Abstract
Aims
We have previously demonstrated that vitamin D deficiency might be associated with worse outcomes in hospitalized Covid‐19 patients. The aim of our study was to explore this relationship with dexamethasone therapy.
Methods
We prospectively studied two cohorts of hospitalized Covid‐19 patients between March and April and between September and December 2020 (n = 192). Patients were tested for serum 25‐hydroxyvitamin D (25‐OH‐D) levels during admission. The first cohort not treated with dexamethasone (n = 107) was divided into vitamin D deficient (25‐OH‐D ≤ 30 nmol/L) (n = 47) and replete subgroups (25‐OH‐D > 30 nmol/L) (n = 60). The second cohort treated with dexamethasone (n = 85) was similarly divided into deficient (25‐OH‐D ≤ 30 nmol/L) (n = 27) and replete subgroups (25‐OH‐D > 30 nmol/L) (n = 58). Primary outcome was in‐hospital mortality and secondary outcomes were elevation in markers of cytokine storm and ventilatory requirement.
Results
No mortality difference was identified between cohorts and subgroups. The “no dexamethasone” cohort 25‐OH‐D deplete subgroup recorded significantly higher peak d‐Dimer levels (1874 vs. 1233 µgFEU/L) (p = 0.0309), CRP (177 vs. 107.5) (p = 0.0055), and ventilatory support requirement (25.5% vs. 6.67%) (p = 0.007) compared to the replete subgroup. Among the 25‐OH‐D deplete subgroup higher peak neutrophil counts, peak CRP, peak LDH, peak ferritin, and lower trough lymphocyte counts were observed, without statistical significance. In the “dexamethasone” cohort, there was no apparent association between 25‐OH‐D deficiency and markers of cytokine storm or ventilatory requirement.
Conclusion: Vitamin D deficiency is associated with elevated markers of cytokine storm and higher ventilatory requirements in hospitalized Covid‐19 patients. Dexamethasone treatment appears to mitigate adverse effects of vitamin D deficiency.
Keywords: covid‐19, cytokine storm, dexamethasone, ventilation, vitamin D
1. INTRODUCTION
The emergence of coronavirus disease (Covid‐19) caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) has fueled global efforts to identify risk factors for adverse outcomes, of which vitamin D is one potential marker subject to scientific interest.
Vitamin D is a secosteroid with important immunomodulatory, anti‐inflammatory, antifibrotic, and antioxidant actions. There is growing evidence of a relationship between vitamin D insufficiency and worse outcomes in Covid‐19. 1 Indeed, Covid‐19 hospitalization and mortality rates appear to be higher at northern latitudes compared with equatorial regions and the disease disproportionately affects people from ethnic minorities. These factors may suggest correlation between sun exposure, vitamin D levels, and Covid‐19 outcomes. 2 , 3
We previously assessed the potential relationship between vitamin D deficiency and Covid‐19 disease severity in hospitalized adults and demonstrated that patients with lower serum concentrations of vitamin D during active Covid‐19 were more likely to develop features of cytokine storm and require ventilatory support. 4
The RECOVERY trial 5 demonstrated a reduction in all‐cause reduction in mortality amongst Covid‐19 patients after 28 days treated with dexamethasone. In light of these data, we aimed to identify the impact of dexamethasone therapy on the association between vitamin D deficiency and Covid‐19 severity, as defined by markers of cytokine storm and ventilatory requirement in hospitalized patients.
2. METHODS
2.1. Population
Patients treated for active Covid‐19 at our institution were recruited during two separate time periods. Active Covid‐19 infection was defined as those with positive real‐time reverse‐transcriptase polymerase chain reaction (RT‐PCR) assay for SARS‐CoV‐2 on nasopharyngeal swab or those being treated for Covid‐19 on clinical and radiological evidence. 6 During the first recruitment period between March 2020–April 2020, no patients received dexamethasone for Covid‐19. In the second recruitment period between October 2020‐December 2020, standard treatment for Covid‐19 in patients with an oxygen requirement was 6 mg dexamethasone daily for 7–10 days. Patients were grouped into those who received dexamethasone and those who did not. Each group was subsequently divided into subgroups for vitamin D‐deficient (25‐OH‐D ≤ 30 nmol/L) and ‐replete (25‐OH‐D > 30 nmol/L), as per national guidelines and local laboratory standards. 7 Patients found vitamin D‐deficient were supplemented in accordance with national guidelines.
2.2. Data collection
Patient demographics and comorbidities were extracted from patient records. Vitamin D (25‐OH‐D) levels were measured for all patients during admission. Biochemical/hematological markers of cytokine storm measured throughout the admission were recorded, including peak values for neutrophils, C reactive protein (CRP), lactate dehydrogenase (LDH), ferritin, troponin T, d‐dimer, and trough values for lymphocyte count. The primary outcome was in‐hospital mortality whilst secondary outcomes included ventilatory support (defined as continuous positive airway pressure, non‐invasive ventilation, or mechanical invasive ventilation) and laboratory markers of cytokine storm.
2.3. Statistical analysis
All statistical analyses were performed on GraphPad Prism version 8. Continuous variables were assessed for normality using Shapiro–Wilk and Kolmogorov–Smirnov tests and tested for significance with either an unpaired t test if parametric or a Mann–Whitney U test if non‐parametric. If possible, outcome sets were normalized by logarithmic transformation and tested for significance using a parametric method. A p < 0.05 (two‐tailed test) was considered statistically significant.
2.4. Ethics
This study was approved by our institution's audit department with reference FH119 using clinically collected, non‐identifiable data which does not fall under the remit of the NHS Research Ethics Committee. All data were collected locally and handled in accordance with local data protection policies. Serum 25‐OH‐D levels were tested alongside routine serum laboratory investigations without the need for any extra phlebotomy. Patients received care as per standard practices for the management of Covid‐19 throughout the study period.
3. RESULTS
During both recruitment periods, a total of 192 Covid‐19 patients were recruited to the study; 85 patients (44%) received dexamethasone and 107 patients (56%) did not (Figure 1). In the “dexamethasone” group”, 27 patients had 25‐OH‐D levels ≤30 nmol/L, with 58 patients having levels >30 nmol/L. In the “no dexamethasone” group, 47 patients were found to have a 25‐OH‐D level ≤30 nmol/L, while 60 had levels >30 nmol/L.
Figure 1.
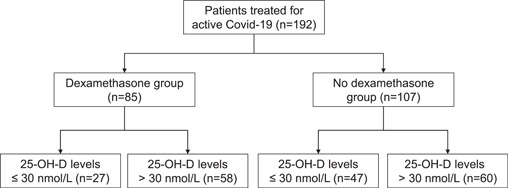
Flow chart depicting allocation of patients to groups based on dexamethasone therapy and subgroups based on inpatient 25‐OH‐D level
Overall, the mean age of the entire study population was 77.7 years ±12.2. Demographics (age, gender, frailty, and body mass index) and comorbidities between the “dexamethasone” and “no dexamethasone groups” and between the subgroups divided by 25‐OH‐D levels were comparable (Table 1). Among the entire cohort, only 7 patients required treatment in the intensive care unit (ICU).
Table 1.
Population characteristics of dexamethasone treatment subgroups further subdivided by 25‐OH‐D status. In addition, the relative prevalence of common co‐morbidities is noted
| No Dexamethasone | p value | Dexamethasone Treated | p value | |||
|---|---|---|---|---|---|---|
| 25‐OH‐D Level | ≤30 nmol/L | >30 nmol/L | ≤30 nmol/L | >30 nmol/L | ||
| Number | 47 | 60 | 27 | 58 | ||
| Age Mean (SD) | 79.3 (+/− 9.3) | 82.7 (+/− 8.4) | 70.1 (+/– 16.6) | 74.9 (+/− 13.0) | ||
| Gender (M:F) | 30:17 | 33:27 | 12:15 | 33:25 | ||
| Rockwood Frailty Score Median (IQR) | 6 (6–7) | 6 (4–6) | 0.1118 | 3 (1–5) | 4 (3–5) | 0.2019 |
| Body Mass Index Median (IQR) | 25 (23–32) | 24 (21–28) | 0.0583 | 28 (24–33) | 28 (25–31) | 0.7436 |
| Number (%) | p value | Number (%) | p value | |||
| Hypertension | 21 (44.68) | 29 (48.33) | 0.7085 | 15 (55.56) | 25 (43.10) | 0.2868 |
| Diabetes | 21 (44.68) | 16 (26.67) | 0.053 | 12 (44.44) | 20 (34.48) | 0.3804 |
| Ischaemic Heart Disease | 9 (19.15) | 17 (28.33) | 0.2741 | 5 (18.52) | 12 (20.69) | 0.8169 |
| Chronic Respiratory Disease | 8 (17.02) | 17 (28.33) | 0.172 | 9 (33.33) | 20 (34.48) | 0.9176 |
| Heart Failure | 7 (14.89) | 13 (21.67) | 0.3742 | 3 (11.11) | 7 (12.07) | 0.8988 |
| Stroke | 9 (19.15) | 7 (11.67) | 0.2839 | 5 (18.52) | 3 (5.17) | 0.0511 |
| Dementia | 8 (17.02) | 8 (13.33) | 0.597 | 4 (14.81) | 4 (6.90) | 0.2477 |
| Chronic Kidney Disease | 13 (27.66) | 16 (26.67) | 0.9094 | 7 (25.93) | 11 (18.97) | 0.4673 |
| Atrial Fibrillation | 7 (14.89) | 13(21.67) | 0.3742 | 6 (22.22) | 16 (27.59) | 0.6009 |
| Malignancy | 4 (8.51) | 6 (10.00) | 0.7937 | 1 (3.70) | 6 (10.34) | 0.3026 |
| Endocrine Disease | 2 (4.26) | 2 (3.33) | 0.8022 | 4 (14.81) | 6 (10.34) | 0.5538 |
Note: In addition, the relative prevalence of common comorbidities is noted.
Abbreviation: IQR, interquartile range.
There was no significant difference in mortality rate between all groups or subgroups. In the “no dexamethasone” group, low 25‐OH‐D levels were associated with statistically significant higher peak CRP (177 vs. 107.5 mg/L, p = 0.006) and d‐dimer (1874 vs. 1233 µgFEU/L, p = 0.03) values (Table 2). The low 25‐OH‐D subgroup produced higher peak neutrophil counts, peak LDH, peak ferritin, and lower trough lymphocyte counts without reaching statistical significance. Amongst patients with lower 25‐OH‐D levels, there was a greater incidence in ventilatory requirement (25.5% vs. 6.67%, p = 0.007). However, in the “dexamethasone” group, there was no apparent association between 25‐OH‐D deficiency and markers of cytokine storm, including neutrophils, CRP, LDH, ferritin, troponin T, d‐dimer, and lymphocytes; or ventilatory requirement.
Table 2.
Biochemical markers of cytokine storm and clinical markers of severity in the dexamethasone and 25‐OH‐D subgroups
| No Dexamethsone | p value | Dexamethasone Treated | p value | |||
|---|---|---|---|---|---|---|
| 25‐OH‐D Level | ≤30 nmol/L | >30 nmol/L | ≤30 nmol/L | >30 nmol/L | ||
| Number | 47 | 60 | 27 | 58 | ||
| Median Value (IQR) | p value | Median Value (IQR) | p value | |||
| Peak Neutrophil count [x109/L] | 8.13 (4.22–10.31) | 6.85 (4.96–10.34) | 0.6855 | 8.86 (6.16–11.39) | 12.35 (8.88–16.30) | 0.4441 |
| Trough Lymphocyte count [x109/L] | 0.95 (0.74–1.27) | 0.97 (0.63–1.40) | 0.9368 | 0.55 (0.45–0.69) | 0.50 (0.35–0.71) | 0.0809 |
| Peak CRP [mg/L] | 177 (108–260) | 107.50 (66.25–175.50) | 0.0055 | 105.5 (72.5) | 137 (86.5–193) | 0.1571 |
| Peak LDH [IU/L] | 264 (217–351) | 232 (176–309) | 0.0691 | 415 (225–572) | 372 (284–511) | 0.1588 |
| Peak Ferritin [ug/L] | 507 (283–1166) | 461 (259–889) | 0.3625 | 890 (532–1118) | 962 (486–2159) | 0.4354 |
| Peak Troponin [ng/L] | 37 (26–93) | 46 (28–89) | 0.8437 | 31 (15–42) | 25 (11–51) | 0.8436 |
| Peak D‐Dimer [ugFEU/L] | 1874 (1195–2654) | 1233 (768–2246) | 0.0309 | 1951 (1171–5564) | 2018 (699–3568) | 0.1232 |
| Number (%) | Number (%) | |||||
| Ventilation | 12 (25.5) | 4 (6.67) | 0.007 | 11 (40.74) | 15 (25.92) | 0.1701 |
| Mortality | 7 (14.8) | 10 (16.6) | 0.8 | 7 (25.92) | 17 (29.31) | 0.7472 |
Abbreviations: CRP, C reactive protein; IQR, interquartile range; LDH, lactate dehydrogenase.
A similar pattern of results was obtained from a post‐hoc analysis using a 25‐OH‐D cut‐off value of 50 nmol/L. The non‐dexamethasone‐treated group showed statistically higher CRP (p = 0.0396) and ventilation requirement (p = 0.023) for the low 25‐OH‐D subgroup. Notably, in this group, mean d‐dimer was still higher in the low 25‐OH‐D cohort, but did not achieve statistical significance. There were no statistically significant differences between the 25‐OH‐D deficient and replete subgroups in those treated with dexamethasone.
4. DISCUSSION
We have previously demonstrated that, in the absence of dexamethasone therapy, patients with vitamin D deficiency recorded increased markers of cytokine storm release (namely CRP and d‐dimer) which are associated with severe Covid‐19. Furthermore, low vitamin D levels were associated with worsened patient outcomes defined by ventilatory requirement. 4
Our current data suggest that, in the presence of dexamethasone, the impact of vitamin D deficiency on cytokine storm markers and ventilatory requirement is reduced. Both legs of our study were performed in the same center and given similarities in demographics and comorbidities between patient populations treated with and without dexamethasone, it is likely that dexamethasone independently mitigates the effects of vitamin D deficiency on cytokine storm and ventilatory requirements.
Vitamin D is a secosteroid synthesized in the skin, liver, and kidneys, and its active hormone, 1,25(OH)2D3, controls phosphate and calcium homeostasis under physiological conditions. As well as being essential for musculoskeletal health, vitamin D plays an important role in interacting with the innate and adaptive immune system. This study adds to the growing body of evidence that vitamin D deficiency is associated with worsened outcomes in Covid‐19. As yet, the underlying pathophysiological mechanism have not been fully elucidated. It has been postulated that vitamin D switches the adaptive immune reaction phenotype 8 , 9 and downregulates differentiation into proinflammatory Th17 cells, 10 , 11 which may reduce the cytokine storm in Covid‐19. Vitamin D also exerts a protective effect on alveolar cells by preserving endothelial integrity and reducing vascular permeability. 12
Combined evidence suggests that dexamethasone should be considered standard of care for critically ill patients with Covid‐19 pneumonitis requiring supplemental oxygen therapy or ventilatory support. Dexamethasone is presently the only corticosteroid to show a statistically significant reduction in all‐cause mortality at 28 days. 13 The mortality benefit was specifically recognized in patients with supplemental oxygen or mechanical ventilatory requirements.
Dexamethasone is a corticosteroid used in a range of conditions for its anti‐inflammatory and immunosuppressive properties with immediate and longer‐term effects. Initial actions of corticosteroids result from: binding to the membrane‐associated glucocorticoid receptors (GR) on target cells (such as T‐lymphocytes) which impairs the cell‐mediated immune response and, secondly, from alterations in trans‐membranous calcium and sodium flux, which provides an acute anti‐inflammatory effect. 14 Sustained effects arise from intracellular GR binding, which results in stimulation of key anti‐inflammatory cytokines and suppression of the proinflammatory cascade. Thereby, corticosteroids modulate important components of the inflammatory and immune response seen in cytokine storm. This may explain why dexamethasone treatment seemingly negates the effects of vitamin D deficiency in hospitalized patients with Covid‐19.
It has also been established that the diverse physiological actions of 1,25(OH)2D3 are initiated through morphisms in gene expression which are mediated by an intracellular vitamin D receptor (VDR). 15 The VDR regulates a variety of metabolic pathways including those involved in the immune response. 16 Both vitamin D and dexamethasone share many VDR pathways. 17 On the basis of these shared VDR attributes, it is reasonable to assume that interplay between both vitamin D and dexamethasone could influence Covid‐19 severity through related pathophysiological mechanisms. 18
There are a growing number of observational studies worldwide connecting the risk of contracting Covid‐19 and severity of illness with vitamin D status. A meta‐analysis of 27 studies found that vitamin D insufficiency among patients with Covid‐19 was significantly associated with higher risks of severe infection, hospitalization, and mortality. 19 At the time of writing, there are several ongoing clinical trials aiming to identify a possible benefit of vitamin D supplementation on hospitalized patient outcomes in Covid‐19. However, the use of dexamethasone is likely to mitigate the identification of any signals due to vitamin D on inpatient outcomes such as respiratory failure.
5. LIMITATIONS
As a single‐center study at a district general hospital in Southern England, we cannot generalize our results. Population demographics and socioeconomic status may not be representative of populations in other areas. Our results may not be as relevant in populations at different latitudes or populations with different ethnicities.
As a study with a limited sample size, the power of our results is reduced. Even though statistical significance was achieved for certain variables, the lack of significance in others does not necessarily mean that there was no association; instead, it may be attributed to the small sample size. Since multiple comparisons were performed in this study, the likelihood of observing a significant difference due to chance is increased. In addition, outcomes may have also been influenced by the changing local and national protocols on management of Covid‐19. 20
We acknowledge that data collection through medical notes requires individual interpretation of those records which despite best efforts, may not demonstrate the full clinical picture. Data collection was performed by more than one individual to reduce such interpretation bias.
We understand that sun exposure may affect the levels of vitamin D and unfortunately, it was a factor we could not accurately quantify or account for. 21 Our study recruited patients over a 5‐month period during which exposure to sunlight greatly varied.
6. CONCLUSION
Our study demonstrates that dexamethasone therapy may lessen adverse effects of vitamin D deficiency in terms of cytokine release and ventilation requirement in hospitalized patients with Covid‐19. However, it is undisputed that vitamin D is a safe and cost‐effective intervention with multiple health benefits and efforts to achieve reference nutrient intakes should be encouraged. Further research might focus on the impact of Vitamin D supplementation in the community and the prevention of hospitalization of Covid‐19 patients.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
ETHICS STATEMENT
This study was approved by our institution's Research, Quality Improvement, and Audit Department with reference FH119. This study does not fall under the remit of the National Health Service Research Ethics Committees. This statement is also present in the methods section of our manuscript. It was not appropriate or possible to involve patients or the public in the design, or conduct, or reporting, or dissemination plans of our research.
AUTHOR CONTRIBUTIONS
All 11 authors contributed to the manuscript and were involved in the design of the study. Charlotte Wenban, Randeep S. Heer, Pirabakaran Kandiah, Theodora Katsanouli, Asmita Pandey, and Afiyah Ajaz collected the data. Vadir Baktash was responsible for the statistical analysis. Charlotte Wenban, Randeep S. Heer, Vadir Baktash, Asmita Pandey, Ryan Goindoo, and Amit K. J. Mandal wrote the manuscript and all authors were involved in the final approval of the manuscript. Amit K. J. Mandal and Constantinos G. Missouris are acting as guarantors of the submitted work.
Wenban C, Heer RS, Baktash V, et al. Dexamethasone treatment May mitigate adverse effects of vitamin D deficiency in hospitalised Covid‐19 patients. J Med Virol. 2021;93:6605‐6610. 10.1002/jmv.27215
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Liu N, Sun J, Wang X, Zhang T, Zhao M, Li H. Low vitamin D status is associated with coronavirus disease 2019 outcomes: a systematic review and meta‐analysis. Int J Infect Dis. 2021;104:58‐64. 10.1016/j.ijid.2020.12.077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sze S, Pan D, Nevill CR, et al. Ethnicity and clinical outcomes in COVID‐19: a systematic review and meta‐analysis. EClinicalMedicine. 2020;29‐30:100630. 10.1016/j.eclinm.2020.100630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Panarese A, Shahini E. Letter: Covid‐19, and vitamin D. Aliment Pharmacol Ther. 2020;51:993‐995. 10.1111/apt.15752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Baktash V, Hosack T, Patel N, et al. Vitamin D status and outcomes for hospitalised older patients with COVID‐19. Postgrad Med J. 2020;97:442‐447. 10.1136/postgradmedj-2020-138712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Recovery Collaborative G, Horby P, Lim WS, et al. Dexamethasone in hospitalized patients with Covid‐19. N Engl J Med. 2021;384:693‐704. 10.1056/nejmoa2021436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Treanor L, Islam N, Ebrahimzadeh S, McInnes M. The Cochrane systematic review on thoracic imaging tests for the diagnosis of COVID‐19. Radiology. 2021;299:210564. 10.1148/radiol.2021210564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Giustina A, Adler RA, Binkley N, et al. Controversies in vitamin D: summary statement from an international conference. J Clin Endocrinol Metab. 2018;104:234‐240. 10.1210/jc.2018-01414 [DOI] [PubMed] [Google Scholar]
- 8. Mattner F, Smiroldo S, Galbiati F, et al. Inhibition of Th1 development and treatment of chronic‐relapsing experimental allergic encephalomyelitis by a non‐hypercalcemic analogue of 1,25‐dihydroxyvitamin. Eur J Immunol. 2000;30:498‐508. [DOI] [PubMed] [Google Scholar]
- 9. Boonstra A, Barrat FJ, Crain C, Heath VL, Savelkoul HF, O'Garra A. 1α,25‐Dihydroxyvitamin D3 has a direct effect on naive CD4+ T cells to enhance the development of Th2 cells. J Immunol. 2001;167:4974‐4980. 10.4049/jimmunol.167.9.4974 [DOI] [PubMed] [Google Scholar]
- 10. Tang J, Zhou R, Luger D, et al. Calcitriol suppresses antiretinal autoimmunity through inhibitory effects on the Th17 effector response. J Immunol. 2009;182:4624‐4632. 10.4049/jimmunol.0801543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Daniel C, Sartory NA, Zahn N, Radeke HH, Stein JM. Immune modulatory treatment of trinitrobenzene sulfonic acid colitis with calcitriol is associated with a change of a T helper (Th) 1/Th17 to a Th2 and regulatory T cell profile. J Pharmacol Exp Ther. 2007;324:23‐33. 10.1124/jpet.107.127209 [DOI] [PubMed] [Google Scholar]
- 12. Gibson CC, Davis CT, Zhu W, et al. Dietary vitamin D and its metabolites non‐genomically stabilize the endothelium. PLOS One. 2015;10:e0140370. 10.1371/journal.pone.0140370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Liu P, Stenger S, Li H, Wenzel L. Toll‐like receptor triggering of a vitamin D‐mediated human antimicrobial response. Science. 2006;311(5768):1770‐1773. [DOI] [PubMed] [Google Scholar]
- 14. Yasir M, Goyal A, Bansal P, et al. Corticosteroid Adverse Effects. Treasure Island (FL): StatPearls 2021.
- 15. Hidalgo AA, Deeb KK, Pike JW, Johnson CS, Trump DL. Dexamethasone enhances 1α,25‐dihydroxyvitamin D3 effects by increasing vitamin D receptor transcription*. J Biol Chem. 2011;286:36228‐36237. 10.1074/jbc.m111.244061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Adorini L, Daniel K, Penna G. Vitamin D receptor agonists, cancer and the immune system: an intricate relationship. Curr Top Med Chem. 2006;6:1297‐1301. 10.2174/156802606777864890 [DOI] [PubMed] [Google Scholar]
- 17. Navarro‐Barriuso J, Mansilla MJ, Naranjo‐Gómez M, et al. Comparative transcriptomic profile of tolerogenic dendritic cells differentiated with vitamin D3, dexamethasone and rapamycin. Sci Rep. 2018;8:8. 10.1038/s41598-018-33248-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Torjesen I. Covid‐19: public health agencies review whether vitamin D supplements could reduce risk. BMJ. 2020;369:m2475. 10.1136/bmj.m2475 [DOI] [PubMed] [Google Scholar]
- 19. Charoenngam N, Shirvani A, Holick MF. Vitamin D and its potential benefit for the COVID‐19 pandemic. Endocr Pract. 2021;27(5):484‐493. 10.1016/j.eprac.2021.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. NICE . COVID‐19. National institute for health and care excellence. 2020. Accessed March 28, 2021. https://www.nice.org.uk/guidance/conditions-and-diseases/respiratory-conditions/covid19
- 21. NHS . How to get vitamin D from sunlight. NHS Choices. 2018. Accessed March 28, 2021. https://www.nhs.uk/live-well/healthy-body/how-to-get-vitamin-d-from-sunlight/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


