Abstract
In response to the Covid‐19 pandemic, medical educators have transformed pre‐clerkship anatomy curricula into online formats. The purpose of this study was to evaluate the effectiveness and student perceptions of an online near‐peer anatomy curriculum. The classes of 2022 and 2023 completed identical foundational anatomy curricula in‐person, whereas the class of 2024 completed an adapted curriculum for remote online learning. Quantitative and qualitative responses were used to compare attitudes between instructional methods. Assessment scores and evaluation survey responses were collected from the classes of 2022 (n = 185), 2023 (n = 184), and 2024 (n = 183). Mean assessment scores (±SD) for the classes of 2022, 2023, and 2024 were 93.64% (±5.86), 93.75% (±4.09), and 92.04% (±4.83), respectively. Post hoc group comparisons showed the class of 2024 scored significantly lower than the two previous classes [2022: (H(1) = 18.58, P < 0.001), 2023: (H(1) = 18.65, P < 0.001)]. Mean survey results concerning curriculum quality were 4.06/5.00 for the class of 2023 and 3.57/5.0 for the class of 2024 (t(365) = 2.67, P = 0.008). Considering a small effect size (η 2 = 0.034), there was no meaningful difference in student assessment scores. A potential drawback of online near‐peer anatomy teaching remains in student perceptions of course quality; qualitative feedback suggested technological limitations and perceptions of online course instructors were partly responsible for lower student satisfaction. Following the Covid‐19 pandemic, medical educators should incorporate the lessons learned from this unique educational inflection point to improve curricula moving forward.
Keywords: Covid‐19, gross anatomy education, medical education, near‐peer teaching, online learning, preclinical courses, undergraduate education
INTRODUCTION
The emergence of the 2019 coronavirus disease (Covid‐19) pandemic disrupted medical education, but provided an opportunity to reflect on and improve didactic practices (Rose, 2020). Social distancing mandates prevented medical faculty from organizing face‐to‐face learning sessions (Evans et al., 2020; Rose, 2020). In response, medical educators transformed curricula and examinations to online formats (Blankenburg et al., 2020; Rose, 2020). Although lecture‐style teaching is easily adapted to a video conferencing platform, kinesthetic learning and conversational didactic sessions, where students interact with other students and instructors, were largely disrupted by this switch (Cuschieri and Agius, 2020; Hilburg et al., 2020). Medical education has increasingly become team‐based, and shifting a team online inevitably disrupts its dynamic (Wayne et al., 2020). However, the disruption also provided an opportunity to try out alternate approaches to establish new methodologies.
Advances in technology played a particularly important role in the evolution of pedagogy in anatomical science curricula during the Covid‐19 pandemic (Evans et al., 2020). In shifting online, medical education responded to new technological problems, reduced student engagement, loss of integrated hands‐on experiences, and a change in teaching pedagogy (Pather et al., 2020; Wilcha, 2020). Medical educators faced many practical challenges in restructuring material for effective online anatomy teaching. To avoid a poor‐quality learning experience, Martin and Bolliger (2018) warned against simply putting existing resources online. Recordings or duplications of in‐person learning activities may not engage online learners or promote deeper learning the way they might in‐person. As medical education begins to resume in‐person activities after the pandemic, it is essential to identify and evaluate the successes and failures of the teaching methodologies adopted during the pandemic (Smith and Pawlina, 2021).
Educators have previously called for research evaluating the effectiveness of online anatomy learning (Pei and Wu, 2019); thus, the forced transition to online anatomy learning caused by Covid‐19 created an opportunity to evaluate whether online approaches can be as effective as in‐person learning (Franchi, 2020). A systematic review of randomized controlled trials comparing eLearning to traditional learning in health professions with outcome goals of understanding student knowledge, skills, satisfaction, and attitudes toward eLearning found that eLearning is equivalent, and possibly superior to traditional learning, with significant heterogeneity among the studies (George et al., 2014).
Learning anatomy remotely has a unique set of challenges compared to other medical curricula. Anatomy is a three‐dimensional subject that requires an understanding of the relationships between structures, which may be difficult to garner from an online‐only platform. It was vital to try to preserve student understanding of anatomical concepts in the switch to virtual learning; medical students traditionally have anatomical knowledge that falls short of preclinical expectations, performing poorly in anatomy relative to their other basic science courses (Malau‐Aduli et al., 2019).
Interest in near‐peer teaching (NPT) within undergraduate medical programs has grown in both literature and practice in recent years (Yu et al., 2011; Johansson et al., 2018). Near‐peer teaching, as a pedagogical approach, involves more experienced students taking on the role of instructor for less experienced students (Topping, 1996; Evans and Cuffe, 2009). It is thought to be a successful teaching method because of social and cognitive congruence between peers, as compared to a student–faculty relationship (Evans and Cuffe, 2009; Benè and Bergus, 2014). Although NPT does not necessarily lead to greater academic achievement, in a systematic review of NPT, medical students were shown to perform similarly on tests of knowledge and skills regardless of having a faculty instructor or near‐peer instructor (Yu et al., 2011; Benè and Bergus, 2014; Stigmar, 2016). Additionally, NPT has been shown to promote critical thinking, learning autonomy, collaboration, and communicative skills (Stigmar, 2016; Wilcha, 2020). Even in a virtual format, NPT increases engagement and creates a safe learning space as compared to faculty lead sessions (Hampshire et al., 2020). Near‐peer teaching of cadaveric anatomy is known to receive positive feedback from medical students related to learning efficacy and course satisfaction (Evans and Cuffe, 2009; Dickman et al., 2017; Agius et al., 2018). During the transition to the Covid‐19 pandemic, the majority of preclinical medical students at the University of Malta in departments of Medicine and Surgery perceived a positive learning experience following the shift to remote lectures; however, this was not the case for small group teaching (Cuschieri and Agius, 2020). In contrast, Uddin et al. (2020) found that virtual NPT was an effective alternative to classroom learning in terms of overall quality, relevance, and usefulness from the perspective of the trainees.
Internal investigations conducted by the authors have validated NPT in foundational anatomy concepts, and it has been employed successfully for many years at the Case Western Reserve University (CWRU) School of Medicine (SOM) (Kiene et al., 2009). However, it is unknown whether NPT of anatomy remains as effective when conducted remotely. Furthermore, Estai and Bunt (2016) called for anatomy teaching modalities to be evaluated not only for their effectiveness, but also for student perceptions. When designing medical education in the wake of Covid‐19, understanding how students experience online learning was a key step in evaluating how that online learning satisfied learning outcomes (Reyna, 2020). Therefore, the aim of this study was to validate online NPT as a learning strategy that promoted student knowledge of anatomy consistent with that of in‐person learning. The objectives of this study were to (1) evaluate the effectiveness of the remote near‐peer anatomy curriculum relative to the equivalent in‐person learning environment using student assessment scores, and (2) collect student perspectives on the online near‐peer learning environment to identify its limitations and potential areas of improvement. The authors hypothesized a difference would be seen between online NPT and in‐person NPT in both student assessment scores and student satisfaction with course quality.
MATERIALS AND METHODS
Anatomical sciences curriculum
This prospective study with historical controls was an investigation regarding the remote near‐peer anatomy curriculum at CWRU SOM in Cleveland, Ohio, USA. The anatomy curriculum at CWRU runs throughout the pre‐clerkship curriculum. It includes a ten‐hour introductory block (Block One anatomy), a two‐week 40‐hour dissection course (Anatomy Bootcamp), followed by a 16‐month, 54 hour curriculum known as Gross Anatomy, Radiology and Living Anatomy (GARLA) (Wish‐Baratz et al., 2019). Block One anatomy consists of four weeks of NPT introductory units, followed by a written examination in the fifth week. Each session is two hours, and takes place with eight first‐year students and one second‐year near‐peer tutor to cover fundamental, introductory topics in anatomy and radiology. A summary of the topics covered and the adaptations made for online learning are illustrated in Table 1. Block One anatomy is evaluated using a written examination, Anatomy Bootcamp is evaluated using a practical examination, and GARLA for blocks two through six is evaluated using both written and practical examinations. The GARLA curriculum has no lectures; during a two‐hour GARLA session, students rotate through three stations: virtual anatomy (gross anatomy), imaging (radiology), and ultrasound/physical diagnosis with standardized patients (living anatomy) while focusing on a specific topic common to all three stations. All lecture material was pre‐recorded and posted on the learning management system used by CWRU SOM students.
TABLE 1.
Concepts covered in the Case Western Reserve University School of Medicine near‐peer introductory anatomy curriculum. In‐person session highlights and their adaptations for remote learning are specified for each session
| Week 1 | Week 2 | Week 3 | Week 4 | |
|---|---|---|---|---|
| Session name (time allotted) |
|
|
|
|
| Topics covered |
|
|
|
|
| In‐person session highlights |
|
|
|
|
| Remote learning adaptations |
|
|
|
|
Abbreviations: CNS, central nervous system; MRI, magnetic resonance imaging.
Near peer teaching small group sessions
Prior to each of the four Block One two‐hour NPT sessions, students were given preparatory material, such as a tutorial on the pelvic and shoulder girdles. Learning sessions were led by two second‐year medical students who were trained on course content in advance of each session. While the leaders directed the session using a PowerPoint presentation (Microsoft Corp., Redmond, WA), students followed along using a written learning module.
When in‐person, the learning sessions accessed skeletal models, practiced palpation/percussion/auscultation with peers, and students participated in drawing exercises. For example, students participated in a “T‐Shirt exercise” where surface anatomy and viscera were drawn on their peers as they wore a blank white T‐shirt. The wiring of central nervous system pathways (i.e., spinal nerves, the stretch reflex, and the sympathetic nervous system) was drawn as a group on classroom whiteboards.
When learning remotely, presentations and models had to be adapted for the online setting. Bony models and skeletons were replaced with tutorials using Complete Anatomy, a three‐dimensional (3D) e‐anatomy software (3D4Medical Ltd., Dublin, Ireland) as a visual aid. Palpation, auscultation, and percussion exercises were performed alone on the student's own body, if possible. Surface anatomy identification (e.g., “T‐shirt exercise”) and central nervous system wiring exercises were transferred to a virtual template, where students collaborated in drawing on Google's Jamboard application (Google LLC., Mountain View, CA). Peer teachers were given active learning multiple‐choice questions to ask learners throughout sessions to facilitate student engagement. Additionally, the online learning environment was fluid in response to emerging student feedback. As a result, online discussion boards and weekly review sessions were created to allow more interaction with faculty and students from other small groups.
End‐of‐block assessment and evaluation
All students at the CWRU SOM were assessed on their anatomy knowledge at the end of the block in a written assessment. At the start of each block, 25 multi‐part anatomy and radiology essay questions are released. This set of questions is titled Gross Anatomy and Radiology Questions (GARQs). From this set of questions, four are chosen as the end‐of‐block assessment (GARQ assessment). These questions consist of clinical scenarios with a strong basis in anatomy and require an understanding of clinically relevant radiology. Researching the answers for each set of GARQs is self‐directed by students individually, using textbooks and internet sources. Additionally, components of many questions are addressed in the small group sessions described above.
Satisfaction with the curriculum and GARQ assessment were evaluated by an anonymous survey given at the end of Block One before the administration of the written examination. End of block evaluation surveys consists of a variety of questions on other curricular activities, which provide additional evidence of anatomy learning satisfaction. The relevant evaluation survey questions and answer options are shown in Supplemental Material File Table 1. Of note, only two items from the end‐of‐block evaluation for the class of 2023 were of direct relevance to this study. Six items were included on the end‐of‐block evaluation for the class of 2024. An additional item on overall block satisfaction was analyzed for both classes. All items were on a five‐point Likert scale.
Study design
This study used a non‐randomized experimental design with a historical control. De‐identified scores for written GARQ assessment, and both quantitative and qualitative evaluation survey responses were collected for all three classes (2022, 2023, 2024). The class of 2024 comprised the experimental group, which completed Block One anatomy through remote online learning. The class of 2022 and the class of 2023 completed the near‐peer anatomy curriculum of Block One in‐person and serve as historical controls. All three classes were evaluated in Block One anatomy using the same set of questions and associated grading rubric.
Evaluation survey responses from the classes of 2023 and 2024 were used to compare attitudes between in‐person and online NPT, respectively. The survey administered to the class of 2023 was mandatory for 25% of the class, while the survey was mandatory for the entirety of the class of 2024. Both surveys had a 100% response rate, with 46 respondents from the class of 2023, and 183 respondents in the class of 2024.
Case Western Reserve University’s Medical Education Research Committee (MERC) is an IRB‐approved (IRB‐2015‐1105) data registry. Researchers may request de‐identified data from curricular activities. This study received MERC approval on July 8, 2020, through which de‐identified reports of examination scores and survey results were obtained.
Statistical analysis
Inferential tests of group means were selected as a method of analysis for quantitative assessment data. Investigation of descriptive statistics and tests of normality and homogeneity of variance (Shapiro–Wilk and Levene's Test) indicated that assumptions for inferential tests were violated. Students' test scores were significantly positively skewed. Nonparametric comparisons were used to explore the assessment performance for the three cohorts (2022, 2023, and 2024). Kruskal–Wallis nonparametric tests were used to investigate class differences. Given the skewed distribution of data, a sub‐analysis was conducted investigating quartiles and Chi‐Square statistics for quartile distributions. Likert scale evaluation survey results were compared for only the class of 2023 and 2024 using two‐tailed independent samples t‐tests assuming equal variance. Evaluation data were provided in aggregate and therefore must be treated as continuous as opposed to ordinal data. Statistics were performed using SPSS statistical package for Windows, version 27 (IBM Corp., Armonk, NY, USA).
Qualitative data were analyzed using conventional content analysis (Hsieh and Shannon, 2005). Qualitative open coding was conducted by a member of the research team. Each piece of written feedback was read in its entirety, and the topics, sentiments, and suggestions presented by the unique piece of data were recorded using a descriptive open coding method. This process was repeated by a second member of the research team. The open codes were then formalized into a set of categories with descriptions to be used for data analysis by consolidation based on shared or overlapping content by both authors (Washburn et al., 2021). The goal of the analysis was to identify the main topics of concern to students. All data were investigated for emerging themes and topics.
RESULTS
Participants
Class size was comparable across all three cohorts with a small decrease of one student per class, with the class of 2022 being slightly larger (n = 185) than the class of 2023 (n = 184) and 2024 (n = 183). Chi‐square statistics indicated there were no differences in the proportion of male and female students between classes. There were slightly more female students in each class compared to male students (female students in the class of 2022, 51.3%; class of 2023, 51.4%; class of 2024, 58.3%). Differences between student race/ethnicity between classes indicated no difference between the proportion of Non‐Hispanic White students (Range = 39%–43%) or Latino students (range = 3%–4%). There was a significant difference in the increased proportion of Asian (Range = 16%–31%) and Black (Range = 4%–12%) students in the class of 2022 compared to the classes of 2023 and 2024 (χ 2 = 13.19; P = 0.04).
End‐of‐block assessment
Evidence of reliability was comparable across classes with Cronbach's Alpha (α) ranging between 0.70 and 0.78. Comparing cohort performance on the end‐of‐block assessment indicated significantly lower scores for the class of 2024. Mean assessment scores for the classes of 2022, 2023, and 2024 were 93.64% (±5.86), 93.75% (±4.09), and 92.04% (±4.83), respectively. Given the non‐normal distribution of the data, measures of central tendency must also be considered. The median and inter‐quartile range for the classes of 2022, 2023, and 224 were 94.9% (6.8), 94.5 (4.25), and 92.8 (4.8), A Kruskal–Wallis between groups test showed a statistically significant difference between all three cohorts (H(2) = 25.69, P < 0.001). Post hoc group comparisons showed no significant difference between the class of 2022 and 2023 (H(1) = 1.99, P = 0.157). There were significant differences between the class of 2022 and 2024 (H(1) = 18.58, P < 0.001) and 2023 and 2024 (H(1) = 18.65, P < 0.001), with the class of 2024 scoring significantly lower than the two previous classes. Post hoc power analysis indicated a sufficient sample size (β = 0.92). Effect size calculations indicated a small effect (η 2 = 0.034).
Further investigation of class‐level performance using a quartile‐level analysis indicated the class of 2022 scored significantly higher than the classes of 2023 and 2024. There were no significant differences between the classes of 2023 and 2024. The quartile values for the classes of 2022, 2023, and 2024 were: first quartile (i.e., the 25th percentile) 91.2, 92.0, and 92.8; second quartiles (i.e., 50th percentile) 94.9, 94.5, and 92.8; third quartile (i.e., 75th percentile) 98.0, 96.3, 95.3. Quartile distributions were investigated using Chi‐square statistics and standardized residuals. The class of 2024 had a significantly lower number of students in the second quartile and a significantly larger number of students in the third quartile compared to the classes of 2022 and 2023 (Χ2(2) = 16.6; P = 0.002).
End‐of‐block evaluation
Both evaluation surveys reported in this study provided evidence of acceptable reliability (α = 0.6 for the class of 2023; α = 0.8). Mean evaluation survey results concerning the overall quality of the anatomy and radiology curriculum differed significantly between cohorts (Figure 1). On average the class of 2023 rated the curriculum as “very good” in comparison to “average” to “very good” for the class of 2024. An independent samples t‐test showed a statistically significant difference between survey means (t(365) = 2.67, P = 0.008). Comparing student overall satisfaction with Block One (anatomy and radiology, histology, epidemiology, biostatistics, population health, health determinants, health systems sciences, and bioethics combined) between cohorts, there was no statistical with an overall rating of “very good” (3.5/5 for the class of 2023 and 3.7/5 for the class of 2024). Mean evaluation survey results for questions without historical controls are illustrated in Figure 2.
FIGURE 1.
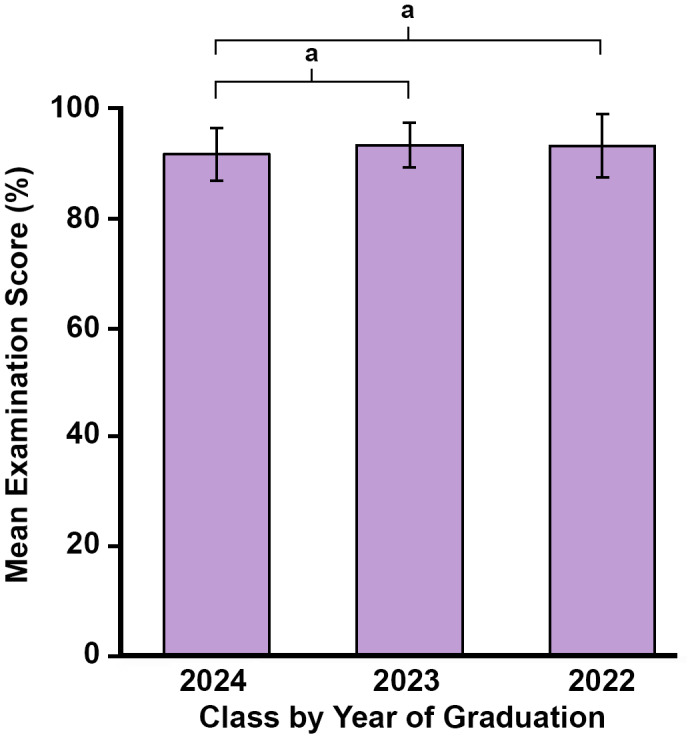
Mean written anatomy examination results (error bars = SD) for medical students from the classes of 2024 (n = 183) with 2023 (n = 184) and 2022 (n = 185); a P < 0.001 using a Kruskal–Wallis test for each comparison, respectively
FIGURE 2.
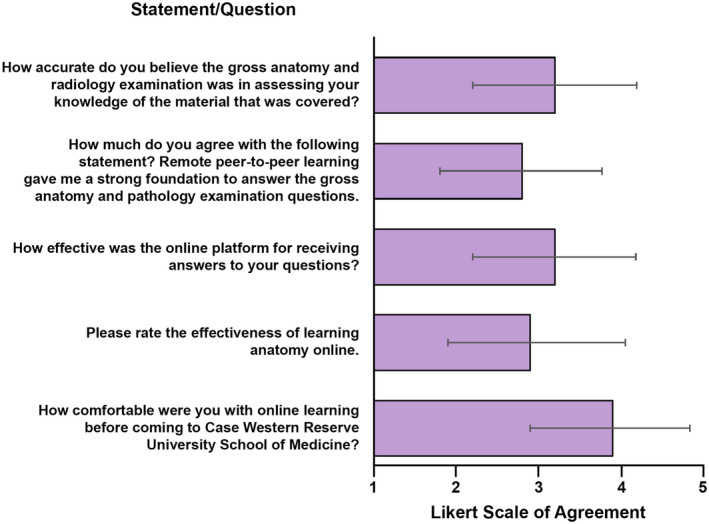
Mean Likert scale survey results (error bars = ±SD) for medical students learning anatomy through near‐peer teaching. Data were obtained using five‐point Likert scale (1 = very inaccurate, strongly disagree, very ineffective, or very uncomfortable and 5 = very accurate, strongly agree, very effective, or very comfortable)
Qualitative written student feedback from the class of 2024 was collected for two optional survey questions. The first question asked for potential improvements to online near‐peer anatomy learning, while the second asked students about the inherent limitations of online near‐peer learning. Of 183 total students, 105 (57.38%) responded to the first survey question, while 92 (50.27%) responded to the second question. The 197 responses were next categorized into five emerging themes (Table 2). Student responses were assigned a total of 231 themes, of which 59 (26.0%) concerned learning modalities, 57 (25.1%) concerned technology limitations, 45 (19.8%) concerned better instruction, 39 (17.2%) concerned curriculum content, and 32 (13.7%) concerned remote communication.
TABLE 2 .
Students' feedback grouped by emerging themes, example quotes, and potentially actionable lessons learned from this feedback
| Emerging theme | Examples | Comments | Lessons learned |
|---|---|---|---|
| Learning modalities | Comments addressing the use of third‐party software, delivery of online content, and/or the ability to research testable questions using available resources. |
|
Prioritize the use of interactive learning exercises |
| Instruction limitations | Comments addressing the quality/preparation of peer‐teachers, and/or faculty interaction |
|
Provide near‐peer teachers with a training module on 3D anatomy software |
| Provide students access to subject matter experts outside of NPT sessions to fill the expertise gap | |||
| Curriculum content | Comments addressing time constraints, session pre‐work, session content, and/or course structure. |
|
Consider incorporating a large group lecture before the NPT session for a narrative overview of learning objectives |
| Remote communication | Comments addressing classmate and faculty interactions, the ability to ask questions, and/or engagement with remote classes |
|
Incorporate frequent, purposeful stops during the NPT session for questions |
| Encourage community building through conversation, and accountability for interacting to generate positive social pressure to be engaged with peers | |||
| Technology Limitations | Comments addressing the inability of technology to replace learning or activities possible in‐person. |
|
Combine high‐quality 2D and 3D images and videos with accompanying descriptive text to make visual aids more cohesive and accessible |
Abbreviations: 2D, two‐dimensional; 3D, three‐dimensional; GARQ, gross anatomy and radiology questions; M2, second‐year medical students; NPT, near‐peer teaching.
DISCUSSION
The present study begins to fill gaps in the literature concerning the viability of remote NPT as an anatomy teaching strategy. Remote NPT was compared to its in‐person equivalent by presenting assessment and quantitative survey data from CWRU SOM students. The authors hypothesized a difference would be found in both student assessment scores and quantitative perceptions of course quality. Further, students from the online cohort shared their perceptions through quantitative survey questions about the transition to online learning in addition to providing qualitative feedback on potential improvements and course limitations. Student written feedback was assimilated into five emerging themes for future recommendations.
The primary objective of this investigation was to evaluate the effectiveness of CWRU SOM's remote near‐peer anatomy curriculum using student GARQ assessment scores. The online translation of the introductory anatomy curriculum showed a significant decrease in student assessment scores relative to prior in‐person cohorts. On average, the online cohort scored 1.65% lower than the classes of 2022 and 2023. While this difference is statistically significant, this statistical significance can be attributed to a robust sample size. An effect size is necessary to understand whether an identified statistically significant difference in group means is trivial or not (Sullivan and Feinn, 2012). The effect size (η 2 = 0.034) for the intervention of moving near‐peer anatomy teaching online is small. This means the magnitude of the experimental effect (i.e., online NPT on assessment scores) was minute. A large sample size, like the one in this study, allows small differences in group means to be detected, despite relatively small effect sizes (Sullivan and Feinn, 2012). Furthermore, the authors conclude a difference of 1.65% in assessment scores for cohorts achieving mean scores above 90% on the assessment does not raise concern for the effectiveness of online near‐peer anatomy teaching.
In order to examine more closely how student performance on the assessment differed between the cohorts, each of the three classes was stratified into quartiles based upon examination scores. Although the class of 2024 collectively was significantly different from the in‐person cohorts, the quartile‐level analysis found no significant differences between the class of 2024 and 2023 in any of the individual quartiles. The students from the online cohort who performed in the lowest quartile, or the 25th percentile, had a quartile value of 92.8. Classes of 2022 and 2023 had first quartile values of 91.0 and 92.0, respectively. This quartile‐level analysis demonstrates that the transition online did not hurt the lowest quartile of students in the class of 2024, which historically has been a concern in transitioning from in‐person to online learning (Beale et al., 2014). This supports that although assessment scores were significantly lower in the class of 2024, the statistically significant difference is not a meaningful difference.
Despite the disruptions to NPT of anatomy during the Covid‐19 pandemic, student assessment scores were not affected in a meaningful way. These results suggest that online NPT of anatomy is comparable to the previous in‐person format. Relative equivalence in student assessment performance after a move to online learning in the anatomical sciences has been observed by other authors (Pinder et al., 2008; Inuwa et al., 2012; Beale et al., 2014; Pei and Wu, 2019; Hillmer et al., 2021). The overall student assessment scores in this study further establish that student assessment performance following online anatomy NPT is as effective as in‐person NPT. Further, a change in assessment scores may not always be meaningful, nor necessary to prevent.
A secondary objective of this study was to collect student perspectives on the effectiveness of online NPT. Ratings of Block One as a whole did not differ between the classes of 2023 and 2024, but students felt the online NPT of anatomy and radiology was significantly less effective than its in‐person equivalent. These results further establish anatomy as a particularly challenging discipline to learn remotely (Longhurst et al., 2020). The authors postulate that the differences in the student perception of effectiveness seen solely within the joint anatomy and radiology curriculum are due in part to increased technological burden on near‐peer teachers. Anatomy is the only part of Block One that relied on hands‐on learning before the Covid‐19 pandemic. For example, the CWRU SOM histology curriculum was taught using virtual microscopic slides, while lecturers in other course content continued to utilize multimedia presentations using Microsoft PowerPoint. Meanwhile, Block One anatomy curriculum requires physical touch with peers and anatomical models in learning the skills of percussion, auscultation, palpation, and the relationships of surface anatomy structures to one another. Therefore, anatomy near‐peer teachers were not only responsible for directing content discussions, but they were also simultaneously responsible for using other learning modalities to facilitate three‐dimensional learning on a two‐dimensional screen. Furthermore, the thematic analysis of student feedback suggests students often perceived their near‐peer teachers to be ill‐prepared for many of their small group sessions. This may be attributable to the aforementioned technological burden on near‐peer anatomy teachers, as the ability to assess student disinterest and frustration, or facilitate interactive learning may have resulted in reduced virtual teaching quality (Co and Chu, 2020; Surkhali and Garbuja, 2020).
After their GARQ assessments, students provided written feedback on curricular improvements and perceived limitations of online NPT. Student feedback provides a particularly useful starting point for future curricular development and refinement in order to make online learning work well for students (Chen et al., 2005; Pinder et al., 2008; Evans et al., 2020; Geraghty et al., 2020). Students are key stakeholders in their own educational resources; as more medical curricula incorporate online learning in the post‐pandemic era, educators should continue to seek student feedback, given the current rapid digital transition (Reyna, 2020). Written feedback concerning limitations of online anatomy NPT and possible course improvements was categorized into five emerging themes (Table 2).
Based on the analysis of qualitative student feedback, the authors suggest the following considerations for adapting online NPT of anatomy: (1) Near‐peer sessions should prioritize the use of interactive‐learning exercises (Pinder et al., 2008; Gadbury‐Amyot et al., 2013; O’Doherty et al., 2018; Singh et al., 2019). (2) Provide near‐peer teachers with a training module on 3D anatomy software prior to the NPT session. (3) Provide students access to subject matter experts outside of NPT sessions to fill the expertise gap. (4) Consider incorporating a large group lecture before the NPT session for the narrative overview of learning objectives. (5) Incorporate frequent, purposeful stops during the NPT session for questions (Dong et al., 2020). (6) Encourage active participation style, community building through conversation, and accountability for interacting to generate positive social pressure to be engaged and connected with peers (Song et al., 2004; Chen et al., 2005; Pinder et al., 2008; Corum et al., 2014; Evans et al., 2020; Roberts et al., 2020). (7) Combine high‐quality two‐dimensional (2D) and 3D images and videos with accompanying descriptive text to make visual aids more cohesive and accessible (O’Doherty et al., 2018). Understanding and addressing these themes in future transitions to online learning may ameliorate differences in student satisfaction compared to in‐person anatomy.
For educators who plan to continue hosting some form of remote anatomy NPT in the post‐pandemic era, it will be necessary to address student concerns about this delivery method. Anatomy educators should be prepared to use whatever innovative methods they have at their disposal in order to push anatomy education forward (Iwanaga et al., 2021). This study has the outlined major areas to focus on for pedagogical improvement and has laid the groundwork for the emergency adaptation of in‐person NPT of anatomy to the online setting. If another pandemic similar to Covid‐19 emerges, this study has established an effective way to transition online without student assessment scores suffering and has outlined areas to improve for a successful future transition. The CWRU SOM plans to resume in‐person NPT of anatomy in the fall of 2021. Based on the lessons learned from student comments, changes will be incorporated into future in‐person curricula to take advantage of and improve from this unique educational inflection point.
Limitations of the study
The results of this study reflect the experience of a single institution and may not be generalized to all medical schools that used NPT in their transition to teaching anatomy remotely. Block One anatomy is the only block at CWRU SOM taught by peer teaching; therefore, this study is limited by the small number of teaching sessions and assessment items in Block One anatomy. Although the assessment scoring rubric was the same for all three cohorts examined in this study, those marking the exams change every year, which may impact quartile‐level score analysis. Some evaluation survey questions were not identical between student cohorts as evaluations are updated annually. The change in survey questions impacted our ability to provide a more in‐depth comparison across cohorts. Additionally, other factors such as faculty remote teaching experience and student stress related to Covid‐19 may have influenced student perceptions. Future studies should allow for comparisons between online and offline anatomy learning environments where NPT is not affected by the aforementioned study design limitations.
CONCLUSIONS
The aim of this study was to validate remote NPT as an online anatomy teaching strategy comparable to previously validated in‐person NPT. In order to identify such strategies, it was critical to evaluate student performance under the online and in‐person conditions included in this study. To the author's knowledge, this is the first study to directly compare the effectiveness and student perceptions of online and in‐person NPT within the same curriculum. The near‐peer anatomy curriculum remained impactful in the move to remote learning. The course design was strong enough to result in no meaningful difference in medical student assessment scores after the transition to online learning; however, a potential drawback remains in reduced student satisfaction and more negative perceptions of course quality. When transitioning to online near‐peer anatomy, medical educators should not be exclusively concerned about a change in the academic success of their students. Educators should also focus considerable attention on continuing to develop online learning environments that adapt to student needs and feedback. The Covid‐19 pandemic has given educators an opportunity to retain the successful practices from this past academic year, but discontinue the failures (Smith and Pawlina, 2021). At this historical inflection point, medical educators should use what has been learned from the trials of the pandemic to bolster positive educational change for the future.
Supporting information
Table S1
Biographies
Mitchell L. Thom, M.Sc., is a third‐year medical student at Case Western Reserve University School of Medicine in Cleveland, Ohio. He is an anatomy TA to first‐ and second‐year medical students. His research interests include orthopedic sports‐related injuries and anatomical education.
Blair A. Kimble, M.A., is a fourth‐year medical student at Case Western Reserve University School of Medicine in Cleveland, Ohio. Her research interests include women's health, clinical ethics, and medical education.
Kelli Qua, Ph.D., is a senior research and evaluation associate in the Office of Curricular Affairs and Assessment at Case Western Reserve University School of Medicine in Cleveland, Ohio. She specializes in educational research and evaluation.
Susanne Wish‐Baratz, Ph.D., M.B.A., is an associate professor of anatomy in the Department of Anatomy at Case Western Reserve University School of Medicine in Cleveland, Ohio. She teaches medical anatomy course and is Director of HoloAnatomy at Case Western Reserve Interactive Commons. Her research interest is in medical education.
Thom ML, Kimble BA, Qua K, Wish‐Baratz S. 2021. Is remote near‐peer anatomy teaching an effective teaching strategy? Lessons learned from the transition to online learning during the Covid‐19 pandemic. Anat Sci Educ, 14: 552–561. 10.1002/ase.2122
Mr. Mitchell L Thom and Ms. Blair A Kimble have contributed equally to this work and share the first authorship.
LITERATURE CITED
- Agius A, Calleja N, Camenzuli C, Sultana R, Pullicino R, Zammit C, Agius JC, Pomara C. 2018. Perceptions of first‐year medical students towards learning anatomy using cadaveric specimens through peer teaching. Anat Sci Educ 11:346–357. [DOI] [PubMed] [Google Scholar]
- Beale EG, Tarwater PM, Lee VH. 2014. A retrospective look at replacing face‐to‐face embryology instruction with online lectures in a human anatomy course. Anat Sci Educ 7:234–241. [DOI] [PubMed] [Google Scholar]
- Benè KL, Bergus G. 2014. When learners become teachers: A review of peer teaching in medical student education. Fam Med 46:783–787. [PubMed] [Google Scholar]
- Blankenburg R, Poitevien P, Gonzalez Del Rey J, Degnon L; Virtual Café Study Team . 2020. Virtual cafes: An innovative way for rapidly disseminating educational best practices and building community during COVID‐19. Acad Pediatr 20:756–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen N, Ko H, Kinshuk *, Lin T. 2005. A model for synchronous learning using the Internet. Innov Educ Teach Int 42:181–194. [Google Scholar]
- Co M, Chu KM. 2020. Distant surgical teaching during COVID‐19 ‐ A pilot study on final year medical students. Surg Pract 24:105–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corum KA, Gadbury‐Amyot CC, Johnson K, Strait TM. 2014. U.S. dental hygiene faculty perceptions of learner outcomes in distance education courses. J Dent Educ 78:530–540. [PubMed] [Google Scholar]
- Cuschieri S, Agius JC. 2020. Spotlight on the shift to remote anatomical teaching during Covid‐19 pandemic: Perspectives and experiences from the University of Malta. Anat Sci Educ 13:671–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickman N, Barash A, Reis S, Karasik D. 2017. Students as anatomy near‐peer teachers: A double‐edged sword for an ancient skill. BMC Med Educ 17:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong C, Lee DW, Aw DC. 2020. Tips for medical educators on how to conduct effective online teaching in times of social distancing. Proc Singap Healthc 2020:2010105820943907. [Google Scholar]
- Estai M, Bunt S. 2016. Best teaching practices in anatomy education: A critical review. Ann Anat 208:151–157. [DOI] [PubMed] [Google Scholar]
- Evans DJ, Bay BH, Wilson TD, Smith CF, Lachman N, Pawlina W. 2020. Going virtual to support anatomy education: A STOPGAP in the midst of the Covid‐19 pandemic. Anat Sci Educ 13:279–283. [DOI] [PubMed] [Google Scholar]
- Evans DJ, Cuffe T. 2009. Near‐peer teaching in anatomy: An approach for deeper learning. Anat Sci Educ 2:227–233. [DOI] [PubMed] [Google Scholar]
- Franchi T. 2020. The impact of the Covid‐19 pandemic on current anatomy education and future careers: A student’s perspective. Anat Sci Educ 13:312–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadbury‐Amyot CC, Singh AH, Overman PR. 2013. Teaching with technology: Learning outcomes for a combined dental and dental hygiene online hybrid oral histology course. J Dent Educ 77:732–743. [PubMed] [Google Scholar]
- George PP, Papachristou N, Belisario JM, Wang W, Wark PA, Cotic Z, Rasmussen K, Sluiter R, Riboli‐Sasco E, Tudor Car L, Musulanov EM, Molina JA, Heng BH, Zhang Y, Wheeler EL, Al Shorbaji N, Majeed A, Car J. 2014. Online eLearning for undergraduates in health professions: A systematic review of the impact on knowledge, skills, attitudes and satisfaction. J Glob Health 4:010406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geraghty JR, Young AN, Berkel TDM, Wallbruch E, Mann J, Park YS, Hirshfield LE, Hyderi A. 2020. Empowering medical students as agents of curricular change: A value‐added approach to student engagement in medical education. Perspect Med Educ 9:60–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampshire K, Phinney L, McCarthy EE, Schwartz B, Chin‐Hong P, Chin‐Hong P. 2020. 1127. Medical school in the era of COVID‐19: Innovations in direct near peer teaching of immunology/microbiology content during the pandemic. Open Forum Infect Dis 7:S593. [Google Scholar]
- Hilburg R, Patel N, Ambruso S, Biewald MA, Farouk SS. 2020. Medical education during the Coronavirus disease‐2019 pandemic: Learning from a distance. Adv Chronic Kidney Dis 27:412–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillmer R, Krippendorf B, Patitucci T. 2021. Comparison of student performance following in‐person or virtual gross anatomy labs during COVID‐19. FASEB J 35:S1.0379 7. [Google Scholar]
- Hsieh HF, Shannon SE. 2005. Three approaches to qualitative content analysis. Qual Health Res 15:1277–1288. [DOI] [PubMed] [Google Scholar]
- Inuwa IM, Taranikanti V, Al‐Rawahy M, Habbal O. 2012. Anatomy practical examinations: How does student performance on computerized evaluation compare with the traditional format? Anat Sci Educ 5:27–32. [DOI] [PubMed] [Google Scholar]
- Iwanaga J, Loukas M, Dumont AS, Tubbs RS. 2021. A review of anatomy education during and after the COVID‐19 pandemic: Revisiting traditional and modern methods to achieve future innovation. Clin Anat 34:108–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson E, Holmin TE, Johansson BR, Braide M. 2018. Improving near‐peer teaching quality in anatomy by educating teaching assistants: An example from Sweden. Anat Sci Educ 11:403–409. [DOI] [PubMed] [Google Scholar]
- Kiene J, Lasek R, Wish‐Baratz S, Freeman B. 2009. Peer teachers introducing anatomy to first year medical students. FASEB J 23:S1.LB3. [Google Scholar]
- Longhurst GJ, Stone DM, Dulohery K, Scully D, Campbell T, Smith CF. 2020. Strength, weakness, opportunity, threat (SWOT) analysis of the adaptations to anatomical education in the United Kingdom and Republic of Ireland in response to the Covid‐19 pandemic. Anat Sci Educ 13:301–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malau‐Aduli BS, Alele FO, Heggarty P, Teague PA, Sen Gupta T, Hays R. 2019. Perceived clinical relevance and retention of basic sciences across the medical education continuum. Adv Physiol Educ 43:293–299. [DOI] [PubMed] [Google Scholar]
- Martin F, Bolliger DU. 2018. Engagement matters: Student perceptions on the importance of engagement strategies in the online learning environment. Online Learn 22:205–222. [Google Scholar]
- O’Doherty D, Dromey M, Lougheed J, Hannigan A, Last J, McGrath D. 2018. Barriers and solutions to online learning in medical education – An integrative review. BMC Med Educ 18:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pather N, Blyth P, Chapman JA, Dayal MR, Flack NA, Fogg QA, Green RA, Hulme AK, Johnson IP, Meyer AJ, Morley JW, Shortland PJ, Štrkalj G, Štrkalj M, Valter K, Webb AL, Woodley SJ, Lazarus MD. 2020. Forced disruption of anatomy education in Australia and New Zealand: An acute response to the Covid‐19 pandemic. Anat Sci Educ 13:284–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pei L, Wu H. 2019. Does online learning work better than offline learning in undergraduate medical education? A systematic review and meta‐analysis. Med Educ Online 24:1666538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinder KE, Ford JC, Ovalle WK. 2008. A new paradigm for teaching histology laboratories in Canada’s first distributed medical school. Anat Sci Educ 1:95–101. [DOI] [PubMed] [Google Scholar]
- Reyna J. 2020. Twelve Tips for COVID‐19 friendly learning design in medical education. MedEdPublish 9:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts V, Malone K, Moore P, Russell‐Webster T, Caulfield R. 2020. Peer teaching medical students during a pandemic. Med Educ Online 25:1772014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose S. 2020. Medical student education in the time of COVID‐19. JAMA 323:2131–2132. [DOI] [PubMed] [Google Scholar]
- Singh K, Bharatha A, Sa B, Adams OP, Majumder MdA. 2019. Teaching anatomy using an active and engaging learning strategy. BMC Med Educ 19:149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith CF, Pawlina W. 2021. A journey like no other: Anatomy 2020! Anat Sci Educ 14:5–7. [DOI] [PubMed] [Google Scholar]
- Song L, Singleton ES, Hill JR, Koh MH. 2004. Improving online learning: Student perceptions of useful and challenging characteristics. Internet High Educ 7:59–70. [Google Scholar]
- Stigmar M. 2016. Peer‐to‐peer teaching in higher education: A critical literature review. Mentor Tutor 24:124–136. [Google Scholar]
- Sullivan GM, Feinn R. 2012. Using effect size—Or why the p value is not enough. J Grad Med Educ 4:279–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surkhali B, Garbuja CK. 2020. Virtual learning during COVID‐19 pandemic: Pros and cons. J Lumbini Med Coll 8:154–155. [Google Scholar]
- Topping KJ. 1996. The effectiveness of peer tutoring in further and higher education: A typology and review of the literature. High Educ 32:321–345. [Google Scholar]
- Uddin A, Laurent E, Hussain S, Toi T, Seraj S, Hadjittofi C, Niaz O, Haque S. 2020. PP27 the virtual near‐peer teaching programme successes are comparable with traditional classroom teaching; A junior doctor perspective. BMJ Simul Technol Enhanc Learn S6:A28. [Google Scholar]
- Washburn M, Zhou S, Sampson M, Palmer A. 2021. A pilot study of peer‐to‐peer SBIRT simulation as a clinical telehealth training tool during COVID‐19. Clin Soc Work J (in press; doi: 10.1007/s10615-021-00799-8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wayne DB, Green M, Neilson EG. 2020. Medical education in the time of COVID‐19. Sci Adv 6:eabc7110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcha RJ. 2020. Effectiveness of virtual medical teaching during the COVID‐19 crisis: Systematic review. JMIR Med Educ 6:e20963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wish‐Baratz S, Gubatina AP, Enterline R, Griswold MA. 2019. A new supplement to gross anatomy dissection: HoloAnatomy. Med Educ 53:522–523. [DOI] [PubMed] [Google Scholar]
- Yu TC, Wilson NC, Singh PP, Lemanu DP, Hawken SJ, Hill AG. 2011. Medical students‐as‐teachers: A systematic review of peer‐assisted teaching during medical school. Adv Med Educ Pract 2:157–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1


