Abstract
Objectives:
Children with Duchene muscular dystrophy have weak muscles, which may impair postural adjustments. These postural adjustments are required for gait and dynamic balance during the daily living activities. The aim was to compare between the effect of bicycle ergometer versus treadmill on functional walking capacity and balance in children with Duchenne muscular dystrophy.
Methods:
Thirty boys aged from 6 to 10 years old diagnosed as Duchene muscular dystrophy participated in this study. Children were assigned randomly into two groups (A&B). Children in group (A) underwent a designed program of physical therapy plus aerobic exercise training in form of bicycle ergometer while, group (B) received the same program as group (A) and aerobic exercise training by treadmill for one hour, at three times a week for three successive months. Functional walking capacity and balance were assessed before and after treatment by using the 6-minute walk test and Biodex balance system equipment respectively.
Results:
The post treatment results revealed significant difference in all measured variables (P<0.05) as compared with its pre-treatment results. Post-treatment values indicated that there was a significant difference in all measured variables in favor of group B.
Conclusions:
treadmill training as an aerobic exercise can improve walking capacity and balance more effectively than bicycle ergometer in children with Duchenne muscular dystrophy.
Keywords: Balance, Bicycle Ergometer, Duchene Muscular Dystrophy, Functional Walking Capacity, Treadmill
Introduction
Duchenne muscular dystrophy (DMD) is a progressive type of muscular dystrophy that occurs mainly in males, although in rare conditions may affect females. DMD leads to progressive muscle weakness including skeletal and heart muscles[1]. Dystrophin absence causes a steady degradation of muscle fibers that leads to progressive loss of muscle strength and functional abilities; So, Exercises that help to improve balance and coordination are essential to any rehabilitation exercise program2.
Our primary goal in treating boys with DMD is to help them to preserve their functional abilities as long as we can[3]. Delaying loss of functional abilities is important for all daily life activities and can increase independence in boys with DMD. The gradual loss of the functional abilities during the course of this disease is mainly due to a progressive decrease in muscle strength and endurance[4,5]. Also, a secondary reduction of physical activity occurs due to limited physical and social activity. When the amount of energy cost a certain activity needs increases, the frequency of falling (with the need for help to stand up) increases, and the developing fear of falling leads to reduction of leg and arm functional abilities, which causes disuse of musculoskeletal and cardiorespiratory systems[6].
Physical therapy acts in a multidisciplinary approach aiming to give supportive therapy to these patients. Treadmill walking is used to improve adaptive mechanisms that are needed for coordination, body orientation, and balance control[7]. The treadmill stimulates the stepping movements in a manner that is repetitive and rhythmic while the patient takes the upright position and bearing his body weight on his lower limbs[8]. Treadmills are considered a continuous- controlled way that attracts both clinicians and researchers. They are used in the clinical field, targeting to improve over ground gait and have been used in research to imitate normal ground walking[9].
Cycle pedal is considered as an aerobic exercise and it is a repetitive, functional activity that depends on reciprocal contraction of agonist and antagonist muscles of the lower limbs in a repeated pattern as that of walking[10]. Cycling exercise is an easy functional treatment method that can be used to motor skills relearning needed for locomotion[11,12]. Cycling is done in sitting position what makes it safe, easy to perform, and can be widely applied regardless of the severity of motor impairment[13]. So, the purpose of this study was to compare between the effects of aerobic exercise training by bicycle ergometer and by treadmill on functional walking capacity and balance in children with DMD.
Materials and methods
Study design
A randomized - controlled trail was carried out in accordance with the Code of Ethics of the World, Medical Association (Declaration of Helsinki) for experiments involving humans and randomized into two equal groups (A & B). Group A received designed program of physical therapy plus an aerobic exercise training by bicycle ergometer while, group B received the same designed program of physical therapy plus an aerobic exercise training by treadmill for three months. Participants, parents/legal guardians provided written informed consent before the study was conducted.
Participants
A convenient sample of thirty boys was selected from Abu El-Rish Pediatric Hospital and Out-patient Clinic, Faculty of Physical Therapy, Kafr El-Sheikh University. They have been screened and included if they were: 1) diagnosed as Duchene muscular dystrophy, 2) aged from 6 to 10 years, 3) having grade 3+ muscle strength in lower limbs and trunk muscles according to Kendall et al.[14], 4) had functional range of motion for upper and lower limb joints, 5) able to walk alone level I and II of Ambulation function classification system for DMD (AFCSD)[15]. Participants are excluded if they had any of the following; 1) congenital or acquired skeletal deformities or cardiopulmonary dysfunction, 2) had undergone previous orthopedic surgery in lower limbs, 3) had abnormal motor development or neurological disease that affect balance and gait, and 4) behavioral problems causing inability to cooperate during the study.
Randomization
Before randomization, five children were excluded, three children were excluded as they did not meet the inclusion criteria and two children were chosen to take their consent and cancel their participation in the study. The children were randomly assigned into two equal groups via the envelope mode. After patients’ agreement to participate in the study, cards with either “bicycle ergometer” or “treadmill training” recorded on them were closed in envelopes; then a blinded physical therapist was asked to select one envelope. According to the selected card, children were assigned to their corresponding group. Dates for starting the allocated therapy were regulated and the therapy was begun after the first week of randomization. The examiner physical therapist was not included in randomization procedures and was unaware of the therapy allocation. Children were asked not to disclose their therapy allocation to the physical therapist during assessment. The participants were informed to report any harmful effects throughout the treatment period (Figure 1).
Figure 1.
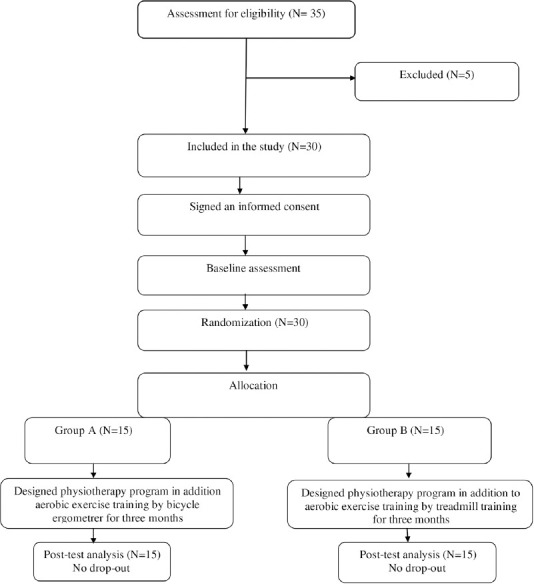
Flow chart demonstrates the experimental design of the study.
Methods and Procedures
Evaluation procedures
Biodex balance system equipment
Biodex Stability System (BSS; Biodex, Inc, Shirley, NY) was used to assess the dynamic balance of all children in the two tested groups which gives an objective assessment of balance[16]. The BBS has an intertester intraclass correlation coefficients (ICCs) equals 0.70 and an intratester ICCs equals 0.82[17]. BSS formed of a dynamic platform that allows movements to occur around the anterior-posterior (AP) and mediallateral (ML) axes simultaneously. This dynamic platform offers eight different levels (1-8) of stability, with level 8 which is considered the most stable and level 1 which is the least stable. Also, BSS has a screen displaying the child position on it and a support handles that can be adjusted according to each child’s height. The screen gives a visual feedback about the degree of tilting that helps the child to maintain the cursor in the center of the screen to obtain a good score of balance. The BSS measures the degree of tilting in all axis during dynamic position and calculates all the indices (a mediolateral stability index (MLSI), an anterior-posterior stability index (APSI) and overall stability index (OSI)), which is the sum of both MLSI and APSI[18]. The BSS determines the average position for each child during all movements through the test. The higher scores in all these indices, the poorer the balance of the child. The child was asked to stand with his/her two legs stance in the middle of the locked platform. Specific parameters like the child’s age, weight, height and stability level (firmness of platform) were entered to the device. During the evaluation, the platform moves freely and simultaneously calculates the degree of tilt about both axes (AP and ML). The balance measurement test was repeated 3 times and the mean of the three repetitions was obtained for data analysis. High values mean that the child had balance difficulty[19].
2- The 6-minute Walk Test (6MWT)
6MWT is a simple, standardized walking test that is used to assess the functional ability in children[20]. It can be applied easily, good tolerated by the children, and gives good reflection of the daily living activities and the functional capacity more than other walking tests[21]. It has a high reliability (r value=0.955 and P value<0.0001) that can be used in ambulatory children with spastic CP; it provides clinical information concerning gait capabilities[22]. Children in both groups completed the test as illustrated in the American Thoracic Society (ATS) statement[23]. Evaluation procedures took place on a thirty-meter long straight corridor with flat and hard surface, without any obstacles in it and every child was allowed to use his comfortable footwear. Verbal instructions or words of encouragement that allowed by the ATS guideline were given to all participants during the test procedure which permits one comment every minute. Before the beginning of test procedures, children were informed that “the purpose of the test is to walk for 6 minutes as far as possible.” During the testing procedure, the evaluator walked behind the child to protect him but without affecting his speed. At the end of test, the distance in meter that the child covered was recorded.
Treatment procedures
The children in both groups (A & B) received a designed physical therapy treatment program. It was applied for 1 hr. / three times per week for three successive months.
This program included the following: Gentle stretching exercises before starting aerobic exercise to prevent the development of any tightness. Stretching was performed for biceps brachii, hamstrings and calf muscles bilaterally. It was applied for 20 s stretching followed by 20 s relaxation and repeated five times for every muscle. In addition to, Isometric muscle contraction was applied for quadriceps, hamstrings, anterior tibial group, calf muscles, biceps and triceps muscles. Every muscle contraction was sustained for 5 s then relaxed for another 5 s, and repeated for five times[24,25]. Also, gait and balance exercise training with obstacles were done. Furthermore, both groups (A&B) received the following:
Group A: Children were trained on the bicycle ergometer for 20 min, at 3 times a week for 3 successive months[26]. Bicycle ergometer (Monark Rehab Trainer model 88 IE) is an electronic ergometer. It contains an electronic meter giving us data about pedal revolutions per min, total pedal revolution and time function. The bicycle has a pedal strap to provide full fixation of the child’s foot and back support in order to fix and prevent excess exhaustion of the back muscles. The training program starts with warm-up exercises in form of a light stretch exercise and walking back and forth for 5 minutes. Next, the child was asked to sit on the bicycle seat and grasp both handles of the bicycle tightly with the back erect and supported. Then, Climb steady program was selected. In this program the resistance is increased gradually according to the muscle power of every child. This program was selected as it was the most suitable one for the present disorder of those children. Applying resistance comes in agreement with the results that confirmed the necessity of resistance training for children with DMD as they have demonstrated decreased anaerobic capacity and strength when compared with their healthy peer children[27]. The child was instructed to do a warm up exercise in the form of a low intensity pedaling movement on a bicycle ergometer for 5 min. Then, pedaling resistance was increased for another 10 min. Finally, the treatment session ended with unloaded cycling for another 5 min as a cooling down exercise[26]. The child was informed to stop exercising immediately if there are any symptoms of pain, fatigue or shortness of breath.
Group B: Children underwent an aerobic exercise program in the form of treadmill training for 20 min. Treadmill apparatus (En Tred) is a steel made device; its length is 2.4 meter (m) and its width is ½ m. It is composed of supporting belt made of synthetic rubber and nylon (3.75 m in length), cylinders (two) and an axle along its width. Also, it has vertical beams attached to parallel bars on each side with the height of the parallel bars are adjusted according to the height of every child. All steps and aims of exercise were explained to all children. The exercise training started with 5 min warm-up exercises involving a light stretch and walking back and forward inside the room. Then, the child asked to grasp both parallel bars of the treadmill by his hands tightly and asked to look forward during walking to avoid falling. At first the child asked to hold the treadmill rails with both hands and then by one hand only till he/she had the confidence and walk on treadmill without any need for support. The treadmill exercise training was practiced at 75% of over ground speed and with an inclination at zero degree for about 20 min, at three times a week for 3 successive months[28]. The child was instructed to stop the exercise at once if there is pain, fatigue, or shortness of breath. Finally, cooling down exercises was performed for 5 min.
Statistical analysis
Results were expressed as mean ± standard deviation (SD). A two-way mixed design MANOVA was run with two independent variables - intervention and measuring periods- and four dependent variables (Medio-lateral stability, Anteroposterior stability, overall stability and six min walking test). There was a linear relationship between the dependent variables, as assessed by scatterplot, and no evidence of multicollinearity, as assessed by Pearson correlation (|r|<0.9). There were no univariate outliers in the data, as assessed by inspection of a boxplot, and no multivariate outliers in the data, as assessed by Mahalanobis distance (p>.001). Medio-lateral stability, Antroposterior stability, overall stability and six min walking test were normally distributed, as assessed by Shapiro-Wilk’s test (p>.05). There was homogeneity of covariance matrices, as assessed by Box’s M test (p=.009), and homogeneity of variances, as assessed by Levene’s Test of Homogeneity of Variance (p>.05). Statistical Package for Social Sciences (SPSS) computer program (version 23 windows) was used for data analysis. P value ≤0.05 was considered significant and <0.01 was considered highly significant.
Results
A total of 30 participants were eligible for inclusion, and were randomized for study intervention. Group A consisted of 15 participants who received designed physical therapy program in addition to aerobic exercise training by bicycle ergometer and group B consisted of 15 participants who received the same designed physical therapy program in addition to aerobic exercise training by treadmill three sessions per week for one hour for three successive months. All randomized participants completed the trial. The groups were similar at baseline (p>0.05) with regard to gender distribution, age, height and weight (Table 1).
Table 1.
General characteristics of participants.
| Group A (n=15) | Group B (n=15) | P value | |
|---|---|---|---|
| Age (yrs.) | 8.34±0.88 | 8.49±0.83 | 0.629NS |
| Weight (Kg) | 31.66±2.84 | 32.6±2.79 | 0.347NS |
| Height (Cm) | 124.13±3.2 | 125.54±2.33 | 0.228NS |
NSP>0.05=non-significant, P=Probability.
The interaction effect between type of intervention and measuring period on the combined dependent variables was statistically significant, F=9.012, p=.0001, Wilks’ Λ=0.41, partial η2=0.59. There was statistically no significant effect of intervention on the combined dependent variables, F=1.519, p=0.227, Wilks’ Λ=.848, partial η2=0.196. While, there was a statistically significant main effect of measuring periods on the combined dependent variables, F=185.60, p=0.001, Wilks’ Λ=0.033, partial η2=0.967. Multiple pairwise comparison tests (Post hoc tests) showed that the Medio-lateral stability, Anteroposterior stability and overall stability showed a significant reduction (p<0.05) within both groups, while the six min walking test showed a significant increase (p<0.05) within both groups. Comparing both groups post-program revealed a statistically significant reduction in Medio-lateral stability, Anteroposterior stability and overall stability and significant increase in six min walking test (p<0.05) in favor to group B in comparison to group A (Table 2).
Table 2.
Descriptive statistics and 2x2 mixed design Multivariate Analysis of Variance (MANOVA) for all dependent variables at different measuring periods at both groups.
| Group A (n=15) | Group B (n=15) | P value* | ||
|---|---|---|---|---|
| ML stability | Pre-program | 3.59 ± 0.47 | 3.58 ± 0.38 | 0.967NS |
| Post-program | 2.78 ± 0.4 | 2.52 ± 0.3 | 0.04S | |
| P value** | 0.001HS | 0.04S | ||
| AP stability | Pre-program | 3.85 ± 0.35 | 3.99 ± 0.36 | 0.295NS |
| Post-program | 2.93 ± 0.43 | 2.57 ± 0.26 | 0.01HS | |
| P value** | 0.001HS | 0.04S | ||
| Overall stability | Pre-program | 3.69 ± 0.77 | 3.66 ± 0.49 | 0.868NS |
| Post-program | 2.9 ± 0.4 | 2.67 ± 0.17 | 0.04S | |
| P value** | 0.001HS | 0.04S | ||
| Six-minute walking test | Pre-program | 324.53 ± 28.57 | 320.6 ± 28.08 | 0.707NS |
| Post-program | 391.86 ± 30.76 | 428.66 ± 22.94 | 0.001HS | |
| P value** | 0.001HS | 0.04S |
Inter-group comparison;
intra-group comparison of the results pre- and post-program. NSP>0.05 = non-significant, HSP<0.01 = highly significant, P=Probability, ML: Medio lateral stability, AP: Anteroposterior stability.
Discussion
This study aimed to compare between the effects of bicycle ergometer versus treadmill on functional walking capacity and balance in children with DMD. However, numerous studies evaluated the effects of treadmill and bicycle ergometer on children with DMD, but to our knowledge, this study is the first to compare the effects of treadmill to bicycle ergometer on functional gait and balance in these populations with selected inclusion criteria.
Pre-treatment mean values of dynamic balance test (overall, anteroposterior and medio-lateral) stability indices in both groups revealed non-significant differences but showed significant increase in their values. Also, pre-treatment mean values of Six minute walking test in both groups showed non-significant differences but showed a significant decrease in their values in comparison to the normal values of the children in the same age group which indicated that they had gait problems.
The post treatment results of this study showed improvement of all measured variables in favor of group B (received treadmill training). The results indicated that treadmill training produced significant improvement in functional walking capacity and balance comparing with bicycle ergometer training. As children with DMD have impaired functional walking and balance disorders due to progressive muscle weakness[29]. Balance disorders in these children limits daily living activities especially walking so, the evaluation of balance is an essential item to direct management[30].
The pretreatment results revealed that there are Balance disorders and impaired functional walking capacity among children with DMD. These findings come in agreement with Holland et al. who found that balance problems and loss of functional walking due to progressive muscle weakness, decrease in muscle endurance and aberrant repair of the muscle tissue are caused by chronic inflammatory response[31].
Post treatment improvement of balance and functional walking in both groups could be attributed to increasing in muscle strength and enhanced coordination between both sides of the body. This is supported by Karimi et al.[32] who reported that we need intact neuromuscular system and sufficient muscle power to bring the center of mass within the base of support when balance is distributed which considered as a suitable motor response. Also, designed physical therapy treatment program might be one cause of significant results in both groups that were reinforced by Petrof and Lim et al. who reported physical training program in form of aerobic exercises might delay secondary functional deterioration of DMD which was caused by a disuse and limited activities but eccentric exercises or high-resisted exercises are avoided[33,34].
The results of the current study were reinforced by those of Bushby et al, who concluded that Current international guidelines recommend regular submaximal activities for boys with DMD[35]. Also, balance improvement occurred in both groups was supported by the findings of Guskiewicz who reported that various muscle groups, including those around the ankle, thigh, trunk and neck is needed to maintain a good postural balance, a motor response to the sensorimotor information[36].
The results of previous studies that were applied on exercise program with cyclic ergometer on spina bifida children and stroke patients agree with our results as there was improvement in both gait parameters and muscle performance so, This effect on muscle strength is further confirmed by the fact that trained patients usually experience a feeling of muscle fatigue after treatment, indicating that exercise training on bicycle ergometer not only guides the movement passively, but it also leads to active participation of lower limb muscles[37,38].
Also, the current study showed that the significant improvement in group A comes in agreement with Benecke et al.[39] who mentioned that the spinal cord circuit responsible for the gait acts in a symmetrical way and the symmetrical movement pattern generated by the bicycle ergometer can make the affected muscles work more effectively and in a more normal temporal way.
The improvement of balance and functional walking occurred in group B may be due to the treadmill training and regular physical therapy program as, the low intensity treadmill training was physiologically beneficial[40,41]. This improvement can be attributed to practicing stepping movements by treadmill which lead to strength and stabilize the involved neural network in producing gait pattern.
Also, functional walking improvement in group B might occur as when the child transfers weight from one leg to the other leg during walking on treadmill that helps in improving the specific mechanism which is responsible for the postural control to maintain the balance. This comes in agree with Ulrich et al.[42] and Dal et al.[43] who mentioned that treadmill training can give many chances to improve balance and strength in muscles of lower limbs and make stimulation to the neuronal connections that are involved in generation of independent balanced walking.
Previous studies concluded that Treadmill training has a positive effect on both spatial and temporal gait parameters especially the temporal pattern as reported by Kubo and Ulrich[44]. More improvement occurred in group B than group A in functional walking and dynamic balance may be due to increases the stress on the tibiofemoral and patellofemoral surfaces that lead to increasing the quadriceps force required to maintain available extension against gravity as result of weight bearing on a flexed knee but also. So, Treadmill differs from walking over ground as the treadmill requires from children to stay for long time with both feet contacting treadmill surface during walking cycle which helps them to improve their walking capacity and balance[45].
The main reason for improvement in group B may be due to increasing the base of support during treadmill training which is considered an important factor that helps to improve stability and balance[45].
Finally, the more significant post treatment improvement recorded in favor of group B was reinforced by Tulchin et al. who stated that, patients receiving treadmill training will have their walking endurance, gait stability, muscle function, aerobic fitness and balance increased to a big degree than others and their habitual activity levels will be higher[46].
Study limitation
The current study was delimited by the small sample size.
Conclusion
The results of the current study suggested that both bicycle ergometer and treadmill training have the ability to make a significant improvement in functional walking capacity and balance in Duchenne muscular dystrophy children. Moreover, treadmill training has been realized as being significantly more effective than bicycle ergometer in improving functional walking capacity and balance for those children.
Authors’ contributions
A.A; H.G. and M.A. was involved in the study concept and design, interpretation of data, and writing of the initial and final drafts of the article. H.G. and A.A. and M.A. were involved in data acquisition and analysis. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Footnotes
The authors have no conflict of interest.
Edited by: G. Lyritis
References
- 1.Van Essen A, Busch H, Meerman G, Kate L. Birth and population prevalence of Duchenne muscular dystrophy in The Netherlands. Hum Genet. 1992;88:258–266. doi: 10.1007/BF00197256. [DOI] [PubMed] [Google Scholar]
- 2.Hoffman E, Brown R, Kunkel L. Dystrophin:the protein product of the Duchene muscular dystrophy locus 1987. Biotechnology. 1992;24:457–466. [PubMed] [Google Scholar]
- 3.Eagle M. Report on the muscular dystrophy campaign workshop:exercise in neuromuscular diseases Newcastle, January 2002. Neuromuscul Disord. 2002;12:975–983. doi: 10.1016/s0960-8966(02)00136-0. [DOI] [PubMed] [Google Scholar]
- 4.McDonald C, Abresch R, Carter G, Fowler W, et al. Profiles of neuromuscular diseases. Duchenne muscular dystrophy. Am J Phys Med Rehabil. 1995;74:70–92. doi: 10.1097/00002060-199509001-00003. [DOI] [PubMed] [Google Scholar]
- 5.Bar-or O, Rowland T. Neuromuscular and musculoskeletal diseases. Pediatric Exercise Medicine from Physiologic Principles to Health Care Application. Human Kinetics. 2004:269–303. [Google Scholar]
- 6.McDonald C. Physical activity, health impairments and disability in neuromuscular disease. Am J Phys Med Rehabil. 2002;81:108–120. doi: 10.1097/00002060-200211001-00012. [DOI] [PubMed] [Google Scholar]
- 7.De Nunzio A, Zanetti C, Schieppati M. Post effect of forward and backward locomotion on body orientation in space during quiet stance. Eur J Appl Physiol. 2009;105:297–307. doi: 10.1007/s00421-008-0903-7. [DOI] [PubMed] [Google Scholar]
- 8.Marc E, Garcez M, William P, et al. Oxidative stress and hematologic and biochemical parameters in individuals with DS. Mayo Clin Proc. 2005;80(12):1607–11. doi: 10.4065/80.12.1607. [DOI] [PubMed] [Google Scholar]
- 9.Collett J, Dawes H, Howells K, et al. Anomalous centre of mass energy fluctuations during treadmill walking in healthy individuals. Gait Posture. 2007;26:400–6. doi: 10.1016/j.gaitpost.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 10.Raasch C, Zajac F. Locomotor strategy for pedaling:muscle groups and biomechanical functions. J Neurophysiol. 1999;82:515–25. doi: 10.1152/jn.1999.82.2.515. [DOI] [PubMed] [Google Scholar]
- 11.Hunt K, Stone B, Negard N, et al. Control strategies for integration of electric motor assist and functional electrical stimulation in paraplegic cycling:utility for exercise testing and mobile cycling. IEEE Trans Neural Syst Rehabil Eng. 2004;12:89–101. doi: 10.1109/TNSRE.2003.819955. [DOI] [PubMed] [Google Scholar]
- 12.Takahashi T, Takazawa M, Nishiyama Y, et al. FES cycling chair for the lower limbs disabled people with electric motor power assist. In:Proceedings of the 9th annual international FES society conference, Sep 6-9;2004, Bournemouth, UK. :247–9. [Google Scholar]
- 13.Brown D, Kautz S, Dairaghi C. Muscle activity adapts to anti-gravity posture during pedalling in per sons with post-stroke hemiplegia. Brain. 1997;120:825–37. doi: 10.1093/brain/120.5.825. [DOI] [PubMed] [Google Scholar]
- 14.Kendall F, McCreary E, Provance P, et al. Muscles:testing and function with posture and pain. 5th ed. Lippincott Williams and Wilkins; 2005. p. 49. [Google Scholar]
- 15.Kim J, Jung Y, Kim S, et al. A New Functional Scale and Ambulatory Functional Classification of Duchenne Muscular Dystrophy:Scale Development and Preliminary Analyses of Reliability and Validity. Ann Rehabil Med. 2018;42(5):690–701. doi: 10.5535/arm.2018.42.5.690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perron M, Hebert L, McFadyen B, et al. The ability of the Biodex Stability System to distinguish level of function in subjects with a second-degree ankle sprain. Clin Rehabil. 2007;21(1):73–81. doi: 10.1177/0269215506071288. [DOI] [PubMed] [Google Scholar]
- 17.Cachupe W, Shifflett B, Kahanov L, Wughalter E. Reliability of Biodex Balance System Measures. Meas Phys Educ Exer Sci. 2001;5(2):97–108. [Google Scholar]
- 18.Arnold B, Schmitz R. Examination of balance measures produced by the Biodex Stability System. J Athl Train. 1998;33(4):323–327. [PMC free article] [PubMed] [Google Scholar]
- 19.Maxwell M, Tarcisio F, Camposb G, et al. Influence of knee position on the postural stability index registered by the Biodex Stability System. Gait. 2008;28(4):668–72. doi: 10.1016/j.gaitpost.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 20.Maher C, Williams M, Olds T. The six-minute walk test for children with cerebral palsy. Int J Rehabil Res. 2008;31:185–8. doi: 10.1097/MRR.0b013e32830150f9. [DOI] [PubMed] [Google Scholar]
- 21.Solway S, Brooks D, Lacasse Y, Thomas S. A qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest. 2001;119:256–70. doi: 10.1378/chest.119.1.256. [DOI] [PubMed] [Google Scholar]
- 22.Vinchhi R, Diwan S, Shah S, Vyas N. Test-retest reliability of six minute walk test in spastic ambulatory children with cerebral palsy. Int J Contemp Pediatrics. 2014;1:10–13. [Google Scholar]
- 23.American Thoracic Society Statement. Guidelines for the Six-Minute Walk Test. Am J Respir Crit Care Med. 2002;166:111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 24.Zaky L, Hassan W. Effect of partial weight bearing program on functional ability and quadriceps muscle performance in hemophilic knee arthritis. Egypt J Med Hum Genet. 2013;14(4):413–8. [Google Scholar]
- 25.Jesudason C, Stiller K. Are bed exercises necessary following hip arthroplasty? Aust J Physiother. 2002;48:73–81. doi: 10.1016/s0004-9514(14)60201-4. [DOI] [PubMed] [Google Scholar]
- 26.Eid M, Ibrahim M, Aly S. Effect of resistance and aerobic exercises on bone mineral density, muscle strength and functional ability in children with DMD. Egypt J Med Hum Genet. 2014;15:139–47. [Google Scholar]
- 27.Falk B, Portal S, Tiktinsky R, et al. Anaerobic power and muscle strength in young DMD patients. Med Sci Sports Exerc. 2000;2:52–57. doi: 10.1097/00005768-200001000-00009. [DOI] [PubMed] [Google Scholar]
- 28.El-Meniawy G, Kamal H, Elshemy S. Role of treadmill training versus suspension therapy on balance in children with Down syndrome. Egypt J Med Hum Genet. 2012;13(1):37–43. [Google Scholar]
- 29.Horlings CG, Kung UM, van Engelen BG, Voermans NC, Hengstman GJ, van der Kooi AJ, Bloem BR, Allum JH. Balance control in patients with distal versus proximal muscle weakness. Neuroscience. 2009;164:1876–86. doi: 10.1016/j.neuroscience.2009.09.063. [DOI] [PubMed] [Google Scholar]
- 30.Aras B, Aras O, Karaduman A. Reliability of balance tests in children with Duchenne muscular dystrophy. Sci Res Essays. 2011;6:4428–31. [Google Scholar]
- 31.Holland A, Murphy S, Dowling P, Ohlendieck K. Pathoproteomic profiling of the skeletal muscle matrisome in dystrophinopathy associated myofibrosis. Proteomics. 2016;16(2):345–66. doi: 10.1002/pmic.201500158. [DOI] [PubMed] [Google Scholar]
- 32.Karimi N, Ebrahimi I, Kahrizi S, et al. Evaluation of postural balance using the Biodex balance system in subjects with and without low back pain. Pak J Med Sci. 2008;6:45–52. [Google Scholar]
- 33.Petrof B. The molecular basis of activity-induced muscle injury in Duchenne muscular dystrophy. Mol Cell Biochem. 1998;179:111–123. doi: 10.1023/a:1006812004945. [DOI] [PubMed] [Google Scholar]
- 34.Lim J, Kim D, Bang M. Effects of exercise and steroid on skeletal muscle apoptosis in the mdx mouse. Muscle Nerve. 2004;30:456–462. doi: 10.1002/mus.20139. [DOI] [PubMed] [Google Scholar]
- 35.Bushby K, Finkel R, Birnkrant D, et al. DMD Care Considerations Working Group. Diagnosis and management of Duchenne muscular dystrophy, part 2:implementation of multidisciplinary care. Lancet Neurol. 2010;9:177–189. doi: 10.1016/S1474-4422(09)70272-8. [DOI] [PubMed] [Google Scholar]
- 36.Guskiewicz K. Impaired postural stability:regaining balance. In: Prentice W, Voight M, editors. Techniques in musculoskeletalrehabilitation. United States of America: McGraw-Hill; 2002. pp. 125–50. [Google Scholar]
- 37.Sharma S, Gupta A. Methodology for study of the effect of cyclic ergometer exercise on improving gait parameters in ambulatoryspina bifida children. Int J Educ Plann Admin. 2011;1(2):109–17. [Google Scholar]
- 38.Luigi D, Melina H, Miriam A, et al. Effects of aerobic exercise using cycle ergometry on balance and functional capacity in post-stroke patients:a systematic review and meta-analysis of randomised clinical trials. Disability and Rehabilitation. 2019:1464–5165. doi: 10.1080/09638288.2019.1670272. [DOI] [PubMed] [Google Scholar]
- 39.Benecke R, Conrad B, Meinck H, et al. Electromyographic analysis of bicycling on an ergometer for evaluation of spasticity of lower limbs in man. Adv Neurol. 1983;39:1035–46. [PubMed] [Google Scholar]
- 40.Faist V, König J, Höger H, Elmadfa I. Decreased mitochondrial oxygen consumption and antioxidant enzyme activities in skeletal muscle of dystrophic mice after low-intensity exercise. Ann Nutr Metab. 2001;45:58–66. doi: 10.1159/000046707. [DOI] [PubMed] [Google Scholar]
- 41.Kaczor J, Hall J, Payne E, Tarnopolsky MA. Low intensity training decreases markers of oxidative stress in skeletal muscle of mdx mice. Free Radic Biol Med. 2007;43(1):145–54. doi: 10.1016/j.freeradbiomed.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 42.Ulrich D, Ulrich B, Angulo-Kinzler R, et al. Treadmill training of infants with Down syndrome:evidence-based developmental outcomes. Pediatrics. 2001;108:84–91. doi: 10.1542/peds.108.5.e84. [DOI] [PubMed] [Google Scholar]
- 43.Dal U, Erdogan T, Resitoglu B, et al. Determination of preferred walking speed on treadmill may lead to high oxygen cost on treadmill walking. Gait Posture. 2010;31:366–9. doi: 10.1016/j.gaitpost.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 44.Kubo M, Ulrich B. Coordination of pelvis-HAT (head arms and trunk) in anterior-posterior and medio-lateral directions during treadmill gait in pre adolescents with/without Down syndrome. Gait Posture. 2006;23:512–8. doi: 10.1016/j.gaitpost.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 45.Matsuno V, Camargo M, Palma G, et al. Analysis of partial body weight support during treadmill and over ground walking of children with CP. Rev Bras Fisioter. 2010;14(5) [PubMed] [Google Scholar]
- 46.Tulchin K, Orendurff M, Karol L. A comparison of multi segment foot kinematics during level over ground and treadmill walking. Gait Posture. 2010:104–8. doi: 10.1016/j.gaitpost.2009.09.007. [DOI] [PubMed] [Google Scholar]


