Abstract
Objective:
Heamophilia is considered a disorder in both children and adolescents which may affect their quality of life seriously than their normal peers; this study investigated the impact of the Neurodynamics Nerve Flossing Technique (NFT) on femoral neuropathy in patients with haemophilia.
Method:
Thirty haemophilic children with Femoral Neuropathy were randomly allocated into two equivalent groups; the study group which received Neurodynamics NFT of the femoral nerve and conventional therapy program, and the control group which received only the conventional therapy program, three sessions/week for 12 weeks. Femoral nerve motor conduction velocity (MCV) and level of pain sensation according to the Visual Analogue Scale (VAS), were assessed pre and post interventions.
Results:
post-treatment comparison between both groups revealed that there was a significant increase in femoral nerve MCV and reduction of pain sensation of the study group compared to the control group (p<0.05).
Conclusion:
Neurodynamics Nerve flossing had a clear effect in the treatment of femoral neuropathy in children with haemophilia.
Keywords: Femoral Nerve, Haemophilia, Nerve Flossing, Neurodynamics, Neuropathy
Introduction
Haemophilia is an inherited disease in which the blood does not clot, caused most commonly by inadequacies of the VIII (FVIII; haemophilia A) and IX (FIX; haemophilia B) coagulation factors, that may cause bleeding for a long time after an injury, and may also encounter internal bleeding, particularly in the joints[1]. Peripheral neuropathy is the most common type of nerve injury in haemophilia, which affected essentially the upper and lower extremities[2]. The iliopsoas, gluteal, gastrocnemius, and forearm muscles are the most common bleeding areas in haemophilia[3], as the iliac and inguinal bleeding in haemophilia may lead to femoral nerve involvement[3,4].
Femoral nerve neuropathy is considered the most frequent nerve injury in haemophilia, because of the iliopsoas haematoma[5]. One of the complications of haemophilia is that the bleeding in joints, muscles, soft tissues causing pseudotumor[6], which may cause compression on the femoral nerve leading to chronic pain and severe disability[7]. The iliopsoas haematoma can cause femoral nerve neuropathy as the volume of the bleeds is usually high in hemophilic patients, with a common presentation of sudden onset of pain which increased in the hip, groin, and inguinal areas that radiated to the anterior aspect of the thigh, and represented also with hip flexion weakness[2,7]. Even small hematoma in close compartments and in the pelvis region could compress the surrounding adjacent organs[8].
The femoral vein and femoral artery are situated medially closely to the femoral nerve laterally, so at the degree of the inguinal ligament in its entrance to the femoral triangle, the compression on the femoral nerve can happen[9,10]. Neurological symptoms in the case of femoral neuropathy like the painful inguinal area as a primary symptom, paresthesia, and muscular weakness which are resulting from bleeding of the iliac muscle, associated usually with hip flexion and extension limitations[11].
The neuropathy symptoms could be improved through the Neurodynamic neural mobilization techniques, as the nervous system had physical properties that pointed to reestablish the mobilized balance between the surrounding mechanical interfaces and the movement of neural tissues, in this manner permitting decreased neural tissue intrinsic pressures and subsequently advancing suitable functions physiologically, additionally to improve the circulation and nutrition to the nerve and improve the nerve normal gliding movements through the increased neural vascularity, the decrease of nerve adherence, and dispersion of noxious fluids[12,13].
Neurodynamic mobilization (NM) otherwise called Nerve Flossing Technique (NFT) which used to treat various disorders of the nervous system concerning the length and mobility of peripheral nerves[14], as the nerve flossing refers to techniques that help to reestablish motion between a nerve and its surrounding soft tissues, thus to treat the nerves that have become entangled within the soft tissue, as it leads to tension release on a nerve by stretching and pulling one end of the nerve during keeping the other end in a relaxed state[15]. There are two common Neurodynamic techniques, the first one is called a “slider technique” which is a flossing technique that done in a gradually controlled way, and the second one is the “tensioner technique” which could be a more vigorous technique that depends on ‘pulls from both ends’ of the nerve, the two techniques could be used as graduation so the NM application could start with the slider technique followed by the tensioner technique[16].
The motor conduction velocity (MCV) of the femoral nerve considered a valid and reliable assessment method, as reported by Mallik and Weir[17] who stated that the nerve conduction study (NCS) could be performed for peripheral neuropathy as a standardized evaluative method, because of its objective in giving data on the nerve condition over the entire body.
However, Femoral Neuropathy had been considered one of the major problem in haemophilic patients, that leading to a prolonged and at times permanent disability so the main objective of this study was to investigate the Neurodynamics NFT influence on motor function and pain sensation in haemophilic patients with femoral neuropathy.
Materials and Methods
Design of the study
The pre and post-experimental design study consisted of two equal groups which were: the study group that received Neurodynamics NFT and the physical therapy conventional program, and the control group that received only the physical therapy conventional program.
Participants
Thirty heamophilic children were recruited from the pediatrics outpatient clinic, October 6 University hospital, and Abo El-Reesh hospital. They were involved in the treatment program three sessions/week for 12 weeks. The inclusion criteria were: all boys were diagnosed and referred by a specialized physician as having the moderate or severe type of hemophilia[18], they were diagnosed as hemophilia A or B, their age was ranging from (12 to 15) years, with bodyweight ranged from (48 to 53) kg, height ranged from (1.42 to 1.58) meter, all the children were able to obey instructions and commands, co-operate with the testing and training protocol, and communicate verbally, while the exclusion criteria were as follow: patients with mild degree hemophilia, patients who had joint pain or muscle bleeding in the lower limb in the preceding three weeks, patients with any other neurological, musculoskeletal disorders or deformities of the lower extremity.
Randomization
All the parents or caregivers of the patients read and signed a consent form before the beginning of the study, the anonymity and confidentiality were assured, and all the procedures were performed in compliance with relevant laws and institutional guidelines, which was approved by the research studies ethical committee. The patients were randomly assigned into two equal groups (study and control group) with the use of a computer-based randomization program. No dropping out of participants from the study was reported after randomization and intervention (Figure 1).
Figure 1.
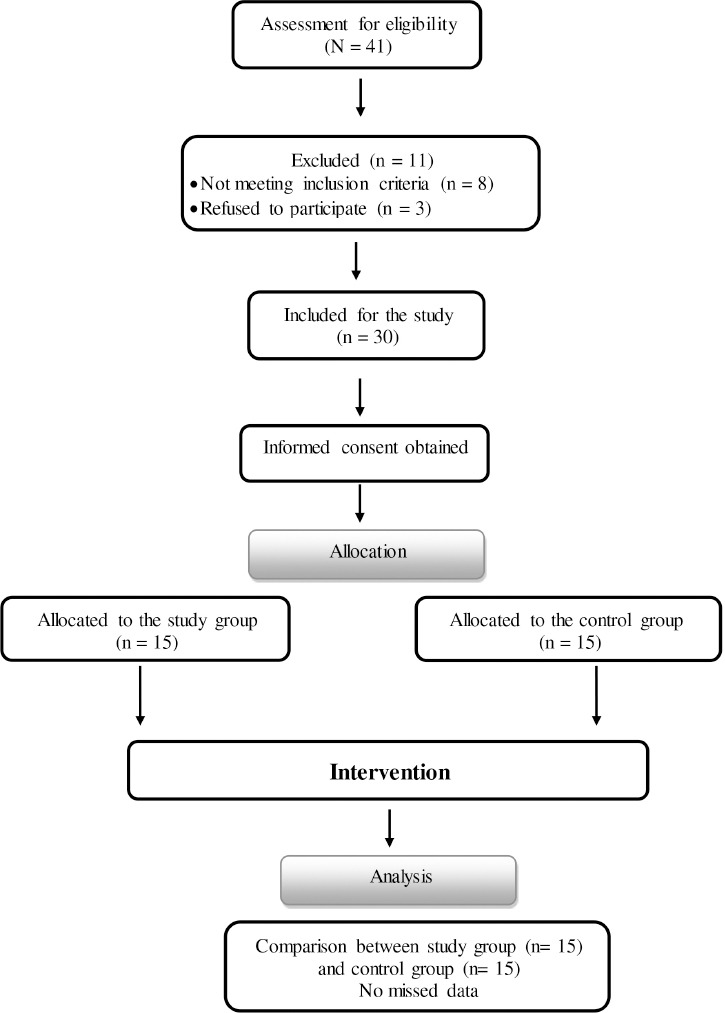
Flow chart showing the experimental design of the study.
Outcomes measures
Femoral Nerve Motor Conduction Velocity
Femoral nerve motor conduction velocity (MCV) was measured via the Neuropack S1 MEB9004 EMG (NIHON KODEN, JAPA) device, as follows: at the central of the rectus femoris, the active recording was placed, and at the patellar upper border, the reference electrode was placed, with the ground electrode placement between both the recording and the stimulation points. While the proximal stimulation point was placed 1 cm lateral to the inguinal femoral artery and the distal stimulation point was applied 10 cm below the proximal stimulation point, also due to the femoral nerve deep position, so the electrode was firmly fixed in its position[19].
Pain Visual Analogue Scale (VAS)
The VAS pain scale is a valid and reliable assessment of pain intensity, as the straight horizontal line of fixed length (10 cm) is considered the simplest VAS, as the distance between the (no pain) anchor and the mark of the patient, giving a scope of values from 1:10 cm[20].
Interventions
All the treatment exercises started after the acute stage subsided and discontinued immediately if the bleeding started again, therefore the treatment included firstly a rest period until the hemostasis had been achieved[5], as the overexertion could lead to injury, so the exercise program started slowly with a graduation at the beginning and progressed into the full program over a period of three to four weeks.
Intervention for the study group
Intervention for the study group who received femoral nerve Neurodynamics NFT with conventional therapy. The NFT procedures were as follows: all the patients received the two neurodynamic NFT, starting firstly with the gentle “slider” technique in the early stage of the program (first 2:3 weeks) then as graduation accompanied with the second technique “tensioner”. Both techniques were performed in the affected limb from prone and side-lying positions as follow: from a prone lying position, the therapist started by neural slider technique as the patient was asked to bend his knee with therapist assistance to guide the movement and stabilize the pelvis, so the patient’s heel came to his bottom, and the patient felt the thigh stretch then relax, with repetitions, then to gradually progress this technique the therapist placed a towel under the knee and repeated the knee bends (Figure 2). While for the neural tensioner technique the same previous steps were done but with adding that the therapist crossed the patient’s other leg behind the affected stretching leg and assisting the patient to push and repeat the action with-holding the stretch[16,21] (Figure 3).
Figure 2.

Femoral nerve Neurodynamics neural slider technique from a prone lying position with a towel under the knee while the patient flexed the knee of the affected side and with the therapist’s assistance to guide the movement and stabilize the pelvis.
Figure 3.

Femoral nerve Neurodynamics neural tensioner technique from a prone lying position with a towel under the knee of the affected side, while the patient’s other leg was crossed behind the affected stretched leg with the therapist’s assistance to push.
While from side-lying position: the therapist started by neural slider technique as the patient was in a side-lying on the non-affected side, and the therapist was positioned behind the patient and asked the patient to bend the above-knee so the heel came to his bottom and to feel the thigh stretch, then the therapist performed extension and adduction of patient’s top hip until the lumbar lordosis level increased and the foot touched the bed as possible with the limit of pain (Figure 4). While for the neural tensioner technique the same steps were performed but with adding that the patient was asked to hold the ankle to his bottom with his hand, then gently pull with therapist assistance so the patient’s knee moved backward and his hip extended causing a stretch, then the patient asked to relax, and repeat the action with holding the stretch[13] (Figure 5). From the previous two positions a graduated (5:10) repetitions for every technique were performed, with 30 seconds hold, and 60 seconds of relaxation between every repetition.
Figure 4.

Femoral nerve Neurodynamics neural slider technique from a side-lying position on the non-affected side. The patient was asked to bend the above-knee, then the therapist performed extension and adduction of the patient’s top hip until the lumbar lordosis level increased.
Figure 5.

Femoral nerve Neurodynamics neural tensioner technique from a side-lying position on the non-affected side. The patient was asked to hold his ankle to his bottom with his hand, then with the therapist’s assistance gently pull backward with hip extension.
The conventional therapy program for the patients of both groups was 60 minutes for each session, in a form of 1-Ultrasound (US) therapy: the application parameters of US was at 3 MHz, with pulsed ratio (1:4), and 1.0 W/cm of intensity 20, for 10 minutes on the groin and anterior and medial aspect of the thigh[22,23]. 2-Pulsed short-wave diathermy (PSWD): This is frequently the treatment option for episodes of bleeding, as the PSWD machines do not emit a continuous beam of energy[24]. The short wave diathermy device (Enraf-Nonius, Curapuls 970) with two flexible capacitive electrodes (12 × 17 cm) was used with the following parameters, Pulsed mode, frequency 27.12 MHz, and power of 240 W[24]. The electrodes were placed over the front part of the thigh using the coplanar technique, as between the electrodes and the skin, the felt protectors with 1 cm of thickness were set to keep away from burning the skin. 3-The flexibility exercises for hip flexors: the patient was lying on his back with the affected leg close to the edge of the bed and the knee bent over the edge of the bed, then the patient was asked to flex the non-affected thigh towards his chest, assisting with his hands, then the therapist instructed the patient to stop as soon as there was a stretching sensation in the affected thigh, and to hold this position with therapist assistance for 30 seconds, then relax, with repetitions of (5:10) times as a graduation[25]. 4-Muscles strengthing exercises: for iliopsoas muscle, the patient was lying on his back with both knees bent, and the therapist’s hand on top of the patient’s knee of affected side, then ask the patient to bend the affected thigh towards his chest against the therapist’s hand, then to hold 10 seconds then relax, gently and gradually increasing the pressure with the limit of pain. While for the quadriceps muscle the patient was lying on his back with a roll under the knee, then the patient was asked to tighten the muscle in front of the thigh, extend the knee and lift the heel, and to hold 10 seconds, then relax, with (5:10) repetitions for every exercise[25].
Statistical Analysis
The IBM SPSS statistical package version 20 for Windows (IBM SPSS, Chicago, IL, USA) was performed for the statistical analysis. The baseline characteristics between groups were compared using the t-test, mean, and standard deviation. The comparison between pre and post scores within and between groups was done via two-way ANOVA. Statistical significance was detected as (P<0.05).
Demographic data
The current study contained thirty patients assigned in a random way into two equivalent groups; the study group and the control group. The demographic data comparison between both groups using the independent t-tests was led for (age, weight, and height), which approved no significant statistical differences between patients in both groups (P>0.05) (Table 1).
Table 1.
Descriptive statistics for the participants’ demographic data for both groups.
| Items | Control Group | Study Group | Comparison | S | |
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | t-value | P-value | ||
| Age (Years) | 13.967± 0.972 | 14.3± 0.819 | 1.0153 | 0.3186 | NS |
| Weight (Kilograms) | 50.733±1.005 | 51.213±1.285 | 1.1394 | 0.2642 | NS |
| Height (Meter) | 1.5040±0.0507 | 1.5193±0.0492 | 0.8407 | 0.4076 | NS |
SD: standard deviation, P: probability, S: significance, NS: non-significant.
Femoral Nerve Motor Conduction Velocity (MCV)
Within and between groups descriptive statistics (mean±SD) and comparison tests for femoral nerve MCV showed in Table 2. There was a significant increase in femoral MCV at post-treatment in comparison to pre-treatment at both groups (control and study); the percentages of improvement were (33.78% and 42.11%) respectively with (p=0.0001). Between groups, the comparison revealed that there was no significant difference pre-treatment between both groups (P>0.05), while post-treatment showed a significant increase in femoral MCV in the study group compared with the control group (p=0.0001).
Table 2.
Mean values of femoral nerve motor conduction velocity pre-treatment and post-treatment test at both groups.
| Femoral Nerve MCV (m/sec) | Pre-treatment | Post- treatment | Mean difference | % of improvement | f-value | P- value |
|---|---|---|---|---|---|---|
| Means ± SD | Means ± SD | |||||
| Control group | 32.9±1.65 | 44.01±0.67 | -11.11 | 33.78% | 850.40 | 0.0001* |
| Study group | 32.68 ±0.915 | 46.44±0.577 | -13.760 | 42.11% | 1303.69 | 0.0001* |
| Mean difference | 0.220 | -2.427 | ||||
| f-value | .333 | 40.547 | ||||
| P- value | 0.566 | 0.0001* |
MCV: motor conduction velocity, m/sec: millimeter/second, SD: standard deviation, %: percentage, P: probability,
Significant level is set at alpha level <0.05
Pain sensation scores on VAS
Within and between groups descriptive statistics (mean±SD) and comparison tests for VAS scores showed in Table 3. There was a significant decrease in pain scores post-treatment compared with pre-treatment at both groups (control and study); the percentages of improvement were (39.86% and 65.094%) respectively with (p=0.0001). Between groups comparison, revealed no significant difference pre-treatment between both groups (P>0.05), while post-treatment revealed a significant reduction in pain scores of the study group compared with that of the control group (p=0.0001).
Table 3.
Mean values of pain sensation (VAS scores) pre-treatment and post-treatment at both groups.
| VAS (cm) | Pre- treatment | Post -treatment | Mean difference | % of improvement | f-value | P- value |
|---|---|---|---|---|---|---|
| Means ± SD | Means ± SD | |||||
| Control group | 7.2±0.676 | 4.33± 0.816 | 2.87 | 39.86% | 100.33 | 0.0001* |
| Study group | 7.066±0.703 | 2.466±0.915 | 4.6 | 65.094% | 285.34 | 0.0001* |
| Mean difference | 0.133 | 1.866 | ||||
| f-value | 0.217 | 42.54 | ||||
| P- value | 0.643 | 0.0001* |
VAS: Visual Analogue Scale, cm: centimeter, %: percentage, SD: standard deviation, P: probability,
Significant level is set at alpha level <0.05.
Discussion
Femoral Neuropathy in Haemophilic patients is considered one of the serious problems that could lead to motor impairment and painful conditions, therefore, the primary purpose of this study was to evaluate the impact of Neurodynamics NFT on the femoral nerve in children with heamophilia, as they were randomly divided into the control group which received the conventional therapy program, and the study group which received the same program in addition to Neurodynamics NFT of the femoral nerve.
The findings of the current study concluded that there were significant improvement in femoral nerve MCV and a significant reduction in pain VAS scores in the study group compared to the control group, the improvement in the femoral nerve MCV may be resulted from axoplasmatic flow normalization, these findings were supported by the work of both Brown et al.[26], and Ellis and Hing[13] who hypothesized that neural mobilization could dissipate the liquids that are destructive to the nerves and enhance axoplasmatic and intraneural flow.
Neural flossing or Neurodynamics, aimed at improving the mobility to different tracts of the nervous system (NS) and reestablishing the homeostasis around and inside the NS[27]. Anikwe et al.[28], showed that in the case of acute sciatica the NFT reduced the symptoms and increased range of motion of the hip, this finding agrees with a previous study[29] which concluded that the combination of NFT and Physiotherapy Conventional treatment was more beneficial in motor function improvement and reducing pain in neuropathic conditions, also a study by Bonser et al.[30], reported that in the comparison of Neurodynamic sliders techniques targeting the sciatic nerve with the traditional stretching, the findings found that the sliders technique was more effective than static traditional stretching in increasing hamstring flexibility.
Santana et al.[31], who studied the effects of NM on peripheral nerve regeneration in the peripheral nerve injury, stated that there were many causes, including nerve mechanical characteristics, that could impact the process of regenerating the nerve as the decrease of nerve mechanosensitivity, intraneural edema, viscoelasticity, and the adhesion to the interfaces of the neural tissue, might be a target to move toward that force loads mechanically to the nerve, this previous study proposed that the NM could enhance the axon regeneration of peripheral nerve by the following mechanisms: a) edema resolution; b) axoplasmatic flow normalization; c) irregular nerve mechanosensitivity reduction, with a reduction of neurogenic inflammation and hyperalgesia; d) improvement of nerve mobility, diminishing the trauma occurrence; e) improvement of Schwann cells (glial) activity in the cell membrane, by the activated movement dependent receptors.
Muscle bleedings in haemophilia commonly in the iliopsoas section, cause significant pain and affect motor activities, as when the pressure on the iliopsoas was elevated by the hematoma, it could compress the nerves running through the pelvis and lead to neuropathy[32]. Therefore the significant decrease in pain intensity post-NFT in the current study could be due to that in the theory of gate control, the mechanoreceptors activation within the joint capsule and surrounding tissues results in diminishing pain at the spinal cord, besides, within the pain-free nerve movement of NFT, it could assist also in reducing entrapment, friction and stress on the nerve and, hence, diminishing its mechanosensitivity[29].
On the other hand, the positive improvement of the MCV and pain sensation in the control group may be as a result of the pulsed US mechanism that enhances the quality of repair in the inflammatory, remodeling, and proliferation stages of the healing process[22,23], also the PSWD diathermy that could improve the extensibility of the soft tissue, enhances the electrophysiological parameters, amount of fiber myelination, and diameter of the axons[33], besides the effect of the stretching exercises that improve tissue extensibility and relieve pain[25], while the strengthening exercises enhance the motor units recruitments and so could improve the neural impulses which increase nerve conduction velocity[25]. The limitation in this study was the inability to investigate the long-term effect of NM on quality of life due to lack of follow up after the treatment period, hence for future studies, it would be beneficial to include the long-term effect of NM on quality of life in haemophilic patients with peripheral neuropathy.
Conclusion
The Neurodynamics Nerve Flossing should be considered as an effective physical therapy intervention in Haemophilic Patients with femoral neuropathy, as it showed a significant improvement in motor function outcomes and a significant reduction in pain scores.
Ethical approval for the study
The Institutional Ethics Committee of the Faculty of Physical Therapy, was approved the study (No: P.T./REC /012/002733), and clinical trials.gov ID NCT04448275.
Footnotes
The authors have no conflict of interest.
Edited by: G. Lyritis
References
- 1.Chandy M. Management of hemophilia with minimal factor replacement in developing countries:role of ancillary therapy. Semin Thromb Hemost. 2005;31:501–6. doi: 10.1055/s-2005-922220. [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez-Merchan EC. Peripheral nerve injuries in haemophilia. Blood Transfus. 2014;12(Suppl):S313. doi: 10.2450/2012.0111-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saraf SK, Singh OP, Singh VP. Peripheral nerve complications in hemophilia. J Assoc Physicians India. 2003;51:167–9. [PubMed] [Google Scholar]
- 4.Balkan C, Kavakli K, Karapinar D. Iliopsoas haemorrhage in patients with haemophilia:results from one centre. Haemophilia. 2005;11:463–7. doi: 10.1111/j.1365-2516.2005.01123.x. [DOI] [PubMed] [Google Scholar]
- 5.Beeton K, Rodriguez-Merchan EC, Alltree J, Cornwall J. Rehabilitation of muscle dysfunction in hemophilia. 2012:24. [Google Scholar]
- 6.Sahu KK, Varma SC, Malhotra P, Prakash G, Khadwal A. Hemophilia, Complications and Management:Series of 3 Cases with a Brief Review of Literature. J Clin Case Rep. 2013;4:325–2. [Google Scholar]
- 7.Kamal AF, Pradana AS, Prabowo Y. Bilateral iliopsoas haemophilic “soft tissue pseudotumours”:A case report. Int J Surg Case Rep. 2015;13:19–23. doi: 10.1016/j.ijscr.2015.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sahu KK, Mishra AK, Zhang P. Femoral neuropathy:a rare presentation of retroperitoneal hematoma with review of literature. Indian J Hematol Blood Transfus. 2020;36(1):174–177. doi: 10.1007/s12288-019-01126-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee S, Shin K, Gil Y, Ha T, Koh K, Song W. Anatomy of the lateral femoral cutaneous nerve relevant to clinical findings in meralgia paresthetica. Muscle Nerve. 2017;55:646–50. doi: 10.1002/mus.25382. [DOI] [PubMed] [Google Scholar]
- 10.Petchprapa CN, Rosenberg ZS, Sconfienza LM, Cavalcanti CFA, La Rocca Vieira R, Zember JS. MR imaging of entrapment neuropathies of the lower extremity:part 1. the pelvis and hip. Radiographics. 2010;30:983–1000. doi: 10.1148/rg.304095135. [DOI] [PubMed] [Google Scholar]
- 11.Kang BS. Acute femoral neuropathy secondary to iliacus hematoma. J Korean Neurosurg Soc. 2006;17:361–5. [Google Scholar]
- 12.Shacklock M. Clinical neurodynamics:a new system of musculoskeletal treatment:Elsevier Health Sciences. 2nd ed. New York: Butterworth-Heinemann; 2005. p. 251. [Google Scholar]
- 13.Ellis RF, Hing WA. Neural mobilization:a systematic review of randomized controlled trials with an analysis of therapeutic efficacy. J Man Manip Ther. 2008;16:8–22. doi: 10.1179/106698108790818594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sharma S, Balthillaya G, Rao R, Mani R. Short term effectiveness of neural sliders and neural tensioners as an adjunct to static stretching of hamstrings on knee extension angle in healthy individuals:a randomized controlled trial. Phys Ther Sport. 2016;17:30–7. doi: 10.1016/j.ptsp.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 15.Nunes GS, Uhlig S, Ribas LMDA, Gonçalves FB, Wageck B, De Noronha M. Influence of neural mobilization of lower limbs on the functional performance and dynamic balance in asymptomatic individuals:a cross-over randomized controlled trial. Hum Mov. 2017;18:10–6. [Google Scholar]
- 16.Coppieters MW, Butler DS. Do 'sliders'slide and 'tensioners'tension?An analysis of neurodynamic techniques and considerations regarding their application. Man Ther. 2008;13:213–21. doi: 10.1016/j.math.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 17.Mallik A, Weir AI. Nerve conduction studies:essentials and pitfalls in practice. J J Neurol Neurosurg Psychiatry. 2005;76:ii23–ii31. doi: 10.1136/jnnp.2005.069138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Benson G, Auerswald G, Dolan G, Duffy A, Hermans C, Ljung R, et al. Diagnosis and care of patients with mild haemophilia:practical recommendations for clinical management. Blood Transfus. 2018;16:535. doi: 10.2450/2017.0150-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leis AA, Schenk MP. Oxford University Press. 2nd ed. New York: Oxford Univ Press; 2013. Atlas of nerve conduction studies and electromyography. [Google Scholar]
- 20.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain:Visual analog scale for pain (vas pain), numeric rating scale for pain (nrs pain), mcgill pain questionnaire (mpq), short-form mcgill pain questionnaire (sf-mpq), chronic pain grade scale (cpgs), short form-36 bodily pain scale (sf-36 bps), and measure of intermittent and constant osteoarthritis pain (icoap) Arthritis Care Res. 2011;63:S240–S252. doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 21.Gilbert KK, Roger James C, Apte G, Brown C, Sizer PS, Brismée J-M, et al. Effects of simulated neural mobilization on fluid movement in cadaveric peripheral nerve sections:implications for the treatment of neuropathic pain and dysfunction. J Man Manip Ther. 2015;23:219–25. doi: 10.1179/2042618614Y.0000000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morishita K, Karasuno H, Yokoi Y, Morozumi K, Ogihara H, Ito T, et al. Effects of therapeutic ultrasound on range of motion and stretch pain. J Phys Ther Sci. 2014;26:711–5. doi: 10.1589/jpts.26.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Higginbottom M, Leckie V. Electrotherapy and its Use in Haemophilia. Physiotherapy Management of Haemophilia. 2000:39–50. [Google Scholar]
- 24.Masiero S, Pignataro A, Piran G, Duso M, Mimche P, Ermani M, et al. Short-wave diathermy in the clinical management of musculoskeletal disorders:a pilot observational study. Int J Biometeorol. 2019:1–8. doi: 10.1007/s00484-019-01806-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Strike K, Mulder K, Michael R. Exercise for haemophilia. Cochrane Database Syst Rev. 2016;12:12. doi: 10.1002/14651858.CD011180.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brown CL, Gilbert KK, Brismee J-M, Sizer PS, Roger James C, Smith MP. The effects of neurodynamic mobilization on fluid dispersion within the tibial nerve at the ankle:an unembalmed cadaveric study. J Man Manip Ther. 2011;19:26–34. doi: 10.1179/2042618610Y.0000000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Basson A, Olivier B, Ellis R, Coppieters M, Stewart A, Mudzi W. The effectiveness of neural mobilization for neuromusculoskeletal conditions:a systematic review and meta-analysis. J Orthop Sports Phys Ther. 2017;47:593–615. doi: 10.2519/jospt.2017.7117. [DOI] [PubMed] [Google Scholar]
- 28.Anikwe EE, Tella BA, Aiyegbusi AI, Chukwu SC. Influence of Nerve Flossing Technique on acute sciatica and hip range of motion. Int J Med Biomed Res. 2015;4:91–9. [Google Scholar]
- 29.Pallipamula K, Singaravelan RM. Efficacy of nerve flossing technique on improving sciatic nerve function in patients with sciatica :a randomized controlled trial. Rom. J. Physical Ther. 2012;18(30):13–22. [Google Scholar]
- 30.Bonser RJ, Hancock CL, Hansberger BL, Loutsch RA, Stanford EK, Zeigel AK, et al. Changes in Hamstring Range of Motion Following Neurodynamic Sciatic Sliders:A Critically Appraised Topic. J Sport Rehabil. 2016;26(4):311–315. doi: 10.1123/jsr.2015-0166. [DOI] [PubMed] [Google Scholar]
- 31.Santana HHS, de Oliveira IA V, Medrado AP, Nunes SáK. Neurodynamic Mobilization and Peripheral Nerve regeneration:A narrative review. Int J Neurorehabil. 2015;2(2):1–7. [Google Scholar]
- 32.Beyer R, Ingerslev J, Sørensen B. Current practice in the management of muscle haematomas in patients with severe haemophilia. Haemophilia. 2010;16:926–31. doi: 10.1111/j.1365-2516.2010.02275.x. [DOI] [PubMed] [Google Scholar]
- 33.Fu T, Lineaweaver WC, Zhang F, Zhang J. Role of shortwave and microwave diathermy in peripheral neuropathy. J Int Med Res. 2019;47:3569–79. doi: 10.1177/0300060519854905. [DOI] [PMC free article] [PubMed] [Google Scholar]


