Abstract
Overnight, as a result of the COVID‐19 pandemic, telehealth rapidly transitioned from limited application to widespread implementation. The field of genetic counseling was well positioned to make this transition to virtual care since there is generally less of a need for patients to be seen in‐person for physical exams or urgent care. Going forward, virtual visits will presumably become a mainstay in the provision of genetic services and it is anticipated that clinics will adopt “hybrid” models with both in‐person and virtual visit options. This commentary highlights the successes and challenges in the rapid implementation of virtual visits, focusing on who has benefited versus who has been challenged or left behind. We also discuss genetic testing considerations, including the additional steps required for patients and clinicians when testing is ordered outside of the clinical setting, which can result in delays or a lack of testing altogether. Future research considerations are presented to address the needs among the most vulnerable and help ensure equitable access and benefit.
Keywords: COVID‐19, disparities, genetic counseling, genetic testing, telegenetics, telehealth, virtual visits
What is known about this topic
Virtual visits were rapidly implemented due to the COVID‐19 pandemic and will presumably be an integral part of genetic counseling practice going forward.
What this paper adds to the topic
This Commentary considers benefits and challenges with virtual visits and presents future research considerations in this area from an equity lens.
1. INTRODUCTION
Overnight, as a result of the COVID‐19 pandemic, telehealth rapidly transitioned from limited application to widespread implementation. In order to comply with stay‐at‐home orders and maintain social distancing, there was a critical need to provide health care to patients in their home settings using telephone or video visits. The field of genetic counseling was well positioned to make this transition to virtual care since there is generally less of a need for patients to be seen in‐person for physical examinations or urgent care. In fact, some genetic counselors had been providing telehealth services for years as part of their work at academic medical centers, outreach clinics, or through positions at commercial genetic counseling and genetic testing companies (Cohen et al., 2019; Du & Becher, 2018; Hilgart et al., 2012; Maiese et al., 2019). Going forward, virtual visits will presumably become a mainstay in provision of genetic services and health care. It is anticipated that clinics will adopt “hybrid” models, offering a combination of both in‐person and virtual care options (Bergstrom et al., 2020; Mahon, 2020; Norman et al., 2020; Pereira et al., 2020).
This commentary highlights the successes and challenges in the rapid implementation of virtual visits, including consideration of who has benefited versus who has been challenged or left behind. Future research considerations are presented from an equity lens. Throughout this commentary, we will use “telehealth” to refer to the remote applications of telephone or videoconferencing in health care and “virtual visits” when specifically referring to videoconferencing visits.
2. PRIOR TELEHEALTH IMPLEMENTATION AND BARRIERS IN PROVISION OF GENETIC SERVICES
Much of the earlier work in expanding the availability of genetic services through telehealth has focused on the effectiveness of telephone counseling (Cohen et al., 2019). Prior trials, mostly in cancer genetics, have demonstrated the extent to which genetic counseling via telephone is non‐inferior to in‐person visits (Bradbury et al., 2018; Kinney et al., 2016). Additionally, studies conducted before the COVID‐19 pandemic have shown strong consensus regarding the benefits of video visits and consideration as a viable alternative to in‐person care. These benefits generally include overcoming geographic distances, reduced costs and travel time, greater convenience, and high patient satisfaction (Gorrie et al., 2021; Hilgart et al., 2012; see also Table 1). Video visits also overcome several inherent limitations of telephone counseling—namely, having the opportunity to see and respond to visual cues and the option to utilize visual counseling aids during the session. Yet prior to COVID‐19, genetic counseling, like many other medical specialties, had limited use of videoconferencing for patient care. The National Society of Genetic Counselors’ 2020 Professional Status Survey found that among respondents who provided direct patient care and used only one service delivery model, just 8% used telephone, and 1% audiovisual (NSGC Professional Status Survey: Service Delivery & Access, 2020a). Use of these modalities for genetic counseling seems to be more prevalent in industry and other non‐clinical settings (Terry et al., 2018).
TABLE 1.
Benefits and challenges of virtual visits for patients
| Virtual visits benefit patients who have… |
|
Transportation issues due to:
|
|
Significant health issues:
|
|
Work issues:
|
|
Childcare, eldercare, or relative care issues:
|
|
School/Sports/Extracurricular Activities:
|
|
Family members in different locations:
|
| Virtual visits challenge patients who have… |
|
Technological device issues:
|
|
Internet access and connectivity issues:
|
|
Video quality issues:
|
|
Distractions:
|
|
Emotional support needs:
|
|
Privacy concerns:
|
|
Inability to complete the additional tasks required for a virtual visit:
|
Table content based on clinical experience, and some appears in table in Mahon (2020).
The limited use of videoconferencing in genetic counseling, and health care in general, had been due to financial costs of platforms and equipment, insurance coverage, logistical issues, and uncertainty regarding its efficacy relative to in‐person care. Many healthcare systems lacked the necessary equipment and infrastructure for video visits (Zierhut et al., 2018). Moreover, both the patient and the healthcare provider were generally required to be at sites with specific encrypted HIPAA‐compliant equipment for use, with additional trained support staff at the remote sites (Greenberg et al., 2020; Mahon, 2020). Limitations in billing and reimbursement have also been among the most commonly cited barriers to widescale implementation of video visits (Zierhut et al., 2018). While policies have been previously implemented at the state level to promote equivalent coverage and reimbursement for telehealth services by commercial payers, these policies varied substantially from state to state (Lacktman et al., 2021) and were largely not in place at the federal level for Medicare and Medicaid beneficiaries.
3. TELEHEALTH IN THE ERA OF COVID‐19
Rapid and widescale implementation of telehealth during the COVID‐19 pandemic was largely made possible by technological solutions, the relaxation of existing telehealth restrictions to allow use of HIPAA non‐compliant platforms, and temporary equivalent reimbursement for video visits and in‐person visits for the duration of the public health emergency (Centers for Medicaid & Medicare Services, 2020; Contreras et al., 2020; Ortega et al., 2020). Some states even relaxed licensure laws, allowing care of patients outside of state boundaries (Pereira et al., 2020). These changes made it possible to rapidly implement virtual visits at home for both patients and clinicians, using a home computer, tablet, or smartphone.
The implementation of virtual visits in diverse genetic and medical settings has demonstrated feasibility and acceptability (Bergstrom et al., 2020; Jeganathan et al., 2020; Madden et al., 2020; Pereira et al., 2020). For example, genetic counselors surveyed in New York City reported being satisfied with providing telehealth services through video (93.1%) and telephone (81.4%) modalities, though 68.6% indicated that they would prefer that the majority of patients be seen in‐person post‐COVID‐19 (Bergstrom et al., 2020). In another study, all patient respondents were willing to use videoconferencing again, and about half reported that they preferred video visits over traveling to an appointment (Pereira et al., 2020).
Virtual visits have also allowed extended family members to be seen simultaneously or simply to be present virtually to support the patient. This would not have been possible in‐person during COVID‐19 given clinic restrictions limiting the number of people who may accompany the patient. Furthermore, virtual visits allow for visual cues which otherwise would be lacking during in‐person visits due to masking of patients and providers.
Other benefits associated with conducting a clinic visit virtually have been reported. For pediatric patients and individuals with special needs, being seen in their home environment allows clinicians the opportunity to observe them in a place where they are comfortable, and potentially better assess their level of functioning (Pereira et al., 2020). Being at home may also lessen patients’ anxiety around the clinic visit and provide more time for decision‐making, without being preoccupied by a blood draw or prenatal procedure following the genetic counseling session (Ahimaz et al., 2021; Pereira et al., 2020). Seeing patients virtually has also led to a greater use of saliva kits for genetic testing (Ahimaz et al., 2021; Mahon, 2020; Shannon et al., 2020) in place of a blood draw, which also benefits patients who might otherwise decline genetic testing due to fear of needles.
Finally, studies have also begun to highlight potential system‐level benefits of virtual visits during the pandemic, with decreased waiting time for an appointment (Ahimaz et al., 2021), lower no show rates, and fewer cancelations (Ahimaz et al., 2021; Jeganathan et al., 2020; Shur et al., 2020). These differences will very likely result in cost savings, as demonstrated previously with the implementation of videoconferencing in cancer genetic counseling (Buchanan et al., 2015). Virtual visits can potentially decrease costs for patients (e.g., no costs for travel or childcare, less time off work needed), clinicians (no travel costs, especially to outreach clinics which can be hours away), and insurers (if covering patient's travel costs). In addition, for clinics in which clinician availability exceeds the number of available rooms, the ability to see patients virtually can allow more patients to be scheduled and enable urgent patients to be more easily accommodated. Furthermore, the use of virtual visits for disclosure of genetic test results can enhance communication by allowing the clinician to pick‐up on nonverbal communication and body language, which is not possible by phone. Virtual result disclosures are potentially billable and use can also free up rooms in clinic if the results would otherwise have been disclosed in person.
Notably, several challenges have also been observed with virtual visits (Ahimaz et al., 2021; see Table 1). Aside from the obvious technological challenges of accessing and learning how to use videoconferencing technology (see next section), our genetics clinics and others have experienced challenges with genetic testing since patients cannot readily provide a sample and documentation of informed consent (Ahimaz et al., 2021; Bergstrom et al., 2020). Multiple steps are now required for form completion and sample collection by saliva or buccal swab kit or making arrangements if a blood sample is required (see Figure 1). While informed consent and other forms can be e‐signed by the patient, provided the patient has the computer capabilities and understands what is needed, this involves multiple steps including the clinician/clinical staff accessing the form and filling in patient identifiers (in clinic, a pre‐printed label would be used), obtaining the patient's email address, the clinician e‐signing after the patient returns the form and the loading of the form in the lab's portal and the patient's electronic medical records. Ahimaz et al. (2021) note that for some of their patients, even locating a shipping location/drop off box for sample return requires assistance.
FIGURE 1.
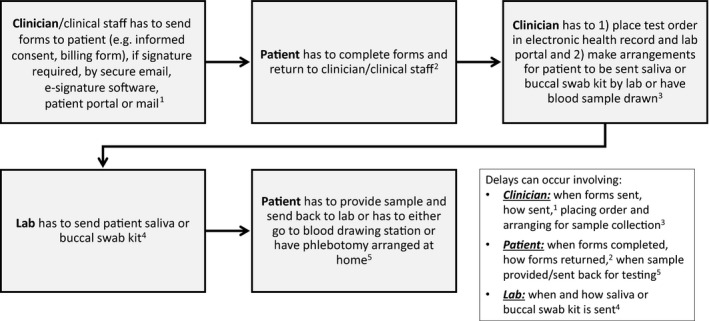
Genetic testing logistics and sources of delay following a virtual visit
Based on our own clinical experiences and others, these added steps for the patient have led to testing delays, and in some cases, a lack of testing altogether, resulting in lower genetic testing completion overall (Ahimaz et al., 2021; Norman et al., 2020; Shannon et al., 2020). Moreover, when an insufficient saliva or buccal swab sample is obtained, the process needs to be repeated, further delaying results, and potentially impacting patient care. Managing these genetic testing logistics impacts clinic efficiency, as genetic counselors and other clinic staff must dedicate more time to track and ensure that all steps (Figure 1) are completed.
Finally, virtual visits may simply not be an option for the assessment of certain genetic or medical conditions. A very limited physical examination may be conducted through videoconferencing, by instructing the patient to show various parts of their body to the camera. Therefore, depending on diagnostic considerations, a virtual visit may not be feasible if a more complete and in‐person physical examination is needed.
4. INEQUITIES IN ACCESS AND CARE WITH VIRTUAL VISITS
Evidence regarding potential inequities in access to genetic services and health care during the pandemic is emerging, raising concerns about the magnification and worsening of disparities for those most vulnerable. Changes in payer mix in genetics clinics and primary care practices have been observed, with a decrease in patients with Medicaid and Medicare insurance, as well as a decrease in non‐English speaking patients seen (Nouri et al., 2020; Pereira et al., 2020). These changes suggest disparities in access to virtual health care with patients of lower socioeconomic backgrounds and non‐English speaking patients being most impacted. Pereira et al. (2020) found that even with bilingual staff, patients who were older or mainly Spanish‐speaking had trouble accessing remote services or were unable to connect at all; several Spanish‐speaking patients opted to wait for in‐person visits.
When a patient cannot be seen virtually and/or has to wait to be seen in‐person, this delays their access to genetic testing and potentially to results that could impact their care. Furthermore, for patients who have limited education or are non‐English speaking, access to genetic testing may be limited by their understanding and ability to complete genetic testing forms and specimen collection via a saliva kit or buccal swab. Prior research by Butrick et al. (2015) demonstrated a lower uptake of genetic testing among minorities receiving genetic counseling by telephone compared with in‐person counseling, but not among whites who participated in the study. This raised questions regarding the additional barriers to accessing testing among minorities in the telephone study arm (Butrick et al., 2015).
Inequities between patient populations are also observed through the lens of technology, with variability in both access to and usage of the technology required for a successful virtual visit. Patients must have access to both a device with audiovisual capabilities and a high‐speed Internet connection, so those lacking either are clearly disadvantaged. About 26% of US adults do not have a desktop or laptop computer, 48% do not have a tablet, and 19% do not have a smartphone (Pew Research Center, 2019a). Furthermore, about 10% of US adults indicate that they do not use the Internet, for various reasons, with even higher proportions among certain demographic groups (Pew Research Center, 2019b). Variability in Internet access may also impact the quality of care patients receive. About 27% of US adults indicate that they do not have a home broadband connection, which is consistent with a growing proportion of Americans who are “smartphone‐dependent,” relying solely on cellular data for their Internet needs (Pew Research Center, 2019b). Smartphone dependency is particularly prevalent among Blacks (23%) and Hispanics (25%), compared to Whites (12%) (Pew Research Center, 2019b). These patients may be more likely to attend virtual visits on mobile devices with smaller screens, and perhaps outside of their home settings, likely diminishing the overall quality of the visit. Lower technology literacy is also a barrier for some patients, including older adults (Kurlander et al., 2019), with a decreased ability to effectively utilize videoconferencing technology. Taken together, these findings suggest a striking digital divide, in which certain patient populations are less able to take advantage of telehealth services than others.
5. GOING FORWARD
The long‐term integration and accessibility of virtual visits in health care will require that relaxations of telehealth rules and provision of equivalent reimbursement for video and in‐person visits be made permanent (Contreras et al., 2020; Ortega et al., 2020). This equivalent reimbursement should also extend to telephone visits, as video visits may not be an option due to technology access and/or patient preferences.
In efforts to address technology access issues, the Federal Communications Commission launched the Connected Care Pilot Program, the COVID‐19 Telehealth Program, and the Rural Health Care Program. These programs, which include allocation of funds to provide necessary hardware and internet access, are increasing telehealth services for low‐income patients and patients in remote areas. Efforts must also expand to residents of urban, inner city areas who are unable to afford high‐speed Internet (Contreras et al., 2020; Ortega et al., 2020).
For patients who speak a different language, virtual visits make it easier for interpreters to be present since there is no travel to the clinic. However, someone who can interpret and provide assistance will likely also be needed prior to the appointment to help the patient access the virtual visit, and afterward for genetic testing and other tests/evaluations. Pereira et al. (2020) found that even with bilingual staff, there were still challenges. Institutional support for coverage of virtual interpreter services and patient navigators, especially ones who can speak different languages, is needed to help patients access health care virtually and even in‐person.
Recognition of genetic counselors as providers by Medicare with passage of legislation to amend federal law is also needed (Anderson & Terry, 2020; National Society of Genetic Counselors, 2020b). Without recognition, genetic counselors cannot use telehealth with patients who have Medicare insurance due to “incident to” rules requiring direct physician supervision; the physician needs to be present in the same office suite. Both the non‐recognition of genetic counselors as providers and supervision stipulations affect access to genetic services and limit the number of patients each provider can see.
Virtual visits open the door to provide genetic counseling simultaneously to family members in different locations, which enables efficient collection and communication of relevant healthcare information and facilitation of cascade screening. Virtual visits can make participation for family members feasible in different states, or even countries, allowing others to be involved in healthcare decisions. The use of virtual visits, particularly in states with a paucity of providers and/or large geographic distances to clinics, can increase access to genetic services. If state licensure and billing compliance issues could be addressed long term, patients could also have the option to be seen by geneticists with specialized expertise regardless of their geographic location (Pereira et al., 2020).
There are several added steps (Figure 1) and inefficiencies with genetic testing which are adding time for clinicians and decreasing the uptake of genetic testing in patients who could benefit. Genetics clinics and genetic testing laboratories must continue to develop systematic, streamlined approaches to facilitate testing logistics in the virtual setting, including use of non‐clinicians (e.g., genetic counseling assistants, patient navigators). Additionally, genetic testing logistics may be aided by greater availability of mobile phlebotomy services when a blood sample is required, at‐home pick‐up of saliva/buccal kits for patients when return of samples is a barrier and allowing patients to send photographs of signed consent forms (Ahimaz et al., 2021).
Finally, it will be important for genetics clinics to tailor their own hybrid care models moving forward, with approaches that will work best for them and their patient populations. For instance, clinics may develop triaging practices for the different modalities based on clinical indications and patient factors that influence clinical outcomes. They must also advocate to garner continued institutional support and dedicated financial resources to facilitate hybrid care.
6. FUTURE RESEARCH CONSIDERATIONS TO HELP ENSURE EQUITABLE ACCESS AND BENEFIT
Any efforts for the continued adoption of virtual visits or implementation of hybrid care models necessitate examination of clinical outcomes, particularly from a health equity lens. We suggest some research areas for consideration in order to prioritize efforts to assess and address the needs among those most vulnerable.
6.1. Examine the implementation and efficacy of virtual visits and/or hybrid care delivery models, with a focus on differential outcomes by subgroups
Little work has been conducted to date on the efficacy of virtual visits, which may vary across age, race/ethnicity, education, income, language, health literacy, medical conditions, psychological status, and other domains. Future research needs to comprehensively examine outcomes of virtual visits (e.g., care outcomes, perceptions of care, comprehension of information, psychological response) across these factors. More explicitly, research needs to focus on who gets left behind.
6.2. Examine patient preferences for care delivery and whether they can be effectively accommodated under a virtual or hybrid model
Studies need to examine patient preferences for virtual or in‐person care and assess how preferences vary by the factors listed above. Are outcomes of genetic counseling (e.g., perceptions of care quality and satisfaction, decisional conflict/regret, decision outcomes) better if patients receive counseling via their preferred model? How does having multiple family members participate from different locations impact care, decision‐making, outcomes, and patient satisfaction with the visit?
There are also quality of care considerations and unknowns about how rapport‐building, psychosocial counseling, and other aspects of genetic counseling are impacted in a video visit format (Zierhut et al., 2018; Zilliacus et al., 2010), and these need to be examined from both patient and provider perspectives. Even with greater convenience, it cannot be assumed that patients will prefer virtual visits over in‐person visits (Solomons et al., 2018), which raises questions about how best to triage and weigh the many factors that may influence a patient's suitability for one mode of genetics service delivery over another.
6.3. Examine the impact of policies that may inadvertently magnify disparities
Researchers should monitor and evaluate the impact of policies on patient care, which may have implications for access and quality of care delivered (e.g., reimbursement for video but not telephone visits). Considerations for who has greater access to certain technologies but not others will likely reveal aspects of policies that may harm certain subgroups of the population.
6.4. Design and test efforts to address/overcome identified barriers
Future studies should not only focus on identifying barriers to access and care, but also actively work to develop intervention strategies and approaches to overcome these challenges (e.g., addressing barriers to off‐site genetic testing). Considerations for interventions should be across different levels of the socioecological model (Stokols, 1992) to ensure that individual‐level solutions and system‐level solutions are examined. Examples of solutions include culturally targeted and sensitive educational materials (Conley et al., 2021; Henderson et al., 2021), interactive digital programs (Wang et al., 2021), and patient outreach and system navigation efforts (Mays et al., 2012).
7. CONCLUSION
The COVID‐19 pandemic has ushered in a new era of widespread use of telehealth with the ability to see patients in their home settings. Yet this transition has also brought about many new challenges and unanswered questions. While prior work has been instrumental to inform our navigation of the evolving telehealth landscape, there remains a great need for research to identify and address these issues to ensure maximization of benefits. The genetics community is now well‐positioned to reflect upon and share lessons learned in recent months as we consider both the successes to carry forward and the challenges that remain to be addressed. In order to establish best practices for hybrid care models, we must continue to ask the right questions, overcome the most pressing barriers that are driving disparities, and serve as advocates for our patients to ensure equitable access to high‐quality virtual care.
AUTHOR CONTRIBUTIONS
Wendy Uhlmann, Andrew McKeon, and Catharine Wang all made substantial contributions to the conception of the work, wrote and revised content, and provided final approval of the version to be published. All agree to be accountable for all aspects of the paper.
COMPLIANCE WITH ETHICAL STANDARDS
CONFLICT OF INTEREST
Wendy Uhlmann receives book royalties from Wiley‐Blackwell: John Wiley & Sons, Inc. Andrew McKeon and Catharine Wang declare that they have no conflict of interest.
HUMAN STUDIES AND INFORMED CONSENT
No data from human subjects were collected by the authors for this commentary.
ANIMAL STUDIES
No animal studies were carried out by the authors for this commentary.
DATA SHARING AND DATA ACCESSIBILITY
Data sharing is not applicable to this commentary as no datasets were generated or analyzed
Uhlmann, W. R., McKeon, A. J., & Wang, C. (2021). Genetic counseling, virtual visits, and equity in the era of COVID‐19 and beyond. Journal of Genetic Counseling, 30, 1038–1045. 10.1002/jgc4.1469
REFERENCES
- Ahimaz, P., Giordano, J., Disco, M., Harrington, E., Levinson, E., Spiegel, E., Andrews, C., Griffin, E., Hernan, R., & Wynn, J. (2021). COVID contingencies: Early epicenter experiences of different genetics clinics at a New York City institution inform emergency adaptation strategies. Journal of Genetic Counseling. 1–11. 10.1002/jgc4.1409. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson, K., & Terry, S. F. (2020). Please wait for the host to start this meeting: A push for H.R. 3235 amid COVID‐19. Genetic Testing and Molecular Biomarkers, 24(11), 689–691. 10.1089/gtmb.2020.29058.sjt [DOI] [PubMed] [Google Scholar]
- Bergstrom, K. L., Brander, T. E., Breen, K. E., & Naik, H. (2021). Experiences from the epicenter: Professional impact of the COVID‐19 pandemic on genetic counselors in New York. American Journal of Medical Genetics Part C Seminars in Medical Genetics, 187(1), 28–36. 10.1002/ajmg.c.31855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradbury, A. R., Patrick‐Miller, L. J., Egleston, B. L., Hall, M. J., Domchek, S. M., Daly, M. B., Ganschow, P., Grana, G., Olopade, O. I., Fetzer, D., Brandt, A., Chambers, R., Clark, D. F., Forman, A., Gaber, R., Gulden, C., Horte, J., Long, J. M., Lucas, T., … Yao, X. (. S. (2018). Randomized noninferiority trial of telephone vs in‐person disclosure of germline cancer genetic test results. Journal of the National Cancer Institute, 110(9), 985–993. 10.1093/jnci/djy015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchanan, A. H., Datta, S. K., Skinner, C. S., Hollowell, G. P., Beresford, H. F., Freeland, T., Rogers, B., Boling, J., Marcom, P. K., & Adams, M. B. (2015). Randomized trial of telegenetics vs. in‐person cancer genetic counseling: Cost, patient satisfaction and attendance. Journal of Genetic Counseling, 24(6), 961–970. 10.1007/s10897-015-9836-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butrick, M., Kelly, S., Peshkin, B. N., Luta, G., Nusbaum, R., Hooker, G. W., Graves, K., Feeley, L., Isaacs, C., Valdimarsdottir, H. B., Jandorf, L., DeMarco, T., Wood, M., McKinnon, W., Garber, J., McCormick, S. R., & Schwartz, M. D. (2015). Disparities in uptake of BRCA1/2 genetic testing in a randomized trial of telephone counseling. Genetics in Medicine, 17(6), 467–475. 10.1038/gim.2014.125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicaid and Medicare Services (2020). Medicare telemedicine health care provider fact sheet. https://www.cms.gov/newsroom/fact‐sheets/medicare‐telemedicine‐health‐care‐provider‐fact‐sheet [Google Scholar]
- Cohen, S. A., Bradbury, A., Henderson, V., Hoskins, K., Bednar, E., & Arun, B. K. (2019). Genetic counseling and testing in a community setting: Quality, access, and efficiency. American Society of Clinical Oncology Educational Book, 39, e34–e44. 10.1200/EDBK_238937 [DOI] [PubMed] [Google Scholar]
- Conley, C. C., Castro‐Figueroa, E. M., Moreno, L., Dutil, J., García, J. D., Burgos, C., Ricker, C., Kim, J., Graves, K. D., Ashing, K. T., Quinn, G. P., Soliman, H., & Vadaparampil, S. T. (2021). A pilot randomized trial of an educational intervention to increase genetic counseling and genetic testing among Latina breast cancer survivors. Journal of Genetic Counseling, 30(2), 394–405. 10.1002/jgc4.1324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contreras, C. M., Metzger, G. A., Beane, J. D., Dedhia, P. H., Ejaz, A., & Pawlik, T. M. (2020). Telemedicine: Patient‐provider clinical engagement during the COVID‐19 pandemic and beyond. Journal of Gastrointestinal Surgery, 24, 1692–1697. 10.1007/s11605-020-04623-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du, L., & Becher, S. I. (2018). Genetic and genomic consultation: Are we ready for direct‐to‐consumer telegenetics? Frontiers in Genetics, 9, 550. 10.3389/fgene.2018.00550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorrie, A., Gold, J., Cameron, C., Krause, M., & Kincaid, H. (2021). Benefits and limitations of telegenetics: A literature review. Journal of Genetic Counseling, 1–14. 10.1002/jgc4.1418. Online early view only. [DOI] [PubMed] [Google Scholar]
- Greenberg, S. E., Boothe, E., Delaney, C. L., Noss, R., & Cohen, S. A. (2020). Genetic counseling service delivery models in the United States: Assessment of changes in use from 2010 to 2017. Journal of Genetic Counseling, 29(6), 1126–1141. 10.1002/jgc4.1265 [DOI] [PubMed] [Google Scholar]
- Henderson, V., Chukwudozie, I. B., Comer‐Hagans, D., Coffey, V., Grumbach, G., Spencer, S., Rodgers, C., Kaur, R., Newsome, J., Balay, L., Maga, T., Kendall, L., Balthazar, C., Watson, K., Winn, R., Odoms‐Young, A., & Hoskins, K. F. (2021). Development of a culturally sensitive narrative intervention to promote genetic counseling among African American women at risk for hereditary breast cancer. Cancer. 10.1002/cncr.33525. in press. [DOI] [PubMed] [Google Scholar]
- Hilgart, J. S., Hayward, J. A., Coles, B., & Iredale, R. (2012). Telegenetics: A systematic review of telemedicine in genetics services. Genetics in Medicine, 14(9), 765–776. 10.1038/gim.2012.40 [DOI] [PubMed] [Google Scholar]
- Jeganathan, S., Prasannan, L., Blitz, M. J., Vohra, N., Rochelson, B., & Meirowitz, N. (2020). Adherence and acceptability of telehealth appointments for high‐risk obstetrical patients during the coronavirus disease 2019 pandemic. American Journal of Obstetrics and Gynecology MFM, 2(4 Suppl.), 1–9. 10.1016/j.ajogmf.2020.100233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinney, A. Y., Steffen, L. E., Brumbach, B. H., Kohlmann, W., Du, R., Lee, J. H., Gammon, A., Butler, K., Buys, S. S., Stroup, A. M., Campo, R. A., Flores, K. G., Mandelblatt, J. S., & Schwartz, M. D. (2016). Randomized noninferiority trial of telephone delivery of BRCA1/2 genetic counseling compared with in‐person counseling: 1‐year follow‐up. Journal of Clinical Oncology, 34(24), 2914–2924. 10.1200/JCO.2015.65.9557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurlander, J., Kullgren, J., Singer, D., Solway, E., Malani, P., Kirch, M., & Saini, S. (2019). Virtual visits: Telehealth and older adults. University of Michigan National Poll on Healthy Aging. http://hdl.handle.net/2027.42/151376 [Google Scholar]
- Lacktman, N. M., Acosta, J. N., Iacomini, S. J., & Levine, S. J. (2021). 50‐state survey of telehealth commercial insurance laws. https://www.foley.com/‐/media/files/insights/publications/2021/02/21mc30431‐50state‐telemed‐reportmaster‐02082021.pdf [Google Scholar]
- Madden, N., Emeruwa, U. N., Friedman, A. M., Aubey, J. J., Aziz, A., Baptiste, C. D., Coletta, J. M., D’Alton, M. E., Fuchs, K. M., Goffman, D., Gyamfi‐Bannerman, C., Kondragunta, S., Krenitsky, N., Miller, R. S., Nhan‐Chang, C., Saint Jean, A. M., Shukla, H. P., Simpson, L. L., Spiegel, E. S., … Ona, S. (2020). Telehealth uptake into prenatal care and provider attitudes during the COVID‐19 pandemic in New York City: A quantitative and qualitative analysis. American Journal of Perinatology, 37, 1005–1014. 10.1055/s-0040-1712939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahon, S. M. (2020). Telegenetics. Clinical Journal of Oncology Nursing, 24(3), 244–248. 10.1188/20.CJON.244-248 [DOI] [PubMed] [Google Scholar]
- Maiese, D., Keehn, A., Lyon, M., Flannery, D., & Watson, M. (2019). Current conditions in medical genetics practice. Genetics in Medicine, 21, 1–4. 10.1038/s41436-018-0417-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mays, D., Sharff, M. E., DeMarco, T. A., Williams, B., Beck, B., Sheppard, V. B., Peshkin, B. N., Eng‐Wong, J., & Tercyak, K. P. (2012). Outcomes of a systems‐level intervention offering breast cancer risk assessments to low‐income underserved women. Familial Cancer, 11(3), 493–502. 10.1007/s10689-012-9541-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Society of Genetic Counselors (2020a). NSGC Professional Status Survey: Service Delivery & Access (2020) (p. 15). nsgc.org [members only access]. [Google Scholar]
- National Society of Genetic Counselors (2020b). Pandemic issue brief: Action needed to ensure Medicare beneficiary access to life saving genetic services in COVID‐19 pandemic. https://www.nsgc.org/page/h.r.‐7083‐documents‐to‐support‐advocacy [Google Scholar]
- Norman, M. L., Malcolmson, J., Armel, S. R., Gillies, B., Ou, B., Thain, E., McCuaig, J. M., & Kim, R. H. (2020). Stay at home: implementation and impact of virtualizing cancer genetic services during COVID‐19. Journal of Medical Genetics. Published Online First: 16 October 2020. 10.1136/jmedgenet-2020-107418. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Nouri, S., Khoong, E. C., Lyles, C. R., & Karliner, L. (2020). Addressing equity in telemedicine for chronic disease management during the COVID‐19 pandemic. New England Journal of Medicine Catalyst. 10.1056/CAT.20.0123 [DOI] [Google Scholar]
- Ortega, G., Rodriguez, J. A., Maurer, L. R., Witt, E. E., Perez, N., Reich, A., & Bates, D. W. (2020). Telemedicine, COVID‐19, and disparities: Policy implications. Health Policy and Technology, 9, 368–371. 10.1016/j.hlpt.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira, E. M., Ahimaz, P., Andrews, C., Anyane‐Yeboa, K., Arsov, T., Berger, S. M., Chilton, I., Cory, D. M., Chung, W. K., Dergham, K. R., Disco, M. M., Ernst, M. E., Forman, T., Galloway, S., Geltzeiler, A. R., Giordano, J. L., Griffin, E., Guzman, E., Harkavy, N., … Chung, W. K. (2020). COVID‐19’s impact on genetics at one medical center in New York. Genetics in Medicine, 22, 1467–1469. 10.1038/s41436-020-0857-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center (2019a). Mobile Fact Sheet. https://www.pewresearch.org/internet/fact‐sheet/mobile/ [Google Scholar]
- Pew Research Center (2019b). Internet/Broadband Fact Sheet. https://www.pewresearch.org/internet/fact‐sheet/internet‐broadband/ [Google Scholar]
- Shannon, K. M., Emmet, M. M., Rodgers, L. H., Wooters, M., & Seidel, M. L. (2020). Transition to telephone genetic counseling services during the COVID‐19 pandemic. Journal of Genetic Counseling, 1–5. 10.1002/jgc4.1365. Currently online in early view. [DOI] [PubMed] [Google Scholar]
- Shur, N., Atabaki, S. M., Kisling, M. S., Tabarani, A., Williams, C., Fraser, J. L., Regier, D. S., & Summar, M. (2020). Rapid deployment of a telemedicine care model for genetics and metabolism during COVID‐19. American Journal of Medical Genetics, 185A, 68–72. 10.1002/ajmg.a.61911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomons, N. M., Lamb, A. E., Lucas, F. L., McDonald, E. F., & Miesfeldt, S. (2018). Examination of the patient‐focused impact of cancer telegenetics among a rural population: Comparison with traditional in‐person services. Telemedicine Journal and e‐Health, 24(2), 130–138. 10.1089/tmj.2017.0073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokols, D. (1992). Establishing and maintaining healthy environments. Toward a social ecology of health promotion. American Psychologist, 47, 6–22. 10.1037//0003-066x.47.1.6 [DOI] [PubMed] [Google Scholar]
- Terry, A. B., Wylie, A., Raspa, M., Vogel, B., Sanghavi, K., Djurdjinovic, L., Caggana, M., & Bodurtha, J. (2018). Clinical models of telehealth in genetics: A regional telegenetics landscape. Journal of Genetic Counseling, 28(3), 673–691. 10.1002/jgc4.1088 [DOI] [PubMed] [Google Scholar]
- Wang, C., Paasche‐Orlow, M. K., Bowen, D. J., Cabral, H., Winter, M. R., Norkunas Cunningham, T., Trevino‐Talbot, M., Toledo, D. M., Cortes, D. E., Campion, M., & Bickmore, T. (2021). Utility of a virtual counselor (VICKY) to collect family health histories among vulnerable patient populations: A randomized controlled trial. Patient Education and Counseling, 104(5), 979–988. 10.1016/j.pec.2021.02.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zierhut, H. A., MacFarlane, I. M., Ahmed, Z., & Davies, J. (2018). Genetic counselors’ experiences and interest in telegenetics and remote counseling. Journal of Genetic Counseling, 27(2), 329–338. 10.1007/s10897-017-0200-x [DOI] [PubMed] [Google Scholar]
- Zilliacus, E., Meiser, B., Lobb, E., Dudding, T. E., Barlow‐Stewart, K., & Tucker, K. (2010). The virtual consultation: Practitioners’ experiences of genetic counseling by videoconferencing in Australia. Telemedicine Journal and e‐Health, 16(3), 350–357. 10.1089/tmj.2009.0108 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this commentary as no datasets were generated or analyzed


