Abstract
The time and type of the States' responses to the COVID‐19 pandemic varied with the severity of the epidemiological situation, the perceived risk, the political organisation and the model of health system of the country. We discuss the response of Germany, Spain, France, Italy, Portugal and the United Kingdom during the first months of the COVID‐19 epidemic in 2020, considering the political organisation of the country and its health system model. We analyse public health measures implemented to contain or mitigate the pandemic, as well as those related to governance, resources and reorganisation of services, financing mechanisms, response of the health system itself and health outcomes. To measure the burden of COVID‐19, we use several indicators. The adoption of measures, to contain and mitigate epidemic varied in degree and time of adoption. All countries reorganised their governance structure and the provision of care, despite the differences in political models and health systems (ranging from a more unitary and centralised political organisational model—France and Portugal; to a decentralised matrix—Germany, Spain, Italy and the United Kingdom). Rather than the differences in political models and health systems, the explanation for the success in tackling the epidemic seems to lay in other social determinants of health.
Keywords: COVID‐19, Europe, health systems, political organisation, State
1. BACKGROUND
The COVID‐19 was first detected in the city of Wuhan, in China, and later identified by the World Health Organization as a cluster of atypical pneumonia cases with unknown aetiology. Far along, it was attributed to the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) and it quickly evolved into a Public Health Emergency of International Concern. 1
The prevalence of non‐communicable diseases has led to a series of adaptations, especially in health systems of high‐income countries leading to sometimes neglecting the prevention and control measures of infections. 2 This resulted in some degree of unpreparedness of countries and governments to deal with the new epidemic, despite international regulations and instruments. As so, in the face of the COVID‐19 pandemic, countries implemented policies that were also influenced by the organisation of the State and the organisation of the provision of health care services, that is, model of health system, 3 among other aspects (i.e., European Union overall policies).
The organisation of the State 4 refers to the country's internal structure with regard to the unity or plurality of the legal‐constitutional order, the most important distinction being made between a unitary and a federal state. In the first case, there is a single body for political decision‐making and a single set of government institutions. At the moment, all democratic unitary states practice at least administrative decentralisation, that is, they attribute the exercise of administrative functions to other legal persons in addition to the state, be it functional and institutional or territorial decentralisation. In territorial decentralisation, the State recognises administrative autonomy to entities with a territorial and social basis, like local authorities. In some unitary states, decentralisation takes on an even more ambitious nature with the state recognising in some territorial entities—Autonomous Regions—political autonomy and giving them legislative power and autonomy. In the federal state, there is a plurality of political powers and constitutional orders: the federal state to which the others are subordinated, integrating and participating in the governing structure of the Federation (or Union) member states. It can be said that the federated states that make up the Federation are true states, insofar as, respecting certain limits, they draw up their own Constitutions and, in the domain of their competences, have typically state structure, organs and activity.
When analysing the response to the pandemic, it is important to consider the organisation of the health systems, which are based on solidarity and universality, with pre‐payment formats for the entire population, and can be divided between those closer to the Bismarck model and those that refer to the Beveridge model.
In the Bismarck model, the social insurance system is mandatory, almost universal, and operates within the scope of sickness insurance funds, as a rule managed by social entities, but subject to the supervision of public bodies. This social insurance undertakes a “mutualisation” of the risks (risk sharing) and the premiums are usually fixed according to the income. The disparity in risk coverage is sometimes offset by the government intervention. In many countries, the system covers the entire population. As a rule, these mutualities are organised around a profession, sector of activity, religious confession or geographical area. The Beveridge model, on the other hand, is based on a national health service and tax financing, and can be organised in an integrated way, in which the financing and provision of care are provided by a single public structure that receives from the state budget the funds needed; or by state services or private entities contracted by autonomous public funds. The NHS is characterised by public institutional management, regardless of the nature of the provider, whether public or contracted, with health care generally free or almost free at point‐of‐care.
In this paper, we analyse the response in the first months of 2020 to the SARS‐CoV‐2 pandemic in Germany, Spain, France, Italy, Portugal and the United Kingdom, in light of the organisation of the state and of the type of health system.
2. METHODS
2.1. Scope of analysis
We have chosen as areas of analysis the public health measures implemented to contain or mitigate the COVID‐19 pandemic, in the first months of the SARS‐CoV‐2 pandemic in 2020, as well as those related to governance, resources and reorganisation of services, financing mechanisms, response of the health system itself and health outcomes.
We selected six European countries: those close to a more unitary and centralised political organisational model (France and Portugal) and others with a more decentralised matrix with a plurality of political powers and constitutional orders (Germany, Spain, Italy and the United Kingdom).
In terms of models of health systems, the chosen countries represent diversity with those closer to a mandatory Bismarck social insurance system (France and Germany) and other countries with a Beveridge model based on NHS (Spain, Italy, Portugal and the United Kingdom).
2.2. Epidemiological analysis
To measure the highest burden of COVID‐19 ever registered until 31 August 2020 in the countries we used the 14‐day infection rate per 100,000 inhabitants. We used the case fatality rate (proportion of deaths in the total of confirmed cases) as a measure of severity of the epidemic 5 ; the age group standardised mortality rate from all causes, registered between 2 January until 2 May 2020 (last available at time of the submission) was used to compare the risk of death caused directly and indirectly by COVID‐19 or other causes; and the percentual maximum variation in all causes mortality in the last 10 years (or last year available) between 1st January and 30th June 2020 (last available at time of the submission) to compare the excess mortality that might have occurred in the countries under analysis due caused directly and indirectly by COVID‐19 or other causes. 6 , 7 , 8
All‐cause mortality captures the direct and indirect effects caused by COVID‐19 pandemic and it gives a comprehensive picture of the full impact of the pandemic in populations health status. Also, focusing on excess mortality estimates, as the difference between the number of deaths from all causes during the pandemic and the expected number of deaths given a historical baseline, is a more reliable metric for comparing countries. 9 , 10 , 11 , 12 In addition, it overcomes the variation between countries in reporting and testing for COVID‐19 and in misclassification of the cause of death in death certificates. However, this analysis remained blind to the underlying causes of death and does not provide an understanding of which causes have exceeded or fallen below the levels expected. Seemingly, age‐specific, sex‐specific and socioeconomic status data were not accessed to understand inequalities in the effects of the pandemic beyond deaths assigned to COVID‐19 as the underlying cause of death. 10 , 13 , 14 , 15 , 16
The data were collected from different and reliable sources available at the time of the analysis. At the time, there was a delay due to communication and aggregation processes. In addition, due to time and data availability and comparability constraints, the authors chose to collect data from the European Centre for Disease Prevention and Control, regarding COVID‐19 infection rates, and the Eurostat (official European institution for statistics) and the Oxford COVID‐19 Government Response Tracker, as a global consortium for COVID‐19 fatality rates analysis.
3. RESULTS
3.1. State organisation and health system models
Germany is a federal parliamentary republic made up of 16 states (Länder), each with its own constitution, which are in line with the national constitution. The concept of decentralisation does not, strictly speaking, reflect the reality of German federalism. The extensive powers exercised by the federal states may seem like an example of devolution, but they were never transferred from the central government to the federal states. Instead, the opposite of devolution occurred: each state transferred certain rights and responsibilities to the Federal Government and, at the same time, retained others. 9 Germany was the first country to introduce a social and health insurance system in 1883. At the heart of the Bismarck system are the principles of mandatory membership and contributions unrelated to individual risk. At the federal level, there are three main institutions: the Federal Assembly (Bundestag), Federal Council (Bundesrat) and the Federal Ministry of Health (Bundesministerium für Gesundheit), which is supported by a series of federal Government Bodies. Depending of the Länder, the responsibility for health might be divided between labour and social affairs, family and youth affairs, environmental affairs and/or consumer protection. The corporatist level comprises regional and federal associations of physicians and dentists, sickness funds and the Federal Association of Sickness Funds. 17
The Spanish Constitution of 1978 established a new political organisation, moving from a highly centralised country to a quasi‐federal organisation, in which the 17 Autonomous Communities (AC) play an essential role in the planning, financing and provision of health, education and social protection services. In the last decade, the decentralisation process has been consolidated and the AC have gained increased capacity for regulation, planning and, above all, financial autonomy. However, with the budget restrictions of AC, financial resources for health became controlled by the Ministry of Finance and the most important political decisions have now been made by the Ministry of Health, without the participation of the Interterritorial Council of the National Health System. 18
In France, the political organisation is markedly decentralised with three administrative levels— municipalities, departments and regions. All levels have elected assemblies and some level of autonomy in clearly identified areas. The State defines the competences of each level. The departments, grouped into 13 regions, are the second administrative level and take responsibilities in health and social security sectors and in the financing and provision of elementary education. The decentralisation process in France is characterised by some level of reluctancy to reduce central control over policy and funding, which results mainly in deconcentration. The French health system is based on social insurance. It is financed by contributions from employers and employees, with monetary and in‐kind benefits. In France, there is a moderate gate‐keeping effect, with outpatient care provided by private, individual or collective entities, while specialised and hospital care is mainly provided by public entities. 19
The Constitution of Italy organises the territory into 20 regions, which differ in size, population and levels of economic development. Each region is governed by a democratically elected Executive and Regional Council. The regions have exclusive legislative power in relation to any matter not expressly reserved by the central level. However, its financial autonomy is quite modest. The gradual return of political power in the 1990s went hand in hand with the tax reform approved in 2000, which (in theory) gave the regions significant autonomy over regional budget revenue and total autonomy over resource allocation. 20 The 1978 reform, which created the NHS, introduced universal health care coverage. The new health system has been partially decentralised in three levels–national, regional and local administration. The central government is responsible for defining the criteria for allocating resources across regions and for planning. Regional health authorities are responsible for local planning in line with the national health objectives, for organising and managing health services and for allocating resources to local health units. 20
Portugal is a unitary state, with two autonomous regions, Azores and Madeira, with governments and regional assemblies. Municipalities and parishes have their own democratically elected level of government. Despite some decentralisation that have occurred since the 2000s, the political power is still relies mainly on the central government. The extent of the financial autonomy granted by the constituent legislator to local authorities is much smaller than that of autonomous regions. The decentralisation of competences in the health sector, which started in 2018, attributed municipal bodies infrastructural planning and management related to primary health care units. 21 The Portuguese NHS was created in 1979, under the principles of centralised control and decentralised management. Formally, decentralisation is a key word in the constitutional framework of the NHS. The 2019 Health Basic Law establishes that the NHS is managed at the regional level, furthering the transfer of the coordination of the provision of health services and allocation of financial resources to the regional level. Nevertheless, responsibility for planning and allocation of resources remains highly centralised, despite the creation of the current five regional health administrations in 1993. 21
The four nations that make up the United Kingdom are represented in the British parliament and have their own governments. In the United Kingdom, the NHS was created in 1948, with the aim of being a national system, managed locally. In 1990, the National Health Service and Community Care Act was approved, which separated the purchase and provision of health services to increase the efficiency and quality of services, based on the principles of market competition. In 1997, the reorganisation of health services in the United Kingdom, with the devolution of political power from the British Parliament to national administrations in Scotland, Wales and Northern Ireland, led to increasingly asymmetric health systems. Devolution means that Scotland, Wales and Northern Ireland can determine their own spending plans, although financial responsibility for revenue collection has remained with the central government of the United Kingdom. 22
3.2. Measures implemented
The adoption of measures, first to contain the SARS‐CoV‐2 epidemic and second to mitigate its possible effects, varied essentially in degree and time of adoption in relation to the epidemiological momentum.
All countries adopted measures of physical distancing such as the suspension of mass events, the closure of educational institutions and the limitation of activity of non‐essential sectors of the society. 6 , 23
Italy was the first country in Europe to adopt physical distancing measures and made the transition to total confinement in a very short period, in late January 2020. 20 All countries closed educational establishments, albeit at different epidemiologic momentums. By the time the schools were closed, the United Kingdom, France and Spain had exceeded 100 cases. Portugal and Italy, on the other hand, chose to adopt this measure close to 10 cases. 6 , 23
The United Kingdom and Germany were the only countries that did not require the closure (or work from home) of non‐essential sectors. The six countries cancelled public events—Germany, Spain and the United Kingdom, more than a week after the 100 cases, Italy and France the day before the 100th case and Portugal five days after the 100 cases. 6 All countries imposed restrictions on gatherings of people, however at different times and with different specifications. The maximum number of people allowed varied over time in all countries, except in the United Kingdom, which always presented the highest level of restriction (up to 10 people). However, the United Kingdom adopted the measure later in time. 6 , 23
For restriction concerning public transportation, the response varied between Germany, which did not adopt any restrictions and Italy, with periods of total suppression or restriction to only specific users. The remaining countries recommended (for periods more or less long) the closure or reduction of routes or circulating vehicles. 6 , 23
As for mandatory stay at home policies, Italy adopted the most restrictive measures, with exceptions to leave home only once a week. 6 In the rest of the countries, citizens were confined to their homes with permitted outlets for exercise, supermarket shopping and essential travel. However, epidemiologic time of adoption of this measure varied between countries. Germany, France, Spain and the United Kingdom implemented it more than a month after the first case was detected and the rest of the countries less than a month after. This restriction was maintained between 45 and 54 days, except for Italy and Spain, where it remained in force for 70 and 73 days, respectively. Only Italy chose to restrict internal movement between cities/regions before reaching 100 cases. 6 The United Kingdom was the last country of those under analysis to adopt travel restrictions. Italy and Portugal implemented them about a week after the first case, while the remaining countries did so a month after. 6
3.3. Governance
In general, the pandemic required governments and governance to adjust, both in general and in the health sector.
In Germany, the Ministry of Health and the Ministry of Interior, Infrastructure and the Community, both federal, took over the management of the epidemic in collaboration with the Robert Koch Institute, the Federal Institute for Medicine and Medical Devices and the Paul‐Ehrlich Institute. The articulation included federal authorities. The symmetric and uniform implementation of prevention and control measures presented itself as a challenge due to the federative nature and respective legal framework. However, in general, the chancellor and the presidents of the federal states have enacted the same measures. 23
In early January 2020, the Spanish Ministry of Health activated the COVID‐19 protocol, in coordination with the 17 AC Health Departments. In early February 2020, the Interterritorial Council of the National Health System (the highest body in the health system) established the basis for collaboration between national and regional health authorities, reinforcing the Council's coordination and surveillance mechanisms in matters of the epidemic. In the following weeks, the Prime Minister called on the regional presidents to make joint decisions on the course of action, depending on the epidemiological evolution. The State of Alarm, enacted on 14 March 2020, conferred full responsibility in implementing measures to the Spanish Government. All health authorities became under the direct order of the Minister of Health, with the operational management of health services remaining at the regional and local levels. The Interterritorial Council was responsible for strategic management in the preparedness and response to health threats, aiming at harmonising interventions throughout the country. 23
In France, the management of the epidemic was assumed, in March 2020, by the Government that coordinated the prevention and management plan, with the support of a scientific commission. A legal framework was created for the adoption of exceptional measures. The National Public Health Agency (Santé Publique France) also assumed responsibility for managing the epidemic, by coordinating epidemiological surveillance. At the subnational level, the role of the health authority was mainly performed by regional and municipal presidents. 23
Italy, a strongly decentralised country, experienced rapid and profound changes in health governance to tackle the pandemic. These mechanisms legitimised state intervention and the activation of the Civil Protection Department, which supports resource allocation such as medicines, medical devices, human resources and infrastructure. While, under normal circumstances, regions would enjoy a high degree of autonomy in decision making, during this period, regional structures could not override the decisions of the central government, despite maintaining some autonomy in decision making in relation to the delivery and organisation of health services. This autonomy led different regions to try different policies responses, contributing to regional asymmetries. 15 In Italy, the national influenza pandemic preparedness and response plan, elaborated in 2006, was implemented in the beginning of the COVID‐19 pandemic. Still, it did not prevent the country from being hit, in a few weeks, by the greatest health crisis since World War II. After the first cases, the State of Emergency was decreed and at the end of January 2020, a cascade of measures were implemented by the central government, with operations coordinated by the Civil Protection Department, while the National Surveillance System obtained data for monitoring the evolution of the epidemic in the various regions. 23
In Portugal, the management of the epidemic was led by the Government with the technical support of the Directorate‐General for Health and the National Institute of Health, among others. The detection of the first case in Portugal (2 March 2020) 6 occurred later than in other European countries, giving more time for preparing and implementing the response mechanisms of the health system. The Ministry of Health was empowered to authorise, regardless of the amount, the necessary expenses for the acquisition of equipment, goods and services for the prevention and treatment of the disease (Decree‐Law no. 10‐E/2020, 24th March), as well as the exemption from the formalities provided for in the Public Contracts (Decree‐Law no. 18/2010, 2nd April). The hiring of professionals was also simplified.
Regular meetings on the evolving epidemic were held between technicians from the Ministry of Health and from academia, the President of the Republic, the Prime Minister and the leaders of political parties with parliamentary representation. In April 2020, the Prime Minister appointed five Secretaries of State to coordinate the services of the central, regional and district administration and the appropriate supramunicipal coordination. The mayors ensured the coordination of social security and health services, civil protection and public security at the local level. The computer platform Trace COVID‐19 was created for follow‐up of non‐hospitalised cases, integrate levels of care and remotely manage the cases allowing for users to interact with health services. 23
The UK's response to COVID‐19 was led by the government agency Public Health England. The response was nationally coordinated, but the different nations (England, Northern Ireland, Scotland and Wales) differed in their policies depending on the capacity of the health system and on the demographic context. On 25th March 2020, emergency legislation (Coronavirus Act 2020) authorised the government to restrict the movement of infected people, limit or prohibit meetings and events, increase the number of health professionals and reduce limitations on overtime. The high case fatality rate that disproportionately affected poor and ethnic minority communities led the British government to promise to conduct an independent inquiry into the pandemic response policy. At issue is the alleged fragmentation of the NHS, public health and social entities and failures in the connection between central and local authorities. 23
3.4. Resources and reorganisation of services
In Germany, laboratory capacity in the health system was increased through the creation of other laboratory networks, in addition to those existing at the hospital level. Germany was the European Union (EU) country with the highest number of hospital beds and in intensive‐care units (ICU) beds equipped with ventilators, per a thousand inhabitants. However, it tripled its capacity. However, initially there was no centralised and coordinated response in terms of the workforce, which was dependent on local and regional initiatives. Subsequently, all part‐time professionals were asked to assume their positions full‐time, health students ordered and retired health professionals hired. Recognition of professional skills obtained abroad was simplified. 23
In Spain, the testing capacity for SARS‐CoV‐2 and the availability of personal protective equipment grew. With the declaration of State of Alarm, the Minister of Health started determining the distribution of human resources, including those of the military forces, health centres and private hospitals. The hiring of health professionals increased, eliminating barriers to hiring or extending contracts. Elective surgeries and non‐urgent consultations were postponed, and measures were introduced to foster distance care, trying, in parallel, not to discontinue essential services. 23
The French health system had to readapt, guaranteeing resources, new processes for case management and mechanisms for financing the system. Private hospitals and clinics increased their capacity by a total of 8000 beds across the country by government indication. Monetary benefits, schools and kindergartens for the children of hospital professionals in a period of confinement, psychological support lines and even activation of the medical care reserve were implemented. 23
Italy recruited 20,000 new health professionals and gave financial bonuses and retirement benefits to retain professional in the public system. 24 It separated the provision of care of people infected with COVID‐19 from the rest through exclusively dedicated structures. Private entities are presently under the obligation to provide personnel, equipment and structures, if necessary. The country ICU capacity doubled through the purchase of ventilators and reorganisation of services. 24 Guidelines and tools were equally developed to allow all health units to provide stress management and burnout prevention services to their workers. As of 1 June 2020, measures were implemented to return to regular activities, with a recommendation to prioritise remote services and reorganise schedules to avoid concentration of people.
Portugal managed to increase the capacity of UCI beds by 35% by purchasing, donation or borrowing of ventilators and further allocating of human and other technical resources. The country implemented specific legislation that facilitated the hiring of health professionals, created banks of health students and of retired professionals. Some schools were kept open during lock down to accommodate children of professionals from essential sectors, including the health sector. Health services were reorganised to concentrate services for COVID‐19 cases in dedicated areas, while protecting health professionals and efficiently use of personal protective equipment and laboratory capacity. Military hospitals and hotel structures were used to ensure response to outbreaks including those in nursing homes. Although the infrastructure and organisation of the home network is the responsibility of another ministry, the health sector has also had to guarantee this response. There were also calls for the industry to redirect its production towards the manufacture of personal protective equipment and ventilators.
In the United Kingdom, initially, all tests were performed at a single centre. Later, another laboratory was included and now this process is conducted in laboratories of Public Health England and acute trusts. Private laboratories were not asked to contribute to the expansion of testing capacity until mid‐March 2020 and offers from many laboratories were not accepted until April 2020. Subsequently, about 50 drive‐through test units were created and, to increase access, self‐test kits were made available. General capacity of hospital and ICU beds was guaranteed by using hotel units and temporary hospitals in several cities. Guidance was also issued on the rapid approval of medical devices such as ventilators without a quality certification mark. To increase the availability of health professionals, the NHS recruited 750,000 volunteers 25 and tens of thousands of former doctors and nurses expressed their interest in supporting the response, alongside with the training of medical and nursing senior students. The response to COVID‐19 was initially carried out in five specialised hospitals across the country, considered to be able to face the risk of infection. Special teams were assigned to transport confirmed cases to hospitals. As the number of cases increased, patients began to be screened at any hospital. Wards and operating rooms were transformed into ICUs to increase installed capacity. 23
3.5. Financing mechanisms
The German financing model, based on social insurance, had to adapt to new ways of remunerating services (e.g., payment of a quota for unoccupied beds, additional remuneration for a new ICU bed, per patient and per nurse). Also, in outpatient care, financial protection mechanisms were created for services not provided due to COVID‐19. Finally, in relation to citizens' social insurance, changes were introduced to cover all costs associated with laboratory tests and services provided in an outpatient or hospital setting. 23
In Italy, the epidemic was tackled with additional funds for the NHS and the Civil Protection Department through state funding and philanthropic activity and from private companies supporting regions, municipalities and health services. The use of funds has been facilitated and mechanisms have been put in place to make the use of money more transparent. 24
In Spain, a new regulation was approved in May allowing AC to use or reallocate European Regional Development Funds 2014–2020. An extraordinary fund, not counted as regional public debt, managed by AC, was approved to cover extraordinary expenses with health (e.g., tests, personal protective equipment). 23
The French Government has updated the methods of payment for acts related to COVID‐19. The funds allocated to the national health insurance cover most of the costs related to the treatment of COVID‐19, with the remainder being covered by additional funds (5% of the population is not covered for the additional costs). Since April 2020, the laboratory test has been fully reimbursed, whether performed in a hospital or in the community. 23
The Portuguese Government created a specific funding line for COVID‐19, introducing changes to the State Budget for the health sector. As the Portuguese health system is based on a universal NHS and tends to be free of charge, all citizens have access, with no additional costs related to laboratory tests, for example.
In the UK, around £1.6 billion has been made available to support local authorities, social assistance and communities. An emergency response fund of £5 billion has been established to invest in NHS, social security and public services. 23
3.6. Epidemiological results
Except for Spain and Italy (those first affected), the response of the services and the behaviour of the populations allowed for a greater distribution of the disease burden over time (Table 1; Figures 1 and 2).
TABLE 1.
Selected COVID‐19 health outcomes and other health outcomes in France, Germany, Italy, Portugal, Spain and the United Kingdom
| Country | COVID‐19 14‐day case infection per 100,000 habitants (maximum) | COVID‐19 cumulative infection rate per 100,000 habitants | COVID‐19 case fatality rate | All‐cause age group standardised mortality rate per 100,000 habitants | Maximum variation (%) in all‐cause mortality (last decade) |
|---|---|---|---|---|---|
| France | 86.4 | 490.9 | 9.3 | 21.2 | 79.3 |
| Germany | 88.7 | 303.9 | 3.7 | – | 13.2 |
| Italy | 124.0 | 461.9 | 12.8 | 22.5 | 98.2 |
| Portugal | 109.0 | 588.8 | 3.0 | 24.7 | 17.4 |
| Spain | 221.1 | 1119.7 | 5.6 | 21.5 | 154.8 |
| United Kingdom | 99.3 | 525.3 | 11.9 | 25.5 | 187.0 |
Note: COVID‐19 maximum 14‐day infection rate per 100,000 inhabitants, COVID‐19 cumulative infection rate per 100,000 inhabitants, COVID‐19 case fatality rate until 31st August 2020, all‐cause age group standardised mortality rate per 100,000 habitants between 2nd January and 2nd May 2020 and maximum variation (%) of all‐cause mortality (10 years period or latest available) between 1st January and 30th June 2020. 6 , 7 , 8
FIGURE 1.
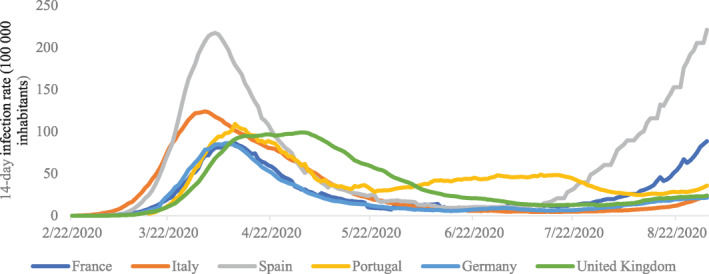
COVID‐19 14‐day infection rate per 100,000 inhabitants, in France, Germany, Italy, Portugal, Spain and the United Kingdom, between 22nd February and 31st August 2020
FIGURE 2.
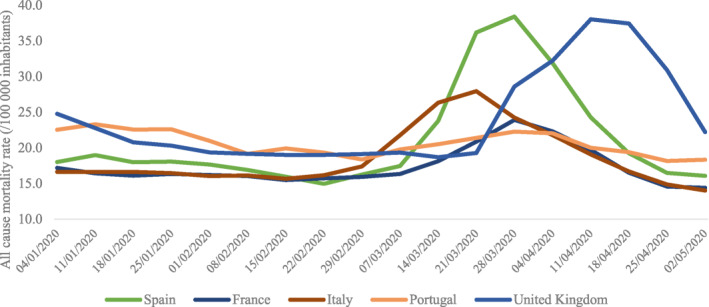
All‐cause age group standardised mortality rate per 100,000 inhabitants, per week, between 2nd January and 2nd May 2020
Italy, France and the United Kingdom have higher case fatality rates compared to Spain (country with the highest cumulative infection rate), which may be associated, for example, with the sub‐diagnosis of positive cases, virus circulation among younger age groups or differences in the protection capacity of risk groups (including nursing homes). Germany appears to have been the country that most effectively broke transmission chains since it registered the lowest cumulative infection rate along with a low case fatality rate. Portugal, despite its high cumulative infection rate, has a very low case fatality rate, which may be related to a greater capacity to detect cases throughout the epidemic.
For all countries under analysis, there seems to be an excess of mortality between late March and April 2020 when comparing to the same period of the last 10 years (Figures 2 and 3). This might have been caused directly or indirectly by COVID‐19 or a delayed access to health services. Spain and Italy have the highest mortality rate, in line with expected, due to the epidemiological situation in these countries. In the United Kingdom, the evolution of the mortality rate has a behaviour that resembles that of the COVID‐19 incidence in the country, that is, lagging in relation to the other countries under analysis. There is also an excess of mortality compared to Spain. The remaining countries do not present abnormal results, despite Portugal having a mortality baseline value (values in January and early February 2020) higher than the others.
FIGURE 3.
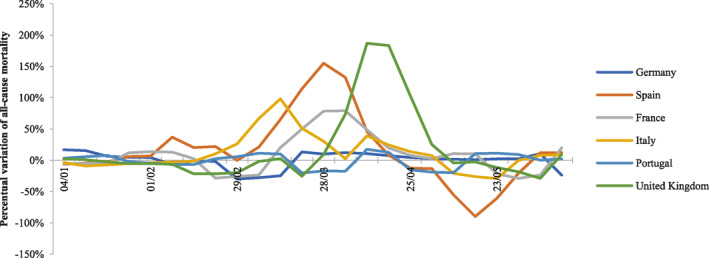
Maximum variation (%) of all‐cause mortality (10 years period or latest available) between 1st January and 30th June 2020
4. DISCUSSION
In the beginning of 2020, in the early detection phase, one of the main objectives of countries was to protect health systems so that they did not exceed their capacity to respond, especially in the hospital sector. Dispersing the occurrence of cases over time was key to maintain supply in relation to demand pose by those infected. Spain and Italy had higher peaks in incidence and may therefore have been close to the limit capacity of their health systems.
In this paper, we analyse the response in the first months of 2020 to the SARS‐CoV‐2 pandemic in Germany, Spain, France, Italy, Portugal and the United Kingdom, in light of the organisation of the state and of the type of health system. In order to complement a more qualitative analysis with epidemiological data, we have included infection rate, fatality rate and all‐cause mortality. Nevertheless, the comparisons made must be read with caution as it has obvious limitations that are common to every research using secondary epidemiological data usually collected for other purposes. 26 , 27 , 28 These limitations comprehend sensitivity, specificity, comparability, availability and quality of data. For instance, COVID‐19 infection rates depend, among others, on the reporting and epidemiological surveillance capacity, testing accessibility and coverage, population knowledge and literacy, along with public health measures in place. COVID‐19 fatality rate, on the other hand, depends on healthcare system delivery and capacity, healthcare workforce adequately prepared and trained and of an appropriate surveillance system and accurate determination of causes of death. The latter factor could have had a serious impact on the quantification of the COVID‐19 pandemic. One must bear in mind that the criteria for COVID‐19 death were being developed as the more knowledge was being gain on the disease, for instance.
The response of countries in terms of the incidence of SARS‐CoV‐2 infection varied widely. Spain was the country with the worse results: high incidence at the end of August 2020 and excess mortality. In view of the response implemented in Italy, the results obtained were also worse than those found in other countries, registering a high case fatality and an excess of mortality. Germany, on the other hand, presented qualitatively good results in all indicators. In Portugal, the results reflect the maintenance of the health system's response capacity, with low case fatality rate and the second lowest excess mortality in the countries analysed (after Germany). Despite Portugal having the second highest mortality rate standardised by all causes, the base value was already higher than that of the other countries and may not represent a consequence of the epidemic by COVID‐19. The United Kingdom, despite its low incidence, had the second highest case fatality rate, the highest standardised mortality rate and the highest excess mortality of all the countries analysed. France also had a low incidence, but a higher case fatality ratio and excess mortality than Portugal and Germany, but still lower than in the United Kingdom, Spain and Italy.
The political organisation of countries and their health system models may have partially influenced the response and, consequently, the results obtained, especially in terms of the disease burden. One might think that countries with a more centralised political‐administrative model and with a National Health Service model would be better equipped to cope with the pandemic, compared to more decentralised countries and with health systems dispersed by a plethora, somehow independent health providers. In the most decentralised countries, decisions would have to be agreed and uptake by the different levels, resulting in regional variations within countries. Nevertheless, even in more decentralised countries, we found that there was a provisional transfer of powers to the central level, in a tentative to reduce heterogeneity in measures and available resources throughout the territory.
The characteristics and the political, economic and social trajectory of each country might have been determining factors. The age structure of the population, the country's economic capacity, the relationship between the people and the State, the level and distribution of income, underlying social inequalities, the economic and social development, education or cultural characteristics, are some of factors in the equation and whose importance cannot be forgotten.
It is true that in countries with Beveridge health systems, public authorities are directly involved in the planning and management of services. The allocation of resources in these countries is a fundamental instrument in health policies and is centralised and to a more or less extension determined by central government. In countries with a Bismarck health system, the functions of the State are less evident and usually the allocation of resources occurs at a lower level, allowing for more heterogeneity according to the care delivery system. However, these models to not stand in different corners anymore and stringent differences in their foundations have now effaced. Our analysis showed that the type of health system is not self‐explanatory and sufficient to explain differences in the countries' responses, nor is it a mirror of the countries' political organisation.
5. CONCLUSIONS
The COVID‐19 pandemic has stressed the fundamental role of the provision of health services and of governance in developing and sustaining an adequate response. States, all over the world had to reorganise themselves, to fulfil one of its fundamental duties–to protect the people. Addressing health needs in times of COVID‐19 is a complex challenge: due to the novelty of the disease, to the rearrangement of the services, to the adaption of decisional structures at all levels of the society. More than the political organisation of a country or the adopted model for providing health care, the response of each country is mainly determined by the social determinants of health (e.g., age structure of the population, distribution and level of income, inequalities) and by its capacity to deal with disruption, as such, future research should focus on these aspects.
CONFLICT OF INTERESTS
Jorge Simões is with the Portuguese Ministry of Health. Gonçalo Figueiredo Augusto is currently advisor to the Assistant State Secretary for Health. André Biscaia is the national coordinator of the Action Plan for the Prevention of Violence in the Health Sector of the Directorate‐General of Health. António da Luz Pereira is currently a Clinical Auditor—Department for Healthcare Quality in the Directorate‐General of Health in Portugal. The other authors declare that there are no conflict of interests.
ETHICS STATEMENT
Publicly available data and published materials were used.
AUTHOR CONTRIBUTIONS
Jorge Simões conceptualised the study, wrote the paper and reviewed and approved the final version. João Paulo Magalhães contributed to the writing of the paper, reviewed the literature and conducted the data analysis. André Biscaia and António da Luz Pereira contributed to the writing of the paper, reviewed the literature and reviewed the paper. Gonçalo Figueiredo Augusto conceptualised the study, contributed to the writing of the paper and reviewed the paper. Inês Fronteira conceptualised the study, contributed to the writing of the paper and reviewed and approved the final version.
ACKNOWLEDGEMENTS
None.
Simões J, Magalhães JPM, Biscaia A, da Luz Pereira A, Augusto GF, Fronteira I. Organisation of the State, model of health system and COVID‐19 health outcomes in six European countries, during the first months of the COVID‐19 epidemic in 2020. Int J Health Plann Mgmt. 2021;36(5):1874‐1886. doi: 10.1002/hpm.3271
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
REFERENCES
- 1. Abduljalil JM, Abduljalil BM. Epidemiology, genome, and clinical features of the pandemic SARS‐CoV‐2: a recent view. New Microbes New Infect. 2020;35:100672. 10.1016/j.nmni.2020.100672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sakellarides C, Araújo F. A public health strategy for the COVID‐19 pandemic in Portugal: learning from international experience. Acta Med Port. 2020;33:7‐8.31928599 [Google Scholar]
- 3. Hsiang S, Allen D, Annan‐Phan S, et al. The effect of large‐scale anti‐contagion policies on the COVID‐19 pandemic. Nature. 2020;582:262‐267. [DOI] [PubMed] [Google Scholar]
- 4. Novais JR. Teoria das Formas Políticas e dos Sistemas de Governo. 2nd ed. Lisboa, Portugal: AAFDL Editor; 2019. [Google Scholar]
- 5. WHO . Estimating Mortality From COVID‐19—Scientific Brief. 2020. https://www.who.int/news‐room/commentaries/detail/estimating‐mortality‐from‐covid‐19. Accessed June 18, 2021. [Google Scholar]
- 6. Oxford COVID‐19 Government Response Tracker. Oxford, UK: Blavatnik School of Government, Oxford University; 2020. https://www.bsg.ox.ac.uk/research/research‐projects/coronavirus‐government‐response‐tracker. Accessed June 18, 2021. [Google Scholar]
- 7. European Centre for Disease Prevention and Control . Today’s data on the geographic distribution of COVID‐19 cases worldwide. 2020. https://www.ecdc.europa.eu/en/publications‐data/download‐todays‐data‐geographic‐distribution‐covid‐19‐cases‐worldwide. Accessed June 18, 2021.
- 8. Eurostat . COVID‐19: Statistics serving Europe. 2020. https://ec.europa.eu/eurostat/data/database. Accessed June 18, 2021.
- 9. Beaney T, Clarke JM, Jain V, et al. Excess mortality: the gold standard in measuring the impact of COVID‐19 worldwide? J R Soc Med. 2020;113(9):329‐334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Németh L, Jdanov DA, Shkolnikov VM. An open‐sourced, web‐based application to analyze weekly excess mortality based on the Short‐term Mortality Fluctuations data series. PLOS ONE. 2021;16(2):e0246663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stang A, Standl F, Kowall B, et al. Excess mortality due to COVID‐19 in Germany. J Infect. 2020;81(5):797‐801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Excess Deaths Associated With COVID‐19. 2021. https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm. Accessed June 12, 2021. [Google Scholar]
- 13. Islam N, Shkolnikov VM, Acosta RJ, et al. Excess deaths associated with covid‐19 pandemic in 2020: age and sex disaggregated time series analysis in 29 high income countries. BMJ. 2021;373:n1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lee E, Lee S, Sejersen TB. The Role of CRVS in Estimating COVID‐19‐Related Excess Deaths in South Korea. 2021. [Google Scholar]
- 15. Kontis V, Bennett JE, Rashid T, et al. Magnitude, demographics and dynamics of the effect of the first wave of the COVID‐19 pandemic on all‐cause mortality in 21 industrialized countries. Nat Med. 2020;26(12):1919‐1928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kontopantelis E, Mamas MA, Deanfield J, Asaria M, Doran T. Excess mortality in England and Wales during the first wave of the COVID‐19 pandemic. J Epidemiol Community Health. 2020;75:213–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Busse R, Blümel M. Germany: health system review. Health Syst Transit. 2014;16(2):1‐296. [PubMed] [Google Scholar]
- 18. Bernal‐delgado E, García‐armesto S, Peña‐longobardo LM, et al. Spain: health system review. Health Syst Transit. 2018;20(2):1‐179. [PubMed] [Google Scholar]
- 19. Chevreul K, Berg Brigham K, Durand‐Zaleski I, Hernandez‐Quevedo C. France: health system review. Health Syst Transit. 2015;17(3):1‐128. [PubMed] [Google Scholar]
- 20. Ferre F, da Belvis AG, Valerio L, et al. Italy: health system review. Health Syst Transit. 2014;16(4):1‐168. [PubMed] [Google Scholar]
- 21. Simões J, Augusto G, Fronteira I, Hernández‐Quevedo C. Portugal: health systems in transition. Health Syst Transit. 2017;30(9):1‐184. [PubMed] [Google Scholar]
- 22. Cylus J, Richardson E, Findley L, Longley M, O’Neill C, Steel D. United Kingdom: health system review. Health Syst Transit. 2015;17(5):1‐126. [PubMed] [Google Scholar]
- 23. WHO Regional Office for Europe, European Commission, European Observatory on Health Systems and Policies . COVID‐19 Health System Response Monitor [Internet]. European Observatory on Health Systems and Policies. 2020. https://www.covid19healthsystem.org/mainpage.aspx
- 24. Organization for Economic Cooperation and Development . Health System Response Tracker. OECD publishing; 2020. https://www.oecd.org/coronavirus/en/ [Google Scholar]
- 25. BBC News . NHS Volunteers to Start Receiving Tasks. BBC; 2020. [Google Scholar]
- 26. Bhopal R. Covid‐19 worldwide: we need precise data by age group and sex urgently. BMJ. 2020;369:m1366. [DOI] [PubMed] [Google Scholar]
- 27. Ricoca Peixoto V, Nunes C, Abrantes A. Epidemic surveillance of covid‐19: considering uncertainty and under‐ascertainment. Portuguese J Public Health. 2020;38(1):23‐29. [Google Scholar]
- 28. Ibrahim NK. Epidemiologic surveillance for controlling covid‐19 pandemic: types, challenges and implications. J Infect Public Health. 2020;13(11):1630‐1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.


