Abstract
Background
Young adult (YA) cancer survivors are at risk for financial toxicity during and after cancer treatment. Financial toxicity has been associated with medical‐related cost‐coping behaviors such as skipping or delaying treatment. The coronavirus disease 2019 (COVID‐19) pandemic has resulted in dire economic consequences that may worsen financial hardship among young survivors.
Methods
This was a cross‐sectional survey; data collection occurred online. A convenience sample was recruited through YA cancer advocacy groups and social media. Negative economic events associated with the COVID‐19 pandemic (eg, income loss, increased debt, and decreased job security) and medical‐related cost‐coping were documented. A validated measure assessed cancer‐related financial toxicity.
Results
Participants (N = 212) had a mean age of 35.3 years at survey completion and a mean age of 27.4 years at diagnosis. Financial toxicity (mean, 14.0; SD, 9.33) was high. Two‐thirds of the sample experienced at least 1 negative economic event during COVID‐19, and 71% engaged in at least 1 medical cost‐coping behavior. Cost‐coping and pandemic‐related negative economic events were significantly correlated with cancer‐related financial toxicity. In multivariable analyses, pandemic‐related negative economic events and financial toxicity were associated with cost‐coping.
Conclusions
Acute negative economic events associated with the COVID‐19 pandemic may exacerbate cancer‐related financial toxicity and overall financial hardship among YAs and lead to cost‐coping behaviors that can compromise survivorship care and health outcomes. Multilevel, systematic interventions are needed to address the financial needs of YA survivors after the global pandemic.
Keywords: coronavirus disease 2019 (COVID‐19), cost‐coping, financial toxicity, survivorship, young adult
Short abstract
This study illustrates how the acute negative economic events associated with the coronavirus disease 2019 pandemic may have exacerbated existing cancer‐related financial toxicity and general financial hardship among young adult cancer survivors. These negative economic events and financial toxicity are associated with cost‐coping behaviors that can compromise survivorship care and health outcomes.
Introduction
Young adult (YA) cancer survivors, a cohort of more than 630,000 survivors aged 18 to 39 years, face financial‐related hardship during and after treatment. 1 , 2 This hardship, often called financial toxicity, occurs at higher rates among YAs than older survivors. 3 , 4 The National Cancer Institute broadly defines financial toxicity as “problems a cancer patient has related to the cost of treatment.” 5 In addition to the high cost of treatment, cancer‐related financial issues may be caused by disruptions in employment and wages (also affecting health insurance coverage), debt related to medical expenses, and increases in cost sharing between insurers and patients. 6 The prevalence of financial toxicity and associated financial hardship is high, with estimates ranging from 42% to 73% in the broader population of cancer survivors, and 90% of YA survivors reporting medically‐related financial needs. 6 , 7 , 8
Having cancer as a YA may delay or inhibit the achievement of milestones crucial to establishing financial independence, including graduation, workforce entry, and/or career development and progression, and lead to financial hardship during and after treatment. 9 , 10 In comparison with noncancer populations, financial toxicity and hardship among cancer survivors have been associated with higher rates of bankruptcy and asset depletion and with increased morbidity and mortality. 8 , 11 Enduring financial effects after a YA cancer diagnosis can lead to medical‐related cost‐coping behaviors (ie, medication nonadherence and/or avoidance of care due to financial reasons) and decreased psychosocial well‐being and quality of life. 1 , 12 , 13 The ongoing global pandemic caused by coronavirus disease 2019 (COVID‐19) is likely to exacerbate financial stressors in all patients with cancer and especially in those in vulnerable populations, including YA survivors. Understanding YA survivor experiences during and after COVID‐19 will be important in developing responsive interventions to ensure continuity of care.
The economic hardships resulting from the COVID‐19 pandemic are well documented, and there is emerging literature exploring COVID‐19's impact on cancer care. 14 An estimated 7.7 million Americans have lost their jobs and employer‐sponsored health insurance, and current evidence suggests that the pandemic worsens cancer‐related financial toxicity for cancer survivors. 15 , 16 Indeed, cancer survivors may be “doubly hit” as they face co‐occurring financial hardships from the pandemic and their cancer care. 17 Cancer survivors with transient or temporary employment, which is more likely in young adulthood, have been reported to be at higher risk for the negative economic effects of COVID‐19. 18 , 19
Little is known about how the pandemic has specifically affected the financial situations of YA cancer survivors, a population already susceptible to financial hardship. To fill this gap, this study aimed to 1) describe cancer‐related financial toxicity, pandemic‐related negative economic events, and medical‐related cost‐coping behaviors in a national sample of YA cancer survivors during COVID‐19; 2) determine the relationships among financial toxicity, pandemic‐related negative economic events, and cost‐coping behaviors; and 3) identify associations with cost‐coping behaviors in multivariate analyses.
Materials and Methods
Design
An anonymous, cross‐sectional survey study was conducted via REDCap, a secure online data collection platform. 20 The Memorial Sloan Kettering institutional review board approved the survey as exempt research. Data were collected from December 2020 to February 2021.
Setting, Participants, and Recruitment
Eligible participants were older than 18 years and were treated for cancer before the age of 40 years. All cancer diagnoses, treatment types, and treatment phases were included. A convenience sample was recruited online through a multifaceted strategy, including social media posts, emails, and paid advertisements. Social media recruitment included Facebook posts on the main pages of YA cancer advocacy organizations and within public and private groups on their pages and Instagram story “swipe‐up” links for advocacy organizations with more than 10,000 followers. On Twitter, tweets were posted by study investigators and from the account created for the study itself: these were then retweeted by YA cancer advocacy organizations, by other health care providers and researchers, and by YA survivors and advocates both within and outside the investigators' individual networks of followers. Hashtags for all social media recruitment included #AYACSM, #AYA, #financialtoxicity, and #cancerisntfree. Email recruitment occurred via YA cancer advocacy organizations and program coordinators of hospital‐based YA support programs. In addition, the research team purchased Facebook and Instagram advertisements and Twitter promoted tweets to appear on the feeds and timelines of users who liked or followed posts and groups associated with YA cancer advocacy. Participants were not paid for completing the survey.
Variables and Measures
Cancer‐related financial toxicity was measured with the Comprehensive Score for Financial Toxicity (COST), a validated 11‐item measure. 21 Responses to 5‐point, Likert‐style, scaled questions were summed (possible range, 0‐44), with lower scores representing worsening financial toxicity. 21 Although COST has not been validated for use in YA samples specifically, our previous use of it in a YA sample suggested excellent internal consistency (α = 0.90). 13
Questions related to pandemic‐related negative economic outcomes of COVID‐19 were drawn from the Centers for Disease Control and Prevention/National Institutes of Health Common Data Element COVID‐19 Bank (https://www.nlm.nih.gov/dr2/COVID‐19_BSSR_Research_Tools.pdf). Respondents reported whether they lacked money for medication, medical expenses, food, gas, or rent/housing because of the pandemic. They also were asked to report COVID‐19–related increases in credit card debt, loss of insurance, and negative changes to employment, including job loss or furlough; decreased hours, pay, or job security; and work disruptions due to childcare.
Medical‐related cost‐coping behaviors were assessed with questions modeled after the Medical Expenditure Panel Survey. Participants selected “yes” if, in the past year, they had engaged in any 1 of 7 cost‐coping behaviors because they were worried about the cost: skipping a medical test, treatment, or follow‐up; having a medical problem but not seeing a provider; not seeing a needed specialist; putting off or postponing preventative care; putting off or postponing mental health care; not filling a prescription; or taking a smaller dose or fewer pills than prescribed (https://www.ahrq.gov/data/meps.html).
Participants also self‐reported demographic information (education, income, race, ethnicity, and relationship status) and clinical information (primary cancer diagnosis, treatment received, phase of treatment, recurrence status, and time since treatment completion).
Analysis
Descriptive statistics characterized demographics, financial toxicity scores, negative economic events, and cost‐coping behaviors. Pandemic‐related negative economic events and cost‐coping were evaluated with a dichotomized variable (if the respondent reported any behavior or event) and a composite sum of all behaviors or events. Univariate testing (2‐sided independent sample t tests, χ2 tests, and Spearman correlations; α = 0.05) examined initial relationships between demographic variables and cancer‐related financial toxicity scores and the sums of negative economic events and cost‐coping behaviors. To learn more about the experience of the impact of COVID‐19, we conducted additional univariate analyses to explore associations between demographic variables and key pandemic‐related economic events (increased credit debt, loss of job/furlough, and not having enough money for medical expenses) and each cost‐coping behavior. Among respondents engaging in at least 1 cost‐coping behavior, a multivariate Poisson regression model was specified to assess the robustness of the associations of pandemic‐related negative economic events and financial toxicity scores with the number of reported cost‐coping behaviors; it controlled for age, race/ethnicity, treatment status, education, full‐time employment, and income. Among all respondents, multivariate binary logistic regression models, controlling for the same variables as the Poisson regression, were specified to assess the likelihood of engaging in any cost‐coping behavior and to assess the likelihood of engaging in each of the 7 cost‐coping behaviors. IBM SPSS Statistics 26 was used for analysis.
Results
Sample
There were 325 YAs who clicked on the survey link, which was received via email, social media posting, or advertisement; 5 were ineligible, and 108 declined participation. This yielded a final sample of 212 (65% response rate among eligible respondents). The participants had a mean age of 35.3 years (SD, 5.25 years) at survey completion and a mean age of 27.4 years (SD, 7.17 years) at diagnosis; most were women (87%) and non‐Hispanic White (73%) and had at least a bachelor's degree (71%). The most common diagnoses were breast cancer (26%) and lymphoma (17%). Most participants (57%) had completed all treatment; 27% were still receiving hormonal or endocrine therapy, and 14% reported being on active treatment. Those who had completed treatment (n = 120) were a mean of 6.2 years (SD, 5.89 years) from completion. See Table 1 for the cohort demographics.
TABLE 1.
Sample Demographics and Clinical Information (N = 212)
| Characteristic | No. (%) |
|---|---|
| Gender | |
| Woman | 185 (87.3) |
| Man | 19 (8.9) |
| Nonbinary | 4 (1.9) |
| Prefer not to respond | 4 (1.9) |
| Race | |
| White | 154 (72.6) |
| Black | 9 (4.2) |
| Hispanic/Latino/a/x | 21 (9.9) |
| Asian | 6 (2.8) |
| Native American/American Indian | 1 (0.5) |
| More than 1 race/unknown | 12 (5.7) |
| Prefer not to respond | 9 (4.2) |
| Current relationship status | |
| Single/not living with partner | 80 (37.7) |
| Married/living with partner | 117 (55.2) |
| Widowed, divorced, or separated | 10 (4.7) |
| Prefer not to respond | 5 (2.4) |
| Highest education | |
| High school | 8 (3.8) |
| Some college or vocational training | 24 (11.3) |
| Associate's degree | 17 (8.0) |
| Bachelor's degree | 69 (32.5) |
| Graduate or professional degree | 89 (42.0) |
| Prefer not to respond | 5 (2.4) |
| Current household income | |
| <$25,000 | 29 (13.7) |
| $25,000‐$49,999 | 37 (17.5) |
| $50,000‐$99,999 | 75 (35.4) |
| ≥$100,000 | 55 (25.9) |
| Do not know | 5 (2.4) |
| Prefer not to respond | 11 (5.2) |
| Employment status a | |
| Working full‐time | 123 (58.0) |
| Working part‐time | 18 (8.5) |
| Homemaker/stay‐at‐home parent | 15 (7.1) |
| In school | 19 (9.0) |
| On disability (short‐ or long‐term) | 37 (17.5) |
| Unemployed | 16 (7.5) |
| Prefer not to respond | 10 (5.8) |
| Diagnosis | |
| Breast | 59 (27.8) |
| Lymphoma | 35 (16.5) |
| Colorectal | 24 (11.3) |
| Leukemia | 20 (9.4) |
| Brain | 15 (7.1) |
| Gynecological | 13 (6.1) |
| Sarcoma | 13 (6.1) |
| Thyroid | 10 (4.7) |
| Other | 17 (8.0) |
| Prefer not to respond | 1 (0.5) |
| Treatment status | |
| Active treatment | 30 (14.2) |
| Receiving hormonal/endocrine therapy | 57 (26.9) |
| Completed treatment | 120 (56.6) |
| Prefer not to respond | 5 (2.4) |
Respondents could select more than 1 answer.
Cancer‐Related Financial Toxicity
Cancer‐related financial toxicity, as measured by COST, was high: the mean score was 14.0 (SD, 9.33), and scores < 26 typically correspond to the presence of financial toxicity, with scores below 14 indicating severe financial toxicity. 21 , 22 The tool demonstrated very good internal consistency in the sample (α = 0.88). In univariate analysis, worse financial toxicity was associated with lacking full‐time employment (mean difference, –4.66; 95% CI, –7.18 to –2.13), less education (ρ = 0.31; P < .001), lower income (ρ = 0.47; P < .001), and a younger age at survey completion (ρ = 0.16; P = .03). Race/ethnicity, diagnosis, and time since treatment were not associated with COST scores. See Table 2 for the univariate analyses.
TABLE 2.
Univariate Analyses
| Spearman ρ Correlation Coefficients | |||||||
|---|---|---|---|---|---|---|---|
| 1. Negative Economic Events | 2. Cost‐Coping Behaviors | 3. COST | 4. Age at Survey | 5. Income | 6. Time Since Treatment | 7. Education | |
| 1 | — | 0.49 a | –0.59 a | –0.11 | –0.38 a | 0.05 | –0.28 a |
| 2 | — | –0.53 a | –0.17 b | –0.20 c | 0.10 | –0.23 c | |
| 3 | — | 0.16 b | 0.47 a | 0.01 | 0.31 a | ||
| 4 | — | 0.08 | 0.13 | 0.16 b | |||
| 5 | — | 0.13 | 0.33 a | ||||
| 6 | 0.01 | ||||||
| Demographic Associations (t/χ2) | ||||||
|---|---|---|---|---|---|---|
| Age at Survey d | Time Since Treatment e | Race/Ethnicity f | Income at Survey g | Highest Education h | Full‐Time Employment i | |
| Experienced ≥1 negative economic events | 2.1 b | 0.4 | 0.4 | 9.7 c | 4.2 b | 4.0 b |
| Engaged in ≥1 cost‐coping behaviors | 1.8 | 0.4 | 0.7 | 6.2 b | 6.7 c | 0.02 |
| Lacking money for medical expenses | 1.0 | 0.5 | 0.09 | 4.6 b | 7.3 c | 2.4 |
| Job loss or furlough | 1.9 | 1.8 | 1.5 | 9.5 c | 0.05 | 6.8 c |
| Credit card debt increase | 1.4 | 0.6 | 1.0 | 4.3 c | 14.1 a | 2.6 |
| Skipping medical test, treatment, or follow‐up | 3.1 c | –1.2 | 0.05 | 2.3 | 3.8 | 0.2 |
| Not seeing provider for health problem | 1.4 | –0.4 | 0.1 | 1.4 | 5.3 b | 1.0 |
| Not seeing a needed specialist | 1.7 | –3.1 c | 0.2 | 1.3 | 1.6 | 0.002 |
| Postponing preventative care | 0.008 | –1.7 | 0.7 | 0.9 | 1.9 | 0.8 |
| Postponing mental health care | 1.8 | 0.2 | 1.9 | 3.4 | 2.0 | 0.02 |
| Not filling a prescription | 2.7 c | 1.2 | 5.2 b | 7.7 c | 18.7 a | 11.4 c |
| Taking a smaller dose than prescribed | 0.7 | 0.008 | 6.6 b | 5.3 b | 14.5 a | 2.9 |
Abbreviation: COST, Comprehensive Score for Financial Toxicity.
P < .001.
P < .05.
P < .01.
df = 194 (t test).
df = 110 (t test).
Non‐Hispanic White versus non‐White and/or Hispanic (χ2 test).
Less than $50,000 versus $50,000 or more annually (χ2 test).
Less than a bachelor's degree versus a bachelor's degree or higher (χ2 test).
Yes versus no (χ2 test).
Pandemic‐Related Negative Economic Events
Figure 1 illustrates the frequency of negative economic events due to COVID‐19 and cost‐coping behaviors. Two‐thirds of the sample reported at least 1 pandemic‐related negative economic event: for those, the mean number of events (of 14 possible) was 2.9 (SD, 2.00). Thirty‐six percent of the sample stated that their credit card debt had increased since the pandemic, and 21% reported not having enough money to pay their rent/mortgage because of the pandemic. Respondents also reported not having enough money for medical expenses (19%), food (17%), and medication (12%) directly because of the pandemic. As for employment, 19% of the sample lost their job or were furloughed, 17% experienced decreased job security, 15% reported decreased pay, 12% lost work hours, and 7% were disrupted in their employment because of childcare.
Figure 1.
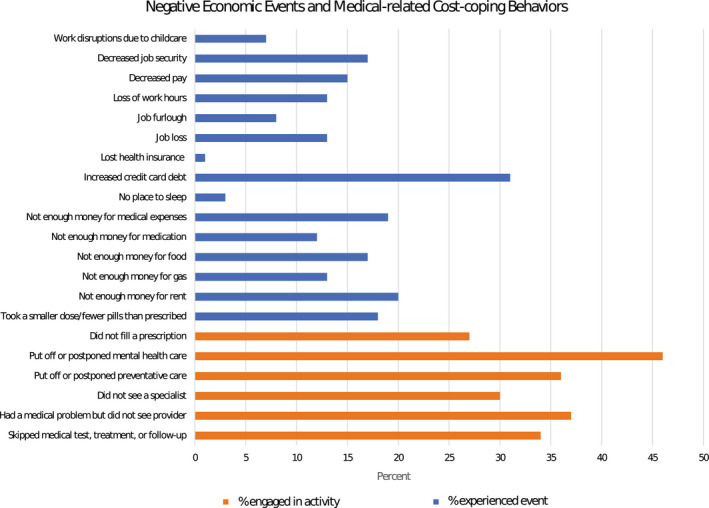
Frequency of pandemic‐related negative events and medical‐related cost‐coping behaviors.
In univariate testing, lacking full‐time employment (mean difference, 0.94; 95% CI, 0.37‐1.51), lower income (ρ = –0.38; P < .001), and lower education (ρ = –0.28; P < .001) were related to experiencing more pandemic‐related negative economic events. Age, race/ethnicity, and time since treatment were not associated with the count of negative economic events. Worse cancer‐related financial toxicity was associated with more pandemic‐related negative economic events (ρ = –0.59; P < .001).
Not having enough money to pay for medical expenses during the pandemic was associated with lower education (χ2 = 7.3; P = .007) and lower income (χ2 = 4.6; P = .03). Age, race/ethnicity, time since treatment, and employment were not associated with not having enough money for medical expenses. Experiencing job loss or a furlough during the pandemic was associated with lower income (χ2 = 9.5; P = .002) and lacking full‐time employment (χ2 = 6.8; P = .009) but was not associated with age, race/ethnicity, time since treatment, or education. A pandemic‐related credit card debt increase was associated with lower education (χ2 = 14.1; P < .001) and lower income (χ2 = 4.3; P = .04) but not with age, race/ethnicity, time since treatment, or employment. See Table 2 for complete χ2 findings.
Medical Cost‐Coping
Seventy‐one percent of the respondents reported at least 1 medical cost‐coping behavior during 2020, including postponing mental health (46%) and/or preventative (36%) care; having a health problem but not seeing a provider (37%); skipping a medical test, treatment, or follow‐up (34%); and not filling a prescription (27%) or taking a smaller dose of a medication than prescribed (18%). Among those who engaged in medical cost‐coping (N = 150), the mean number of behaviors (of 7 possible) was 3.2 (SD, 1.89), and the responses followed a Poisson distribution (Kolmogorov–Smirnov = 0.97; P = .31).
In univariate testing, younger age (ρ = –0.17; P = .02), lower income (ρ = –0.20; P = .004), and lower education (ρ = –0.23; P = .001) were related to engaging in more cost‐coping behaviors. Employment, race/ethnicity, diagnosis, and time since treatment were not associated with cost‐coping. Worse cancer‐related financial toxicity was associated with more cost‐coping behaviors (ρ = –0.53; P < .001).
At the item level, demographic variables were typically not significantly associated with cost‐coping behaviors with the following exceptions: skipping a medical test, treatment, or follow‐up was associated with younger age (mean difference, 2.39; 95% CI, 0.87‐3.90); having a health problem but not seeing a provider was associated with lower education (χ2 = 5.3; P = .02); not seeing a needed specialist was associated with a longer time since treatment (mean difference, –3.48; 95% CI, –5.84 to –1.12); not filling a prescription was associated with younger age (mean difference, 2.27; 95% CI, 0.84‐3.92), lower income (χ2 = 7.7; P = .006), lower education (χ2 = 18.7; P < .001), a race/ethnicity other than White non‐Hispanic (χ2 = 5.2; P = .02), and lacking full‐time employment (χ2 = 11.4; P = .001); and taking a smaller dose than prescribed was associated with lower income (χ2 = 5.3; P = .02), lower education (χ2 = 14.5; P < .001), and a race/ethnicity other than White non‐Hispanic (χ2 = 6.7; P = .01). See Table 2 for complete χ2 findings.
Multivariate Analysis
A Poisson regression model was run to predict the number of cost‐coping behaviors on the basis of the number of pandemic‐related negative economic events and COST score; it controlled for age, race/ethnicity, treatment status, education, full‐time employment, and income. For each additional pandemic‐related negative economic event experienced, there was an estimated 6.5% increase in the number of cost‐coping behaviors (95% CI, 1.3%‐11.9%; P = .013). For each point increase in the COST score (suggesting better outcomes), there was an estimated 1.8% decrease in the number of cost‐coping behaviors (95% CI, 0.1%‐3.4%; P = .036). The overall model was significant (likelihood χ2 = 20.1(2); P < .001). Although negative economic events related to the pandemic and financial toxicity were correlated in univariate analyses, collinearity diagnostics suggested that multicollinearity was not an issue in the model (variance inflation factors of 1.44 [pandemic‐related negative economic events] and 1.54 [COST score]) 23 (see Table 3).
TABLE 3.
Multivariate Associations With Cost‐Coping Behaviors
| Poisson Regression: Total Cost‐Coping Behaviors a | Odds Ratio | 95% CI | Standard Error | Wald |
|---|---|---|---|---|
| Total negative economic events | 1.06 | 1.10 | 0.03 | 6.1 b |
| COST | 0.98 | 0.97‐0.99 | 0.01 | 4.3 b |
| Multiple Logistic Regression a | Odds Ratio | 95% CI | Standard Error | Wald |
|---|---|---|---|---|
| Any cost coping behavior | ||||
| Total negative economic events | 1.50 | 1.09‐2.06 | 0.16 | 6.1 b |
| COST | 0.91 | 0.86‐0.96 | 0.03 | 12.2 d |
| Skipped a medical test, treatment, or follow‐up | ||||
| Total negative economic events | 1.44 | 1.14‐1.81 | 0.12 | 9.4 c |
| COST | 0.86 | 0.80‐0.93 | 0.04 | 16.4 d |
| Had a medical problem but did not see a provider | ||||
| Total negative economic events | 1.44 | 1.16‐1.78 | 0.11 | 10.9 c |
| COST | 0.94 | 0.89‐0.99 | 0.03 | 4.7 b |
| Did not see a specialist | ||||
| Total negative economic events | 1.35 | 1.10‐1.67 | 0.11 | 8.2 c |
| COST | 0.93 | 0.88‐0.99 | 0.03 | 6.0 b |
| Postponed preventative care | ||||
| Total negative economic events | 1.33 | 1.09‐1.63 | 0.10 | 7.6 c |
| COST | 0.94 | 0.89‐0.99 | 0.03 | 5.6 b |
| Postponed mental health care | ||||
| Total negative economic events | 0.96 | 0.79‐1.17 | 0.10 | 0.1 |
| COST | 0.89 | 0.85‐0.94 | 0.03 | 16.5 d |
| Did not fill a prescription | ||||
| Total negative economic events | 1.24 | 1.01‐1.53 | 0.11 | 4.2 b |
| COST | 0.96 | 0.90‐1.02 | 0.03 | 2.1 |
| Took a smaller dose or fewer pills than described | ||||
| Total negative economic events | 1.19 | 0.95‐1.49 | 0.12 | 2.3 |
| COST | 0.98 | 0.92‐1.04 | 0.03 | 0.5 |
Abbreviation: COST, Comprehensive Score for Financial Toxicity.
Controlling for age, income, education, race/ethnicity, treatment status, and full‐time employment.
P < .05.
P < .01.
P < .001.
In a logistic regression model controlling for age, race/ethnicity, treatment status, education, full‐time employment, and income, more pandemic‐related negative events and worse financial toxicity were also predictive of the likelihood of engaging in any cost‐coping. For each additional pandemic‐related negative economic event experienced, there was an estimated 51.5% increase in the likelihood of a cost‐coping behavior (95% CI, 10%‐108.5%; P = .011). For each point increase in the COST score, there was an estimated 9.5% decrease in the likelihood of a cost‐coping behavior (95% CI, 4.4%‐14.3%; P < .001).
Pandemic‐related negative economic events and financial toxicity were also generally associated with the odds of each of the individual cost‐coping behaviors in logistic regression models controlling for the same variables noted previously. Exceptions included putting off/postponing mental health care (only financial toxicity was associated), not filling a prescription (only negative economic events were associated), and taking a smaller dose than prescribed (neither was associated; see Table 3).
Discussion
Our findings demonstrate the significant financial impact of the COVID‐19 pandemic on YA cancer survivors, a patient group at increased risk for cancer‐related financial hardship, and how this negatively affected health care use. In a national sample of YA cancer survivors, we found frequent use of medical‐related cost‐coping behaviors (71%) and high levels of cancer‐related financial toxicity. Two‐thirds of the sample experienced a negative economic event as a result of the COVID‐19 pandemic; this included 1 in 5 respondents reporting that they did not have enough money for medical expenses. In multivariate analyses, more medical‐related cost‐coping was associated with worse cancer‐related financial toxicity and more negative economic events due to the pandemic.
Established risk factors for a financial burden include a younger age at diagnosis or treatment, non‐White race, lower income, and female sex, and YA survivors face a unique convergence of additive risk factors that make them particularly susceptible. 24 Cancer‐related financial hardship may be worsened by financial challenges endured by many YAs in the general population, including having student loans, credit card debt, and limited savings and assets; earning entry‐level wages; and facing high costs associated with living independently and/or building and raising a family. 25 , 26 The high levels of cancer‐related financial toxicity and overall financial hardship found in our sample illustrate these effects. Over time, these experiences may worsen because cancer‐related costs can continue after treatment on account of ongoing health care needs to address late and long‐term effects, surveillance tests, the repayment of medical debt, and/or the inability to return to work due to physical demands; this potentially leaves survivors in a continual state of “catching up,” a situation likely only exacerbated by the COVID‐19 pandemic. 1 , 27 , 28 , 29 , 30 Indeed, financial toxicity in this sample was worse than that in a similar sample from the pre–COVID‐19 era (mean, 18.8; SD, 10.80). 13
Cancer survivors face long‐term adverse effects of treatment and health risks, and this suggests that the high frequency of medical‐related cost‐coping in our sample may be worrisome. More than one‐third of the sample reported postponing necessary medical care and/or skipping medical tests/treatment because of financial reasons: forgoing such care can lead to increased morbidity, which may necessitate additional, and more expensive, health care. 31 , 32 Failing to adequately manage the late and long‐term effects of treatment can also result in persistent physical and psychosocial impairments. 1 , 33 , 34
The chronic health conditions that may result from cancer or its treatment can hinder YA survivors' ability to safely work outside the home during the pandemic because comorbidities and immunosuppression may place some survivors at high risk for severe COVID‐19. 35 , 36 This risk occurs in addition to the difficulties that YA survivors report regarding their ability to work. In prior research, more than one‐half of adolescent and YA survivors who were working or in school at diagnosis reported problems with returning after treatment. 30 At 15 to 35 months after their diagnosis, 22% of these YA survivors had not returned to full‐time school/work, with 12% “completely unable” to work or go to school. 30 In our sample, nearly 1 in 5 respondents lost their job or were furloughed because of the pandemic, and 17% reported decreased job security. The co‐occurring difficulties of a prior cancer experience and the increased risks associated with COVID‐19 infection may be significant barriers to YAs aiming to return to work or seeking new employment; in addition, survivors may be at risk for workplace and hiring‐based discrimination because of their health history. 37 Future, in‐depth research is needed to explore employment experiences, particularly those related to employment recovery, workplace discrimination, and employer‐sponsored insurance coverage, among YA survivors as time progresses during and after the pandemic.
The COVID‐19 pandemic may also have a profound impact on the mental health of YA survivors. 38 , 39 Nearly one‐half of the sample (46%) reported delaying mental health care during 2020, and financial toxicity was associated with delaying mental health care in multivariate modeling. These are problematic findings because of the negative psychosocial outcomes associated with both financial toxicity and the social isolation and anxiety that may have occurred during periods of quarantine and/or lockdowns. 13 , 40 A study of mental health among cancer survivors of all ages in Hong Kong, conducted early in the pandemic (April to May 2020), found that those with a cancer history were more likely to catastrophize COVID‐19 and experienced more generalized health anxiety than noncancer controls. 41 Similarly, among 177 adolescent and YA cancer patients and survivors also surveyed in April to May 2020, 62% felt more anxiety than before the pandemic, and one‐third had psychological distress scores in a range of clinical concern. 42 These findings are supported by survey research later in the pandemic that suggested adult survivors of childhood cancer experienced anxiety related to the uncertainty of their health risks, with 81% of a sample of 120 meeting clinical definitions of anxiety. A qualitative study exploring the isolation of YA cancer patients and survivors in Denmark during COVID‐19 highlighted themes of loneliness and anxiety. 40 The authors commented on how the pandemic was yet another disruption to the developmental trajectory of YA cancer survivors and stressed the value that participants placed on social interactions (eg, peer‐to‐peer support); they called on health care providers to creatively address the mental health and social needs of their patients, including creating online peer support groups and, when it is safe and feasible to do so, shifting peer support to an outdoor setting.
Multilevel, systematic interventions are needed to address the financial needs of YA survivors in the aftermath of the global pandemic. Telemedicine visits, when clinically appropriate, have been shown to reduce costs for patients with cancer and may help to alleviate some of the financial stress (eg, commuting, parking, and childcare costs) and safety concerns of YAs. 43 Emerging evidence suggests high levels of patient satisfaction and confidence with telemedicine visits during COVID‐19 and, among adult survivors of childhood cancers, a preference for telemedicine visits over in‐person visits. 44 , 45 Telemedicine may, however, present difficulties for YAs in rural areas with unreliable internet service or for those with limited English proficiency, who may require coordination with a medical interpreter. Although YAs in the United States generally report high access to and comfort with digital tools, this should not be assumed. 46 Health care systems and providers need to be cognizant of potential disparities in access when designing and implementing their telemedicine platforms. 47
In terms of tangible assistance, financial advocates can help the newly unemployed to navigate Marketplace insurance plans and unemployment filings, and charitable organizations have responded to acute needs with COVID‐19–specific education sessions and emergency assistance funds. 48 , 49 Financial navigation and counseling programs may help YAs to better understand the complex workings of health care financing systems and empower them to engage in cost‐related conversations with health care providers: previous research in this regard has found that YAs desire navigation assistance throughout the cancer treatment continuum, including survivorship. 50 , 51 , 52 , 53 Governmental support will also be key in helping YAs to recover economically from the pandemic; research from outside the United States has shown that universal financial support programs have helped to mitigate the negative impact of job loss on health‐related quality of life. 54
The generalizability of our findings is limited by the demographic composition of our sample and the use of social media recruitment strategies. Social media recruitment allowed us to reach a national sample of YA cancer survivors, but our findings came from a convenience sample and may not be generalizable to the broader YA patient population because social media strategies may attract more engaged survivors whose online activities are connected to cancer‐related organizations or groups and whose identities may not be representative of all YA cancer survivors. 55 For example, despite our survey being shared by several of the largest YA cancer advocacy organizations, only approximately 27% of our sample were respondents of color, and only 9% identified as a cisgender or transgender man. Nonetheless, because of the ubiquity with which YAs engage with social media and the digital world more broadly, social media and other crowdsourcing techniques are recommended for recruiting this hard‐to‐reach patient group. 56 , 57 However, it is incumbent on research teams to construct digital recruitment strategies that yield samples that are representative of the populations from which they are drawn, and this may entail creating strategies that combine online and offline recruitment. Because of the high formal educational attainment of our sample and the well‐established positive correlation between formal education and income, our findings are likely an underestimation of the financial issues and economic hardships faced by YA cancer survivors during the COVID‐19 pandemic. 58 Furthermore, because the pandemic has had a disproportionately negative impact on Black, Indigenous, and Latino communities, our findings may not have captured the breadth of experiences of cancer survivors in these communities. 59 , 60 , 61 Future research must acknowledge and take steps to address the influence of such health inequities and systemic racism on experiences of financial hardship and the provision of care. Finally, our study is limited in that we did not capture any COVID‐19–related‐health information from respondents: a COVID‐19 diagnosis and/or prolonged associated illness could have contributed to, or exacerbated, financial hardship, particularly among respondents with transient employment or inadequate health insurance.
In conclusion, this study illustrates the acute negative economic events resulting from the COVID‐19 pandemic and demonstrates the association between these events and cancer‐related financial toxicity and medical cost‐coping among YA survivors. Further longitudinal analyses will be required in diverse YA samples to fully understand the lasting impact of COVID‐19 on this vulnerable and historically understudied population.
Funding Support
This study was funded in part by Cancer Center Support Grant P30 CA008748 (National Institutes of Health/National Cancer Institute) and the Chanel Endowment to Fund Survivorship Research. Danielle N. Friedman is supported by an American Cancer Society Clinician Scientist Development Grant.
Conflict of Interest Disclosures
Catherine Benedict reports being a board member of Stupid Cancer (unpaid) and having stock in GRYT Health. The other authors made no disclosures.
Author Contributions
Bridgette Thom: Data analysis; study conception and design; data collection and interpretation; and manuscript writing, editing, and approval. Catherine Benedict: Study conception and design; data collection and interpretation; and manuscript writing, editing, and approval. Danielle N. Friedman: Study conception and design; data collection and interpretation; and manuscript writing, editing, and approval. Samantha E. Watson: Study conception and design; data collection and interpretation; and manuscript writing, editing, and approval. Michelle S. Zeitler: Study conception and design; data collection and interpretation; and manuscript writing, editing, and approval. Fumiko Chino: Data analysis; financial support; study conception and design; data collection and interpretation; and manuscript writing, editing, and approval.
Thom B, Benedict C, Friedman DN, Watson SE, Zeitler MS, Chino F. Economic distress, financial toxicity, and medical cost‐coping in young adult cancer survivors during the COVID‐19 pandemic: Findings from an online sample. Cancer. 2021. 10.1002/cncr.33823
We thank the young adult cancer survivor advocacy groups and individuals who shared our study on social media, and we also thank the study participants for sharing their experiences.
References
- 1. Landwehr MS, Watson SE, Macpherson CF, Novak KA, Johnson RH. The cost of cancer: a retrospective analysis of the financial impact of cancer on young adults. Cancer Med. 2016;5:863‐870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Miller KD, Nogueira L, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69:363‐385. [DOI] [PubMed] [Google Scholar]
- 3. Zafar SY, Abernethy AP. Financial toxicity, part I: a new name for a growing problem. Oncology. 2013;27:80‐81. [PMC free article] [PubMed] [Google Scholar]
- 4. Salsman JM, Bingen K, Barr RD, Freyer DR. Understanding, measuring, and addressing the financial impact of cancer on adolescents and young adults. Pediatr Blood Cancer. 2019;66:e27660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Financial Toxicity (Financial Distress) and Cancer Treatment (PDQ®)–Patient Version. National Cancer Institute. Published 2019. https://www.cancer.gov/about‐cancer/managing‐care/track‐care‐costs/financial‐toxicity‐pdq. Accessed January 06, 2021. [Google Scholar]
- 6. Gordon LG, Merollini KM, Lowe A, Chan RJ. A systematic review of financial toxicity among cancer survivors: we can't pay the co‐pay. Patient. 2017;10:295‐309. [DOI] [PubMed] [Google Scholar]
- 7. Keegan TH, Lichtensztajn DY, Kato I, et al. Unmet adolescent and young adult cancer survivors information and service needs: a population‐based cancer registry study. J Cancer Surviv. 2012;6:239‐250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Altice CK, Banegas MP, Tucker‐Seeley RD, Yabroff KR. Financial hardships experienced by cancer survivors: a systematic review. J Natl Cancer Inst. 2016;109:djw205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Docherty SL, Kayle M, Maslow GR, Santacroce SJ. The adolescent and young adult with cancer: a developmental life course perspective. Semin Oncol Nurs. 2015;31:186‐196. [DOI] [PubMed] [Google Scholar]
- 10. Kayser K, Smith L, Washington A, Harris LM, Head B. Living with the financial consequences of cancer: a life course perspective. J Psychosoc Oncol. 2021;39:17‐34. [DOI] [PubMed] [Google Scholar]
- 11. Ramsey SD, Bansal A, Fedorenko CR, et al. Financial insolvency as a risk factor for early mortality among patients with cancer. J Clin Oncol. 2016;34:980‐986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kaul S, Avila JC, Mehta HB, Rodriguez AM, Kuo YF, Kirchhoff AC. Cost‐related medication nonadherence among adolescent and young adult cancer survivors. Cancer. 2017;123:2726‐2734. [DOI] [PubMed] [Google Scholar]
- 13. Thom B, Benedict C. The impact of financial toxicity on psychological well‐being, coping self‐efficacy, and cost‐coping behaviors in young adults with cancer. J Adolesc Young Adult Oncol. 2019;8:236‐242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wang Q, Berger NA, Xu R. Analyses of risk, racial disparity, and outcomes among US patients with cancer and COVID‐19 infection. JAMA Oncol. 2021;7:220‐222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fronstin P, Woodbury SA. How many Americans have lost jobs with employer health coverage during the pandemic?. Commonwealth Fund. Published October 7, 2020. https://www.commonwealthfund.org/publications/issue‐briefs/2020/oct/how‐many‐lost‐jobs‐employer‐coverage‐pandemic. Accessed January 06, 2021. [Google Scholar]
- 16. Staehler MD, Battle DJ, Bergerot CD, Pal SK, Penson DF. COVID‐19 and financial toxicity in patients with renal cell carcinoma. World J Urol. Published online October 22, 2020. doi: 10.1007/s00345-020-03476-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Baddour K, Kudrick LD, Neopaney A, et al. Potential impact of the COVID‐19 pandemic on financial toxicity in cancer survivors. Head Neck. 2020;42:1332‐1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kong YC, Sakti VV, Sullivan R, Bhoo‐Pathy N. Cancer and COVID‐19: economic impact on households in Southeast Asia. Ecancermedicalscience. 2020;14:1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Contingent and alternative employment arrangements. US Bureau of Labor Statistics. Published June 7, 2018. https://www.bls.gov/news.release/pdf/conemp.pdf. Accessed January 06, 2021. [Google Scholar]
- 20. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377‐381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. de Souza JA, Yap BJ, Hlubocky FJ, et al. The development of a financial toxicity patient‐reported outcome in cancer: the COST measure. Cancer. 2014;120:3245‐3253. [DOI] [PubMed] [Google Scholar]
- 22. Esselen KM, Gompers A, Hacker MR, et al. Evaluating meaningful levels of financial toxicity in gynecologic cancers. Int J Gynecol Cancer. 2021;31:801‐806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kim JH. Multicollinearity and misleading statistical results. Korean J Anesthesiol. 2019;72:558‐569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Smith GL, Lopez‐Olivo MA, Advani PG, et al. Financial burdens of cancer treatment: a systematic review of risk factors and outcomes. J Natl Compr Canc Netw. 2019;17:1184‐1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Thom B, Benedict C, Friedman DN, Kelvin JF. The intersection of financial toxicity and family building in young adult cancer survivors. Cancer. 2018;124:3284‐3289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hoeve M, Stams GJ, van der Zouwen M, Vergeer M, Jurrius K, Asscher JJ. A systematic review of financial debt in adolescents and young adults: prevalence, correlates and associations with crime. PLoS One. 2014;9:e104909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gupta SK, Mazza MC, Hoyt MA, Revenson TA. The experience of financial stress among emerging adult cancer survivors. J Psychosoc Oncol. 2020;38:435‐448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Macpherson CF, Johnson RH, Landwehr MS, Watson SE, Stegenga K. “Aftermath”: financial resource requirements of young adults moving forward after cancer treatment. J Adolesc Young Adult Oncol. 2020;9:354‐358. [DOI] [PubMed] [Google Scholar]
- 29. Guy GP Jr, Ekwueme DU, Yabroff KR, et al. Economic burden of cancer survivorship among adults in the United States. J Clin Oncol. 2013;31:3749‐3757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Parsons HM, Harlan LC, Lynch CF, et al. Impact of cancer on work and education among adolescent and young adult cancer survivors. J Clin Oncol. 2012;30:2393‐2400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Simpson SH, Eurich DT, Majumdar SR, et al. A meta‐analysis of the association between adherence to drug therapy and mortality. BMJ. 2006;333:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Suh E, Stratton KL, Leisenring WM, et al. Late mortality and chronic health conditions in long‐term survivors of early‐adolescent and young adult cancers: a retrospective cohort analysis from the Childhood Cancer Survivor Study. Lancet Oncol. 2020;21:421‐435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chao C, Bhatia S, Xu L, et al. Chronic comorbidities among survivors of adolescent and young adult cancer. J Clin Oncol. 2020;38:3161‐3174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Parsons HM, Schmidt S, Harlan LC, et al. Young and uninsured: insurance patterns of recently diagnosed adolescent and young adult cancer survivors in the AYA HOPE study. Cancer. 2014;120:2352‐2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Luo L, Fu M, Li Y, et al. The potential association between common comorbidities and severity and mortality of coronavirus disease 2019: a pooled analysis. Clin Cardiol. 2020;43:1478‐1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Nystad W, Hjellvik V, Larsen IK, et al. Underlying conditions in adults with COVID‐19. Tidsskr Nor Laegeforen. 2020;140:20.0512. [DOI] [PubMed] [Google Scholar]
- 37. Shim S, Kang D, Bae KR, et al. Association between cancer stigma and job loss among cancer survivors. Psychooncology. Published April 5, 2021. doi: 10.1002/pon.5690 [DOI] [PubMed] [Google Scholar]
- 38. Verbruggen LC, Wang Y, Armenian SH, et al. Guidance regarding COVID‐19 for survivors of childhood, adolescent, and young adult cancer: a statement from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Pediatr Blood Cancer. 2020;67:e28702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Galea S, Merchant RM, Lurie N. The mental health consequences of COVID‐19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. 2020;180:817‐818. [DOI] [PubMed] [Google Scholar]
- 40. Hanghøj S, Pappot N, Hjerming M, Taarnhøj GA, Boisen KA, Pappot H. Experiences of social isolation during the COVID‐19 lockdown among adolescents and young adult cancer patients and survivors. J Adolesc Young Adult Oncol. 2021;10:142‐147. [DOI] [PubMed] [Google Scholar]
- 41. Ng DWL, Chan FHF, Barry TJ, et al. Psychological distress during the 2019 coronavirus disease (COVID‐19) pandemic among cancer survivors and healthy controls. Psychooncology. 2020;29:1380‐1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Košir U, Loades M, Wild J, et al. The impact of COVID‐19 on the cancer care of adolescents and young adults and their well‐being: results from an online survey conducted in the early stages of the pandemic. Cancer. 2020;126:4414‐4422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Shaverdian N, Gillespie EF, Cha E, et al. Impact of telemedicine on patient satisfaction and perceptions of care quality in radiation oncology. J Natl Compr Canc Netw. Published online January 4, 2021. doi: 10.6004/jnccn.2020.7687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Hasson SP, Waissengrin B, Shachar E, et al. Rapid implementation of telemedicine during the COVID‐19 pandemic: perspectives and preferences of patients with cancer. Oncologist. 2021;26:e679‐e685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Kenney LB, Vrooman LM, Lind ED, et al. Virtual visits as long‐term follow‐up care for childhood cancer survivors: patient and provider satisfaction during the COVID‐19 pandemic. Pediatr Blood Cancer. 2021;68:e28927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Demographics of internet and home broadband usage in the United States. Pew Research Center. https://www.pewresearch.org/internet/fact‐sheet/internet‐broadband/. Accessed January 06, 2021. [Google Scholar]
- 47. Samuels‐Kalow M, Jaffe T, Zachrison K. Digital disparities: designing telemedicine systems with a health equity aim. Emerg Med J. 2021;38:474‐476. [DOI] [PubMed] [Google Scholar]
- 48. Financial advocacy during a pandemic. Association of Community Cancer Centers. Published August 21, 2020. https://www.accc‐cancer.org/acccbuzz/blog‐post‐template/accc‐buzz/2020/08/21/financial‐advocacy‐during‐a‐pandemic. Accessed January 06, 2021. [Google Scholar]
- 49. COVID‐19 financial resources for people with cancer. Cancer.Net. https://www.cancer.net/navigating‐cancer‐care/financial‐considerations/covid‐19‐financial‐resources‐people‐with‐cancer. Accessed January 06, 2021. [Google Scholar]
- 50. Pannier ST, Warner EL, Fowler B, Fair D, Salmon SK, Kirchhoff AC. Age‐specific patient navigation preferences among adolescents and young adults with cancer. J Cancer Educ. 2019;34:242‐251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kircher SM, Yarber J, Rutsohn J, et al. Piloting a financial counseling intervention for patients with cancer receiving chemotherapy. J Oncol Pract. 2019;15:e202‐e210. [DOI] [PubMed] [Google Scholar]
- 52. Shankaran V, Leahy T, Steelquist J, et al. Pilot feasibility study of an oncology financial navigation program. J Oncol Pract. 2018;14:e122‐e129. [DOI] [PubMed] [Google Scholar]
- 53. Sherman D, Fessele KL. Financial support models: a case for use of financial navigators in the oncology setting. Clin J Oncol Nurs. 2019;23:14‐18. [DOI] [PubMed] [Google Scholar]
- 54. Ikeda T, Igarashi A, Odani S, Murakami M, Tabuchi T. Health‐related quality of life during COVID‐19 pandemic: assessing impacts of job loss and financial support programs in Japan. Appl Res Qual Life. Published online January 30, 2021. doi: 10.1007/s11482-021-09918-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Benedict C, Hahn AL, Diefenbach MA, Ford JS. Recruitment via social media: advantages and potential biases. Digit Health. 2019;5:2055207619867223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lee YJ, Arida JA, Donovan HS. The application of crowdsourcing approaches to cancer research: a systematic review. Cancer Med. 2017;6:2595‐2605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Esselen KM, Stack‐Dunnbier H, Gompers A, Hacker MR. Crowdsourcing to measure financial toxicity in gynecologic oncology. Gynecol Oncol. 2021;161:595‐600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Education pays: earnings and unemployment rates by educational attainment, 2020. US Bureau of Labor Statistics. Published April 21, 2021. https://www.bls.gov/emp/chart‐unemployment‐earnings‐education.htm. Accessed January 06, 2021. [Google Scholar]
- 59. Robbins MA, Awosogba OOR, Knox‐Rice TK. Cancer, COVID‐19, and the Black community. J Psychosoc Oncol. 2021;39:305‐308. [DOI] [PubMed] [Google Scholar]
- 60. Poulson M, Neufeld M, Geary A, et al. Intersectional disparities among Hispanic groups in COVID‐19 outcomes. J Immigr Minor Health. 2021;23:4‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Muñoz‐Price LS, Nattinger AB, Rivera F, et al. Racial disparities in incidence and outcomes among patients with COVID‐19. JAMA Netw Open. 2020;3:e2021892. [DOI] [PMC free article] [PubMed] [Google Scholar]


