in many patients hospitalized with Covid-19 [2]. Angiotensin-converting enzyme 2 (ACE-2), the receptor for cellular entry of SARS-CoV-2, has been demonstrated to be expressed in thyroid follicular cells, making them a potential target for SARS-CoV-2 infection [4]. To our knowledge, there are only two prior reports describing SAT following administration of the SARS-CoV-2 vaccine [5], [6]. A rising vaccination rate and possibility of future booster SARS-CoV-2 vaccine administration raises the question of whether post-vaccination SAT may become a more commonly observed clinical phenomenon.
Subacute thyroiditis can mimic other disease entities including acute infectious thyroiditis, Graves' thyrotoxicosis and toxic multinodular goiter [3]. Thyroid US is the imaging modality of choice in the work-up of hyperthyroidism [3]. Iodinated-contrast medium should be avoided due to the risk of inducing thyrotoxicosis. For patients with moderate to severe symptoms related to SAT, the American Thyroid Association guidelines recommend treatment with NSAIDs and glucocorticoid therapy (prednisone 40 mg daily for one to two weeks followed by a taper based on clinical response) [3]. Our patient had an excellent clinical response to initiation of NSAIDs and glucocorticoid therapy with rapid symptomatic improvement after the first dose of prednisone.
4. Conclusion
Otolaryngologists should be well versed in the diagnosis and management of SAT due to the prolonged, symptomatic clinical course with a delay in treatment and potential precipitating factor of recent SARS-CoV-2 infection or vaccination. Prompt diagnosis and treatment with NSAIDs and glucocorticoid therapy are critical to achieving rapid resolution of systemic symptoms and preventing disease sequelae.
Meeting presentation
None.
Declaration of competing interest
None to report.
References
- 1.Desailloud R., Hober D. Viruses and thyroiditis: an update. Virol J. 2009;6:5. doi: 10.1186/1743-422X-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muller I., Cannavaro D., Dazzi D., et al. SARS-CoV-2-related atypical thyroiditis. Lancet Diabetes Endocrinol. 2020;8:739–741. doi: 10.1016/S2213-8587(20)30266-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ross D.S., Burch H.B., Cooper D.S., et al. 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid. 2016;26:1343–1421. doi: 10.1089/thy.2016.0229. [DOI] [PubMed] [Google Scholar]
- 4.Rotondi M., Coperchini F., Ricci G., et al. Detection of SARS-COV-2 receptor ACE-2 mRNA in thyroid cells: a clue for COVID-19-related subacute thyroiditis. J Endocrinol Invest. 2021;44:1085–1090. doi: 10.1007/s40618-020-01436-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iremli B.G., Sendur S.N., Unluturk U. Three cases of subacute thyroiditis following SARS-CoV-2 vaccine: post-vaccination ASIA syndrome. J Clin Endocrinol Metab. September 2021;106(9):2600–2605. doi: 10.1210/clinem/dgab373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Franquemont S., G J. Subacute thyroiditis after mRNA vaccine for Covid-19. J Endocr Soc. April-May 2021;5(Supplement_1):A956–A957. [Google Scholar]