Abstract
Introduction
Little is known about the relationship between moral distress and mental health problems. We examined moral distress in 2579 frontline healthcare workers (FHCWs) caring for coronavirus disease 2019 (COVID‐19) patients during the height of the spring 2020 pandemic surge in New York City. The goals of the study were to identify common dimensions of COVID‐19 moral distress; and to examine the relationship between moral distress, and positive screen for COVID‐19‐related posttraumatic stress disorder (PTSD) symptoms, burnout, and work and interpersonal functional difficulties.
Method
Data were collected in spring 2020, through an anonymous survey delivered to a purposively‐selected sample of 6026 FHCWs at Mount Sinai Hospital; 2579 endorsed treating COVID‐19 patients and provided complete survey responses. Physicians, house staff, nurses, physician assistants, social workers, chaplains, and clinical dietitians comprised the sample.
Results
The majority of the sample (52.7%–87.8%) endorsed moral distress. Factor analyses revealed three dimensions of COVID‐19 moral distress: negative impact on family, fear of infecting others, and work‐related concerns. All three factors were significantly associated with severity and positive screen for COVID‐19‐related PTSD symptoms, burnout, and work and interpersonal difficulties. Relative importance analyses revealed that concerns about work competencies and personal relationships were most strongly related to all outcomes.
Conclusion
Moral distress is prevalent in FHCWs and includes family‐, infection‐, and work‐related concerns. Prevention and treatment efforts to address moral distress during the acute phase of potentially morally injurious events may help mitigate risk for PTSD, burnout, and functional difficulties.
Keywords: burnout, COVID‐19, functioning, mental health, moral distress, PTSD
1. INTRODUCTION
Moral distress, characterized by feelings such as guilt and worry, can result from living through traumatic or highly stressful events that violate one's deeply held morals and values, (Williams et al., 2020) such as experiences where one is constrained from doing what one believes is right (e.g,. when factors prevent healthcare workers from providing proper care; Jameton, 1984, 2017). While moral distress may be transient and resolves on its own, researchers have proposed that it may evolve into moral injury (Čartolovni et al., 2021; Epstein & Hamric, 2009; Williams et al., 2020) which is characterized by persistent psychological, existential and/or spiritual pain resulting from the values violation (Griffin et al., 2019; Litz et al., 2009). Moral injury is associated with mental health problems, including posttraumatic stress disorder (PTSD) and suicidal ideation (Bryan et al., 2013; Griffin et al., 2019; Litz et al., 2009).
Among healthcare workers, moral distress has been associated with concurrent feelings of burnout, low job satisfaction, sleep problems and intent to resign from one's job (Fumis et al., 2017; Hines et al., 2020; Lamiani et al., 2017; Rittenmeyer & Huffman, 2009). However, little is known about the relationship between moral distress at the time that a potentially morally injurious event is unfolding and concurrent mental health problems such as PTSD symptoms or work/family functioning (Čartolovni et al., 2021). Characterization of the prevalence and correlates of moral distress at the time of the event is critical to elucidating its role in shaping risk for mental health outcomes and for potentially preventing longer term problems (Hines et al., 2021).
Studying frontline healthcare workers (FHCWs) during a coronavirus disease 2019 (COVID‐19) surge offers an opportunity to learn more about moral distress as potentially morally injurious events are unfolding (Huang et al., in press; Lu et al., 2020; Pereira‐Sanchez et al., 2020; Shanafelt et al., 2020; Shechter et al., 2020). Commentaries and surveys suggest that moral distress and moral injury are common during the pandemic, particularly among FHCWs treating COVID‐19 patients (Borges et al., 2020; Haller et al., 2020; Maguen & Price, 2020; Miljeteig et al., 2021). An exemplar of this was the pandemic surge in New York City in the spring of 2020, the first surge in the U.S. when little was known about the virus. Many FHCWs faced unprecedented levels of death and dying, with few tools available to help them feel like they could “do enough” to help patients. Some witnessed patients dying in isolation away from loved ones, which may have violated values about rituals around death and dying (Watson et al., 2020). Some were reassigned to work outside of their specialty areas where they may have felt like they did not have adequate training or experience (Watson et al., 2020). Some had to prioritize which patients got potentially life‐saving resources or had to make life and death decisions (Truog et al., 2020). FHCWs had to navigate caring for their families while fulfilling their professional duties. Some worried about infecting family members, loved ones, colleagues, or even patients. Across these difficult situations, FHCWs may have been constrained by circumstance from doing what they believed was right and may have had to take actions that went against deeply held values or had to make choices (e.g., between family and work) that forced them to violate one set of values to honor another. Such situations are ripe for possible moral distress (Jameton, 2017).
Researchers who study moral distress have noted the need for better understanding of mental health correlates in healthcare workers in general (Lamiani et al., 2017) and specific to COVID‐19 (Haller et al., 2020). In the current study, we examined moral distress in a sample of 2579 FHCWs treating COVID‐19 patients in a large medical center in Manhattan during the height of the spring 2020 surge in New York City. We queried distress in the form of worries about events presumed to be potentially morally distressing for FHCWs during the pandemic surge. The specific aims were to (1) characterize the prevalence of moral distress among FHCWs; (2) identify common dimensions of COVID‐19 moral distress; and (3) examine the relationship between moral distress, and severity and positive screen for COVID‐19‐related PTSD, burnout, and work and interpersonal difficulties.
2. METHODS
2.1. Sample
Data were collected between April 14th and May 11th, 2020, during the peak of COVID‐19 cases, through an anonymous survey delivered via email to a purposively‐selected sample of 6026 FHCWs at the Mount Sinai Hospital, an urban tertiary care hospital in Manhattan, New York. Of those invited to participate, 3360 (55.8%) completed the survey and 2579 (76.8%) endorsed directly treating patients with COVID‐19 and provided sufficient responses to outcome variables. Physician‐level faculty, house staff, nurses, physician assistants, chaplains, social workers, and clinical dietitians comprised the sample. Survey participants were eligible to receive a $25 gift card for completing the survey. The study was approved by the Institutional Review Board at the Icahn School of Medicine at Mount Sinai.
2.2. Assessments
Moral distress in COVID‐19 healthcare workers: A multi‐disciplinary research team consisting of psychiatrists, clinical psychologists, internists, and experts in medical education developed items to assess 23 worries and concerns that FHCWs might encounter during the pandemic. Eleven of these items reflected potentially morally distressing circumstances that FHCWs might encounter while treating COVID‐19 patients, as they asked about potentially morally injurious events (i.e., situations where some may need to engage in, fail to prevent, or witness acts that go against deeply held values or beliefs; e.g., Griffin et al., 2019; Litz et al., 2009); see Table 1. The items queried moral distress in the form of worries (Williams et al., 2020) about work‐related situations, such as having to make difficult decisions in prioritizing COVID‐19 patients; family‐related situations such as worry about the effects of working with COVID‐19 patients on relationships with loved ones, and worries about potentially infecting others.
Table 1.
Prevalence and factor loadings of COVID‐19 moral distress items
| Prevalence, n (%) a | Family‐related items | Infection‐related items | Work‐related items | |
|---|---|---|---|---|
| Feel torn between desire/duty to help patients versus loved ones (family, friends, etc) | 1650 (64.0%) | 0.761 | 0.059 | 0.159 |
| Worry about how COVID‐19 might affect ability to care for children/dependents | 1371 (53.2%) | 0.752 | 0.094 | 0.091 |
| Feel that those with whom you live are fearful to be near you due to possible COVID‐19 exposure at work | 1360 (52.7%) | 0.738 | 0.11 | 0.087 |
| Worry about infecting family with COVID‐19 | 2265 (87.8%) | 0.566 | 0.476 | 0.169 |
| Worry about how COVID‐19 will affect personal relationships | 1778 (68.9%) | 0.477 | 0.294 | 0.289 |
| Worry about not being able to visit or assist loved ones who are ill or become ill with COVID‐19 | 2159 (83.7%) | 0.435 | 0.404 | 0.333 |
| Worry about infecting patients with COVID‐19 | 1814 (70.3%) | 0.115 | 0.911 | 0.213 |
| Worry about infecting colleagues with COVID‐19 | 1902 (73.7%) | 0.164 | 0.904 | 0.242 |
| Worry about not being able to do enough for COVID‐19 patients | 2116 (82.0%) | 0.112 | 0.176 | 0.854 |
| Worry about not having enough knowledge or experience to take adequate care of COVID‐19 patients | 1885 (73.1%) | 0.118 | 0.154 | 0.832 |
| Worry about having to make extremely difficult decisions involving prioritizing health/survival of one COVID‐19 patient over another | 1473 (57.1%) | 0.285 | 0.274 | 0.613 |
Note: Items beginning with “worry” were assessed using the stem: “How much do you worry abouat the following work‐related concerns?” and a five‐point scale ranging from “Not worried at all” to “Worried nearly all of the time.” The item “Feel torn between desire/duty to help patients versus loved ones (family, friends, etc)” was assessed using the stem: “In the last week, how often have you felt torn between your desire/duty to help your patients and your desire/duty to loved ones (family, friends, etc.)?” and a five‐point scale ranging from “None of the time” to “All of the time.” “Feel that those with whom you live are fearful to be near you due to possible COVID‐19 exposure at work” was assessed using the stem: “In the last week, how often have you felt that those who live with you are fearful to be near you due to your possible COVID exposure at work?” and a five‐point scale ranging from “None of the time” to “All of the time.” Family‐related factor: eigenvalue = 4.61, 41.9% cumulative variance explained; Cronbach's α = .78.Infection‐related factor: eigenvalue = 1.37, 12.5% variance explained; Cronbach's α = .93.Work‐related factor: eigenvalue = 1.03, 9.4% of variance; Cronbach's α = .75. Bolded values indicate factors loadings >0.40.
Abbreviation: COVID, coronavirus disease.
Positive item endorsement was operationalized as reporting feeling “sometimes worried,” “often worried,” or “worried nearly all of the time;” or “some of the time,” “most of the time,” or “all of the time.”
COVID‐19‐related PTSD Symptoms: PTSD symptoms were assessed using an abbreviated 4‐item version (Geier et al., 2020) of the PTSD Checklist for DSM‐5 (Weathers et al., 2013), with questions modified to assess PTSD symptoms related to COVID‐19 exposure (e.g., “Over the past two weeks, how often were you bothered by repeated, disturbing, and unwanted memories of your experiences related to the COVID‐19 pandemic?”) A positive screen for PTSD symptoms was defined by a cutoff score ≥8 (Geier et al., 2020; Cronbach's α = .85).
Burnout: Burnout was assessed using the single‐item Mini‐Z measure rated on a five‐point scale (Rohland et al., 2004). The item offered a definition of burnout (“Burnout is a long term stress reaction characterized by depersonalization, including cynical or negative attitudes toward patients, emotional exhaustion, a feeling of decrased personal achievement and a lack of empathy for patients”) and asked participants to use the definition to choose the best answer (1–5) ranging from “I enjoy my work. I have no symptoms of burnout” to “I feel completely burnt out. I am at the point where I may need to seek help.” The presence of burnout was indicated by a score of 3 (“I am definitely burning out and have one or more symptoms of burnout, e.g., emotional exhaustion”), 4 (“The symptoms of burnout that I am experiencing won't go away. I think about work frustrations a lot”) or 5 (“I feel completely burned out. I am at the point where I may need to seek help”). The Mini‐Z has been validated against the emotional exhaustion subscale of the Maslach Burnout Inventory (MBI) with a correlation of 0.64 (p < .001) (Rohland et al., 2004).
Functional difficulties: The brief inventory of psychosocial functioning (B‐IPF) (Bovin et al., 2018; Kleiman et al., 2018) was used to assess functional difficulties in seven functional domains, including romantic relationships, family relationships, work, friendships and socializing, self‐care, education, and parenting. Exploratory factor analysis of B‐IPF items in the current sample revealed a two‐factor solution, with one factor containing items reflecting work difficulties (e.g., “I had trouble at work;” factor loadings = 0.55–0.78; Cronbach's α = .78) and relationship difficulties (e.g., “I had trouble with my family relationships;” factor loadings = 0.51–0.80; Cronbach's α = .79).
2.2.1. Data analysis
Data analyses proceeded in five steps. First, we computed descriptive statistics to summarize sociodemographic, exposure, and clinical characteristics. Second, we conducted an exploratory factor analysis with promax rotation to identify the factor structure of COVID‐19 moral distress items. Third, we conducted multivariable regression analyses to determine whether COVID‐19 moral distress factors were related to dependent variables; age, gender, marital status, profession, years in practice, and number of COVID‐19 patients treated were entered in Step 1 of this analysis and guilt‐related worries in Step 2. Fourth, we conducted planned secondary regression analyses of significant COVID‐19 moral distress factors to identify items that drove associations with dependent variables. Fifth, we conducted relative importance analyses using the R package relaimpo to assess the unique proportion of variance in dependent variables that was explained by significant moral distress items. These analyses partition the explained variance in a dependent variable that is attributable to each independent variable while accounting for intercorrelations among independent variables (Tonidandel & LeBreton, 2010).
3. RESULTS
3.1. Sample characteristics
Of the 2579 FHCWs, 1408 (54.6%) were 18–34 years old, 581 (22.5%) 35–44, 330 (12.8%) 45–54, and 260 (10.1%) 55 and older; n = 1897 were female (73.6%) and 1821 were married/partnered (70.6%). With regard to profession, n = 1082 (42.0%) were registered nurses, 541 (21.0%) house staff, 398 (15.4%) attending physicians, 394 (15.3%) physician assistants or advanced practice registered nurses, and 164 (6.4%) other (i.e., social workers, psychologists, chaplains). The median number of years in practice was 6.0 (interquartile range [IQR] = 8.0); median number of hours working onsite was 37.5 (IQR = 10.3); and median number of COVID‐19 patients treated was 30.0 (IQR = 48.0).
3.2. Prevalence and factor structure of COVID‐19 moral distress items
The most frequently endorsed moral distress items were worries about infecting family, not being able to visit or assist loved ones who are ill/become ill, and not being able to do enough for COVID‐19 patients. Exploratory factor analysis of the 11 items revealed a three‐factor solution; Table 1 shows factor loadings, eigenvalues, and reliability data.
3.3. Associations between moral distress factors, and mental health and functional difficulties
Table 2 shows results of multivariable regression analyses of associations between moral distress factors and dependent variables. Results revealed significant associations between family, infection, and work‐related distress on all of these variables. Planned secondary analyses of individual moral distress item revealed that the strongest correlates of severity and positive screen for COVID‐19 related PTSD symptoms, and work and interpersonal difficulties were worry about how COVID‐19 will affect personal relationships. Having to make a difficult decision regarding the prioritization of COVID‐19 patients was additionally strongly associated with severity and positive screen for COVID‐19 related PTSD symptoms; and worry about not having enough knowledge regarding how to take adequate care of COVID‐19 patients was additionally strongly associated with work difficulties, while feeling that those with whom one lives fearful to be near you due to possible COVID‐19 exposure at work was additionally strongly associated with interpersonal difficulties. Feeling torn between helping patients versus loved ones and worry about not being able to do enough for COVID‐19 patients were most strongly associated with burnout.
Table 2.
Results of multivariable regression analyses of associations between COVID‐19 moral distress, COVID‐19‐related PTSD, burnout, and work and relationship difficulties in frontline health care workers
| Severity of COVID‐19 related PTSD Symptoms (adjusted R 2 = 0.36) | Positive Screen for COVID‐19 related PTSD Symptoms (Nagelkerke R 2 = 0.34) | Burnout (Nagelkerke R 2 = 0.16) | Work Difficulties (adjusted R 2 = 0.16) | Interpersonal Difficulties (adjusted R 2 = 0.13) | |
|---|---|---|---|---|---|
| β | OR (95% CI) | OR (95% CI) | β | β | |
| Primary analyses | |||||
| Family‐related moral distress | 0.32*** | 2.17 (1.92‐2.45)*** | 1.51 (1.38‐1.66)*** | 0.19*** | 0.25*** |
| Infection‐related moral distress | 0.22*** | 1.79 (1.59‐2.02)*** | 1.20 (1.09‐1.31)*** | 0.12*** | 0.10*** |
| Work‐related moral distress | 0.36*** | 2.32 (2.05‐2.62)*** | 1.60 (1.45‐1.75)*** | 0.25*** | 0.17*** |
| Secondary analyses | |||||
| Feel torn between desire/duty to help patients versus loved ones (family, friends, etc.) | 0.02 | 1.11 (0.97‐1.27) | 1.40 (1.25‐1.56)*** | 0.09*** | 0.07** |
| Worry about how COVID‐19 might affect ability to care for children/dependents | 0.10*** | 1.14 (1.05‐1.25)** | 0.97 (0.91‐1.04) | 0.01 | 0.04 |
| Feel that those with whom you live are fearful to be near you due to possible COVID‐19 exposure at work | 0.05* | 1.10 (0.97‐1.25) | 1.02 (0.92‐1.14) | 0.05* | 0.09*** |
| Worry about how COVID‐19 will affect personal relationships | 0.21*** | 1.37 (1.23‐1.53)*** | 1.20 (1.11‐1.31)*** | 0.17*** | 0.28*** |
| Worry about not being able to visit or assist loved ones who are ill or become ill with COVID‐19 | 0.07*** | 1.28 (1.12‐1.47)*** | 1.08 (0.98‐1.19) | −0.01 | −0.03 |
| Worry about infecting family with COVID‐19 | −0.02 | 0.97 (0.85‐1.10) | 0.98 (0.88‐1.08) | 0.07** | 0.06* |
| Worry about infecting patients with COVID‐19 | 0.08* | 1.32 (1.11‐1.56)** | 0.99 (0.87‐1.14) | 0.01 | 0.01 |
| Worry about infecting colleagues with COVID‐19 | −0.02 | 0.85 (0.71‐1.02) | 0.95 (0.83‐1.10) | 0.05 | 0.02 |
| Worry about not having enough knowledge or experience to take adequate care of COVID‐19 patients | 0.05** | 1.13 (1.01‐1.28)* | 0.97 (0.88‐1.07) | 0.14*** | 0.08** |
| Worry about not being able to do enough for COVID‐19 patients | 0.11*** | 1.22 (1.06‐1.40)** | 1.39 (1.25‐1.55)*** | 0.06* | 0.03 |
| Worry about having to make extremely difficult decisions involving prioritizing health/survival of one COVID‐19 patient over another | 0.17*** | 1.33 (1.20‐1.47)*** | 1.09 (1.01‐1.18)* | 0.02 | −0.01 |
Note: Results are adjusted for age, gender, marital status, profession, years in practice, and number of COVID‐19 patients treated.
Abbreviations: 95% CI, 95% confidence interval; COVID‐19, coronavirus disease 2019; OR, odds ratio; PTSD, posttraumatic stress disorder.
p < .05
p < .01
p < .001.
3.4. Relative importance analyses
Figure 1, 2, 3, 4, 5 show results of relative importance analyses of moral distress items associated with each of the dependent variables. Overall, worries about how COVID‐19 will affect personal relationships, not being able to do enough for COVID‐19 patients, and not having enough knowledge or experience to take care of COVID‐19 patients were the items that most often explained the majority of variance in the dependent variables.
Figure 1.
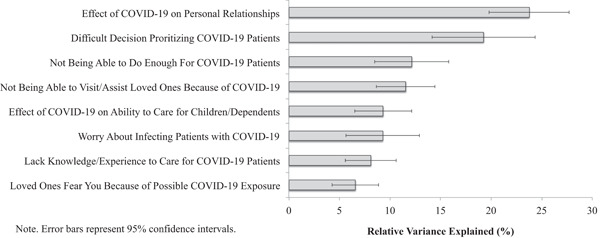
Relative importance of moral distress items associated with COVID‐19‐related PTSD symptoms in frontline health care workers. Error bars represent 95% confidence intervals. COVID‐19, coroanvirus disease 2019; PTSD, posttraumatic stress disorder
Figure 2.
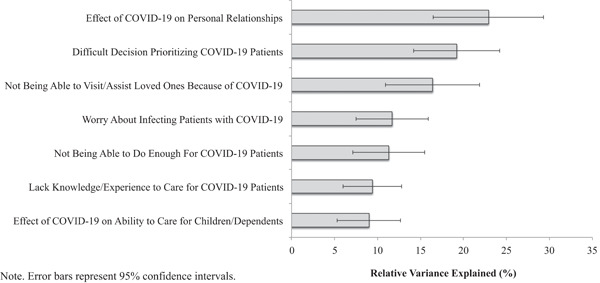
Relative importance of moral distress items associated with positive screen for positive screen for COVID‐19‐related PTSD in frontline health care workers. Error bars represent 95% confidence intervals. COVID‐19, coroanvirus disease 2019; PTSD, posttraumatic stress disorder
Figure 3.
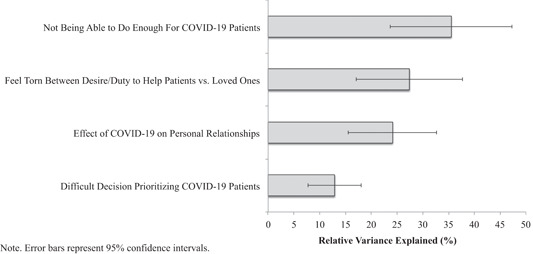
Relative importance of moral distress items associated with positive screen for burnout in frontline health care workers. Error bars represent 95% confidence intervals. COVID‐19, coroanvirus disease 2019
Figure 4.
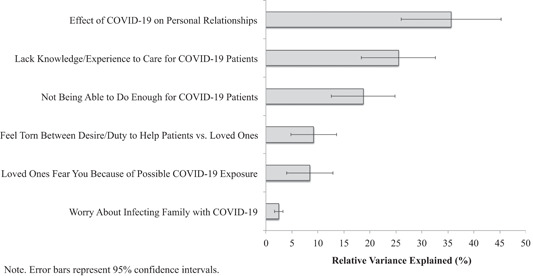
Relative importance of moral distress items associated with work difficulties in frontline health care workers. Error bars represent 95% confidence intervals. COVID‐19, coroanvirus disease 2019
Figure 5.
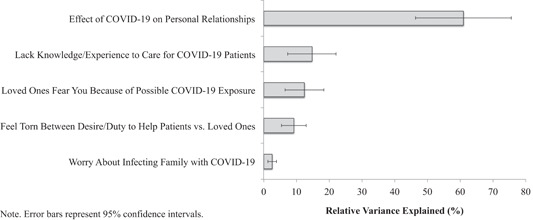
Relative importance of moral distress items associated with interpersonal difficulties in frontline health care workers. Note. Error bars represent 95% confidence intervals. COVID‐19, coroanvirus disease 2019
4. DISCUSSION
This study is the first, to our knowledge, to examine the prevalence, mental health and functional correlates of moral distress among FHCWs responding to the initial epicenter of the COVID‐19 pandemic in NYC. FHCWs were queried about how much distress (i.e., worries; Williams et al., 2020) they experienced in response to COVID‐19‐specific potentially morally distressing situations. Endorsement of each of these concerns was high, ranging from 52% to 87%. Moral distress about infecting family, not being able to visit or assist loved ones who are ill, and not being able to do enough for COVID‐19 patients were the most prevalent (endorsed by >80% of FHCWs). Factor analysis revealed that moral distress items were organized into domains of family‐, infection‐, and work ‐related concerns. All three domains were related to severity and positive screen for COVID‐19‐related PTSD symptoms, burnout, and greater work and interpersonal difficulties. It is noteworthy that moral distress explained more variance in COVID‐19‐related PTSD symptoms than in work and interpersonal functioning. One explanation is that the onset of mental health symptoms is the most immediate response to moral distress, whereas functional difficulties may intensify over time.
Relative importance analyses revealed that concerns about relationships and work competencies were consistently strongly related to these outcomes, although which specific concerns varied. Distress regarding how one's work may affect personal relationships may have been salient because FHCWs may have had to choose among options that violated values—if they moved out to not worry about infecting family, they may have felt like they abandoned family responsibilities; if they stayed home, they may have worried about infecting loved ones. This strain on relationships may have, in turn, led to psychological distress and work/personal functional difficulties.
Distress in regard to work‐related competencies (e.g., worrying about not knowing enough or being able to do enough for COVID‐19 patients, having to make decisions with life‐and‐death ramifications) may be particularly distressing because it taps fundamental aspects of a person's self‐worth and identity as a caregiver. Our finding that feeling torn between helping patients and being there for loved ones was particularly strongly associated with burnout aligns with literature documenting work‐life integration challenges (i.e., work stress “spillover”) can be a key driver of burnout among healthcare professionals (Shanafelt et al., 2012). Although it is not uncommon for FHCWs to face extremely stressful life‐and‐death situations, stress related to balancing work/home life, and to feel like they cannot do enough (LaDonna et al., 2018; Mullangi & Jagsi, 2019), the extreme conditions of the pandemic likely amplified these experiences and accompanying emotional reactions. Distress related to infecting others was most strongly linked to interpersonal functioning, possibly because those who were most worried about this took more steps to distance themselves from others.
This study is novel in several ways. Studies examining mental health correlates of initial reactions of moral distress following potentially morally injurious events are lacking. Similarly, while several commentaries have described the potential for moral distress among FHCWs during COVID‐19, this study is among the first to present data showing that it is in fact associated with mental health and functional difficulties. Our findings build on other studies that have identified risk factors for PTSD symptoms, such as greater personal exposures to the virus, having underlying conditions that would put one at risk for severe COVID‐19 symptoms, pre‐pandemic burnout, having insufficient PPE, difficulty sleeping, and experiencing the death of a coworker (Feingold et al., 2021; Mosheva et al., 2020).
These findings have three notable clinical and research implications. First, assessing moral distress at the time of potentially morally injurious events may be important, as it can be highly prevalent, and may help inform risk for mental health and functional problems. In this study, we developed items that were salient to the experience of FHCWs during the pandemic and found that they factored together into three categories of moral distress reflecting family‐, infection‐, and work‐related concerns. Although measures of moral distress specific to healthcare workers exist (Giannetta et al., 2020), our findings underscore that moral distress measures that can be used across situations and populations are needed. Such measures would allow us to learn about similarities and differences across populations and traumatic situations and make it possible to offer measurement‐based support to impacted populations.
Second, although causality cannot be ascertained from a cross‐sectional study, results suggest that it may be worthwhile to evaluate efforts to prevent or mitigate moral distress. A variety of strategies to reduce risk of moral distress from pandemic‐related events have been proposed (Maguen & Price, 2020; Watson et al., 2020; Williams et al., 2020), including psychological first aid (National Child Traumatic Stress Network, 2018), self‐care strategies, such as seeking support around difficult decisions; strategies colleagues can use to help each other such as checking in and listening, and strategies leaders can apply such as clear communication around changing policies and creating a culture where seeking help is not stigmatized. Strategies to prevent moral distress and injury specifically among FHCWs during COVID‐19 have also been suggested. For example, hospital and unit leaders have been advised to help build social support among staff and to provide spaces for FHCWs to debrief emotional experiences (Blake et al., 2020; Gold et al., 2016; Kishore et al., 2016; Roycroft et al., 2020). Another suggestion is to establish protocols that shift decision‐making burden (e.g. prioritizing one life over another) away from individual professionals and onto teams (Blake et al., 2020; Roycroft et al., 2020). Resources to help employees with family responsibilities (e.g. access to child/elder care, lodging for staff away from family, and hazard pay) have also been recommended (Sinclair et al., 2020). More support (e.g., education, consultation) for staff deployed to work outside of their specialty areas and scheduling that allowed more time between shifts may also help. While these suggested strategies to mitigate moral distress and moral injury have good “face validity,” empirical evaluation is needed to determine their effectiveness.
Third, results of this study also suggest that early intervention may be warranted for FHCWs who experience moral distress. It has been proposed that moral distress may be a precursor to moral injury for some individuals (Čartolovni et al., 2021; Epstein & Hamric, 2009; Williams et al., 2020) and one study of FHCWs during COVID‐19 showed that over 3 months, moral distress did not resolve on its own (Hines et al., 2021). Studies suggest that among those with PTSD, moral injury can often be effectively treated with evidence‐based PTSD treatment (e.g., Held et al., 2018). There are also novel transdiagnostic treatments with promising preliminary data, such as Trauma‐Informed Guilt Reduction Therapy (Norman et al., 2014), that aim to reduce suffering from moral injury. Whether these can be adapted to mitigate moral distress close to the time morally injurious events occur is another important empirical question. Longitudinal studies to understand downstream consequences of moral distress, and studies to understand how to prevent and intervene early on moral distress are critical next steps. With regard to COVID‐19, the pandemic presents an opportunity to evaluate experiences of moral distress in medicine and how to help mitigate this distress.
Several limitations to this study should be noted. First, the survey was open for a 1‐month period in which there was rapid change in clinical volume. Thus, FHCWs may have responded differently depending on when in the study period they completed the survey. Second, given that this study was cross‐sectional, causal associations between moral distress and mental health and functioning measures cannot be ascertained. Third, COVID‐19‐related PTSD symptoms were ascertained over a two‐week period and criterion A was not assessed, so these symptoms may reflect acute stress reactions rather than PTSD. Fourth, while this survey was completely anonymous, some FHCWs may have underreported their symptoms for fear of stigma; others may have overreported symptoms to help catalyze institutional action. Further, response bias may have been introduced if non‐responders were too stressed to complete the survey. Fifth, given that there is no known measure of moral distress related to the unique experiences of working the frontlines of a global pandemic, we employed a set of items that has not been validated. Consequently, more research is needed to develop an assessment of moral distress that may be applied across different occupational settings. Relatedly, it is possible that other aspects of moral distress experienced by FHCWs were not captured with the items administered in our survey. We assessed circumstances presumed to be morally distressing for frontline healthcare workers during the pandemic but were not able to assess the prevalence or types of all potentially morally distressing events. Mixed‐methods studies would be helpful in identifying the full range of potentially morally distressing experiences in this population (e.g., feeling betrayed by supervisors and/or leadership). Finally, the wording of the moral distress items was such that it is not clear if FHCWs experienced these events or were distressed in anticipation of experiencing them.
Notwithstanding these limitations, this study is among the first to document the prevalence and mental health burden of moral distress while a situation with many traumatic and potentially morally injurious events is unfolding. Results extend the literature on moral distress, adding support to the notion that it may be an important mechanism related to the prevalence and severity of posttraumatic distress in its many forms, including symptoms and functioning. Further research is needed to evaluate the prognostic utility of moral distress in predicting moral injury and long‐term mental health problems; examine interrelationships between moral distress/injury and mental health outcomes over time; and evaluate the efficacy of moral distress interventions in mitigating risk for moral injury, and mental health and functional difficulties in FHCWs and other trauma‐affected populations.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1002/da.23205
Norman, S. B. , Feingold, J. H. , Kaye‐Kauderer, H. , Kaplan, C. A. , Hurtado, A. , Kachadourian, L. , Feder, A. , Murrough, J. W. , Charney, D. , Southwick, S. M. , Ripp, J. , Peccoralo, L. , & Pietrzak, R. H. (2021). Moral distress in frontline healthcare workers in the initial epicenter of the COVID‐19 pandemic in the United States: Relationship to PTSD symptoms, burnout, and psychosocial functioning. Depression Anxiety, 38, 1007–1017. 10.1002/da.23205
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Blake, H. , Bermingham, F. , Johnson, G. , & Tabner, A. (2020). Mitigating the psychological impact of COVID‐19 on healthcare workers: A digital learning package. International Journal of Environmental Research and Public Health, 17(9). 10.3390/ijerph17092997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges, L. M. , Barnes, S. M. , Farnsworth, J. K. , Bahraini, N. H. , & Brenner, L. A. (2020). A commentary on moral injury among health care providers during the COVID‐19 pandemic. Psychological Trauma: Theory Research, Practice and Policy, 12, 138. 10.1037/tra0000698 [DOI] [PubMed] [Google Scholar]
- Bovin, M. J. , Black, S. K. , Rodriguez, P. , Lunney, C. A. , Kleiman, S. E. , Weathers, F. W. , Schnurr, P. P. , Spira, J. , Keane, T. M. , & Marx, B. P. (2018). Development and validation of a measure of PTSD‐related psychosocial functional impairment: The inventory of psychosocial functioning. Psychological services, 15(2), 216–229. 10.1037/ser0000220 [DOI] [PubMed] [Google Scholar]
- Bryan, C. J. , Morrow, C. E. , Etienne, N. , & Ray‐Sannerud, B. (2013). Guilt, shame, and suicidal Iideation in a military outpatient clinical sample. Depression and Anxiety, 30(1), 55–60. 10.1002/da.22002 [DOI] [PubMed] [Google Scholar]
- Čartolovni, A. , Stolt, M. , Scott, P. A. , & Suhonen, R. (2021). Moral injury in healthcare professionals: A scoping review and discussion. Nursing Ethics, 969733020966776. 10.1177/0969733020966776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein, E. G. , & Hamric, A. B. (2009). Moral distress, moral residue, and the crescendo effect. The Journal of Clinical Ethics, 20(4), 330–342. [PubMed] [Google Scholar]
- Feingold, J. H. , Peccoralo, L. , Chan, C. C. , Kaplan, C. A. , Kaye‐Kauderer, H. , Charney, D. , Verity, J. , Hurtado, A. , Burka, L. , Syed, S. A. , Murrough, J. W. , Feder, A. , Pietrzak, R. H. , & Ripp, J. (2021). Psychological impact of the COVID‐19 pandemic on frontline health care workers during the pandemic surge in New York City. Chronic Stress, 5, 2470547020977891. 10.1177/2470547020977891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fumis, R. R. L. , Junqueira Amarante, G. A. , de Fátima Nascimento, A. , & Vieira Junior, J. M. (2017). Moral distress and its contribution to the development of burnout syndrome among critical care providers. Annals of Intensive Care, 7, 7. 10.1186/s13613-017-0293-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geier, T. J. , Hunt, J. C. , Hanson, J. L. , Heyrman, K. , Larsen, S. E. , Brasel, K. J. , & deRoon‐Cassini, T. A. (2020). Validation of abbreviated four‐ and eight‐item versions of the PTSD checklist for DSM‐5 in a traumatically injured sample. Journal of Traumatic Stress, 33(3), 218–226. 10.1002/jts.22478 [DOI] [PubMed] [Google Scholar]
- Giannetta, N. , Villa, G. , Pennestrì, F. , Sala, R. , Mordacci, R. , & Manara, D. F. (2020). Instruments to assess moral distress among healthcare workers: A systematic review of measurement properties. International Journal of Nursing Studies, 111, 103767. 10.1016/j.ijnurstu.2020.103767 [DOI] [PubMed] [Google Scholar]
- Gold, K. J. , Andrew, L. B. , Goldman, E. B. , & Schwenk, T. L. (2016). “I would never want to have a mental health diagnosis on my record”: A survey of female physicians on mental health diagnosis, treatment, and reporting. General Hospital Psychiatry, 43, 51–57. 10.1016/j.genhosppsych.2016.09.004 [DOI] [PubMed] [Google Scholar]
- Griffin, B. J. , Purcell, N. , Burkman, K. , Litz, B. T. , Bryan, C. J. , Schmitz, M. , Villierme, C. , Walsh, J. , & Maguen, S. (2019). Moral injury: An integrative review. Journal of Traumatic Stress, 32(3), 350–362. 10.1002/jts.22362 [DOI] [PubMed] [Google Scholar]
- Haller, M. , Norman, S. B. , Davis, B. C. , Capone, C. , Browne, K. , & Allard, C. B. (2020). A model for treating COVID‐19‐related guilt, shame, and moral injury. Psychological Trauma: Theory Research, Practice and Policy, 12, 174. 10.1037/tra0000742 [DOI] [PubMed] [Google Scholar]
- Held, P. , Klassen, B. J. , Brennan, M. B. , & Zalta, A. K. (2018). Using prolonged exposure and cognitive processing therapy to treat veterans with moral injury‐based PTSD: Two case examples. Cognitive and behavioral practice, 25(3), 377–390. 10.1016/j.cbpra.2017.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hines, S. E. , Chin, K. H. , Glick, D. R. , & Wickwire, E. M. (2021). Trends in moral injury, distress, and resilience factors among healthcare workers at the beginning of the COVID‐19 pandemic. International Journal of Environmental Research and Public Health, 18(2). 10.3390/ijerph18020488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hines, S. E. , Chin, K. H. , Levine, A. R. , & Wickwire, E. M. (2020). Initiation of a survey of healthcare worker distress and moral injury at the onset of the COVID‐19 surge. American Journal of Industrial Medicine, 63, 830–833. 10.1002/ajim.23157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, J. , Liu, F. , Teng, Z. , Chen, J. , Zhao, J. , Wang, X. , & Wu, R. n.d. Care for the psychological status of frontline medical staff fighting against COVID‐19. Clinical Infectious Diseases, 71, 3268–3269. 10.1093/cid/ciaa385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jameton, A. (1984). Nursing practice: The ethical issues. Prentice‐Hall. [Google Scholar]
- Jameton, A. (2017). What moral distress in nursing history could suggest about the future of health care. AMA Journal of Ethics, 19(6), 617–628. 10.1001/journalofethics.2017.19.6.mhst1-1706 [DOI] [PubMed] [Google Scholar]
- Kishore, S. , Dandurand, D. E. , Mathew, A. , & Rothenberger, D. (2016). Breaking the culture of silence on physician suicide. NAM Perspectives, 6. 10.31478/201606a [DOI] [Google Scholar]
- Kleiman, S. E. , Bovin, M. J. , Black, S. K. , Rodriguez, P. , Brown, L. G. , Brown, M. E. , Lunney, C. A. , Weathers, F. W. , Schnurr, P. P. , Spira, J. , Keane, T. M. , & Marx, B. P. (2018). Psychometric properties of a brief measure of posttraumatic stress disorder‐related impairment: The brief inventory of psychosocial functioning. Psychological services, 17, 187–194. 10.1037/ser0000306 [DOI] [PubMed] [Google Scholar]
- LaDonna, K. A. , Ginsburg, S. , & Watling, C. (2018). “Rising to the Level of Your Incompetence”: What physicians' self‐assessment of their performance reveals about the imposter syndrome in medicine. Academic Medicine: Journal of the Association of American Medical Colleges, 93(5), 763–768. 10.1097/ACM.0000000000002046 [DOI] [PubMed] [Google Scholar]
- Lamiani, G. , Borghi, L. , & Argentero, P. (2017). When healthcare professionals cannot do the right thing: A systematic review of moral distress and its correlates. Journal of Health Psychology, 22(1), 51–67. 10.1177/1359105315595120 [DOI] [PubMed] [Google Scholar]
- Litz, B. T. , Stein, N. , Delaney, E. , Lebowitz, L. , Nash, W. P. , Silva, C. , & Maguen, S. (2009). Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clinical Psychology Review, 29(8), 695–706. 10.1016/j.cpr.2009.07.003 [DOI] [PubMed] [Google Scholar]
- Lu, W. , Wang, H. , Lin, Y. , & Li, L. (2020). Psychological status of medical workforce during the COVID‐19 pandemic: A cross‐sectional study. Psychiatry Research, 288, 112936. 10.1016/j.psychres.2020.112936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maguen, S. , & Price, M. A. (2020). Moral injury in the wake of coronavirus: Attending to the psychological impact of the pandemic. Psychological Trauma: Theory Research, Practice and Policy, 12, 131. 10.1037/tra0000780 [DOI] [PubMed] [Google Scholar]
- Miljeteig, I. , Forthun, I. , Hufthammer, K. O. , Engelund, I. E. , Schanche, E. , Schaufel, M. , & Onarheim, K. H. (2021). Priority‐setting dilemmas, moral distress and support experienced by nurses and physicians in the early phase of the COVID‐19 pandemic in Norway. Nursing Ethics, 28(1), 66–81. 10.1177/0969733020981748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosheva, M. , Hertz‐Palmor, N. , Ilan, S. D. , Matalon, N. , Pessach, I. M. , Afek, A. , Ziv, A. , Kreiss, Y. , Gross, R. , & Gothelf, D. (2020). Anxiety, pandemic‐related stress and resilience among physicians during the COVID‐19 pandemic. Depression and Anxiety, 37(10), 965–971. 10.1002/da.23085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullangi, S. , & Jagsi, R. (2019). Imposter Syndrome: Treat the Cause, Not the Symptom. Journal of the American Medical Association, 322(5), 403–404. 10.1001/jama.2019.9788 [DOI] [PubMed] [Google Scholar]
- National Child Traumatic Stress Network (NCTSN) . (2018). Psychological first aid (PFA) field operations guide: 2nd Edition. The National Child Traumatic Stress Network. Retrieved from https://www.nctsn.org/resources/psychological-first-aid-pfa-field-operations-guide-2nd-edition
- Norman, S. B. , Wilkins, K. C. , Myers, U. S. , & Allard, C. B. (2014). Trauma informed guilt reduction therapy with combat veterans. Cognitive and Behavioral Practice, 21(1), 78–88. 10.1016/j.cbpra.2013.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira‐Sanchez, V. , Adiukwu, F. , El Hayek, S. , Bytyçi, D. G. , Gonzalez‐Diaz, J. M. , Kundadak, G. K. , Larnaout, A. , Nofal, M. , Orsolini, L. , Ramalho, R. , Ransing, R. , Shalbafan, M. , Soler‐Vidal, J. , Syarif, Z. , Teixeira, A. L. S. , & da Costa, M. P. (2020). COVID‐19 effect on mental health: Patients and workforce. The Lancet. Psychiatry, 7(6), e29–e30. 10.1016/S2215-0366(20)30153-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rittenmeyer, L. , & Huffman, D. (2009). How professional nurses working in hospital environments experience moral distress: A systematic review. JBI Library of Systematic Reviews, 7(28), 1234–1291. 10.11124/01938924-200907280-00001 [DOI] [PubMed] [Google Scholar]
- Rohland, B. M. , Kruse, G. R. , & Rohrer, J. E. (2004). Validation of a single‐item measure of burnout against the Maslach burnout inventory among physicians. Stress and Health, 20(2), 75–79. 10.1002/smi.1002 [DOI] [Google Scholar]
- Roycroft, M. , Wilkes, D. , Pattani, S. , Fleming, S. , & Olsson‐Brown, A. (2020). Limiting moral injury in healthcare professionals during the COVID‐19 pandemic. Occupational Medicine, 70(5), 312–314. 10.1093/occmed/kqaa087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanafelt, T. , Ripp, J. , & Trockel, M. (2020). Understanding and addressing sources of anxiety among health care professionals during the COVID‐19 pandemic. Journal of the American Medical Association, 323, 2133–2134. 10.1001/jama.2020.5893 [DOI] [PubMed] [Google Scholar]
- Shanafelt, T. D. , Boone, S. , Tan, L. , Dyrbye, L. N. , Sotile, W. , Satele, D. , West, C. P. , Sloan, J. , & Oreskovich, M. R. (2012). Burnout and satisfaction with work‐life balance among US physicians relative to the general US population. Archives of Internal Medicine, 172(18), 1377–1385. 10.1001/archinternmed.2012.3199 [DOI] [PubMed] [Google Scholar]
- Shechter, A. , Diaz, F. , Moise, N. , Anstey, D. E. , Ye, S. , Agarwal, S. , Birk, J. L. , Brodie, D. , Cannone, D. E. , Chang, B. , Claassen, J. , Cornelius, T. , Derby, L. , Dong, M. , Givens, R. C. , Hochman, B. , Homma, S. , Kronish, I. M. , Lee, S. , … Abdalla, M. (2020). Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID‐19 pandemic. General Hospital Psychiatry, 66, 1–8. 10.1016/j.genhosppsych.2020.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair, R. R. , Allen, T. , Barber, L. , Bergman, M. , Britt, T. , Butler, A. , Ford, M. , Hammer, L. , Kath, L. , Probst, T. , & Yuan, Z. (2020). Occupational health science in the time of COVID‐19: Now more than ever. Occupational Health Science, 1–22. 10.1007/s41542-020-00064-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonidandel, S. , & LeBreton, J. M. (2010). Determining the relative importance of predictors in logistic regression: An extension of relative weight analysis. Organizational Research Methods, 13(4), 767–781. 10.1177/1094428109341993 [DOI] [Google Scholar]
- Truog, R. D. , Mitchell, C. , & Daley, G. Q. (2020). The toughest triage—Allocating ventilators in a pandemic. New England Journal of Medicine, 382(21), 1973–1975. 10.1056/NEJMp2005689 [DOI] [PubMed] [Google Scholar]
- Watson, P. , Norman, S. B. , Maguen, S. , & Hamblen, J. L. (2020). Moral injury in healthcare workers. National Center for PTSD. https://www.ptsd.va.gov/professional/treat/cooccurring/moral_injury_hcw.asp
- Weathers, F. W. , Litz, B. T. , Keane, T. M. , Palmeri, P. A. , Marx, B. P. , & Schnurr, P. P. (2013). The PTSD checklist for DSM‐5 (PCL‐5). Scale Available from the National Center for PTSD. Retrieved from https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp
- Williams, R. D. , Brundage, J. A. , & Williams, E. B. (2020). Moral injury in times of COVID‐19. Journal of Health Service Psychology, 1–5. 10.1007/s42843-020-00011-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


