Abstract
Anchored on the Ecological Systems Theory, this study aimed to determine how psychological distress operates as an underlying mechanism in the impact of socio‐ecological factors on the quality of life of Filipino adults during coronavirus disease 2019 (COVID‐19) crisis. A cross‐sectional online survey was conducted to assess perceptions of 401 adults on socio‐ecological factors (i.e., safety at home, trust in public institutions, and financial difficulties), psychological distress, and quality of life during the early phase of COVID‐19 community quarantine in the Philippines. Using latent variable path analysis, all three socio‐ecological factors have significant direct effects on both psychological distress and quality of life. More importantly, the proposed model was confirmed in terms of a significant partial mediation of psychological distress on the impact of safety at home, trust in public institutions, and financial difficulties on the quality of life of Filipino adults. The study offers novel insights into the role of psychological distress as an underlying mechanism that operates on the influence of socio‐ecological factors on the quality of life of adults during a global health crisis. Implications on psychological interventions and policies in preventing mental health problems vis‐à‐vis improving Filipinos' quality of life during the COVID‐19 pandemic are discussed.
Keywords: COVID‐19, Philippines, psychological distress, quality of life, socio‐ecological factors
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic has disrupted the lives of billions of people across the world. Millions of people worldwide have lost their family members, friends, and their livelihood (OECD, 2020; World Health Organization, 2021a). Corollary to this is the prevalence of mental health concerns across the world (United Nations, 2020). A global health crisis such as the COVID‐19 pandemic brings about consequences in the different layers of society. Hence, examining people's quality of life during the pandemic has to be viewed from a perspective that takes into account the different layers of a person's environment. While a few recent studies have focused on identifying the antecedents of people's quality of life during the COVID‐19 crisis, one noticeable gap is the limited research that examined the predictors of quality of life during the pandemic within the socio‐ecological framework. The socio‐ecological framework (Bronfenbrenner, 1979) proposed that the factors in a person's wider environment could indirectly affect one's development, including emotional distress and well‐being. The objective of the present study was to examine the influence of socio‐ecological factors that include individual‐level (i.e., psychological distress), family‐level (i.e., safety at home and financial difficulties), and societal‐level (i.e., trust in public institutions [TPIs]) on the quality of life in a sample of adults in the Philippines during the COVID‐19 crisis. More specifically, we tested a model showing the mediating influence of psychological distress on the impact of safety at home, TPIs, and financial difficulties on Filipino adults' quality of life amid the pandemic.
1.1. The COVID‐19 pandemic
Since the discovery of the COVID‐19 infection in China in December 2019, it has quickly spread across the world resulting in a global pandemic. Countries across the world implemented a strict lockdown for several months to minimize virus transmission. Despite the implementation of lockdowns and health protocols, the COVID‐19 has infected and killed millions of people worldwide. As of May 2021, there are >165 million infected people with >3.4 million deaths worldwide (World Health Organization, 2021a). In terms of economic impact, the pandemic has resulted in an economic shutdown in many countries, which caused high unemployment rates (International Labor Organization, 2020).
In the Philippines, the national government implemented a community quarantine (lockdown) in Metro Manila and the entire island of Luzon on March 16, 2020, and later extended to the rest of the country due to the rapid local transmission of the COVID‐19 virus (ECQ and GCQ Guidelines, 2020). Varying forms of community quarantines were implemented across the country based on the scale of contagion. For example, an enhanced community quarantine (ECQ) was implemented in areas with high rates of transmission, strictly requiring citizens to stay at home and could leave their homes only for essential activities (e.g., buying food). Areas under ECQ canceled most public transportations, closed businesses and public offices, and implemented a work‐from‐home working arrangement. On the other hand, general community quarantine (GCQ) was a less stringent type of lockdown in areas with a decreasing trend of COVID‐19 cases. Under GCQ, local communities are allowed to operate public transportation and businesses but with reduced capacity. Later on, other forms of community quarantines were implemented (ECQ and GCQ Guidelines, 2020). The COVID‐19 pandemic has caused the closure of many small businesses and a reduction in the manpower of larger businesses in the country, which led to an unprecedented unemployment rate. The Philippine Statistics Authority (PSA) reported a staggering unemployment rate in the country with nearly 18% in April 2020 (Philippine Statistics Authority, 2020). Based on a mobile phone survey released in July 2020, the job loss has reached approximately 46% (Social Weather Stations, 2020). As of May 2021, there were >1.1 million confirmed COVID‐19 cases with >19,000 deaths in the country (World Health Organization, 2021b). For a developing nation like the Philippines, the adversities caused by the COVID‐19 pandemic can have a greater impact on the quality of life of its citizens. To further understand the quality of life among individuals in a developing nation, we aim to identify the socio‐ecological antecedents of quality of life using a sample of adults from the Philippines.
1.2. Socio‐ecological predictors of quality of life
Previous research has identified several predictors of quality of life. For instance, evidence found that social support among caregivers in Ireland (Brand et al., 2016), religiosity among caregivers in the United States (Banthia et al., 2007), lesser feelings of loneliness among older chronically ill Appalachians (Theeke et al., 2012), and social participation among patients with multiple sclerosis (Mikula et al., 2017) were found to be important factors in improving the quality of life. On the other hand, lower education and income were found to be associated with poor quality of life among caregivers in the United States (Banthia et al., 2007). During the COVID‐19 crisis, the quality of life of people worldwide has been significantly affected (Lieberoth et al., 2021; Van Bavel et al., 2020; Yamada et al., 2021). For instance, recent research showed that job loss and financial struggles can reduce the quality of life among people in Japan (Ikeda et al., 2021). Moreover, the psychological distress brought about by the pandemic can decrease the quality of life among residents in China and Vietnam (An et al., 2020; Ma et al., 2020; Nguyen et al., 2020; Zhang & Ma, 2020). Additionally, residents in Portugal (Ferreira et al., 2021) who experience higher anxiety reported lower levels of quality of life during home quarantine in the days of the pandemic. On the other hand, better physical health, more frequent physical exercises, and lower depression and anxiety symptoms were found to be associated with better quality of life among residents in Italy and Israel during the pandemic (Aharon et al., 2021). Furthermore, governmental support and programs were found to be effective in maintaining people's quality of life in Japan (Ikeda et al., 2021).
Despite the ubiquitous interest in quality of life among researchers, two critical limitations were identified. First, although previous evidence showed that several factors on a person's environment (e.g., personal characteristics and resources, social support, governmental support) could indirectly influence one's quality of life (Banthia et al., 2007; Brand et al., 2016; Zhang & Ma, 2020), there is a noticeable lack of research that examined the predictors of people's quality of life within a socio‐ecological framework. Second, there is a paucity of studies that investigated people's quality of life in developing countries during a global health crisis such as the COVID‐19 pandemic.
During the COVID‐19 crisis, people's lives have been changing due to the consequences of the pandemic (e.g., unemployment, isolation, and health threats) and the adjustments (e.g., lockdown and prohibition of social gatherings) that societies needed to make to respond effectively to the crisis. Guided by the literature, we selected relevant factors in a person's socio‐ecological environment, such as psychological distress (individual‐level factor), safety at home (family‐level factor), financial difficulties in the family caused by the COVID‐19 crisis (family‐level factor), and TPIs (societal‐level factor) that can potentially contribute to the quality of life. In terms of individual‐level factors, emerging studies conducted during the COVID‐19 pandemic showed that psychological distress negatively predicted quality of life (An et al., 2020; Ma et al., 2020; Nguyen et al., 2020; Zhang & Ma, 2020). For example, evidence showed that experiencing psychological distress during COVID‐19 resulted in a significant decline in the quality of life among COVID‐19 patients, frontline nurses, and residents in China (An et al., 2020; Ma et al., 2020; Zhang & Ma, 2020) and those with suspected COVID‐19 symptoms in Vietnam (Nguyen et al., 2020).
In terms of family‐level factors, studies suggest that financial difficulties and one's sense of safety at home influence quality of life (Lam et al., 2017; Mulvey, 2002). For example, individuals from low‐income families reported poor quality of life among the general population in Hong Kong (Lam et al., 2017). On the other hand, residents in the United States who reported greater threats to their safety at home and in the community reported lower levels of quality of life (Mulvey, 2002). In terms of societal‐level factors, previous studies highlighted the importance of people's TPIs to their quality of life in times of adversities. For example, findings among the survivors of the Sichuan earthquake in China demonstrated that individuals with lower trust in their government showed declining levels of quality of life (Liang, 2016). Taken together, the present study proposed that socio‐ecological factors, such as psychological distress, safety at home, financial difficulties, and trust in institutions can contribute to the quality of life among Filipino adults during the COVID‐19 pandemic.
1.3. Psychological distress as an underlying mechanism
We reason that psychological distress can operate as a mediating mechanism that links the influence of socio‐ecological factors (i.e., safety at home, TPIs, and financial difficulties) on people's quality of life. Studies showed that experiencing a greater sense of safety at home during the COVID‐19 pandemic was associated with lower levels of emotional distress among adult Filipinos (Aruta, 2021) and Israeli Jews (Kimhi, Eshel, et al., 2020a). Moreover, TPIs serves as a protective factor against emotional distress in people across 58 countries during the COVID‐19 crisis (O'Hara et al., 2020). Furthermore, people who faced financial difficulties due to COVID‐19 reported higher levels of psychological distress (Aruta, 2021; Kimhi, Marciano, et al., 2020b). Given the evidence on the influence of socio‐ecological factors, including safety at home, TPIs, and financial difficulties on psychological distress, and substantial evidence on the link between psychological distress and quality of life (Aharon et al., 2021; An et al., 2020; Ferreira et al., 2021; Ikeda et al., 2021; Ma et al., 2020; Nguyen et al., 2020; Zhang & Ma, 2020), we speculate that psychological distress can serve as an underlying mechanism that mediates the influence of socio‐ecological factors on people's quality of life. We presented our hypothesis in the next part of this article.
1.4. The present study
To our knowledge, there are no studies that examined the socio‐ecological factors influencing the quality of life in the context of the COVID‐19 crisis in the Philippines. Anchored on the Ecological Systems Theory (Bronfenbrenner, 1979), the present study investigated the socio‐ecological determinants of quality of life among Filipino adults during the COVID‐19 pandemic. Ecological Systems Theory (Bronfenbrenner, 1979) proposed that an individual's mental health, including one's quality of life, is influenced by several systems: microsystems, mesosystems, exosystems, and macrosystems. Factors within these systems range from the aspects that directly influence a person (i.e., individual capacities and characteristics) to factors that indirectly influence a person that includes family characteristics (e.g., relationships, support, and socioeconomic status) and societal factors (e.g., public institutions).
This study examined the socio‐ecological determinants of quality of life in terms of psychological distress (individual‐level factor), safety at home and financial difficulties (family‐level factor), and TPIs (societal‐level factor) among Filipino adults during the COVID‐19 crisis. Bronfenbrenner (1979) explained that while a person's characteristics or individual‐level factors directly influence a person's development, mental health, and quality of life; there are also factors in the immediate and extended environment that can play an indirect role in an individual's quality of life. We propose that psychological distress, as an individual‐level factor, may operate as a mechanism mediating the indirect impact of the ecological‐level factors, such as safety at home, financial difficulties, and trust in institutions on the quality of life of Filipino adults.
Simply put, we sought to examine the following hypotheses:
-
1.
Individuals with a greater sense of safety and TPIs during the COVID‐19 crisis at home will report greater levels of quality of life.
-
2.
Individuals who faced more financial difficulties during the COVID‐19 crisis will report lower levels of quality of life.
-
3.
Psychological distress will mediate the positive impact of safety at home and trust in institutions on the quality of life.
-
4.
Psychological distress will mediate the negative impact of financial difficulties on quality of life.
2. METHOD
2.1. Participants
The study involved 401 adults with ages ranging from 18 to 68 years old (M = 30.09, SD = 11.14), who were recruited using convenience and snowball sampling during the early phase of community quarantine in the Philippines. Slightly more than half of the participants were in the age bracket 22–29 years (55.36%), and most participants reported being single (72.57%). There were 146 males (36.41%), 254 females (63.34%), and one did not report gender. In addition, the majority of participants earned bachelor's degrees (66.83%), and more than a third of them reported having higher than average income (39.40%).
2.2. Instruments
2.2.1. Psychological distress
Psychological distress during the COVID‐19 pandemic was assessed using eight items from the Brief Symptoms Inventory (BSI; Derogatis & Savitz, 2000; Derogatis & Spencer, 1982), which described symptoms related to anxiety (e.g., “A feeling of tension”) and depression (e.g., “A feeling of worthlessness”). Participants responded to the items on a 5‐point scale, from 1 = not at all to 5 = to a very great extent with a higher score indicating greater distress symptoms. Previous studies utilized the abbreviated BSI as a valid and reliable tool in measuring distress symptoms in Filipino (Callueng et al., 2020) and Jewish Israeli (Kimhi, Eshel, et al., 2020a) adults during the COVID‐19 crisis. In this study, the confirmatory factor analysis (CFA) solution of the abbreviated BSI scale yielded an adequate data fit for a modified single‐factor model: χ 2 = 69.21, df = 18, p = 0.00, comparative fit index (CFI) = 0.96, Tucker–Lewis index (TLI) = 0.94, standardized root mean square residual (SRMR) = 0.04, root mean square error approximation (RMSEA) = 0.08. All items had strong factor loadings (λ), ranging from 0.51 to 0.81. Model fit was improved by allowing error terms of Items 1 and 6 as well as Items 6 and 7 to correlate. Participants' responses yielded high reliability (α = 0.90 and ω = 0.91).
2.2.2. Quality of life
The 9‐item My Life Today (MLT) scale (Kimhi & Eshel, 2009; Kimhi & Shamai, 2004) was used to measure the participants' perceptions of various life domains (e.g., health), including the assessment of life in general. The participants responded to the question, “What is your life like at the present?”, and rated each item on a 6‐point scale (1 = not good at all to 6 = very good). An overall index of quality of life was calculated by summing up the scores in all items. Recent studies utilized MLT as a valid instrument in assessing people's life quality with an internal consistency of α = 0.82 (Kimhi, Eshel, et al., 2020b; Kimhi, Marciano, et al., 2020a). In this study, the CFA solution of the MLT scale yielded an adequate data fit for a modified single‐factor model: χ 2 = 65.24, df = 26, p = 0.00, CFI = 0.95, TLI = 0.94, SRMR = 0.04, RMSEA = 0.06. All items had strong factor loadings (λ), ranging from 0.44 to 0.80. Model fit was improved by allowing errors of Items 4 and 8 to correlate. Participants' scores yielded high reliability (α = 0.86 and ω = 0.86).
2.2.3. TPIs
TPIs was measured using five items from the National Resilience Scale (Kimhi & Eshel, 2019) that was part of a larger international survey to assess the extent of trust in national government during the COVID‐19 crisis. Participants were asked to rate their level of TPIs (i.e., education, police, health, media, and legislative) using a 6‐point scale, from 1 = no trust at all to 6 = very high trust. In this study, the CFA solution of the TPI yielded an adequate data fit for a modified single‐factor model: χ2 = 4.18, df = 2, p = 0.12, CFI = 0.99, TLI = 0.99, SRMR = 0.01, RMSEA = 0.06. All items had strong factor loadings (λ), ranging from 0.81 to 0.86. Participants' scores yielded high reliability (α = 0.88 and ω = 0.88).
2.2.4. Safety at home
Safety at home during the COVID‐19 crisis was assessed using a single item, “How safe are you at your home during this period of the Coronavirus crisis?” Participants responded using a 5‐point scale from 1 = not at all to 5 = to a very great extent. Recent studies used this item in assessing Israeli adults' feelings of safety at home during the COVID‐19 crisis (Kimhi, Eshel, et al., 2020a).
2.2.5. Financial difficulties in the family
Financial difficulties faced by one's family as a result of the COVID‐19 crisis was measured using a single item, “Do you or your family currently experience financial difficulties due to the Coronavirus crisis (such as unemployment, reduced business activity, and so on)?” Participants responded to this item using a 5‐point scale (1 = not at all to 5 = to a very great extent).
2.3. Procedures
Guided by the double‐translation and reconciliation method (International Test Commission, 2018), we translated all items from English to the Filipino language. First, two bilingual experts who are native speakers of the Filipino language translated the survey materials from English to Filipino independently. Second, a third expert who also is a native speaker of Filipino reviewed the materials item by item. Lastly, all three experts discussed together identifying the areas for corrections with consideration for the linguistic, psychological, and cultural equivalence. After reconciling the areas for improvement, the three experts arrived at the final translated version of the survey.
The current research was part of a cross‐country study approved by the Institutional Review Board of the Tel Aviv University. Local approval was secured from the administration of Cavite State University‐General Trias. The survey materials were transformed into an online questionnaire. After securing informed consent, the participants completed the online survey. Data were collected during the early phase of community quarantine in the Philippines, which was between the last week of April and the second week of May in 2020.
2.4. Data analysis
Several analytical procedures were employed in the data. Initially, psychometric properties of the BSI abbreviated version, MLT scale, and TPI scale were evaluated through CFA for construct validity and Cronbach α for reliability. CFA was conducted for each scale using maximum likelihood (ML) estimation in Mplus 7.0 (Muthén & Muthén, 1998‐2012). The goodness of data‐model fit was evaluated using CFI and TLI values between 0.90 and 0.95 as well as RMSEA and SRMR values of < 0.08 as criteria for an adequate model fit. CFI and TLI values > 0.95 and RMSEA and SRMR values < 0.05 were criteria for a good model fit (Kenny, 2014; Kline, 2011). In addition, factor loadings of λ ≥ 0.50 were considered as strong such that they account for ≥ 0.25% of the variance on the latent factor (Renshaw, 2018). For scale reliability, Cronbach's α and McDonald's omega (ω) were estimated to assess the internal consistency of scores, with α and ω ≥ 0.70 indicating strong reliability. CFA and reliability cannot be estimated for safety at home and financial difficulties since these variables were assessed by a single item only.
Next, descriptive statistics and normality assumption procedures were calculated for each study variable. Bivariate correlation using Pearson r also was established between the study variables. These procedures were calculated using IBM SPSS Statistics 27.
Finally, latent variable path analysis (LVPA) through structural equation modeling (SEM) was conducted to examine the direct effects of socio‐ecological factors on quality of life. ML estimation was employed using Mplus 7.0 (Muthén & Muthén, 1998‐2012). SEM was recommended for mediation analysis as it allows for a simplified estimation of more complicated mediation models in a single analysis (Gunzler et al., 2013; Hayes & Preacher, 2013), hence, avoiding the problems commonly faced when using standard regression with ad hoc methods. Moreover, SEM approach includes data model fit for the hypothesized mediation model providing evidence for the plausibility of the causality assumptions (Gunzler et al., 2013). More importantly, indirect effects of psychological distress on the relationship between socio‐ecological factors and quality of life were assessed using bootstrapping procedures with 5000 bootstrap samples recommended by Hayes (2018). Results of the LVPA were evaluated using the same model‐fit indices for CFA as described previously.
3. RESULTS
3.1. Preliminary analyses
Table 1 presents the descriptive statistics, normality distribution characteristics, and bivariate correlation of study variables. Scores of all the variables met assumptions of normality distribution with skewness and kurtosis consistently < /2/. Results of Pearson correlation showed that safety at home was positively and significantly correlated with TPIs and quality of life, but negatively and significantly correlated with psychological distress. Financial difficulties were positively and significantly correlated with psychological distress but negatively and significantly correlated with quality of life. TPIs was negatively and significantly correlated with psychological distress but positively correlated with quality of life. Psychological distress was negatively and significantly correlated with quality of life. Lastly, financial difficulties were not significantly correlated with safety at home and TPIs.
Table 1.
Descriptive statistics and bivariate correlation of study variables
| Variables | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1. Safety at home | – | ||||
| 2. Financial difficulties | −0.07 | – | |||
| 3. Trust in public institutions | 0.21*** | 0.07 | – | ||
| 4. Psychological distress | −0.28*** | 0.17*** | −0.30*** | – | |
| 5. Quality of life | 0.39*** | −0.27*** | 0.42*** | −0.52*** | – |
| M | 3.66 | 2.62 | 3.55 | 2.32 | 4.58 |
| SD | 0.84 | 1.01 | 1.17 | 0.83 | 0.70 |
| Skewness | −0.57 | 0.05 | −0.24 | 0.79 | −0.70 |
| Kurtosis | 0.48 | −0.31 | −0.53 | 0.43 | 0.63 |
p ≤ 0.001.
3.2. Mediation analysis
To address the hypotheses previously stated, we tested a mediation model consisting of (1) direct effects of safety at home, TPIs, and financial difficulties on psychological distress and quality of life; (2) direct effect of psychological distress on quality of life; and (3) indirect effects of safety at home, TPIs, and financial difficulties on quality of life via psychological distress. In addition, we decided to add a covariation between safety at home and TPIs as informed by the significant bivariate correlation. Results of the path analysis indicated a good data‐model fit: (χ 2 = 4.97, df = 2, p = 0.08; CFI = 0.99, TLI = 0.96, SRMR = 0.02, RMSEA [90% CI] = 0.06 [0.000 − 0.13]).
3.2.1. Direct effects
Figure 1 shows the direct effects of safety at home, TPIs, and financial difficulties on psychological distress and quality of life, as well as psychological distress on quality of life. The direct effects of safety at home (B = −0.27, β = −0.21, SE = 0.05, p ≤ 0.001), TPIs (B = −0.19, β = −0.27, SE = 0.05, p ≤ 0.001), and financial difficulties (B = 0.15, β = 0.18, SE = 0.05, p ≤ 0.001) on psychological distress were found to be significant. This suggests that participants who perceived a greater sense of safety at home and TPIs tend to experience lower levels of psychological distress during the COVID‐19 pandemic. On the other hand, those who reported greater financial difficulties tend to experience higher levels of psychological distress. The squared multiple correlations (R 2) indicate that the combination of the three socio‐ecological variables accounted for approximately 17% of the variance of psychological distress.
Figure 1.
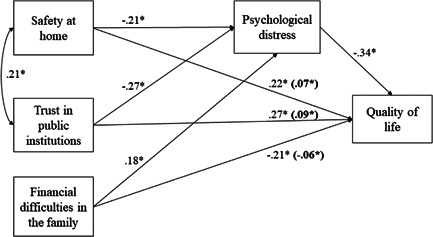
Path model illustrating the partial mediating role of psychological distress on the influence of socio‐ecological factors on quality of life. Reported coefficients are standardized (β) Coefficients in bold represent indirect effects. *p ≤ 0.001
Additionally, direct effects of safety at home (B = 0.19, β = 0.22, SE = 0.05, p ≤ 0.001), TPIs (B = 0.18, β = 0.27, SE = 0.04, p ≤ 0.001), financial difficulties (B = −0.15, β = −0.21, SE = 0.05, p ≤ 0.001), and psychological distress (B = −0.29, β = −0.34, SE = 0.04, p ≤ 0.001) on quality of life were found to be significant. This suggests that participants who perceived a greater sense of safety at home and TPIs tend to experience higher levels of quality of life during the COVID‐19 pandemic. On the other hand, those who reported greater financial difficulties and psychological distress tend to experience a lower level of quality of life. The squared multiple correlations (R 2) indicate that the combination of socio‐ecological variables and psychological distress explained approximately 43% of the variance of quality of life. Overall, the significant direct effects of the three socio‐ecological factors on quality of life confirmed Hypotheses 1 and 2.
3.2.2. Indirect effects
To determine the mediating role of psychological distress on the relationship between socio‐ecological factors and the quality of life of participants during the COVID‐19 pandemic, we adopted a procedure suggested by Hayes (2018) by conducting bootstrapping to generate an accurate sampling distribution that was used for establishing confidence intervals (CIs). Including CIs in estimating mediation effects minimize biases that may be attributed to non‐normality in the sampling distribution of indirect effects (Shrout & Bolger, 2002). Utilizing 5000 bootstrap samples, results indicated that psychological distress partially mediated the positive influence of safety at home (B = 0.06, β = 0.07, SE = 0.02, p ≤ 0.001) and TPIs (B = 0.06, β = 0.09, SE = 0.02, p ≤ 0.001) on quality of life. This implies that participants who perceive greater levels of safety at home and TPIs tend to have lower levels of psychological distress, which, in turn, can contribute to a greater sense of the quality of life. Furthermore, psychological distress partially mediated the negative relationship between financial difficulties (B = −0.04, β = −0.06, SE = 0.02, p ≤ 0.001) and quality of life—implying that participants who reported greater financial difficulties tend to have a higher level of psychological distress, which, in turn, can contribute to a lower sense of the quality of life. Taken together, findings on indirect effects confirmed Hypotheses 3 and 4.
Table 2 summarizes the direct, indirect, and total effects of the mediation model.
Table 2.
Direct, indirect, and total effects of the mediation model
| Type of effect | B | β | SE | BCa 95% CI |
|---|---|---|---|---|
| Safety at home | ||||
| Direct effect | ||||
| Safety at home → QoL | 0.19 | 0.22* | 0.05 | 0.13, 0.32 |
| Indirect effect | ||||
| Safety at home → PD → QoL | 0.06 | 0.07* | 0.02 | 0.03, 0.10 |
| Total effect | 0.25 | 0.29* | 0.05 | 0.19, 0.39 |
| Trust in public institutions | ||||
| Direct effect | ||||
| Trust in public institutions → QoL | 0.18 | 0.27* | 0.04 | 0.20, 0.35 |
| Indirect effect | ||||
| Trust in public institutions → PD → QoL | 0.06 | 0.09* | 0.02 | 0.05, 0.13 |
| Total effect | 0.24 | 0.36* | 0.04 | 0.29, 0.44 |
| Financial difficulties | ||||
| Direct effect | ||||
| Financial difficulties → PD | −0.15 | −0.21* | 0.05 | −0.30, −0.13 |
| Indirect effect | ||||
| Financial difficulties → PD → QoL | −0.04 | −0.06* | 0.02 | −0.09, −0.03 |
| Total effect | −0.19 | −0.27* | 0.05 | −0.36, −0.19 |
Note: Confidence intervals (CIs) based on 5000 bootstrapped samples.
Abbreviations: B, unstandardized coefficients; β, standardized coefficients; PD, psychological distress; QoL, quality of life; SE, standard error.
p ≤ 0.001.
4. DISCUSSION
This study aimed to examine the influence of socio‐ecological factors, such as safety at home, TPIs, and financial difficulties on the quality of life of Filipino adults during the COVID‐19 crisis. Specifically, we tested the mediating influence of psychological distress on the impact of each socio‐ecological factor on the quality of life. Overall, our findings demonstrated that psychological distress operates as an underlying mechanism explaining how safety at home, TPIs, and financial difficulties predict the quality of life of Filipino adults in the days of the COVID‐19 pandemic.
4.1. Key findings
Our first notable finding was that people who have a greater sense of safety at home and higher levels of TPIs during the COVID‐19 crisis reported better quality of life (e.g., a greater sense of connection with friends and families, greater enjoyment of leisure time, and more effective daily functioning), confirming Hypothesis 1 and past research (e.g., Liang, 2016; Mulvey, 2002). Extending these lines of research, this study showed that psychological distress partially mediated the positive impact of safety at home and TPIs on the quality of life—confirming Hypothesis 3. Consistent with this finding, safety at home was found to be negatively associated with COVID‐19 distress among Jewish Israeli adults (Kimhi, Eshel, et al., 2020a). Additionally, recent research found that Chinese adults experienced stress, helplessness, and lower quality of life due to the COVID‐19 pandemic (Zhang & Ma, 2020). Compared with Chinese COVID‐19 patients without depression, patients with depression reported lower levels of quality of life (Ma et al., 2020).
To ensure people's safety, the Philippines has implemented a nationwide community quarantine with varying degrees of tightness based on the spread of cases across regions. Safety protocols, such as work‐from‐home setup and online delivery of business transactions, schoolwork, and suspension of public transportation, among others, were implemented to enhance safety (ECQ and GCQ Guidelines, 2020). Coronavirus is highly contagious and the possibility of being in proximity with COVID‐19 cases may heighten people's stress system posing threat to their home's safety. Our stress systems have evolved to respond to environmental threats, thereby enabling humans to adapt (Allen & Badcock, 2006; Nettle, 2004). The distress that humans experienced during the COVID‐19 pandemic may be an adaptive response to the threat posed by the crisis, thereby explaining why individuals facing lower levels of safety at home reported greater levels of depression and anxiety symptoms, and reduced the quality of life. We note that participants in the current study are all adults and a substantial number are parents. Filipinos have strong family‐centered values embedded in their social sphere (Morillo et al., 2013). Parents are responsible for ensuring their family's safety, especially in times of crisis, such as the COVID‐19 pandemic, potentially explaining why safety at home was associated with levels of depression and anxiety symptoms and better quality of life among Filipino adults.
Another notable finding demonstrated that levels of psychological distress partially mediated the positive impact of TPIs (i.e., police, health, congress, and education departments) on quality of life. This suggests that Filipinos who believe that the public institutions are capable of responding effectively to the COVID‐19 crisis are less likely to experience emotional distress, which, in turn, can lead to a better quality of life. Indeed, recent transnational research involving participants from 58 countries showed that individuals who have higher trust in their government reported lower depression and anxiety during the COVID‐19 crisis (O'Hara et al., 2020). Consistent with our findings on distress as an underlying mechanism predicting quality of life, facing emotional distress during the COVID‐19 pandemic was found to lead to a significant decrease in quality of life among Vietnamese with suspected COVID‐19 symptoms (Nguyen et al., 2020), and among COVID‐19 patients, frontline nurses, and residents in China (An et al., 2020; Ma et al., 2020; Zhang & Ma, 2020). This study indicates that since policies and measures in responding to the COVID‐19 pandemic in the Philippines are created and implemented by public institutions, Filipinos' perceived effectiveness of public institutions' crisis response protocol is a critical protective factor against psychological distress and poor quality of life in the days of a global pandemic. Indeed, building safety and trust could alleviate distress and promote recovery (Li et al., 2011; O'Hara et al., 2020) and may serve as a building block for a better quality of life (Zhang & Ma, 2020).
Our findings supported Hypothesis 2 and consistent with previous research (e.g., Aruta, 2021; Lam et al., 2017; Mulvey, 2002) reporting that individuals who faced financial difficulties reported lower levels of quality of life. Extending this line of research, our findings provided support for Hypothesis 4 by demonstrating that psychological distress partially mediated the negative impact of financial difficulties on quality of life during the COVID‐19 crisis. Similarly, previous research found that financial difficulties directly impact people's quality of life (Lam et al., 2017; Mulvey, 2002) and that quality of life reduction is associated with the psychological distress faced in their daily lives (Floyd et al., 2011; Rebholz et al., 2016). As mentioned above, Filipinos are known to strongly endorse family‐centered values (Morillo et al., 2013). Since the present study involved Filipino adults, those who faced financial losses during the COVID‐19 crisis may have experienced more pronounced negative consequences to their mental health and a lower perception of living conditions because they were the ones responsible for the needs of their families. Indeed, the detrimental impact of financial difficulties on Filipinos' mental health and quality of life may have been more salient due to the impact of the COVID‐19 crisis on the Philippine economy. Nationwide data showed that unemployment skyrocketed at about 18% (7.3 million job losses) in April 2020 (Philippine Statistics Authority, 2020) and a survey revealed that unemployment increased to 46% in July 2020 (Social Weather Stations, 2020). Given the alarming unemployment rate in the country during the pandemic, it is not surprising that Filipinos who face financial losses may experience mental health concerns and a decline in their quality of life.
Putting together, our findings indicate that psychological distress explains why safety at home, financial difficulties, and trust in institutions indirectly impact people's quality of life during the COVID‐19 crisis. Our findings provided support for the proposition of Ecological Systems Theory that microsystem (i.e., factors within an individual's immediate environment) is not the only layer that influences the person, and that the other systems, including mesosystem (family, school, peers, etc.), exosystem (e.g., economic, political, government system, etc), macrosystem (overarching beliefs and values), and chronosystem (dimension of time) can influence the individual including one's quality of life. In particular, the present findings contributed to the literature by demonstrating that Ecological Systems Theory (Bronfenbrenner, 1979) can be applied in explaining the socio‐ecological factors that contribute to people's quality of life in the context of the COVID‐19 crisis in the Philippines. We found that family‐level factors, such as safety at home and financial difficulties in the family, and a societal‐level factor such as TPIs have an indirect impact on the quality of life via an individual factor, psychological distress. Moreover, our most important finding indicated that psychological distress serves as an underlying mechanism that mediates the influence of socio‐ecological factors on quality of life. This illustrates the key role of mental health in impacting people's quality of life in times of great adversities like the COVID‐19 pandemic. Hence, giving sufficient attention to and support for people's mental health in the days of the COVID‐19 crisis may protect them from the pandemic's potential inimical consequences to the overall quality of life.
4.2. Limitations and future research
Through its limitations, this study offers opportunities for future research. First, although the current research determined psychological distress, safety at home, financial difficulties, and TPIs as socio‐ecological factors, other potential factors in the social and ecological environment may directly or indirectly influence the quality of life of Filipinos during the COVID‐19 crisis. Future studies may include community‐level factors, such as the characteristics of a community (e.g., the density of the community and trust in local leaders), which may explain variations in people's quality of life. Second, the current research does not claim that the sample used was representative of Filipinos. Future research may consider replicating the study using a larger sample across regions, socioeconomic status, and developmental stages. For instance, the participants in the present study were mostly young and middle adults. Examining the quality of life of older adults during the COVID‐19 pandemic may be a worthwhile direction given that this age cohort is at higher risk for coronavirus infection. Third, we measured safety at home and financial difficulties using single‐item measures. Future research may utilize more robust measures of safety at home and financial difficulties to increase the accuracy of the findings. Lastly, since the data were collected using an online survey, only Filipinos who have internet access were able to participate in the study. Therefore, future studies may consider gathering data from more representative samples through direct and online survey administration procedures.
4.3. Implications
Our findings have implications for clinical practice and government policies on overall health, in general, and on mental health, in particular, during the time of the pandemic.
4.3.1. Psychosocial support services
Prevention and intervention efforts that integrate individual and ecological factors in addressing mental health vis‐à‐vis improving well‐being may provide mental health professionals with a more holistic view of the psychosocial concerns of individuals. This study identified that people facing issues with safety at home, financial difficulties, and those with lower trust in the government can be more vulnerable to developing depression and anxiety symptoms and poor quality of life. Careful attention to individuals with these specific profiles may inform practitioners in providing more targeted support services and resources to address their mental health concerns.
4.3.2. Policymaking
To mitigate the impact of the COVID‐19 crisis on the mental health of Filipinos, government institutions can focus their efforts on ensuring that Filipinos feel safe at home. For example, strict and effective contact tracing, isolation of suspected COVID‐19 cases, and implementation of precautionary measures at the local community level may increase people's sense of safety, leading to better mental health and quality of life. Efforts in generating income opportunities that fit the contexts of Filipino families during the COVID‐19 crisis are needed as a way to prevent mental health problems and to preserve their quality of life. For instance, creating a barter system and practices locally known as community pantries in local communities may ease the need for finances by exchanging goods and products that people currently possess for the goods needed in the family. Lastly, gaining the trust of the Filipinos in public institutions by providing transparent and well‐planned interventions, and observable management of the crisis is recommended to invigorate people's mental health and quality of life. In summary, government policies that focus on effectively controlling the spread of the new coronavirus, providing income opportunities, and jump‐starting the economy can help decrease Filipinos' psychological distress and facilitate a better quality of life.
5. CONCLUSIONS
Our findings indicate that psychological distress is a psychological mechanism that can partly explain why socio‐ecological factors (i.e., safety at home, financial difficulties, and trust in institutions) impact the quality of life of Filipino adults during the COVID‐19 crisis. People facing threats to home safety, financial instability, and distrust in public institutions in times of crisis are vulnerable to emotional symptoms, and reduced quality of life. These findings, therefore, provide evidence regarding the role of ecological factors in the development of and prevention from mental health concerns and diminished quality of life in times of great adversities such as the COVID‐19 pandemic. Our findings offer several meaningful insights on mental health prevention in clinical practice and policymaking.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
ACKNOWLEDGMENTS
The authors would like to thank Alelie Briones‐Diato for assisting with the data collection.
Aruta, J. J. B. R. , Callueng, C. , Antazo, B. G. , & Ballada, C. J. A. (2022). The mediating role of psychological distress on the link between socio‐ecological factors and quality of life of Filipino adults during COVID‐19 crisis. Journal of Community Psychology, 50, 712–726. 10.1002/jcop.22668
DATA AVAILABILITY STATEMENT
The data associated with this study will be made available from any party upon reasonable request.
REFERENCES
- Aharon, A. A. , Dubovi, I. , & Ruban, A. (2021). Differences in mental health and health‐related quality of life between the Israeli and Italian population during a COVID‐19 quarantine. Quality of Life Research, 30(6), 1675–1684. 10.1007/s11136-020-02746-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen, N. B. , & Badcock, P. B. T. (2006). Darwinian models of depression: A review of evolutionary accounts of mood and mood disorders. Progress in Neuro‐Psychopharmacology and Biological Psychiatry, 30(5), 815–826. 10.1016/j.pnpbp.2006.01.007 [DOI] [PubMed] [Google Scholar]
- An, Y. , Yang, Y. , Wang, A. , Li, Y. , Zhang, Q. , Cheung, T. , Ungvari, G. S. , Qin, M. Z. , An, F. R. , & Xiang, Y. T. (2020). Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID‐19 outbreak. Journal of Affective Disorders, 276, 312–315. 10.1016/j.jad.2020.06.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aruta, J. J. B. R. (2021). Socio‐ecological determinants of distress in Filipino adults during COVID‐19 crisis. Current Psychology, 1–11. 10.1007/s12144-020-01322-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banthia, R. , Moskowitz, J. T. , Acree, M. , & Folkman, S. (2007). Socioeconomic differences in the effects of prayer on physical symptoms and quality of life. Journal of Health Psychology, 12(2), 249–260. 10.1177/1359105307074251 [DOI] [PubMed] [Google Scholar]
- Brand, C. , Barry, L. , & Gallagher, S. (2016). Social support mediates the association between benefit finding and quality of life in caregivers. Journal of Health Psychology, 21(6), 1126–1136. 10.1177/1359105314547244 [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner, U. (1979). The ecology of human development: Experiments by nature and design. Harvard University Press. [Google Scholar]
- Callueng, C. , Aruta, J. J. B. R. , Antazo, B. G. , & Briones‐Diato, A. (2020). Measurement and antecedents of national resilience in Filipino adults during coronavirus crisis. Journal of Community Psychology, 48(8), 2608–2624. 10.1002/jcop.22438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis, L. R. , & Savitz, K. L. (2000). The SCL–90–R and Brief Symptom Inventory (BSI) in primary care. In Maruish M. E. (Ed.), Handbook of psychological assessment in primary care settings (pp. 297–334). Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Derogatis, L. R. , & Spencer, P. M. (1982). The Brief Symptom Inventory (BSI): Administration, and procedures manual‐I. Clinical Psychometric Research. [Google Scholar]
- ECQ and GCQ Guidelines . (2020). Kaayusan (Security) laging isakatuparan. Retrieved from: https://www.covid19.gov.ph/ecq-gcq-guidelines/
- Ferreira, L. N. , Pereira, L. N. , da Fé Brás, M. , & Ilchuk, K. (2021). Quality of life under the COVID‐19 quarantine. Quality of Life Research, 30(5), 1389–1405. 10.1007/s11136-020-02724-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floyd, A. , Dedert, E. , Ghate, S. , Salmon, P. , Weissbecker, I. , Studts, J. L. , Stetson, B. , & Sephton, S. E. (2011). Depression may mediate the relationship between sense of coherence and quality of life in lung cancer patients. Journal of Health Psychology, 16(2), 249–257. 10.1177/1359105310371856 [DOI] [PubMed] [Google Scholar]
- Gunzler, D. , Chen, T. , Wu, P. , & Zhang, H. (2013). Introduction to mediation analysis with structural equation modeling. Shanghai Archives of Psychiatry, 25(6), 390–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes, A. F. (2018). Introduction to mediation, moderation, and conditional process analysis: A Regression‐based approach (2nd ed.). Guilford. [Google Scholar]
- Hayes, A. F. , & Preacher, K. J. (2013). Conditional process modeling: Using structural equation modeling to examine contingent causal processes, Quantitative methods in education and the behavioral sciences: Issues, research, and teaching. Structural equation modeling: A second course (pp. 219–266). IAP Information Age Publishing. [Google Scholar]
- Ikeda, T. , Igarashi, A. , Odani, S. , Murakami, M. , & Tabuchi, T. (2021). Health‐related quality of life during COVID‐19 pandemic: Assessing impacts of job loss and financial support programs in Japan. Applied Research in Quality of Life, 1–17. 10.1007/s11482-021-09918-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Labor Organization . (2020). As job losses escalate, nearly half of global workforce at risk of losing livelihoods. https://www.ilo.org/global/about-the-ilo/newsroom/news/WCMS_743036/lang--en/indexhtm
- International Test Commission . (2018). The ITC guidelines for translating and adapting tests (second edition). International Journal of Testing, 18(2), 101–134. [Google Scholar]
- Kenny, D. A. (2014). Measuring model fit in structural equation modeling. www.davidakenny.net/cm/fit.htm
- Kimhi, S. , & Eshel, Y. (2009). Individual aiknd public resilience and coping with long‐term outcomes of war. Journal of Applied Biobehavioral Research, 14(2), 70–89. 10.1111/j.1751-9861.2009.00041.x [DOI] [Google Scholar]
- Kimhi, S. , & Eshel, Y. (2019). Measuring national resilience: A new short version of the scale (NR‐13). Journal of Community Psychology, 47, 517–528. 10.1002/jcop.22135 [DOI] [PubMed] [Google Scholar]
- Kimhi, S. , Eshel, Y. , Marciano, H. , & Adini, B. (2020a). Distress and resilience in the days of COVID‐19: Comparing two ethnicities. International Journal of Environmental Research and Public Health, 17, 3956. 10.3390/ijerph17113956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimhi, S. , Eshel, Y. , Marciano, H. , & Adini, B. (2020b). A renewed outbreak of the COVID− 19 pandemic: A longitudinal study of distress, resilience, and subjective well‐being. International Journal of Environmental Research and Public Health, 17(21), 7743. 10.3390/ijerph17217743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimhi, S. , Marciano, H. , Eshel, Y. , & Adini, B. (2020a). Resilience and demographic characteristics predicting distress during the COVID‐19 crisis. Social Science & Medicine, 265, 113389. 10.1016/j.socscimed.2020.113389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimhi, S. , Marciano, H. , Eshel, Y. , & Adini, B. (2020b). Recovery from the COVID‐19 pandemic: Distress and resilience. International Journal of Disaster Risk Reduction, 50, 101843. 10.1016/j.ijdrr.2020.101843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimhi, S. , & Shamai, M. (2004). Community resilience and the impact of stress: Adult response to Israel's withdrawal from Lebanon. Journal of Community Psychology, 32(4), 439–451. 10.1002/jcop.20012 [DOI] [Google Scholar]
- Kline, R. B. (2011). Principles and practice of structural equation modeling (3rd ed.). Guilford Press. [Google Scholar]
- Lam, C. L. K. , Guo, V. Y. , Wong, C. K. H. , Yu, E. Y. T. , & Fung, C. S. C. (2017). Poverty and health‐related quality of life of people living in Hong Kong: Comparison of individuals from low‐income families and the general population. Journal of Public Health, 39(2), 258–265. 10.1093/pubmed/fdw046 [DOI] [PubMed] [Google Scholar]
- Li, Y. , Sun, F. , He, X. , & Chan, K. S. (2011). Sense of community and depressive symptoms among older earthquake survivors following the 2008 earthquake in Chengdu China. Journal of Community Psychology, 39(7), 776–785. 10.1002/jcop.20469 [DOI] [Google Scholar]
- Liang, Y. (2016). Trust in Chinese government and quality of life (QOL) of Sichuan earthquake survivors: Does trust in government help to promote QOL? Social Indicators Research, 127, 541–564. 10.1007/s11205-015-0967-9 [DOI] [Google Scholar]
- Lieberoth, A. , Lin, S. Y. , Stöckli, S. , Han, H. , Kowal, M. , Gelpi, R. , Tran, T. P. , Jeftić, A. , Rasmussen, J. , Cakal, H. , Milfont, T. L. COVIDiSTRESS global survey Consortium . (2021). Stress and worry in the 2020 coronavirus pandemic: Relationships to trust and compliance with preventive measures across 48 countries in the COVIDiSTRESS global survey. Royal Society Open Science, 8(2), 200589. 10.1098/rsos.200589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma, Y. F. , Li, W. , Deng, H. B. , Wang, L. , Wang, Y. , Wang, P. H. , Bo, H. X. , Cao, J. , Wang, Y. , Zhu, L. Y. , Yang, Y. , Cheung, T. , Ng, C. H. , Wu, X. , & Xiang, Y. T. (2020). Prevalence of depression and its association with quality of life in clinically stable patients with COVID‐19. Journal of Affective Disorders, 275, 145–148. 10.1016/j.jad.2020.06.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikula, P. , Nagyova, I. , Krokavcova, M. , Vitkova, M. , Rosenberger, J. , Szilasiova, J. , Gdovinova, Z. , Stewart, R. E. , Groothoff, J. W. , & van Dijk, J. P. (2017). Self‐esteem, social participation, and quality of life in patients with multiple sclerosis. Journal of Health Psychology, 22(8), 984–992. 10.1177/1359105315621778 [DOI] [PubMed] [Google Scholar]
- Morillo, H. M. , Capuno, J. J. , & Mendoza, A. M. (2013). Views and values on family among Filipinos: An empirical exploration. Asian Journal of Social Science, 41(1), 5–28. 10.1163/15685314-12341278 [DOI] [Google Scholar]
- Mulvey, A. (2002). Gender, economic context, perceptions of safety, and quality of life: A case study of Lowell, Massachusetts (U.S.A.), 1982–961. American Journal of Community Psychology, 30(5), 655–679. 10.1023/A:1016321231618 [DOI] [PubMed] [Google Scholar]
- Muthén, L. K. , & Muthén, B. O . (1998‐2012). Mplus user's Guide: Statistical Analysis with Latent Variables (7th ed.). Los Angeles, CA Muthén & Muthén. [Google Scholar]
- Nettle, D. (2004). Evolutionary origins of depression: A review and reformulation. Journal of Affective Disorders, 81(2), 91–102. 10.1016/j.jad.2003.08.009 [DOI] [PubMed] [Google Scholar]
- Nguyen, H. C. , Nguyen, M. H. , Do, B. N. , Tran, C. Q. , Nguyen, T. T. P. , Pham, K. M. , Pham, L. V. , Tran, K. V. , Duong, T. T. , Tran, T. V. , Duong, T. H. , Nguyen, T. T. , Nguyen, Q. H. , Hoang, T. M. , Nguyen, K. T. , Pham, T. T. M. , Yang, S. H. , Chao, J. C. J. , & Duong, T. V. (2020). People with suspected COVID‐19 symptoms were more likely depressed and had lower health‐related quality of life: The potential benefit of health literacy. Journal of Clinical Medicine, 9, 965. 10.3390/jcm9040965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- OECD . (2020). Unemployment Rates, OECD‐Updated: September 2020. https://www.oecd.org/newsroom/unemployment-rates-oecd-update-september-2020.htm
- O'Hara, L. , Abdul Rahim, H. F. , & Zhi, Z. (2020). Gender and trust in government modify the association between mental health and stringency of social distancing related public health measures to reduce COVID‐19. A Global Online Survey, 10.1101/2020.07.16.20155200 [DOI] [Google Scholar]
- Philippine Statistics Authority . (2020). Employment situation in April 2020. https://psa.gov.ph/content/employment-situation-april-2020
- Rebholz, W. N. , Cash, E. , Zimmaro, L. A. , Bayley‐Veloso, R. , Phillips, K. , Siwik, C. , Chagpar, A. B. , Dhabhar, F. S. , Spiegel, D. , Bell, B. S. , & Sephton, S. E. (2016). Distress and quality of life in an ethnically diverse sample awaiting breast cancer surgery. Journal of Health Psychology, 23(11), 1438–1451. 10.1177/1359105316659916 [DOI] [PubMed] [Google Scholar]
- Renshaw, T. L. (2018). Psychometrics of the revised College Student Subjective Wellbeing Questionnaire. Canadian Journal of School Psychology, 33(2), 136–149. 10.1177/0829573516678704 [DOI] [Google Scholar]
- Shrout, P. E. , & Bolger, N. (2002). Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods, 7(4), 422–445. 10.1037/1082-989X.7.4.422 [DOI] [PubMed] [Google Scholar]
- Social Weather Stations . (2020). SWS July 3‐6, 2020 National Mobile Phone Survey – Report No. 16: Adult joblessness rises to record‐high 45.5%. http://www.sws.org.ph/swsmain/generalArtclSrchPage/?page=1%26srchprm=%26arttyp=3%26stdtrng=%26endtrng=%26swityp=8
- Theeke, L. A. , Goins, R. T. , Moore, J. , & Campbell, H. (2012). Loneliness, depression, social support, and quality of life in older chronically ill Appalachians. The Journal of Psychology, 146(1‐2), 155–171. 10.1080/00223980.2011.609571 [DOI] [PubMed] [Google Scholar]
- United Nations . (2020). Launch of the policy brief on COVID‐19 and mental health. https://www.un.org/en/coronavirus/mental-health-services-are-essential-part-all-government-responses-covid-19
- Van Bavel, J. J. , Cichocka, A. , Capraro, V. , Sj, H. , Nezlek, J. B. , Griffin, S. M. , Pavlović, T. , Alfano, M. R. , Gelfand, J. , Azevedo, F. , Birtel, M. D. , Cislak, A. , Lockwood, P. , Ross, R. M. , Stoyanova, K. , Abts, K. , Agadullina, E. , Amodio, D. M. , Apps, M. A. J. ,… Boggio, P. S. (2020). National identity predicts public health support during a global pandemic. https://psyarxiv.com/ydt95 [DOI] [PMC free article] [PubMed]
- World Health Organization . (2021a). WHO Coronavirus Disease. (COVID‐19) Dashboard. https://covid19.who.int/
- World Health Organization . (2021b). WHO Coronavirus Disease. (COVID‐19) Dashboard Philippines. https://covid19.who.int/region/wpro/country/ph
- Yamada, Y. , Ćepulić, D. B. , Coll‐Martín, T. , Debove, S. , Gautreau, G. , Han, H. , Rasmussen, J. , Tran, T. P. , Travaglino, G. A. , COVIDiSTRESS Global Survey, C. , & Lieberoth, A. (2021). COVIDiSTRESS Global Survey dataset on psychological and behavioural consequences of the COVID‐19 outbreak. Scientific Data, 8(1), 1–23. 10.1038/s41597-020-00784-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, Y. , & Ma, Z. F. (2020). Impact of the COVID‐19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: A cross‐sectional study. International Journal of Environmental Research and Public Health, 17(7), 2381. 10.3390/ijerph17072381 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data associated with this study will be made available from any party upon reasonable request.


