Abstract
Researchhas shown that posttraumatic reactions can co‐occur in trauma‐exposed individuals. Many studies have assessed the co‐occurring patterns of two types of reactions, but few have assessed the patterns of multiple reactions. To build on existing knowledge, the present study examined co‐occurring patterns of posttraumatic stress disorder (PTSD) symptoms, depressive symptoms, and posttraumatic growth (PTG) among adolescents during the COVID‐19 pandemic. Participants (N = 683) were adolescents selected from an area in China severely affected by COVID‐19 who completed the PTSD Checklist, a measure of depression, a PTG inventory, and a cognitive emotional regulation questionnaire. Latent profile analysis and multinomial logistic regression were used for the data analyses. The results showed three heterogeneous patterns characterized by growth (n = 248, 36.3%), distress (n = 101, 14.8%), and struggle (n = 334, 48.9%). Positive refocusing and reappraisal were associated with membership in the growth group compared with distress group, OR = 0.83, 95% CI [0.75, 0.93] and OR = 0.78, 95% CI [0.68, 0.90], whereas rumination, catastrophizing, and “putting into perspective” were associated with membership in the distress group compared with growth group, ORs = 1.15–1.44. These findings suggest that posttraumatic reactions show heterogeneous characteristics: struggle, rather than growth or distress, is common among adolescents during COVID‐19; and distinct cognitive emotional regulation strategies have distinguishing roles in the three patterns of posttraumatic reactions.
抽象
Traditional and Simplified Chinese Abstracts by the Asian Society for Traumatic Stress Studies (AsianSTSS)
簡體及繁體中文撮要由亞洲創傷心理研究學會翻譯
Traditional Chinese
新冠肺炎爆發期間青少年創傷後壓力症、抑鬱及創傷後成長的潛在模式
摘要
研究表明, 創傷後的反應可以同時出現在受到創傷的人身上。許多研究評估了兩種反應的共存模式, 但很少評估多種反應的模式。在現有知識的基礎上, 本研究考察了新冠肺炎爆發期間青少年中創傷後壓力 (PTSD) 症狀、抑鬱症狀及創傷後成長 (PTG) 的共同發生模式。研究對象(N = 683)來自中國受新冠肺炎影響嚴重的地區, 他們完成了創傷後壓力症 (PTSD) 檢查表、抑鬱量表、PTG量表及認知情緒調節問卷。數據分析採用了潛勢分析及多叉邏輯回歸。結果顯示了三種異質模式, 其特點是成長 (n = 248, 36.3%) 、痛苦 (n = 101, 14.8%) 及掙扎 (n = 334, 48.9%) 。與痛苦組相比, 積極的重新聚焦及重新評價與成長組成員相關, OR = 0.83, 95%CI[0.75, 0.93]及OR = 0.78, 95%CI[0.68, 0.90], 而與成長組相比, 反芻、災難化及 “將心比心 ”與痛苦組成員相關, ORs = 1.15‐1.44。這些發現表明, 創傷後反應顯示出異質性的特點:在新冠肺炎期間, 掙扎, 而不是成長或痛苦, 在青少年中很常見;不同的認知情緒調節策略在三種創傷後反應模式中具有不同的作用。
Simplified Chinese
新冠肺炎爆发期间青少年创伤后压力症、抑郁及创伤后成长的潜在模式
摘要
研究表明, 创伤后的反应可以同时出现在受到创伤的人身上。许多研究评估了两种反应的共存模式, 但很少评估多种反应的模式。在现有知识的基础上, 本研究考察了新冠肺炎爆发期间青少年中创伤后压力 (PTSD) 症状、抑郁症状及创伤后成长 (PTG) 的共同发生模式。研究对象(N = 683)来自中国受新冠肺炎影响严重的地区, 他们完成了创伤后压力症 (PTSD) 检查表、抑郁量表、PTG量表及认知情绪调节问卷。数据分析采用了潜势分析及多叉逻辑回归。结果显示了三种异质模式, 其特点是成长 (n = 248, 36.3%) 、痛苦 (n = 101, 14.8%) 及挣扎 (n = 334, 48.9%) 。与痛苦组相比, 积极的重新聚焦及重新评价与成长组成员相关, OR = 0.83, 95%CI[0.75, 0.93]及OR = 0.78, 95%CI[0.68, 0.90], 而与成长组相比, 反刍、灾难化及 “将心比心 ”与痛苦组成员相关, ORs = 1.15‐1.44。这些发现表明, 创伤后反应显示出异质性的特点:在新冠肺炎期间, 挣扎, 而不是成长或痛苦, 在青少年中很常见;不同的认知情绪调节策略在三种创伤后反应模式中具有不同的作用。
COVID‐19 has presented a major global public health crisis. The coronavirus that causes COVID‐19 spread rapidly across the world, with large numbers of corresponding deaths and illnesses and images of overrun hospitals, mass graves, and COVID‐19 patients on assisted ventilation commonly reported in the media (Shevlin et al., 2020). Many individuals throughout the world have likely have felt threatened and horrified by the existential threat posed by COVID‐19. Shevlin et al. (2020) emphasized that COVID‐19 can be considered to be a major traumatic event. The “shattered assumptions theory” (Janoff‐Bulman, 2010) suggests that a traumatic event can shatter individuals’ stable belief systems, resulting in cognitive disequilibrium, which engenders negative cognitions about the self, others, and the world and leads to depression and posttraumatic distress (Janoff‐Bulman, 2010). Extant studies have found that when considered to be a traumatic event, COVID‐19 has resulted in numerous reports of various psychological problems (F. Chen et al., 2020; Kang et al., 2020; Vindegaard & Benros, 2020). Posttraumatic stress disorder (PTSD) and depression are two common psychopathologies found in individuals following exposure to COVID‐19 (Dutheil et al., 2020; Vindegaard & Benros, 2020). For example, a recent review showed that the prevalence of COVID‐19–related PTSD ranged from 7% to 53.8 % and the prevalence of COVID‐19–related depression ranged from 14.6% to 48.3% in the general population (Xiong et al., 2020).
Drawing from Janoff‐Bulman's (2010) shattered assumptions theory, Tedeschi and Calhoun (2004) developed a cognitive model of posttraumatic growth (PTG). They emphasized that the cognitive disequilibrium elicited by a traumatic event also activates deliberate rumination, which enables an individual to reconstruct their positive understanding about the posttraumatic self, others, and the world; this reconstruction is actualized as PTG. Given this theoretical assumption, recent studies have demonstrated that in addition to various negative psychological reactions, some individuals have reported experiencing PTG during the COVID‐19 pandemic (Cui et al., 2020; Hamam et al., 2021; Tomaszek & Muchacka‐Cymerman, 2020), suggesting that among certain individuals, psychological functioning has improved during the pandemic. For example, Cui et al. (2020) found that 43.7% of nurses reported higher‐than‐average PTG scores, suggesting that PTG may be a prevalent positive psychological reaction.
The commonality of PTSD, depression, and PTG raises the question as to whether these reactions can co‐occur in individuals. Theoretically, trauma survivors may simultaneously report many types of psychological outcomes (Cenat et al., 2021; C. Liu et al., 2021) due to their shared factors and complex associations (Angelakis & Nixon, 2015; Ginzburg et al., 2010; Zhou et al., 2019b). In this way, the hypotheses of causality and factors such as comorbid PTSD and depression suggest that PTSD is a risk factor for depression, depression increases the risk for PTSD, and PTSD and depression share common factors (e.g., sleep problems, negative affect; Zhen et al., Wu, 2019). Therefore, as two distinct sources of psychological distress, PTSD and depression may demonstrate a positive association. However, the cognitive model of PTG (Tedeschi & Calhoun, 2004) indicates psychological distress can activate a series of coping strategies in an individual as the individual struggles with negative outcomes following a traumatic event. In turn, this can help the individual to reframe their understanding of the posttraumatic self, others, and the world, resulting in PTG (Zhou, Wu, & Chen, 2015). Based on these findings, we propose that PTSD and depression may lead to PTG, and PTSD, depression, and PTG may, therefore, demonstrate coexistent characteristics. Findings from extant empirical studies have also supported the co‐occurrence of PTSD, depression, and PTG in trauma‐exposed individuals (Schneider et al., 2019; Wu et al., 2018). However, there are individual differences in both the availability of and changes in resources, which Hobfoll's (2002) conservation of resources theory suggests often result from highly disruptive events that play crucial roles in human adaptability to extreme stress. This theory posits that posttraumatic reactions may vary with individual differences in the use of resources; for example, some individuals show a low level of distress and a high level of growth, whereas others may report a high degree of distress and low degree of growth (C. Cao et al., 2018; J. Chen & Wu, 2017a; Zhou, Wu, & Zhen, 2018). Therefore, co‐occurring psychological reactions may emerge as a heterogeneous presentation in distinct individuals following the same traumatic event, posing challenges for mental health care. Clarifying the heterogeneity in the presentation of psychological reactions is, therefore, important for recognizing, diagnosing, and treating trauma‐exposed individuals (Palic & Elklit, 2011).
Latent profile analysis (LPA) offers a useful person‐centered approach to clarifying the heterogeneity of comorbid PTSD, depression, and PTG, as it uses continuous variables to group cases into discrete subgroups based on correlations among indicators (Lubke & Muthén, 2007). This means that each subgroup comprises homogeneous individuals, but individuals in different subgroups are heterogeneous. That is, the presentation features of a particular variable in a particular subgroup may differ from those for the same variable in another subgroup (Zhou, Wu, Wang, et al., 2018). Therefore, LPA is an effective approach for identifying heterogeneous coexisting patterns of these three reactions in a sample of adolescents.
Previous studies have used LPA to examine the co‐occurring patterns of PTSD and depression in various populations, including veterans, patients with cancer, and individuals who have experienced natural disasters. These studies have found several distinct patterns, such as low‐level symptoms, PTSD only, depression only, and combined PTSD and depression (Armour et al., 2015; X. Cao et al., 2015; Yang et al., 2020; Zhen et al., 2019). Regarding the relation between PTSD and PTG, Calhoun and Tedeschi's (2006) PTG theory suggests that PTSD and PTG are independent psychological constructs, but distress may activate the cognitive processes of trauma survivors. This may lead to more positive perspectives of the self, others, and the world, which would, in turn, result in PTG, meaning that PTSD and PTG can co‐occur in the same individual. In such a case, the heterogeneous patterns of these two types of reactions have also attracted research attention (Birkeland et al., 2015; Zhou et al., 2020). Several distinct co‐occurring patterns have been found among survivors of natural disasters, including low levels of PTSD symptoms and high‐level PTG, low‐level PTSD and low‐level PTG, high‐level PTSD and high‐level PTG, and high‐level PTSD and low‐level PTG (C. Cao et al., 2018; J. Chen & Wu, 2017a; Zhou, Wu, & Zhen, 2018). However, the heterogeneous patterns of depression and PTG in trauma‐exposed individuals remain unclear, although depression has been associated with PTG (Bianchini et al., 2015; Schneider et al., 2019).
Furthermore, previous findings have demonstrated that trauma‐exposed individuals can show diverse negative psychological reactions (Liang et al., 2021; Unseld et al., 2020). However, these studies have typically depended on the co‐occurring patterns of PTG and one negative psychological outcome, such as PTSD, to determine growth (J. Chen & Wu, 2017b; Zhou, Wu, Wang, et al., 2018). These studies may have overlooked the role of other negative outcomes, resulting in biased conclusions about the characteristics of trauma‐exposed individuals. Therefore, other negative psychological outcomes, such as depression, should be considered when examining patterns of PTSD and PTG, especially as depression is often comorbid with PTSD (Klein et al., 2020; Lazarov et al., 2020) and has also been shown to be related to PTG (Magruder et al., 2015; Schneider et al., 2019). Unfortunately, few studies have assessed patterns related to these three factors, and the nature of these co‐occurring patterns remains unclear.
Most previous studies have focused on trauma‐exposed individuals following war or natural disasters, and caution is needed when generalizing these results to other types of traumatic events, including COVID‐19. The COVID‐19 pandemic is considered to be a major traumatic event that threatens individuals’ lives (Shevlin et al., 2020). Compared with war and natural disasters that often affect specific geographic areas, COVID‐19 has spread across all parts of the world and affected nearly every global citizen. Therefore, it remains unclear whether the patterns of psychological presentation in trauma‐exposed individuals after war or natural disasters can be generalized to individuals in the context of the COVID‐19 pandemic. Moreover, in the context of Chinese collective culture, individuals responded positively to the government's call to be “united as one” during the pandemic and concentrate their efforts on working to combat the virus, which resulted in getting the virus under control in China. However, whether adolescents showed less psychological distress and more growth remains an important issue worth discussing. To advance these issues, the first aim of the present study was to examine the patterns of PTSD symptoms, depressive symptoms, and PTG among adolescents during the COVID‐19 pandemic. Because previous research has demonstrated positive associations among psychological distress, PTSD, and depression in adolescents (Ying et al., 2012) and given the possible distinct co‐existing patterns of PTSD and PTG (X. Cao et al., 2018; J. Chen & Wu, 2017a; Zhou, Wu, Wang, et al., 2018), we proposed four possible patterns: low distress and high growth, low distress and low growth, high distress and high growth, and high distress and low growth.
Following clarification of the patterns of psychological presentations, it is important to understand specific predictors of distinct patterns, which may reveal targets for psychological intervention. Freedy et al. (1992) proposed a model of risk factors associated with disaster adjustment, which emphasized that pretraumatic factors, such as sex and age, may exert effects on posttraumatic reactions. Female sex has been considered to be a risk factor for psychological distress (Moghanibashi‐Mansourieh, 2020), and women and girls have been found to be more likely to show higher levels of psychological distress (Zhu et al., 2020) and lower levels of growth (Kimhi et al., 2009) than men and boys due to a tendency to engage in rumination when distressed (Nolen‐Hoeksema, Larson, & Grayson, 1999). Children and adolescents have underdeveloped pretrauma schema and limited abilities to employ effective coping strategies to negotiate stressful events (Cryder et al., 2006; Meyerson et al., 2011). Previous studies showed that younger individuals are more likely to report a higher degree of distress (Murata et al., 2021) and less growth (Currier et al., 2009) than older individuals. In addition to pretraumatic factors, the model posited by Freedy et al. (1992) emphasizes the role of within‐trauma factors (i.e., the type of trauma exposure) and posttraumatic factors (e.g., coping strategies) in posttraumatic reactions. However, the psychosocial framework of posttraumatic stress (Joseph & Linley, 2008) suggests that traumatic events may activate individuals’ cognitive thinking about these events in conscious or unconscious ways and affect their emotional status. People may, therefore, adopt distinct cognitive or emotional regulation strategies to cope with trauma, resulting in different psychological outcomes (Joseph et al., 1997). In addition to trauma exposure, this theory suggests that cognitive emotional regulation is another important factor that affects posttraumatic reactions.
Cognitive emotional regulation is defined as one's belief in their ability to manage the demands of posttraumatic recovery (Cieslak et al., 2008). This construct includes maladaptive strategies, such as self‐blame, blame of others, rumination, and catastrophizing, as well as adaptive strategies, including acceptance, positive refocusing, planning, positive reappraisal, and putting the event into perspective (Garnefski et al., 2001). Results from recent studies have found maladaptive emotional regulation strategies to be associated with increased posttraumatic distress, including symptoms of PTSD or depression (Huh et al., 2017; Kaczkurkin et al., 2017; J. Liu et al., 2019; McLean et al., 2019), whereas adaptive strategies have been shown to be related to positive changes, such as PTG, following trauma exposure (Hussain & Bhushan, 2011; Lee et al., 2018; Thomas et al., 2020).
Although these studies have examined the effect of cognitive emotional regulation strategies on PTSD, depression, and PTG, it remains unclear whether these strategies can distinguish distinct co‐occurring patterns of PTSD, depression, and PTG. Moreover, because cognitive emotional regulation encompasses nine different strategies (Garnefski et al., 2001) that have various roles in posttraumatic reactions, it is unclear whether different strategies have distinct effects on co‐occurring patterns. To fill this knowledge gap, the second aim of the present study was to examine the role of these nine cognitive emotional regulation strategies in differentiating distinct co‐occurring patterns of PTSD, depression, and PTG. Drawing on the psychosocial framework of posttraumatic stress (Joseph & Linley, 2008), Garnefski et al.’s (2001) theoretical views, and previous findings (Lee et al., 2018; McLean et al., 2019), we proposed that trauma exposure and maladaptive emotional regulation strategies would be associated with higher levels of posttraumatic distress and lower degrees of posttraumatic growth, whereas adaptive strategies would be related to less distress and more growth.
Method
Participants and Procedure
Six months after the COVID‐19 outbreak in China (i.e., July 2020), we recruited adolescents from Hubei province, China, which was severely affected by the virus. First, we contacted a psychology teacher from a high school in Huang'gang city, Hubei province. With their help, we selected 12 first‐grade classrooms in this high school, each comprising approximately 60 students, that did not have other scheduled teaching activities on the assessment date. In total, 683 students were enrolled in the study. Of these 683 students, 341 (49.9%) were male, 301 (44.1%) were female, and 41 (6.0%) did not report their sex. The mean participant age was 16.06 years (SD = 0.56 years, range: 15–18 years).
The study was approved by the Research Ethics Committee of the Department of Psychological and Behavioral Sciences, Zhejiang University. All students in the selected classrooms attended school on the assessment date, and all students agreed to participate in the investigation and complete self‐report questionnaires. Participants were informed of the study aims and the voluntary nature of participation before the survey, and written informed consent was obtained from all students and their guardians. Assessments were conducted under the supervision of trained psychology postgraduate students.
Measures
Pandemic Exposure
A questionnaire developed by Zhen and Zhou (2020) was used to assess the severity of COVID‐19 pandemic exposure. Participants were asked to respond “yes” or “no” to 10 items (e.g., “family members were quarantined”), with scores summed to create a total exposure severity score. In the present study, the mean severity score was 2.52 (SD = 1.35).
PTSD Symptoms
A translated version (Zhou et al., 2017) of the PTSD Checklist (PCL) for the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM‐5; i.e., the PCL‐5; Weathers et al., 2013) was used to assess PTSD symptoms. The PCL‐5 includes 20 items that are used to capture the severity and frequency of PTSD symptoms; in the present study, participants were asked to rate symptoms in relation to their COVID‐19–related experiences. Previous studies have validated the Chinese version of the PCL‐5 in adolescent samples (Zhou et al., 2019, 2019b). Participants were asked to rate the frequency of each symptom during the past 2 weeks, scoring responses on a scale of 0 (not at all/only once) to 4 (almost every day). The PCL‐5 contains four subscales, each corresponding with a DSM‐5 PTSD symptom cluster: Intrusions, Negative Alterations in Cognitions and Mood, Avoidance, and Alterations in Arousal and Reactivity (i.e., hyperarousal). In the present study, the internal consistency of the total scale was very good, Cronbach's α = .89.
Depressive Symptoms
We assessed depressive symptoms using the Chinese version of the Center for Epidemiologic Studies Depression Scale for Children (CES‐DC; Fendrich et al., 1990). The original CES‐DC is a 20‐item, self‐report measure that is used to assess emotional, cognitive, and behavioral symptoms of depression. The CES‐DC has four subscales: Somatic Problems, Depressed Affect, Positive Affect, and Interpersonal Problems. Participants were required to report the frequency of their emotional, behavioral, and cognitive symptoms of depression during the last 2 weeks, rating responses on a scale of 0 (never) to 3 (always). The Chinese version of the CES‐DC had demonstrated good reliability and construct validity in various Chinese populations (e.g., Ying et al. 2012). In the present sample, the internal consistency of the scale in this study was adequate, Cronbach's α = .79.
PTG
We assessed PTG using a modified version of the Posttraumatic Growth Inventory (PTGI; Zhou et al., 2015). The original PTGI was developed by Tedeschi and Calhoun (1996) and comprises 21 items broken into five subscales: Personal Strength, New Possibilities, Relating to Others, Appreciation of Life, and Spiritual Change. Items are scored on a 6‐point scale ranging from 0 (no change) to 5 (a very great degree of change). The modified PTGI we used included 22 items on three subscales: Perceived Changes in Self (nine items, e.g., “I'm more likely to try to change things which need changing”), Changed Sense of Relationship With Others (seven items, e.g., “A sense of closeness with others”), and Changed Life Philosophy (six items, e.g., “An appreciation for the value of my own life”); this modified version has demonstrated good applicability in Chinese children and adolescents following trauma exposure (Zhou et al., 2019a, 2019b). In the present sample, the reliability of the modified PTGI was excellent, Cronbach's α = .92.
Cognitive Emotional Regulation
Cognitive emotional regulation strategies were assessed using the revised Chinese version (Zhu et al., 2007) of the Cognitive Emotion Regulation Questionnaire (CERQ; Garnefski et al., 2001). This 36‐item instrument was used to measure adolescents’ specific cognitive coping strategies when confronted with COVID‐19, with a focus on nine specific strategies: self‐blame, acceptance, rumination, positive refocusing, refocus on planning, positive reappraisal, putting the event into perspective, catastrophizing, and other blame. All items are rated on a 5‐point Likert scale ranging from 0 (completely disagree) to 4 (completely agree). In the present sample, the full CERQ demonstrated good internal reliability, Cronbach's α = .91, with Cronbach's alpha values for the nine subscales ranging from .69 to .89.
Data Analysis
In the present sample, data were missing for less than 4.1% of measured variables. Missing response values were analyzed using Little's Missing Completely at Random test, which revealed the data were missing randomly, χ2(269, N = 683) = 249.923, p = .792. Therefore, the maximum likelihood estimation method was used to handle missing data. In addition, we examined the distribution of scale scores and found that skewness for primary variables ranged from −0.39 to 0.69, and kurtosis for these variables ranged from −0.55 to 0.92; that is, all variables showed relatively normal distribution.
Next, we employed two procedures to examine the study hypotheses. In the first procedure, latent profile analysis (LPA) was conducted using Mplus (Version 7.0; Muthén & Muthén, 2012) to identify coexisting patterns of PTSD symptoms, depressive symptoms, and PTG among participants. The LPA indicators were the total scores for each scale (i.e., continuous variables). To determine the optimal number of latent classes, one‐ to six‐class solutions were evaluated and compared based on fit statistics, interpretability, and theoretical considerations. A good model fit was indicated by lower Bayesian information criterion, adjusted Bayesian information criterion, and Akaike information criterion values; a higher entropy value; a significant Lo–Mendell–Rubin likelihood ratio test (LMR‐LRT); and a significant adjusted LMR‐LRT (ALMR‐LRT).
In the second procedure, we used SPSS (Version 17.0) to carry out the multinomial logistic regression to identify the associations among sex, age, pandemic exposure, and cognitive emotional regulation strategies and the most likely class membership variables. We considered p values of .05 and lower to be statistically significant. In the multinomial logistic regression, the most likely class membership variable was considered the outcome variable, and sex, age, pandemic exposure, and cognitive emotional regulation strategies were considered the independent variables. We proposed that sex, age, pandemic exposure, and cognitive emotional regulation strategies could differentiate distinct latent classes.
Results
Prevalence of PTSD Symptoms, Depressive symptoms, and PTG
Based on a cutoff score of 31 to indicate probable PTSD in children and adolescents (Foa et al., 2018) and a cutoff score of 16 used to indicate probable depression, our results showed the prevalence of probable PTSD and was 35.4% (n = 242), and the prevalence of probable depression was 68.1% (n = 465). Based on a cutoff score of 66 to reflect PTG (Zhou et al., 2018), the prevalence of PTG was 22.0% (n = 150) in the present sample. In addition, we assessed the correlation among PTSD symptoms, depressive symptoms, and PTG and found that PTSD symptoms had a positive association with depressive symptoms, r = .73, p < .001, and a nonsignificant association with PTG, r = ‐0.01, p = .842. Depressive symptoms were significantly and negatively associated with PTG, r = −.14, p < .001.
Latent Patterns of PTSD Symptoms, Depressive Symptoms, and PTG Levels
Table 1 shows the latent class solution for PTSD symptoms, depressive symptoms, and PTG among participating adolescents. We found that the value of entropy exceeded 0.70 for the two‐ to six‐class solutions, but the entropy in the three‐class solution was higher than that in other class solutions. This suggested that the three‐class solution had better between‐group distinction than other solutions. Moreover, the findings also indicated that the LMR‐LRT and ALMR‐LRT values were significant for the two‐ and three‐class solutions but not the four‐, five‐, or six‐class solutions. The prevailing standard is that when the LMR‐LRT and ALMR‐LRT values are significant for multiple solutions, the solution with the largest number of classes should be accepted (Rosellini et al., 2014); therefore, we selected the three‐class solution as the optimal solution.
Table 1.
Goodness‐of‐Fit Indices for Distinct Solutions
| Model | AIC | BIC | aBIC | Entropy | LMR‐LRT | ALMR‐LRT |
|---|---|---|---|---|---|---|
| 1 class | 16,392.041 | 16,419.200 | 16,400.149 | – | – | – |
| 2 classes | 16,060.799 | 16,106.064 | 16,074.312 | 0.704 | 339.242*** | 326.727*** |
| 3 classes | 15,903.882 | 15,967.253 | 15,922.801 | 0.756 | 164.917 *** | 158.833 *** |
| 4 classes | 15,869.304 | 15,950.780 | 15,893.628 | 0.739 | 42.578 | 41.007 |
| 5 classes | 15,847.638 | 15,947.221 | 15,877.368 | 0.725 | 29.666 | 28.571 |
| 6 classes | 15,828.771 | 15,946.460 | 15,863.907 | 0.738 | 26.867 | 25.876 |
Note. Bolding indicates the best‐fitting model. AIC = Akaike information criterion; BIC = Bayesian information criterion; aBIC = adjusted BIC; LMR‐LRT = Lo–Mendell–Rubin likelihood ratio test.
***p < .001.
Figure 1 depicts the standardized z ‐scores for measures of PTSD, depression, and PTG for the latent three‐class solution. Table 2 shows the unstandardized total and subscale scores for PTSD, depression, and PTG as well as the results of the multivariate analysis of variance. We found that apart from the nonsignificant between‐class difference in the Changed Life Philosophy PTGI subscale, the between‐class difference in other subscale and total scores for PTSD, depression, and PTG were significant. As shown in Figure 1 and Table 2, we labeled Class 1 the “growth” group (n = 248, 36.3%), which was characterized by lower levels of PTSD symptoms and depressive symptoms and a higher level of PTG. Class 2 was characterized by higher levels of PTSD symptoms and depressive symptoms and a lower level of PTG and was labeled the “distress” group (n = 101, 14.8%). Class 3 showed moderate levels of PTSD and depressive symptoms and a higher level of PTG that was similar to the level found among participants in Class 1; therefore, this class was named the “struggling” group (n = 334, 48.9%).
Figure 1.
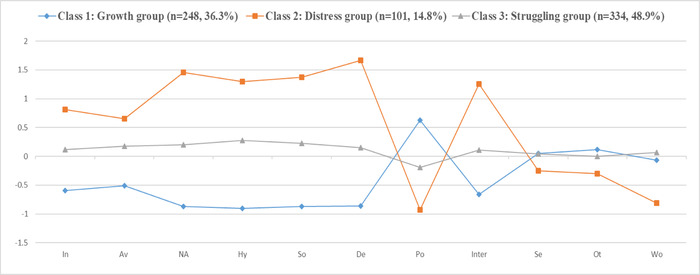
Standardized z Scores for Measure of Posttraumatic Stress Disorder Symptoms, Depression, and Posttraumatic Growth for the Latent Three‐Class Solution
Note. In = intrusions; Av = avoidance; NA = negative alterations in cognition and mood; Hy = alterations in arousal and reactivity; So = somatic problems; De = depressed affect; Po = positive affect; Inter = interpersonal problems; Se = perceived changes in self; Ot = changed sense of relationships with others; Wo = changed life philosophy.
Table 2.
Class Means for the Three‐Class Solution
| Class 1: Growth group | Class 2: Distress group | Class 3: Struggling group | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | M | SD | M | SD | M | SD | F(2, 580) | ηp 2 | Post hoc pairwise comparisons (p < .05) |
| In | 3.05 | 2.88 | 8.36 | 4.55 | 6.03 | 3.16 | 89.43*** | .24 | 1 < 3 < 2 |
| Av | 1.20 | 1.39 | 3.20 | 1.89 | 2.39 | 1.58 | 57.73*** | .17 | 1 < 3 < 2 |
| NA | 4.18 | 2.96 | 17.73 | 4.47 | 10.43 | 3.76 | 462.55*** | .61 | 1 < 3 < 2 |
| Hy | 4.13 | 3.10 | 15.66 | 3.70 | 10.34 | 3.49 | 397.01*** | .58 | 1 < 3 < 2 |
| So | 4.53 | 2.76 | 14.12 | 3.25 | 9.26 | 2.67 | 417.79*** | .59 | 1 < 3 < 2 |
| De | 1.82 | 1.80 | 13.68 | 3.11 | 6.60 | 2.84 | 752.35*** | .72 | 1 < 3 < 2 |
| Po | 6.89 | 2.69 | 2.43 | 1.89 | 4.56 | 2.32 | 128.47*** | .31 | 1 < 3 < 2 |
| Inter | 0.41 | 0.79 | 3.40 | 1.68 | 1.61 | 1.29 | 219.04*** | .43 | 1 < 3 < 2 |
| Se | 21.45 | 10.59 | 18.63 | 9.55 | 21.29 | 8.28 | 3.88* | .01 | 2 < (1 = 3) |
| Ot | 17.52 | 9.05 | 14.19 | 7.73 | 16.62 | 6.99 | 5.23** | .02 | 2 < (1 = 3) |
| Wo | 11.47 | 6.33 | 11.53 | 7.13 | 12.31 | 5.82 | 2.13 | .01 | — |
| PTSD | 12.60 | 7.16 | 44.81 | 9.51 | 29.10 | 7.41 | 584.21*** | .67 | 1 < 3 < 2 |
| Depression | 11.83 | 5.09 | 40.88 | 6.71 | 24.83 | 5.35 | 987.25*** | .77 | 1 < 3 < 2 |
| PTG | 50.56 | 24.24 | 44.64 | 21.68 | 50.21 | 18.54 | 3.46** | .01 | 2 < (1 = 3) |
Note. In = intrusions; Av = avoidance; NA = negative alterations in cognition and mood; Hy = alterations in arousal and reactivity; So = somatic problems; De = depressed affect; Po = positive affect; Inter = interpersonal problems; Se = perceived changes in self; Ot = changed sense of relationships with others; Wo = changed life philosophy; PTSD = posttraumatic stress disorder; PTG = posttraumatic growth.
***p < .001.
**p < .01.
*p < .05.
Cognitive Emotional Regulation Strategies Differentiating Distinct Latent Patterns
To elucidate the risk and protective factors for psychological problems, we set the growth group as the reference group and examined the roles of COVID‐19 exposure and cognitive emotional regulation. Table 3 shows the results of the analysis of different cognitive emotional regulation strategies in differentiating distinct patterns of PTSD symptoms, depressive symptoms, and PTG. We found that male participants and older adolescents were more likely to belong to the growth group than the other groups. COVID‐19 exposure severity was more likely to be related to the distress group than the other groups. Three cognitive emotional regulation strategies—acceptance, planning, and self‐blame—had nonsignificant roles in distinguishing distinct groups, but other strategies showed significant roles in differentiating the three patterns. Positive refocusing and reappraisal were more likely to be associated with the growth group than the other groups. Blaming others was less likely to be associated with the distress group than the other groups, whereas rumination, catastrophizing, and putting the event into perspective were associated with the distress group.
Table 3.
Role of Cognitive Emotional Regulation in Differentiating Distinct Patterns
| Distress group vs. growth group | Struggling group vs. growth group | Struggling group vs. distress group | ||||
|---|---|---|---|---|---|---|
| Variable | OR | 95%CI | OR | 95%CI | OR | 95%CI |
| Male (ref. = female) | 0.34** | [0.18, 0.63] | 0.45*** | [0.29, 0.68] | 1.33 | [0.76, 2.31] |
| Age | 2.02* | [1.18, 3.47] | 1.44 | [0.99, 2.08] | 0.71 | [0.44, 1.14] |
| Pandemic exposure | 1.30* | [1.04, 1.62] | 1.10 | [0.95, 1.28] | 0.85 | [0.70, 1.03] |
| Acceptance | 1.09 | [0.98, 1.22] | 1.05 | [0.97, 1.13] | 0.96 | [0.87, 1.06] |
| Positive refocusing | 0.83** | [0.75, 0.93] | 0.90* | [0.84, 0.98] | 1.08 | [0.99, 1.19] |
| Planning | 1.06 | [0.93, 1.21] | 1.05 | [0.96, 1.16] | 1.00 | [0.89, 1.11] |
| Positive reappraisal | 0.78*** | [0.68, 0.90] | 0.88** | [0.80, 0.97] | 1.12** | [1.00, 1.26] |
| Putting into perspective | 1.24** | [1.10, 1.41] | 1.07 | [0.98, 1.17] | 0.86*** | [0.77, 0.96] |
| Self‐blame | 1.08 | [0.97, 1.21] | 1.02 | [0.94, 1.11] | 0.94 | [0.86, 1.04] |
| Other‐blame | 0.86* | [0.77, 0.97] | 0.95 | [0.87, 1.03] | 1.10 | [1.00, 1.20] |
| Rumination | 1.15*** | [1.06, 1.24] | 1.15*** | [1.07, 1.24] | 1.00 | [0.99, 1.01] |
| Catastrophizing | 1.44*** | [1.28, 1.62] | 1.19*** | [1.08, 1.30] | 0.82*** | [0.75, 0.90] |
Note. OR = odds ratio; ref. = reference group.
***p < .001.
**p < .01.
*p < .05.
Discussion
To our knowledge, this was the first study to examine heterogeneous co‐occurring patterns of PTSD symptoms, depressive symptoms, and PTG levels among adolescents during the COVID‐19 pandemic. The findings revealed three heterogeneous patterns: a growth group, characterized by lower levels of both PTSD and depressive symptoms and a higher level of PTG; a distress group, characterized by higher levels of both PTSD and depressive symptoms and a lower level of PTG; and a struggling group, characterized by moderate levels of PTSD and depressive symptoms and a higher level of PTG. Our results supported findings reported in previous studies that have indicated multiple posttraumatic reactions may co‐occur heterogeneously among trauma‐exposed adolescents (C. Cao et al., 2015; X. Cao et al., 2018; Zhou, Wu, Wang, et al., 2018). Moreover, we found that the nine cognitive emotional regulation strategies had distinct roles in distinguishing different patterns of PTSD, depression, and PTG, which reflected essential differences among these strategies.
Although we found three patterns of posttraumatic reaction, labeled the distress, growth, and struggling groups, we did not find a resilient group marked by low levels of PTSD symptoms and low levels of PTG. This finding was inconsistent with previous studies (J. Chen & Wu, 2017a, 2017b) and did not support previous assumptions that resilience is common following trauma exposure (Bonanno et al., 2012; Self‐Brown et al., 2013). A possible explanation is that previous researchers conducted their studies with samples of survivors following trauma exposure (J. Chen & Wu, 2017a, 2017b), whereas this study was conducted during the COVID‐19 outbreak. That is, adolescents in the present sample had suffered from the consequences of the COVID‐19 pandemic wherein their psychological functioning was challenged and had not yet recovered to pre–COVID‐19 levels; therefore, the present findings reflect adolescents’ distress rather than their resilience.
Because the cognitive abilities of children and adolescents are immature and malleable (Tedeschi & Calhoun, 2004), new cognitive models are easily formed when their cognitive function has been challenged by traumatic events. This can help individuals to reconstruct their understanding of traumatic events. Findings from previous studies have demonstrated that this reinterpretation can promote finding meaning in one's world and realizing positive change and growth following trauma exposure (Tedeschi & Calhoun, 2004; Zhou et al., 2015; Zhou, Wu, Wang, et al., 2018). Therefore, a group characterized by growth emerged in the present study even though these adolescents were still experiencing COVID‐19 exposure.
Interestingly, there were more adolescents in the struggling group (n = 334, 48.9%) than in the other two groups, suggesting that many adolescents were struggling during the COVID‐19 outbreak. This finding is inconsistent with previous studies that have shown more adolescents with membership in a group characterized by resilience than other groups (J. Chen & Wu, 2017a, 2017b), which may be explained by the time during which the present study was conducted. In the context of the COVID‐19 outbreak, especially given the pervasiveness and uncertainty of this pandemic, most adolescents had to continually use the resources available to them to cope with their experiences, potential outbreak threats, and pandemic‐related negative emotions. This finding supports the coexistence of PTSD and PTG in trauma‐exposed individuals (e.g., Tedeschi & Calhoun, 2004), which suggested that PTG in these individuals may be considered a potential coping strategy but not actual growth as a psychological outcome. Therefore, PTG in these individuals may be considered an illusory aspect that made their struggle more bearable (Maercker & Zoellner, 2004).
With regard to the second study aim, we found that male students and older adolescents were more likely to belong to the growth group than the other two groups. Men and boys tend to engage in immersive thinking on trauma less often than women and girls (Jose & Brown, 2008), which may make it easier for male adolescents to distract their attention from traumatic events and demonstrate an ability to rethink these experiences, which can result in positive change. In addition, older adolescents are better able to identify and verbalize symptoms compared with younger adolescents (Contractor et al., 2013), which may help relieve their distress and promote positive adjustment and growth. Moreover, we found that COVID‐19 exposure was strongly related to the distress group, which may be explained by the shattered assumptions theory (Janoff‐Bulman, 1992). This theory suggests that trauma exposure can challenge individuals’ stable belief systems about the self, others, and the world and lead to negative assumptions, thereby eliciting negative emotions and ultimately leading to psychological distress (Janoff‐Bulman, 2010).
We also found that positive refocusing and reappraisal were more likely to be associated with membership in the growth group, which is consistent with previous studies (Garnefski et al., 2008; Thomas et al., 2020). These two strategies lead individuals to reassess various aspects of traumatic events and their emotions related to these events (Puechlong et al., 2020), which can promote the reframing of one's understanding of traumatic experiences and finding meaning in one's world, resulting in positive changes or growth following trauma exposure (Zhou & Wu, 2018).
In contrast to previous studies (Garnefski et al., 2005; Kraaij et al., 2008), we found that blaming others was less likely to be associated with the distress group than the growth group, which may be explained by attribution theory (Weiner, 1993). Following negative events, attribution to internal rather than external causes had a reliable and significant association with increased mental problems (Joiner & Wagner, 1995; Sweeney et al., 1986); that is, attribution to external factors (e.g., blaming others) may be related to less distress when individuals confront negative events because it may function to diffuse an individual's sense of responsibility for that event, which may relieve stress (O'Connor et al., 2011). In the context of the COVID‐19 pandemic, the outbreak was associated with interpersonal infection due to the highly contagious nature of the virus. In the present sample, placing responsibility for COVID‐19 on other individuals might have diffused participants’ sense of responsibility and released their negative emotions, resulting in lower levels of distress.
In concert with previous studies (Garnefski et al., 2005; Kraaij et al., 2008; Puechlong et al., 2020), we found that rumination and catastrophizing were associated with membership in the distress group. This finding may be explained by the cognitive model of trauma (Ehlers & Clark, 2000). This model assumes that a combination of a more negative appraisal of the self, others, and the world after trauma exposure contributes to psychopathology. Moreover, putting the event into perspective, which is often considered an adaptive cognitive emotional regulation strategy, was correlated with increased distress in the present sample. This finding was inconsistent with findings reported by Puechlong et al. (2020) and Wisco et al. (2013), but supported results reported by Garnefski et al. (2003). Slanbekova et al. (2019) noted that putting traumatic experiences into perspective is a form of emotion‐focused coping in which individuals distance themselves from distress by making themselves believe that an experience was not terrible compared with other experiences. To some extent, this reflects a self‐deceptive component of this coping strategy, which may be beneficial in coping with trauma exposure in the short term (Wu et al., 2015). However, continuing exposure to COVID‐19 may challenge the self‐deceptive component of coping among these individuals, forcing them to take a more realistic perspective and interpret the events as traumatic; therefore, they may experience increased distress in the long term.
An interesting finding of the present study was that planning and acceptance did not differentiate distinct groups. In the context of China's collectivist culture, Chinese citizens responded positively to the government's call to adopt a series of strategies to protect themselves from COVID‐19. This meant that they had detailed plans to protect themselves, including avoiding infected individuals and making corresponding arrangements in their daily lives (e.g., work, school). This may explain why planning had a nonsignificant role in differentiating distinct groups. In addition, because COVID‐19 had become an inevitable and inescapable traumatic event, all residents had to accept this new reality, making it likely that acceptance did not play a role in differentiating distinct groups with various patterns.
Several study limitations should be noted. First, extant studies have found that various posttraumatic reactions may coexist in trauma‐exposed individuals (Cenat et al., 2021; C. Liu et al., 2021). However, the present study only considered PTSD, depression, and PTG and overlooked other psychological outcomes following trauma exposure. Therefore, further studies should consider other posttraumatic reactions to assess the patterns of psychological presentations. Similarly, many factors and sociodemographic characteristics influence psychological presentations, and further studies are needed to examine other potential factors. Third, although the present study was conducted during the COVID‐19 pandemic, psychological presentations may show differences in distinct developmental phases of the pandemic; therefore, the present results should be interpreted with consideration of the restricted period. In addition, we only focused on a sample of Chinese adolescents, and generalization to other samples in other countries should be made with caution. In addition to age, sex, trauma exposure, and cognitive emotional regulation strategies, our dataset included other factors that may have impacted posttraumatic reactions; however, these factors were not included in the present analyses given the focus of this study. Moreover, we plan to investigate participants’ prior traumatic experiences in a further study, as these experiences could also have affected their psychological outcomes during COVID‐19.
Despite these limitations, the present findings extend knowledge from previous studies that were focused on two types of co‐occurring patterns of posttraumatic reactions by using three types of reactions and covering both negative and positive aspects. This approach offered more detailed psychological presentations present during the COVID‐19 pandemic. The findings indicate that most adolescents were struggling during the pandemic, although some adolescents reported growth or positive changes through this struggle. In addition, only 14.8% of participants in the present sample were grouped in the class characterized by distress, suggesting that most adolescents faced the pandemic without experiencing high levels of distress. Moreover, we found that distinct cognitive emotional regulation strategies had different roles in distinguishing the distress, growth, and struggling groups, wherein positive refocusing and reappraisal led to positive changes, but rumination, catastrophizing, and putting the event into perspective were associated with distress. In the context of clinical practice, these findings may inform psychological interventions for adolescents during the COVID‐19 pandemic. Based on the heterogeneity of posttraumatic reactions, clinicians can divide individual adolescents into different subgroups with distinct psychological outcomes. This may allow for the provision of targeted interventions for specific individuals or subgroups, thereby optimizing the effect of psychological interventions. For adolescents experiencing distress, interventions could focus on reducing the use of rumination, catastrophizing, and putting the event into perspective as well as increasing the use of positive refocusing and reappraisal. During the COVID‐19 pandemic, the public was asked to stay indoors in quarantine at home for extended periods to reduce the chances of being infected. Therefore, community‐based trauma interventions could be used to achieve the previously described objectives.
Open Practices Statement
The study reported in this article was not formally preregistered. Neither the data nor the materials have been made available on a permanent third‐party archive; requests for the data or materials should be sent via email to the corresponding author at psyzx@zju.edu.cn
The present study was supported by the National Youth Project for National Social Science Fund of China (Education; CHA200259).
References
- Angelakis, S. , & Nixon, R. D. V. (2015). The comorbidity of PTSD and MDD: Implications for clinical practice and future research. Behaviour Change, 32(1), 1–25. 10.1017/bec.2014.26 [DOI] [Google Scholar]
- Armour, C. , Contractor, A. , Elhai, J. D. , Stringer, M. , Lyle, G. , Forbes, D. , & Richardson, J. D. (2015). Identifying latent profiles of posttraumatic stress and major depressive symptoms in Canadian veterans: Exploring differences across profiles in health related‐functioning. Psychiatry Research, 228(1), 1–7. 10.1016/j.psychres.2015.03.011 [DOI] [PubMed] [Google Scholar]
- Bianchini, V. , Roncone, R. , Giusti, L. , Casacchia, M. , Cifone, M. G. , & Pollice, R. (2015). PTSD growth and substance abuse among a college student community: Coping strategies after 2009 L'aquila earthquake. Clinical Practice and Epidemiology in Mental Health, 11(1), 140–143. 10.2174/1745017901511010140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birkeland, M. S. , Hafstad, G. S. , Blix, I. , & Heir, T. (2015). Latent classes of posttraumatic stress and growth. Anxiety, Stress, & Coping, 28(3), 272–286. 10.1080/10615806.2014.956097 [DOI] [PubMed] [Google Scholar]
- Bonanno, G. A. , Mancini, A. D. , Horton, J. L. , Powell, T. M. , Leardmann, C. A. , Boyko, E. J. , Wells, T. S. , Hooper, T. I. , Gackstetter, G. D. , & Smith, T. C. (2012). Trajectories of trauma symptoms and resilience in deployed U.S. military service members: Prospective cohort study. British Journal of Psychiatry, 200(4), 317–323. 10.1192/bjp.bp.111.096552 [DOI] [PubMed] [Google Scholar]
- Calhoun, L. G. , & Tedeschi, R. G. (2006). The foundations of posttraumatic growth: An expanded framework. In Calhoun L. G. & Tedeschi R. G. (Eds.), Handbook of posttraumatic growth (pp. 1–23). Lawrence Erlbaum Associates. [Google Scholar]
- Cao, C. , Wang, L. , Wu, J. , Li, G. , Fang, R. , Cao, X. , Liu, P. , Luo, S. , Hall, B. J. , & Elhai, J. D. (2018). Patterns of posttraumatic stress disorder symptoms and posttraumatic growth in an epidemiological sample of Chinese earthquake survivors: A latent profile analysis. Frontiers in Psychology, 9. 10.3389/fpsyg.2018.01549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao, X. , Wang, L. , Cao, C. Q. , Zhang, J. X. , Liu, P. , Zhang, B. A. , Wu, Q. , Zhang, H. , Zhao, Z. , Fan, G. , & Elhai, J. D. (2015). Patterns of DSM‐5 posttraumatic stress disorder and depressive symptoms in an epidemiological sample of Chinese earthquake survivors: A latent profile analysis. Journal of Affective Disorders, 186, 58–65. 10.1016/j.jad.2015.06.058 [DOI] [PubMed] [Google Scholar]
- Cenat, J. M. , Blais‐Rochette, C. , Kokou‐Kpolou, C. K. , Noorishad, P.‐G. , Mukunzi, J. N. , McIntee, S. ‐E. , Dalexis, R. D. , Goulet, M. A. , & Labelle, P. R. (2021). Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID‐19 pandemic: A systematic review and meta‐analysis. Psychiatry Research, 295, 113599. 10.1016/j.psychres.2020.113599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, F. , Zheng, D. , Liu, J. , Gong, Y. , Guan, Z. , & Lou, D. (2020). Depression and anxiety among adolescents during COVID‐19: A cross‐sectional study. Brain, Behavior, and Immunity, 88, 36–38. 10.1016/j.bbi.2020.05.061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, J. L. , & Wu, X. C. (2017a). Post‐traumatic stress symptoms and post‐traumatic growth among children and adolescents following an earthquake: A latent profile analysis. Child and Adolescent Mental Health, 22(1), 23–29. 10.1111/camh.12175 [DOI] [PubMed] [Google Scholar]
- Chen, J. L. , & Wu, X. (2017b). Posttraumatic stress symptoms and posttraumatic growth in children and adolescents following an earthquake: A latent transition analysis. Journal of Traumatic Stress, 30(6), 583–592. 10.1002/jts.22238 [DOI] [PubMed] [Google Scholar]
- Cieslak, R. , Benight, C. C. , & Lehman, V. C. (2008). Coping self‐efficacy mediates the effects of negative cognitions on posttraumatic distress. Behaviour Research and Therapy, 46(7), 788–798. 10.1016/j.brat.2008.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contractor, A. A. , Layne, C. M. , Steinberg, A. M. , Ostrowski, S. A. , Ford, J. D. , & Elhai, J. D. (2013). Do gender and age moderate the symptom structure of PTSD? Findings from a national clinical sample of children and adolescents. Psychiatry Research, 210(3), 1056–1064. [DOI] [PubMed] [Google Scholar]
- Cryder, C. H. , Kilmer, R. P. , Tedeschi, R. G. , & Calhoun, L. G. (2006). An exploratory study of posttraumatic growth in children following a natural disaster. American Journal of Orthopsychiatry, 76(1), 65–69. 10.1037/0002-9432.76.1.65 [DOI] [PubMed] [Google Scholar]
- Cui, P. P. , Wang, P. P. , Wang, K. , Ping, Z. , Wang, P. , & Chen, C. (2020). Post‐traumatic growth and influencing factors among frontline nurses fighting against COVID‐19. Occupational and Environmental Medicine, 78(2), 129–135. 10.1136/oemed-2020-106540 [DOI] [PubMed] [Google Scholar]
- Currier, J. M. , Hermes, S. , & Phipps, S. (2009). Brief report: Children's response to serious illness: perceptions of benefit and burden in a pediatric cancer population. Journal of Pediatric Psychology, 34(10), 1129–1134. 10.1093/jpepsy/jsp021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutheil, F. , Mondillon, L. , & Navel, V. (2020). PTSD as the second tsunami of the SARS‐Cov‐2 pandemic. Psychological Medicine. Advance online publication. 10.1017/S0033291720001336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers, A. , & Clark, D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345. 10.1016/S0005-7967(99)00123-0 [DOI] [PubMed] [Google Scholar]
- Fendrich, M. , Weissman, M. M. , & Warner, V. (1990). Screening for depressive disorder in children and adolescents: Validating the Center for Epidemiologic Studies Depression Scale for Children. American Journal of Epidemiology, 131(3), 538–551. 10.1093/oxfordjournals.aje.a115529 [DOI] [PubMed] [Google Scholar]
- Freedy, J. R. , Resnick, H. S. , & Kilpatrick, D. G. (1992). Conceptual framework for evaluating disaster impact: Implications for clinical intervention. In Austin L. S. (Ed.). Responding to disaster: A guide for mental health professionals (pp. 6–14). American Psychiatric Press; [Google Scholar]
- Foa, E. B. , Asnaani, A. , Zang, Y. , Capaldi, S. , & Yeh, R. (2018). Psychometrics of the Child PTSD Symptom Scale for DSM‐5 for Trauma‐Exposed Children and Adolescents. Journal of Clinical Child & Adolescent Psychology, 47(1), 38–46. 10.1080/15374416.2017.1350962 [DOI] [PubMed] [Google Scholar]
- Garnefski, N. , Baan, N. , & Kraaij, V. (2005). Psychological distress and cognitive emotion regulation strategies among farmers who fell victim to the foot‐and‐mouth crisis. Personality and Individual Differences, 38(6), 1317–1327. 10.1016/j.paid.2004.08.014 [DOI] [Google Scholar]
- Garnefski, N. , Boon, S. , & Kraaij, V. (2003). Relationships between cognitive strategies of adolescents and depressive symptomatology across different types of life events. Journal of Youth and Adolescence, 32(6), 401–408. 10.1023/A:1025994200559 [DOI] [Google Scholar]
- Garnefski, N. , Kraaij, V. , Schroevers, M. J. , & Somsen, G. A. (2008). Post‐traumatic growth after myocardial infarction: A matter of personality, psychological health, or cognitive coping? Journal of Clinical Psychology in Medical Settings, 15(4), 270–277. 10.1007/s10880-008-9136-5 [DOI] [PubMed] [Google Scholar]
- Garnefski, N. , Kraaij, V. , & Spinhoven, P. (2001). Negative life events, cognitive emotion regulation, and emotional problems. Personality and Individual Differences, 30(8), 1311–1327. 10.1016/S0191-8869(00)00113-6 [DOI] [Google Scholar]
- Ginzburg, K. , Ein‐Dor, T. , & Solomon, Z. (2010). Comorbidity of posttraumatic stress disorder, anxiety and depression: A 20‐year longitudinal study of war veterans. Journal of Affective Disorders, 123(1–3), 249–257. 10.1016/j.jad.2009.08.006 [DOI] [PubMed] [Google Scholar]
- Hamam, A. A. , Milo, S. , Mor, I. , Shaked, E. , Eliav, A. S. , & Lahav, Y. (2021). Peritraumatic reactions during the COVID‐19 pandemic: The contribution of posttraumatic growth attributed to prior trauma. Journal of Psychiatric Research, 132, 23–31. 10.1016/j.jpsychires.2020.09.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobfoll, S. E. (2002). Social and psychological resources and adaptation. Review of General Psychology, 6(4), 307–324. 10.1037/1089-2680.6.4.307 [DOI] [Google Scholar]
- Huh, H. J. , Kim, K. H. , Lee, H.‐K. , & Chae, J.‐H. (2017). The relationship between childhood trauma and the severity of adulthood depression and anxiety symptoms in a clinical sample: The mediating role of cognitive emotion regulation strategies. Journal of Affective Disorders, 213, 44–50. 10.1016/j.jad.2017.02.009 [DOI] [PubMed] [Google Scholar]
- Hussain, D. , & Bhushan, B. (2011). Posttraumatic stress and growth among Tibetan refugees: The mediating role of cognitive‐emotional regulation strategies. Journal of Clinical Psychology, 67(7), 720–735. 10.1002/jclp.20801 [DOI] [PubMed] [Google Scholar]
- Janoff‐Bulman, R. (1992). Shattered assumptions: Towards a new psychology of trauma. Free Press. [Google Scholar]
- Janoff‐Bulman, R. (2010). Shattered assumptions. Simon & Schuster. [Google Scholar]
- Joiner, Jr., T. E. , & Wagner, K. D. (1995). Attributional style and depression in children and adolescents: A meta‐analytical review. Clinical Psychology Review, 15(8), 777–798. 10.1016/0272-7358(95)00046-1 [DOI] [Google Scholar]
- Jose, P. E. , & Brown, I. (2008). When does the gender difference in rumination begin? Gender and age differences in the use of rumination by adolescents. Journal of Youth & Adolescence, 37(2), 180–192. [Google Scholar]
- Joseph, S. , & Linley, P. A. (2008). Positive psychological perspectives on posttraumatic stress: An intergrative psychosoical framework. In Joseph S. & Linley P. A. (Eds.), Trauma, recovery, and growth: Positive psychological perspective on posttraumatic stress. Wiley. [Google Scholar]
- Joseph, S. , Williams, R. , & Yule, W. (1997). Understanding post‐traumatic stress: A psychosocial perspective on PTSD and treatment. Wiley. [Google Scholar]
- Kaczkurkin, A. N. , Zang, Y. , Gay, N. G. , Peterson, A. L. , Yarvis, J. S. , Borah, E. V. , Dondanville, K. A. , Hembree, E. A. , Litz, B.T. , Mintz, J. , Young‐McCaughan, S. , & Foa, E. B. (2017). Cognitive emotion regulation strategies associated with the DSM‐5 posttraumatic stress disorder criteria. Journal of Traumatic Stress, 30(4), 343–350. 10.1002/jts.22202 [DOI] [PubMed] [Google Scholar]
- Kang, L. , Li, Y. , Hu, S. , Chen, M. , Yang, C. , Yang, B. X. , Wang, Y. , Hu, J. , Lai, J. , Ma, X. , Chen, J. , Guan, L. , Wang, G. , Ma, H. , & Liu, Z. (2020). The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. The Lancet Psychiatry, 7(3), e14. 10.1016/S2215-0366(20)30047-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimhi, S. , Eshel, Y. , Zysberg, L. , & Hantman, S. (2009). Getting a life: Gender differences in postwar recovery. Sex Roles, 61(7), 554–565. 10.1007/s11199-009-9660-2 [DOI] [Google Scholar]
- Klein, A. B. , Dutra, S. J. , Bovin, M. J. , Keane, T. M. , & Marx, B. P. (2020). The role of negative affect in differentiating posttraumatic stress disorder, depression, and their comorbidity among United States veterans. Journal Traumatic Stress, 34(2), 322–332. 10.1002/jts.22612 [DOI] [PubMed] [Google Scholar]
- Kraaij, V. , Garnefski, N. , & Vlietstra, A. (2008). Cognitive coping and depressive symptoms in definitive infertility: A prospective study. Journal of Psychosomatic Obstetrics & Gynecology, 29(1), 9–16. 10.1080/01674820701505889 [DOI] [PubMed] [Google Scholar]
- Lazarov, A. , Suarez‐Jimenez, B. , Levi, O. , Coppersmith, D. D. L. , Lubin, G. , Pine, D. S. , Bar‐Haim, Y. , Abend, R. , & Neria, Y. (2020). Symptom structure of PTSD and co‐morbid depressive symptoms: A network analysis of combat veteran patients. Psychological Medicine, 50(13), 2154–2170. 10.1017/s0033291719002034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, S. , Gwon, M. G. , & Kim, Y. J. (2018). The relationship between post‐traumatic growth, trauma experience, and cognitive emotion regulation in nurses. Korean Journal of Stress Research, 26(1), 31–37. 10.17547/kjsr.2018.26.1.31 [DOI] [Google Scholar]
- Liang, Y. , Zhou, Y. , & Liu, Z. (2021). Consistencies and differences in posttraumatic stress disorder and depression trajectories from the Wenchuan earthquake among children over a 4‐year period. Journal of Affective Disorders, 279, 9–16. 10.1016/j.jad.2020.09.107 [DOI] [PubMed] [Google Scholar]
- Liu, C. H. , Erdei, C. , & Mittal, L. (2021). Risk factors for depression, anxiety, and PTSD symptoms in perinatal women during the COVID‐19 Pandemic. Psychiatry Research, 295, 113552. 10.1016/j.psychres.2020.113552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, J. , Subramaniam, M. , Chong, S. A. , & Mahendran, R. (2019). A systematic examination of cognitive emotion regulation strategies, global emotion dysregulation, and cognitive insight in relation to posttraumatic stress disorder symptoms among trauma‐exposed patients with early nonaffective psychosis. Psychological Trauma: Theory, Research, Practice, and Policy. 10.1037/tra0000531 [DOI] [PubMed] [Google Scholar]
- Lubke, G. , & Muthén, B. O. (2007). Performance of factor mixture models as a function of model size, covariate effects, and class‐specific parameters. Structural Equation Modeling: A Multidisciplinary Journal, 14(1), 26–47. 10.1080/10705510709336735 [DOI] [Google Scholar]
- Maercker, A. , & Zoellner, T. (2004). The Janus face of self‐perceived growth: Toward a two‐component model of posttraumatic growth. Psychological Inquiry, 15(1), 41–48. [Google Scholar]
- Magruder, K. M. , Kilic, C. , & Koryurek, M. M. (2015). Relationship of posttraumatic growth to symptoms of posttraumatic stress disorder and depression: A pilot study of Iraqi students. International Journal of Psychology, 50(5), 402–406. 10.1002/ijop.12146 [DOI] [PubMed] [Google Scholar]
- McLean, C. P. , Zang, Y. , Gallagher, T. , Suzuki, N. , Yarvis, J. S. , Litz, B. T. , Mintz, J. , Young‐McCaughan, S. , Peterson, A. L. , & Foa, E. B. (2019). Trauma‐related cognitions and cognitive emotion regulation as mediators of PTSD change among treatment‐seeking active‐duty military personnel with PTSD. Behavior Therapy, 50(6), 1053–1062. 10.1016/j.beth.2019.03.006 [DOI] [PubMed] [Google Scholar]
- Meyerson, D. A. , Grant, K. E. , Carter, J. S. , & Kilmer, R. P. (2011). Posttraumatic growth among children and adolescents: A systematic review. Clinical Psychology Review, 31(6), 949–964. 10.1016/j.cpr.2011.06.003 [DOI] [PubMed] [Google Scholar]
- Moghanibashi‐Mansourieh, A. (2020). Assessing the anxiety level of Iranian general population during COVID‐19 outbreak. Asian Journal of Psychiatry, 51, 102076. 10.1016/j.ajp.2020.102076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murata, S. , Rezeppa, T. , Thoma, B. , Marengo, L. , Krancevich, K. , Chiyka, E. , Hayes, B. , Goodfriend, E. , Deal, M. , Zhong, Y. , Brummit, B. , Coury, T. , Riston, S. , Brent, D. , & Melhem, N. M. (2021). The psychiatric sequelae of the COVID‐19 pandemic in adolescents, adults, and health care workers. Depression and Anxiety, 38(2), 233–246. 10.1002/da.23120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén, L. K. , & Muthén, B. O. (2012). Mplus statistical modeling software: Release 7.0. Muthén & Muthén. [Google Scholar]
- Nolen‐Hoeksema, S. , Larson, J. , & Grayson, C. (1999). Explaining the gender difference in depressive symptoms. Journal of Personality and Social Psychology, 77(5), 1061–1072. 10.1037/0022-3514.77.5.1061 [DOI] [PubMed] [Google Scholar]
- O'Connor, N. , Kotze, B. , & Wright, M. (2011). Blame and accountability 1: Understanding blame and blame pathologies. Australasian Psychiatry, 19(2), 113–118. [DOI] [PubMed] [Google Scholar]
- Palic, S. , & Elklit, A. (2011). Psychosocial treatment of posttraumatic stress disorder in adult refugees: A systematic review of prospective treatment outcome studies and a critique. Journal of Affective Disorders, 131(1–3), 8–23. 10.1016/j.jad.2010.07.005 [DOI] [PubMed] [Google Scholar]
- Puechlong, C. , Weiss, K. , Le Vigouroux, S. , & Charbonnier, E. (2020). Role of personality traits and cognitive emotion regulation strategies in symptoms of post‐traumatic stress disorder among flood victims. International Journal of Disaster Risk Reduction, 50, 101688. 10.1016/j.ijdrr.2020.101688 [DOI] [Google Scholar]
- Rosellini, A. J. , Coffey, S. F. , Tracy, M. , & Galea, S. (2014). A person‐centered analysis of posttraumatic stress disorder symptoms following a natural disaster: Predictors of latent class membership. Journal of Anxiety Disorders, 28(1), 16–24. 10.1016/j.janxdis.2013.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider, S. , Rasul, R. , Liu, B. , Corry, D. , Lieberman‐Cribbin, W. , Watson, A. , Kerath, S. M. , Taioli, E. , & Schwartz, R. M. (2019). Examining posttraumatic growth and mental health difficulties in the aftermath of Hurricane Sandy. Psychological Trauma‐Theory Research Practice and Policy, 11(2), 127–136. 10.1037/tra0000400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Self‐Brown, S. , Lai, B. S. , Thompson, J. E. , McGill, T. , & Kelley, M. L. (2013). Posttraumatic stress disorder symptom trajectories in Hurricane Katrina–affected youth. Journal of Affective Disorders, 147(1–3), 198–204. 10.1016/j.jad.2012.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shevlin, M. , Hyland, P. , & Karatzias, T. (2020). Is posttraumatic stress disorder meaningful in the context of the COVID‐19 pandemic? A response to van Overmeire's commentary on Karatzias et al. (2020). Journal of Traumatic Stress, 33(5), 866–868. 10.1002/jts.22592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slanbekova, G. K. , Man Cheung, C. , Ayupova, G. T. , Kabakova, M. P. , Kalymbetova, E. K. , & Korotkova‐Ryckewaert, N. V. (2019). The relationship between posttraumatic stress disorder, interpersonal sensitivity and specific distress symptoms: The role of cognitive emotion regulation. Psychiatric Quarterly, 90(4), 803–814. 10.1007/s11126-019-09665-w [DOI] [PubMed] [Google Scholar]
- Sweeney, P. D. , Anderson, K. , & Bailey, S. (1986). Attributional style in depression: A meta‐analytic review. Journal of Personality and Social Psychology, 50(5), 974–991. 10.1037/0022-3514.50.5.974 [DOI] [PubMed] [Google Scholar]
- Tedeschi, R. G. , & Calhoun, L. G. (1996). The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9(3), 455–471. [DOI] [PubMed] [Google Scholar]
- Tedeschi, R. G. , & Calhoun, L. G. (2004). Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry, 15(1), 1–18. 10.1207/s15327965pli1501_01 [DOI] [Google Scholar]
- Thomas, E. A. , Hamrick, L. A. , Owens, G. P. , & Tekie, Y. T. (2020). Posttraumatic growth among undergraduates: Contributions from adaptive cognitive emotion regulation and emotional intelligence. Traumatology, 26(1), 68–73. 10.1037/trm0000203 [DOI] [Google Scholar]
- Tomaszek, K. , & Muchacka‐Cymerman, A. (2020). Thinking about my existence during COVID‐19, I feel anxiety and awe: The mediating role of existential anxiety and life satisfaction on the relationship between PTSD symptoms and Post‐traumatic growth. International Journal of Environmental Research and Public Health, 17(19), 7062. 10.3390/ijerph17197062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unseld, M. , Zeilinger, E. L. , Fellinger, M. , Lubowitzki, S. , Krammer, K. , Nader, I. W. , Hafner, M. , Kitta, A. , Adamidis, F. , Masel, E. K. , Preusser, M. , Jager, U. , & Gaiger, A. (2020). Prevalence of pain and its association with symptoms of post‐traumatic stress disorder, depression, anxiety and distress in 846 cancer patients: A cross‐sectional study. Psycho‐Oncology, 30(4), 504–510. 10.1002/pon.5595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard, N. , & Benros, M. E. (2020). COVID‐19 pandemic and mental health consequences: Systematic review of the current evidence. Brain, Behavior, and Immunity, 89, 531–542. 10.1016/j.bbi.2020.05.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner, B. (1993). On sin versus sickness: A theory of perceived responsibility and social motivation. American Psychologist, 48(9), 957–965. 10.1037/0003-066x.48.9.957 [DOI] [PubMed] [Google Scholar]
- Wisco, B. E. , Sloan, D. M. , & Marx, B. P. (2013). Cognitive emotion regulation and written exposure therapy for posttraumatic stress disorder. Clinical Psychological Science, 1(4), 435–442. 10.1177/2167702613486630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, X. , Wang, W. , Zhou, X. , Chen, Q. , & Lin, C. (2018). Investigation on the mental health state of adolescents after 8.5 years of Wenchuan earthquake. Psychological Development and Education, 34, 80–89. [Google Scholar]
- Wu, X. , Zhou, X. , Chen, J. , & Zeng, M. (2015). The relationship among deliberate rumination, posttraumatic stress disorder, and posttraumatic growth: Evidence from a longitudinal study of adolescents after Wenchuan earthquake. Psychological Development and Education, 31, 334–341. [Google Scholar]
- Xiong, J. , Lipsitz, O. , Nasri, F. , Lui, L. M. W. , Gill, H. , Phan, L. , Chen‐Li, D. , Iacobucci, M. , Ho, R. , Majeed, A. , & McIntyre, R. S. (2020). Impact of COVID‐19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64. 10.1016/j.jad.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang, X. , Wu, X. , Gao, M. , Wang, W. , Quan, L. , & Zhou, X. (2020). Heterogeneous patterns of posttraumatic stress symptoms and depression in cancer patients. Journal of Affective Disorders, 273, 203–209. 10.1016/j.jad.2020.04.033 [DOI] [PubMed] [Google Scholar]
- Ying, L. , Wu, X. , & Lin, C. (2012). Longitudinal linkages between depressive and posttraumatic stress symptoms in adolescent survivors following the Wenchuan earthquake in China: A three‐wave, cross‐lagged study. School Psychology International, 33(4), 416–432. 10.1177/0143034311421271 [DOI] [Google Scholar]
- Zhen, R. , & Zhou, X. (2020). Predictive factors of public anxiety under the outbreak of COVID‐19. Chinese Journal of Applied Psychology, 26(2), 99–107. [Google Scholar]
- Zhen, R. , Zhou, X. , & Wu, X. (2019). Patterns of posttraumatic stress disorder and depression among adolescents following an earthquake: A latent profile analysis. Child Indicators Research, 12(6), 2173–2187. 10.1007/s12187-019-09634-6 [DOI] [Google Scholar]
- Zhou, X. , & Wu, X. (2018). The mediating roles of acceptance and cognitive reappraisal in the relation between hope and posttraumatic growth among adolescents after the Ya'an earthquake. Journal of Pacific Rim Psychology, 12, e25. 10.1017/prp.2018.14 [DOI] [Google Scholar]
- Zhou, X. , Wu, X. , & Chen, J. (2015). Longitudinal linkages between posttraumatic stress disorder and posttraumatic growth in adolescent survivors following the Wenchuan earthquake in China: A three‐wave, cross‐lagged study. Psychiatry Research, 228(1), 107–111. 10.1016/j.psychres.2015.04.024 [DOI] [PubMed] [Google Scholar]
- Zhou, X. , Wu, X. , Fu, F. , & An, Y. (2015). Core belief challenge and rumination as predictors of PTSD and PTG among adolescent survivors of the Wenchuan earthquake. Psychological Trauma: Theory, Research, Practice, and Policy, 7(4), 391–397. [DOI] [PubMed] [Google Scholar]
- Zhou, X. , Wu, X. , Wang, W. , & Tian, Y. (2018). The relation between repetitive trauma exposure and posttraumatic stress disorder: Understanding the roles of feelings of safety and cognitive reappraisal. Psychological Development & Education, 34, 90–97. [Google Scholar]
- Zhou, X. , Wu, X. , & Zhen, R. (2017). Assessing the latent structure of DSM‐5 PTSD among Chinese adolescents after the Ya'an earthquake. Psychiatry Research, 254, 33–39. 10.1016/j.psychres.2017.04.029 [DOI] [PubMed] [Google Scholar]
- Zhou, X. , Wu, X. , & Zhen, R. (2018). Patterns of posttraumatic stress disorder and posttraumatic growth among adolescents after the Wenchuan earthquake in China: A latent profile analysis. Journal of Traumatic Stress, 31(1), 57–63. 10.1002/jts.22246 [DOI] [PubMed] [Google Scholar]
- Zhou, X. , Zhen, R. , & Wu, X. (2019a). How does parental attachment contribute to post‐traumatic growth among adolescents following an earthquake? Testing a multiple mediation model. European Journal of Psychotraumatology, 10(1), 1605280. 10.1080/20008198.2019.1605280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, X. , Zhen, R. , & Wu, X. (2019b). Shared and unique mechanisms underlying the association of trauma exposure with posttraumatic stress symptoms and growth among adolescents following the Jiuzhaigou earthquake. Psychological Trauma: Theory, Research, Practice, and Policy. Advance online publication. 10.1037/tra0000526 [DOI] [PubMed] [Google Scholar]
- Zhou, Y. , Liang, Y. , Tong, H. , & Liu, Z. (2020). Patterns of posttraumatic stress disorder and posttraumatic growth among women after an earthquake: A latent profile analysis. Asian Journal of Psychiatry, 51. 10.1016/j.ajp.2019.10.014 [DOI] [PubMed] [Google Scholar]
- Zhu, X. , Luo, F. , Yao, S. , & Pauerbach, R. (2007). Reliability and validity of the Cognitive Emotion Regulation Questionnaire: Chinese version. Chinese Journal of Clinical Psychology, 15, 121–124. [Google Scholar]
- Zhu, K. , Niu, Z. , Freudenheim, J. L. , Zhang, Z. , Lei, L. , Homish, G. G. , Cao, Y. , Zorich, S. C. , Yue, Y. , Liu, R. , & Mu, L. (2021). COVID‐19 related symptoms of anxiety, depression, and PTSD among U.S. adults. Psychiatry Research, 301, 113959. 10.1016/j.psychres.2021.113959 [DOI] [PMC free article] [PubMed] [Google Scholar]


