Abstract
Viral infections have been on the rise for the past decades. The impact of the viruses worsened amidst the pandemic burdening the already overwhelmed health care system in African countries. This article sheds light on how the coronavirus together with the already existing viral infections, some of which re‐emerged, impacted the continent. The strategies in place such as immunization, education, will have to be strengthened in all African countries to reduce the burden. Furthermore, governments can further collaborate with other countries in creating guidelines to reduce co‐infection of the diseases.
Keywords: Africa, COVID‐19, immunization, viral infections
1. INTRODUCTION
Endemic diseases remain a great public health concern around the world, especially in Africa, where a wide variety of factors, such as under‐resourced health services, dire poverty, and poor knowledge, put African nations at a greater risk for viral diseases. The attitude of Africa towards health practices mostly depends on traditional cultural beliefs. These, along with climate change, have diversely contributed to the increased risk of zoonotic and vector‐borne viral disease epidemics in the region. 1
In West African countries, for example, high rates of zoonotic transmission of human immunodeficiency virus (HIV) were observed among forest‐inhabiting hunter‐gatherers of the Pygmy and Bantu tribes. Monkeypox in Western Africa is also highly prevalent because of dependence on bushmeat by the local population. Zoonotic viral diseases were also reported in many different parts of Africa, including Rift Valley fever, Crimean‐Congo hemorrhagic fever, West Nile virus, chikungunya virus, yellow fever, and dengue fever. 1 In addition, Lassa fever also remains an epidemic‐prone rodent‐borne disease, affecting up to 500,000 individuals in Africa annually and causing approximately 5000 deaths per year in Western Africa. 2
Close contact with animals has also been indicated as a crucial factor in determining the progression of numerous viral diseases. For instance, swine farming in Africa is also known to be a driving factor for influenza virus outbreaks, with pigs being an important host for transmission of human and avian influenza strains. 1 Furthermore, contact with wild animals and subsequently human‐to‐human, is one of the main factors responsible for the recent outbreaks of Ebola on the continent. 2
The existence of numerous endemic viral diseases contributes to the overload in the health system of African countries as there is also a need to deal with simultaneous and frequent outbreaks of potentially fatal diseases. With the recent outbreak of coronavirus disease 2019 (COVID‐19), a new burden has been added to the already fragile structure of the African health system, especially that the region has already been dealing with significant sanitary issues and concerns. Hence, this paper aims to discuss the implications of viral infections amidst COVID‐19 in Africa and, ultimately, to present recommendations.
1.1. How it got worse amidst COVID‐19?
To fight infectious diseases, local and international health programs set three main objectives, which include: awareness campaigns, early diagnosis, and effective treatment. 3 These targets help eradicate viruses and limit their spread, especially in the populous Africa, whose health system is not only feeble but has also been suffering a lot. For instance, even before the pandemic, Africa had a limited health workforce already.
When COVID‐19 achieved a “pandemic” status from the World Health Organization (WHO), 3 the limited number of healthcare workers and resources in Africa had to be redirected to respond to this new threat. Hence, the pandemic has intensified the difficulty in accessing health services and has also negatively affected the surveillance, testing, treatment, and vaccination measures for other infectious diseases. In turn, this can reverse the progress made so far in reducing the prevalence and mortality from these fatal viral infections. Similar behavior has been observed in other parts of the world, such as Guinea, Brazil, India, Pakistan, and Afghanistan, where the pandemic has negatively affected the epidemiological surveillance of endemic infectious diseases like Ebola, 4 dengue, 5 , 6 chikungunya, 7 Zika, 8 polio, 9 , 10 and typhoid. 11
Meanwhile, even though models predicting a massive COVID‐19 spread in Africa turned less efficient than expected, the outcome was otherwise more accurate when it comes to studying the spread of other viruses as the new global pandemic worsened various infectious diseases across the sub‐Saharan region. 12 One of the main reasons is that due to national lockdowns, mass population immunization had to be halted at first, which increased the risk of a new surge in the existing infectious illnesses. 13
The COVID‐19 pandemic also made an impact on the management of chronic viral diseases such as HIV. It is estimated that over the coming year (2020–2021), a six‐month complete interruption in HIV response could result in more than 500 000 fatalities in Sub‐Saharan Africa. 14 Moreover, at the beginning of the pandemic, many scientists and international institutions feared that with the imposed lockdowns and the concerns of catching the coronavirus, ill people would have difficulties getting their regular treatment. These concerns turned true, as several reports showed that about 13% to even 50% of people could not get their medications in South Africa, Kenya, and Nigeria as of May 2020. 12 , 13 , 15 In Zimbabwe, patients usually would not be able to get a refill for their antiretroviral drug against HIV infection. 16
In fact, the World Health Organization confirmed that last 2020, five countries in sub‐Saharan Africa where the HIV treatment stock was sufficient to only 3 months or less. Even though these declines were later recuperated in July during that same year, and HIV patients taking treatment in 2020 were slightly higher than in 2019, 17 recent studies have shown that antiretroviral medication initiations and HIV testing decreased sharply by 50% in April, with only a slight improvement over the next months, never reaching their pre‐lockdown levels. 17 , 18 The Central African Republic adopted an extensive National HIV Strategic Plan 2021–2025 in 2020, with the goal of eliminating inequality, halving HIV Infections, and ensuring that 95% of HIV patients have the therapeutic benefit of ART by 2025. 19 Meanwhile, UNAIDS’ 2020 targets were to: (a) newly diagnose 1.1 million people that have HIV; (b) provide 3 million additional patients on treatment; and, (c) help also 3 million people achieve viral suppression. 17 Although the last mentioned target was somehow accomplished by keeping patients on their regular medications, the first two were not fully attained.
These failures can be explained by different causes. First, resources and healthcare workers were diverted from the HIV departments to the COVID‐19 to help fight the pandemic. For example, in South Africa, 28,000 HIV employees changed positions. 18 Moreover, the lack of large centers enabling social distancing, the reduced staff and operation times among most establishments, as well as the challenges involved in attending facilities during lockdowns from transport struggles to high costs and scarce resources, have made people less engaged to refer to the clinics and seek help. 18
In consequence, the United Nations program to fight AIDS has failed more than what was expected, bringing back the situation and making it miss its 90–90–90 goal for the year 2020. However, it is worth noting that the findings suggest that worse projected studies did not play out and large disruptions in HIV management did not happen; hence, HIV morbidity and mortality were not highly affected. 18
On the other hand, other contagious infectious diseases were even more disrupted by the COVID‐19 pandemic. Measles, for example, is an infection currently affecting 15 countries in the sub‐Saharan African region and is getting on a rise in recent years due to many factors—of which, limited health systems are one. In 2019 alone, the disease killed more than 6000 people in the Democratic Republic of Congo. 20 The COVID‐19 pandemic has even worsened the immunization campaigns against the Measles virus, leaving extra 1.32 million African children under one‐year‐old without the first dose of their measles vaccine between the period of January and August 2020, as compared to 2019. 21 Moreover, in April 2020, about 24 countries were reported to have paused measles vaccination following the guideline released by WHO. 22 Thus, the increased numbers of unvaccinated populations in Africa may result into higher risks of childhood mortality and in future measles outbreaks.
Aside from the measles outbreak, the WHO (2020) also confirmed yellow fever cases in South Sudan. Although there is no record of an outbreak in the country, wherein the last was registered in November 2018 23 the appearance of new cases shows how fragile the situation is and how easily the reduction of measures to prevent disease, especially vaccination, can lead to change in epidemiological control of the disease. Meanwhile, among the main reasons for Ebola and Lassa Fever outbreaks in the region is the socioeconomic downturn due to COVID‐19, which has also affected the surveillance and treatment of patients infected within countries where they are prevalent. In addition, swift case detection and contact tracing are paramount for surveillance for these viral infections, especially the Ebola virus which has been noted to be similar to COVID‐19. 24 However, lessons learned in previous outbreaks, such as the Ebola outbreak in the Democratic Republic of Congo, have been efficient in guiding response to COVID‐19 in these countries. 25
There is also a relatively higher seroprevalence of arboviruses, like dengue in Africa, compared to the number of reported outbreaks, as cases go undetected owing to the poor public health systems in many African countries. 26 This could also be the case for other viral infections, as public health attention is mainly on COVID‐19 surveillance and vaccination. Furthermore, many other local viruses with no big outbreaks are being fought all over the African countries, leaving the continent with a high disease burden.
1.2. Implications of the coexistence of the COVID‐19 pandemic and other viral infectious diseases
Africa is a high‐risk area for the spread of viral diseases mainly due to overpopulation, poverty, under‐resourced health care system, inadequate healthcare workforce, low testing capacities, and poor surveillance system present in the region. Of 25 countries highly exposed to infectious diseases reported by Infectious Disease Vulnerability Index in 2016, 22 were from the African region. 27 According to WHO Africa, 213 million Africans are infected with malaria, 71 million with hepatitis B and C, 2.5 million with tuberculosis, and 26 million with HIV. 28 , 29 , 30 , 31 Owing to the combined effects of these infectious diseases, coupled with the recent emergence of the COVID‐19 pandemic in Africa, health systems in the region are experiencing a major burden from these infectious diseases.
As focus shifts to COVID‐19 management, data on viral infections in most African nations is scarce and unclear, resulting in a lapse in contact tracing and management of patients who are left undiagnosed and untreated. The fact that many viral diseases have similar clinical presentations may exacerbate the problem. This can have a negative effect, mainly because there may be an overlap of symptoms between diseases, making diagnosis and management of a specific disease entity more difficult.
For instance, COVID‐19, which is caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), is a disease characterized predominantly by the involvement of the lower respiratory tract—with fever and neurological damage (or mental status alteration) as some of its clinical findings Such signs and symptoms from a patient may coincide with other viral infections common in the continent such as yellow fever, 32 dengue, and tick‐borne encephalitis which may further cause confusion and delay of the necessary and appropriate treatment methods. 33 Ultimately, this can aggravate the current health condition of the patient, which may lead to unfavorable clinical outcomes and worse prognosis, especially when the patient is confirmed to have the SARS‐CoV‐2 infection while suffering from another underlying disease such as HIV‐AIDS.
1.3. Recommendations
In response to the challenges brought about by the coexistence of COVID‐19 and other viral infections in the African regions, the following are therefore recommended:
(1) Strengthen the call for immunization against common viral infections, including COVID‐19.
(2) Promote awareness and education on the benefits of vaccination, especially among the vulnerable populations.
(3) Promote community engagement through cultural and religious leaders.
(4) Enable risk communication in local languages for quick identification of red flag symptoms of the various viral infections, especially in local communities.
(5) Equip healthcare workers with proper protection and hazard pay benefits as well as health infrastructures with better facilities and equipment.
(6) Use telemedicine as one of the options for healthcare workers to reach patients safely as well as to overcome the challenges of the low workforce and strengthen infectious disease surveillance. Poor power supply and internet connection, lack of political will, and poor infrastructure are major factors affecting the implementation of telemedicine in local communities. However, efforts to mitigate these challenges will provide cost‐effective and sustainable improvement in infectious disease surveillance, response, and vaccination in resource‐limited settings in Africa. 34
(7) Conduct extensive profiling of COVID‐19 cases throughout the African continent so as to increase the knowledge and preparedness regarding the disease's various clinical presentations among its populations and how such may coincide with other possible viral infections that are already present and prevalent in these regions even before the pandemic.
A summary of challenges and recommendations is provided in Figure 1.
Figure 1.
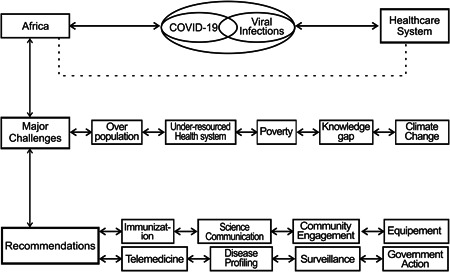
A summary of challenges and recommendations to combat viral infections amid the COVID‐19 pandemic in Africa
2. CONCLUSION
It has been a huge struggle for African countries to curtail the spread of COVID‐19, especially with the emergence and/or presence of other viral infection outbreaks, given the limited healthcare workforce, inadequate medical infrastructures and equipment, similarities with respect to the clinical presentations, and disturbances in the continuity of immunization and COVID‐19 surveillance. Hence, the COVID‐19 pandemic has exacerbated the already poor healthcare response of Africa to other viral diseases such as HIV, measles, dengue, and Ebola—making the continent more vulnerable and less able to fight these already existing multiple viruses. Even worse, the status was aggravated as many new people were left undiagnosed as well as improperly and/or inadequately attended to among the various healthcare units. Hence, various recommendations have been duly presented to ultimately decrease the mortality and morbidity among African populations, especially with the presence of detrimental but treatable and preventable viral infections amidst the COVID‐19 pandemic.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Mohammad Yasir Essar conceived the idea and design for this manuscript; Olivier Uwishema, Irem Adanur, Abdulhammed Opeyemi Babatunde, Osman Kamal Osman Elmahi, Kolawole Barakat Olajumoke, and Nzeribe Emmanuella wrote the first draft; Mohammad Mehedi Hasan and Ana Carla dos Santos Costa edited the second draft; Shoaib Ahmad and Mohammad Yasir Essar made the critical comments and revision; Mohammad Mehedi Hasan edited the final draft. All authors revised and approved the final draft.
Uwishema O, Adanur I, Babatunde AO, et al. Viral infections amidst COVID‐19 in Africa: Implications and recommendations. J Med Virol. 2021;93:6798‐6802. 10.1002/jmv.27211
REFERENCES
- 1. Chauhan RP, Dessie ZG, Noreddin A, El Zowalaty ME. Systematic review of important viral diseases in africa in light of the ‘one health’ concept. Pathogens. 2020;9(4). 10.3390/pathogens9040301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Usuwa IS, Akpa CO, Umeokonkwo CD, et al. Knowledge and risk perception towards Lassa fever infection among residents of affected communities in Ebonyi State, Nigeria: implications for risk communication. BMC Public Health. 2020;20(1):217. 10.1186/s12889-020-8299-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. WHO Director‐General's opening remarks at the media briefing on COVID‐19—11 March 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Accessed April 30, 2021.
- 4. Aborode AT, Tsagkaris C, Jain S, et al. Ebola outbreak amid COVID‐19 in the Republic of Guinea: priorities for achieving control. Am J Trop Med Hyg. 2021;104(6):1966‐1969. 10.4269/ajtmh.21-0228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Phadke R, Mohan A, Çavdaroğlu S, et al. Dengue amidst COVID‐19 in India: The mystery of plummeting cases. J Med Virol. 2021;93(7):4120‐4121. 10.1002/jmv.26987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rabiu AT, Mohan A, Çavdaroğlu S, et al. Dengue and COVID‐19: A double burden to Brazil. J Med Virol. 2021;93(7):4092‐4093. 10.1002/jmv.26955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jain S, Rocha ICN, Maheshwari C, et al. Chikungunya and COVID‐19 in Brazil: The danger of an overlapping crises. J Med Virol. 2021;93(7):4090‐4091. 10.1002/jmv.26952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Costa AC, Dos S, Hasan MM, Xenophontos E, et al. COVID‐19 and Zika: An emerging dilemma for Brazil. J Med Virol. 2021;93(7):4124‐4126. 10.1002/jmv.27006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ahmad S, Babar MS, Ahmadi A, Essar MY, Khawaja UA, Lucero‐Prisno DE. Perspective piece polio amidst COVID‐19 in Pakistan: What are the efforts being made and challenges at hand? Am J Trop Med Hyg. 2021;104(2):446‐448. 10.4269/ajtmh.20-1438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ahmadi A, Essar MY, Lin X, Adebisi YA, Lucero‐Prisno DE. Polio in Afghanistan: the current situation amid COVID‐19. Am J Trop Med Hyg. 2020;103(4):1367‐1369. 10.4269/ajtmh.20-1010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ahmad S, Tsagkaris C, Aborode AT, et al. A skeleton in the closet: The implications of COVID‐19 on XDR strain of typhoid in Pakistan. Public Heal Pract. 2021;2:100084. 10.1016/j.puhip.2021.100084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yiba . HSRC Study on COVID‐19. https://yiba.co.za/hsrc-study-on-COVID-19-indicates-overwhelming-compliance-with-the-lock-down/. Accessed May 1, 2021.
- 13. Hosken G. Sunday Times. Coronavirus fears keep HIV, TB patients from medication. https://www.timeslive.co.za/sunday-times/news/2020-05-17-coronavirus-fears-keep-hiv-tb-patients-from-medication/. Accessed May 1, 2021.
- 14. UNAIDS report on the global AIDS epidemic shows that 2020 targets will not be met because of deeply unequal success; COVID‐19 risks blowing HIV progress way off course. UNAIDS. https://www.unaids.org/en/resources/presscentre/pressreleaseandstatementarchive/2020/july/20200706_global-aids-report. Accessed June 3, 2021.
- 15. Trust Finmark. Livelihood impacts of Covid‐19 in Kenya, Nigeria and South Africa. https://techcentral.co.za/livelihood-impacts-of-COVID-19-in-kenya-nigeria-and-south-africa/97669/. Accessed May 1, 2021.
- 16. International AIDS Society . COVID‐19 DSD Resources Community responses and perspectives. https://differentiatedservicedelivery.org/Resources/Resource-Library/COVID-19-DSD-Resources-Community-responses. Accessed May 1, 2021.
- 17. UNAIDS . Report of the Secretary General. https://www.unaids.org/en. Accessed May 1, 2021.
- 18. Dorward J, Khubone T, Gate K, et al. The impact of the COVID‐19 lockdown on HIV care in 65 South African primary care clinics: an interrupted time series analysis. Lancet HIV. 2021;8(3):e158‐e165. 10.1016/S2352-3018(20)30359-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Central African Republic : producing HIV estimates in the context of crisis. UNAIDS. https://www.unaids.org/en/resources/presscentre/featurestories/2021/january/20210128_central-african-republic. Accessed June 3, 2021.
- 20. Deaths from Democratic Republic of the Congo measles outbreak top 6000. WHO . https://www.afro.who.int/news/deaths-democratic-republic-congo-measles-outbreak-top-6000. Accessed June 3, 2021.
- 21. Regional Office for Africa . Opening statement, COVID‐19 Press Conference, 5 November 2020. https://www.afro.who.int/fr/node/13599. Accessed May 1, 2021.
- 22. Roberts L. Measles is on the rise—and COVID‐19 could make it worse. https://media.nature.com/original/magazine-assets/d41586-020-01011-6/d41586-020-01011-6.pdf. Accessed May 1, 2021.
- 23. WHO . Yellow fever—Republic of South Sudan. https://www.who.int/csr/don/10-april-2020-yellow-fever-south-sudan/en/. Accessed May 1, 2021.
- 24. Rugarabamu S, Mboera L, Rweyemamu M, et al. Forty‐two years of responding to ebola virus outbreaks in Sub‐Saharan Africa: a review. BMJ Glob Heal. 2020;5(3):1955. 10.1136/bmjgh-2019-001955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mobula LM, Samaha H, Yao M, et al. Recommendations for the COVID‐19 response at the national level based on lessons learned from the ebola virus disease outbreak in the Democratic Republic of the Congo. Am J Trop Med Hyg. 2020;103(1):12‐17. 10.4269/ajtmh.20-0256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Simo FBN, Bigna JJ, Kenmoe S, et al. Dengue virus infection in people residing in Africa: a systematic review and meta‐analysis of prevalence studies. Sci Rep. 2019;9(1):1‐9. 10.1038/s41598-019-50135-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. COVID‐19 cases top 10 000 in Africa. WHO. https://www.afro.who.int/news/covid-19-cases-top-10-000-africa. Accessed May 10, 2021.
- 28. Moeti M. World AIDS Day 2019—Message of WHO Regional Director for Africa. WHO. https://www.afro.who.int/regional-director/speeches-messages/world-aids-day-2019-message-who-regional-director-africa-dr. Accessed May 10, 2021.
- 29. Moeti M. World Hepatitis Day 2019—Message of WHO Regional Director for Africa. WHO. https://www.afro.who.int/regional-director/speeches-messages/world-hepatitis-day-2019-message-who-regional-director-africa. Accessed May 10, 2021.
- 30. World Tuberculosis Day 2019. WHO. https://www.afro.who.int/media-centre/events/world-tuberculosis-day-2019. Accessed May 10, 2021.
- 31. The “World malaria report 2019” at a glance. https://www.who.int/news-room/feature-stories/detail/world-malaria-report-2019. Accessed May 10, 2021.
- 32. Çavdaroğlu S, Hasan MM, Mohan A, et al. The spread of Yellow fever amidst the COVID‐19 pandemic in Africa and the ongoing efforts to mitigate it. J Med Virol. April 2021:7. jmv.2702. 10.1002/jmv.27027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Baig AM. Neurological manifestations in COVID‐19 caused by SARS‐CoV‐2. CNS Neurosci Ther. 2020;26(5):499‐501. 10.1111/cns.13372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Okereke M, Babatunde AO, Samuel ST, Ogunkola IO, Mogessie YG, Lucero‐Prisno DE. Applications of telemedicine in the supply and distribution of COVID‐19 vaccines in Africa. J Glob Health. 2021;11:03039. 10.7189/jogh.11.03039 [DOI] [PMC free article] [PubMed] [Google Scholar]


