Dear Editor
1.
The spike (S) protein is a homotrimer on the SARS‐CoV‐2 surface which targets the angiotensin‐converting enzyme‐2 in humans (ACE2). The Spike (S) coronavirus 2 (SARS‐CoV‐2) protein is a major driving force for viral infectivity and antigenicity. Several mutations of the SARS‐CoV‐2 spike protein have been found and their effects are explored in the evasion of the immune system and increased transmission due to increased disease and death. Spike (S) proteins are of key interest to scientists from pathogenic and epidemiological points of view. In the new study, the tyrosine‐protein kinase receptor UFO (AXL) was found to bind specifically to SARS‐CoV‐2 Spike (S) protein. AXL overexpression facilitated viral entrance to the same extent that ACE2 overexpression did in HEK293T cells (Human embryonic kidney cells).
AXL inhibition, but not ACE2 inhibition, dramatically decreased SARS‐CoV‐2 infection of lung cells. In cells producing high amounts of AXL, soluble human recombinant AXL but not ACE2 inhibited SARS‐CoV‐2 infection. Taken together, these findings imply that AXL is a unique host receptor that interacts with the N‐terminal domain (NTD) of SARS‐CoV‐2 Spike (S), facilitating the virus's entrance into human cells.1 Since the antibody‐mediated protection depends on the target antigen structure, any mutation causing the target antigen's productive conformational shift may reduce its binding effect and degrade its protective function.2, 3 This study examined how mutations in the NTD of Spike (S) proteins result in a decrease in the effectiveness of neutralizing antibodies in vaccinated individuals.
Various versions of SARS‐CoV‐2 have shown increased concern for accelerated transmission and viral fatality and lowered the effectiveness of vaccination protection since the onset of the second wave of COVID‐19 infection.4, 5 Recent research has revealed that Spike (S) protein variants from six continents have been documented in Asia, Africa, Europe, Oceania, South America, and North America.6
After 1 year of extension of the global spread of SARS‐CoV‐2 in the UK, South Africa, Brazil, United States (California), and in some other countries, improved transmissibility and antibody resistance were observed. Since the beginning of 2021, the appearance of a new lineage called B.1.617 has also caused an increase in instances. The three principal sublineages, B.1.617.1 (Kappa), B.1.617.2 (Delta), and B.1.617.3 are contained in this report. These non‐RBD antibodies are quite widespread and may account for more than 80% of the anti‐Spike IgG response, even though 90% of neutralizing activity is directed against the RBD.7, 8 The changes in NTD include deletion and substitution of a tiny percentage of the amino acid sequences at certain positions in spike proteins in SARS CoV‐2 virus.9, 10, 11 Furthermore, according to recent research, certain therapeutic monoclonal antibodies, including Bamlavinimab, have stopped binding to the mutant Spike proteins and hence are no longer neutralizing B.1.617.2. Thus, before administering therapeutic mAbs in persons at risk for severe forms of COVID‐19 it is important to identify a virus strain in patients. This study indicated further that B.1.617.2 is less susceptible to sera than those with natural immunity.12 Thus, considering the nature and biological consequences of the novel SARS‐CoV‐2 variants induced by various Spike (S) protein NTD mutations, many single Spike (S) variations in SARS‐CoV‐2 undoubtedly are a disturbing occurrence including linked to antiantibody evasion.13
Antiviral immunity also relies on adaptive cellular immunity, with the antiviral effectors being cytotoxic CD8+ T lymphocytes that identify infected cells expressing viral proteins rather than antibodies. In contrast to antibodies, viral proteins are identified as protein fragments (peptides) associated with major histocompatibility complexes and T cell receptors. Recent investigations demonstrate that the present mutant versions of SARS‐CoV‐2 have a negligible effect on T cell‐based immunity, which may compensate for the crippling effect these mutations may have on parallel humoral response.14, 15 In addition, CD8+ T lymphocytes specific for the SARS‐CoV‐2 spike glycoprotein were not found in the previous study of peripheral blood from nonvaccinated or two‐dose‐vaccinated donors. However, many immunocompromised individuals, immunodeficient individuals, or individuals with a disease that suppresses immunity, such as those receiving chemotherapy or immunotherapy, may not generate adequate cellular immunity against SARS‐CoV‐2 following vaccination (Figure 1).
Figure 1.
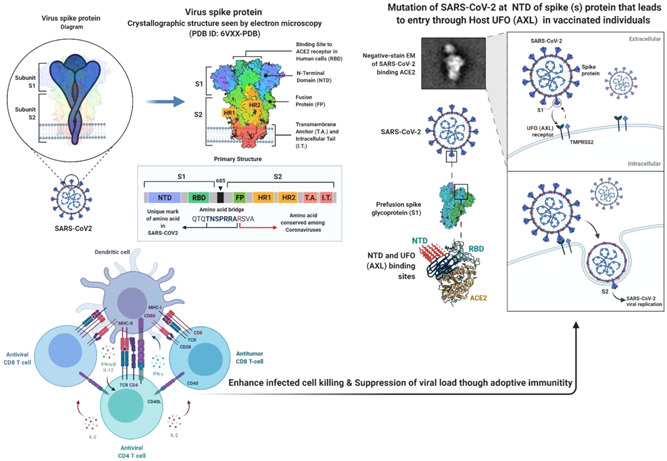
N‐terminal domain of SARS CoV‐2 Spike (S) protein mutation associated reduction in effectivity of neutralizing antibody with vaccinated individuals and SARS‐CoV‐2‐reactive T cell‐based adoptive cellular immunotherapy of COVID‐19 infection
These above findings conclude that the combination of COVID‐19 vaccination and SARS‐CoV‐2‐reactive T cells may be a potent tool for developing T cell‐based adoptive cellular immunotherapy of COVID‐19 in the NTD of SARS CoV‐2 Spike (S) protein mutation associated with a decrease in neutralizing antibody effectivity in vaccinated individuals.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Yogendra Singh, Neeraj Kumar Fuloria, and Shivkanya Fuloria gave the initial idea and participated in drafted manuscript. Vetriselvan Subramaniyan Dhanalekshmi and Unnikrishnan Meenakshi participated in all the sections of the manuscript development. Srikumar Chakravarthi, Usha Kumari, and Navneet Joshi participated in all the sections of the manuscript development and technical comments. Gaurav Gupta finalized the manuscript for publication. All authors read and approved the final version of manuscript.
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
REFERENCES
- 1.Wang S, Qiu Z, Hou Y, et al. AXL is a candidate receptor for SARS‐CoV‐2 that promotes infection of pulmonary and bronchial epithelial cells. Cell Res. 2021;31(2):126‐140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kwarteng A, Asiedu E, Sylverken AA, Larbi A, Sakyi SA, Asiedu SO. Molecular characterization of interactions between the D614G variant of SARS‐CoV‐2 S‐protein and neutralizing antibodies: A computational approach. Infect Genet Evol. 2021;91:104815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Q, Wu J, Nie J, et al. The impact of mutations in SARS‐CoV‐2 spike on viral infectivity and antigenicity. Cell. 2020;182(5):1284‐1294.e1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ke Z, Oton J, Qu K, et al. Structures and distributions of SARS‐CoV‐2 spike proteins on intact virions. Nature. 2020;588(7838):498‐502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hodcroft EB, Domman DB, Snyder DJ, et al. Emergence in late 2020 of multiple lineages of SARS‐CoV‐2 Spike protein variants affecting amino acid position 677. medRxiv. 2021;2021. 10.1101/2021.02.12.21251658 [DOI] [Google Scholar]
- 6.Hassan SS, Lundstrom K, Choudhury PP, et al. Implications derived from S‐protein variants of SARS‐CoV‐2 from six continents. bioRxiv2021. 2021.9(3):243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andreano E, Rappuoli R. SARS‐CoV‐2 escaped natural immunity, raising questions about vaccines and therapies. Nature Med. 2021;27(5):759‐761. [DOI] [PubMed] [Google Scholar]
- 8.Chi X, Yan R, Zhang J, et al. A neutralizing human antibody binds to the N‐terminal domain of the Spike protein of SARS‐CoV‐2. Science. 2020;369(6504):650‐655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Voss WN, Hou YJ, Johnson NV, et al. Prevalent, protective, and convergent IgG recognition of SARS‐CoV‐2 non‐RBD spike epitopes in COVID‐19 convalescent plasma. bioRxiv. 2020;372(6546):1108–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCallum M, De Marco A, Lempp FA, et al. N‐terminal domain antigenic mapping reveals a site of vulnerability for SARS‐CoV‐2. Cell. 2021;184(9):2332‐2347.e2316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Plante JA, Mitchell BM, Plante KS, Debbink K, Weaver SC, Menachery VD. The variant gambit: COVID‐19's next move. Cell Host Microbe. 2021;29(4):508‐515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Planas D, Veyer D, Baidaliuk A, et al. Reduced sensitivity of infectious SARS‐CoV‐2 variant B.1.617.2 to monoclonal antibodies and sera from convalescent and vaccinated individuals. bioRxiv. 2021;2021. 10.1101/2021.05.26.445838 [DOI] [Google Scholar]
- 13.Dearlove B, Lewitus E, Bai H, et al. A SARS‐CoV‐2 vaccine candidate would likely match all currently circulating variants. Proceedings of the National Academy of Sciences. 2020;117(38):23652‐23662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tarke A, Sidney J, Methot N, et al. Negligible impact of SARS‐CoV‐2 variants on CD4 (+) and CD8 (+) T cell reactivity in COVID‐19 exposed donors and vaccinees. bioRxiv. 2021 10.1101/2021.02.27 [DOI] [Google Scholar]
- 15.Rosendahl Huber S, Van Beek J, De Jonge J, Luytjes W, Van Baarle D. T cell responses to viral infections—opportunities for peptide vaccination. Front Immunol. 2014;5:171. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.


