Abstract
Background
There is accumulating evidence about detrimental impacts of the pandemic on population mental health, but knowledge on risk of groups specifically affected by the pandemic and variations across time is still limited.
Methods
We surveyed approximately n=1,000 Austrian residents in 12 waves between April and December 2020 (n=12,029). Outcomes were suicidal ideation (Beck Suicidal Ideation Scale), depressive symptoms (Patient Health Questionnaire-9), anxiety (Hospital Anxiety Depression Scale), and domestic violence. We also assessed the perceived burden from the pandemic. Demographic and Covid-19 specific occupational and morbidity-related variables were used to explain outcomes in multivariable regression analyses, controlling for well-established risk factors of mental ill-health, and variations over time were analyzed.
Results
Young age, working in healthcare or from home, and own Covid-19 illness were consistent risk factors controlling for a wide range of known mental health risk factors. Time patterns in the perceived burden from Covid-19-related measures were consistent with the time sequence of restrictions and relaxations of governmental measures. Depressive and anxiety symptoms were relatively stable over time, with some increase of depression during the second phase of lockdowns. Domestic violence increased immediately after both hard lockdowns. Suicidal ideation decreased slightly over time, with a low during the second hard lockdown. Mental health indicators for women and young people showed some deterioration over time, whereas those reporting own Covid-19 illness improved.
Limitations
Data from before the pandemic were not available.
Conclusions
Among mental health outcomes, increases in domestic violence and, to some smaller extent, depressive symptoms, appeared most closely related to the timing of hard lockdowns. Healthcare staff, individuals working from home, those with Covid-19, as well as young people and women are non-traditional risk groups who warrant heightened attention in prevention during and in the aftermath of the pandemic.
Keywords: Covid-19, Pandemic, Mental health, Survey, Austria
1. Introduction
With many countries now being in a prolonged situation of tightening and relaxing wide-ranging measures to curb the Covid-19 pandemic, its impact on population mental health has become an increasing concern (Gunnell et al., 2020; Holmes et al., 2020; United Nations, 2020; WHO, 2020). Studies suggest that particularly adolescents and young adults (Czeisler et al., 2020; O’Connor et al., 2021; Pieh et al., 2020; Pierce et al., 2020; Ueda et al., 2020; Xiong et al., 2020), individuals with pre-existing mental disorders (Czeisler et al., 2020; Vindegaard and Benros, 2020; Winkler et al., 2020; Xiong et al., 2020; Pan et al., 2021), and medical personnel working at the frontlines to treat patients (Kreh et al., 2020; Vindegaard and Benros, 2020) experience strong mental health challenges during the pandemic.
In spite of the accumulating evidence of the detrimental impact of the pandemic on mental health, there are still large gaps in the literature. Particularly, there is currently little information from multivariable models about socio-demographic, occupational, economic, and health-related characteristics in the population that are independently associated with mental health outcomes. Risk groups for mental-ill health during the pandemic appear to include traditional risk groups such as individuals with low income (Pieh et al., 2020) or with mental disorders (Pan et al., 2021), but also new risk groups such as healthcare staff (Kreh et al., 2020) or parents of young children (Pierce et al., 2020). These risk profiles might also differ between various mental health outcomes. Many of the available studies have investigated depressive symptoms and anxiety (O’Connor et al., 2021; Pieh et al., 2020; Ueda et al., 2020; Wang et al., 2020; Winkler et al., 2020), but less is known about other important outcomes such as suicidal ideation (Czeisler et al., 2020; O’Connor et al., 2021; Winkler et al., 2020) or domestic violence. Regarding domestic violence, there have been concerns raised about possible detrimental impact of the pandemic. More people staying at home, including in cramped conditions might act as a possible contributor to household stress, and potentially, interpersonal violence (Feder et al, 2020; Roesch et al, 2020).
Furthermore, it remains unknown if and how population mental health responds and varies with the current epidemic situation, where periods of lockdowns are followed by relaxations and further lockdowns. Studies have reported higher rates of depressive symptoms and anxiety during phases of strict physical distancing (Marroquína et al., 2020; O’Connor et al., 2021), which has resulted in calls to avoid hard lockdowns. The available studies, however, typically have not assessed whether mental health outcomes bounced back toward baseline after the end of lockdown periods, remained elevated, or increased independent of hard lockdowns.
In the present study, we present data from a repeated cross-sectional survey in the Austrian population that is representative of age, gender, education, and region of residence. We assessed depressive symptoms, anxiety, suicidal ideation, and domestic violence, as well as the perceived burden on life in various areas of life at twelve equally-spaced times across the pandemic. The aim of the study was
-
1.
to identify specific risk factors particularly related to household size and composition, Covid-19 morbidity and occupational risk of Covid-19 exposure, controlling for a range of well-established risk factors for mental-ill health;
-
2.
to investigate overall changes in mental health outcomes over the course of the pandemic; as well as time trends among various demographic groups; those affected by Covid-19 illness; and among occupational risk groups.
1.1. Overview of the pandemic course in Austria
Austria was one of the first countries in middle Europe to implement a first hard lockdown with severe restrictions on movement and far-reaching closures of shops and restaurants in March 2020. This first lockdown lasted until late April 2020 (including wave #1 of the present survey) (Desvars-Larrive et al., 2020). Afterwards, a period of lower incidence of registered Covid-19 cases and relaxed measures followed (waves #2 to #9). In fall 2020, the epidemic situation deteriorated and a soft lockdown was implemented from November 3 to 16 (wave #10 of the survey). Measures were later tightened to a second hard lockdown which was in place from November 17 to December 6 (wave #11). This lockdown was perceived as less effective than the first, and resulted only in minor relaxations during the last survey phase (wave #12).
2. Methods
2.1. Study design, setting, and participant recruitment
Between April 23 and December 22, 2020, we conducted a repeated cross-sectional online quota survey in 12 waves (i.e., every three weeks). For each wave, a new sample of approximately 1,000 participants representative of the Austrian population of 16 years and older in terms of gender, age, education, and region of residence was recruited. Recruitment was done by Ipsos, a marketing company. A quota sampling methodology based on population statistics from Statistics Austria was employed with quotas based on gender (i.e., male, female, diverse), age (i.e., 16-29, 30-39, 40-49, 50-59, 60-69, 70+), region (i.e., all nine federal states), and education (i.e., compulsory, upper secondary with “Matura” – a final exam which is required for attending university–, or university education). In addition, the dataset for each wave was weighted to achieve representativeness across combinations of all four variables, e.g., age interlocked with gender.
For each wave, members of the online panel, which included 30,000 registered members, were invited by email to take part in an online survey on Covid-19 and mental health. Invitations were sent out based on the open quotas and individual response probabilities estimated by the panel algorithm. In total, 78,936 invitations were sent to panel members (i.e., 6,578 invitations per wave), and 19,361 invitations were accepted. Participants were able to participate in the survey numerous times, but only once per wave. Informed consent was obtained from 18,942 participants. N=5,339 participants were screened out because quotas were already fulfilled and n=1,574 participants dropped out before completing the survey. Drop-outs did not considerably vary across waves, with a mean drop-out rate of 11.6%, ranging from 8.2% to 14.4%, without any trend in drop-outs over time.
Participants who met the required quotas completed a range of self-report measures of various psychological and social measures. At the end of the survey, they received contact information of organizations offering help in mental health crises. The study was approved by the Research Ethics Board of the Medical University of Vienna (study protocol 1391/2020, April 23, 2020) and pre-registered at aspredicted.org (#52796).
2.2. Variables
2.2.1. Demographic, socio-economic, and morbidity-related data
In addition to gender, age, region of residence and education, we also collected the following socio-demographic and morbidity measures: occupational status, household net per capita income (calculated as the net household income divided by the square root of household members, see Keeley, 2015), and pre-existing mental and somatic illness. In addition, we collected data on household size, presence of school-aged children in household, occupational risk of Covid-19 exposure, and self-reported Covid-19 illness in participants and others in their household and family (see Table 1 for the categories of each variable).
Table 1.
Socio-demographic and morbidity-related characteristics as well as mental health outcomes of participants across all twelve survey waves (n=12,029).
| Characteristic | Total waves 1-12, not weighted, n (%) | Total waves 1-12, weighted, n (%) |
|---|---|---|
| Gender | ||
| Male | 5,861 (48.7) | 5,814 (48.3) |
| Female | 6,144 (51.1) | 6,191 (51.5) |
| Diverse | 24 (0.2) | 24 (0.2) |
| Age group | ||
| 16-29 | 2,402 (20.0) | 2,493 (20.7) |
| 30-39 | 1,939 (16.1) | 1,879 (15.6) |
| 40-49 | 1,916 (15.9) | 2,358 (19.6) |
| 50-59 | 2,230 (18.5) | 1,944 (16.2) |
| 60-69 | 1,630 (13.6) | 1,501 (12.5) |
| 70+ | 1,912 (15.9) | 1,854 (15.4) |
| Occupational status | ||
| Employed | 5,412 (45.0) | 5,540 (46.1) |
| Unemployed | 1,206 (10.0) | 1,198 (10.0) |
| Retired | 3,579 (29.8) | 3,403 (28.3) |
| Homemaker | 279 (2.3) | 287 (2.4) |
| Attending school / university | 856 (7.1) | 890 (7.4) |
| Disability pension | 127 (1.1) | 127 (1.1) |
| Civil servants | 15 (0.1) | 16 (0.1) |
| Parental leave | 277 (2.3) | 284 (2.4) |
| Other | 278 (2.3) | 286 (2.4) |
| Education | ||
| Below upper secondary (Matura) | 8,988 (74.7) | 8,961 (74.5) |
| Secondary education | 1,673 (13.9) | 1,650 (13.7) |
| University | 1,368 (11.4) | 1,417 (11.8) |
| Household net per capita income (in Euro) | ||
| <500 | 550 (4.6) | 571 (4.7) |
| 501-1000 | 1,231 (10.2) | 1,256 (10.4) |
| 1001-<1500 | 3,473 (28.9) | 3,511 (29.2) |
| 1501-<2000 | 3,348 (27.8) | 3,330 (27.7) |
| 2001-<2500 | 2,586 (21.5) | 2,549 (21.2) |
| >2500 | 841 (7.0) | 814 (6.8) |
| Number of household members | ||
| 1 | 2,990 (24.9) | 2,956 (24.6) |
| 2 | 4,741 (39.4) | 4,630 (38.5) |
| 3 | 2,017 (16.8) | 2,046 (17.0) |
| 4 | 1,571 (13.1) | 1,644 (13.7) |
| >4 | 710 (5.9) | 753 (6.3) |
| Civil status | ||
| Single | 3,802 (31.6) | 3,875 (32.2) |
| Partnered | 2,533 (21.1) | 2,561 (21.3) |
| Married | 4,658 (38.7) | 4,598 (38.2) |
| Widowed | 387 (3.2) | 367 (3.1) |
| Divorced | 649 (5.4) | 628 (5.2) |
| School-aged children | 2,266 (18.8) | 2,388 (19.8) |
| Pre-existing mental health problems | 1,748 (14.5) | 1,762 (14.6) |
| Pre-existing somatic disorder | 3,810 (31.7) | 3,757 (31.2) |
| Occupational risk, Covid-19 exposure | ||
| Yes but not right now (e.g., working from home) | 615 (5.1) | 627 (5.2) |
| Yes, healthcare | 701 (5.8) | 719 (6.0) |
| Yes, not healthcare | 1,507 (12.5) | 1,537 (12.8) |
| No | 9,206 (76.5) | 9,147 (76.0) |
| Own Covid-19 illness | 163 (1.4) | 162 (1.3) |
| Covid-illness others in household | 252 (2.1) | 255 (2.1) |
| Covid-illness family not in household | 816 (6.8) | 824 (6.8) |
| Suicidal ideation | 828 (6.9) | 838 (7.0) |
| Depressive Symptoms | 2,579 (21.4) | 2,617 (21.8) |
| Anxiety | 2,816 (23.4) | 2,851 (23.7) |
| Domestic violence | 2,220 (18.5) | 2,273 (18.9) |
Values are presented as frequencies with percentages given in parentheses.
2.2.2. Current burden from restrictions in various domains of life
In order to assess perceptions of the amount of burden from the pandemic and restrictions, participants were asked to quantify the burden they perceived to be currently present from the pandemic and related measures. Participants rated six areas of their lives (i.e., family life, professional affairs, school/university life, social life, cultural life, consumption and shopping) on a 4-point scale ranging from 1 (no problems/restrictions) to 4 (very big problems/restrictions), with another option to indicate that the specific area was not relevant to them.
2.2.3. Suicidal ideation
Suicidal ideation was assessed with the short form of the Beck Scale for Suicidal Ideation, consisting of five items according to the intensity of suicidal ideation rated on a 3-point scale from 0 to 2 (Beck and Steer, 1993). The scale consists of five screening items, which capture suicidal ideation in the past week. Three items assess the wish to live and the wish to die and two items assess the desire to attempt suicide (i.e., ratings capture the wish to live; wish to die; reasons for living/dying; desire to make an active suicide attempt; and passive suicide desire). Participants with scores >0 were considered to be potentially suicidal (Brown, 2000).
2.2.4. Depressive symptoms
Depressive symptoms in the past two weeks were assessed with the PHQ-9 (Patient Health Questionnaire) consisting of nine items rating depressive symptoms in the last two weeks on a scale from 0 (not at all) to 3 (nearly every day) (Kroenke et al., 2001). Participants with scores >9 were considered to have moderate or high levels of depressive symptoms (Manea et al., 2012).
2.2.5. Anxiety
Anxiety in the past week was assessed with the anxiety subscale of the Hospital Anxiety and Depression Scale (HADS). The scale consists of seven items rating the severity of anxiety from 0 to 3 (Zigmond and Snaith, 1983). Participants with scores of ≥8 were considered to have moderate/high levels of anxiety (Olsson et al., 2005). The scale has frequently been used in general population surveys.
2.2.6. Domestic violence
Domestic violence experienced in the past two weeks was measured with two items (“Did you experience any (A) psychological/ (B) physical violence by your partner or any other family member in the last two weeks?” followed by a brief definition of psychological and physical violence). Participants rated their experience on a 5-point scale from 1 (not at all) to 5 (very much). Participants with scores >1 on any of these scales were considered to have experienced domestic violence.
2.2.7. Changes in suicidal ideation, anxiety, and interpersonal conflicts compared to before Covid-19
Participants rated the frequency and amount of their current suicidal ideation, anxiety, and interpersonal conflicts as compared to before the pandemic on a scale from 1 (much smaller or much less frequent) to 5 (much greater or much more frequent). For suicidal ideation, there was also one category stating “I have no suicidal ideation”. Scores >3 were considered to indicate an increase in suicidal ideation, anxiety, and conflicts, respectively.
2.3. Statistical analysis
In order to identify associations between socio-demographic, economic, occupational and morbidity-related variables and mental health outcomes (i.e., suicidal ideation, depressive symptoms, anxiety, domestic violence, as well as perceived changes in suicidal ideation, anxiety, and interpersonal conflicts compared to before Covid-19) we used crude and multivariable binary logistic regression analyses (the latter controlling for all other assessed variables). All analyses were additionally controlled for wave number (i.e., time) by including a dummy variable for each wave. Each of the mental health outcomes was dichotomized according to the respective cut-off values, and the results are presented as odds ratios (ORs) with 95% confidence intervals. Frequencies, percentages, and regression models were weighted by the quota sampling weights. Confidence intervals were not adjusted for multiple testing and should be interpreted as exploratory.
We performed a sensitivity analysis to assess whether patterns differed if only participants who completed not more than two survey waves across the entire survey period were included. The analysis revealed very similar patterns to the reported findings (not shown).
We calculated changes over time (i.e., with wave number) for perceptions of the amount of burden in the different areas of life and for mental health outcomes. Mental health outcomes were used as quantitative variables in these analyses, and means for each wave were compared to wave #1 (the phase of hard lockdown) with independent sample t-tests (Welch's t-tests). Curve fitting was used to assess any changes of mental health outcomes over time for genders and age groups, groups at occupational risk of exposure to Covid-19, as well as those reporting own (present or past) Covid-19 morbidity.
IBM SPSS version 26 was used for all analyses. Visualizations were done with Julia (juliaplots.org) and R.
3. Results
3.1. Participant characteristics
Table 1 presents an overview of weighted and unweighted participant characteristics. Overall, differences between weighted and unweighted data were minimal. A total of n=12,029 participants (range per wave: 1,000-1,007) completed the survey across the 12 waves. On average, participants took part 1.43 times across the twelve waves. N=7,792 (64.8%) participated only one time, n=3,849 (32.0%) two times, n=193 (1.6%) three times, and n=195 (1.6%) more than three times.
Over the course of the pandemic, n=838 (7.0%) of participants scored above the cut-off for possible suicidal ideation; n=2,617 (21.8%) for moderate to severe depression; n=2,851 (23.7%) for potentially clinically relevant anxiety; and n=2,273 (18.9%) for experiences of any degree of domestic violence.
3.2. Mental health outcomes across waves by socio-demographic characteristics and morbidity
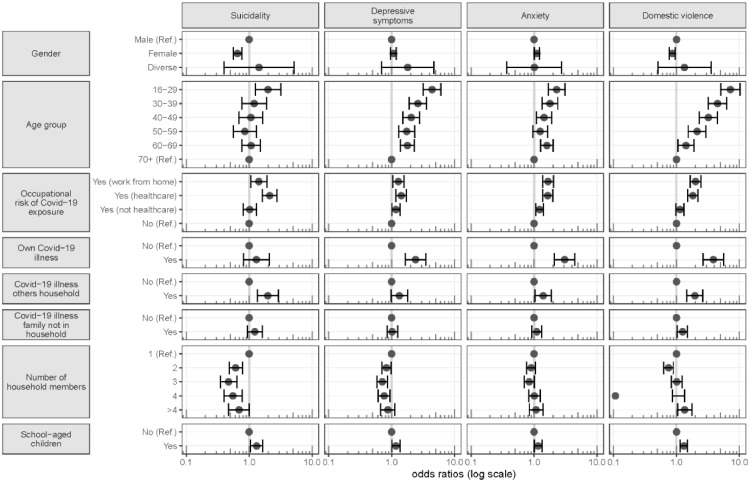
Fig. 1 shows adjusted odds ratios of suicidal ideation, depressive symptoms, anxiety and domestic violence for demographic groups, household size and composition, occupational risk groups, and Covid-19 morbidity of participants and their families. These associations are adjusted for all variables listed in Table 1 as well as wave number.
Fig. 1.
Adjusted odds ratios of demographic groups, occupational and Covid-19 morbidity-related risk factors for suicidal ideation, depressive symptoms, anxiety, and domestic violence. These estimates are adjusted for all other variables presented in this figure and additionally for wave number and for any of those additionally presented in Table 1.
A full overview presenting adjusted odds ratios for all variables assessed is provided in Supplemental Fig. 1 (appendix). The specific odds ratios along with 95% confidence intervals are provided in Supplemental Tables 1 (crude estimates) and 2 (adjusted for all other variables and wave number), see appendix.
3.3. Suicidal ideation
Controlling for a wide range of socio-economic and morbidity-related risk factors of mental ill-health, participants of 16 to 29 years (OR: 1.99), those with occupational exposure to Covid-19 in healthcare settings (OR: 2.11), and participants with family members with Covid-19 illness among household members (OR: 1.98) all had moderately increased odds of suicidal ideation as compared to the respective reference group. To a smaller degree, also individuals working from home (OR: 1.42) and participants with school-aged children in the household (OR: 1.31) had higher odds of suicidal ideation as compared to the respective reference group. Females (OR: 0.65) as well as members of larger households (e.g., >4 household members, OR: 0.69) had lower odds of suicidal ideation as compared to males and 1-person households, respectively.
3.4. Depressive symptoms
There was a large-sized association of young age of 16 to 29 years with depressive symptoms (OR: 4.38), which gradually decreased for older age groups. A smaller, but still moderate-sized odds ratio was present for individuals reporting own Covid-19 illness (OR: 2.40), as compared to the respective reference group. To some lesser extent, having school-aged children (OR: 1.17), working in healthcare (OR: 1.42), having some risk of exposure to Covid-19 outside of healthcare (1.17), and working from home (OR: 1.28) were factors with increased odds of depressive symptoms as compared to having no occupational risk.
3.5. Anxiety
Patterns for anxiety were generally similar to those of depressive symptoms. The odds ratio of anxiety was large for participants who reported own Covid-10 illness (OR: 3.06). Young age of 16 to 29 (OR: 2.28) as compared to age of 70 years and older was moderately associated with anxiety.
3.6. Domestic violence
A clear dose-response relationship emerged for age, with participants in the youngest age group of 16 to 29 showing very large odds of 7.21 as compared to participants of 70 years and older. The odds remained strongly increased for the group of 30 to 39 year olds (OR: 4.50), and there was still a large association up to the age of 49 (OR: 3.21). The second-largest increase in odds after younger people was seen for participants who reported own Covid-19 illness (OR: 3.85). Smaller increases were present if others in the household had Covid-19 (OR: 1.96) and when family members outside the own household were affected (OR: 1.25). Members of large households of more than four participants reported slightly increased odds of domestic violence (1.35) as compared to one-person households. Participants working from home during the pandemic (OR: 2.01), those with school-aged children (OR: 1.31) and participants working in healthcare (OR: 1.82) also had increased odds of domestic violence as compared to the respective reference group.
3.7. Perceived changes as compared to before Covid-19
We assessed this outcome for suicidal ideation, anxiety, and interpersonal conflicts in order to get an impression of who perceived their mental health to have changed compared to before the onset of the pandemic.
As shown in Table 2 with regard to suicidal ideation, particularly young people up to 29 years (OR: 2.60), those with own Covid-19 illness (OR: 2.18) as well as participants with pre-existing mental health problems (OR: 1.81) reported an increase in suicidal ideation. Odds were also increased for individuals with below higher secondary education (Matura), OR: 1.61.
Table 2.
Multivariable associations between socio-demographic and morbidity-related characteristics and changes in suicidality, anxiety and perceived interpersonal conflicts compared to before Covid-19 across all waves.
| Suicidality changed to worse | Anxiety changed to worse | Conflict changed to worse | |
|---|---|---|---|
| Gender | |||
| Male | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Female | 1.08 (0.85, 1.38) | 1.11 (0.99, 1.24) | 1.27 (1.16, 1.39) |
| Diverse | 0.72 (0.09, 6.01) | 1.70 (0.63, 4.58) | 3.07 (1.32, 7.14) |
| Age group | |||
| 16-29 | 2.60 (1.11, 6.09) | 1.80 (1.28, 2.54) | 1.80 (1.36, 2.38) |
| 30-39 | 2.10 (0.92, 4.81) | 1.56 (1.12, 2.17) | 1.81 (1.38, 2.36) |
| 40-49 | 1.57 (0.70, 3.53) | 1.58 (1.15, 2.16) | 1.75 (1.36, 2.26) |
| 50-59 | 1.15 (0.51, 2.56) | 1.34 (0.99, 1.81) | 1.59 (1.24, 2.04) |
| 60-69 | 1.79 (0.92, 3.46) | 1.34 (1.04, 1.71) | 1.40 (1.15, 1.72) |
| 70+ | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Education | |||
| Below upper secondary (Matura) | 1.12 (0.77, 1.65) | 0.63 (0.54, 0.74) | 0.71 (0.62, 0.82) |
| Secondary | 1.61 (1.04, 2.49) | 0.86 (0.70, 1.05) | 0.84 (0.71, 0.99) |
| University | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Occupational status | |||
| Employed | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Unemployed | 1.37 (0.97, 1.93) | 1.12 (0.93, 1.35) | 1.11 (0.94, 1.29) |
| Retired | 0.80 (0.45, 1.41) | 0.89 (0.69, 1.14) | 0.81 (0.66, 0.99) |
| Homemaker | 1.38 (0.66, 2.87) | 0.77 (0.52, 1.14) | 0.73 (0.54, 0.99) |
| Attending school / university | 0.99 (0.65, 1.51) | 1.40 (1.11, 1.77) | 1.29 (1.06, 1.57) |
| Disability pension | 1.63 (0.81, 3.26) | 1.43 (0.94, 2.18) | 0.83 (0.55, 1.25) |
| Civil servants | 0.82 (0.09, 7.25) | 0.43 (0.06, 3.23) | 1.26 (0.43, 3.74) |
| Parental leave | 1.97 (0.91, 4.30) | 1.07 (0.75, 1.53) | 1.30 (0.99, 1.72) |
| Other | 0.92 (0.43, 1.96) | 1.03 (0.73, 1.44) | 1.35 (1.04, 1.76) |
| Household per capita income (in Euro) | |||
| <500 | 1.38 (0.64, 2.97) | 1.38 (0.95, 2.01) | 1.46 (1.09, 1.95) |
| 500 until 1000 | 1.20 (0.60, 2.40) | 1.84 (1.33, 2.54) | 1.31 (1.01, 1.68) |
| 1000 until 1500 | 0.85 (0.45, 1.61) | 1.47 (1.11, 1.96) | 1.29 (1.04, 1.61) |
| 1500 until 2000 | 0.84 (0.45, 1.57) | 1.48 (1.12, 1.95) | 1.32 (1.07, 1.63) |
| 2000 until 2500 | 0.87 (0.46, 1.64) | 1.23 (0.92, 1.63) | 1.14 (0.92, 1.41) |
| More than 2500 | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Number of household members | |||
| 1 | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| 2 | 0.95 (0.66, 1.38) | 1.07 (0.89, 1.28) | 0.99 (0.86, 1.15) |
| 3 | 0.50 (0.32, 0.78) | 0.80 (0.64, 0.99) | 0.83 (0.69, 0.99) |
| 4 | 0.90 (0.55, 1.47) | 1.16 (0.91, 1.47) | 1.12 (0.92, 1.36) |
| >4 | 0.75 (0.43, 1.31) | 1.03 (0.76, 1.38) | 1.01 (0.79, 1.29) |
| Civil status | |||
| Single | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Partnered | 0.85 (0.61, 1.17) | 1.00 (0.85, 1.17) | 1.06 (0.93, 1.20) |
| Married | 0.95 (0.65, 1.40) | 0.87 (0.73, 1.04) | 0.84 (0.73,0.98) |
| Widowed | 1.93 (0.85, 4.41) | 1.53 (1.08, 2.16) | 1.06 (0.79, 1.43) |
| Divorced | 1.06 (0.57, 2.01) | 0.86 (0.65, 1.13) | 1.08 (0.87, 1.33) |
| School-aged children | |||
| Yes | 1.22 (0.87, 1.71) | 1.20 (1.02, 1.41) | 1.10 (0.96, 1.25) |
| No | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Pre-existing mental health problems | |||
| Yes | 1.81 (1.42, 2.32) | 2.75 (2.41, 3.13) | 1.73 (1.54, 1.95) |
| No | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Pre-existing somatic morbidity | |||
| Yes | 1.22 (0.95, 1.57) | 1.57 (1.39, 1.77) | 1.25 (1.13, 1.38) |
| No | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Occupational risk, Covid-19 exposure | |||
| Yes but not right now (e.g., home office) | 1.29 (0.87, 1.90) | 1.19 (0.95, 1.49) | 1.39 (1.15, 1.67) |
| Yes, healthcare | 1.03 (0.68, 1.55) | 1.00 (0.80, 1.26) | 1.55 (1.30, 1.83) |
| Yes, not healthcare | 0.96 (0.67, 1.37) | 1.21 (1.03, 1.42) | 1.29 (1.13, 1.47) |
| No | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Own Covid-19 illness | |||
| Yes | 2.18 (1.34, 3.54) | 1.52 (1.03, 2.26) | 0.97 (0.68, 1.39) |
| No | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Covid-19 illness others household | |||
| Yes | 1.17 (0.71, 1.94) | 0.85 (0.59, 1.22) | 1.18 (0.89, 1.58) |
| No | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Covid-19 illness family not in household | |||
| Yes | 1.23 (0.82, 1.83) | 1.11 (0.91, 1.35) | 1.01 (0.86, 1.20) |
| No | 1 (Ref) | 1 (Ref) | 1 (Ref) |
Values are odds ratios with 95% confidence intervals given in parentheses estimated with multivariable binary logistic regression analyses. Models are adjusted for wave number and all other variables in the table.
Regarding anxiety, particularly participants with pre-existing mental health problems (OR: 2.75), young people (16-29 years: OR: 1.80), those with low income (500 to 1,000 Euro (OR: 1.84)), and participants with pre-existing somatic morbidity (OR: 1.57) and attending school/university (OR: 1.40) indicated an increase in symptoms of anxiety as compared to before the pandemic. Also individuals reporting own Covid-illness and widowed participants were at higher odds of reporting a deterioration (OR: 1.52 and 1.53, respectively).
Regarding conflicts, gender-diverse individuals (OR: 3.07), young people (e.g., up to 29 years: OR: 1.80), individuals with pre-existing mental health problems (OR: 1.73), those working in healthcare (OR: 1.55), in other occupations with risk of Covid-19 exposure (OR: 1.29), or working from home (OR: 1.39) had higher odds of reporting a deterioration as compared to before Covid-19.
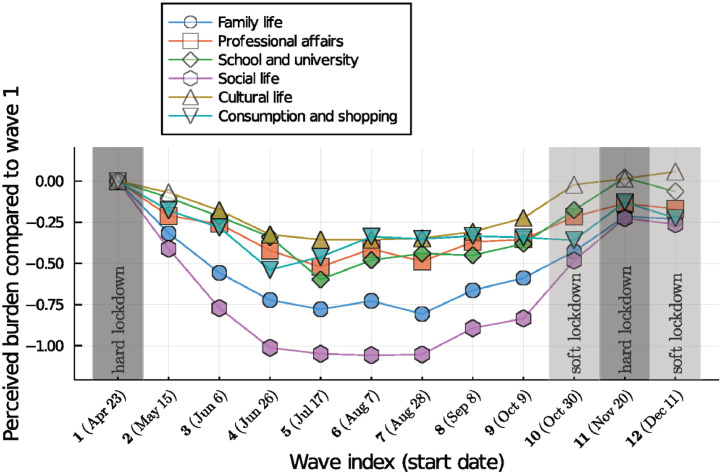
3.8. Perceived burden in different areas of life over time
The perceived burden in specific areas of life showed a characteristic pattern across the pandemic (Fig. 2 ). These are shown for family life; social life; professional affairs; school and university, cultural life, and consumption and shopping. Means and standard deviations are provided in Supplemental Table 3B (appendix).
Fig. 2.
Perceived burden in different areas of life over time. Values indicate changes in means for perception of the current burden from restrictions in each area of life relative to values at wave #1. Coloured time points indicate significant differences in means from wave #1 as estimated with independent sample t-tests.
The perceived burden from Covid-19 and related measures in different areas of life was clearly most pronounced during and shortly after the first lockdown, then gradually decreased for family and social life over the summer (a period of relaxed restrictions), and then increased again toward the second hard lockdown. A similar decrease in the perceived burden for the summer/vacation months was also visible for professional and school/university life. The greatest burden overall was perceived in the areas of social and cultural life, with burden from cultural restrictions showing the smallest decrease during the summer. The largest changes over time were seen for burdens related to social life; followed by family life; school and university life; professional affairs; consumption/shopping; and cultural life (see Fig. 2).
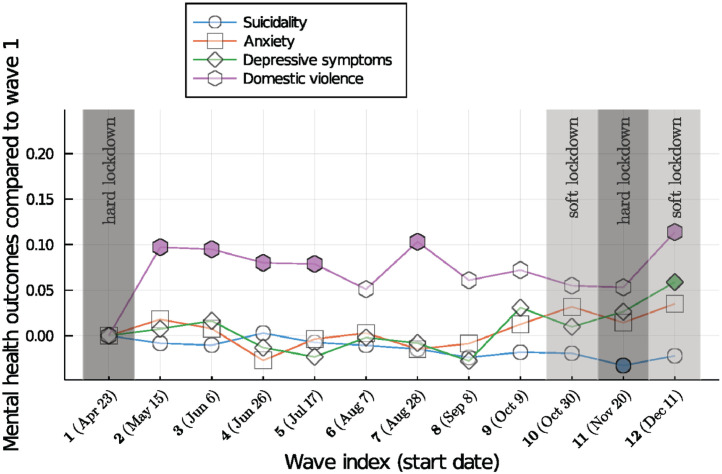
3.9. Mental health outcomes over time
Suicidal ideation, depressive symptoms, anxiety and domestic violence showed distinct patterns over time (see Fig. 3 ). Means and standard deviations are provided in Supplemental Table 3A (see appendix). In general, variations across time were less pronounced than for the perceptions of burden in various areas of life. Compared to wave #1, the first hard lockdown, the strongest changes were present for domestic violence, whereas depressive symptoms, anxiety and suicidal ideation showed only small and non-significant changes across most (for anxiety, all) of the subsequent waves.
Fig. 3.
Mental health outcomes over time. Values indicate changes in means for mental health outcomes relative to values at wave #1. Coloured time points indicate significant differences in means from wave #1 as estimated with independent sample t-tests.
Domestic violence showed an immediate increase after the first lockdown phase in March 2020 and remained elevated afterwards. A second increase was seen immediately after the second hard lockdown. Depressive symptoms did not change significantly during the pandemic summer and autumn until shortly before the second hard lockdown. A similar pattern was present for anxiety. Suicidal ideation showed a slight downward trend across the pandemic months with a low that was significantly different from wave #1 (the first hard lockdown) during the second hard lockdown (Fig. 3).
3.10. Gender patterns over time
Formal interaction tests using product terms (wave*gender) in the models did not reveal any significant interactions with regard to the dichotomous mental health outcomes. Using the continuous measures, there was a linear increasing trend of depressive symptoms for females (but not males), F (1, 6188.8) = 9.09, p = 0.003, mean squares (MSe) = 3.91; and anxiety F (1, 6188.8) = 4.43, p = 0.035, MSe = 1.54; as well as some decrease in suicidal ideation F (1, 6188.8) = 4.43, p = 0.035, MSe = 0.44, which was also present for males F (1, 5812.3) = 4.26, p = 0.039, MSe = 0.37.
3.11. Patterns for age groups over time
Formal interaction tests did using product terms (wave*age group) in the models did not reveal any significant interactions with regard to the dichotomous mental health outcomes. Using the continuous measures, participants of young age 16-29, but also of 30-39 years experienced an increase in depressive symptoms F (1, 2583.2) = 16.57, p <0.0001, MSe = 7.20, 30-39 years: F (1, 1871.6) = 6.08, p = 0.014, MSe= 2.48. Anxiety increased in 16-29 year olds, but not in other age groups, F (1, 2483.2) = 10.09, p = 0.002, MSe = 3.19. Suicidal ideation decreased in the age groups 40-49 and 50-59 (40–49 years, F (1, 2351.4) = 9.83, p=0.002, MSe= 0.89, 50-59 years, F (1, 1940.1) = 9.64, p = 0.003, MSe= 0.60). There was an increase in domestic violence in participants of 70 years and older, which was close to statistical significance (F (1, 1848.1) = 3.54, p = 0.060, MSe = 0.56).
3.12. Patterns for occupational groups over time
Formal interaction tests using product terms (wave*occupational group) did not reveal any significant interactions with regard to the dichotomous mental health outcomes. Using the continuous measures, for healthcare staff and others with possible exposure to Covid-19, there was a linear increase in depressive symptoms over time, healthcare: F (1, 715.7) = 3.97, p = 0.047, MSe = 1.45, others: F (1, 1526.7) = 11.47, p < 0.01, MSe = 4.40. The latter group also reported an increased in anxiety F (1, 1526.7) = 6.78, p = 0.547, MSe = 2.19. Groups at no occupational risk reported a decrease in suicidal ideation over time F (1, 9130.9) = 12.02, p = 0.001, MSe = 1.05.
3.13. Patterns for those reporting own Covid-19 illness
Formal interaction tests did using product terms (wave*own Covid-19 illness) drevealed significant interactions with regard to depressive symptoms (p=0.003), anxiety (p=0.002), and domestic violence (p=0.002) with regard to the dichotomous mental health outcomes. Using the continuous measures, participants reporting own Covid-19 illness reported a decrease in depressive symptoms, (F (1, 159.5) = 11.81, p = 0.001, MSe = 5.05), anxiety (F (1, 159.5) = 14.7, p < 0.0001, MSe = 4.97), suicidal ideation (F (1, 159.5) = 28.91, p < 0.0001, MSe= 4.67), and domestic violence F (1, 159.5) = 17.25, p < 0.001, MSe = 28.19. Means and SDs for the outcomes for each of the groups analysed are presented in Supplemental Tables 4–7 for suicidal ideation, depressive symptoms, anxiety, and domestic violence.
4. Discussion
This multi-wave cross-sectional survey study provides evidence about population groups most affected by mental ill-health across the first 9 months of the Covid-19 pandemic. Beside well-established markers of mental ill health such as low socio-economic status and mental illness, young age, occupational factors such as working in healthcare or home-office as well as own Covid-19 illness were the most consistent risk factors across mental health outcomes. Regarding domestic violence, also factors that are related to where people spend most of the day were clearly associated with an increased risk: Living in large households, living with others who had Covid-19 in a household, or working from home all had independent and moderate associations with domestic violence. These findings highlight new risk factors that appear quite specific to the current situation have emerged during the pandemic and warrant attention from public health and prevention in addition to those groups with well-established risk of mental ill-health.
A group that has been reported to experience negative mental health outcomes from the current pandemic in several population studies are young individuals. The present findings of a nearly 4.5-fold likelihood of moderately to severe depression symptoms and even a 7-fold odds of domestic violence in participants up to 29 years of age compared to the oldest segment of the population highlight the urgency of action to provide mental health support for young people. This is further corroborated by the observation that depressive symptoms as well as anxiety increased further during the course of the pandemic. Findings from before the Covid-19 pandemic already suggested increased mental distress in young people, and the current findings likely reflect both accumulating distress from the pandemic, but also broader pre-existing generational problems that existed already before the pandemic (Wagner et al., 2017; Twenge et al., 2019; Elmer et al., 2020).
With regard to the reporting of own Covid-19 illness, we found a more than 2-fold likelihood of anxiety at a level of clinical concern and a more than 3-fold odds of domestic violence for those who reported Covid-19 illness. Additional data surveyed during some waves indicated that about half (47.1%) of those reporting own Covid-19 illness had a positive test result. These data suggest that this group included individuals who had Covid-19, but also others who were strongly concerned about having it without any further verification. International reports indicate that a considerably larger proportion of the population believe they had Covid-19 than registered cases suggest (Boggs, 2020). Previous studies have shown that worries about Covid-19 per se were a risk factor for mental ill-health (Winkler et al., 2020). Emerging evidence further suggests that Covid-19 illness is associated with an increased incidence of new psychiatric disorders (Taquet et al., 2021), which might also partly explain some of the observed risk in that group. The present findings, however, also highlight that for participants reporting own Covid-19 illness, mental health has somewhat improved over the course of the pandemic. In the course of the pandemic, with increasing numbers of individuals having Covid-19 and recovering from it, the stigma of having or worries about having had Covid-19 might have decreased over time. Mental health impacts later on in the pandemic for those worried about own Covid-19 might have become somewhat less severe as compared to the early phase of the pandemic when there was only very little secure information about the course of illness and treatment options.
With regard to occupational risk, we found that working in healthcare, but, to a smaller extent also working from home because of Covid-19 were associated with mental ill-health. Large workloads, perceived helplessness, and anxiety from becoming infected or transmitting the disease to others are likely important risk factors for those working in healthcare settings (Kreh et al., 2020; Vindegaard and Benros, 2020; Giorgi et al., 2020). Particularly for healthcare staff, mental health showed a deteriorating trend of depressive symptoms over the course of the observation period, highlighting the accumulated mental and physical distress in this group over time. The same pattern was present for those working outside healthcare with some risk of occupational exposure, which includes individuals working in sale.
Working from home might be related to difficulties in satisfying both family and job-related duties and appeared to be most closely related to the risk of domestic violence. Long periods of physical closeness to family members might contribute to this association, and might also partly explain the observed associations for persons in multi-person households, married participants, and participants with school-aged children. Of note, pupils were in home-schooling for about 40-60% of the school period in the year 2020 since the start of the pandemic in Austria. An increased risk of mental ill-health in parents with young children was also reported in survey studies from the United Kingdom (Pierce et al., 2020) and the United States (Czeisler et al., 2020).
With regard to variations in mental health indicators over time, the present study highlights that the perceived burden in various areas of life was quite consistent with the course of the pandemic and the timing of restrictions and relaxations of measures. The burden from restrictions in social and family life showed the greatest variation across time, consistent with the strong effect of measures during hard lockdowns and their relaxation during the summer months of 2020 on the ability to meet others in person. In contrast, shopping and cultural venues remained more strongly affected by the pandemic measures even during periods of relaxations, and the present analysis indicated the smallest variations of perceived burdens over time in these areas of life. In contrast to perceptions of burdens in various areas of life, suicidal ideation, depressive symptoms, anxiety and domestic violence, did not appear to directly respond to changes in the epidemic situation or measures. Anxiety and depressive symptoms were at high levels already at the beginning of the pandemic. A representative survey from 2014 using the PHQ-8 (instead of PHQ-9 which we have used) reported a prevalence of depressive symptoms of only 4% (Statistik Austria, 2015). The estimate of moderate to severe depressive symtoms affecting 22% of the population identified across the 9-months period under investigation is consistent with the 21% estimate from another Austrian survey conducted during the first lockdown (Pieh et al., 2020). Depressive symptoms and anxiety showed little variations after the first hard lockdown during a period of relaxations, but there was some further increase in depressive symptoms during a late period of further lockdowns. This finding appears to corroborate the hypothesis that strong social distancing has a cumulative negative effect on mental health, and it might point to some mental exhaustion in the population that materialized after the summer when the school year started again and the pandemic situation got worse.
With regard to domestic violence, a different pattern emerged that appeared to be more directly related to phases of hard lockdowns. There was a clear increase in reported violence immediately after the first lockdown, and the risk remained elevated for several subsequent months. A second possible increase was seen immediately after the second hard lockdown. Prolonged physical closeness between victims and perpetrators of domestic violence at times of movement restrictions might result in subsequent increases in domestic violence. These findings are consistent with anecdotal mass media reports about more family violence and high demands for women shelter after the first lockdown in Austria (Vienna, 2020).
Yet another time pattern emerged for suicidal ideation over time, which appeared to show a slightly declining trend over time, with lowest values during the second hard lockdown. Divergences between findings for suicidal ideation and other mental health indicators have also been reported in a UK study, although that study used a shorter time frame with three time points of assessments only (O’Connor et al., 2021). The present findings are generally consistent with reports about suicides in Austria and internationally, which either reported a decrease or no change in suicides in the first phase of the pandemic, including the first lockdown, across 16 high income countries and regions (Pirkis et al., 2021; Niederkrotenthaler et al., 2020; Deisenhammer and Kemmler, 2021). In the light of the high prevalence of depressive symptoms, anxiety, and domestic violence, which are all risk factors for suicidal ideation and behaviour, continuing surveillance of suicide risk appears highly warranted (Pirkis et al., 2021; Niederkrotenthaler et al., 2020; Deisenhammer and Kemmler, 2021).
As noted, some trends in mental health outcomes were present for specific population groups over the course of the pandemic. Beside young people, those in healthcare or in other occupational settings with possible Covid-19 exposure, women experienced an increase in depressive symptoms and anxiety over time during the pandemic. Studies have highlighted the burden from the current double strain on women based on their traditional family roles and work responsibilities (Takaku and Yokoyama, 2020). Some research further suggests that the pandemic has reinforced these traditional gender roles (Yamamura and Tsustsui, 2021), and females have been shown to be more affected by unemployment during the pandemic in Austria (Bock-Schappelwein and Hyll, 2020) and elsewhere (Ueda et al., 2020).
A possible increase close to the boundary of statistical significance was also seen for the oldest segment of the population of 70 years and older with regard to domestic violence. Severe and prolonged restrictions in movement for this group, particularly among residents of elderly homes, might have contributed to deteriorations over time (Calleja-Agius and Calleja, 2021).
4.1. Strengths and limitations
A strength of the present study is the repeated assessment in different national representative samples, which allows for a comprehensive identification of risk groups across the first nine months of the pandemic. The sample size was large and the study sample reflected the overall population composition well, as indicated by the consistency of weighted with unweighted samples. Limitations of the present study are the focus on self-report data, which might result in recall bias, particularly regarding questions on changes in mental health as compared to before Covid-19. We do not have data from before the outbreak, limiting the ability to compare the data with earlier points in time. Further, although new samples were drawn for each of the twelve waves of the survey, some participants took part more than once, which might result in some bias in estimates. We conducted a sensitivity analysis that excluded any participants who participated more than twice to check if there were any discrepancies in patterns found. Although the patterns were very similar, we cannot rule out some residual bias from clustering in repeat measures from the same individuals. Another limitation is that we cannot rule out that some of the observed fluctuations might be related to known seasonal variations in mood. Seasonal depression is particularly prevalent in fall and winter months (Kurlansik and Ibay, 2012). Finally, the associations identified have not been controlled for multiple testing. This approach appears justified, because all tests were exploratory only. The exploratory nature of this analysis, however, needs to be kept in mind when interpreting the present findings.
5. Conclusion
Risk groups for mental-ill health during Covid-19 include well-recognized groups, but also groups that are strongly and specifically affected by the pandemic. Young people, groups with some occupational risk of Covid-19 exposure, and those affected by Covid-19 morbidity are important target groups for mental health support. Markers of mental health changed differently over time and, in contrast to perceived burden from restrictions in different areas of life, did not generally appear to immediately respond to relaxations of measures. Among the outcomes assessed in this study, domestic violence appeared to be most closely related to periods of hard lockdowns with prolonged physical closeness between family members. Depressive symptoms appeared to have accumulated over time as further hard lockdowns were implemented. Although mental ill-health is a risk factor for suicidal ideation and behaviour, there were no signs of increasing suicidal ideation during the investigated period of analysis, consistent with Austrian and international data on suicides. The present findings highlight that risk factors are at a high level and further screening and prolonged mental health support is needed for both well-recognized and new risk groups for mental ill-health.
Funding
This study has been funded by the Vienna Science and Technology Fund (WWTF) through project COV20-027 (PI: TN). DG further acknowledges funding from the Vienna Science and Technology Fund through the project “Emotional Well-Being in the Digital Society” (Grant No. VRG16-005). MB is funded by the Austrian Science Fund (FWF; grant number: KLI627-B30). SK is funded by the Austrian Science Fund (FWF; grant number: P30918-B27). The funder did not have any involvement in the study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Ethical standards
Ethical approval for this study was obtained from the Ethical Review Board of the Medical University of Vienna (protocol number 1391/2020, April 24 2020). All participants provided informed consent online. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2013.
Availability of data and materials
Selected data from this study can be obtained from the authors upon reasonable request after the completion of ongoing work with this dataset.
CRediT authorship contribution statement
T. Niederkrotenthaler: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Supervision, Visualization, Writing – original draft. Z. Laido: Formal analysis, Validation, Writing – original draft. S. Kirchner: Conceptualization, Writing – review & editing. M. Braun: Conceptualization, Data curation, Writing – review & editing. H. Metzler: Conceptualization, Writing – review & editing. T. Waldhör: Formal analysis, Software, Writing – review & editing. M.J. Strauss: Visualization, Writing – review & editing. D. Garcia: Conceptualization, Methodology, Writing – review & editing. B. Till: Conceptualization, Data curation, Investigation, Methodology, Project administration, Writing – original draft.
Declaration of Competing Interest
None.
Acknowledgement
None.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.08.153.
Appendix. Supplementary materials
References
- Beck A.T., Steer R.A. Psychological Corporation; San Antonio, TX: 1993. Beck Scale for Suicidal Ideation: Manual. [Google Scholar]
- Boggs, J., 2020. Poll finds 1 in 10 Americans think they have been infected with Covid-19, The Denver Channel, 24 April. (larly). Accessed 22 February 2021.
- Brown, G.K., 2000. A review of suicide assessment measures for intervention research with adults and older adults. ( https://www.sprc.org/sites/default/files/migrate/library/BrownReviewAssessmentMeasuresAdultsOlderAdults.pdf ). Accessed 22 February 2021.
- Bock-Schappelwein J., Hyll W. WIFO Research Brief 09/2020. Österreichisches Institut für Wirtschaftsforschung; Wien: 2020. Covid-19-Pandemie: Beschäftigungssituation für Frauen schwieriger. [Google Scholar]
- Calleja-Agius J., Calleja N. Domestic violence among the elderly during the Covid-19 pandemic. Violencia doméstica entre los ancianos durante la pandemia Covid-19. Rev. Esp. Geriatr. Gerontol. 2021;56:64. doi: 10.1016/j.regg.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.E., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Nijai R., Weaver M.D., Robbins R., Facer-Childs E.R.F., Barger L.K., Czeisler C.A., Howard M.E., Rajaratnam S.M.W. Mental health, substance use, and suicidal ideation during the Covid-19 Pandemic — United States, June 24–30, 2020. Morbid. Mortal. Week. Rep. 2020;69(32):1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deisenhammer E.A., Kemmler G. Decreased suicide numbers during the first 6 months of the Covid-19 pandemic. Psychiatry Res. 2021;295 doi: 10.1016/j.psychres.2020.113623. [DOI] [PubMed] [Google Scholar]
- Desvars-Larrive A., Dervic E., Haug N., Niederkrotenthaler T., Chen J., Di Natale A., Lasser J., Gliga D.S., Roux A., Sorger J., Chakraborty A., Ten A., Dervic A., Pacheco A., Jurczak A., Cserjan D., Lederhilger D., Bulska D., Berishaj D., Thames E.F., Álvarez F.S., Takriti H., Korbel J., Reddish J., Grzymala-Moszczynska J., Stangl J., Hadziavdic L., Stoeger L., Gooriah L., Geyrhofer L., Ferreira M.R., Bartoszek M., Vierlinger R., Holder S., Haberfellner S., Ahne V., Reisch V., Servedio V.D.P., Chen X., Pocasangre-Orellana X.M., Garncarek Z., Garcia D., Thurner S. A structured open dataset of government interventions in response to Covid-19. Sci. Data. 2020;7(1):285. doi: 10.1038/s41597-020-00609-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elmer T., Mepham K., Stadtfeld C. Students under lockdown: comparisons of students’ social networks and mental health before and during the Covid-19 crisis in Switzerland. PLoS ONE. 2020;15(7) doi: 10.1371/journal.pone.0236337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feder G., d'Oliveira A.F.L., Rishal P., Johnson M. Domestic violence during the pandemic. BMJ. 2020;372:n722. doi: 10.1136/bmj.n722. [DOI] [PubMed] [Google Scholar]
- Giorgi G., Lecca L.I., Alessio F., Finstad G.L., Bondanini G., Lulli L.G., Arcangeli G., Mucci N. Covid-19 related mental health effects in the workplace: a narrative review. Int. J. Environ. Res. Public Health. 2020;17(21):7857. doi: 10.3390/ijerph17217857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnell D., Appleby L., Arensman E., Hawton K., John A., Kapur N., Khan M., O'Connor R., Pirkis J. Covid-19 Suicide Prevention Research Collaboration, 2020. Suicide risk and prevention during the Covid-19 pandemic. Lancet Psychiatry. 2020;7(6):468–471. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R., Perry V.H., Tracey I.T., Wessely S., Arseneault L., Ballard C., Christensen H., Silver R.C., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the Covid-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keeley B. Income Inequality: the Gap between Rich and Poor. OECD Publishing; Paris: 2015. What are income and wealth? [Google Scholar]
- Kreh, A., Brancaleoni, R., Magalini, S.C., Chieffo, D.P.R., Flad, B., Ellebrecht, N., Juen, B., 2020. Ethical and psychosocial considerations for hospital personnel in the Covid-19 crisis: moral injury and resilience. MedRXiv, doi.org/10.1101/2020.11.18.20232272. [DOI] [PMC free article] [PubMed]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: validity of a brief depression severity measure. J. Gen. Inter. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurlansik S.L., Ibay A.D. Seasonal affective disorder. Am. Fam. Physician. 2012;86(11):1037–1041. [PubMed] [Google Scholar]
- Manea L., Gilbody S., McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. Can. Med. Assoc. J. 2012;184(3):E191–E196. doi: 10.1503/cmaj.110829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marroquína B., Vineb V., Morgana R. Mental health during the Covid-19 pandemic: Effects of stay-at-home policies, social distancing behavior, and social resources. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niederkrotenthaler T., Gunnell D., Arensman E., Pirkis J., Appleby L., Hawton K., John A., Kapur N., Khan M., O'Connor R.C., Platt S., International Covid-19 Suicide Prevention Research Collaboration Suicide research, prevention, and Covid-19. Crisis. 2020;41(5):321–330. doi: 10.1027/0227-5910/a000731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor R.C., Wetherall K., Cleare S., McClelland H., Melson A.J., Niedzwiedz C.L., O’Carroll R.E., O’Connor D.B., Platt S., Scowcroft E., Watson B., Zortea T., Ferguson E., Robb K.A. Mental health and well-being during the Covid-19 pandemic: longitudinal analyses of adults in the UK Covid-19 Mental Health & Wellbeing study. Br. J. Psychiatry. 2021;218:326–333. doi: 10.1192/bjp.2020.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsson I., Mykletun A., Dahl A.A. The hospital anxiety and depression rating scale: a cross-sectional study of psychometrics and case finding abilities in general practice. BMC Psychiatry. 2005;5(46) doi: 10.1186/1471-244X-5-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan K.J., Kok A.A.L., Eikelenboom M., Horsfall M., Jörg F., Luteijn R.A., Rhebergen D., van Oppen P., Giltay E.J., Penninx B. The mental health impact of the Covid-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry. 2021;8(2):121–129. doi: 10.1016/S2215-0366(20)30491-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieh C., Budimir S., Probst T. The effects of age, gender, income, work and physical activity on mental health during coronavirus disease (Covid-19) lockdown in Austria. J. Psychosom. Res. 2020;136 doi: 10.1016/j.jpsychores.2020.110186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., Kontopantelis E., Webb R., Wessely S., McManus S., Abel K.M. Mental health before and during the Covid-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7(10):883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirkis J., John A., Shin S., DelPozo-Banos M., Arya V., Analuisa Aguilar P., Appleby L., Arensman E., Bantjes J., Baran A., Bertolote J.M., Borges G., Brecic P., Caine E., Castelpietra G., Chang S.S., Colchester D., Crompton D., Curkovic M., Deisenhammer E.A., Du C., Dwyver J., Erlangsen A., Faust J.S., Fortune S., Garrett A., George D., Gerstner R., Gilissen R., Gould M., Hawton K., Kanter J., Kapur N., Khan M., Kirtley O.J., Knipe D., Kolves K., Leske S., Marahatta K., Mittendorfer-Rutz E., Neznanov N., Niederkrotenthaler T., Nielsen E., Nordentoft M., Oberlechner H., O`Connor R.C., Pearson M., Phillips M.R., Platt S., Plener P.L., Psota G., Qin P., Radeloff D., Rados C., Reif A., Reif-Leonhard C., Rozanov V., Schlang C., Schneider B., Semenova N., Sinyor M., Townsend E., Ueda M., Vijayakumar L., Webb R.T., Weerasinghe M., Zalsman G., Gunnell D., Spittal M.J. Suicide trends in the early months of the Covid-19 pandemic: interrupted time series analysis of preliminary data from 21 countries. Lancet Psychiatry. 2021;8(7):579–588. doi: 10.1016/S2215-0366(21)00091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roesch E., Amin A., Gupta J. Violence against women during the Covid-19 pandemic restrictions. BMJ. 2020;369:m1712. doi: 10.1136/bmj.m1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistik Austria, 2015. Österreichische Gesundheitsbefragung 2014. Hauptergebnisse des Austrian Health Interview Survey (ATHIS) und methodische Dokumentation [Austrian Health Survey 201. Main results of the Austrian Health Interview Survey (ATHIS) and methodological documentation], p. 2014, Statistik Austria, Wien 2015.
- Takaku R., Yokoyama I. SSRN; 2020. What School Closure Left in its Wake: Contrasting Evidence Between Parents and Children from the first Covid-19 Outbreak. [DOI] [Google Scholar]
- Taquet M., Luciano S., Geddes J.R., Harrison P.J. Bidirectional associations between Covid-19 and psychiatric disorder: retrospective cohort studies of 62354 Covid-19 cases in the USA. Lancet Psychiatry. 2021;8(2):130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge J.M., Cooper A.B., Joiner T.E., Duffy M.E., Binau S.G. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. J. Abnorm. Psychol. 2019;128(3):185–199. doi: 10.1037/abn0000410. [DOI] [PubMed] [Google Scholar]
- Ueda M., Stickley A., Sueki H., Matsubayashi T. Mental health status of the general population in Japan during the Covid-19 pandemic. Psychiatry Clin. Neurosci. 2020;74(9):496–512. doi: 10.1111/pcn.13105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations, 2020. Covid-19 and the need for action on mental health, policy brief. ( https://www.un.org/sites/un2.un.org/files/un_policy_brief-covid_and_mental_health_final.pdf ). Accessed 22 February 2021.
- Vienna,. at, 2020. Häusliche Gewalt: Anstieg gegen Ende der Beschränkungen [domestic violence—increase towards end of restrictions], Vienna.at, 21 September. ( https://www.vienna.at/live-studie-zu-haeuslicher-gewalt-waehrend-corona-wird-praesentiert/6746655 ). Accessed 22 February 2021.
- Vindegaard N., Benros M.E. Covid-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner G., Zeiler M., Waldherr K., Philipp J., Truttmann S., Dür W., Treasure J.L., Karwautz A.F.K. Mental health problems in Austrian adolescents: a nationwide, two-stage epidemiological study applying DSM-5 criteria. Eur. Child Adolesc. Psychiatry. 2017;26(12):1483–1499. doi: 10.1007/s00787-017-0999-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Choo F.N., Tran B., Ho R., Sharma V.K., Ho C. A longitudinal study on the mental health of general population during the Covid-19 epidemic in China. Brain Behav. Immun. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkler P., Formanek T., Mlada K., Kagstrom A., Mohrova Z., Mohr P., Csemy L. Increase in prevalence of current mental disorders in the context of Covid-19: analysis of repeated nationwide cross-sectional surveys. Epidemiol. Psychiatr. Sci. 2020;29(e173):1–8. doi: 10.1017/S2045796020000888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, 2020. Mental health and psychosocial considerations during the Covid-19 outbreak, WHO/2019-nCoV/MentalHealth/2020.1, WHO Headquarters.
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of Covid-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamura E., Tsustsui Y. The impact of closing schools on working from home during the Covid-19 pandemic: evidence using panel data from Japan. Rev. Econ. Househ. 2021:1–20. doi: 10.1007/s11150-020-09536-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Selected data from this study can be obtained from the authors upon reasonable request after the completion of ongoing work with this dataset.